Abstract
The health consequences of obesity and overweight have been well documented, but less research has examined their social and economic consequences. This paper examines the long-term consequences of early adult overweight for midlife health and socioeconomic attainment using prospective nationally representative panel data from American adults in the Monitoring the Future Study (1986–2008). Growth mixture models identified 2 distinct latent classes of trajectories of body mass index (BMI) from age 19 to 35 years: a persistently overweight class (BMI >25 kg/m2) and a second class exhibiting more moderate growth in BMI to age 35 years. Women (odds ratio (OR) = 2.16, 95% confidence interval (CI): 1.39, 3.36) and those from a lower childhood socioeconomic position (OR = 1.71, 95% CI: 1.30, 2.24) were more likely to be in the persistently overweight class. Compared with those in the moderately increasing BMI class, those in the persistently overweight class were more likely to have a chronic health problem at age 40 years (OR = 2.74, 95% CI: 2.20, 3.43), to have no further education beyond high school (OR = 1.33, 95% CI: 1.04, 1.69), and to have a higher odds of receiving welfare or unemployment compensation at age 40 years (OR = 1.76, 95% CI: 1.49, 2.04). These findings highlight the importance of addressing persistent obesity and overweight early in the life course.
Keywords: human development, obesity, social class
The prevalence of obesity has been increasing (1–6), with well-documented health consequences (7, 8). Obesity has repeatedly been associated with increased risk for cardiovascular disease, diabetes, cancer, and physical disability (9–12), with adverse effects of lifetime cumulative obesity for subsequent mobility limitations (13), mortality (14–16), and the onset of physical impairment up to 50 years later (17).
A parallel but smaller body of work has examined the social and economic consequences of early life obesity and overweight. Obesity is associated with lower self-esteem in adolescent girls (7, 18) and with persistent deleterious effects on self-esteem (19), as well as lower wages (20), into adulthood. American women who were obese in adolescence were found to have lower levels of social achievement in early adulthood (fewer years of advanced education, lower rates of marriage, higher rates of poverty) than women who were not obese at the same ages (21). Similar findings were found using data from the British Cohort Study, where persistent obesity in women between the ages of 10 and 30 years was associated with never having been gainfully employed and not having a current partner (22). However, obesity limited only to childhood showed no persistent socioeconomic effects into adulthood (22).
From a life course perspective (23, 24), the long-term health and socioeconomic consequences of early life overweight and obesity may unfold through processes of cumulative disadvantage (25–30). Evidence from clinical and population studies suggests that early life socioeconomic disadvantage beginning in utero leads to low birth weight and rapid growth during infancy, which increases the risk for childhood as well as adult obesity, along with the subsequent risk for adult chronic diseases (31–37). In turn, health problems decrease socioeconomic reserves to manage and cope with existing conditions, resulting in the progression of health problems and reinforcement of socioeconomic disadvantage throughout the life course.
Yet, most of the literature on the long-term implications of overweight and obesity is not based on prospective longitudinal data with repeated measures to permit a full examination of this process of cumulative disadvantage over the life course. Typically, researchers use 2 data points to relate early life weight with later life health and mortality (e.g., Viner and Cole (22)). As a result, the full scope of variability within 2 discrete data points is ignored. Moreover, it is unclear from these studies whether it is simply early life obesity or persistent obesity across adulthood that has consequences for later health and socioeconomic attainment—issues that cannot be differentiated with only 2 data points.
This paper uses repeated measures of weight gathered prospectively from age 19 to 40 years to capture the full course of weight change across the transition from young adulthood to midlife. We hypothesize that there may be distinct patterns of weight gain over adulthood with different consequences for midlife health and socioeconomic attainment. We bring together the literatures in life course epidemiology with those in obesity research using nationally representative prospective data on American young adults and their transition to mid-adulthood over a 22-year period.
MATERIALS AND METHODS
Study population
Data were drawn from the Monitoring the Future project, a nationwide school-based survey of substance use and related attitudes and beliefs conducted annually in the United States since 1975 (38). The survey also includes self-reported measures of respondents’ weight and height collected since 1986. Monitoring the Future is a cohort sequential study (described in more detail elsewhere (39)) involving a nationally representative sample of high school seniors surveyed in the spring of each year (approximately 15,000 per year). Each year's data collection takes place in about 135 public and private high schools selected to provide an accurate representative cross section of 12th graders throughout the coterminous United States.
A representative subsample (∼2,400 students/year) is randomly selected from each cohort for 7 biennial follow-ups to the age of 32 years, and then at age 35 years and every 5 years thereafter, using self-completed mailed questionnaires. Drug users were oversampled for participation in the panel component by a factor of 3.0 and then reweighted in the analyses, as discussed below. To ease respondent burden, panel respondents are randomly assigned to receive 1 of 5 different questionnaires, each with its own set of questions. Since 1986, a random one-fifth of respondents (approximately 480 students per class) received the questionnaire asking about height and weight. For our purposes we focus on subjects in 11 high school cohorts entering the study between 1976 and 1986 (inclusive), yielding 5,233 individuals who were between the ages of 19 and 40 years over this 22-year period. Repeat measures of height and weight are modeled from 1986 forward to 2008 or age 40 years, whichever comes first. There were no exclusion criteria. All study procedures are reviewed and approved on an annual basis by the University of Michigan's Institutional Review Board for compliance with federal guidelines for the treatment of human subjects.
