Abstract
Protein kinase C θ (PKCθ) functions as a core component of the immunological synapse and serves as a key protein in the integrated T-cell antigen receptor (TCR)/CD28-induced signaling cascade leading to T-cell activation. However, the involvement of PKCθ in host-mediated immune responses to pathogens has not been thoroughly investigated. We tested the consequences of PKCθ ablation on the host response to infection by Plasmodium berghei ANKA (PbA). We found that both PKCθ+/+ and PKCθ−/− C57BL/6J mice are susceptible to infection with PbA. However, despite a similar parasite burden, PKCθ+/+ mice had an earlier onset of neurological signs, characteristics of experimental cerebral malaria (ECM), resulting in an earlier death. These mice suffered from an early and pronounced splenomegaly with a concomitant increase in the total number of CD4+ splenic T cells. In contrast, a large proportion of PbA-infected PKCθ−/− mice overcame the acute phase characterized by neurological symptoms and survived longer than PKCθ+/+ mice. The partial resistance of PKCθ−/− mice to ECM was associated with an impaired production of Th1-type cytokines, including gamma interferon and tumor necrosis factor alpha/lymphotoxin-α, which are known to exacerbate symptoms leading to ECM. In addition, PbA infection-induced LFA-1 expression in CD8+ T cells was suppressed in PKCθ-deficient T cells, suggesting a diminished ability to adhere to endothelial cells and sequester in brain microvasculature, which may explain the decrease in neurological symptoms. These data implicate PKCθ in CD4+ Th1+ and CD8+ T-cell-mediated immune responses during PbA infection that contribute to the development of ECM.
Protein kinase C θ (PKCθ) is a member of the PKC family of serine-threonine kinases (5). It is a calcium-independent isoform that relays essential signals downstream of the activated T-cell antigen receptor (TCR) (2). It is unique among the PKC isoforms in its ability to translocate from the cytosol to the center of the immunological synapse of activated T cells, where it colocalizes with the TCR (39, 40). Translocation of PKCθ was found to be regulated by the Lck protein tyrosine kinase and correlated with the catalytic activation of PKCθ by inducible cofactors that are produced along the phosphatidylinositol 3-kinase- and Vav-dependent pathway (59).
Thymocyte development in PKCθ-deficient mice appears to be normal, whereas TCR-induced activation of PKCθ-deficient mature T cells is impaired (55). For example, the proliferative response of antigen-triggered PKCθ-deficient T cells is inhibited, predominantly because of inhibition of both interleukin-2 (IL-2) production and upregulation of CD25, the high-affinity subunit of the IL-2 receptor (55). These defects reflect the impaired TCR-linked signal transduction in PKCθ-deficient T cells, which fail to respond by activation of the AP-1 and NF-κB transcription factors (55). Additional studies, using a second line of PKCθ-deficient mice, demonstrated that activation of the NF-AT transcription factor is also compromised (45). These effects are likely to account for the defect in IL-2 production, since the IL-2 gene promoter possesses critical binding sites for AP-1, NF-κB and NF-AT transcription factors, in addition to the Oct-1 (25).
Recent studies with PKCθ-deficient mice substantiated the in vivo role of PKCθ in T-cell activation. These studies showed that lack of PKCθ differentially affects T-cell differentiation into specific lineages, depending on the nature of the antigen or the immunological insult. For example, PKCθ was found to be essential for the induction of efficient Th2-mediated responses against the helminth Nippostrongylus brasiliensis, or the parasite Leishmania major, and during allergic lung inflammation induced by an inhaled allergen (35, 43, 49). Th1-mediated responses in these three models were almost unaffected (35, 49). In addition, studies in primary PKCθ−/− CD8+ T cells activated by peptide-MHC complexes revealed severe defects in ERK and JNK (but not p38) activation (6), suggesting that PKCθ is also required for optimal Tc-mediated immune responses.
Whereas the in vitro responses of PKCθ-deficient T cells have been thoroughly investigated, the importance of PKCθ in host resistance to pathogens is only at its initial phase.
Human malaria is caused by four different species of Plasmodium, of which P. falciparum is the most virulent. It is one of the seven neglected diseases worldwide, reaching a morbidity of 500 million infections per year and an annual mortality rate of about one million (10). Malaria infection induces innate, humoral, and cell-mediated responses, and the cross talk between these responses affect the outcome of the disease (7, 11, 30, 31, 38, 46, 52, 65). It may range from mild symptoms of synchronous waves of fever and parasite removal, to severe syndromes of anemia, respiratory distress, and cerebral disorders, which are responsible for most malaria-related deaths (7, 11, 23, 30, 31, 38, 46, 52, 58, 65). The reasons for this wide range of responses are not yet clear, but the use of animal models can contribute to the understanding of the malaria-induced pathogenesis. For example, mouse models, which do suffer from some obvious limitations (62), can serve as powerful tools for genetic, molecular, and biochemical analyses of immune-mediated responses to pathogens (28, 29). Moreover, the availability of “knockout” mouse strains lacking genes and proteins that are critical for certain immune responses can help us identify more accurately the role of these molecules in immune resistance to specific pathogens (32, 41, 48, 51).
In the present study we analyzed the potential role of PKCθ in host resistance to infection by the malaria-causing parasite, Plasmodium berghei ANKA (PbA). Utilizing the PKCθ-deficient mouse model, we demonstrated that lack of PKCθ decreases the susceptibility of C57BL/6J mice to PbA infection-induced experimental cerebral malaria (ECM). The lower frequency of ECM correlated with reduced pathological symptoms in the brain and a generalized decrease in Th1 and CD8+ T-cell responses.
MATERIALS AND METHODS
Animals.
C57BL/6J mice were purchased from Harlan Laboratories, Inc. (Jerusalem, Israel). PKCθ-deficient (PKCθ−/−) mice on a 129-C57BL/6J mixed background were a gift from D. Littman (New York University, School of Medicine, New York, NY) (55). The mice were crossed with C57BL/6J mice for 12 generations to create a congenic line of C57BL/6J-PKCθ−/− mice. Wild-type (PKCθ+/+) and PKCθ-deficient (PKCθ−/−) littermates were obtained by breeding of PKCθ+/− heterozygous mice. Mice were maintained in a temperature (22 ± 1°C)- and humidity-controlled animal facility on a 12-h light/dark cycle. All studies conformed to the principles outlined by the Animal Welfare Act and the National Institutes of Health guidelines for the care and use of animals in biomedical research. Mouse genotyping was performed by PCR amplification, using tail tip genomic DNA as a template. DNA was amplified using the sense primers—5′-TAAGAGTAATCTTCCAGAGC-3′ (wild type) and 5′-ACTGCATCTGCGTGTTCGAA-3′ (neomycin; knockout)—and a common antisense primer 5′-TTGGTTCTCTTGAACTCTGC-3′, designed to amplify 426 and 600 bp, for wild-type and knockout mice, respectively. After 4 min of initial denaturation at 95°C, the PCR conditions consisted of 35 cycles of 94°C for 1 min, 56°C for 45 s, and 72°C 1 min. DNA products were resolved on a 1.0% agarose gel for 30 min and visualized with ethidium bromide.
Parasites.
PbA strains were maintained in vivo by serial passage of PbA-parasitized red blood cells (PbA-pRBC; 5 × 104/mouse) into C57BL/6J mice. This clone was selected based on its capacity to induce ECM in C57BL/6J mice. Experiments were initiated by intraperitoneal injection of 5 × 104 PbA-pRBC in 100 μl of phosphate-buffered saline (PBS) into 6- to 8-week-old PKCθ+/+ and PKCθ−/− male and female C57BL/6J mice. After infection, mortality was monitored daily, and parasitemia was assessed every second or third day by light microscopy of Giemsa stained blood smears. Mice were determined as having ECM if they displayed the characteristic neurological signs and died within 11 days postinfection (p.i.).
Histology.
Mice were deeply anesthetized until cessation of breathing. Brains and spleens were removed, fixed in a 4% formaldehyde solution for 24 h, and embedded in paraffin. Tissue sections (5-μm thick) were prepared and stained with hematoxylin and eosin according to standard procedures.
Preparation of splenic mononuclear cells.
Spleen cells from control and infected mice were used in a proliferation assay, cytokine production assay, or surface staining followed by flow cytometry. Spleens were removed aseptically and placed in complete medium (RPMI supplemented with 2% heat-inactivated fetal calf serum, 2 mM l-glutamine, 50 U of penicillin/ml, and 50 μg of streptomycin/ml (all from Biological Industries, Beit Haemek, Israel). A single-cell suspension was obtained by mincing off the spleen and passing the disrupted tissue through a 70-μm-pore-size nylon strainer (BD Falcon). Erythrocytes were lysed by using Sigma's RBC lysing buffer. The cells were washed twice in fresh medium and filtered to remove residual cell debris. Cell viability was determined by trypan blue exclusion and was always >90%.
