Abstract
We assessed the prediction that access of the viral NS1 protein to cellular PDZ domain protein networks enhances the virulence of highly pathogenic avian influenza A viruses. The NS1 proteins of most avian influenza viruses bear the C-terminal ligand sequence Glu-Ser-Glu-Val (ESEV) for PDZ domains present in multiple host proteins, whereas no such motif is found in the NS1 homologues of seasonal human virus strains. Previous analysis showed that a C-terminal ESEV motif increases viral virulence when introduced into the NS1 protein of mouse-adapted H1N1 influenza virus. To examine the role of the PDZ domain ligand motif in avian influenza virus virulence, we generated three recombinants, derived from the prototypic H5N1 influenza A/Vietnam/1203/04 virus, expressing NS1 proteins that either have the C-terminal ESEV motif or the human influenza virus RSKV consensus or bear a natural truncation of this motif, respectively. Cell biological analyses showed strong control of NS1 nuclear migration in infected mammalian and avian cells, with only minor differences between the three variants. The ESEV sequence attenuated viral replication on cultured human, murine, and duck cells but not on chicken fibroblasts. However, all three viruses caused highly lethal infections in mice and chickens, with little difference in viral titers in organs, mean lethal dose, or intravenous pathogenicity index. These findings demonstrate that a PDZ domain ligand sequence in NS1 contributes little to the virulence of H5N1 viruses in these hosts, and they indicate that this motif modulates viral replication in a strain- and host-dependent manner.
The transmission of highly pathogenic avian influenza A viruses (HPAIV) of the H5N1 subtype to humans since the year 1997 has caused a high mortality rate of almost 60% (62). Patients infected with H5N1 influenza virus developed mainly severe respiratory disease, characterized by fever, cough, shortness of breath, and pneumonia, that frequently progressed to acute respiratory distress syndrome (ARDS) and multiorgan failure (28, 68, 69). In fatal cases, the median time from onset to death was 9 to 10 days (1). Systemic spread (18) and hypercytokinemia (11) have been described as possible disease-aggravating factors of HPAIV-H5N1 viruses, but the reasons for their high virulence in humans are incompletely understood.
Due to the potential pandemic threat presented by H5N1 viruses, there is great interest in the identification of viral virulence determinants and their mode of action. This is critical not only for a better understanding of the pathogenic mechanisms induced by these viruses but also for the development of new drugs to treat the infections. The high virulence of HPAIV-H5N1 isolates in the avian host correlates with the presence of a polybasic cleavage site in the hemagglutinin (HA), facilitating its intracellular cleavage by furin-like proteases (27, 50). Further, amino acid substitutions in the PA protein (T515A) (30) and in the NS1 protein (V149A) (40) have been reported to regulate the virulence of corresponding HPAIV-H5N1 isolates in ducks and chickens. The known molecular determinants of virulence in mammalian hosts also include the polybasic cleavage site in the HA (23) and several polymorphisms in the PB2 polymerase subunit and the proapoptotic PB1-F2 protein. Thus, a serine residue at position 66 in the PB1-F2 protein increased viral replication and decreased survival in the mouse model (9). Also, specific amino acid polymorphisms within PB2 (E627K or D701N) can increase virulence in mice (23, 39) and viral replication in mammalian cells (7, 57, 58). Furthermore, the nonstructural NS1 protein, which has a major function in the inhibition of type I interferon (IFN) (17, 19) and in the limitation of the antiviral effects of IFN-induced proteins, including PKR (4, 22), OAS/RNase L (45), and RIG-I (16, 48, 63, 64), contributes to virulence in mammals (34, 55).
The domain structure of the NS1 protein is well characterized; it includes an N-terminal RNA binding and dimerization domain and a nuclear localization signal (NLS) at positions 34 to 38 (summarized in reference 19). The NS1 proteins of most human strains circulating between 1950 and 1986 also contain a second NLS at positions 219 to 227 (NLS-2), which includes four conserved basic amino acids (K219, R220, R224, R227) (44). A large-scale sequence analysis showed that the NS1 proteins of avian and human influenza viruses differ in their C-terminal sequences, indicating possible differences in the associated activity (46). Among most high- and low-pathogenicity avian influenza viruses, the last four NS1 amino acids consist of the conserved sequence ESEV (3,007 of 3,692 isolates described in the NCBI database [3]), while for the majority of seasonal human influenza viruses, the motif RSKV is typical (1,911 of 2,713 isolates). Significantly, only the NS1 protein carrying the “avian” ESEV motif interacted in vitro with 24 cellular factors carrying a PDZ (postsynaptic density protein 95, Drosophila disc large tumor suppressor, and zonula occludens 1 protein) domain. The human genome encodes at least 214 proteins containing one or more of these protein interaction modules that recognize short peptide motifs, which are most often present at the C termini of their targets (36, 38). Many PDZ domain proteins have been shown to mediate the formation and localization of higher-order complexes and to participate in various cellular signaling events regulating, for instance, cell polarity and neuronal function (31). Therefore, it was hypothesized that the abundant expression of “avian” NS1 protein capable of interacting with human PDZ domains could possibly disturb their function and aggravate disease severity in H5N1 infections (46). However, there is only limited experimental support for the universal validity of this hypothesis. The grafting of the “avian” ESEV sequence into the C terminus of NS1 protein expressed by mouse-adapted influenza A/WSN/33 virus (H1N1) decreased the mean lethal dose by about 1 order of magnitude (32). Still, it is not clear to what extent this motif contributes to the virulence of HPAIV-H5N1 and other natural influenza A viruses in avian and mammalian hosts.
The goal of the present study was to elucidate the role of the C-terminal NS1 motif in viral replication and disease caused by the prototypic influenza A/Vietnam/1203/04 (VN/1203) virus, isolated in a fatal human case (60). This virus expresses an NS1 protein that is very similar or identical at positions 1 to 215 to homologues expressed by other HPAIV-H5N1 strains but naturally lacks the 10 C-terminal amino acids (aa), including the terminal ESEV motif, due to a premature stop codon (Fig. 1). We used reverse genetics to produce a recombinant VN/1203 wild-type (WT) virus and two variants with reconstituted NS1 C termini ending either with the “avian” ESEV or with the “human” RSKV sequence. Experimental infections of mice and chickens revealed that all three viruses caused highly lethal infections in both species, with only moderate differences in viral titers in the organs of the mice. Thus, we show that the C-terminal ESEV motif of the NS1 protein contributes little to the virulence of H5N1 viruses in mice and chickens, and we suggest that this motif modulates viral virulence in a strain- and host-dependent manner.
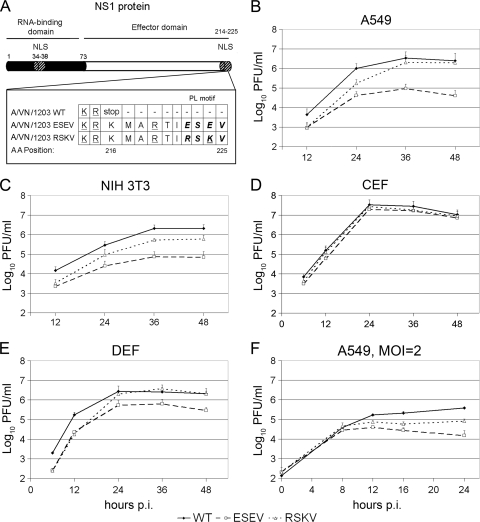
FIG. 1.
Growth kinetics of recombinant VN/1203 viruses expressing WT or elongated NS1 proteins in human, murine, and avian cells. (A) Scheme of the viral VN/1203-NS1 protein with the RNA binding domain and the nuclear localization signals (NLS) at positions 34 to 38 and 214 to 225 indicated. Amino acids involved in NLS2 function are underlined. The C-terminal sequences of the WT and elongated mutant NS1 proteins are given, and the PL motif is shown in boldface. (B to E) Human A549 alveolar cells, murine NIH 3T3 fibroblasts, chicken embryo fibroblasts (CEFs), or EFB-R1 duck embryo fibroblasts (DEFs) were infected with recombinant VN/1203-WT, -ESEV, or -RSKV viruses at an MOI of 0.001. Aliquots of supernatants were harvested at the indicated time points, and samples were titrated by plaque assays in MDCK cells. (F) Human A549 cells were infected at an MOI of 2, and virus titers in supernatants taken at the indicated time points were determined by plaque assays. Results are averages for at least two independent experiments with biological duplicates. Error bars indicate standard deviations.
