Abstract
Purpose
Many children with chronic kidney disease have urinary incontinence due to urological disorders and/or a urine concentrating defect. We determined the prevalence and impact of incontinence on health related quality of life in children with chronic kidney disease.
Materials and Methods
The Chronic Kidney Disease in Children study is a prospective, observational cohort of children recruited from 47 sites in the United States and Canada. Eligibility requirements are age 1 to 16 years and an estimated glomerular filtration rate of 30 to 90 ml per minute per 1.73 m2. Demographics, continence status, glomerular filtration rate and physical examination were assessed at study entry. Health related quality of life was measured using the parent and child versions of PedsQL™. PedsQL scores in participants 5 years old or older were compared among children who were toilet trained and not bed-wetting, bed-wetting or not toilet trained using multivariate linear regression.
Results
Overall median age of the 329 participants was 12.5 years, 61.4% were male, 70% were white and 55.5% had a urological disorder. Of participants 71.4% were toilet trained at study enrollment, 23.1% had bed-wetting and 5.5% were not toilet trained. Children who were not yet toilet trained had an average total score that was 13.5 points lower (95% CI −25.2, −1.8) on the PedsQL child report than in those who were toilet trained (p = 0.02). Physical functioning (−15.0, 95% CI −28.2, −1.9) and school functioning (−15.3, 95% CI −29.8, −0.8) were also lower in this group (p = 0.03 and 0.04, respectively). On the PedsQL parent proxy report physical functioning (−14.2, 95% CI −26.7, −1.6) was similarly affected by child incontinence (p = 0.03).
Conclusions
Urinary incontinence is common in pediatric patients with chronic kidney disease and associated with lower health related quality of life on the PedsQL child and parent proxy reports. Early recognition of and treatment for urinary incontinence may improve health related quality of life in this population.
Keywords: kidney, kidney diseases, questionnaires, urinary incontinence, quality of life
Childhood structural urological disease is the leading cause of CKD, accounting for up to 60% of underlying diagnoses in the 0 to 12-year age group.1–3 Obstructive uropathy has long been recognized as an important cause of renal failure.4 Reflux nephropathy associated with vesicoureteral reflux is also a common urological etiology of CKD. Analysis of the ItalKid Project showed that 25.4% of 1,348 pediatric patients in a CKD registry had an underlying diagnosis of vesicoureteral reflux.5 Incontinence and delayed toilet training are common in children with structural urological disease and may disproportionately affect HRQOL.
Urinary continence is a developmental milestone that is usually achieved by most children by age 5 years.6 Incontinence that lasts longer than this is thought to be socially stigmatizing with negative implications for self-esteem and independence.7,8 QOL in neurologically healthy children with urinary incontinence is also impaired.9 Children with underlying congenital urological disease leading to significant kidney disease may have incontinence due to bladder outlet obstruction and subsequent abnormal bladder function. Children with CKD may also have persistent urinary incontinence for other reasons. As concentrating ability decreases and urine volume increases, new onset incontinence may develop. Thus, as kidney function decreases, all children with CKD are at risk for diurnal or nocturnal incontinence due to increased urine volume. There is little research into incontinence in children with kidney disease, although it was assessed in adult transplant recipients.10
Children and adolescents with CKD have a significant disease burden and are known to have impaired HRQOL.11 Treatment with dialysis, anemia and poor linear growth are implicated as potential causes of impaired HRQOL in children with kidney disease.11–13 Although it is likely that urinary incontinence may adversely affect HRQOL in these children, its impact on children with CKD is not well measured. We determined the prevalence and impact of urinary incontinence on HRQOL in children with CKD enrolled in the CKiD cohort study (http://www.statepi.jhsph.edu/ckid). We hypothesized that children with persistent incontinence after age 5 years would have worse generic HRQOL on PedsQL than those with normal continence.
MATERIALS AND METHODS
Chronic Kidney Disease in Children Study
CKiD is a prospective, observational cohort of children with mild to moderate CKD.14 There are 2 clinical coordinating centers and 47 recruitment sites in the United States and Canada (Appendix 1). Institutional review board approval for the study was obtained at each site. The study began in 2003 with enrollment commencing in 2005. The study was recently renewed by the National Institutes of Health to continue longitudinal followup through 2013. CKiD inclusion criteria are age 1 to 16 years and mildly to moderately impaired kidney function, as defined by estimated GFR between 30 and 90 ml per minute per 1.73 m2 by the Schwartz formula. This GFR level is consistent with mild to moderate CKD and not yet severe enough to require dialysis or be considered end stage renal disease. The subpopulation of the CKiD cohort that we studied included children 5 to 16 years old to conform to International Children’s Continence Society standard terminology with incontinence status data and PedsQL data available for analysis.15 Since CKiD was designed as a longitudinal cohort of children with CKD, no healthy controls were included. In this study comparisons and inferences were planned among CKiD cohort groups and, thus, a healthy control group was not recruited.
Continence Status
Continence status was ascertained from a parent completed questionnaire at study entry that included questions on child age at toilet training and cessation of bed-wetting. Parents were asked whether their child was currently toilet trained and, if so, at what age this occurred. Parents were also asked whether bed-wetting occurred after toilet training and, if so, parents were asked until what age the child had bed-wetting. Participants were categorized into 3 continence groups, including previously toilet trained but currently bed-wetting, not yet toilet trained, and previously toilet trained and not currently bed-wetting.