Proliferation assays.
Spleen cells were cultured in triplicate wells of 96-well flat-bottom tissue culture plates (Costar, Cambridge, MA), in complete medium, at a concentration of 4 × 105 cells/200 μl/well. The cells were cultured in the presence of 2.5 μg of concanavalin A (ConA)/ml, 10 μg of lipopolysaccharide (LPS)/ml, 100 ng of phorbol myristate acetate (PMA)/ml combined with 200 ng of ionomycin/ml, 10 μg of phytohemagglutinin (PHA)/ml (all from Sigma Chemical, Israel), or soluble anti-CD3 (ascites, Armenian hamster monoclonal antibody [MAb] clone 145-2C11 [dilution, 1:500]) in the presence of a soluble anti-CD28 MAb (ascites [dilution, 1:250]). Cells cultured in medium alone were used as background controls. All cultures were incubated in a humidified chamber containing 5% CO2 at 37°C for 3 days. Cultures were pulsed with 1 μCi of [methyl-3H]thymidine/well for the final 6 h of culture. Cells were harvested by using an automated cell harvester (Connectorate AG, Switzerland), and filter-bound radioactivity was measured by using a Wallac 1409 DSA liquid scintillation counter (Wallac, Turku, Finland).
In vitro production of cytokines by mitogen-stimulated spleen cells.
Spleen cells were adjusted to 3 × 106/ml in complete medium, and 1-ml aliquots were cultured in triplicates in wells of 24-well tissue culture plates in the presence or absence of 2.5 μg of ConA/ml. Cultures were incubated at 37°C in a humidified 5% CO2 incubator for 48 h, after which supernatants were collected and stored at −20°C. The levels of IL-2, IL-10, tumor necrosis factor alpha (TNF-α), and gamma interferon (IFN-γ) were determined in triplicates by using commercial enzyme-linked immunosorbent assay (ELISA) kits (IL-2 [BD Biosciences Pharmingen, San Diego, CA], IL-10 and TNF-α [BioSource International, Inc., Camarillo, CA], and IFN-γ [R&D Systems, Minneapolis, MN]) according to the manufacturer's instructions. The optical absorbance was read at 405 nm using a microplate reader (Thermo Fisher Scientific, Waltham, MA) with a reference wavelength of 492 nm. Cytokine concentrations were calculated in pg/ml using standard curves obtained for recombinant mouse cytokines. Otherwise, results were presented as relative units of optical density.
Serum cytokine assay.
Blood samples were collected from eight to ten control uninfected or PbA-infected mice at 2, 4, 6, and 12 days p.i. The serum was separated and stored at −20°C until used. Serum levels of IFN-γ, TNF-α, IL-6, and IL-10 cytokines and monocyte chemoattractant protein 1 (MCP-1)/CCL2 chemokine were quantified in duplicates using a Quansys Q-Plex multiplex ELISA array, according to the manufacturer's instructions (Quansys Biosciences, Logan, UT). Quantification of chemiluminescence and data analysis were performed by using the Q-View imaging system and Q-View software.
Flow cytometry analysis.
Spleen cells (106/sample) were washed and resuspended in staining buffer (PBS with 1% bovine serum albumin and 0.01% sodium azide). Fc receptors were blocked by incubation with optimal amount of anti-mouse CD16 and CD32 receptor (FcRIII and FcRII) antibodies (eBioscience, San Diego, CA) for 15 min on ice. Cell staining was performed on ice by 30 min of incubation in the presence of different combinations of antibodies, including Pacific Blue-conjugated anti-CD3; biotin-conjugated anti-CD3, followed by 30 min of additional incubation with streptavidin-conjugated phycoerythrin-Cy5; Pacific Blue-conjugated anti-CD4; fluorescein isothiocyanate (FITC)-conjugated anti-lymphocyte function-associated antigen 1 (LFA-1); phycoerythrin (PE)-conjugated anti-CD8α (all from eBioscience San Diego, CA); and PE-conjugated anti-B220 (Pharmingen/Becton Dickinson, San Jose, CA). Cells were washed twice in staining buffer, resuspended in 200 μl of staining buffer, and analyzed on a FACS Canto II flow cytometer (BD Bioscience). The staining intensity was presented as the mean fluorescence intensity (MFI), and all data were analyzed by using FlowJo software from Tree Star.
Statistical analysis.
Values of all experiments performed in triplicates were expressed as mean ± the standard errors of the mean (SEM), unless otherwise noted. The statistical significances of differences between groups were calculated by using the two-tailed Student t test and, differences were considered significant when P values were <0.05. Kaplan-Meier curves show the overall survival of PKCθ+/+ and PKC−/− mice, which were compared by using the Mantel-Cox version of the log-rank test.
RESULTS
Lack of PKCθ reduces the mortality rate of PbA-infected C57BL/6J mice without affecting the course of parasitemia.
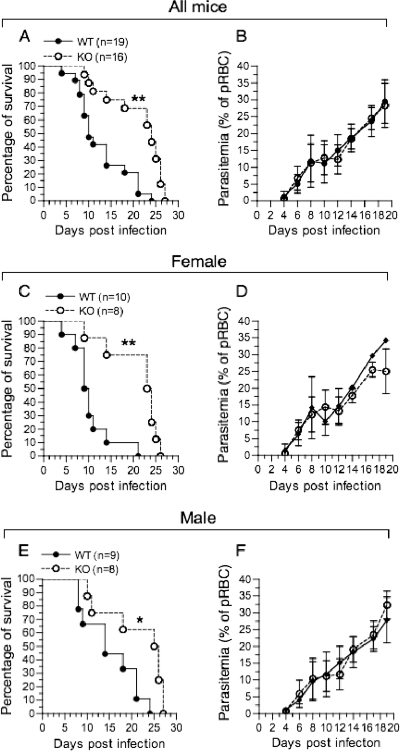
PKCθ+/+ and PKCθ−/− C57BL/6J mice were infected with PbA-pRBC, and the course of parasitemia and survival rates were monitored. Both wild-type and PKCθ-deficient mice succumbed to the infection (Fig. 1 A). However, the mortality rate was faster in PKCθ+/+ mice, where 18 of 19 mice (95%) died of malaria within 21 days p.i., whereas only 5 of 16 (31%) mice in the PKCθ−/− group succumbed at this time point (Fig. 1A). Furthermore, the majority of the PKCθ+/+ mice (59%) died during the acute phase of infection (days 4 to 11 p.i.), with symptoms characteristics of CM, including convulsions, paralysis, and loss of coordination. In contrast, only 3 of 16 PKCθ−/− mice (19%) died within 11 days p.i., exhibiting ECM symptoms (Fig. 1A), whereas the majority of PKCθ−/− mice overcame the acute phase of ECM and died of severe anemia at later time points.
FIG. 1.
PKCθ-deficient mice exhibit extended survival after infection with PbA. Six-to eight-week-old PKCθ+/+ mice (WT; n = 19) and PKCθ−/− (KO; n = 16) C57BL/6J mice were injected intraperitoneally with 5 × 104 PbA-infected RBC and monitored daily for mortality. The left panel shows Kaplan-Meier survival curves of all PKCθ+/+ (solid lines) and PKCθ−/− mice (dashed lines) tested (A), whereas panels C and E show results obtained with female and male mice, respectively. The right panels show the extent of parasitemia that was determined every other day for all mice tested (B) or for female (D) and male (F) mice. Kaplan-Meier curves of overall survival were compared by using the Mantel-Cox version of the log-rank test. Parasitemia values represent means ± the standard deviation (SD). The percentages of infected RBC in PKCθ+/+ and PKCθ−/− mice at each time point show no statistical difference (P > 0.5 at each time point). The data represent one of three independent experiments performed with a minimum of 13 mice per group. pRBC, parasitized red blood cells. *, P < 0.05; **, P < 0.01.
Gender-based differences in resistance to parasite infection have been observed in mice (27, 63), which led us to analyze whether the relative resistance of PKCθ−/− mice to PbA infection is gender dependent. Comparison of mortality rates revealed that the relative resistance of PKCθ−/− mice to PbA infection is found both in female and male mice (Fig. 1C and E, respectively).
The increased resistance of PKCθ−/− mice to PbA infection is evident despite the fact that the course of the infection in both mouse strains was comparable (Fig. 1B, D, and F).
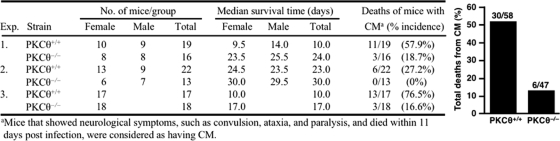
A summary of the results obtained in three independent experiments is shown in Fig. 2. It demonstrates that 30 of 58 PKCθ+/+ mice (51.7%), compared to only 6 of 47 PKCθ−/− mice (12.8%) died within the first 11 days after PbA infection, the time frame considered to represent death caused by ECM (14, 19).
