Abstract
Background.
Increasingly, researchers have begun to explore pathways through which psychosocial factors might influence cardiovascular disease, with some emphasis on early markers. The current study examined the cross-sectional association between psychosocial factors and aortic pulse wave velocity (an early marker of cardiovascular disease) in a biracial cohort of older adults. We were particularly interested in determining whether the association between psychosocial factors and aortic pulse wave velocity differed for older blacks compared with whites.
Methods.
Participants were 2,488 (40% black and 52% female) older adults from the Health, Aging, and Body Composition Study. Carotid–femoral aortic pulse wave velocity was assessed using standard methodologies. Depressive symptoms, anxiety symptoms, negative life events, and inadequate emotional support were assessed, and a summary psychosocial risk index was created.
Results.
In multivariable linear regression models, psychosocial risk was not associated with aortic pulse wave velocity (Estimate [Est] = .00, p = .83), but there was a significant Race × Psychosocial risk interaction (Est = .07, p = .01), after adjusting for age, race, sex, and education. Further analyses revealed that this association was driven by the inadequate emotional support component of psychosocial risk (Race × Inadequate emotional support, p = .005). In race-stratified analyses, inadequate emotional support was associated with higher levels of arterial stiffness in older blacks (Est = .05, p = .04) but not whites (Est = −.04, p = .13). This association persisted after adjusting for demographics, cardiovascular risk factors, and social network characteristics.
Conclusions.
Findings suggest that older blacks may be particularly vulnerable to the effects of inadequate emotional support on vascular health. Interventions aimed at increasing social support among this population might be beneficial in reducing cardiovascular disease risk.
Keywords: Psychosocial, Social support, Arterial stiffness, Cardiovascular disease, African-Americans
BACKGROUND
Numerous studies have documented an association between psychosocial risk factors and cardiovascular disease (CVD) morbidity and mortality (1). Psychosocial factors consistently associated with CVD include negative affect (eg, symptoms of depression or anxiety) (2,3), social ties (ie, social networks, social support) (4,5), and psychological stressors (high perceived stress and negative life events) (6,7). These associations have been observed in populations both with and without preexisting clinical disease (2,4–6).
Increasingly, researchers have begun to explore pathways through which psychosocial factors might influence CVD (8,9), with some emphasis on early markers. Arterial stiffness—measured by aortic pulse wave velocity (aPWV)—is an early marker of CVD that increases with age (10,11) and is believed to reflect the cumulative impact of risk factors on the vascular system (12,13). It is associated with other indicators of atherosclerotic disease (14,15) and is predictive of incident CVD events and mortality (16–18). However, to date, there have been few studies (19–22) examining the association between psychosocial factors and aPWV.
The primary goal of the current study was to examine the association between psychosocial risk factors and aPWV in a sample of older black and white adults from the Health, Aging, and Body Composition Study. Psychosocial risk factors of interest were depressive symptoms, anxiety symptoms, negative life events, and inadequate emotional support. In keeping with several prior studies, we were particularly interested in psychosocial risk burden (ie, the combination of these psychosocial risk factors) as an indicator of overall psychosocial risk (23,24).
We were also interested in determining whether associations between psychosocial risk factors and aPWV were more pronounced in older black compared with white adults. Black men and women typically have a worse psychosocial risk profile compared with whites, reporting higher rates of depressive symptoms, more negative life events, and in some instances, less social support (24–26). Black populations also have higher rates of arterial stiffening (27). Thus, they may be particularly vulnerable to the adverse effects of psychosocial risk factors on aPWV. However, with few exceptions (20), studies examining psychosocial risk and aPWV in the United States have been conducted in predominantly white samples.
We hypothesized that higher reports of psychosocial risk burden would be associated with greater aPWV in our sample of older adults. We further hypothesized that these associations would be stronger in older blacks compared with older whites. We tested these hypotheses in a series of cross-sectional linear regression models.
METHODS
Participants
The Health, Aging, and Body Composition Study is a study of high-functioning black and white elderly participants. From 1997 to 1998, Health, Aging, and Body Composition staff recruited Medicare-eligible beneficiaries between the ages of 70 and 79 years from the areas surrounding Pittsburgh, Pennsylvania, and Memphis, Tennessee. Individuals were eligible for the study if they were able to communicate and reported no difficulty walking one quarter of a mile, climbing 10 steps, or performing activities of daily living. Participants also had to be free of cancer requiring current treatment and plan to remain in the area for at least 3 years. Ultimately, 3,075 participants (51.5% women and 41.7% black) enrolled. aPWV was only assessed at baseline; thus, all data for the current analyses were taken from the baseline assessment. aPWV data were missing for 587 participants—354 because of equipment problems and another 233 due to unusable wave forms (either unacceptable quality or out of range values). An additional 34 were missing data on psychosocial risk factors, resulting in a final sample of 2,454 (52.5% women and 40.2% black) for analyses.