MATERIALS AND METHODS
Cells and viruses.
Human 293T embryonic kidney cells and human A549 lung epithelial cells were grown in Dulbecco's modified Eagle's medium (D-MEM) supplemented with 10% fetal bovine serum and antibiotics. Mouse NIH 3T3 fibroblasts were grown in 2× D-MEM supplemented with 10% fetal bovine serum plus antibiotics. The EFB-R1 duck embryo fibroblast (DEF) cell line was obtained from the cell bank at the Friedrich-Loeffler-Institute (Insel Riems, Germany) and was maintained in D-MEM supplemented with 10% fetal bovine serum. Primary chicken embryo fibroblast (CEF) cultures were prepared from 11-day-old embryonated eggs and grown in D-MEM supplemented with 10% fetal bovine serum. All cells were incubated at 37°C under 5% CO2. Stocks of the influenza A virus strains A/Panama/2007/99 (H3N2) and A/PR8/34 (H1N1) were grown in 10-day-old embryonated chicken eggs and titrated on MDCK cells by plaque assays. The recombinant A/PR8 delNS1 virus was amplified in 6-day-old embryonated chicken eggs (41). The allantoic fluid collected from inoculated eggs was harvested, divided into aliquots, and stored at −80°C until use.
Construction of plasmids.
For the generation of a plasmid-based reverse genetic system of A/VN/1203, the complete cDNAs of the PB1 (GenBank accession number EF467808), PB2 (EF467805), PA (AY818132), and NP (AY818138) segments were synthesized by a commercial supplier (Geneart, Regensburg, Germany), while the cDNAs of the remaining segments—HA, NA, M, and NS—were prepared by reverse transcription-PCR (RT-PCR) using viral RNA obtained from the World Influenza Centre at the National Institute for Medical Research, London, United Kingdom. Viral cDNAs were cloned into the pHW2000 vector as described previously (26), and Stratagene's QuikChange site-directed mutagenesis kit was used to generate the NS1-ESEV and -RSKV mutant alleles.
Generation of recombinant influenza A/VN/1203 viruses.
Plasmids coding for the eight viral gene segments were transfected into human 293T cells using Lipofectamine 2000 (Invitrogen). Cells were incubated at 37°C for 24 h, and supernatants of transfected cells containing the recombinant viruses were passaged in the allantoic cavities of 10-day-old embryonated chicken eggs for 36 h. The virus titers were determined by plaque assays on MDCKII cells. To confirm the identity of the rescued viruses, viral RNA was extracted and analyzed by RT-PCR and cycle sequencing. Virus rescue and all subsequent experiments were conducted under the biosafety level 3 conditions approved for work with these viruses by local authorities.
Replication assay.
A549, NIH 3T3, and Vero cells, DEFs, and CEFs were infected with WT, ESEV, and RSKV viruses at the multiplicities of infection (MOIs) indicated in the figure legends and were incubated in D-MEM-0.2% bovine albumin containing 1 μg/ml trypsin (Sigma). Supernatants were collected at the indicated time points and were titrated by plaque assays on MDCKII cells.
Immunoblot analysis of viral protein levels in infected A549 cells.
A549 cells were infected at a multiplicity of 5 with WT, ESEV, and RSKV viruses. Cells were lysed 2, 4, 8, 12, 16, and 24 h postinfection (hpi), and the lysates were subjected to immunoblot analysis under identical conditions using rabbit anti-NS1, goat anti-PB1, and mouse anti-A/NP antibodies, with a monoclonal anti-β-actin antibody (Sigma) as a loading control.
Microscopic analysis of the intracellular localization of NS1 proteins in transfected and infected cell cultures.
Human A549 cells were transfected with pHW2000 plasmids encoding the NS1 proteins of A/VN/1203-WT, -ESEV, or -RSKV viruses. Twenty-four hours later, cells were prepared for microscopic analysis as described previously (54); subsequently, they were stained with an NS1-specific rabbit antiserum, followed by detection with goat anti-rabbit IgG conjugated with Alexa Fluor 488 dye as a secondary antibody (Invitrogen). To study NS1 localization during infection, A549 cells, DEFs, and CEFs were infected with WT, ESEV, or RSKV virus at a multiplicity of 2 and were stained with an NS1-specific antiserum as described above. Imaging of cells was done on an LSM510 Meta confocal laser scanning microscope equipped with a C-Apochromat 63× (numerical aperture, 1.2) water objective lens (Zeiss, Jena, Germany) as described elsewhere (54). Data were analyzed and processed by the Zeiss LSM Image Browser (version 3.5) and Adobe Photoshop (version 4.0) software packages.
Analysis of IFN-β promoter activity in infected cells.
IFN-β promoter activity in infected cells was analyzed as described previously (10). Briefly, MDCKII cells were transfected with the IFN-β promoter luciferase reporter plasmid p125-Luc and an expression plasmid for the VN/1203-NS1 WT, -ESEV, or -RSKV protein or an empty vector (pHW2000). In all assays, plasmid pRL-TK-Luc, encoding constitutively expressed Renilla luciferase, was cotransfected and used as an internal control to normalize the results. One day posttransfection, cells were stimulated by infection with the A/PR8 ΔNS1 virus at an MOI of 1 or were mock treated. Luciferase activities in cell extracts were determined 8 hpi. The value for a virus-induced increase in vector-transfected cells was arbitrarily set to 100% and compared to the induction observed in NS1-expressing cells. The NP protein was detected by immunoblotting to confirm the infection by the virus lacking the NS1 gene (delNS1 virus).
Quantification of IFN-β secretion.
A549 cells were infected at an MOI of 0.01. Following infection, cells were incubated at 37°C in D-MEM-0.2% bovine albumin containing 1 μg/ml trypsin, and the supernatants were harvested at 24 and 48 hpi. Samples were analyzed with a commercial IFN-β enzyme-linked immunosorbent assay (ELISA) as recommended by the manufacturer (Invitrogen).
Animal experiments.
All mouse and chicken infectivity experiments were approved by the local committees and were conducted in accordance with national guidelines for the care and use of laboratory animals. BALB/c mice were bred in the animal facility of the Federal Institute for Risk Assessment (Berlin, Germany). Specific-pathogen-free chickens were purchased from Lohmann Tierzucht (Cuxhaven, Germany). Groups of six 7-week-old female BALB/c mice were anesthetized with isoflurane and were inoculated intranasally with different dilutions of the WT, ESEV, or RSKV virus using 5, 10, 102, or 103 PFU per mouse in a volume of 50 μl to determine the mean lethal dose. Mice were monitored for signs of disease, and their body weights were measured daily. According to the approved protocols, mice had to be euthanized when weight loss exceeded 20% of the initial value and/or when severe clinical symptoms became apparent. To study the viral load and spread to organs, the lungs, brains, hearts, spleens, kidneys, and livers of euthanized mice were aseptically prepared. The collected tissues were homogenized using a FastPrep-24 homogenizer (MP Biomedicals) and were titrated by standard plaque assays. For pathohistological analysis, parts of the collected lungs were fixed, dehydrated, and embedded in paraffin. Samples were stained with hematoxylin and eosin (H&E) or with a polyclonal goat anti-influenza A virus antibody (Serotec OBT 1551), followed by development with a suitable secondary IgG conjugated to horseradish peroxidase. The virulence of the recombinant viruses in chickens was compared by determination of the intravenous pathogenicity index (IVPI) according to the standard OIE protocol (65). Groups of 6-week-old, specific-pathogen-free chickens were infected intravenously with 104 PFU of recombinant WT, ESEV, or RSKV virus, and the mean clinical score was recorded. Infected animals were clinically scored daily as 0 (healthy), 1 (sick), 2 (severely sick), or 3 (dead). Groups of five 6-week-old chickens were also infected by the intranasal route with 104 PFU of recombinant WT, ESEV, or RSKV virus. Oropharyngeal and cloacal swab samples were collected daily in D-MEM supplemented with 5% fetal calf serum and antimicrobial drugs. All individual swabs were tested by a real-time RT-PCR (rRT-PCR) specific for subtype H5N1 (25), and the genomic load was semiquantified by the threshold cycle (CT) value.
