Abstract
Objectives
The risk factors for maxillary fungal ball are largely unknown. The aim of this study was to determine whether endodontic treatment of maxillary teeth is a risk factor for fungal ball development in the maxillary sinus, and to identify other possible risk factors.
Methods
One hundred and twelve case patients diagnosed with maxillary fungal ball (FB group) and age and gender matched control patients diagnosed with chronic paranasal rhinosinusitis (PNS group) were included to determine associations between previous endodontic treatment and maxillary fungal ball. In addition, we reviewed the dental extraction status of maxillary teeth and the underlying disease in both groups to analyze the other risk factors for maxillary fungal ball.
Results
There were 36.3% of patients in the FB group and 16.1% in the PNS group showed evidence of endodontic treatment on the maxillary teeth (P<0.001). Even after correction for possible confounding factor - the frequency of dental extractions - the rate of endodontic treatment remained higher in the FB group. The mean number of endodontically treated maxillary teeth in the FB group and PNS group were 0.63 and 0.27, respectively (P=0.001). In addition, 20.5% of the patients in the FB group and 13.4% in the PNS group has diabetes mellitus (P=0.154).
Conclusion
Endodontic treatment on maxillary teeth was a significant risk factor for the development of fungal balls in the maxillary sinus.
Keywords: Fungal sinusitis, Fungal ball, Endodontics, Endodontic treatment, Maxillary sinus
INTRODUCTION
A fungal ball of the maxillary sinus is the most common fungal disease that usually develops unilaterally in the maxillary sinus without bony invasion. It is most frequently found in older individuals, especially in their sixties, and has a female preponderance (1). A maxillary fungal ball is frequently diagnosed in patients with prolonged history of symptoms of recurrent maxillary sinusitis, or is incidentally diagnosed on imaging studies, such as computed tomography (CT) or magnetic resonance imaging (MRI). They can also be found during endoscopic sinus surgery (ESS) in patients diagnosed with chronic paranasal rhinosinusitis, even without typical CT findings (2). The treatment of choice for a fungal ball is complete surgical removal by ESS. After the surgery, the recurrence rate is very low (3-5).
Although invasive types of fungal sinusitis are common in immune-compromised patients, non-invasive fungal ball of the maxillary sinus is frequently found in healthy individuals without risk factors for fungal infection. The pathogenesis of the fungal ball of the maxillary sinus remains largely unknown. However, it is generally considered to be related to the inflammatory process associated with dental procedures on the maxillary teeth (6-11). However, confirmation of this correlation has not been reported.
Therefore, a case-control study was performed to determine whether the history of endodontic treatment on maxillary teeth is an independent risk factor for the development of a fungal ball in the maxillary sinus, and to identify other possible risk factors for the development of fungal balls in the maxillary sinus.
MATERIALS AND METHODS
Subjects
Patients diagnosed with fungal balls in the maxillary sinus (FB group), with pathology confirmation after ESS at the Samsung Medical Center between May 1996 and January 2006 were included in the study. Paranasal sinuses and status of the maxillary teeth were evaluated by preoperative CT imaging. A total of 112 patients were enrolled in the FB group; one of the patients had bilateral involvement of the maxillary sinuses. Therefore, 113 maxillary sinuses were analyzed in total in the FB group.
For each case, an age and gender matched control was selected from 1,074 patients diagnosed with chronic paranasal rhinosinusitis (PNS group). All patients had pathology confirmation, during the same period of time. In addition, all paranasal sinuses and the status of the maxillary teeth were evaluated by preoperative CT scans in the PNS group. Therefore, a total of 112 patients were enrolled in the PNS group. Since every patient in the PNS group had bilateral involvement of the maxillary sinuses. Thus, 224 maxillary sinuses were analyzed.
The study protocol was approved by the Institutional Ethics Committee at the Samsung Medical Center, and informed consent was obtained from all patients prior to study enrollment.
Dental evaluation and underlying disease
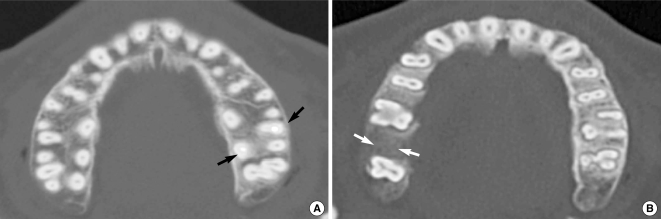
Previous endodontic treatment was assumed if visible hyperdense spots, considered to be root filling material, were identified as shown in Fig. 1A of a CT scan axial image (Fig. 1). For the cases with endodontic treatment or dental extraction, the number of teeth involved was recorded. Teeth included in the study for analysis were: canine, first premolar, second premolar, first molar and second molar, referred to as the maxillary teeth.