PedsQL Description
HRQOL was measured using the PedsQL child and parent proxy reports at a study visit 3 to 6 months after study entry.16 PedsQL is a set of questionnaires that is used to measure generic HRQOL in children 2 to 18 years old. It is brief with only 23 items and usually requires less than 4 minutes to complete. The score range is 0 to 100 with higher scores indicating better QOL. A clinically meaningful difference in the total score was determined by the instrument developers to be approximately 4.5 points.16 It is considered developmentally appropriate with age specific versions. There is a child self-report for ages 5 to 7, 8 to 12 and 13 to 18 years. A parent proxy report is available for ages 2 to 4, 5 to 7, 8 to 12 and 13 to 18 years. The instrument is multidimensional, assessing physical, emotional, social and school functioning.16 The instrument provides a total score and 4 subscale scores for different health domains, including physical, emotional, social and school functioning (Appendix 2). The normal population mean ± SD of the PedsQL child report total score is 83 ± 13.16 PedsQL is well validated and reliable with an internal consistency reliability á coefficient of 0.89 and 0.92 for the child and parent proxy reports, respectively. Previous studies by the developers showed construct validity. PedsQL can differentiate healthy children and children with chronic health conditions.17 It also distinguishes the severity of a chronic health condition. Data suggest that PedsQL shows responsiveness with time.18,19
Covariates
Demographic covariates were age in years, gender (male or female) and race (white or other). We used 2 measures of socioeconomic status, including maternal education duration (12 years or less, 13 to 15, or 16 or greater) and household income (less than $36,000, $36,000 to $75,000 or greater than $75,000). Clinical variables were the underlying diagnosis, categorized as urological or nonurological. Kidney function was measured by iGFR using methodology previously described by Schwartz et al.20 Other clinical variables were hemoglobin in gm/dl, the height percentile for age and years since dryness was attained by those who were currently dry. IQ was measured using the age appropriate Wechsler Scale of Intelligence and included in analysis since it was associated with incontinence in previous studies.21
Statistical Analysis
Baseline characteristics, and the PedsQL child report (for participants 8 years old or older) and the parent proxy report (for participants 5 years old or older) were determined for each continence category. We created multivariate linear regression models for PedsQL child and parent report total and subscale scores in the whole group, adjusting for potential confounders. The demographic variables adjusted for were age in years, gender (male or female), race (white or other), maternal education (12 years or less, 13 to 15, or 16 or greater) and household income (less than $36,000, $36,000 to $75,000 or greater than $75,000). Clinical variables in the regression model were underlying diagnosis (urological or nonurological), kidney function by iGFR, hemoglobin in gm/dl, height percentile for age and years since dryness was attained by those who were currently toilet trained. As measured by age appropriate Wechsler Scale of Intelligence tests, IQ was included in the models as a continuous variable.
The exposure variable was defined as urinary continence status and divided into 3 groups based on baseline questionnaire data obtained from a parent, as described. Participants were categorized into 3 continence groups, including previously toilet trained and not currently bed-wetting (referent on regression analysis), previously toilet trained but currently bed-wetting and not yet toilet trained. The outcome variable was defined as the transformed total and individual domain scores obtained in the PedsQL child report (available for children 8 years or older only) and in the PedsQL parent proxy report (available for children 5 years or older).
Sensitivity analysis was also done by restricting PedsQL parent proxy report analysis to participants 8 years or older to correspond to the age range of participants with PedsQL child report data available. Statistical analysis was performed using SAS®, version 9.1.
RESULTS
Cohort Baseline Characteristics
A total of 329 CKiD participants met eligibility requirements for this analysis. Of the 540 patients with baseline data in CKiD 449 had visit 1b data, of whom 438 had PedsQL data available. Of the 438 patients with PedsQL data available 373 had continence data available, of whom 329 were 5 years or older. Median age in this subcohort was 12.5 years (IQR 8.9, 15.2), 61.4% were male, 70% were white and 55.5% had an underlying urological diagnosis. Overall 235 of 329 participants (71.4%) were toilet trained, 76 (23%) had bed-wetting and 18 (5.5%) were not yet toilet trained. Those in the not toilet trained category were younger (median age 8.6 years), a smaller proportion were white (61.1%), had slightly lower socioeconomic status and lower median IQ, and a higher proportion had an underlying urological diagnosis (table 1).
Table 1.