Measures
Weight gain over adulthood was captured with measurement of body mass index (BMI; kg/m2). A BMI score of 25–29 is used to define “overweight,” while a BMI score of 30 or above represents “obese” (40). Three variables capture key indicators of early social position found to be related to lifetime obesity as well as to midlife health and socioeconomic attainment: 1) gender; 2) race/ethnicity (self-reported by respondents and modeled using 3 dummy variables contrasting black, Hispanic, and other race/ethnic (including Asian) respondents with non-Hispanic white respondents); and 3) childhood socioeconomic status (SES) (the maximum of the respondent's parents’ education, dichotomized as high school degree or less vs. college degree or higher). Region of residence in senior year of high school (South, North Central, Northeast, and West) captures elements of the surrounding socioeconomic and environmental context that may be related to BMI trajectories over and above individual socioeconomic and sociodemographic risk (41). We also adjust for high school academic performance captured through an ordinal 9-category measure of average grade in high school (modeled using the midpoint value of each category).
Five measures capture health and social position at age 40 years. The presence of any chronic health problem is captured with a dummy variable to indicate any 1 of 6 medically diagnosed chronic health conditions reported by the respondent at age 40 years (hypertension, diabetes, asthma, chronic lung disease (including chronic bronchitis or emphysema), heart disease, and cancer). Four dummy variables capture social and economic hardship at age 40 years: was on welfare or received unemployment compensation in the previous year; home ownership; no current partner; and those who, by age 40 years, had not received any further education beyond high school.
Statistical analyses
We used generalized growth mixture modeling to identify latent classes of individuals according to their long-term patterns of BMI growth and then examined the relation between trajectory classes and midlife health and social outcomes at age 40 years. Growth mixture modeling is an extension of conventional growth modeling that relaxes the assumption of a single population trajectory. By using latent trajectory classes (categorical latent variables), the growth mixture model allows different classes of individuals to vary around different mean growth curves (42, 43). The trajectory of interest in this paper is weight gain (captured with BMI), measured prospectively from young adulthood (age 19 years) to age 35 years, as it relates to midlife health and social outcomes at age 40 years.
The structural part of the model incorporates the growth model within a larger latent variable model by relating the growth factors to other observed and latent variables. Of particular interest is the latent trajectory class variable, which represents the unobserved subpopulation of membership for respondents. Early life sociodemographic covariates predict class membership in a multinomial logistic regression. As a general extension of the growth mixture model, we include distal outcomes, health, and socioeconomic attainment at age 40 years, which are predicted from the growth model controlling for early life sociodemographic covariates (43).
Model building proceeded in a sequential process by first specifying the measurement model and then incrementally increasing the number of latent classes. Good-fitting models are characterized by 1) a low value for the Bayesian Information Criterion and Akaike Information Criterion; 2) a statistically significant Lo-Mendell-Rubin likelihood ratio test; 3) distinct posterior probabilities for individual class membership; and 4) differences in the mean outcome variable across classes (42, 43). All models are estimated in Mplus version 5.2 (44) using full information maximum likelihood with robust standard errors. Multiple random starts are used to minimize local optimal in the likelihood. Respondent-level weights are used to adjust for unequal selection probabilities in the panel study.
Retention rates in the panel respondents are highest in the first follow-up after high school (averaging 70%) and fall to an average of 64% in the biennial follow-ups through to age 32 years. Longer-term retention rates (at ages 35–40 years) are about 52% (38). Using logistic regression analysis (with backward elimination), we modeled the probability of study retention to age 40 years according to a broad array of baseline characteristics and found that white race and reporting of a higher average grade in high school increased the odds of retention. By including these variables in our models, maximum likelihood produces unbiased coefficients under the assumption that the attrition process is conditional on observed variables in our models (45–47).
RESULTS
Sociodemographic characteristics at senior year for the study sample are presented in Table 1. On average, respondents had a normal weight in the year following high school (BMI = 22.6; standard deviation, 3.0; Table 1), but these cohorts of American adults gained weight steadily over adulthood, reporting an average BMI of 27.0 (standard deviation, 4.4) by age 40 years. Consistent with other national surveys (e.g., the National Health and Nutrition Examination Survey 1999–2000), hypertension was diagnosed in almost one-fifth of the study sample by midlife, and roughly one-third had any 1 of 6 chronic health problems. A minority of respondents were receiving welfare or unemployment compensation at the age of 40 years, and just under half had no further education beyond high school.
Table 1.