Fig. 1.
Evaluation of the maxillary teeth on the axial cut of the osteomeatal unit computed tomography: root filling material used in endodontic treatment showed hyperdense spots along the tooth root in the right first molar, second molar and left first molar (arrows, A); the right first premolar was extracted (arrows, B).
The medical records were reviewed for diabetes mellitus, allergic rhinitis and asthma. Diabetes mellitus was defined as a fasting glucose concentration of 126 mg/dL or higher, and selfreport of the diagnosis of diabetes mellitus. Asthma was diagnosed by clinical symptoms, medical history and pulmonary function testing based on the guidelines of the American Thoracic Society. Patients with asthma had a forced expiratory volume in 1 second (FEV1) of less than 80% of normal, based on methacholine provocation test data. The diagnosis of allergic rhinitis was confirmed by medical history and skin testing, or specific IgE testing with the radioallergosorbent test (RAST).
Statistical analysis
The chi-square test was used to compare endodontic treatment between the FB and PNS groups. Logistic regression analysis was performed for the possible confounding factor of dental extractions. In addition, the chi-square test was performed to compare dental extractions between the two groups. The frequency of endodontic treatment and dental extraction in the FB and PNS groups was compared by the Student t-test. Finally, the chi-square test was performed to compare the frequency of underlying disease, such as diabetes mellitus, allergic rhinitis and asthma. The data were recorded and analyzed using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). A P-value of less than 0.05 was considered to be statistically significance.
RESULTS
Demographic data
Both the FB and PNS groups were consisted of 39 males and 73 females respectively. There were 1.87 times more females than males. The mean age of the FB and PNS groups were 55.5±1.1 and 54.6±0.7, respectively. The age and gender distribution in both groups were: 1 female patient in her twenties, 4 males and 5 females in their thirties, 9 males and 10 females in their forties, 15 males and 24 females in their fifties, 9 males and 28 females in their sixties, and 2 males and 5 females in their seventies.
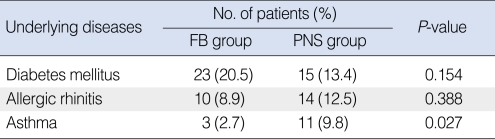
Relevance of underlying disease to fungal ball development
Twenty-three patients (20.5%) in the FB group had diabetes mellitus compared to 15 patients (13.4%) in the PNS group (P=0.154). Ten patients (8.9%) in the FB group had allergic rhinitis compared to 14 patients (12.5%) in the PNS group (P=0.388). Three patients (2.7%) in the FB group had asthma, compared to 11 patients (9.8%) in the PNS group (P=0.027) (Table 1).
Table 1.
Underlying diseases in the FB and PNS group
FB: fungal balls; PNS: paranasal rhinosinusitis.
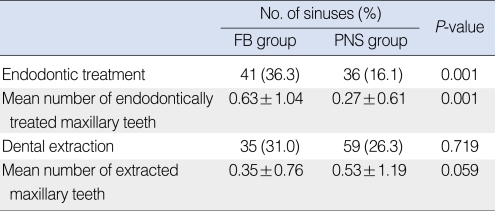
Relevance of endodontic treatment and dental extraction to fungal ball development
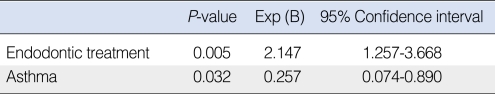
More than one endodontically treated maxillary tooth was found in 41 cases (36.3%) in 113 maxillary sinuses (112 patients) of the FB group, and in 36 cases (16.1%) in 224 maxillary sinuses (112 patients) of the PNS group (P=0.001). The mean number of endodontically treated maxillary teeth in the FB group was 0.63±1.04, compared to 0.27±0.61 in the PNS group (P=0.001). More than 1 extracted maxillary tooth was found in 35 cases (31.0%) from 113 maxillary sinuses of the FB group, and 59 cases (26.3%) from 224 maxillary sinuses of the PNS group. These differences were not statistically significant (P=0.719). The mean number of extracted maxillary teeth in the FB group was 0.35±0.76, compared to 0.53±1.19 in the PNS group (P=0.059). After correction for the effect of asthma through multivariate analysis, the frequency of endodontic treatment was 2.147 times higher in the FB group, compared to the PNS group (P=0.005) (Tables 2 and 3).