RESULTS
Generation of recombinant H5N1 VN/1203 influenza viruses.
The VN/1203 virus expresses an NS1 protein of 215 aa that, due to a premature stop codon, lacks the C-terminal 10 aa including the PDZ ligand domain (PL) present in the NS1 proteins of most other avian influenza A viruses (Fig. 1A). To study the role of the PL motif for viral pathogenicity, we generated an eight-plasmid set for the rescue of recombinant VN/1203 virus. In addition to wild-type virus, we produced two variants engineered to express a reconstituted full-length NS1 protein of 225 aa ending either with the typical “avian” consensus motif ESEV or with the RSKV sequence, which is present in human influenza viruses (Fig. 1A). The E222R amino acid substitution in the NS1-RSKV protein unavoidably changes the amino acid at position 70 in the NS2/nuclear export protein, which is encoded in an overlapping reading frame, from serine to glycine.
The ESEV PL motif reduced viral growth on human, murine, and duck cells but not on chicken embryo fibroblasts.
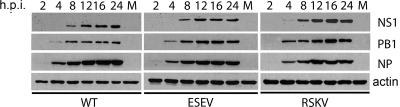
To study the contribution of the C-terminal sequence to viral replication in vitro, we compared the multicyclic growth of the VN/1203-WT, -ESEV, and -RSKV viruses in human A549 epithelial cells, murine NIH 3T3 fibroblasts, chicken embryo fibroblasts (CEFs), and EFB-R1 duck embryo fibroblasts (DEFs) (Fig. 1B to E). This analysis showed that the presence of the ESEV motif compromised viral growth in human and murine cells by more than 1 order of magnitude in comparison to the growth of the WT and the RSKV variant. In addition, we observed a slightly delayed growth kinetic for the RSKV virus compared to the WT. Interestingly, the replication kinetics of the three recombinant viruses on duck cells resembled their growth behaviors in the mammalian cells, with reduced titers of the ESEV variant, but little difference was observed on chicken fibroblasts (Fig. 1D and E). A less pronounced but visible reduction in the growth of the ESEV variant was also apparent in monocyclic infections of human A549 cells, indicating that the basic level of replication of this variant was decelerated compared to that of the WT (Fig. 1F). However, only small differences were found in the accumulation levels and kinetics of the viral NS1, NP, and PB1 proteins for the three viruses in human cells infected at a high multiplicity (Fig. 2). Taken together, these findings indicate that the presence of the PL motif reduces the capacity of the NS1 protein to support viral replication in a species-specific manner.
FIG. 2.
Viral protein expression in infected human A549 cells. A549 cells either were infected with the recombinant VN/1203-WT, -ESEV, or -RSKV virus at an MOI of 5 or were mock treated (M). Cells were lysed at the indicated time points, and the lysates were analyzed for the viral proteins NS1, PB1, and NP by immunoblotting under identical conditions. Cellular actin was detected as a loading control.
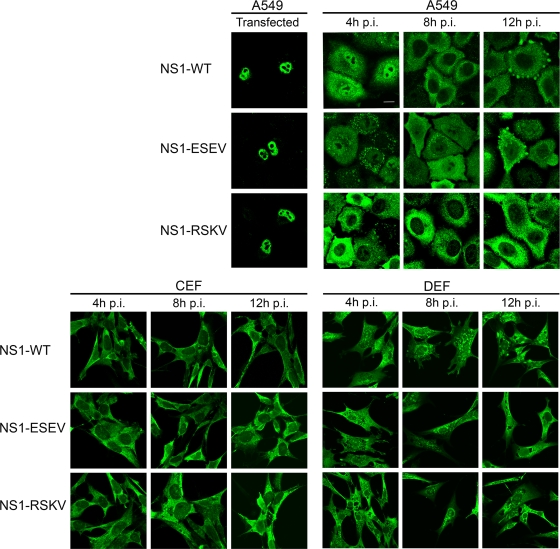
The PL motif modulates intracellular localization of the NS1 protein in human but not in avian cells.
It has not been determined whether the C-terminal amino acids of the truncated NS1 of VN/1203 exhibit NLS activity (44). However, by using fluorescence microscopy, we considered the possibility that the C-terminal elongation in the NS1-ESEV and -RSKV proteins could alter their trafficking to the cell nucleus and influence their activity. First, we localized the three NS1 proteins, expressed from transfected plasmids, in human A549 cells and found that they accumulated indistinguishably in the nucleoplasm, excluding the nucleoli (Fig. 3). Next, we immunolocalized the NS1 proteins in human, chicken, and duck cells infected with the three recombinant viruses from early to late time points of infection (4 to 12 hpi). Interestingly, we observed marked differences in NS1 localization from that in transfected cells; also, the trafficking of the different NS1 proteins differed slightly in human but not in avian cells (Fig. 3). The WT protein was located both in the cytoplasm and in the nucleoplasm at 4 hpi in human cells but was hardly detectable in the nucleus at later time points, indicating that NS1 localization to the nucleus was regulated during infection. Similarly, the reconstituted full-length NS1-ESEV protein localized mainly to the cytoplasm but remained detectable in the nuclear compartment during the whole observation period. However, only a very small fraction of the full-length NS1-RSKV protein localized to the nucleus in human cells at all time points, although it retained four basic amino acids important for NLS-2 activity (K214, R215, R219, R222). In contrast, we observed no differences in the mainly cytosolic localization of the three viral NS1 proteins in chicken and duck fibroblasts, in which a minor fraction, remarkably, was also detected in the nucleoli (Fig. 3). This finding indicates that the nuclear accumulation of the NS1 protein is also controlled in avian cells. The distribution of the NP protein during infection showed similar patterns for WT, ESEV, and RSKV viruses in human and avian cells (data not shown).
FIG. 3.
Intracellular NS1 localization in human and avian cells. (Top left panels) Human A549 cells were transfected with 1 μg of a plasmid encoding the NS1-WT, -RSKV, or -ESEV protein of VN/1203; 24 h later, the cells were prepared for staining with an NS1-specific rabbit antiserum and microscopic analysis. (Top center and right panels and bottom panels) Human A549 cells, chicken embryo fibroblasts (CEFs), and duck embryo fibroblasts (DEFs) were infected with the corresponding recombinant WT, RSKV, or ESEV virus at an MOI of 2. Cells were fixed at the indicated time points, permeabilized, and stained with a NS1-specific rabbit serum and suitable secondary antibodies. Cells were analyzed by confocal laser scanning microscopy. Bar, 10 μm.
The WT and variant NS1 proteins suppress viral IFN-β induction.
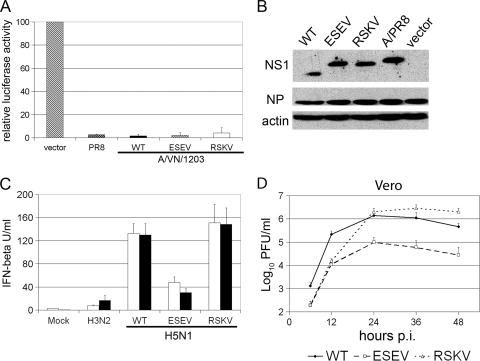
A main function of the NS1 protein is to suppress the activation of the type I IFN genes, which is governed by the RIG I sensor protein for viral genomic RNA (16, 48). The observed differences in NS1 localization in human and avian cell cultures raised the question of whether all NS1 variants inhibited IFN-β induction to the same extent. To address this question, we first investigated the ability of the NS1 proteins to inhibit the viral activation of the IFN-β gene (Fig. 4 A). MDCK cells were cotransfected with an IFN-β promoter luciferase reporter plasmid and one of the corresponding NS1 expression plasmids and were subsequently stimulated by infection with a mutant influenza virus lacking the NS1 gene (delNS1 virus). In this assay, all three H5N1 NS1 proteins were equally able to inhibit viral activation of the IFN-β promoter as efficiently as the NS1 of the A/PR/8/34 strain, which served as a positive control (Fig. 4A) (41). Equal expression of NS1 proteins and infection of cells by the delNS1 virus were confirmed by immunoblot analysis (Fig. 4B).
FIG. 4.