The study protocol was approved by the Institutional Review Boards at the University of Pittsburgh and the University of Tennessee. All participants provided written informed consent.
Measures
Pulse Wave Velocity.—
aPWV was measured by taking simultaneous recordings of the arterial flow waves from the right common carotid and right femoral arteries with nondirectional transcutaneous Doppler flow probes (model 810-a, 10 MHZ; Parks Medical Electronics, Aloha, OR). Three data collection runs were performed, each obtaining a minimum of 10 pairs of simultaneously recorded flow waves. The flow waves were then averaged, and the time from the R wave of the electrocardiogram to the foot of the pressure wave was established. aPWV was calculated as the above body–measured distance between the carotid and femoral arteries divided by the time differential in the arrival of the pressure wave at these locations (16). Higher aPWV values indicate stiffer vessels. Because aPWV scores were non-normally distributed, we used the natural logarithm of each value in analyses.
The National Institute on Aging, Laboratory of Cardiovascular Science, Gerontology Research Center (Baltimore, Maryland) trained and certified all study personnel, read the wave forms, and evaluated data quality. Replicate measures of aPWV in 14 participants revealed intraclass correlations of 0.88 between sonographers and 0.84 between readers.
Psychosocial Risk Factors.—
Depressive Symptoms.—
Depressive symptoms over the past week were assessed with the 20-item Center for Epidemiological Studies-Depression scale (CES-D) (28). The CES-D has been widely used with good reliability and validity in both younger and older adult populations (29,30). Possible scores range from 0 to 60.
Anxiety Symptoms.—
Anxiety symptoms were measured with three items from the anxiety subscale of the well-validated Hopkins Symptom Checklist. Participants were asked how often they had experienced the following symptoms of anxiety in the past week: feeling nervous or shaky inside, feeling tense or keyed up, and feeling fearful. Possible scores on the anxiety subscale range from 0 to 9.
Negative Life Events.—
Participants were asked if they had experienced the following negative events over the past year: (a) death of a partner or spouse; (b) death of a child, grandchild, close friend, or relative; (c) death of a pet; (d) illness or serious accident in close friend or family member; (e) being assaulted or robbed/having a family member be assaulted or robbed; (f) having a close friend or family member be arrested or in trouble with the law; and (g) having a relationship with a close friend or family member change for the worse. Possible number of negative life events ranged from 0 to 7.
Inadequate Emotional Support.—
Inadequate emotional support was assessed with a single question: “In the past year, could you have used more support than you received?” Responses were “yes” = 1 or “no” = 0.
Psychosocial Risk Burden.—
Because we were interested in assessing the affect of concomitant psychosocial risk factors, we combined the above measures to create a psychosocial risk burden index, as previously detailed (23) for this cohort. Each psychosocial risk variable was standardized into a continuous variable ranging from 0 to 1 by dividing each individual scale score by the maximum possible scale score. For the CES-D, each participant’s total CES-D score was divided by 60; for anxiety symptoms, each participant’s total score was divided by 9; and for life events, each total score was divided by 7. Inadequate emotional support was retained as a dichotomous (0–1) measure. The four standardized measures were then summed to create a continuous psychosocial risk burden score ranging from 0 to 4.
Covariates.—
Covariates were chosen for the current analyses on the basis of their previously documented association with both psychosocial risk and CVD (1). In addition to race (black or white), sociodemographic variables included age, sex, and educational level, all assessed by self-report. The presence of baseline hypertension, diabetes, or CVD was assessed via self-report and confirmed by use of specific medications or procedures. Medications taken in the past 2 weeks were brought in, recorded, and coded according to the Iowa Drug Information System. Baseline CVD was defined as a history of myocardial infarction, angina, stroke, transient cerebral ischemia, or any vascular surgery, including endarterectomy or angioplasty. Systolic blood pressure was the average of two sitting blood pressures, measured by a mercury sphygmomanometer. Fasting blood glucose and high-density lipoprotein cholesterol values were determined by a colorimetric technique on a Vitros 950 analyzer, and low-density lipoprotein cholesterol was calculated using the Friedewald equation (31). Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Smoking status (current, former, or never) and physical activity (inactive, lifestyle active, or exercise, as previously coded (32)) were assessed by self-report.