Table 2.
Endodontic treatment and dental extraction in the FB and PNS groups
FB: fungal balls; PNS: paranasal rhinosinusitis.
Table 3.
Multivariate analysis of endodontic treatment and asthma in the FB and PNS groups
FB: fungal balls; PNS: paranasal rhinosinusitis.
DISCUSSION
The incidence of fungal sinusitis varies between different countries and is known to account for between 4% and 13% of chronic rhinosinusitis cases (12-15). Despite variable incidence of fungal sinusitis, it is almost certain that one of the important etiologies is the fungus, and the effort to determine possible risk factors of the fungal ball is important for the treatment of chronic rhinosinusitis.
The results of this study showed that the frequency of endodontic treatment of maxillary teeth in the FB group was higher than that in the PNS group. There were 36.3% of patients in the FB group who underwent previous endodontic treatment on adjacent maxillary teeth, regardless of the dental extraction status. This is the first study to confirm that endodontic treatment is more frequently associated with the development of a maxillary fungal ball compared to chronic rhinosinusitis.
The floor of the maxillary sinus or sinus mucosa can be damaged by chemical and physical trauma causing inflammation as a result of endodontic treatment (16-18). Anatomically, the roots of the upper first premolar, second premolar, first molar and second molar are in close contact with the floor of the maxillary sinus and may protrude into the maxillary sinus in some cases (18, 19). Endodontic treatment is performed to cure neural damage resulting from dental caries. During the procedure, a hole is made in the target tooth first and then the nerve and vessels within the root canal are removed, followed by filling with inert materials. These filling materials can extrude during treatment and are frequently introduced into the maxillary sinus beyond the root canal, due to their close anatomical proximity. These procedural complications are common and part of everyday clinical practice. As a result, inflammatory response may involve the sinus mucosa (16-18). Root-filling materials containing zinc oxide-eugenol have been reported to microbiologically promote the growth of Aspergiollosis fumigates (20), and may reduce the protective function of the respiratory epithelium by paralyzing the cilia or by inducing soft tissue hypervascularization and edema (21, 22). Therefore, root filling materials are suspected to be the causative agents of maxillary sinus aspergillosis due to these mechanisms, as well as the anatomical proximity of the maxillary sinus and maxillary teeth (6-10).
In the present study, patients were matched by age and gender to control subjects. Because the development of fungal ball is known to occur more frequently in females than males and in older individuals, especially in their sixties. However, chronic rhinosinusitis is mostly encountered in younger individuals, in contrast to fungal ball development. Also, the tooth mortality rate increases with gingival recession, a loss of gingival attachment and decrease of the remaining teeth with normal aging (1, 23). If there were more elderly subjects included in a group, the frequency of dental extraction rate would escalate. And it could be difficult to compare the frequency of dental extraction and endodontic treatment between the FB and PNS groups. Therefore, randomly selected age and gender matched controls in patients with chronic rhinosinusitis who underwent ESS during the same period as the FB group were compared in the present study.
In addition, the association of dental extraction with the development of maxillary fungal ball was evaluated in this study. Dental extraction is often performed to manage dental caries. The floor of the maxillary sinus can be opened during extraction, which can cause maxillary fungal ball development or rhinosinusitis. The results of the present study showed that the number of dental extractions was not significantly different between the two groups. Therefore, no causal relationship was found between dental extraction and the development of fungal ball in the maxillary sinus.
The frequency of endodontic treatment on maxillary teeth in the present study was somewhat low compared to previous studies. Mensi et al. (11) found that 89.2% of patients with maxillary fungal balls and 36.9% of controls had undergone endodontic treatment on their maxillary teeth. Beck-Mannagetta et al. (6) reported that 44.1% of patients with a maxillary fungal ball had undergone endodontic treatment. These prior results were relatively higher than the findings of the present study. This discrepancy may be due to the difference in study groups selection. In previous studies, subjects were selected from patients visiting a dental clinic, which might have included patients with higher possibility of previous dental treatment. However, in the present study the subjects selected were from one otolaryngology clinic.
