Abstract
OBJECTIVES:
To study the prevalence of noncalcified plaque in asymptomatic low-risk patients with no or mild coronary artery calcium (CAC).
METHODS:
From 502 patients with coronary risk factors who underwent 64-slice computed tomography, 224 asymptomatic patients were identified with no CAC (n=117) or mild CAC (n=107; defined as patients with Agatston scores from 1 to 100).
RESULTS:
Patients with no CAC were younger and had diabetes less often. Medications and laboratory data were not significantly different between the two groups. The prevalence of noncalcified plaque was 11.1% in patients with no CAC and 23.4% in the mild CAC group (P=0.0142). Multiple plaques were detected in 2.6% of the group with no CAC and 3.7% of the group with mild CAC (P=0.5934). Significant coronary artery stenosis was found in one patient in the group with no CAC (0.9%) and three patients in the group with mild CAC (2.8%, P=0.3506).
CONCLUSIONS:
Significant percentages of noncalcified plaque were found in asymptomatic low-risk patients with no or mild coronary calcium.
Keywords: Computed tomography, Coronary artery calcium, Coronary artery disease, Noncalcified coronary plaque
Abstract
OBJECTIFS :
Étudier la prévalence de plaque non calcifiée chez les patients asymptomatiques à faible risque ayant peu de calcium, sinon aucun, dans les artères coronaires (CAC).
MÉTHODOLOGIE :
Des 502 patients ayant des facteurs de risque coronarien qui ont subi une tomodensitométrie à 64 coupes, on a établi que 224 patients asymptomatiques n’avaient pas de CAC (n=117) ou en avaient peu (n=107; défini comme les patients ayant un indice d’Agatston de 1 à 100).
RÉSULTATS :
Les patients n’ayant pas de CAC étaient plus jeunes et moins souvent diabétiques. La différence entre la médication et les données de laboratoire n’était pas significative entre les deux groupes. La prévalence de plaque non calcifiée s’élevait à 11,1 % chez les patients n’ayant pas de CAC et à 23,4 % dans le groupe en ayant peu (P=0,0142). On a décelé de multiples plaques dans 2,6 % du groupe n’ayant pas de CAC et dans 3,7 % de celui en ayant peu (P=0,5934). On a découvert une sténose marquée des artères coronaires chez un patient du groupe n’ayant pas de CAC (0,9 %) et chez trois patients de celui en ayant peu (2,8 %, P=0,3506).
CONCLUSION :
On a découvert des pourcentages importants de plaque non calcifiée chez les patients asymptomatiques à faible risque ayant peu de calcium, sinon aucun, dans les artères coronaires.
NONCALCIFIED CORONARY PLAQUE
Coronary artery disease is the leading cause of death in developing and developed countries (1). Assessment of conventional risk factor burden is necessary but may not accurately estimate the risk of cardiovascular disease (2). Most patients in whom myocardial infarction (MI) develops have one or more conventional risk factors for atherosclerosis, but these risk factors are also prevalent in the general population (3,4).
Coronary artery calcification (CAC) signifies the presence of coronary atherothrombosis, and a strong linear correlation exists between total coronary artery atherothrombotic plaque burden and the extent of CAC (5,6). Patients without detectable calcium have a very low rate of coronary artery disease death or MI (0.4%) over three to five years of observation (7–11).
Sixty-four-slice computed tomography (CT) has emerged as a promising modality to evaluate coronary artery disease. Sixty-four-slice CT has been shown to have both a sensitivity and a specificity in the range of 95% for the detection of hemodynamically relevant stenosis, which is higher than those associated with stress myocardial perfusion imaging (12–16). In particular, its ability to detect coronary plaque noninvasively is increasingly being recognized (17–22).
Therefore, we studied the prevalence of noncalcified plaque in asymptomatic patients with no or mild CAC by 64-slice CT.
METHODS
Patients
From December 2005 through March 2007, 502 patients with coronary risk factors underwent 64-slice CT. Among these patients, asymptomatic patients who were evaluated in a primary prevention program in an outpatient setting were selected.
Patients were excluded who had angina pectoris or angina-equivalent symptoms; a stress test or coronary angiography during the one year before entry into the study; a history of MI, heart failure or coronary revascularization; or electrocardiographic evidence of Q-wave MI, ischemic ST segment or T-wave changes, or complete left bundle branch block.