FIG. 2.
Median survival time and incidence of deaths from ECM in PbA-infected PKCθ+/+ and PKCθ−/− C57BL/6J mice.
Histological examination of brain tissue and lungs.
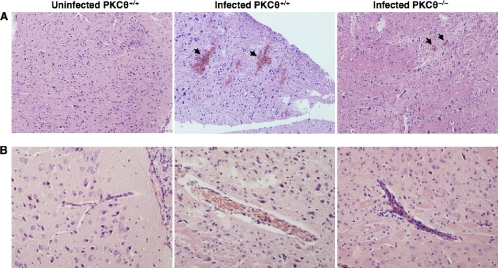
The central theory of the pathogenesis of cerebral malaria (CM) argues that adherence and sequestration of pRBC, immune cells (particularly monocytes), and platelets in brain microvasculature (53, 57), together with endothelial cell damage (1), lead to blood vessel obstruction, hemorrhages, and hypoxia of the brain parenchyma (58). To test whether PKCθ may affect the pathogenesis of ECM, histological sections of brains of PbA-infected PKCθ+/+ and PKCθ−/− mice were compared. Brains of PbA-infected PKCθ+/+ mice displayed pathological changes, including extensive petechial hemorrhages, predominantly in the brain cortex (Fig. 3 A) and cerebellum (data not shown). They also demonstrated distended cerebral vessels with disruption or loss of endothelial cells, and lumens that are packed with erythrocytes and mononuclear cells (Fig. 3B). These pathological changes were less prominent and less frequent in the brains of PbA-infected PKCθ−/− mice. The majority of blood vessels observed in brain sections of PbA-infected PKCθ−/− mice were intact with well-defined endothelial lining, and intravessel aggregates of nucleated cells were rarely found (Fig. 3B).
FIG. 3.
PbA-infected PKCθ−/− mice display reduced pathological changes in the brain. Brains were removed from control uninfected or PbA-infected PKCθ+/+ and PKCθ−/− mice 7 days postinfection, fixed in paraformaldehyde, and embedded in paraffin, and 5-μm sections were stained with hematoxylin and eosin. (A) Representative sections of the cortex of a control PKCθ+/+ mouse and PbA-infected PKCθ+/+ and PKCθ−/− mice, demonstrating hemorrhagic foci (arrows) in the brain cortex (magnification, ×100). (B) Increased accumulation of erythrocytes and leukocytes in cerebral vessels of PKCθ+/+ mice (magnification, ×200). The results are representative of two independent experiments, with four mice analyzed per group.
Acute pulmonary edema in malaria-infected individuals is a frequent pathological symptom, secondary to sequestration of inflammatory cells and pRBC in microvessels of the lung tissue (44). Gross examination of lungs from infected mice revealed severe pulmonary edema in all four PKCθ+/+ mice tested on day 12 p.i., whereas only mild signs of edema were observed in all four PbA-infected (day 12 p.i.) PKCθ−/− mice (data not shown).
Analysis of the effect of PbA infection on spleen size and morphology in PKCθ+/+ and PKCθ−/− mice.
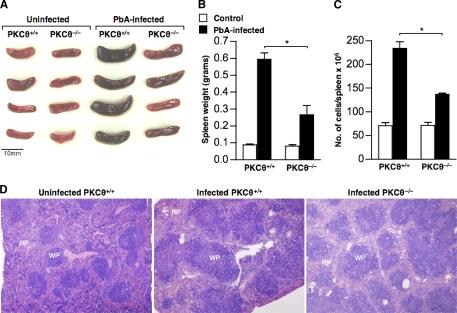
The spleen has a major role in host defense against malaria by clearing pRBC from the bloodstream (13). Since malaria infection is often associated with splenomegaly that may also reflect an altered regulation of T cells, we analyzed the consequences of ablation of PKCθ on the development of hyperplasia of the spleen. Control and PbA-infected PKCθ+/+ and PKCθ−/− mice were killed on day 7 p.i., and the spleens were examined macroscopically and weighed. The results showed that although PbA infection induced splenomegaly in both strains (Fig. 4 A), the increase in spleen size and weight in PKCθ+/+ mice (80 ± 12 mg/spleen in uninfected mice versus 595 ± 54 mg/spleen in infected mice) was significantly higher than in PKCθ−/− mice (88 ± 7.5 mg/spleen in uninfected mice versus 266 ± 75 mg/spleen in infected mice) (Fig. 4B). Differences in spleen weight correlated with differences in the total number of nuclear cells per organ (Fig. 4C). Low-magnification histological examination of spleen architecture revealed significant hyperplasia of lymphoid follicles and enlarged germinal centers in the white pulp of PbA-infected PKCθ+/+ mice (4.2-fold increase in the average area of germinal centers). In contrast, germinal centers in the spleens of PbA-infected PKCθ−/− mice were less affected (2.15-fold increase), showing only initial phases of hyperplasia (Fig. 4D).
FIG. 4.
PbA infection induces splenomegaly which is reduced in PKCθ−/− mice. Spleens were removed from control and Pb-A-infected PKCθ+/+ and PKCθ−/− mice (7 days p.i.; 4 mice/group), photographed (A), and weighed (B). A single cell suspension was prepared from individual spleens, and the total number of nucleated cells was determined (C). The data in panels B and C are means ± the SEM of eight individual mice per group pooled from two similar experiments. (D) Spleens from uninfected and infected mice (four/group) were fixed in paraformaldehyde and embedded in paraffin. Five-micrometer sections were stained with hematoxylin and eosin and examined by using a light microscope (magnification, ×40). A single representative section is shown from uninfected and infected PKCθ+/+ mice and infected PKCθ−/− mice. The white pulp (WP) of the spleen represents the lymphatic area, including germinal centers, and the red pulp (RP) is the site of destruction of senescent red blood cells. *, P < 0.05 (PKCθ+/+ versus PKCθ−/−) as determined by Student t test.
Quantitative analysis of T and B cells in the spleens of uninfected control and PbA-infected PKCθ+/+ and PKCθ−/− mice.
Both B and T lymphocytes play a role in the immune response against the blood-stage forms of different malarial species (36, 47, 60). These cell types may also be involved in the physiological responses leading to the malaria-induced splenomegaly. Furthermore, the PbA infection-induced splenomegaly may reflect a hyperproliferative response of one or more selected subpopulations of splenocytes. Because PKCθ was found to negatively regulate PbA infection-induced splenomegaly, we tested whether the lack of PKCθ has a general effect on the total number of cells in the spleen, or perhaps a selective effect, on one or more defined spleen cell subpopulations.
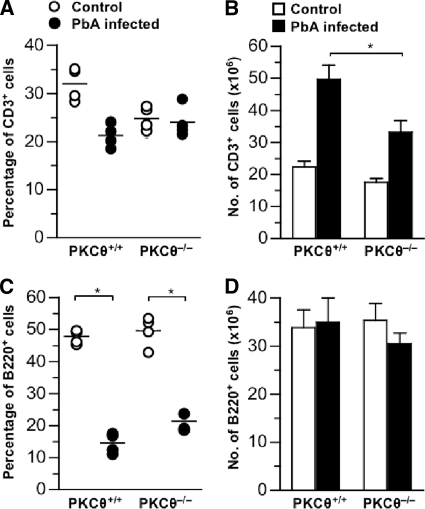
We therefore determined the effect of PbA infection on the proportion and total numbers of splenic B and T cells in PKCθ+/+ and PKCθ−/− mice on day 12 p.i. (Fig. 5). Similar proportions and total numbers of B220+ B cells were found in the spleens of uninfected PKCθ+/+ and PKCθ−/− mice (Fig. 5C and D, respectively). The proportions of splenic CD3+ T cells were slightly higher in PKCθ+/+ mice, but the total number of T cells in the spleens of the two mouse strains was statistically insignificant (Fig. 5A and B). The total number of splenic B220+ B cells in either PKCθ+/+ or PKCθ−/− mice was not significantly altered after infection with PbA, but their percentage was reduced in the PbA-infected hyperplastic spleens (Fig. 5C and D). An opposite effect was observed when T cells were analyzed: while their percentage was slightly reduced (in PKCθ+/+ mice) or not altered (in PKCθ−/− mice), their total number was roughly doubled (Fig. 5A and B).
FIG. 5.
Quantitative analysis of T and B lymphocytes in the spleens of control and PbA-infected PKCθ+/+ and PKCθ−/− mice. Control uninfected mice or PbA-infected PKCθ+/+ and PKCθ−/− mice (four per group) were prepared in parallel to the mice in Fig. 2, experiment 2. Spleens were removed on day 12 p.i., and the spleen cells were stained with PE-conjugated anti-B220 and Pacific Blue-conjugated anti-CD3 antibodies, followed by FACS analysis. The data show the percentages of CD3+ T lymphocytes (A) and B220+ B lymphocytes (C) per spleen, respectively, and the mean absolute numbers of CD3+ T lymphocytes (B) and B220+ B lymphocytes (D) per spleen. The data are means ± the SEM from four individual mice per group and represent one of two independent experiments. *, P < 0.05 (PKCθ+/+ versus PKCθ−/−) as determined by a Student t test.