Statistical Analysis.—
Descriptive statistics were used to characterize the sample on variables of interest. t tests and chi-squared tests were conducted to test for black–white differences in participant characteristics. Multivariable linear regression models were run to examine associations among race, psychosocial risk burden, and log-transformed aPWV. The initial model tested the main effect of psychosocial risk burden on aPWV, after adjusting for age, race, sex, education, and clinical site (Pittsburgh or Memphis). The second model added a term for the Race × Psychosocial risk burden interaction.
A series of additional analyses were then run to examine the association between each individual psychosocial variable and log aPWV. Although we were primarily interested in testing the association between overall psychosocial risk burden and aPWV, preliminary analyses revealed very low values on most psychosocial variables of interest. Thus, we sought to determine whether any observed associations were being “driven” by one or two individual psychosocial predictors. Each psychosocial risk factor was modeled following the steps outlined above: the initial minimally adjusted model examined the main effect of the psychosocial factor on aPWV, and the second model tested the Race × Psychosocial factor interaction. We then examined whether any observed associations were independent of CVD, hypertension, diabetes, systolic blood pressure, high-density lipoprotein, low-density lipoprotein, BMI, smoking status, and physical activity. All significant Race × Psychosocial factor interactions were further explored in race-stratified models. Preliminary analyses revealed no significant interactions with baseline CVD status; thus, we did not run models stratified by CVD. Similarly, there were no significant interactions between psychosocial risk factors and sex in preliminary analyses; consequently, we did not run additional sex-stratified models. All models were run using SPSS version 15 (SPSS Inc., Chicago, IL).
RESULTS
Participant Characteristics
Participant characteristics are presented for the full sample and by race in Table 1. Participants were, on average, 74 years of age, 52.5% female, with 43% reporting a college education or more. Ten percent were smokers, 26% were current exercisers, and the average BMI was 27.4. Twenty-seven percent of participants had prevalent CVD at baseline, approximately 15% had prevalent diabetes, and 54% had prevalent hypertension. Black participants were slightly younger, more likely to be female, and less likely to have a college education than white participants (all p values < .05). Black participants had higher BMIs, were more likely to be current smokers, and less likely to be exercisers compared with whites (all p values < .05). Blacks also had a significantly higher prevalence of diabetes and hypertension (all p values < .001) and higher log-transformed aPWV values (p < .01) than their white counterparts.
Table 1.
Demographic, Behavioral, and Physiological Characteristics for the Full Sample and by Race
| Variable | All | Blacks | Whites | p value |
| Age (years) | 73.7 (2.9) | 73.5 (2.9) | 73.8 (2.8) | .02 |
| Female, % | 52.5 | 56.9 | 49.3 | <.001 |
| College educated, % | 43.1 | 27.3 | 53.7 | <.001 |
| Body mass index (kg/m2) | 27.4 (4.8) | 28.6 (5.4) | 26.8 (4.2) | <.001 |
| Current smoker, % | 10.2 | 16.5 | 6 | <.001 |
| Physical activity group, % | ||||
| Inactive | 22.4 | 25.7 | 20.2 | <.001 |
| Lifestyle active | 51.3 | 57.4 | 47.2 | |
| Exerciser | 26.2 | 16.9 | 32.7 | |
| High-density lipoprotein cholesterol (mg/dL) | 54.53 (16.98) | 57.75 (17.63) | 52.37 (16.18) | <.001 |
| Low-density lipoprotein cholesterol (mg/dL) | 121.80 (34.78) | 124.32 (36.82) | 120.08 (33.22) | <.001 |
| Fasting glucose (mg/dL) | 104.74 (35.99) | 105.62 (37.28) | 104.15 (35.10) | .33 |
| Systolic blood pressure (mm Hg) | 136.39 (20.74) | 139.99 (21.73) | 133.96 (19.69) | <.001 |
| Prevalent cardiovascular disease, % | 27.1 | 28.6 | 26 | .15 |
| Prevalent diabetes, % | 14.8 | 20.7 | 10.9 | <.001 |
| Prevalent HTN, % | 54.1 | 65.8 | 46 | <.001 |
| Pulse wave velocity, log | 6.73 (.39) | 6.76 (.39) | 6.71 (.37) | <.001 |
Note: Values shown are mean (SD) or N (%). p values are from t tests or chi-square tests comparing blacks and whites.