Study group characteristics
| Characteristic | Toilet Trained | Bed-Wetting | Not Toilet Trained | Overall | ||||
|---|---|---|---|---|---|---|---|---|
| No. pts | 235 | 76 | 18 | 329 | ||||
| Median yrs age at enrollment (IQR) (years) | 13.4 | (9.8, 15.5) | 10.1 | (8.0, 13.0) | 8.6 | (6.3, 13.5) | 12.5 | (8.9, 15.2) |
| Median yrs to toilet training (IQR) | 2 | (2, 3) | 3 | (2, 3) | 8.6 | (6.3, 13.5) | 2 | (2, 3) |
| Median yrs bed-wetting after toilet training (IQR) | 0.6 | (0, 5) | 7.7 | (5.3, 10.7) | 0 | 2 | (0, 6) | |
| Median yrs from stopping bed-wetting to enrollment (IQR) | 7.9 | (3.3, 11.6) | 0 | 0 | 4.1 | (0, 9.7) | ||
| No. male (%) | 136 | (57.9) | 57 | (75.0) | 9 | (50) | 202 | (61.4) |
| No. white (%) | 164 | (70.1) | 54 | (71.1) | 11 | (61.1) | 229 | (69.8) |
| No. $1,000 household income (%): | ||||||||
| Less than 36 | 86 | (37.9) | 28 | (36.8) | 8 | (44.4) | 122 | (38.0) |
| 36–75 | 73 | (32.2) | 24 | (31.6) | 8 | (44.4) | 105 | (32.7) |
| Greater than 75 | 68 | (30.0) | 24 | (31.6) | 2 | (11.1) | 94 | (29.3) |
| No. maternal education (%): | ||||||||
| 12 Yrs or less | 100 | (43.5) | 26 | (34.7) | 9 | (50) | 135 | (41.8) |
| 13–15 Yrs | 66 | (28.7) | 19 | (25.3) | 6 | (33.3) | 91 | (28.2) |
| 16 Yrs or greater | 64 | (27.8) | 30 | (40) | 3 | (16.7) | 97 | (30) |
| No. urological diagnosis (%): | 128 | (55.2) | 42 | (55.3) | 11 | (61.1) | 181 | (55.5) |
| Obstructive uropathy | 40 | (31.3) | 18 | (42.9) | 5 | (45.5) | 63 | (34.8) |
| Reflux nephropathy | 42 | (32.8) | 7 | (16.7) | 2 | (18.2) | 51 | (28.2) |
| Aplastic/hypoplastic/dysplastic kidneys | 35 | (27.3) | 11 | (26.2) | 3 | (27.3) | 49 | (27.1) |
| Other | 4 | (3.1) | 2 | (4.8) | 0 | 6 | (3.3) | |
| Abdominal musculature agenesis syndrome | 4 | (3.1) | 1 | (2.4) | 0 | 5 | (2.8) | |
| Hydronephrosis | 2 | (1.6) | 2 | (4.8) | 0 | 4 | (2.2) | |
| Vacterl syndrome | 1 | (0.8) | 1 | (2.4) | 1 | (9.1) | 3 | (1.7) |
| Median ml/min/1.73 m2 iGFR (IQR) | 44 | (33, 55) | 39 | (30, 48) | 42 | (35, 52) | 42 | (33, 54) |
| No. CKD stage (%): | ||||||||
| I | 0 | 0 | 0 | 0 | ||||
| II | 33 | (14.4) | 14 | (19.7) | 2 | (11.8) | 49 | (15.5) |
| III | 147 | (64.2) | 51 | (71.8) | 11 | (64.7) | 209 | (65.9) |
| IV | 49 | (21.4) | 5 | (7.0) | 4 | (23.5) | 58 | (18.3) |
| V | 0 | 1 | (1.4) | 0 | 1 | (0.3) | ||
| Median ml/dl hematocrit (IQR) | 37 | (34, 40) | 35 | (33, 38) | 37 | (34, 40) | 37 | (33, 40) |
| Median gm/dl hemoglobin (IQR) | 12.4 | (11.6, 13.5) | 12.3 | (11.3, 13.2) | 12.0 | (11.6, 13.7) | 12.4 | (11.5, 13.5) |
| No. anemia (%) | 99 | (42.9) | 38 | (50.7) | 6 | (35.3) | 143 | (44.3) |
| Median IQ (IQR) | 98 | (86, 109) | 98 | (86, 107) | 91 | (85, 98) | 97 | (86, 109) |
| Median ht percentile (IQR) | 22 | (8, 49) | 23 | (6, 49) | 29 | (4, 51) | 22 | (7, 50) |
| No. Tanner stage (%): | ||||||||
| I | 101 | (44.3) | 54 | (71.0) | 11 | (64.7) | 166 | (51.7) |
| II | 29 | (12.7) | 11 | (14.5) | 1 | (5.9) | 41 | (12.8) |
| III | 25 | (11.0) | 4 | (5.3) | 2 | (11.8) | 31 | (9.7) |
| IV | 48 | (21.0) | 6 | (7.9) | 1 | (5.9) | 55 | (17.1) |
| V | 25 | (11.0) | 1 | (1.3) | 2 | (11.8) | 28 | (8.7) |
Table 1 shows the specific underlying urological diagnoses in participants in each continence category. Overall 181 of 329 participants (55.5%) had a urological diagnosis. In this group the most common diagnosis was obstructive uropathy (34.8% of cases), followed by reflux nephropathy (28.2%) and aplastic/hypoplastic/dysplastic kidneys (27.1%). Nonurological diagnoses were present in 145 of 329 participants (44.5%) with focal segmental glomerulosclerosis the most common cause of CKD (17%). Of those not yet toilet trained 61.1% had underlying urological diagnoses with obstructive uropathy in about half.