The fact that infection with PbA induced a dramatic increase in the total number of splenocytes could not be accounted for by the relatively small increase in the number of lymphocytes suggests that the main reason for the PbA-induced splenomegaly is the accumulation of monocytes/macrophages, considered to be the hallmark of malaria infection.
The in vitro proliferative response of splenic T cells from PbA-infected PKCθ+/+ and PKCθ−/− mice is severely impaired.
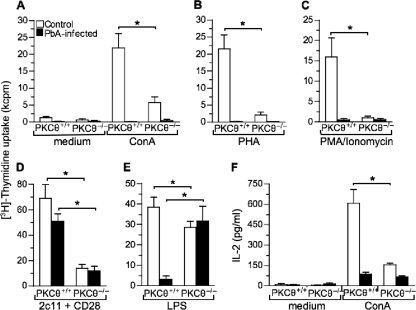
Our results indicated that the PbA infection-induced splenomegaly in PKCθ+/+ mice is in direct correlation with an increase in the total number of splenic T cells and that both phenomena are partially ameliorated in the absence of PKCθ (Fig. 3 and 4). In addition, published data demonstrated that PKCθ−/− T cells are defective in proliferative responses and IL-2 production following TCR stimulation (45, 55). We therefore tested the effect of infection with PbA on the mitogen responses of splenic lymphocyte of both strains. Spleen cells from control or PbA-infected mice were cultured in the presence or absence of different mitogens for 3 days, and the incorporation of [methyl-3H]thymidine to the cells during the last 6 h of culture was measured. PKCθ−/− spleen cells were found to be impaired in their proliferative response to ConA, PHA, PMA+ionophore, and anti-CD3 plus anti-CD28 MAbs (Fig. 6 A to D). Splenocytes from PbA-infected mice of both strains were almost anergic to most mitogens tested (Fig. 6A to C), except for the response to anti-CD3 plus anti-CD28 MAbs, whereby the decreases in the proliferative response were only 26.1 and 14.1% lower for PKCθ+/+ and PKCθ−/− cells, respectively (Fig. 6D).
FIG. 6.
In vitro proliferation and IL-2 production by spleen cells from control and PbA-infected PKCθ+/+ and PKCθ−/− mice in response to mitogenic stimuli. Spleen cells from control or PbA-infected PKCθ+/+ and PKCθ−/− mice (day 12 p.i.) were cultured in wells of microtiter plates (4 × 105 cells/200 μl/well) in triplicates in the presence of medium only or 2.5 μg of ConA/ml (A), 10 μg of PHA/ml (B), 100 ng of PMA/ml plus 200 ng of Ionomycin/ml (C), anti-CD3 (ascites, 145-2C11 [dilution, 1:500]) plus anti-CD28 (ascites [dilution, 1:250]) (D), or 10 μg of LPS/ml (E). After 3 days in culture, cells were pulsed with 1 μCi of [methyl-3H]thymidine/well for 6 h and then harvested, and [3H]thymidine incorporation was determined for each group. The data are presented in a bar graph as means ± the SD. (G) IL-2 levels in control and ConA-stimulated cell culture supernatants were determined by ELISA. The data are presented as means ± the the SD of four mice per group and are representative of two independent experiments. *, P < 0.05 (PKCθ+/+ versus PKCθ−/−) as determined by Student t test.
The proliferative response of spleen cells of both mouse strains to the B-cell mitogen, LPS, differed only slightly (Fig. 6E), a finding consistent with the observation that B cells do not express PKCθ (37). However, the proliferative response of splenic B cells from PKCθ+/+ mice dropped by 91% after PbA infection, whereas that of cells from PKCθ−/− mice was not changed. The implications of this finding for the differential resistance of PKCθ+/+ and PKCθ−/− mice to PbA infection were not clear. However, it is possible that congenital absence of PKCθ is compensated, perhaps by other PKC isoforms, which enables PKCθ−/− T cells assist B cells via a PKCθ-independent mechanism. This is in contrast to B cells in wild-type mice, which are dependent for their functions on PKCθ-expressing T helper cells. Once the T cells are altered due to PbA infection, the responses of B cells of wild-type mice are downregulated, whereas those of PKCθ−/− B cells are not affected.
Because IL-2 is an essential growth factor for T-cell proliferation, we further analyzed the ability of splenic lymphocytes from PKCθ+/+ or PKCθ−/− mice to produce IL-2 in response to ConA stimulation. Deficiency in PKCθ resulted in ∼80% inhibition of IL-2 production after cell stimulation with ConA (155.2 ± 12.3 pg/ml in PKCθ−/− splenocytes versus 608.5 ± 102 pg/ml in PKCθ+/+ splenocytes; P < 0.01) (Fig. 6F). Mouse infection with PbA decreased the amount of IL-2 produced by splenic lymphocytes of PKCθ+/+ and PKCθ−/− mice by ∼85% (86 ± 14.2 pg/ml) and ∼56% (66.8 ± 8.4 pg/ml), respectively (Fig. 6F). The reduced IL-2 levels produced by uninfected PKCθ−/− splenocytes and after PbA infection of both strains correlate with the reduced proliferative responses of the splenocytes to T-cell mitogens (Fig. 6A to C).
Alterations in cytokine expression pattern in PbA-infected PKCθ+/+ and PKCθ−/− mice and correlation with the differential susceptibility of the mice to ECM.
To analyze whether PKCθ has a role in promoting Th1 or Th2-type immune responses in PbA-infected mice and test whether it may affect the balance between Th1- and Th2-mediated immune responses, we analyzed cytokine production by PKCθ+/+ and PKCθ−/− mice by using two complementary assays.
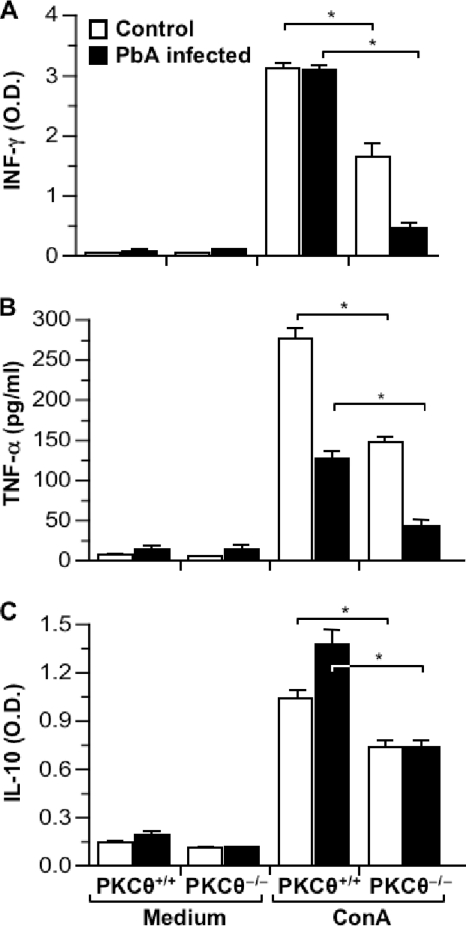
In the first assay, spleen cells from uninfected and PbA-infected mice were cultured in vitro in the presence of ConA, and their ability to respond by cytokine production and secretion was determined on the culture supernatants, using an ELISA. Both PKCθ+/+ and PKCθ−/− splenocytes responded to ConA by producing high levels of IFN-γ and TNF-α (Th1-type cytokines) and IL-10 (Th2-type cytokine) (Fig. 7 A, B, and C, respectively). However, cytokine expression levels were ca. 30 to 50% lower in PKCθ−/− splenocytes. The effect of PbA infection on the production of these cytokines in PKCθ+/+ and PKCθ−/− mice varied: while a similar drop in TNF-α was observed in the two strains (Fig. 7B), there was an increase in the level of IL-10 produced by PKCθ+/+ splenocytes, whereas no change was observed in PKCθ−/− cells (Fig. 7C). The most pronounced effect of infection was observed with regard to IFN-γ: whereas no change was observed in PKCθ+/+, a sharp decrease occurred in PKCθ−/− cells (Fig. 7A).
FIG. 7.
In vitro production of IFN-γ, TNF-α, and IL-10 by spleen cells from control mice and PbA-infected PKCθ+/+ and PKCθ−/− mice in response to ConA stimulation. Spleen cells from control or PbA-infected PKCθ+/+ and PKCθ−/− mice (day 12 p.i.) were cultured in 24-well plates (3 × 106cells/1.6 ml/well) in the presence or absence of 2.5 μg of ConA/ml. Culture supernatants were collected after 48 h, and the levels of IFN-γ (A), TNF-α (B), and IL-10 (C) were quantified by ELISA. The data are means ± the SEM of spleen cells from four individual mice per group. *, P < 0.05 (PKCθ+/+ versus PKCθ−/−) as determined by Student t test.