Table 2 presents psychosocial risk burden characteristics for the full sample and by race. On average, participants had an overall psychosocial risk burden score of .59. For both blacks and whites, values on psychosocial variables of interest were relatively low, with an average CES-D score of 4 (out of 60), anxiety score of less than 1 (out of 9), and one negative life event in the past year. Scores on the inadequate emotional support indicator were a bit higher, with approximately 28% of participants reporting that they needed more emotional support than they received in the past year. There were significant black–white differences in the overall psychosocial risk burden score (p < .001); however, there were no significant race differences in depressive symptoms or anxiety symptoms and only a marginally significant difference in reports of negative life events over the previous year, with blacks reporting slightly more negative life events than whites. There were significant black–white differences in inadequate emotional support, with more blacks reporting inadequate emotional support over the previous year compared with whites (p < .001).
Table 2.
Participant Psychosocial Characteristics by Race
| Variable | All | Blacks | Whites | p value |
| Psychosocial risk burden | .59 (.58) | .66 (.02) | .53 (.02) | <.001 |
| CES-D (0–60) | 4.65 (5.33) | 4.66 (5.2) | 4.63 (5.42) | .90 |
| High CES-D (≥16), % | 4.5 | 4.5 | 4.5 | .99 |
| Anxiety (0–9) | .66 (1.2) | .63 (1.17) | .68 (1.23) | .25 |
| Life events (0–7) | 1.15(1.0) | 1.2 (1.06) | 1.11 (.95) | .05 |
| Inadequate emotional support, % | 27.5 | 35.1 | 22.5 | <.001 |
Note: CES-D = Center for Epidemiological Studies-Depression scale. Values shown are mean (SD) or N (%). p values are from t tests or chi-square tests comparing blacks and whites.
Psychosocial Risk Burden, Individual Psychosocial Risk Factors, and aPWV
In an initial multivariable linear regression model adjusted for age, sex, race, education, and site, overall psychosocial risk burden was not associated with aPWV (Estimate [Est] = .00, p = .83), however, there was a significant Race × Psychosocial risk burden index interaction (Est = .07, p = .01).
Additional analyses designed to identify the individual psychosocial risk factors underlying this association are presented in Table 3. In models adjusted for age, sex, race, education, and site, there were no significant main effects or Race × Psychosocial factor interaction effects for depressive symptoms, anxiety symptoms, or negative life events. There was a significant Race × Inadequate emotional support interaction (Est = .11. p = .001; Table 3).
Table 3.
Main and Interactive Effects of Individual Psychosocial Risk Burden Components on Aortic Pulse Wave Velocity
| Variable | Estimate | SE | p value |
| CES-D | .01 | .09 | .91 |
| Race × CES-D | .05 | .18 | .80 |
| Anxiety | .03 | .06 | .64 |
| Race × Anxiety | -.02 | .12 | .90 |
| Life events | -.05 | .05 | .37 |
| Race × Life events | -.02 | .11 | .83 |
| Inadequate support | .01 | .02 | .67 |
| Race × Inadequate support | .11 | .04 | .001 |
Note: CES-D = Center for Epidemiological Studies Depression scale. Results from linear regression models adjusted for age, race, sex, education, and study site. Models with interactions are also adjusted for the main effect of the psychosocial predictor.
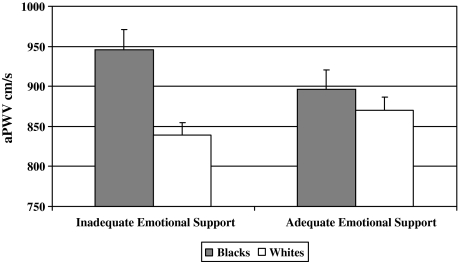
The Race × Inadequate emotional support interaction remained significant after further adjustments for behavioral and physiological cardiovascular risk factors (Est = .10, p = .005). This interaction is graphically illustrated in Figure 1 using back-transformed values of adjusted log aPWV means to facilitate interpretation. The association between inadequate emotional support and aPWV appeared to be considerably stronger in older blacks compared with whites. Adjusted aPWV for blacks with inadequate emotional support was 945.77 cm/s compared with 838.82 cm/s in whites with inadequate emotional support. Among those with adequate support, adjusted aPWV values for blacks and whites were more similar, at 896.05 cm/s and 870.44 cm/s, respectively (Figure 1).
Figure 1.