The effects of other nasal or systemic diseases on the development of fungal ball or chronic rhinosinusitis were also evaluated. Because fungal ball of the sinus - the most common fungal disease entity - has been found in healthy, immune-competent individuals unlike other types of invasive fungal sinusitis (12, 14, 24). There was no significant difference between the study groups with regard to the frequency of diabetes mellitus or allergic rhinitis, as expected. However, asthma was more frequently found in the PNS group compared to the FB group. Asthma is known to be associated with chronic rhinosinusitis and to aggravate the symptoms of chronic rhinosinusitis (25-28).
Therefore, the results of this study confirm that endodontic treatment on the maxillary teeth can be a significant risk factor for the development of a maxillary fungal ball, independent of prior dental extraction. In the future, the frequency of the endodontic treatment will increase with an aging population. Therefore, clinicians should consider the relevance of endodontic treatment to maxillary fungal ball. In addition, all endodontic instruments and materials should be restricted to the confines of the root canal system during treatment. Also, alternatives to zinc oxide are needed for root filling material during endodontic procedures that may decrease the frequency of fungal ball development in the maxillary sinus. As a result, we can reduce the physical and economic burden associated with fungal ball removal.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Grosjean P, Weber R. Fungus balls of the paranasal sinuses: a review. Eur Arch Otorhinolaryngol. 2007 May;264(5):461–470. doi: 10.1007/s00405-007-0281-5. [DOI] [PubMed] [Google Scholar]
- 2.Dhong HJ, Ha BS, Jung YS, Chung SK, Chang BC. Clinical characteristics of chronic sinusitis with asthma. Korean J Otolaryngol-Head Neck Surg. 2000 May;43(5):514–519. [Google Scholar]
- 3.deShazo RD, Chapin K, Swain RE. Fungal sinusitis. N Engl J Med. 1997 Jul 24;337(4):254–259. doi: 10.1056/NEJM199707243370407. [DOI] [PubMed] [Google Scholar]
- 4.Dufour X, Kauffmann-Lacroix C, Ferrie JC, Goujon JM, Rodier MH, Karkas A, et al. Paranasal sinus fungus ball and surgery: a review of 175 cases. Rhinology. 2005 Mar;43(1):34–39. [PubMed] [Google Scholar]
- 5.Uri N, Cohen-Kerem R, Elmalah I, Doweck I, Greenberg E. Classification of fungal sinusitis in immunocompetent patients. Otolaryngol Head Neck Surg. 2003 Oct;129(4):372–378. doi: 10.1016/S0194-59980301304-4. [DOI] [PubMed] [Google Scholar]
- 6.Beck-Mannagetta J, Necek D. Radiologic findings in aspergillosis of the maxillary sinus. Oral Surg Oral Med Oral Pathol. 1986 Sep;62(3):345–349. doi: 10.1016/0030-4220(86)90019-8. [DOI] [PubMed] [Google Scholar]
- 7.De Foer C, Fossion E, Vaillant JM. Sinus aspergillosis. J Craniomaxillofac Surg. 1990 Jan;18(1):33–40. doi: 10.1016/s1010-5182(05)80601-8. [DOI] [PubMed] [Google Scholar]
- 8.Kopp W, Fotter R, Steiner H, Beaufort F, Stammberger H. Aspergillosis of the paranasal sinuses. Radiology. 1985 Sep;156(3):715–716. doi: 10.1148/radiology.156.3.4023231. [DOI] [PubMed] [Google Scholar]
- 9.Krennmair G, Lenglinger F. Maxillary sinus aspergillosis: diagnosis and differentiation of the pathogenesis based on computed tomography densitometry of sinus concretions. J Oral Maxillofac Surg. 1995 Jun;53(6):657–663. doi: 10.1016/0278-2391(95)90164-7. [DOI] [PubMed] [Google Scholar]
- 10.Legent F, Billet J, Beauvillain C, Bonnet J, Miegeville M. The role of dental canal fillings in the development of Aspergillus sinusitis: a report of 85 cases. Arch Otorhinolaryngol. 1989;246(5):318–320. doi: 10.1007/BF00463584. [DOI] [PubMed] [Google Scholar]