The NS1 protein variants of VN/1203 inhibit viral activation of the human IFN-β promoter. (A) MDCKII cells were transfected with the IFN-β promoter reporter plasmid p125-Luc and either an expression plasmid for the A/VN/1203/NS1-WT, -ESEV, or -RSKV protein or an empty vector (pHW2000). In all assays, plasmid pRL-TK-Luc, encoding Renilla luciferase under the control of a constitutive promoter, was cotransfected and used to normalize the results. Cells were stimulated 1 day posttransfection by infection with the A/PR8 ΔNS1 virus at an MOI of 1 or were mock treated. Luciferase activities in cell extracts were determined 8 h postinfection. The value for the virus-induced increase in vector-transfected cells was arbitrarily set to 100% and was compared to the induction observed in NS1-expressing cells. Experiments were done in triplicate. Error bars indicate standard deviations. (B) Lysates of cells transfected as described for panel A were analyzed by immunoblotting to verify the expression of NS1 proteins and infection with A/PR8 ΔNS1. (C) IFN-β secretion of infected A549 cells. A549 cells were infected with a recombinant VN/1203-WT, -RSKV, or -ESEV virus or with the A/Panama/2007/99 (H3N2) virus at an MOI of 0.01. Aliquots of supernatants were harvested at 24 (open bars) and 48 (solid bars) hpi, and IFN-β concentrations were determined by ELISA. Results are averages for two independent experiments with biological duplicates; error bars indicate standard deviations. (D) To assess viral propagation in IFN-deficient hosts, Vero cells were infected with a recombinant VN/1203-WT, -ESEV, or -RSKV virus at an MOI of 0.01. Aliquots of supernatants were harvested every 12 h, and samples were titrated by plaque assays on MDCK cells. Results are averages for two independent experiments with biological duplicates. Error bars indicate standard deviations.
In order to test whether the HPAIV-H5N1 WT and variant NS1 proteins differed in their capacities to suppress IFN induction during virus infection, human cells were infected at a low multiplicity with the influenza VN/1203-WT, -ESEV, or -RSKV virus, and IFN-β levels in the supernatants were determined by ELISA at 24 and 48 hpi. As a control, cells were infected with a seasonal H3N2 strain (A/Panama/2007/99). Interestingly, we detected 130 to 150 IU/ml of IFN-β in the supernatants of VN/1203-WT or -RSKV virus-infected cells (Fig. 4C). The IFN-β levels in samples collected from ESEV virus-infected cells were considerably lower (∼40 IU), correlating with the reduced replication of this variant (Fig. 1B). However, this level was still 2-fold higher than the levels induced by the seasonal H3N2 virus. It could be argued that the attenuation of the ESEV virus in mammalian cells was influenced by type I IFN. However, this variant also replicated about 1 order of magnitude less well than the WT and RSKV viruses in IFN-deficient Vero cells, suggesting that its attenuation was not caused by enhanced IFN susceptibility (Fig. 4D). These findings recapitulate the reportedly higher capacity of HPAIV-H5N1 viruses than of seasonal strains for type I IFN induction (6, 52). In parallel, they suggest that the C-terminal motif does not play a major role in NS1-dependent inhibition of the type I IFN response by H5N1 viruses in human cells.
The VN/1203-WT, -ESEV, and -RSKV viruses show similar levels of virulence in mice and chickens.
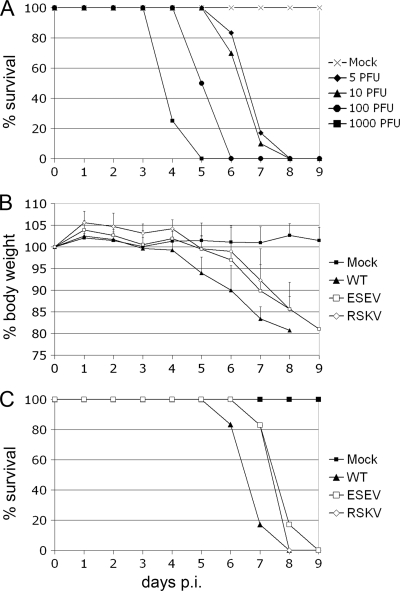
To investigate the pathogenicity of the recombinant VN/1203 WT virus in a mammalian host, we determined the mean lethal dose by intranasal infection of BALB/c mice with decreasing doses of virus (Fig. 5 A). The survival data demonstrated that the 50% mean lethal dose (MLD50) of the recombinant A/VN/1203-WT virus is less than 5 PFU per mouse, consistent with previous findings for the corresponding patient isolate (67). In our experiments, mice either succumbed to the infection or had to be euthanized when they had lost more than 20% of their initial body weight.
FIG. 5.
Virulence of recombinant VN/1203 viruses in BALB/c mice. (A) Groups of six 7-week-old BALB/c mice were inoculated intranasally with the indicated doses of the recombinant VN/1203 WT virus. The percentages of surviving mice during the course of the experiment are given. Mice had to be euthanized when they lost more than 20% of their initial body weight. (B and C) Morbidity and mortality were analyzed for mice intranasally infected with 5 PFU of the VN/1203-WT, -ESEV, or -RSKV virus. (B) The body weights of infected mice were recorded up to 9 days p.i. Error bars indicate standard deviations. (C) The mortality data are expressed as the percentages of mice infected with 5 PFU that survived.
For further studies, we measured body weight and clinical signs after infection with a low lethal dose of 5 PFU per mouse in order to detect small differences in morbidity and mortality (Fig. 5B). The ESEV and RSKV viruses appeared slightly less virulent than the WT virus: a delayed loss of body weight and a slight increase in the mean time to death (MTD) were observed with the RSKV virus (MTD, 7.8 days postinfection [p.i.]) and the ESEV virus (MTD, 8.0 days p.i.) in comparison to the recombinant WT virus (MTD, 7.0 days p.i.). However, no differences were found in overall mortality, since no infected mouse survived beyond day 9 p.i. Subsequently, we studied the systemic spread of the three viruses by determining viral loads in different mouse organs 12 h, 3 days, and 6 days postinfection, but we found no major differences between the three recombinants (Fig. 6). At 12 h, the viruses were recovered only from the lungs. Three days p.i., we were able also to isolate viruses from the heart and spleen. The lower titers of the WT virus than of the ESEV and RSKV variants in the heart did not reach statistical significance (P, >0.05 by Student's test). At day 6, viruses were also found in the brain, kidney, and liver. Again, we observed no significant differences in the organ titers between the three viruses.
FIG. 6.
Determination of viral loads and the spread of VN/1203 viruses to different organs of mice. Groups of four 7-week-old female BALB/c mice were infected with 5 PFU of the VN/1203-WT, -ESEV, or -RSKV virus per mouse and were euthanized 12 h, 3 days (3 d), or 6 days postinfection. The indicated organs were prepared from infected mice at the indicated time points. Organs were homogenized, and cleared supernatants were analyzed by plaque assays on MDCKII cells. Virus titers were determined as PFU/g of tissue. Error bars indicate standard deviations.
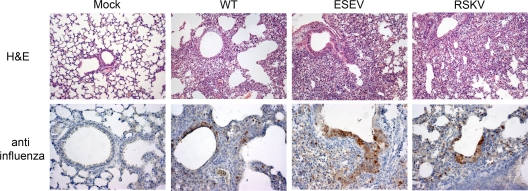
For histopathological analysis, samples from the lungs were fixed with paraformaldehyde and embedded in paraffin. Lung sections were stained with hematoxylin and eosin, and viral antigens were detected by immunohistochemistry (Fig. 7). Lung sections of mice sacrificed at 12 hpi revealed no tissue damage or changes in comparison to the mock control (data not shown). However, lung samples obtained 3 or 6 days p.i. showed perivascular and peribronchiolar infiltrates of lymphocytes and some neutrophil granulocytes infiltrating the alveolar septa, in addition to some bronchial epithelial necrosis. Moreover, necrotic pneumonia with strong bronchiolar epithelial necrosis was found at day 6. The lumina of some bronchioles were filled with neutrophils and macrophages, as well as detritus. Accordingly, we detected viral antigen within type II alveolar and bronchiolar epithelial cells, with similar distribution patterns for the WT, ESEV, and RSKV viruses (Fig. 7).
FIG. 7.