Racial differences in the association between inadequate emotional support and aPWV. Note: Values shown are mean levels of aortic pulse wave velocity by race for participants with inadequate and adequate levels of emotional support, adjusted for age, gender, education, prevalent cardiovascular disease, hypertension, diabetes, systolic blood pressure, fasting glucose, body mass index, smoking, low-density lipoprotein, high-density lipoprotein, and physical activity. p value for Race × Inadequate support interaction = .005.
These results were further supported in fully adjusted race-stratified models (Table 4), where findings revealed a significant association between inadequate emotional support and aPWV in older blacks (Est = .05, p = .04) but not whites (Est = −.04, p = .13).
Table 4.
Linear Regression Analysis: Inadequate Emotional Support and Log Aortic Pulse Wave Velocity by Race
| Blacks |
Whites |
|||||
| Variable | Estimate | SE | p value | Estimate | SE | p value |
| Inadequate emotional support | .05 | .03 | .04 | −.04 | .03 | .13 |
Note: Models are adjusted for age, gender, education, prevalent cardiovascular disease, hypertension, diabetes, fasting glucose, systolic blood pressure, body mass index, smoking, low-density lipoprotein, high-density lipoprotein, and physical activity. Model R2 = .11 for blacks and Model R2 = .12 for whites.
We then ran additional exploratory analyses to determine if racial differences in the association between inadequate emotional support and aPWV were largely determined by other factors known to (a) differ by race and (b) influence both emotional support and indicators of CVD. Thus, we included social network characteristics (friend and family social integration and number of people in the household) and marital status as potential “third variables” or confounders that might influence the race, inadequate emotional support, and aPWV association. Including these variables did not alter our results (data not shown).
DISCUSSION
We examined the associations among race, psychosocial risk factors, and arterial stiffening (measured by aPWV) in a sample of high-functioning older black and white adults. We were particularly interested in examining the affect of psychosocial risk burden—a combined index of depressive symptoms, anxiety symptoms, negative life events, and inadequate emotional support—on aPWV. We found a significant Race × Psychosocial risk burden interaction that appeared to be primarily driven by the “inadequate emotional support” component of the index.
Inadequate emotional support was associated with higher levels of arterial stiffening in older blacks but not Whites. This association was independent of behavioral and physiological cardiovascular risk factors, such as CVD, hypertension, diabetes, systolic blood pressure, high-density lipoprotein, low-density lipoprotein, BMI, smoking status, and physical activity. The observed association was also independent of social network characteristics and marital status.
We did not observe associations between any of the other psychosocial risk factors and aPWV for either racial/ethnic group. It is unclear whether this is due to the actual absence of an association between depressive symptoms, anxiety symptoms, negative life events, and aPWV or if our values on these variables were simply too low to observe associations. In one of the few studies to examine associations between psychosocial risk factors and aPWV, Tiemeier colleagues (19) also reported no association between depressive symptoms and aPWV. The few studies examining the association between anxiety symptoms and/or negative life events and aPWV have reported mixed results (20,21).
Inadequate emotional support has been linked to CVD morbidity and mortality in a number of prior studies (4,5) and is believed to be particularly relevant for older adult populations (33,34); however, it is unclear why it was only associated with aPWV in older blacks. Older blacks in our cohort were significantly more likely to report inadequate levels of emotional support compared with older whites, and in fact, this was the only psychosocial variable on which there were significant black–white differences. Because blacks, on average, die at younger ages than whites, this may be due to differences in mortality rates among close others, that is, the high-functioning older blacks in our cohort may have lost more close friends to premature death compared with high-functioning older whites. Indeed, similar to findings from other cohorts (35,36), exploratory analyses in our sample revealed that older blacks had slightly lower levels of social contact with friends and slightly higher levels of social contact with family compared with older whites (data not shown); however, controlling for these factors did not alter black–white differences in the association between inadequate emotional support and aPWV. Exploratory analyses also revealed that older blacks were less likely to be married and more likely to be widowed compared with older whites (data not shown); again, however, including marital status in the model did not alter our results.
Because older blacks have historically had much larger kin and extended kin networks than older whites (37), it is possible that the experience of having inadequate emotional support is felt more profoundly by older blacks compared with older whites, with older blacks expecting more emotional support and being particularly distressed when it is not present. Thus, one might expect the association between inadequate emotional support and aPWV in older blacks to be mediated by psychological distress. However, because neither anxiety symptoms nor depressive symptoms were associated with aPWV in this sample, factors other than psychological distress are likely accounting for the observed association.