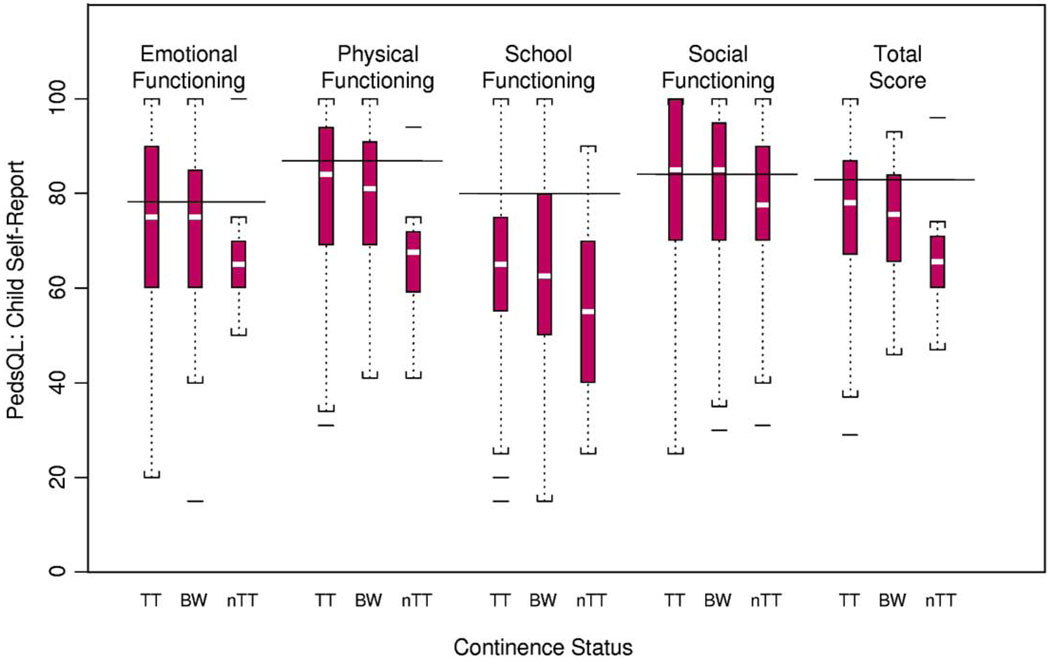
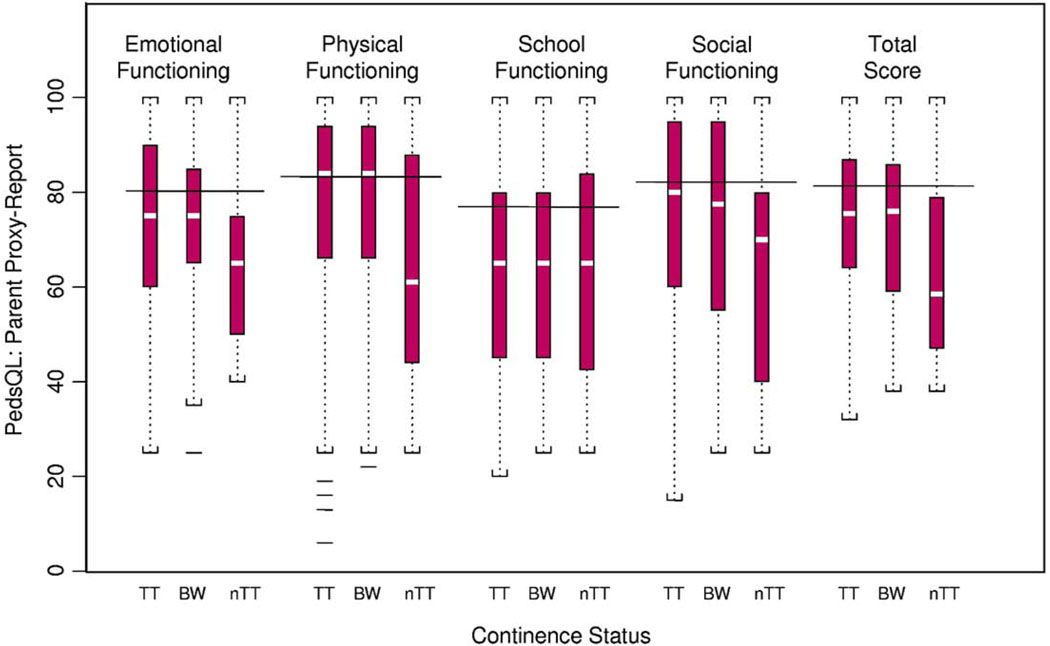
Unadjusted PedsQL Scores
Figures 1 and 2 show unadjusted PedsQL child and parent proxy report scores. Total scores of children not yet toilet trained on the child report were 9.2 points lower than the scores of those who were toilet trained. Throughout the subscales and total score of the PedsQL child report worsening incontinence severity (from toilet trained to bed-wetting only to not toilet trained) was associated with worsening HRQOL, especially in the physical health and school functioning subscales. Children who were not toilet trained also consistently reported impaired HRQOL compared to published available pediatric PedsQL norms (fig. 1). Throughout most subscales and total scores of the PedsQL parent proxy report worsening incontinence was associated with worsening HRQOL, especially in the emotional functioning, and physical health and social functioning subscales. Parents of children who were not toilet trained also consistently reported impaired HRQOL compared to the published available pediatric PedsQL norms (fig. 2).
Figure 1.
Child reported PedsQL by continence group. BW, toilet trained and bed wetting. nTT, not toilet trained. TT, toilet trained and not bed wetting. Solid lines indicate population based norms.16
Figure 2.
Parent proxy reported PedsQL by continence group. BW, toilet trained and bed wetting. nTT, not toilet trained. TT, toilet trained and not bed wetting. Solid lines indicate population based norms.16
PedsQL Score Multivariate
Linear Regression Models
Child self-report
The association of incontinence with lower HRQOL persisted after adjusting for potential confounders, including IQ. Table 2 lists the results of multivariate linear regression models for the PedsQL child report. Estimates and the 95% CI for each incontinence category and for important potential confounders are shown. When adjusted for potential confounders, children who were not toilet trained scored an average of 13.5 points (95% CI −25.2, −1.8) lower on the child self-report total score than children who were toilet trained (p = 0.02, table 2).
Table 2.