Histopathological analysis of infected mouse lung tissue. BALB/c mice were infected with 5 PFU of the VN/1203-WT, -ESEV, or -RSKV virus and were euthanized 6 days postinfection. Prepared lungs were fixed with paraformaldehyde, embedded in paraffin, and sectioned. Tissues were stained with H&E or were antigen stained using a goat anti-influenza A polyclonal antiserum. Magnifications, ×10 for H&E-stained images and ×20 for antigen-stained images.
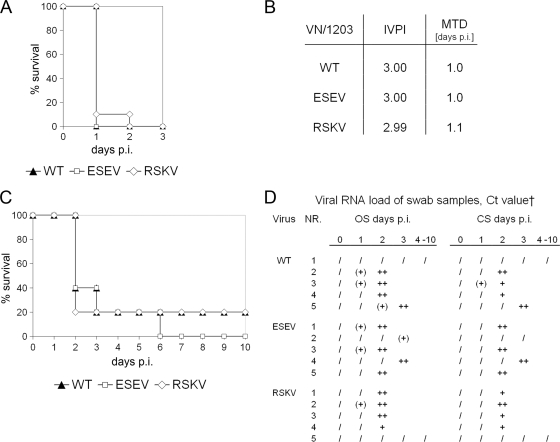
To study the pathogenicity of the influenza VN/1203-WT, -ESEV, and -RSKV viruses in an avian host, we infected groups of 6-week-old chickens (Gallus gallus domesticus) with 104 PFU by the intravenous (Fig. 8 A and B) and oronasal (Fig. 8C and D) routes. Oral and cloacal swabs were taken every day, and samples were analyzed by real-time reverse transcription-PCR (rRT-PCR) (25). Most animals infected intravenously died within 1 day (10 of 10 animals infected with the WT or ESEV virus; 9 of 10 animals infected with the RSKV virus). The calculation of the intravenous pathogenicity index (IVPI) confirmed the high virulence in chickens and revealed almost no differences between the WT (IVPI, 3.0), ESEV (IVPI, 3.0) and RSKV viruses (IVPI, 2.99). Oronasally infected chicken survived for as long as 6 days, but still 3 of 5 chickens infected with either the WT or the ESEV virus and 4 chickens infected with the RSKV virus did not survive past day 2 p.i. The birds showed no visible symptoms until death, presumably due to the short infection period. On day 3, the fourth chickens in the WT and ESEV groups died, and on day 6, the last chicken in the ESEV group succumbed to the infection. One chicken each in the WT and RSKV groups survived until the end of the experiment, but their cloacal and oral swabs were rRT-PCR negative, and no seroconversion was detectable in either bird, suggesting a lack of virus exposure. Thus, we concluded that all three viruses showed comparable virulence in the avian host regardless of the route of infection.
FIG. 8.
Virulence of recombinant VN/1203 viruses in chickens. (A and B) Groups of 10 6-week-old chickens were intravenously infected with 104 PFU of the VN/1203-WT, -ESEV, or -RSKV virus. (A) Percentages of birds surviving on days 1 to 3. (B) Calculated intravenous pathogenicity index (IVPI) for each virus. (C and D) Groups of five 6-week-old chickens were infected oronasally with 104 PFU of the WT, ESEV, or RSKV virus. (C) Percentages of chickens surviving during the course of the experiment. (D) Swab samples were collected daily and analyzed for viral RNA by real-time RT-PCR. OS, oropharyngeal swab; CS, cloacal swab. †, real-time RT-PCR results are presented as threshold cycle (CT) values as follows: /, >40; (+), >30 to 40; +, >25 to <30; ++, >20 to <25; +++, <20.
DISCUSSION
PDZ domains are found ubiquitously in the proteomes of higher eukaryotes; they are present in 0.2 to 0.5% of open reading frames in humans, Drosophila melanogaster, and Caenorhabditis elegans (21). Their structural features mediate interactions with short C-terminal peptides in target proteins in a sequence-specific manner (59). PDZ domain-containing proteins play important roles in various biological pathways involved in development and homeostasis, including the recruitment of proteins to specific membrane compartments and their assembly into supramolecular complexes, and in the establishment of cell polarity (21, 31, 36). Given the shortness of PL motifs, which consist of only 4 to 5 amino acids, it is not surprising that pathogenic viruses and bacteria have evolved gene products with PL motifs to target cellular PDZ domain-dependent protein networks (2, 24, 33). One well-studied example is the human papillomavirus E6 protein, which binds the tumor suppressor protein Scribble, resulting in a loss of epithelial cell polarization and concomitant hyperproliferation (14). Recent in silico analysis identified more than 80 additional viral proteins with predicted C-terminal PDZ recognition motifs that potentially interfere with normal host cell functions (59). Hence, PDZ domain-driven virus-host interactions may be considered an emerging field of research that can lead to an improved understanding of the strategies employed by pathogens to control the host cell.
The virulence of influenza viruses is a multigenic trait, but the viral determinants and pathogenic processes underlying H5N1 infections are only incompletely understood (7, 13). By using reverse genetics, we assessed the concept that the PL motif ESEV, present in the NS1 proteins of many HPAIV-H5N1 strains but not in seasonal virus strains, confers disease-related functions and contributes to enhanced viral virulence (37, 46). Thus, the properties of isogenic virus variants expressing NS1 protein with either the avian influenza virus-like ESEV motif, the human influenza virus-like RSKV motif, or a naturally occurring 10-amino-acid truncation were compared in vitro and in animal models. Growth curve analyses revealed that the avian ESEV motif attenuated viral replication on human A549 cells and murine NIH 3T3 fibroblasts, although viral protein synthesis was not affected during monocyclic infection. These findings suggest that the capacity to interact with PDZ domain networks actually hampers efficient replication of the VN/1203 virus on human cells, which may have led to the selection of this variant lacking the PL motif in the human patient. Length variations in the NS1 protein are not uncommon for human influenza viruses; C-terminal truncations of 10 to 13 amino acids can be detected in 1.4% of seasonal influenza viruses, isolated from human patients, that have circulated since the year 1918 (3). Also, the pandemic H1N1-2009 virus encodes a shortened NS1 protein of 219 amino acids, lacking 11 amino acids present in many seasonal strains. A recent study showed that this truncation hardly affects the replication and virulence of the pandemic H1N1 virus in mammalian hosts, confirming that influenza viruses can adapt so as to propagate efficiently without the functions executed by the NS1 C terminus (20). Hence, there is no absolute requirement for the maintenance of a specific length of NS1 proteins in human strains, but further analysis will be necessary to determine the precise reasons for the occurrence of such variations.
The NS1-PL motif abuts basic amino acids at positions 214 to 219 that, in other virus strains, are part of a nuclear targeting signal (44). We therefore reasoned that the PL motif could affect various virus-supportive NS1 functions in the cytosolic and nuclear compartments by altering its intracellular localization. However, cell-based studies showed no effect on the nuclear accumulation of transiently expressed NS1 in human cells. We did note a surprisingly different and mainly cytosolic localization of the NS1-WT protein during the late stages of virus infection, which may be related to interactions with other viral and cellular components in the cytosol, such as viral RNP, RIG-I, or cellular translation factors (5, 43, 48). The NS1-ESEV and -RSKV proteins differed only slightly from the WT in their intracellular localization during infection. Still, it is possible that the delayed withdrawal of the NS1-ESEV protein from the nucleus contributed to the attenuation of the corresponding virus in human cells. Given the presence of a functional NLS, it was similarly surprising that all three NS1 proteins remained in cytosolic aggregates of chicken and duck cells throughout infection, with only a small fraction entering the nucleus. Here the NS1 proteins localized to the nucleoli, although they clearly lack the C-terminal nucleolar targeting signal present in the NS1 proteins of older human strains (44), a finding that confirms a recent report (61). The functional significance of the localization of NS1 to the nucleolus and the responsible targeting signal remain to be elucidated.