It is possible that there are different physiological pathways through which inadequate emotional support affects aPWV for older blacks compared with whites, but there has been limited research in this area. Inadequate emotional support has been linked to hypothalamic–pituitary–adrenal axis dysregulation (38) and cardiovascular reactivity (39). Of these, cardiovascular reactivity may be particularly relevant for aPWV (40), given the relatively strong associations between measures of blood pressure (41), heart rate variability (10), and aPWV. To our knowledge, however, only one study has examined the associations among race, emotional support, and cardiovascular reactivity. In a sample of young black and white adults, Grewen colleagues (42) found that in the presence of an affectionate relationship (“warm partner contact”), blacks demonstrated much less cardiovascular reactivity than whites, indicating that emotional support may be particularly important for the cardiovascular health of black compared with white adults. Because this study focused on young adults, it is difficult to determine whether these findings would extend to an older population; however, they provide some support for the notion that the observed black–white differences in the association between inadequate emotional support and aPWV in our cohort could potentially be mediated through cardiovascular reactivity. Additional research in this area is warranted.
This study has limitations that should be noted. First, our sample was comprised of high-functioning black and white adults aged 70–79 years. Their high-functioning status may partially explain why we observed such low levels of depressive symptoms and anxiety. Consequently, this group may not be representative of older adults in general (and older blacks more specifically), which could limit the generalizability of these results. Second, we used a one-item measure of emotional support, which may not have captured all relevant aspects of this construct. Finally, our data were cross-sectional. Longitudinal studies are needed to determine the temporality of the observed associations and whether they persist over time.
Despite these limitations, our study has several strengths. To our knowledge, this study is the first to examine the associations between multiple indicators of psychosocial risk and aPWV. The study was conducted in a community-dwelling cohort, with large numbers of older black and white adults. We also used state-of-the-art assessment of arterial stiffening and controlled for a wide range of possible confounds.
In conclusion, we report for the first time an association between inadequate emotional support and aPWV in older blacks but not whites. The mechanisms underlying this association have yet to be determined; however, findings suggest that inadequate emotional support may be an important contributor to cardiovascular health in older black adults. Interventions aimed at improving emotional support may ultimately prove beneficial for older black adults.
FUNDING
The Health, Aging, and Body Composition Study was funded by the National Institute on Aging (N01-AG-6-2101, N01-AG-6-2103, and N01-AG-6-2106). T.T.L. received additional support from a Visiting Scholar Award funded by the National Center for Minority Health and Health Disparities and a Career Development Award funded by the National Heart, Lung, and Blood Institute (HL092591). This research was supported in part by the Intramural Research Program of the National Institutes of Health, National Institute on Aging.
References
- 1.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 2.Shen B-J, Avivi YE, Todaro JF, et al. Anxiety characteristics independently and prospectively predict myocardial infarction in men: the unique contribution of anxiety among psychologic factors. J Am Coll Cardiol. 2008;51:113–119. doi: 10.1016/j.jacc.2007.09.033. [DOI] [PubMed] [Google Scholar]
- 3.Wulsin LR, Vaillant GE, Wells VE. A systematic review of the mortality of depression. Psychosom Med. 1999;61:6–17. doi: 10.1097/00006842-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Krumholz HM, Butler J, Miller J, et al. Prognostic importance of emotional support for elderly patients hospitalized with heart failure. Circulation. 1998;97:958–964. doi: 10.1161/01.cir.97.10.958. [DOI] [PubMed] [Google Scholar]