PedsQL child self-report multivariate linear regression models in 209 participants 8 years old or older
| Emotional |
Physical |
School |
Social |
Total Score |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Covariates* | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | |||||
| Continence status: | |||||||||||||||
| Not toilet trained | −14.2 | (−29.2, 0.8) | 0.06 | −15.0 | (−28.2, −1.9) | 0.03 | −15.3 | (−29.8, −0.8) | 0.04 | −10.3 | (−26.3, 5.7) | 0.20 | −13.5 | (−25.2, −1.8) | 0.02 |
| Bed-wetting | −6.5 | (−14.9, 1.9) | 0.13 | 0.44 | (−7.0,7.8) | 0.91 | −4.6 | (−12.7,3.5) | 0.26 | 1.3 | (−7.7, 10.3) | 0.78 | −1.9 | (−8.5, 4.7) | 0.56 |
| Toilet trained | Referent | Referent | Referent | Referent | Referent | ||||||||||
| Age | 1.3 | (0.2, 2.5) | 0.02 | 1.3 | (0.3, 2.3) | 0.01 | 1.1 | (0.03, 2.2) | 0.04 | 1.4 | (0.2, 2.6) | 0.03 | 1.3 | (0.4, 2.2) | 0.005 |
| Nonwhite vs white | −1.7 | (−7.7, 4.2) | 0.57 | −2.2 | (−7.4, 3.0) | 0.41 | −0.8 | (−6.5, 5.0) | 0.79 | 0.9 | (−5.4, 7.3) | 0.77 | −1.1 | (−5.7, 3.6) | 0.65 |
| Male vs female | 4.6 | (−0.7, 9.9) | 0.09 | 1.0 | (−3.6, 5.7) | 0.66 | −1.8 | (−6.9, 3.3) | 0.48 | −1.4 | (−7.1, 4.3) | 0.62 | 0.6 | (−3.5, 4.7) | 0.77 |
| Income ($1,000): | |||||||||||||||
| Less than 36 | 0.8 | (−5.7, 7.4) | 0.80 | −0.1 | (−5.8, 5.6) | 0.98 | 1.7 | (−4.5, 8.0) | 0.59 | −2.8 | (−9.7, 4.1) | 0.43 | −0.04 | (−5.1, 5.0) | 0.99 |
| 36–75 | 3.4 | (−2.9, 9.7) | 0.28 | 2.6 | (−2.9, 8.2) | 0.35 | 6.3 | (0.2, 12.3) | 0.04 | 0.06 | (−6.6, 6.8) | 0.99 | 3.0 | (−1.9, 7.9) | 0.22 |
| Greater than 75 | Referent | Referent | Referent | Referent | Referent | ||||||||||
| Maternal education (yrs): | |||||||||||||||
| 12 or Less | −3.4 | (−10.0, 3.1) | 0.30 | −0.7 | (−6.4, 5.0) | 0.81 | −1.6 | (−7.9, 4.7) | 0.63 | −2.9 | (−9.8, 4.1) | 0.41 | −2.0 | (−7.1, 3.1) | 0.44 |
| 13–15 | −6.1 | (−12.9, 0.8) | 0.08 | −1.3 | (−7.3, 4.7) | 0.68 | −5.0 | (−11.7, 1.5) | 0.13 | −7.5 | (−14.8, −0.2) | 0.04 | −4.5 | (−9.8, 0.9) | 0.10 |
| 16 or Greater | Referent | Referent | Referent | Referent | Referent | ||||||||||
| CKD diagnosis: | |||||||||||||||
| Urological | −0.3 | (−5.5, 5.0) | 0.92 | 4.5 | (−0.09, 9.2) | 0.05 | 3.9 | (−1.2, 8.9) | 0.13 | 0.8 | (−4.8, 6.4) | 0.78 | 2.5 | (−1.6, 6.6) | 0.23 |
| Nonurological | Referent | Referent | Referent | Referent | Referent | ||||||||||
| IQ | 0.008 | (−0.2, 0.2) | 0.93 | 0.1 | (0.009, 0.30) | 0.04 | 0.4 | (0.2, 0.5) | <0.0001 | 0.1 | (−0.04, 0.3) | 0.12 | 0.2 | (0.04, 0.3) | 0.01 |
Additional covariates adjusted for were GFR, hemoglobin, percentile height for age, and years since dryness was attained.
Parent proxy report
From the parent perspective these results were consistent, although the magnitude of the effect was smaller and only statistically significant for the physical functioning subscale (−14.2, 95% CI −26.7, −1.6; p = 0.03). Table 3 lists the results of multivariate linear regression models for the PedsQL parent proxy report. Estimates and the 95% CI of each incontinence category and of important potential confounders are shown. After adjusting for potential confounders parents of children who were not toilet trained scored an average of 9.3 points (95% CI −18.9, 0.03) lower on the total score of the parent proxy report than those whose children were toilet trained (p = 0.06, table 3). Sensitivity analysis was done, restricting analysis to parents of participants 8 years old or older to correspond to the age range of participants with PedsQL child report data available. Results were consistent but not statistically significant.
Table 3.