Experimental infections of mice showed that all three recombinant VN/1203 viruses caused highly lethal infections, with only minor differences. The WT virus was slightly more virulent than the ESEV and RSKV variants, as judged by faster weight loss and shorter average survival time. However, no differences were detected in the 100% mortality on day 9, or in viral loads and spread to internal organs. The ESEV virus replicated to titers comparable to those of the WT and RSKV viruses and caused similar pathological changes in the lung. These findings indicate that the specific C-terminal NS1 amino acids cannot be considered a major virulence determinant of HPAIV-H5N1 in mice, although the observed growth restriction in vitro was compensated for on the level of the infected animal. This notion is in full agreement with and confirms the predictions of a recent bioinformatics analysis, in which no significant association between virulence in mammals and the PDZ binding sequence ESEV or EPEV in the NS1 protein was identified (42). Our study therefore documents a clear difference between HPAIV-H5N1 and two viruses in which the conversion of the C-terminal NS1 amino acids into a functional PL motif clearly decreased the lethal virus doses: the mouse-adapted A/WSN/33 virus and a low-pathogenicity H7N1 avian influenza virus (32, 56). Such a distinction in the control of viral pathogenesis between closely related viruses is not without precedent. For instance, a PDZ binding sequence in the Tax1 protein expressed by human T-cell leukemia virus type 1 (HTLV-1) was associated with enhanced proliferation of T cells, whereas this motif is absent in the homologous Tax2 protein of the less leukemogenic HTLV-2 (24, 66).
The severity of H5N1 disease in humans has been associated with an exaggerated cytokine response (6, 8, 11, 29, 53), although a causative link has recently been questioned (12, 15, 51). In fact, we did observe secretion of about 5-fold larger amounts of IFN-β from human lung epithelial cells following infection with the VN/1203-WT virus than following infection with seasonal H3N2 influenza virus. However, the increased IFN-β amounts secreted from H5N1 virus-infected human lung epithelial cells were not caused by a defect in NS1 function or by the PL motif, since all three NS1 variants efficiently inhibited the induction of the human IFN-β promoter. Clearly, further analysis is needed to determine whether the VN/1203 virus produces enhanced levels of viral gene segments with 5′-triphosphate ends that stimulate RIG-I-dependent signaling (49) or whether accumulation of the NS1 protein is delayed or is too low to prevent enhanced IFN-β secretion. Moreover, it will be interesting to compare the induction of cytokines by the three virus variants in the mouse lung in order to test for a correlation with the slightly delayed mortality for the ESEV and RSKV viruses.
The C-terminal PL motif in NS1 is conserved in the vast majority of avian influenza A virus strains, indicating that it is maintained to benefit virus propagation and/or spread in birds. Therefore, it was surprising to find no differences in the growth of the three variants in chicken cells and lower titers for the ESEV variant in duck cells. Moreover, infections of chickens via the intravenous or oronasal route showed indistinguishable high virulence for all three recombinant VN/1203 viruses. Thus, despite the conservation, there was little influence of the NS1-ESEV motif on the high pathogenicity of the VN/1203 virus in chickens. We consider two non-mutually exclusive explanations for those results. First, the contribution of the NS1-PL motif to viral fitness may have remained below the limit of detection due to the background of a highly pathogenic virus, with a multibasic cleavage site in the HA protein being a superior virulence determinant. Second, most avian influenza viruses propagate in a low-pathotype form in cells of the gastrointestinal tracts of feral birds belonging to the orders Anseriformes and Charadriiformes, such as ducks, geese, and gulls (47). It is possible that those hosts, but not gallinaceous poultry like chickens, express one or more PDZ domain proteins that are recognized by the conserved NS1-ESEV motif and that regulate viral propagation and/or dampen pathological processes. In fact, while this article was in revision, Soubies et al. reported that the NS1-ESEV motif, in comparison to the RSKV variant, decreased the replication of a low-pathogenicity H7N1 avian influenza virus in the intestinal mucosae of ducks (56). This phenotype was accompanied by reduced type I IFN induction and intensified excretion of ESEV virus, which, in principle, could confer an advantage by reducing inflammatory reactions and increasing the chances for viral spread. It should be possible to identify such a regulatory factor(s) once large-scale RNA interference-based screening technology becomes available for natural influenza virus host species (35). Taken together, our results indicate that a PL motif at the C terminus of the NS1 protein has no major impact on the virulence of the highly pathogenic H5N1 VN/1203 virus in mice, in chickens, and possibly also in humans. Given the differing findings for mouse-adapted H1N1 and low-pathogenicity avian influenza viruses (32, 56), we concluded that the ESEV motif in the NS1 protein modulates influenza virus pathogenicity in a strain- and host-dependent manner.
Acknowledgments
We thank Gudrun Heins and Andrea Zöhner for excellent technical assistance.
This work was supported by grants from the European Commission (FP6 project “Euroflu,” contract SP5B-CT-2007-044098 [to T.W.]) and the Influenza Research Program “FSI” of the Federal German government (to T.W., D.K., and M.B.).
Footnotes
Published ahead of print on 4 August 2010.
REFERENCES
- 1.Abdel-Ghafar, A. N., T. Chotpitayasunondh, Z. Gao, F. G. Hayden, D. H. Nguyen, M. D. de Jong, A. Naghdaliyev, J. S. Peiris, N. Shindo, S. Soeroso, and T. M. Uyeki. 2008. Update on avian influenza A (H5N1) virus infection in humans. N. Engl. J. Med. 358:261-273. [DOI] [PubMed] [Google Scholar]
- 2.Alto, N. M., F. Shao, C. S. Lazar, R. L. Brost, G. Chua, S. Mattoo, S. A. McMahon, P. Ghosh, T. R. Hughes, C. Boone, and J. E. Dixon. 2006. Identification of a bacterial type III effector family with G protein mimicry functions. Cell 124:133-145. [DOI] [PubMed] [Google Scholar]
- 3.Bao, Y., P. Bolotov, D. Dernovoy, B. Kiryutin, L. Zaslavsky, T. Tatusova, J. Ostell, and D. Lipman. 2008. The influenza virus resource at the National Center for Biotechnology Information. J. Virol. 82:596-601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bergmann, M., A. Garcia-Sastre, E. Carnero, H. Pehamberger, K. Wolff, P. Palese, and T. Muster. 2000. Influenza virus NS1 protein counteracts PKR-mediated inhibition of replication. J. Virol. 74:6203-6206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burgui, I., T. Aragon, J. Ortin, and A. Nieto. 2003. PABP1 and eIF4GI associate with influenza virus NS1 protein in viral mRNA translation initiation complexes. J. Gen. Virol. 84:3263-3274. [DOI] [PubMed] [Google Scholar]
- 6.Chan, M. C., C. Y. Cheung, W. H. Chui, S. W. Tsao, J. M. Nicholls, Y. O. Chan, R. W. Chan, H. T. Long, L. L. Poon, Y. Guan, and J. S. Peiris. 2005. Proinflammatory cytokine responses induced by influenza A (H5N1) viruses in primary human alveolar and bronchial epithelial cells. Respir. Res. 6:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen, H., R. A. Bright, K. Subbarao, C. Smith, N. J. Cox, J. M. Katz, and Y. Matsuoka. 2007. Polygenic virulence factors involved in pathogenesis of 1997 Hong Kong H5N1 influenza viruses in mice. Virus Res. 128:159-163. [DOI] [PubMed] [Google Scholar]