These results demonstrate a general diminished cytokine response of PKCθ-deficient spleen cells, which is even more profound following the infection by PbA. The reduced production of cytokines by splenocytes of PbA-infected PKCθ−/− mice may reflect the reduction in total number of T cells observed in their spleens (in comparison to PbA-infected PKCθ+/+ mice), or perhaps a PKCθ-dependent and PbA infection-modulated regulatory mechanism that affect cytokine production.
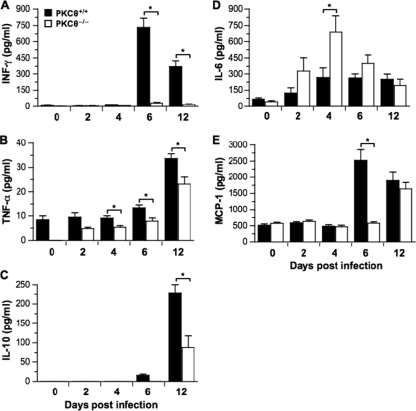
In the second assay, cytokine levels in the serum of control and infected mice were quantified by using the Q-Plex multiplex ELISA array. The IFN-γ levels in both strains were negligible during the first 4 days p.i. (Fig. 8 A). In mice of both strains an increase in IFN-γ level was observed on day 6 p.i, which was ∼23-fold higher in PKCθ+/+ (732.7 ± 83.6 pg/ml) versus PKCθ−/− (31.3 ± 8.3 pg/ml) mice. Despite an ∼50% reduction in the level of IFN-γ in PKCθ+/+ mice on day 12 p.i., it was still significantly higher than that in PKCθ−/− mice (371.2 ± 52.1 pg/ml versus 17.8 ± 5.4 pg/ml, respectively) (Fig. 8A).
FIG. 8.
Time kinetics of serum cytokine levels after PbA-infection of PKCθ+/+ and PKCθ−/− mice. Peripheral blood was collected from control uninfected or PbA-infected PKCθ+/+ and PKCθ−/− mice on days 2, 4, 6, and 12 p.i. with PbA. The serum levels of IFN-γ (A), TNF-α (B), IL-10 (C), IL-6 (D), and MCP-1 (E) were quantified by Q-Plex array, and the results are presented in a bar graph. Values are mean ± the SEM of four mice per group. *, P < 0.05 (PKCθ+/+ versus PKCθ−/−) as determined by Student t test.
TNF-α levels increased gradually with time in both strains, reaching a maximal response on day 12 p.i, and were higher in PKCθ+/+ mice at all time points tested (Fig. 8B).
IL-10 was detected on day 6 p.i. only in PKCθ+/+ mice, followed by a sharp increase in both strains on day 12 p.i. (Fig. 8C). However, they were significantly higher in PKCθ+/+ mice (227.6 ± 22.5 pg/ml versus 88.0 ± 29.4 pg/ml).
We tested serum levels of two additional soluble mediators, IL-6 and MCP-1, both of which were shown to be produced in excess during malaria infection (20, 34). PbA infection increased circulating IL-6 and MCP-1 levels in both mouse strains (Fig. 8D and E). However, the overall IL-6 response of PKCθ−/− mice was significantly higher than that of PKCθ+/+ mice, suggesting that the decrease in the cytokine response of PKCθ−/− mice (Fig. 8A to C) is not a general phenomenon.
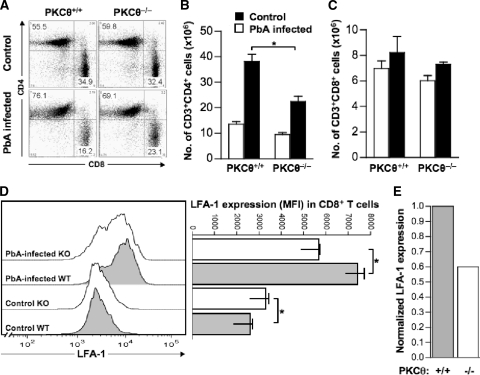
Impaired upregulation of LFA-1 in PKCθ−/− CD8+ splenic T cells after mouse infection with PbA.
CD4+ and CD8+ T cells are involved in the pathogenesis of ECM (22, 64). Our studies revealed significant increases in the total number of spleen cells in PbA-infected mice (Fig. 4C), which reflected a predominant increase in CD3+ T cells that was more pronounced in PKCθ+/+ mice (Fig. 5B). To evaluate which of the CD3+ T-cell subsets contributes to this increase, we stained splenocytes from control and PbA-infected mice with antibodies specific for different cell surface markers and analyzed the cells by flow cytometry. Spleens from uninfected PKCθ+/+ and PKCθ−/− mice showed similar percentages and total numbers of CD4+ and CD8+ cell populations (Fig. 9 A). Infection with PbA led to a significant increase in the total number (Fig. 9B) and relative proportions (Fig. 9A) of CD4+ T cells, which were more prominent in the spleens of PKCθ+/+ mice (a 37.1% increase versus a 15.5% increase in the relative proportions of CD4+ T cells in the spleens of PKCθ+/+ and PKCθ−/− mice, respectively) (Fig. 9A). In contrast, the total numbers of CD8+ T cells in spleens of PKCθ+/+ and PKCθ−/− mice were similar in uninfected mice and increased in both mouse strains by <10% after PbA infection (Fig. 9C).
FIG. 9.
Quantitation of CD4+ and CD8+ splenic T cells, and surface expression of LFA-1 on CD8+ T cells from control and PbA-infected PKCθ+/+ and PKCθ−/− mice. Spleens were removed from control and PbA-infected PKCθ+/+ and PKCθ−/− mice on day 12 p.i. Cells were counted and stained with Pacific Blue-conjugated anti-CD4, PE-conjugated anti-CD8, and FITC-conjugated anti-LFA-1 antibodies, followed by FACS analysis. The data represent the proportions (A) and total numbers of CD3+ CD4+ (B) and CD3+ CD8+ (C) T cells per spleen. A dot plot representing one of four independent experiments is shown in panel A. The bar graphs (B and C) demonstrate average values of cell numbers obtained by analyses of spleens from four individual mice per group. Representative histograms show LFA-1 expression on splenic CD3+CD8+ T cells from uninfected and PbA-infected PKCθ+/+ and PKCθ−/− mice (D, left panel), and values in the bar graph show the MFI values of the cells obtained from analyses of spleens from four individual mice per group (D, right panel). PbA infection-induced increase in LFA-1 expression on the surfaces of CD3+ CD8+ T cells is shown in panel E. Values represent averages of the MFI in cells from infected mice (n = 4) divided by the MFI of LFA-1 in cells from control, uninfected mice (n = 4). The data are means ± the SEM of four individual mice per group, representing one of two individual experiments. *, P < 0.05 (PKCθ+/+ versus PKCθ−/−) as determined by Student t test. Gray and white bars in panels E and F represent data from PKCθ+/+ and PKCθ−/− cells, respectively.
The involvement of CD8+ cytotoxic T cells in the pathogenesis of ECM was demonstrated in both CD8+ T-cell-deficient mice and perforin-deficient mice, which were found to be resistant to ECM (42). Parasite-specific CD8+ T cells were also found to accumulate intravascularly in the brains of P. berghei-infected mice and to directly or indirectly promote the brain pathology (33). Furthermore, sequestration of CD8+ T cells in the brain of PbA-infected mice correlated with increased surface expression of adhesion molecules, such as LFA-1, whereas infusion of anti-LFA-1 antibodies prevented ECM development (4, 8, 16).
To test whether PKCθ is involved in the regulation of LFA-1 expression and thereby may affect the LFA-1-mediated sequestration of CD8+ T cells in the brain, splenocytes were stained for LFA-1 and analyzed by fluorescence-activated cell sorting (FACS). The results demonstrated similar low levels of LFA-1 on the surface of CD8+ T cells of healthy PKCθ+/+ and PKCθ−/− mice (Fig. 9D). PbA infection of mice resulted in upregulation of LFA-1 expression on CD8+ T cells in both strains (Fig. 9D). However, LFA-1 MFI on PKCθ+/+ CD8+ T cells increased by ∼2.8-fold after PbA infection compared to an increase of ∼1.7-fold on PKCθ−/− CD8+ T cells (a 40% reduction; Fig. 9E). It appears therefore that PKCθ is involved in the regulation of LFA-1 expression in activated CD8+ T cells. The results suggest that the reduced LFA-1 expression in PKCθ−/− CD8+ T cells may possibly contribute to decreased cell sequestration in the brain and a reduction in the intensity and severity of CD8+ T cell-mediated brain pathologies.