PedsQL parent proxy report multivariate linear regression models in 254 participants 5 years old or older
| Emotional |
Physical |
School |
Social |
Total Score |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Covariates* | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | |||||
| Continence status: | |||||||||||||||
| Not toilet trained | −8.5 | (−19.1, 2.1) | 0.12 | −14.2 | (−26.7, −1.6) | 0.03 | 1.6 | (−11.0, 14.3) | 0.80 | −9.3 | (−22.1, 3.5) | 0.15 | −9.3 | (−18.9, 0.3) | 0.06 |
| Bed-wetting | −1.1 | (−8.0, 5.7) | 0.74 | −0.02 | (−8.1, 8.1) | 0.99 | 1.5 | (−6.3, 9.2) | 0.71 | −1.1 | (−9.4, 7.3) | 0.80 | 0.2 | (−6.0, 6.4) | 0.95 |
| Toilet trained | Referent | Referent | Referent | Referent | Referent | ||||||||||
| Age | 0.15 | (−0.7, 1.0) | 0.72 | −0.6 | (−1.5, 0.4) | 0.27 | −0.8 | (−1.8, 0.1) | 0.09 | −0.5 | (−1.5, 0.6) | 0.38 | −0.4 | (−1.1, 0.4) | 0.32 |
| Nonwhite vs white | −2.7 | (−7.9, 2.5) | 0.31 | −5.2 | (−11.4, 1.0) | 0.10 | −3.4 | (−9.3, 2.4) | 0.25 | −6.9 | (−13.2, −0.5) | 0.03 | −4.6 | (−9.3, 0.1) | 0.06 |
| Male vs female | −1.9 | (−6.7, 2.9) | 0.43 | −3.0 | (−8.7, 2.6) | 0.29 | − 8.0 | (−13.4, −2.7) | 0.003 | −6.0 | (−11.7, −0.2) | 0.04 | −4.5 | (−8.8, −0.2) | 0.04 |
| Income ($1,000): | |||||||||||||||
| Less than 36 | −8.6 | (−14.5, −2.7) | 0.005 | −7.3 | (−14.3, −0.3) | 0.04 | −2.5 | (−9.1, 4.1) | 0.46 | −5.2 | (−12.3, 2.0) | 0.15 | −6.2 | (−11.5, −0.9) | 0.02 |
| 36–75 | 0.2 | (−5.5, 6.0) | 0.93 | 1.9 | (−4.9, 8.7) | 0.58 | 2.5 | (−4.0, 9.0) | 0.45 | 2.6 | (−4.4, 9.6) | 0.47 | 2.2 | (−3.0, 7.5) | 0.41 |
| Greater than 75 | Referent | Referent | Referent | Referent | Referent | ||||||||||
| Maternal education (yrs): | |||||||||||||||
| 12 or Less | 3.6 | (−2.4, 9.6) | 0.24 | 0.1 | (−7.0, 7.2) | 0.97 | 2.9 | (−3.9, 9.6) | 0.40 | −0.1 | (−7.4, 7.2) | 0.98 | 1.6 | (−3.9, 7.0) | 0.57 |
| 13–15 | 0.5 | (−5.6, 6.5) | 0.88 | 2.2 | (−5.0, 9.3) | 0.55 | 3.6 | (−3.2, 10.4) | 0.30 | 1.8 | (−5.5, 9.1) | 0.63 | 1.9 | (−3.5, 7.4) | 0.48 |
| 16 or Greater | Referent | Referent | Referent | Referent | Referent | ||||||||||
| CKD diagnosis: | |||||||||||||||
| Urological | 2.4 | (−2.3, 7.0) | 0.32 | −0.81 | (−6.3, 4.7) | 0.77 | 2.7 | (−2.5, 7.9) | 0.31 | 3.6 | (−2.1, 9.2) | 0.21 | 1.6 | (−2.7, 5.8) | 0.47 |
| Nonurological | Referent | Referent | Referent | Referent | Referent | ||||||||||
| IQ | 0.2 | (0.02, 0.3) | 0.02 | 0.2 | (0.02, 0.4) | 0.03 | 0.4 | (0.3, 0.6) | <0.0001 | 0.3 | (0.1, 0.5) | 0.003 | 0.3 | (0.1, 0.4) | 0.0003 |
Additional covariates adjusted for were GFR, hemoglobin, percentile height for age, and years since dryness was attained.
DISCUSSION
Urinary incontinence is common, occurring in approximately 29% of children with CKD, and associated with impaired HRQOL, as measured by PedsQL child and parent proxy reports. This suggests that recognizing and treating incontinence may be a potentially important way to help maximize HRQOL in children with CKD. Children who were not toilet trained had an average total score that was 13.5 points lower on the PedsQL child report. This difference was statistically significant and clinically meaningful. Physical and school functioning was most affected from the child perspective, while physical functioning only was most affected from the parent perspective. In children with bed-wetting scores were generally between the scores of children who were and were not toilet trained.
Previous research demonstrated that adolescents with CKD have impaired HRQOL and adverse effects are most pronounced in those with advanced CKD or end stage renal disease requiring dialysis.11,12 Physical measures such as kidney function, anemia and short stature are associated with worse HRQOL in these children. A parent proxy generic health status instrument, the Child Health Questionnaire, was used to determine the negative effect of anemia on HRQOL in adolescents with CKD, especially in the physical functioning domain.11,22 Changes in physical and psychosocial functioning in adolescents with CKD were documented by Fadrowski et al using the Child Health Questionnaire-parent form.13 Better growth in measured height was associated with an improved physical summary score, while worsening kidney function was associated with a decreased physical summary score.
Although the symptom of urinary incontinence is common in patients with CKD and often treated by urologists, assessing its impact on the life of the child or adolescent is not often quantified from the child point of view or by parent proxy. Previous studies suggest that enuresis may lead to poor self-esteem.7,8 This led to interest in developing a disease specific HRQOL tool for children with bladder dysfunction.23 Although a kidney disease specific module for children on dialysis was developed for PedsQL, to our knowledge none is currently available for urinary incontinence.24 In contrast, HRQOL measurement in adults with urinary incontinence has been extensively studied in the last decade with a significant impact on research of and treatment for adult incontinence.25
Although this analysis represents one of the largest studies of incontinence and pediatric CKD to date, our study has several limitations. One is its observational nature. Although an association was seen between incontinence and worse HRQOL, this analysis does not prove causality. However, as more longitudinal data are collected in CKiD, temporality may be explored. For example, in future studies observations may be made about changes in HRQOL when child continence status changes from incontinence to dryness and vice versa.