- 8.Cheung, C. Y., L. L. Poon, A. S. Lau, W. Luk, Y. L. Lau, K. F. Shortridge, S. Gordon, Y. Guan, and J. S. Peiris. 2002. Induction of proinflammatory cytokines in human macrophages by influenza A (H5N1) viruses: a mechanism for the unusual severity of human disease? Lancet 360:1831-1837. [DOI] [PubMed] [Google Scholar]
- 9.Conenello, G. M., D. Zamarin, L. A. Perrone, T. Tumpey, and P. Palese. 2007. A single mutation in the PB1-F2 of H5N1 (HK/97) and 1918 influenza A viruses contributes to increased virulence. PLoS Pathog. 3:1414-1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dauber, B., G. Heins, and T. Wolff. 2004. The influenza B virus nonstructural NS1 protein is essential for efficient viral growth and antagonizes beta interferon induction. J. Virol. 78:1865-1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Jong, M. D., C. P. Simmons, T. T. Thanh, V. M. Hien, G. J. Smith, T. N. Chau, D. M. Hoang, N. V. Chau, T. H. Khanh, V. C. Dong, P. T. Qui, B. V. Cam, D. Q. Ha, Y. Guan, J. S. Peiris, N. T. Chinh, T. T. Hien, and J. Farrar. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat. Med. 12:1203-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deng, R., M. Lu, C. Korteweg, Z. Gao, M. A. McNutt, J. Ye, T. Zhang, and J. Gu. 2008. Distinctly different expression of cytokines and chemokines in the lungs of two H5N1 avian influenza patients. J. Pathol. 216:328-336. [DOI] [PubMed] [Google Scholar]
- 13.de Wit, E., Y. Kawaoka, M. D. de Jong, and R. A. Fouchier. 2008. Pathogenicity of highly pathogenic avian influenza virus in mammals. Vaccine 26(Suppl. 4):D54-D58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doorbar, J. 2006. Molecular biology of human papillomavirus infection and cervical cancer. Clin. Sci. (Lond.) 110:525-541. [DOI] [PubMed] [Google Scholar]
- 15.Droebner, K., S. J. Reiling, and O. Planz. 2008. Role of hypercytokinemia in NF-κB p50-deficient mice after H5N1 influenza A virus infection. J. Virol. 82:11461-11466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gack, M. U., R. A. Albrecht, T. Urano, K. S. Inn, I. C. Huang, E. Carnero, M. Farzan, S. Inoue, J. U. Jung, and A. Garcia-Sastre. 2009. Influenza A virus NS1 targets the ubiquitin ligase TRIM25 to evade recognition by the host viral RNA sensor RIG-I. Cell Host Microbe 5:439-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garcia-Sastre, A., A. Egorov, D. Matassov, S. Brandt, D. E. Levy, J. E. Durbin, P. Palese, and T. Muster. 1998. Influenza A virus lacking the NS1 gene replicates in interferon-deficient systems. Virology 252:324-330. [DOI] [PubMed] [Google Scholar]
- 18.Gu, J., Z. Xie, Z. Gao, J. Liu, C. Korteweg, J. Ye, L. T. Lau, J. Lu, B. Zhang, M. A. McNutt, M. Lu, V. M. Anderson, E. Gong, A. C. Yu, and W. I. Lipkin. 2007. H5N1 infection of the respiratory tract and beyond: a molecular pathology study. Lancet 370:1137-1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hale, B. G., R. E. Randall, J. Ortin, and D. Jackson. 2008. The multifunctional NS1 protein of influenza A viruses. J. Gen. Virol. 89:2359-2376. [DOI] [PubMed] [Google Scholar]
- 20.Hale, B. G., J. Steel, B. Manicassamy, R. A. Medina, J. Ye, D. Hickman, A. C. Lowen, D. R. Perez, and A. Garcia-Sastre. 2010. Mutations in the NS1 C-terminal tail do not enhance replication or virulence of the 2009 pandemic H1N1 influenza A virus. J. Gen. Virol. 91:1737-1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris, B. Z., and W. A. Lim. 2001. Mechanism and role of PDZ domains in signaling complex assembly. J. Cell Sci. 114:3219-3231. [DOI] [PubMed] [Google Scholar]
- 22.Hatada, E., S. Saito, and R. Fukuda. 1999. Mutant influenza viruses with a defective NS1 protein cannot block the activation of PKR in infected cells. J. Virol. 73:2425-2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hatta, M., P. Gao, P. Halfmann, and Y. Kawaoka. 2001. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science 293:1840-1842. [DOI] [PubMed] [Google Scholar]
- 24.Higuchi, M., and M. Fujii. 2009. Distinct functions of HTLV-1 Tax1 from HTLV-2 Tax2 contribute key roles to viral pathogenesis. Retrovirology 6:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoffmann, B., T. Harder, E. Starick, K. Depner, O. Werner, and M. Beer. 2007. Rapid and highly sensitive pathotyping of avian influenza A H5N1 virus by using real-time reverse transcription-PCR. J. Clin. Microbiol. 45:600-603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoffmann, E., G. Neumann, Y. Kawaoka, G. Hobom, and R. G. Webster. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. U. S. A. 97:6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Horimoto, T., K. Nakayama, S. P. Smeekens, and Y. Kawaoka. 1994. Proprotein-processing endoproteases PC6 and furin both activate hemagglutinin of virulent avian influenza viruses. J. Virol. 68:6074-6078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hui, D. S. 2008. Review of clinical symptoms and spectrum in humans with influenza A/H5N1 infection. Respirology 13(Suppl. 1):S10-S13. [DOI] [PubMed] [Google Scholar]
- 29.Hui, K. P., S. M. Lee, C. Y. Cheung, I. H. Ng, L. L. Poon, Y. Guan, N. Y. Ip, A. S. Lau, and J. S. Peiris. 2009. Induction of proinflammatory cytokines in primary human macrophages by influenza A virus (H5N1) is selectively regulated by IFN regulatory factor 3 and p38 MAPK. J. Immunol. 182:1088-1098. [DOI] [PubMed] [Google Scholar]
- 30.Hulse-Post, D. J., J. Franks, K. Boyd, R. Salomon, E. Hoffmann, H. L. Yen, R. J. Webby, D. Walker, T. D. Nguyen, and R. G. Webster. 2007. Molecular changes in the polymerase genes (PA and PB1) associated with high pathogenicity of H5N1 influenza virus in mallard ducks. J. Virol. 81:8515-8524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hung, A. Y., and M. Sheng. 2002. PDZ domains: structural modules for protein complex assembly. J. Biol. Chem. 277:5699-5702. [DOI] [PubMed] [Google Scholar]
- 32.Jackson, D., M. J. Hossain, D. Hickman, D. R. Perez, and R. A. Lamb. 2008. A new influenza virus virulence determinant: the NS1 protein four C-terminal residues modulate pathogenicity. Proc. Natl. Acad. Sci. U. S. A. 105:4381-4386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Javier, R. T. 2008. Cell polarity proteins: common targets for tumorigenic human viruses. Oncogene 27:7031-7046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiao, P., G. Tian, Y. Li, G. Deng, Y. Jiang, C. Liu, W. Liu, Z. Bu, Y. Kawaoka, and H. Chen. 2008. A single-amino-acid substitution in the NS1 protein changes the pathogenicity of H5N1 avian influenza viruses in mice. J. Virol. 82:1146-1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karlas, A., N. Machuy, Y. Shin, K. P. Pleissner, A. Artarini, D. Heuer, D. Becker, H. Khalil, L. A. Ogilvie, S. Hess, A. P. Maurer, E. Muller, T. Wolff, T. Rudel, and T. F. Meyer. 2010. Genome-wide RNAi screen identifies human host factors crucial for influenza virus replication. Nature 463:818-822. [DOI] [PubMed] [Google Scholar]
- 36.Kim, E., and M. Sheng. 2004. PDZ domain proteins of synapses. Nat. Rev. Neurosci. 5:771-781. [DOI] [PubMed] [Google Scholar]
- 37.Krug, R. M. 2006. Virology clues to the virulence of H5N1 viruses in humans. Science 311:1562-1563. [DOI] [PubMed] [Google Scholar]