Then, patients with no CAC (no CAC group) and those with mild CAC (mild CAC group) were selected. The no CAC group was defined as patients with no coronary calcium and the mild CAC group was defined as patients with Agatston scores from 1 to 100, because an Agatston score of 100 is a frequently used cut-off point for risk assessment.
The 64-slice CT
All patients were scanned with a 64-slice CT scanner (SOMATOM Sensation 64 Cardiac; Siemens AG Medical Solutions, Germany).
Patients with a heart rate of more than 70 beats/min received oral metoprolol 20 mg before the 64-slice CT scan. To achieve coronary vasodilation, 0.8 mg of sublingual nitroglycerin was administered before the scan.
A native scan without contrast dye was performed to determine the total calcium burden of the coronary tree (sequential scan with 32 mm × 0.6 mm collimation, tube current 60 mA at 120 kV). Contrast-enhanced CT angiography data were acquired with the use of a spiral scan with 32 mm × 0.6 mm collimation, 330 ms gantry rotation, a pitch of 0.2 and a tube voltage of 120 kV.
A total of 64 overlapping 0.6 mm slices per rotation were acquired with the use of a focal spot periodically moving in the longitudinal direction (z-flying focal spot).
Tube current was modulated according to the electrocardiogram, with a maximum current of 850 mA to 950 mA during a time period of approximately 330 ms centred at 375 ms before the next R wave and reduction by 80% during the remaining cardiac cycle. Contrast agent (60 mL to 70 mL; 370 mg iodine/mL) was injected intravenously (4.0 mL/s), followed by a 30 mL saline chaser. Transaxial images were reconstructed using an electrocardiogram-gated half-scan reconstruction algorithm (temporal resolution 164 ms) and a B30f kernel.
The 64-slice CT image interpretation
CT data sets were transferred to an off-line workstation (Aquarius NetStation; Terarecon Inc, USA) for image analysis. Total calcium scores for all patients were calculated using dedicated software and were expressed as Agatston scores. The Agatston score is a commonly used scoring method that calculates the total amount of calcium on the basis of the number, areas and peak Hounsfield units (HU) of the detected calcified lesions (23).
Two reviewers independently evaluated the contrast-enhanced 64-slice CT scans with maximum-intensity and curved multiplanar reconstruction techniques along multiple longitudinal axes and transversely. The coronary artery tree was segmented according to a modified American Heart Association classification system and the segments were evaluated visually for the presence of coronary artery stenosis (24).
Noncalcified atherosclerotic plaque was defined as any discernible structure that could be clearly assignable to the vessel wall, that had a CT density of lower than the contrast-enhanced coronary lumen but greater than the surrounding connective tissue, and that could be identified in at least two independent planes (14). Standard display settings were used for the evaluation of the contrast-enhanced 64-slice CT scans (window width 800 HU; window centre 250 HU).
Two observers identified coronary segments using a modified American Heart Association classification. Segments were classified as normal (smooth parallel or tapering borders), having nonsignificant stenosis (luminal irregularities or less than 50% stenosis) or having significant stenosis.
Informed consent for the clinical procedure and research protocol was received from all studied patients. The present study was approved by an institutional review board.
Statistical analysis
Data are expressed as mean ± SD. Discrete variables were expressed as counts or percentages, and were compared using the χ2 or Fisher’s exact tests. The difference in the prevalence of coronary plaque between the two groups was calculated by the Mann-Whitney U test. P<0.05 was considered to be statistically significant.
RESULTS
A total of 224 asymptomatic patients were identified with no CAC (n=117) and with mild CAC (n=107).
Clinical characteristics of the patients studied are shown in Table 1. Patients in the no CAC group were younger and had a lower prevalence of diabetes. Medications and laboratory data were not significantly different between the two groups.
TABLE 1.