- 5.Berkman LF, Leo-Summers L, Horwitz RI. Emotional support and survival after myocardial infarction. A prospective, population-based study of the elderly. Ann Intern Med. 1992;117:1003–1009. doi: 10.7326/0003-4819-117-12-1003. [DOI] [PubMed] [Google Scholar]
- 6.Iso H, Date C, Yamamoto A, et al. Perceived mental stress and mortality from cardiovascular disease among Japanese men and women: the Japan Collaborative Cohort Study for Evaluation of Cancer Risk Sponsored by Monbusho (JACC Study) Circulation. 2002;106:1229–1236. doi: 10.1161/01.cir.0000028145.58654.41. [DOI] [PubMed] [Google Scholar]
- 7.Matthews KA, Gump BB. Chronic work stress and marital dissolution increase risk of posttrial mortality in men from the Multiple Risk Factor Intervention Trial. Arch Intern Med. 2002;162:309–315. doi: 10.1001/archinte.162.3.309. [DOI] [PubMed] [Google Scholar]
- 8.Harris KF, Matthews KA, Sutton-Tyrrell K, Kuller LH. Associations between psychological traits and endothelial function in postmenopausal women. Psychosom Med. 2003;65:402–409. doi: 10.1097/01.psy.0000035720.08842.9f. [DOI] [PubMed] [Google Scholar]
- 9.Lewis TT, Everson-Rose SA, Colvin A, Matthews K, Bromberger JT, Sutton-Tyrrell K. Interactive effects of race and depressive symptoms on calcification in African American and white women. Psychosom Med. 2009;71:163–170. doi: 10.1097/PSY.0b013e31819080e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitchell GF, Parise H, Benjamin EJ, et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham Heart Study. Hypertension. 2004;43:1239–1245. doi: 10.1161/01.HYP.0000128420.01881.aa. [DOI] [PubMed] [Google Scholar]
- 11.Mitchell GF, Guo C-Y, Benjamin EJ, et al. Cross-sectional correlates of increased aortic stiffness in the community: the Framingham Heart Study. Circulation. 2007;115:2628–2636. doi: 10.1161/CIRCULATIONAHA.106.667733. [DOI] [PubMed] [Google Scholar]
- 12.Vaitkevicius PV, Fleg JL, Engel JH, et al. Effects of age and aerobic capacity on arterial stiffness in healthy adults. Circulation. 1993;88:1456–1462. doi: 10.1161/01.cir.88.4.1456. [DOI] [PubMed] [Google Scholar]
- 13.Najjar SS, Scuteri A, Lakatta EG. Arterial aging: is it an immutable cardiovascular risk factor? Hypertension. 2005;46:454–462. doi: 10.1161/01.HYP.0000177474.06749.98. [DOI] [PubMed] [Google Scholar]
- 14.van Popele NM, Grobbee DE, Bots ML, et al. Association between arterial stiffness and atherosclerosis: the Rotterdam Study. Stroke. 2001;32:454–460. doi: 10.1161/01.str.32.2.454. [DOI] [PubMed] [Google Scholar]
- 15.Kullo IJ, Bielak LF, Turner ST, Sheedy PF, 2nd, Peyser PA. Aortic pulse wave velocity is associated with the presence and quantity of coronary artery calcium: a community-based study. Hypertension. 2006;47:174–179. doi: 10.1161/01.HYP.0000199605.35173.14. [DOI] [PubMed] [Google Scholar]
- 16.Sutton-Tyrrell K, Najjar SS, Boudreau RM, et al. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation. 2005;111:3384–3390. doi: 10.1161/CIRCULATIONAHA.104.483628. [DOI] [PubMed] [Google Scholar]
- 17.Willum Hansen T, Staessen JA, Torp-Pedersen C, et al. Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation. 2006;113:664–670. doi: 10.1161/CIRCULATIONAHA.105.579342. [DOI] [PubMed] [Google Scholar]
- 18.Mattace-Raso FUS, van der Cammen TJM, Hofman A, et al. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation. 2006;113:657–663. doi: 10.1161/CIRCULATIONAHA.105.555235. [DOI] [PubMed] [Google Scholar]
- 19.Tiemeier H, Breteler MMB, van Popele NM, Hofman A, Witteman JCM. Late-life depression is associated with arterial stiffness: a population-based study. J Am Geriatr Soc. 2003;51:1105–1110. doi: 10.1046/j.1532-5415.2003.51359.x. [DOI] [PubMed] [Google Scholar]
- 20.Midei AJ, Matthews KA. Social relationships and negative emotional traits are associated with central adiposity and arterial stiffness in healthy adolescents. Health Psychol. 2009;28:347–353. doi: 10.1037/a0014214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nomura K, Nakao M, Karita K, Nishikitani M, Yano E. Association between work-related psychological stress and arterial stiffness measured by brachial-ankle pulse-wave velocity in young Japanese males from an information service company. Scand J Work Environ Health. 2005;31:352–359. doi: 10.5271/sjweh.918. [DOI] [PubMed] [Google Scholar]
- 22.Janice EW, Rebecca D-D, Moyses S. Trait anger and arterial stiffness: results from the Atherosclerosis Risk in Communities (ARIC) study. Prev Cardiol. 2006;9:14–20. doi: 10.1111/j.1520-037x.2006.1610.x. [DOI] [PubMed] [Google Scholar]