- 11.Mensi M, Piccioni M, Marsili F, Nicolai P, Sapelli PL, Latronico N. Risk of maxillary fungus ball in patients with endodontic treatment on maxillary teeth: a case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Mar;103(3):433–436. doi: 10.1016/j.tripleo.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 12.Blitzer A, Lawson W. Fungal infections of the nose and paranasal sinuses: part I. Otolaryngol Clin North Am. 1993 Dec;26(6):1007–1035. [PubMed] [Google Scholar]
- 13.Lee BJ, Kim H, Kim JH, Kim YJ. Fungal sinusitis: clinical features and treatment outcomes with emphasis on endoscopic sinus surgery. Korean J Otolaryngol-Head Neck Surg. 1998 Mar;41(3):318–322. [Google Scholar]
- 14.Stammberger H. Endoscopic surgery for mycotic and chronic recurring sinusitis. Ann Otol Rhinol Laryngol Suppl. 1985 Sep–Oct;119:1–11. doi: 10.1177/00034894850940s501. [DOI] [PubMed] [Google Scholar]
- 15.Granville L, Chirala M, Cernoch P, Ostrowski M, Truong LD. Fungal sinusitis: histologic spectrum and correlation with culture. Hum Pathol. 2004 Apr;35(4):474–481. doi: 10.1016/j.humpath.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 16.Dodd RB, Dodds RN, Hocomb JB. An endodontically induced maxillary sinusitis. J Endod. 1984 Oct;10(10):504–506. doi: 10.1016/s0099-2399(84)80209-5. [DOI] [PubMed] [Google Scholar]
- 17.Kobayashi A. Asymptomatic aspergillosis of the maxillary sinus associated with foreign body of endodontic origin: report of a case. Int J Oral Maxillofac Surg. 1995 Jun;24(3):243–244. doi: 10.1016/s0901-5027(06)80138-4. [DOI] [PubMed] [Google Scholar]
- 18.Hauman CH, Chandler NP, Tong DC. Endodontic implications of the maxillary sinus: a review. Int Endod J. 2002 Feb;35(2):127–141. doi: 10.1046/j.0143-2885.2001.00524.x. [DOI] [PubMed] [Google Scholar]
- 19.Schuh E, Schmiedl R, Vogel G. Anatomic limits of endosseous dental implantation. Z Stomatol. 1984 Apr;81(2):81–90. [PubMed] [Google Scholar]
- 20.Ross IS. Some effects of heavy metals on fungal cells. Trans Br Mycol Soc. 1975 Apr;64(2):175–193. [Google Scholar]
- 21.Hybbinette JC, Mercke U. A method for evaluating the effect of pharmacological substances on mucociliary activity in vivo. Acta Otolaryngol. 1982 Jan–Feb;93(1-2):151–159. doi: 10.3109/00016488209130866. [DOI] [PubMed] [Google Scholar]
- 22.Reinhold JG. Trace elements: a selective survey. Clin Chem. 1975 Apr;21(4):476–500. [PubMed] [Google Scholar]
- 23.Listgarten MA. Pathogenesis of periodontitis. J Clin Periodontol. 1986 May;13(5):418–425. doi: 10.1111/j.1600-051x.1986.tb01485.x. [DOI] [PubMed] [Google Scholar]
- 24.Kim SW, Park YJ, Kim SW, Kang MG, Joo YH, Cho JH. A clinical analysis of fungal sinusitis. Korean J Otolaryngol-Head Neck Surg. 2005 Mar;48(3):332–337. [Google Scholar]
- 25.Kim HY, So YK, Dhong HJ, Chung SK, Choi DC, Kwon NH, et al. Prevalence of lower airway diseases in patients with chronic rhinosinusitis. Acta Otolaryngol Suppl. 2007 Oct;(558):110–114. doi: 10.1080/03655230701624988. [DOI] [PubMed] [Google Scholar]
- 26.Dhong HJ, Kim HY, Chung YJ, Kim TW, Kim JH, Chung SK, et al. Computed tomographic assessment of chronic rhinosinusitis with asthma. Am J Rhinol. 2006 Sep–Oct;20(5):450–452. doi: 10.2500/ajr.2006.20.2929. [DOI] [PubMed] [Google Scholar]
- 27.Kim HY, Dhong HJ, Chung SK, Chung YJ, Kim MG. Clinical characteristics of chronic rhinosinusitis with asthma. Auris Nasus Larynx. 2006 Dec;33(4):403–408. doi: 10.1016/j.anl.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 28.Dhong HJ, Kim HY, Cho DY. Histopathologic characteristics of chronic sinusitis with bronchial asthma. Acta Otolaryngol. 2005 Feb;125(2):169–176. doi: 10.1080/00016480410015767. [DOI] [PubMed] [Google Scholar]