Clinical characteristics of patients
| No CAC (n=117) | Mild CAC (n=107) | P | |
|---|---|---|---|
| Age, years, mean ± SD | 62.4±10.4 | 67.4±8.5 | 0.0003 |
| Male sex | 59 (50.4) | 59 (55.1) | 0.9999 |
| Hypertension | 51 (43.6) | 60 (56.1) | 0.0616 |
| Hyperlipidemia | 48 (41.0) | 55 (51.4) | 0.1193 |
| Diabetes mellitus | 19 (16.2) | 36 (33.6) | 0.0024 |
| Active smoker | 34 (29.1) | 36 (33.6) | 0.4596 |
| Obesity | 22 (18.8) | 24 (22.4) | 0.5023 |
| Therapy | |||
| Acetylsalicylic acid | 21 (17.9) | 20 (18.7) | 0.8596 |
| Statin | 40 (34.2) | 35 (32.7) | 0.4548 |
| ARB/ACE-I | 51 (43.6) | 48 (44.9) | 0.6593 |
| CCB | 40 (34.2) | 38 (35.5) | 0.7663 |
| BB | 13 (11.1) | 8 (7.5) | 0.2467 |
| Laboratory data, mean ± SD | |||
| BS, mmol/L | 7.3±3.2 | 8.0±3.3 | 0.2736 |
| HbA1c, % | 6.70±1.74 | 6.62±1.40 | 0.9767 |
| TC, mmol/L | 5.52±0.91 | 5.64±0.97 | 0.7046 |
| TG, mmol/L | 1.64±0.96 | 1.98±1.01 | 0.1585 |
| HDL-C, mmol/L | 1.45±0.41 | 1.38±0.34 | 0.4654 |
| LDL-C, mmol/L | 2.84±0.60 | 3.78±0.92 | 0.2294 |
Data presented as n (%) unless otherwise indicated. ACE-I Angiotensin-converting enzyme inhibitor; ARB Angiotensin receptor blocker; BB Beta-blocker; BS Blood sugar; CAC Coronary artery calcium; CCB Calcium channel blocker; DM Diabetes mellitus; HbA1c Hemoglobin A1c; HDL-C High-density lipoprotein cholesterol; LDL-C Low-density lipoprotein cholesterol; TC Total cholesterol; TG Triglyceride
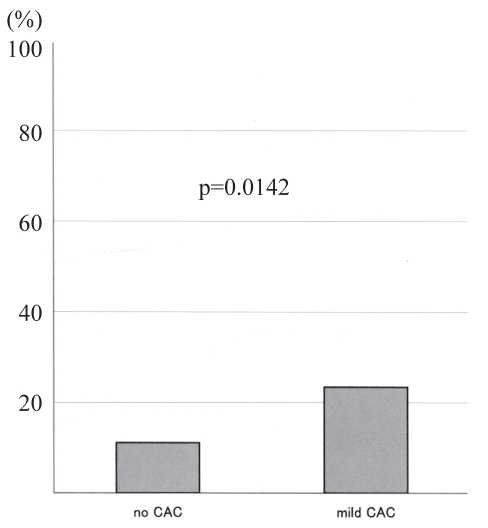
Figure 1 shows the prevalence of noncalcified plaque in the two groups. The incidence of noncalcified plaque was 11.1% in the no CAC group and 23.4% in the mild CAC group (P=0.0142).
Figure 1).
Prevalence of noncalcified plaque. CAC Coronary artery calcium
Table 2 shows the number of noncalcified plaques in the two groups. Multiple plaques were detected in 2.6% of the no CAC group and 3.7% of the mild CAC group (P=0.5934).
TABLE 2.
Number of noncalcified plaque in the two groups
| Noncalcified plaque, n | No CAC (n=117), n | Mild CAC (n=107), n | P |
|---|---|---|---|
| 0 | 104 | 82 | |
| 1 | 10 | 21 | |
| 2 | 2 | 3 | |
| 3 or more | 1 | 1 | 0.5934 |
CAC Coronary artery calcium
Significant coronary artery stenosis was found in one patient in the no CAC group (0.9%) and three patients in the mild CAC group (2.8%, P=0.3506).
DISCUSSION
The present study’s results showed that the prevalence of noncalcified plaque was 11.1% in the no CAC group and 23.4% in the mild CAC group, a significant percentage of nonobstructive plaque.
CAC provides an accurate estimate of total coronary plaque burden (5,25,26) and has been found to be the most powerful predictor of cardiac events, providing independent and incremental information over risk factor-based assessment of the asymptomatic patients (7–11).
Individuals with CAC scores of 0 have not yet developed detectable calcified coronary plaque, but they may have fatty streaking and early stages of plaque, and may have obstructive disease. Noncalcified plaques are present in many young adults (27).