- 23.Vogelzangs N, Beekman AT, Kritchevsky SB, et al. Psychosocial risk factors and the metabolic syndrome in elderly persons: findings from the Health, Aging and Body Composition study. J Gerontol A Biol Sci Med Sci. 2007;62:563–569. doi: 10.1093/gerona/62.5.563. [DOI] [PubMed] [Google Scholar]
- 24.Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychol. 2003;22:300–309. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- 25.Ituarte PH, Kamarck TW, Thompson HS, Bacanu S. Psychosocial mediators of racial differences in nighttime blood pressure dipping among normotensive adults. Health Psychol. 1999;18:393–402. doi: 10.1037//0278-6133.18.4.393. [DOI] [PubMed] [Google Scholar]
- 26.Skarupski KA, Mendes de Leon CF, Bienias JL, et al. Black-white differences in depressive symptoms among older adults over time. J Gerontol B Psychol Sci Soc Sci. 2005;60:P136–P142. doi: 10.1093/geronb/60.3.p136. [DOI] [PubMed] [Google Scholar]
- 27.Heffernan KS, Jae SY, Fernhall B. Racial differences in arterial stiffness after exercise in young men. Am J Hypertens. 2007;20:840–845. doi: 10.1016/j.amjhyper.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 28.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 29.Roberts RE. Reliability of the CES-D scale in different ethnic contexts. Psychiatry Res. 1980;2:125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- 30.Breslau N. Depressive symptoms, major depression, and generalized anxiety: a comparison of self-reports on CES-D and results from diagnostic interviews. Psychiatry Res. 1985;15:219–229. doi: 10.1016/0165-1781(85)90079-4. [DOI] [PubMed] [Google Scholar]
- 31.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 32.Brach JS, Simonsick EM, Kritchevsky S, Yaffe K, Newman AB. The association between physical function and lifestyle activity and exercise in the health, aging and body composition study. J Am Geriatr Soc. 2004;52:502–509. doi: 10.1111/j.1532-5415.2004.52154.x. [DOI] [PubMed] [Google Scholar]
- 33.Lincoln KD, Taylor RJ, Chatters LM. Correlates of emotional support and negative interaction among older black Americans. J Gerontol B Psychol Sci Soc Sci. 2003;58:S225–S233. doi: 10.1093/geronb/58.4.s225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously. A theory of socioemotional selectivity. Am Psychol. 1999;54:165–181. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- 35.Ajrouch KJ, Antonucci TC, Janevic MR. Social networks among blacks and whites: the interaction between race and age. J Gerontol B Psychol Sci Soc Sci. 2001;56:S112–S118. doi: 10.1093/geronb/56.2.s112. [DOI] [PubMed] [Google Scholar]
- 36.Mendes de Leon CF, Gold DT, Glass TA, Kaplan L, George LK. Disability as a function of social networks and support in elderly African Americans and Whites: the Duke EPESE 1986–1992. J Gerontol B Psychol Sci Soc Sci. 2001;56:S179–S190. doi: 10.1093/geronb/56.3.s179. [DOI] [PubMed] [Google Scholar]
- 37.Taylor RJ, Chatters LM, Tucker MB, Lewis E. Developments in research on black-families—a decade review. J Marriage Fam. 1990;52:993–1014. [Google Scholar]
- 38.Seeman TE, McEwen BS. Impact of social environment characteristics on neuroendocrine regulation. Psychosom Med. 1996;58:459–471. doi: 10.1097/00006842-199609000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Kamarck TW, Manuck SB, Jennings JR. Social support reduces cardiovascular reactivity to psychological challenge: a laboratory model. Psychosom Med. 1990;52:42–58. doi: 10.1097/00006842-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 40.Malik AR, Kondragunta V, Kullo IJ. Forearm vascular reactivity and arterial stiffness in asymptomatic adults from the community. Hypertension. 2008;51:1512–1518. doi: 10.1161/HYPERTENSIONAHA.107.106088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Najjar SS, Scuteri A, Shetty V, et al. Pulse wave velocity is an independent predictor of the longitudinal increase in systolic blood pressure and of incident hypertension in the Baltimore Longitudinal Study of Aging. J Am Coll Cardiol. 2008;51:1377–1383. doi: 10.1016/j.jacc.2007.10.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grewen KM, Anderson BJ, Girdler SS, Light KC. Warm partner contact is related to lower cardiovascular reactivity. Behav Med. 2003;29:123–130. doi: 10.1080/08964280309596065. [DOI] [PubMed] [Google Scholar]