DISCUSSION
PKCθ is a critical component of the TCR-linked signaling pathways that regulate T-cell behavior and an array of T-cell-mediated immune responses (24). Recent studies utilized PKCθ-deficient mice in order to analyze the requirement for PKCθ in different models of experimental murine diseases. Depending on the disease model used, the results indicated that PKCθ is required for Th2-type immune-mediated responses (35, 43, 49), as well as for responses mediated by Th1 (21, 49), Th17 (50, 56), and CD8+ T cells (6).
In the present study we show that PKCθ has an important role in the regulation of host responses during infections with PbA. PKCθ had no direct effect on the viability of the parasite and its ability to propagate in mice. However, PKCθ-regulated mechanisms determine the quality and intensity of the host immune responses that affect specific target organs, such as the brain, and the resulting pathological consequences, which may lead to ECM. Both C57BL/6J PKCθ+/+ and PKCθ−/− mice were found to be susceptible to PbA infection, and all mice succumbed to the parasitic infection. In addition, the extent of parasitemia was comparable in the two mouse strains, suggesting no major direct effect of PKCθ on the host immune response against the parasite. However, during the first 11 days p.i., while parasitemia is relatively low (1 to 12% pRBC), the majority of the PKCθ+/+ mice developed neurological symptoms, such as loss of coordination and paralysis, and died of ECM. In contrast, the majority of the PbA-infected PKCθ−/− mice survived the infection for more then 20 days and, despite the continuous rise in the amount of parasitized erythrocytes, they did not develop severe neurological symptoms. Gender-based effects on survival of mice were negligible, since the differences in survival time of PKCθ+/+ and PKCθ−/− mice were maintained in both female and male mice.
Histological analysis of brain sections revealed frequent hemorrhages in the brains of PbA-infected PKCθ+/+ mice, accompanied by widening of blood vessels, disruption of vascular endothelial cells, and the accumulation of erythrocytes and mononuclear cells within their lumens. This is in contrast to brain sections of PbA-infected PKCθ−/− mice, which showed only modest histological changes. PbA-infected PKCθ+/+ mice that were killed on day 12 p.i., suffered from severe pulmonary edema, compared to a mild edema in the lungs of infected PKCθ−/− mice. A similar difference was observed when analyzing the spleen, whereby PbA-infected PKCθ+/+ mice developed severe splenomegaly accompanied by hyperplasia of the germinal centers, and increase in the total number of CD3+CD4+ splenic T cells, compared to only moderate symptoms in infected PKCθ−/− mice.
To characterize these splenic T cells, we first tested their ability to respond to mitogens. As expected, spleen cells from control PKCθ+/+ mice responded to T-cell mitogens by strong proliferation and IL-2 production, which was 5- to 20-fold higher than that of spleen cells from PKCθ−/− mice. PbA infection drastically reduced the ability of splenocytes of both PKCθ+/+ and PKCθ−/− mice to respond to ConA by proliferation and IL-2 production. Furthermore, spleen cells from PbA-infected PKCθ−/− mice produced lower levels of the Th1-type cytokines, IFN-γ and TNF-α, in response to ConA.
The two major functionally distinct CD4+ T-cell subsets include the IFN-γ- and TNF-α-producing Th1 cells, which promote cellular immunity, and IL-4-, IL-5-, IL-10- and IL-13-producing Th2 cells, which promote humoral and allergic immune responses. Analyses of the role of these cytokines in experimental murine malaria demonstrated that brain pathologies and ECM correlate with high levels of both IFN-γ and TNF-α (3, 48), although other studies indicated that lymphotoxin-α, and not TNF-α, is the principle mediator of ECM (15). Our results suggest, therefore, that the inability of PKCθ−/− mice to mount strong Th1-type immune responses correlates with the mild effects of IFN-γ and TNF-α on the brain tissue, which is reflected by the low frequency of ECM. Measurements of serum levels of these two cytokines substantiated the findings obtained with cultured spleen cells, namely, that PKCθ−/− mice produce lower levels of both IFN-γ and TNF-α, either before or after PbA infection.
The reduced serum levels of Th1-type cytokines in PbA-infected PKCθ−/− mice can only partially be explained by the reduced number of CD3+CD4+ T cells in the spleen, since the number of CD3+CD4+ T cells in PbA-infected PKCθ−/− mice was ∼2-fold lower than that in PbA-infected PKCθ+/+ mice, compared to >25-fold lower levels of IFN-γ in PbA-infected PKCθ−/− mice. It is therefore possible that additional cell types, besides splenocytes, are involved in determining the serum levels of cytokines.
Shifts in the balance of Th1/Th2 toward a predominance of Th2 may increase mouse resistance to malaria, and IL-10 was found to play a protective role against experimental ECM (26). However, the partially impaired IL-10 response of PKCθ−/− mice did not seem to have a major effect on ECM development in these mice. The defect in cytokine production in PKCθ−/− mice was not general, since serum IL-6 levels were higher in PKCθ−/− mice than in PKCθ+/+ mice. Nevertheless, the direct relevance of IL-6 to parasite clearance is not clear (17).
CD8+ T cells can also affect the outcome of a malaria disease and regulate the development of ECM after infection with P. berghei (4, 9, 42). In agreement, brain sequestration of CD8+ T cells was found to correlate with increased neurological symptoms and ECM-induced mortality (8). CD8+ T cells are also involved in circulatory shock and respiratory distress in P. berghei-infected mice (12), whereas in immunized mice they were found to provide long-term immunity to P. berghei infection (61).
Leukocyte sequestration into the brain is regulated by adhesion molecules, including LFA-1 (54). In agreement, blocking of LFA-1 in PbA-infected mice (using LFA-1-blocking antibodies) partially prevented ECM formation, concomitant with decreasing circulatory levels of TNF (16, 18). We found that PbA infection of PKCθ+/+ mice induces increased expression of LFA-1 on CD3+ CD8+ splenic T cells and that the increase in PKCθ−/− cells was decreased by ∼40%. It is possible therefore that a lack of PKCθ decreases the sequestration of CD8+ T-cell in brain capillaries and postcapillary venules during the early phase of infection with PbA, thereby reducing CD8+ T-cell-mediated effects that damage the endothelial cells and brain tissue, leading to ECM and mortality.
Acknowledgments
We thank Judith Waknine-Grinberg for technical assistance.
This research was supported in part by the USA-Israel Binational Science Foundation, the Israeli-Taiwanese Scientific Research Cooperation, the Israel Science Foundation, the Israel Cancer Research Fund, Chief Scientist's office, the Israel Ministry of Health, the Israel Cancer Association through a donation by Ida and Harry Shooster, a donation by Linda Osofsky, SZCUF Australia, and the Bloch Trust. N.I. holds the Joseph H. Krupp Chair in Cancer Immunobiology.
Editor: J. H. Adams
Footnotes
Published ahead of print on 26 July 2010.
REFERENCES
- 1.Adams, S., H. Brown, and G. Turner. 2002. Breaking down the blood-brain barrier: signaling a path to cerebral malaria? Trends Parasitol. 18:360-366. [DOI] [PubMed] [Google Scholar]
- 2.Altman, A., N. Isakov, and G. Baier. 2000. Protein kinase Cθ: a new essential superstar on the T-cell stage. Immunol. Today 21:567-573. [DOI] [PubMed] [Google Scholar]
- 3.Amani, V., A. M. Vigario, E. Belnoue, M. Marussig, L. Fonseca, D. Mazier, and L. Renia. 2000. Involvement of IFN-gamma receptor-medicated signaling in pathology and anti-malarial immunity induced by Plasmodium berghei infection. Eur. J. Immunol. 30:1646-1655. [DOI] [PubMed] [Google Scholar]
- 4.Bagot, S., F. Nogueira, A. Collette, V. do Rosario, F. Lemonier, P. A. Cazenave, and S. Pied. 2004. Comparative study of brain CD8+ T cells induced by sporozoites and those induced by blood-stage Plasmodium berghei ANKA involved in the development of cerebral malaria. Infect. Immun. 72:2817-2826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baier, G., D. Telford, L. Giampa, K. M. Coggeshall, G. Baier-Bitterlich, N. Isakov, and A. Altman. 1993. Molecular cloning and characterization of PKCθ, a novel member of the protein kinase C (PKC) gene family expressed predominantly in hematopoietic cells. J. Biol. Chem. 268:4997-5004. [PubMed] [Google Scholar]
- 6.Barouch-Bentov, R., E. E. Lemmens, J. Hu, E. M. Janssen, N. M. Droin, J. Song, S. P. Schoenberger, and A. Altman. 2005. Protein kinase C-theta is an early survival factor required for differentiation of effector CD8+ T cells. J. Immunol. 175:5126-5134. [DOI] [PubMed] [Google Scholar]
- 7.Belkaid, Y. 2007. Regulatory T cells and infection: a dangerous necessity. Nat. Rev. Immunol. 7:875-888. [DOI] [PubMed] [Google Scholar]
- 8.Belnoue, E., M. Kayibanda, A. M. Vigario, J. C. Deschemin, N. van Rooijen, M. Viguier, G. Snounou, and L. Renia. 2002. On the pathogenic role of brain-sequestered αβ CD8+ T cells in experimental cerebral malaria. J. Immunol. 169:6369-6375. [DOI] [PubMed] [Google Scholar]
- 9.Belnoue, E., S. M. Potter, D. S. Rosa, M. Mauduit, A. C. Gruner, M. Kayibanda, A. J. Mitchell, N. H. Hunt, and L. Renia. 2008. Control of pathogenic CD8+ T-cell migration to the brain by IFN-gamma during experimental cerebral malaria. Parasite Immunol. 30:544-553. [DOI] [PubMed] [Google Scholar]
- 10.Breman, J. G., A. Mills, R. W. Snow, J. O. Mulligan, C. Lengeler, K. Mendis, B. Sharp, C. Morel, P. Marchesini, N. J. White, R. W. Steketee, and O. K. Doumbo. 2006. Conquering malaria, p. 413-431. In D. T. Jamison, J. G. Breman, A. R. Measham, et al. (ed.), Disease control priorities in developing countries, 2nd ed. The World Bank Group, Geneva, Switzerland.