Several studies have investigated the prevalence of noncalcified plaque in patients without coronary calcium. Cheng et al (28) studied 416 low-intermediate-risk patients without coronary calcium and found noncalcified plaque in 6.5% of them. Hausleiter et al (29) found noncalcified plaque in 15.9% of patients with intermediate risk and no coronary calcium. Schroeder et al (30) found noncalcified plaque in 10% of 29 patients with multiple risk factors. Rubinshtein et al (31) found noncalcified plaque in 20.0% of 125 patients with chest pain syndrome.
The incidence of noncalcified plaque was similar between our study and other studies. However, the incidence of significant coronary artery stenosis is quite different. We found significant stenosis in only 0.9% of patients, but the incidence of significant stenosis was 6.0% in the study by Cheng et al (28) and 7.2% in the study by Rubinshtein et al (31). Our study patients represent a lower-risk population than previous similar studies, explaining the lower prevalence of significant coronary stenosis.
As for patients with mild coronary calcium, the incidence of non-calcified plaque was 23.4% in our patients. However, the incidence was 65.2% in the study by Cheng et al (28) and 53.8% in the study by Rubinshtein et al (31). Also, the incidence of significant stenosis was 2.8% in our study compared with 8.7% and 17.0% in other studies (28,31).
A recent study by Schenker et al (32) using a hybrid positron emission tomography/CT scanner showed that, even in patients with no CAC, the frequency of ischemia was 16.0%, and its absence only afforded a negative predictive value of 84.0%. Risk-adjusted survival analysis demonstrated a stepwise increase in event rates with increasing CAC scores in patients with and without ischemia on positron emission tomography myocardial perfusion imaging.
Also, Detrano et al (33) demonstrated that while the coronary event rate was very low in patients with a CAC score of 0, there was a significant event rate in patients with a CAC score of 1 to 100. They found that the hazard ratio of major coronary events in patients with a CAC score of 1 to 100 was 3.89 compared with patients without CAC.
Thus, although increasing CAC content is generally predictive of a higher likelihood of ischemia, the finding of no CAC or a low CAC level does not guarantee good endothelial/coronary health, and such patients may still be at risk.
Our results show that the asymptomatic population, from which intermediate- and high-risk profile patients are excluded, still has 10% to 20% of nonobstructive plaque, which is a significant finding, emphasizing the potential risk in these patients and the need for intense risk factor modification with prophylactic medical treatment.
Limitations
There were some limitations in our study. First, the number of studied patients was relatively small. Therefore, a large study is needed to confirm our results. Second, the ability of multidetector CT to detect coronary atherosclerotic plaques is not definitively confirmed. In a study by Achenbach et al (20), the sensitivity and specificity of 16-slice CT for the detection of any plaque were 82% and 88%, respectively, compared with intravascular ultrasound. The sensitivity and specificity for the detection of calcified plaque were high (94% and 94%, respectively) but those for the detection of noncalcified plaque were modest (78% and 87%, respectively). Coronary plaques not detected by 16-slice CT had a smaller plaque thickness and were located in smaller coronary arteries. Although there is no study to investigate the ability of 64-slice CT to detect coronary atherosclerotic plaques compared with intravascular ultrasound, with the enhanced spatial resolution (approximately 0.4 mm) of 64-slice CT technology, a further improvement in noncalcified plaque detection could be expected. Third, the major limitations of 64-slice CT are radiation dose and renal toxicity of contrast media. Therefore, the potential benefit of plaque detection by 64-slice CT needs to be weighted against these potential hazards.
CONCLUSION
Our results show that significant percentages of noncalcified plaque were found in asymptomatic low-risk patients with no or mild coronary calcium.
Footnotes
DISCLOSURES: The authors had full access to the data and take responsibility for its integrity. All authors have read and agree to the manuscript as written. None of the authors have any potential conflicts of interest.