- 38.Letunic, I., T. Doerks, and P. Bork. 2009. SMART 6: recent updates and new developments. Nucleic Acids Res. 37:D229-D232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li, Z., H. Chen, P. Jiao, G. Deng, G. Tian, Y. Li, E. Hoffmann, R. G. Webster, Y. Matsuoka, and K. Yu. 2005. Molecular basis of replication of duck H5N1 influenza viruses in a mammalian mouse model. J. Virol. 79:12058-12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li, Z., Y. Jiang, P. Jiao, A. Wang, F. Zhao, G. Tian, X. Wang, K. Yu, Z. Bu, and H. Chen. 2006. The NS1 gene contributes to the virulence of H5N1 avian influenza viruses. J. Virol. 80:11115-11123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ludwig, S., X. Wang, C. Ehrhardt, H. Zheng, N. Donelan, O. Planz, S. Pleschka, A. Garcia-Sastre, G. Heins, and T. Wolff. 2002. The influenza A virus NS1 protein inhibits activation of Jun N-terminal kinase and AP-1 transcription factors. J. Virol. 76:11166-11171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lycett, S. J., M. J. Ward, F. I. Lewis, A. F. Poon, S. L. Kosakovsky Pond, and A. J. Brown. 2009. Detection of mammalian virulence determinants in highly pathogenic avian influenza H5N1 viruses: multivariate analysis of published data. J. Virol. 83:9901-9910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marion, R. M., T. Zurcher, S. de la Luna, and J. Ortin. 1997. Influenza virus NS1 protein interacts with viral transcription-replication complexes in vivo. J. Gen. Virol. 78(Pt. 10):2447-2451. [DOI] [PubMed] [Google Scholar]
- 44.Melen, K., L. Kinnunen, R. Fagerlund, N. Ikonen, K. Y. Twu, R. M. Krug, and I. Julkunen. 2007. Nuclear and nucleolar targeting of influenza A virus NS1 protein: striking differences between different virus subtypes. J. Virol. 81:5995-6006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Min, J. Y., and R. M. Krug. 2006. The primary function of RNA binding by the influenza A virus NS1 protein in infected cells: inhibiting the 2′-5′ oligo(A) synthetase/RNase L pathway. Proc. Natl. Acad. Sci. U. S. A. 103:7100-7105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Obenauer, J. C., J. Denson, P. K. Mehta, X. Su, S. Mukatira, D. B. Finkelstein, X. Xu, J. Wang, J. Ma, Y. Fan, K. M. Rakestraw, R. G. Webster, E. Hoffmann, S. Krauss, J. Zheng, Z. Zhang, and C. W. Naeve. 2006. Large-scale sequence analysis of avian influenza isolates. Science 311:1576-1580. [DOI] [PubMed] [Google Scholar]
- 47.Olsen, B., V. J. Munster, A. Wallensten, J. Waldenstrom, A. D. Osterhaus, and R. A. Fouchier. 2006. Global patterns of influenza A virus in wild birds. Science 312:384-388. [DOI] [PubMed] [Google Scholar]
- 48.Opitz, B., A. Rejaibi, B. Dauber, J. Eckhard, M. Vinzing, B. Schmeck, S. Hippenstiel, N. Suttorp, and T. Wolff. 2007. IFNβ induction by influenza A virus is mediated by RIG-I which is regulated by the viral NS1 protein. Cell. Microbiol. 9:930-938. [DOI] [PubMed] [Google Scholar]
- 49.Rehwinkel, J., C. P. Tan, D. Goubau, O. Schulz, A. Pichlmair, K. Bier, N. Robb, F. Vreede, W. Barclay, E. Fodor, and E. S. C. Reis. 2010. RIG-I detects viral genomic RNA during negative-strand RNA virus infection. Cell 140:397-408. [DOI] [PubMed] [Google Scholar]
- 50.Rott, R., H. D. Klenk, Y. Nagai, and M. Tashiro. 1995. Influenza viruses, cell enzymes, and pathogenicity. Am. J. Respir. Crit. Care Med. 152:S16-S19. [DOI] [PubMed] [Google Scholar]
- 51.Salomon, R., E. Hoffmann, and R. G. Webster. 2007. Inhibition of the cytokine response does not protect against lethal H5N1 influenza infection. Proc. Natl. Acad. Sci. U. S. A. 104:12479-12481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sandbulte, M. R., A. C. Boon, R. J. Webby, and J. M. Riberdy. 2008. Analysis of cytokine secretion from human plasmacytoid dendritic cells infected with H5N1 or low-pathogenicity influenza viruses. Virology 381:22-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schmolke, M., D. Viemann, J. Roth, and S. Ludwig. 2009. Essential impact of NF-κB signaling on the H5N1 influenza A virus-induced transcriptome. J. Immunol. 183:5180-5189. [DOI] [PubMed] [Google Scholar]
- 54.Schneider, J., B. Dauber, K. Melen, I. Julkunen, and T. Wolff. 2009. Analysis of influenza B virus NS1 protein trafficking reveals a novel interaction with nuclear speckle domains. J. Virol. 83:701-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Seo, S. H., E. Hoffmann, and R. G. Webster. 2002. Lethal H5N1 influenza viruses escape host anti-viral cytokine responses. Nat. Med. 8:950-954. [DOI] [PubMed] [Google Scholar]
- 56.Soubies, S. M., C. Volmer, G. Croville, J. Loupias, B. Peralta, P. Costes, C. Lacroux, J. L. Guerin, and R. Volmer. 2010. Species-specific contribution of the four C-terminal amino acids of influenza A virus NS1 protein to virulence. J. Virol. 84:6733-6747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Steel, J., A. C. Lowen, S. Mubareka, and P. Palese. 2009. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog. 5:e1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Subbarao, E. K., W. London, and B. R. Murphy. 1993. A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. J. Virol. 67:1761-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tonikian, R., Y. Zhang, S. L. Sazinsky, B. Currell, J. H. Yeh, B. Reva, H. A. Held, B. A. Appleton, M. Evangelista, Y. Wu, X. Xin, A. C. Chan, S. Seshagiri, L. A. Lasky, C. Sander, C. Boone, G. D. Bader, and S. S. Sidhu. 2008. A specificity map for the PDZ domain family. PLoS Biol. 6:e239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tran, T. H., T. L. Nguyen, T. D. Nguyen, T. S. Luong, P. M. Pham, V. C. Nguyen, T. S. Pham, C. D. Vo, T. Q. Le, T. T. Ngo, B. K. Dao, P. P. Le, T. T. Nguyen, T. L. Hoang, V. T. Cao, T. G. Le, D. T. Nguyen, H. N. Le, K. T. Nguyen, H. S. Le, V. T. Le, D. Christiane, T. T. Tran, M. de Jong, C. Schultsz, P. Cheng, W. Lim, P. Horby, and J. Farrar. 2004. Avian influenza A (H5N1) in 10 patients in Vietnam. N. Engl. J. Med. 350:1179-1188. [DOI] [PubMed] [Google Scholar]
- 61.Volmer, R., B. Mazel-Sanchez, C. Volmer, S. M. Soubies, and J. L. Guerin. 2010. Nucleolar localization of influenza A NS1: striking differences between mammalian and avian cells. Virol. J. 7:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.WHO. 5 July 2010. Cumulative number of confirmed human cases of avian influenza A/(H5N1) reported to WHO. WHO, Geneva, Switzerland. www.who.int/csr/disease/avian_influenza/country/cases_table_2010_07_05/en/index.html.
- 63.Wolff, T., and S. Ludwig. 2009. Influenza viruses control the vertebrate type I interferon system: factors, mechanisms, and consequences. J. Interferon Cytokine Res. 29:549-557. [DOI] [PubMed] [Google Scholar]
- 64.Wolff, T., F. Zielecki, M. Abt, D. Voss, I. Semmler, and M. Matthaei. 2008. Sabotage of antiviral signaling and effectors by influenza viruses. Biol. Chem. 389:1299-1305. [DOI] [PubMed] [Google Scholar]
- 65.World Organisation for Animal Health. 17 January 2010. Manual of diagnostic tests for terrestrial animals. http://www.oie.int/fr/normes/mmanual/A_summry.htm.
- 66.Xie, L., B. Yamamoto, A. Haoudi, O. J. Semmes, and P. L. Green. 2006. PDZ binding motif of HTLV-1 Tax promotes virus-mediated T-cell proliferation in vitro and persistence in vivo. Blood 107:1980-1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yen, H. L., A. S. Monto, R. G. Webster, and E. A. Govorkova. 2005. Virulence may determine the necessary duration and dosage of oseltamivir treatment for highly pathogenic A/Vietnam/1203/04 influenza virus in mice. J. Infect. Dis. 192:665-672. [DOI] [PubMed] [Google Scholar]
- 68.Yu, H., Z. Gao, Z. Feng, Y. Shu, N. Xiang, L. Zhou, Y. Huai, L. Feng, Z. Peng, Z. Li, C. Xu, J. Li, C. Hu, Q. Li, X. Xu, X. Liu, Z. Liu, L. Xu, Y. Chen, H. Luo, L. Wei, X. Zhang, J. Xin, J. Guo, Q. Wang, Z. Yuan, K. Zhang, W. Zhang, J. Yang, X. Zhong, S. Xia, L. Li, J. Cheng, E. Ma, P. He, S. S. Lee, Y. Wang, T. M. Uyeki, and W. Yang. 2008. Clinical characteristics of 26 human cases of highly pathogenic avian influenza A (H5N1) virus infection in China. PLoS One 3:e2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yuen, K. Y., P. K. Chan, M. Peiris, D. N. Tsang, T. L. Que, K. F. Shortridge, P. T. Cheung, W. K. To, E. T. Ho, R. Sung, and A. F. Cheng. 1998. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet 351:467-471. [DOI] [PubMed] [Google Scholar]