Another limitation of these data is the ascertainment of continence status. Continence status was determined from a limited number of questions about toilet training and bed-wetting asked of parents in a structured questionnaire. The questions are not identical to recent International Children’s Continence Society definitions of continence terminology.15 The magnitude of effect sizes in the regression models was relatively large. Although we adjusted for potential demographic and clinical confounders that were available to us in the data set, it is possible that unmeasured confounders were not accounted for in the analysis. For example, a detailed medical history, including the type and number of surgeries and hospitalizations, was not available to us. Also, bowel function and lower urinary tract symptoms may be other important factors to consider in future studies.
Future longitudinal studies may inform the timing of surgical intervention for incontinence by identifying at what age surgery should be performed to help maximize HRQOL. If the negative effects of incontinence on HRQOL become more pronounced in later childhood, this information could guide surgeons in planning the most appropriate time to intervene. PedsQL may also be a useful tool to examine the effects of incontinence on HRQOL in other pediatric populations, including pediatric urology populations.
CONCLUSIONS
Urinary incontinence is common, occurring in approximately 29% of children with CKD. It is associated with clinically and statistically significantly impaired HRQOL, as measured by the PedsQL child and parent proxy reports. This suggests that recognizing and treating incontinence may be a potentially important way to help maximize HRQOL in children with CKD. Also, PedsQL may be a useful tool to examine the effects of incontinence on HRQOL in other pediatric populations, including pediatric urology populations.
Acknowledgments
Study received institutional review board approval at each site.
Supported by the National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Neurological Disorders and Stroke, National Institute of Child Health and Human Development, and National Heart, Lung and Blood Institute Grants UO1-DK-66143, UO1-DK-66174 and UO1-DK-66116, National Institute of Diabetes and Digestive and Kidney Diseases Grant 1K23DK078671 (JLD), and a National Kidney Foundation of Maryland Professional Development Award (JLD).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or National Institutes of Health.
Abbreviations and Acronyms
- CKD
chronic kidney disease
- CKiD
Chronic Kidney Disease in Children Study
- GFR
glomerular filtration rate
- HRQOL
health related QOL
- iGFR
GFR determined by plasma iohexol disappearance
- QOL
quality of life
APPENDIX 1
CKiD Recruitment Sites in United States and Canada
East Coast Sites
The Johns Hopkins Children’s Center, Children’s Hospital of Michigan, Children’s Memorial Hospital, Children’s National Medical Center, Nationwide Children’s Hospital, Inova Fairfax Hospital for Children, Riley Hospital for Children, University of Maryland, C. S. Mott Children’s Hospital-University of Michigan, University of North Carolina, University of Texas-Houston, Maria Fareri Children’s Hospital, Children’s Hospital at Montefiore, Maimonides Medical Center, Mount Sinai Medical Center, University of Rochester Medical Center/Golisano Children’s Hospital at Strong, University of Virginia, Robert W. Johnson Medical School/University of Medicine and Dentistry of New Jersey-University of New Jersey, University of Florida, DeVos Children’s Hospital, Carolinas Medical Center, State University of New York Downstate and University of Illinois-Chicago.
Midwest Sites
Children’s Mercy Hospital, Medical College of Wisconsin, University of New Mexico Children’s Hospital, Oregon Health Science University, Cincinnati Children’s Hospital and Medical Center, Stanford University Medical Center, Children’s Hospital of Boston, British Columbia Children’s Hospital, Children’s Hospital of Alabama, St. Louis Children’s Hospital, Rainbow Babies and Children’s Hospital, University of Wisconsin, Oklahoma University Health Sciences Center, Children’s Hospital and Medical Center Seattle, Cardinal Glennon Hospital, Children’s Hospital of Winnipeg, LeBonheur Children’s Medical Center, University of California-Los Angeles, University of California-San Diego, University of Texas Southwest Medical Center, University of California-San Francisco Children’s Renal Center, Egleston Children’s Hospital-Emory University, Emanuel Children’s Hospital and Children’s Kidney Specialists, Idaho.