REFERENCES
- 1.Third Report of National Cholesterol Educational Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 2.Brindle P, Beswick A, Fahey T, Ebrahim S. Accuracy and impact of risk assessment in the primary prevention of cardiovascular disease: A systematic review. Heart. 2006;92:1752–9. doi: 10.1136/hrt.2006.087932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greenland P, Abrama J, Aurigemma GP, et al. Prevention Conference V: Beyond secondary prevention: Identifying the high-risk patient for primary prevention: Noninvasive tests of atherosclerotic burden: Writing Group III. Circulation. 2000;101:E16–22. doi: 10.1161/01.cir.101.1.e16. [DOI] [PubMed] [Google Scholar]
- 4.Kullo IJ, Ballantyne CM. Conditional risk factors for atherosclerosis. Mayo Clin Proc. 2005;80:219–30. doi: 10.4065/80.2.219. [DOI] [PubMed] [Google Scholar]
- 5.Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation. 1995;92:2157–62. doi: 10.1161/01.cir.92.8.2157. [DOI] [PubMed] [Google Scholar]
- 6.Sangiorgi G, Rumberger JA, Severson A, et al. Arterial calcification and not lumen stenosis is highly correlated with atherosclerotic plaque burden in humans: A histologic study of 723 coronary artery segments using nondecdalcifying methodology. J Am Coll Cardiol. 1998;31:126–33. doi: 10.1016/s0735-1097(97)00443-9. [DOI] [PubMed] [Google Scholar]
- 7.Raggi P, Callister TQ, Cooil B, et al. Identification of patients at increased risk of first unheralded acute myocardial infarction by electron-beam computed tomography. Circulation. 2000;101:1850–5. doi: 10.1161/01.cir.101.8.850. [DOI] [PubMed] [Google Scholar]
- 8.Arad Y, Spadaro LA, Goodman K, Newstein D, Guerci AD. Prediction of coronary events with electron beam computed tomography. J Am Coll Cardiol. 2000;36:1253–60. doi: 10.1016/s0735-1097(00)00872-x. [DOI] [PubMed] [Google Scholar]
- 9.Kondos GT, Hoff JA, Sevrukov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: A 37-months follow-up of 5635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107:2571–6. doi: 10.1161/01.CIR.0000068341.61180.55. [DOI] [PubMed] [Google Scholar]
- 10.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–5. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 11.Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: The St. Francis Heart Study. J Am Coll Cardiol. 2005;46:158–65. doi: 10.1016/j.jacc.2005.02.088. [DOI] [PubMed] [Google Scholar]
- 12.Mollet NR, Cademartiri F, van Mieghem C, et al. High-resolution spiral computed tomography coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation. 2005;112:2318–23. doi: 10.1161/CIRCULATIONAHA.105.533471. [DOI] [PubMed] [Google Scholar]
- 13.Ropers D, Rixe J, Anders K, et al. Usefulness of multidetector row spiral computed tomography with 64-×0.6-mm collimation and 330-ms rotation for the noninvasive detection of significant coronary artery stenosis. Am J Cardiol. 2006;97:343–8. doi: 10.1016/j.amjcard.2005.08.050. [DOI] [PubMed] [Google Scholar]
- 14.Leber AW, Knez A, von Ziegler F, et al. Quantitation of obstructive and nonobstructive coronary lesions by 64-slice computed tomography. J Am Coll Cardiol. 2005;46:147–54. doi: 10.1016/j.jacc.2005.03.071. [DOI] [PubMed] [Google Scholar]
- 15.Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552–7. doi: 10.1016/j.jacc.2005.05.056. [DOI] [PubMed] [Google Scholar]
- 16.Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: First experience. Eur Heart J. 2005;26:1482–7. doi: 10.1093/eurheartj/ehi261. [DOI] [PubMed] [Google Scholar]
- 17.Leber AW, Becker A, Knez A, et al. Accuracy of 64-slice computed tomography to classify and quantify plaque volumes in the proximal coronary system. J Am Coll Cardiol. 2006;47:672–7. doi: 10.1016/j.jacc.2005.10.058. [DOI] [PubMed] [Google Scholar]
- 18.Carrascosa PM, Capuñay CM, Garcia-Merletti P, Carrascosa J, Garcia MJ. Characterization of coronary atherosclerotic plaques by multidetector computed tomography. Am J Cardiol. 2006;97:598–602. doi: 10.1016/j.amjcard.2005.09.096. [DOI] [PubMed] [Google Scholar]