- 11.Casares, S., and T. L. Richie. 2009. Immune evasion by malaria parasites: a challenge for vaccine development. Curr. Opin. Immunol. 21:321-330. [DOI] [PubMed] [Google Scholar]
- 12.Chang, W. L., S. P. Jones, D. J. Lefer, T. Welbourne, G. Sun, L. Yin, H. Suzuki, J. Huang, D. N. Granger, and H. C. van der Heyde. 2001. CD8+-T-cell depletion ameliorates circulatory shock in Plasmodium berghei-infected mice. Infect. Immun. 69:7341-7348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chotivanich, K., R. Udomsangpetch, R. McGready, S. Proux, P. Newton, S. Pukrittayakamee, S. Looareesuwan, and N. J. White. 2002. Central role of the spleen in malaria parasite clearance. J. Infect. Dis. 185:1538-1541. [DOI] [PubMed] [Google Scholar]
- 14.Coban, C., K. J. Ishii, S. Uematsu, N. Arisue, S. Sato, M. Yamamoto, T. Kawai, O. Takeuchi, H. Hisaeda, T. Horii, and S. Akira. 2007. Pathological role of Toll-like receptor signaling in cerebral malaria. Int. Immunol. 19:67-79. [DOI] [PubMed] [Google Scholar]
- 15.Engwerda, C. R., T. L. Mynott, S. Sawhney, J. B. De Souza, Q. D. Bickle, and P. M. Kaye. 2002. Locally upregulated lymphotoxin alpha, not systemic tumor necrosis factor alpha, is the principle mediator of murine cerebral malaria. J. Exp. Med. 195:1371-1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Falanga, P. B., and E. C. Butcher. 1991. Late treatment with anti-LFA-1 (CD11a) antibody prevents cerebral malaria in a mouse model. Eur. J. Immunol. 21:2259-2263. [DOI] [PubMed] [Google Scholar]
- 17.Grau, G. E., K. Frei, P. F. Piguet, A. Fontana, H. Heremans, A. Billiau, P. Vassalli, and P. H. Lambert. 1990. Interleukin 6 production in experimental cerebral malaria: modulation by anticytokine antibodies and possible role in hypergammaglobulinemia. J. Exp. Med. 172:1505-1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grau, G. E., P. Pointaire, P. F. Piguet, C. Vesin, H. Rosen, I. Stamenkovic, F. Takei, and P. Vassalli. 1991. Late administration of monoclonal antibody to leukocyte function-antigen 1 abrogates incipient murine cerebral malaria. Eur. J. Immunol. 21:2265-2267. [DOI] [PubMed] [Google Scholar]
- 19.Hansen, D. S., M. A. Siomos, L. Buckingham, A. A. Scalzo, and L. Schofield. 2003. Regulation of murine cerebral malaria pathogenesis by CD1d-restricted NKT cells and the natural killer complex. Immunity 18:391-402. [DOI] [PubMed] [Google Scholar]
- 20.Hanum, P. S., M. Hayano, and S. Kojima. 2003. Cytokine and chemokine responses in a cerebral malaria-susceptible or -resistant strain of mice to Plasmodium berghei ANKA infection: early chemokine expression in the brain. Int. Immunol. 15:633-640. [DOI] [PubMed] [Google Scholar]
- 21.Healy, A. M., E. Izmailova, M. Fitzgerald, R. Walker, M. Hattersley, M. Silva, E. Siebert, J. Terkelsen, D. Picarella, M. D. Pickard, B. LeClair, S. Chandra, and B. Jaffee. 2006. PKCθ-deficient mice are protected from Th1-dependent antigen-induced arthritis. J. Immunol. 177:1886-1893. [DOI] [PubMed] [Google Scholar]
- 22.Hunt, N. H., J. Golenser, T. Chan-Ling, S. Parekh, C. Rae, S. Potter, I. M. Medana, J. Miu, and H. J. Ball. 2006. Immunopathogenesis of cerebral malaria. Int. J. Parasitol. 36:569-582. [DOI] [PubMed] [Google Scholar]
- 23.Idro, R., N. E. Jenkins, and C. R. Newton. 2005. Pathogenesis, clinical features, and neurological outcome of cerebral malaria. Lancet Neurol. 4:827-840. [DOI] [PubMed] [Google Scholar]
- 24.Isakov, N., and A. Altman. 2002. Protein kinase Cθ in T-cell activation. Annu. Rev. Immunol. 20:761-794. [DOI] [PubMed] [Google Scholar]
- 25.Jain, J., C. Loh, and A. Rao. 1995. Transcriptional regulation of the IL-2 gene. Curr. Opin. Immunol. 7:333-342. [DOI] [PubMed] [Google Scholar]
- 26.Kossodo, S., C. Monso, P. Juillard, T. Velu, M. Goldman, and G. E. Grau. 1997. Interleukin-10 modulates susceptibility in experimental cerebral malaria. Immunology 91:536-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krucken, J., J. V. Braun, M. A. Dkhil, A. Grunwald, and F. Wunderlich. 2005. Deletion of LTβR augments male susceptibility to Plasmodium chabaudi. Parasite Immunol. 27:205-212. [DOI] [PubMed] [Google Scholar]
- 28.Lamb, T. J., D. E. Brown, A. J. Potocnik, and J. Langhorne. 2006. Insights into the immunopathogenesis of malaria using mouse models. Expert Rev. Mol. Med. 8:1-22. [DOI] [PubMed] [Google Scholar]
- 29.Lamikanra, A. A., D. Brown, A. Potocnik, C. Casals-Pascual, J. Langhorne, and D. J. Roberts. 2007. Malarial anemia: of mice and men. Blood 110:18-28. [DOI] [PubMed] [Google Scholar]
- 30.Langhorne, J., C. Cross, E. Seixas, C. Li, and T. von der Weid. 1998. A role for B cells in the development of T-cell helper function in a malaria infection in mice. Proc. Natl. Acad. Sci. U. S. A. 95:1730-1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Langhorne, J., F. M. Ndungu, A. M. Sponaas, and K. Marsh. 2008. Immunity to malaria: more questions than answers. Nat. Immunol. 9:725-732. [DOI] [PubMed] [Google Scholar]
- 32.Li, C., L. A. Sanni, F. Omer, E. Riley, and J. Langhorne. 2003. Pathology of Plasmodium chabaudi chabaudi infection and mortality in interleukin-10-deficient mice are ameliorated by anti-tumor necrosis factor alpha and exacerbated by anti-transforming growth factor beta antibodies. Infect. Immun. 71:4850-4856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lundie, R. J., T. F. de Koning-Ward, G. M. Davey, C. Q. Nie, D. S. Hansen, L. S. Lau, J. D. Mintern, G. T. Belz, L. Schofield, F. R. Carbone, J. A. Villadangos, B. S. Crabb, and W. R. Heath. 2008. Blood-stage Plasmodium infection induces CD8+ T lymphocytes to parasite-expressed antigens, largely regulated by CD8α+ dendritic cells. Proc. Natl. Acad. Sci. U. S. A. 105:14509-14514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lyke, K. E., R. Burges, Y. Cissoko, L. Sangare, M. Dao, I. Diarra, A. Kone, R. Harley, C. V. Plowe, O. K. Doumbo, and M. B. Sztein. 2004. Serum levels of the proinflammatory cytokines interleukin-1β (IL-1β), IL-6, IL-8, IL-10, tumor necrosis factor alpha, and IL-12(p70) in Malian children with severe Plasmodium falciparum malaria and matched uncomplicated malaria or healthy controls. Infect. Immun. 72:5630-5637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marsland, B. J., T. J. Soos, G. Spath, D. R. Littman, and M. Kopf. 2004. Protein kinase C theta is critical for the development of in vivo T helper (Th)2 cell but not Th1 cell responses. J. Exp. Med. 200:181-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meding, S. J., and J. Langhorne. 1991. CD4+ T cells and B cells are necessary for the transfer of protective immunity to Plasmodium chabaudi chabaudi. Eur. J. Immunol. 21:1433-1438. [DOI] [PubMed] [Google Scholar]
- 37.Meller, N., Y. Elitzur, and N. Isakov. 1999. Protein kinase Cθ (PKCθ) distribution analysis in hematopoietic cells: proliferating T cells exhibit high proportions of PKCθ in the particulate fraction. Cell. Immunol. 193:185-193. [DOI] [PubMed] [Google Scholar]
- 38.Miller, L. H., D. I. Baruch, K. Marsh, and O. K. Doumbo. 2002. The pathogenic basis of malaria. Nature 415:673-679. [DOI] [PubMed] [Google Scholar]
- 39.Monks, C. R., B. A. Freiberg, H. Kupfer, N. Sciaky, and A. Kupfer. 1998. Three-dimensional segregation of supramolecular activation clusters in T cells. Nature 395:82-86. [DOI] [PubMed] [Google Scholar]
- 40.Monks, C. R., H. Kupfer, I. Tamir, A. Barlow, and A. Kupfer. 1997. Selective modulation of protein kinase C-theta during T-cell activation. Nature 385:83-86. [DOI] [PubMed] [Google Scholar]
- 41.Niikura, M., S. Kamiya, A. Nakane, K. Kita, and F. Kobayashi. 2010. IL-10 plays a crucial role for the protection of experimental cerebral malaria by coinfection with non-lethal malaria parasites. Int. J. Parasitol. 40:101-108. [DOI] [PubMed] [Google Scholar]
- 42.Nitcheu, J., O. Bonduelle, C. Combadiere, M. Tefit, D. Seilhean, D. Mazier, and B. Combadiere. 2003. Perforin-dependent brain-infiltrating cytotoxic CD8+ T lymphocytes mediate experimental cerebral malaria pathogenesis. J. Immunol. 170:2221-2228. [DOI] [PubMed] [Google Scholar]
- 43.Ohayon, A., G. Dong, and N. Isakov. 2007. Involvement of PKCθ in CD4+ T-cell polarization and mouse resistance to cutaneous leishmaniasis, p. 221-238. In N. Isakov (ed.), Lymphocyte activation and signal transduction. Transworld Research Network, Trivandrum, Kerala, India.