APPENDIX 2
PedsQL Description16
| Total Scale Score |
Summary Scores | Scales |
|---|---|---|
| Total score (23 items) |
Physical health (8 items) Psychosocial health (15 items) |
Physical functioning (8 items) Emotional functioning (5 items) Social functioning (5 items) School functioning (5 items) |
REFERENCES
- 1.NAPRTCS Annual Report, 2007. Boston: North American Pediatric Renal Trials and Collaborative Studies; 2007. [Google Scholar]
- 2.Zilleruelo G, Andia J, Gorman HM, et al. Chronic renal failure in children: analysis of main causes and deterioration rate in 81 children. Int J Pediatr Nephrol. 1980;1:30. [PubMed] [Google Scholar]
- 3.Wong C, Furth S. Epidemiology of renal disease in children. In: Kher K, Makker SP, Schnaperr HW, editors. Clinical Pediatric Nephrology. 2nd ed. London: Informa Healthcare; 2007. [Google Scholar]
- 4.Roth KS, Koo HP, Spottswood SE, et al. Obstructive uropathy: an important cause of chronic renal failure in children. Clin Pediatr (Phila) 2002;41:309. doi: 10.1177/000992280204100503. [DOI] [PubMed] [Google Scholar]
- 5.Ardissino G, Avolio L, Dacco V, et al. Long-term outcome of vesicoureteral reflux associated chronic renal failure in children. Data from the ItalKid Project. J Urol. 2004;172:305. doi: 10.1097/01.ju.0000129067.30725.16. [DOI] [PubMed] [Google Scholar]
- 6.Behrman RE, Kliegman R, Jenson HB. Nelson Textbook of Pediatrics. 18th ed. Philadelphia: WB Saunders Co; 2004. [Google Scholar]
- 7.Longstaffe S, Moffatt ME, Whalen JC. Behavioral and self-concept changes after six months of enuresis treatment: a randomized, controlled trial. Pediatrics. 2000;105:935. [PubMed] [Google Scholar]
- 8.Landgraf JM, Abidari J, Cilento BG, et al. Coping, commitment, and attitude: quantifying the everyday burden of enuresis on children and their families. Pediatrics. 2004;113:334. doi: 10.1542/peds.113.2.334. [DOI] [PubMed] [Google Scholar]
- 9.Gladh G, Eldh M, Mattson S. Quality of life in neurologically healthy children with urinary incontinence. Acta Pediatr. 2006;95:1648. doi: 10.1080/08035250600752458. [DOI] [PubMed] [Google Scholar]
- 10.Heit M, Blackwell L, Thomas S, et al. Prevalence and severity of urinary incontinence in kidney transplant recipients. Am Coll Obstet Gynecol. 2004;103:352. doi: 10.1097/01.AOG.0000109520.27286.84. [DOI] [PubMed] [Google Scholar]
- 11.Gerson A, Hwang W, Fiorenza J, et al. Anemia and health-related quality of life in adolescents with chronic kidney disease. Am J Kidney Dis. 2004;44:1017. doi: 10.1053/j.ajkd.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 12.Gerson AC, Riley A, Fivush BA, et al. Assessing health status and health care utilization in adolescents with chronic kidney disease. J Am Soc Nephrol. 2005;16:1427. doi: 10.1681/ASN.2004040258. [DOI] [PubMed] [Google Scholar]
- 13.Fadrowski J, Cole SR, Hwang W, et al. Changes in physical and psychosocial functioning among adolescents with chronic kidney disease. Pediatr Nephrol. 2006;21:394. doi: 10.1007/s00467-005-2122-3. [DOI] [PubMed] [Google Scholar]
- 14.Furth SL, Cole SR, Moxey-Mims M, et al. Design and methods of the Chronic Kidney Disease in Children (CKiD) prospective cohort study. Clin J Am Soc Nephrol. 2006;1:1006. doi: 10.2215/CJN.01941205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neveus T, von Gontard A, Hoebeke P, et al. The standardization of terminology of lower urinary tract function in children and adolescents: report from the Standardisation Committee of the International Children’s Continence Society. J Urol. 2006;176:314. doi: 10.1016/S0022-5347(06)00305-3. [DOI] [PubMed] [Google Scholar]
- 16.Varni JW, Burwinkle TM, Seid M, et al. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3:329. doi: 10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 17.Varni J, Seid M, Kurtin PS. PedsQL™ 4.0: reliability and validity of the Pediatric Quality of Life Inventory™ version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Varni J, Seid M, Smith-Knight T, et al. The PedsQL™ 4.0 Generic core scales: sensitivity, responsiveness, and impact on clinical decision-making. J Behav Med. 2002;25:175. doi: 10.1023/a:1014836921812. [DOI] [PubMed] [Google Scholar]
- 19.Varni J, Seid M, Smith-Knight T, et al. The PedsQL™ in pediatric rheumatology: reliability, validity, and responsiveness of the Pediatric Quality of Life Inventory™ generic core scales and rheumatology module. Arthritis Rheum. 2002;46:714. doi: 10.1002/art.10095. [DOI] [PubMed] [Google Scholar]
- 20.Schwartz GJ, Furth S, Cole SR, et al. Glomerular filtration rate via iohexol disappearance: pilot study for chronic kidney disease in children. Kidney Int. 2006;69:2070. doi: 10.1038/sj.ki.5000385. [DOI] [PubMed] [Google Scholar]
- 21.Joinson C, Heron J, Butler R, et al. A United Kingdom population-based study of intellectual capacities in children with and without soiling, daytime wetting, and bed-wetting. Pediatrics. 2007;120:e308. doi: 10.1542/peds.2006-2891. [DOI] [PubMed] [Google Scholar]
- 22.Landgraf J, Abetz L, Ware JE. Child Health Questionnaire (CHQ): A User’s Manual. Boston: The Health Institute, New England Medical Center; 1996. [Google Scholar]
- 23.Bower WF, Wong EM, Yeung CK. Development of a validated quality of life tool specific to children with bladder dysfunction. Neurourol Urodyn. 2006;25:221. doi: 10.1002/nau.20171. [DOI] [PubMed] [Google Scholar]
- 24.Goldstein SL, Graham N, Burwinkle T, et al. Health-related quality of life in pediatric patients with ESRD. Pediatr Nephrol. 2006;21:846. doi: 10.1007/s00467-006-0081-y. [DOI] [PubMed] [Google Scholar]
- 25.Padmanabhan P, Nitti VW. Female stress urinary incontinence: how do patient and physician perspectives correlate in assessment of outcomes? Curr Opin Urol. 2006;16:212. doi: 10.1097/01.mou.0000232038.72556.b1. [DOI] [PubMed] [Google Scholar]