- 19.Ferencik M, Nieman K, Achenbach S. Noncalcified and calcified coronary plaque detection by contrast-enhanced multi-detector computed tomography: A study of interobserver agreement. J Am Coll Cardiol. 2006;47:207–9. doi: 10.1016/j.jacc.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Achenbach S, Moselewski F, Ropers D, et al. Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography. A segment-based comparison with intravascular ultrasound. Circulation. 2004;109:14–7. doi: 10.1161/01.CIR.0000111517.69230.0F. [DOI] [PubMed] [Google Scholar]
- 21.Leber AW, Knez A, Becker A, et al. Accuracy of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques. A comparative study with intravascular ultrasound. J Am Coll Cardiol. 2004;43:1241–7. doi: 10.1016/j.jacc.2003.10.059. [DOI] [PubMed] [Google Scholar]
- 22.Leber AW, Knez A, von Zieger F, et al. Quantitation of obstructive and nonobstructive coronary lesions by 64-slice computed tomography. A comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol. 2005;46:147–54. doi: 10.1016/j.jacc.2005.03.071. [DOI] [PubMed] [Google Scholar]
- 23.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 24.Austen WG, Edwards JE, Frye RL, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975;51:5–40. doi: 10.1161/01.cir.51.4.5. [DOI] [PubMed] [Google Scholar]
- 25.Baumgart D, Schmermund A, Görge G, et al. Comparison of electron-beam computed tomography with intracoronary ultrasound and coronary angiography for detection of coronary atherosclerosis. J Am Coll Cardiol. 1997;30:57–64. doi: 10.1016/s0735-1097(97)00147-2. [DOI] [PubMed] [Google Scholar]
- 26.Schmermund A, Baumgart D, Görge G, et al. Coronary artery calcium in acute coronary syndrome: A comparative study of electron-beam computed tomography, coronary angiography, and intracoronary ultrasound in survivors of acute myocardial infarction and unstable angina. Circulation. 1997;96:1461–9. doi: 10.1161/01.cir.96.5.1461. [DOI] [PubMed] [Google Scholar]
- 27.Tuzcu EM, Kapadia SR, Tutar E, et al. High prevalence of coronary atherosclerosis in asymptomatic teenagers and young adults: Evidence from intravascular ultrasound. Circulation. 2001;103:2705–10. doi: 10.1161/01.cir.103.22.2705. [DOI] [PubMed] [Google Scholar]
- 28.Cheng VY, Lepor NE, Madyoon H, Fshaghian S, Naraghi AL, Shah PK. Presence and severity of noncalcified coronary plaque on 64-slice computed tomographic coronary angiography in patients with zero and low coronary artery calcium. Am J Cardiol. 2007;99:1183–6. doi: 10.1016/j.amjcard.2006.12.026. [DOI] [PubMed] [Google Scholar]
- 29.Hausleiter J, Meyer T, Hadamitzky M, Kastrati A, Martinoff S, Schömig A. Prevalence of noncalcified coronary plaques by 64-slice computed tomography in patients with an intermediate risk for significant coroanary artery disease. J Am Coll Cardiol. 2006;48:312–8. doi: 10.1016/j.jacc.2006.02.064. [DOI] [PubMed] [Google Scholar]
- 30.Schroeder S, Kuettner A, Kopp AF, et al. Noninvasive evaluation of the prevalence of noncalcified atherosclerotic plaques by multi-slice detector computed tomography: Results of a pilot study. Int J Cardiol. 2003;92:151–5. doi: 10.1016/s0167-5273(03)00104-9. [DOI] [PubMed] [Google Scholar]
- 31.Rubinshtein R, Gasper T, Halon DA, Goldstein J, Peled N, Lewis BS. Prevalence and extent of obstructive coronary artery disease in patients with zero or low calcium score undergoing 64-slice cardiac multidetector computed tomography for evaluation of a chest pain syndrome. Am J Cardiol. 2007;99:472–5. doi: 10.1016/j.amjcard.2006.08.060. [DOI] [PubMed] [Google Scholar]
- 32.Schenker MP, Dorbala S, Hong ECT, et al. Interrelation of coronary calcification, myocardial ischemia, and outcomes in patients with intermediate likelihood of coronary artery disease. A combined positron emission tomography/computed tomography study. Circulation. 2008;117:1693–700. doi: 10.1161/CIRCULATIONAHA.107.717512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–45. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]