- 44.Patnaik, J. K., B. S. Das, S. K. Mishra, S. Mohanty, S. K. Satpathy, and D. Mohanty. 1994. Vascular clogging, mononuclear cell margination, and enhanced vascular permeability in the pathogenesis of human cerebral malaria. Am. J. Trop. Med. Hyg. 51:642-647. [PubMed] [Google Scholar]
- 45.Pfeifhofer, C., K. Kofler, T. Gruber, N. G. Tabrizi, C. Lutz, K. Maly, M. Leitges, and G. Baier. 2003. Protein kinase Cθ affects Ca2+ mobilization and NFAT cell activation in primary mouse T cells. J. Exp. Med. 197:1525-1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pierce, S. K., and L. H. Miller. 2009. World Malaria Day 2009: what malaria knows about the immune system that immunologists still do not. J. Immunol. 182:5171-5177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Podoba, J. E., and M. M. Stevenson. 1991. CD4+ and CD8+ T lymphocytes both contribute to acquired immunity to blood-stage Plasmodium chabaudi AS. Infect. Immun. 59:51-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rudin, W., H. P. Eugster, G. Bordmann, J. Bonato, M. Muller, M. Yamage, and B. Ryffel. 1997. Resistance to cerebral malaria in tumor necrosis factor-alpha/beta-deficient mice is associated with a reduction of intercellular adhesion molecule-1 upregulation and T helper type 1 response. Am. J. Pathol. 150:257-266. [PMC free article] [PubMed] [Google Scholar]
- 49.Salek-Ardakani, S., T. So, B. S. Halteman, A. Altman, and M. Croft. 2004. Differential regulation of Th2 and Th1 lung inflammatory responses by protein kinase C theta. J. Immunol. 173:6440-6447. [DOI] [PubMed] [Google Scholar]
- 50.Salek-Ardakani, S., T. So, B. S. Halteman, A. Altman, and M. Croft. 2005. Protein kinase Cθ controls Th1 cells in experimental autoimmune encephalomyelitis. J. Immunol. 175:7635-7641. [DOI] [PubMed] [Google Scholar]
- 51.Sanni, L. A., W. Jarra, C. Li, and J. Langhorne. 2004. Cerebral edema and cerebral hemorrhages in interleukin-10-deficient mice infected with Plasmodium chabaudi. Infect. Immun. 72:3054-3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Scholzen, A., G. Minigo, and M. Plebanski. 2009. Heroes or villains? T regulatory cells in malaria infection. Trends Parasitol. 26:16-25. [DOI] [PubMed] [Google Scholar]
- 53.Sein, K. K., Y. Maeno, H. V. Thuc, T. K. Anh, and M. Aikawa. 1993. Differential sequestration of parasitized erythrocytes in the cerebrum and cerebellum in human cerebral malaria. Am. J. Trop. Med. Hyg. 48:504-511. [DOI] [PubMed] [Google Scholar]
- 54.Senaldi, G., C. Vesin, R. Chang, G. E. Grau, and P. F. Piguet. 1994. Role of polymorphonuclear neutrophil leukocytes and their integrin CD11a (LFA-1) in the pathogenesis of severe murine malaria. Infect. Immun. 62:1144-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sun, Z., C. W. Arendt, W. Ellmeier, E. M. Schaeffer, M. J. Sunshine, L. Gandhi, J. Annes, D. Petrzilka, A. Kupfer, P. L. Schwartzberg, and D. R. Littman. 2000. PKCθ is required for TCR-induced NF-κB activation in mature but not immature T lymphocytes. Nature 404:402-407. [DOI] [PubMed] [Google Scholar]
- 56.Tan, S. L., J. Zhao, C. Bi, X. C. Chen, D. L. Hepburn, J. Wang, J. D. Sedgwick, S. R. Chintalacharuvu, and S. Na. 2006. Resistance to experimental autoimmune encephalomyelitis and impaired IL-17 production in protein kinase Cθ-deficient mice. J. Immunol. 176:2872-2879. [DOI] [PubMed] [Google Scholar]
- 57.Turner, G. 1997. Cerebral malaria. Brain Pathol. 7:569-582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.van der Heyde, H. C., J. Nolan, V. Combes, I. Gramaglia, and G. E. Grau. 2006. A unified hypothesis for the genesis of cerebral malaria: sequestration, inflammation, and hemostasis leading to microcirculatory dysfunction. Trends Parasitol. 22:503-508. [DOI] [PubMed] [Google Scholar]
- 59.Villalba, M., K. Bi, J. Hu, Y. Altman, P. Bushway, E. Reits, J. Neefjes, G. Baier, R. T. Abraham, and A. Altman. 2002. Translocation of PKCθ in T cells is mediated by a nonconventional, PI3K- and Vav-dependent pathway, but does not absolutely require phospholipase C. J. Cell Biol. 157:253-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.von der Weid, T., N. Honarvar, and J. Langhorne. 1996. Gene-targeted mice lacking B cells are unable to eliminate a blood stage malaria infection. J. Immunol. 156:2510-2516. [PubMed] [Google Scholar]
- 61.Weiss, W. R., M. Sedegah, R. L. Beaudoin, L. H. Miller, and M. F. Good. 1988. CD8+ T cells (cytotoxic/suppressors) are required for protection in mice immunized with malaria sporozoites. Proc. Natl. Acad. Sci. U. S. A. 85:573-576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.White, N. J., G. D. Turner, I. M. Medana, A. M. Dondorp, and N. P. Day. 2009. The murine cerebral malaria phenomenon. Trends Parasitol. 26:11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wunderlich, F., M. A. Dkhil, L. I. Mehnert, J. V. Braun, M. El-Khadragy, E. Borsch, D. Hermsen, W. P. Benten, K. Pfeffer, H. Mossmann, and J. Krucken. 2005. Testosterone responsiveness of spleen and liver in female lymphotoxin beta receptor-deficient mice resistant to blood-stage malaria. Microbes Infect. 7:399-409. [DOI] [PubMed] [Google Scholar]
- 64.Yanez, D. M., D. D. Manning, A. J. Cooley, W. P. Weidanz, and H. C. van der Heyde. 1996. Participation of lymphocyte subpopulations in the pathogenesis of experimental murine cerebral malaria. J. Immunol. 157:1620-1624. [PubMed] [Google Scholar]
- 65.Yazdanbakhsh, M. 2010. Why does immunity to parasites take so long to develop? Nat. Immunol. Rev. 10:80-81. [DOI] [PMC free article] [PubMed] [Google Scholar]