Descriptive Statistics for the Study Sample (Ages 19–40 Years), Monitoring the Future Study, 1986–2008 (N = 5,233)
| Overall Sample |
Latent Class 1 (Normative Weight Gain) |
Latent Class 2(Persistently Overweight) |
||||
| Weighted Percent | Mean (SD) | Weighted Percent | Mean (SD) | Weighted Percent | Mean (SD) | |
| Sociodemographic characteristics | ||||||
| Female | 51.9 | 48.5 | 75.3 | |||
| White | 78.7 | 84.8 | 81.2 | |||
| Non-Hispanic black | 11.9 | 7.6 | 11.2 | |||
| Hispanic | 4.0 | 2.9 | 2.3 | |||
| Other race/ethnicity | 5.3 | 4.7 | 5.3 | |||
| Childhood SES | ||||||
| Parents have high school education or less | 63.8 | 59.7 | 74.8 | |||
| Parents have college degree or higher | 36.2 | 40.3 | 25.2 | |||
| Average grade in high school | 84.0 (5.9) | 84.4 (6.7) | 82.7 (6.7) | |||
| Region of residence at baselinea | ||||||
| South | 31.5 | 28.0 | 36.3 | |||
| Northeast | 23.5 | 24.9 | 19.7 | |||
| North Central | 29.2 | 31.2 | 28.7 | |||
| West | 15.7 | 15.9 | 15.3 | |||
| BMI over early adulthood, kg/m2 | ||||||
| Age 19 years | 22.6 (3.0) | 21.5 (2.2) | 26.0 (4.3) | |||
| Age 21 years | 23.3 (3.4) | 21.9 (2.3) | 27.4 (4.5) | |||
| Age 23 years | 23.4 (3.4) | 22.1 (2.4) | 28.0 (4.3) | |||
| Age 25 years | 23.9 (3.5) | 22.5 (2.5) | 28.7 (4.2) | |||
| Age 27 years | 24.3 (3.6) | 22.9 (2.7) | 29.4 (3.9) | |||
| Age 29 years | 24.8 (3.8) | 23.3 (2.9) | 30.1 (3.9) | |||
| Age 31 years | 25.2 (3.8) | 23.6 (2.9) | 30.8 (3.9) | |||
| Age 35 years | 25.8 (3.9) | 24.2 (3.0) | 31.3 (3.7) | |||
| Health status at age 40 years | ||||||
| Hypertension | 17.2 | |||||
| Diabetes | 2.9 | |||||
| Asthma | 8.7 | |||||
| Lung disease | 2.2 | |||||
| Heart disease | 2.6 | |||||
| Cancer | 4.3 | |||||
| Any chronic health problem | 30.9 | 25.9 | 48.2 | |||
| SES at age 40 years | ||||||
| Receiving welfare or unemployment compensation | 6.9 | 6.8 | 9.8 | |||
| Home ownership | 81.5 | 81.6 | 80.2 | |||
| No further education beyond high school | 41.9 | 40.7 | 55.4 | |||
| No current partner | 9.0 | 8.5 | 9.1 | |||
Abbreviations: BMI, body mass index; SD, standard deviation; SES, socioeconomic status.
Baseline refers to senior year of high school.
Table 2 reports the fit statistics for a progression of growth mixture models. The first row (model A) pertains to the linear single-class model. Average BMI at age 19 years is 22.4 (intercept) and increases by 0.23 points each year (slope, P < 0.001) until age 35 years. (The distribution of BMI at each time point is roughly normal, justifying the linear model.) The fit of the model improves by allowing for correlated error between BMI measures at adjacent time points (model B) (all 7 correlations are statistically significant at P < 0.0001).
Table 2.
Linear Growth Mixture Models for BMI Trajectories Over Adulthood (Ages 19–35 Years), Monitoring the Future Study, 1986–2008 (N = 5,233)
| Model | Log Likelihood | BIC | AIC | |
| A: | Single-class linear growth | −43,898.6 | 87,906.0 | 87,823.2 |
| B: | + Correlated measurement error over time | −43,685.8 | 87,538.9 | 87,411.5 |
| C: | + Two-class solution | −43,227.7 | 86,673.1 | 86,507.5 |
| D: | + Covariates | −39,629.4 | 79,847.0 | 79,400.9 |
Abbreviations: AIC, Akaike Information Criterion; BIC, Bayesian InFormation Criterion; BMI, body mass index.
The third row of Table 2 (model C) reports the fit statistics for the 2-class solution. The change in the Bayesian Information Criterion and Akaike Information Criterion values, coupled with a significant Lo-Mendell-Rubin likelihood ratio test (P < 0.001), suggests that a 2-class solution is preferable to a single-class model. Membership in each class showed good classification quality, with individuals most likely to belong to their predicted class (posterior probability is markedly higher (>0.90) than for the other class). Adding a third class (model not shown) did not result in any improvement in model fit, and the posterior probabilities did not differentiate class membership well.
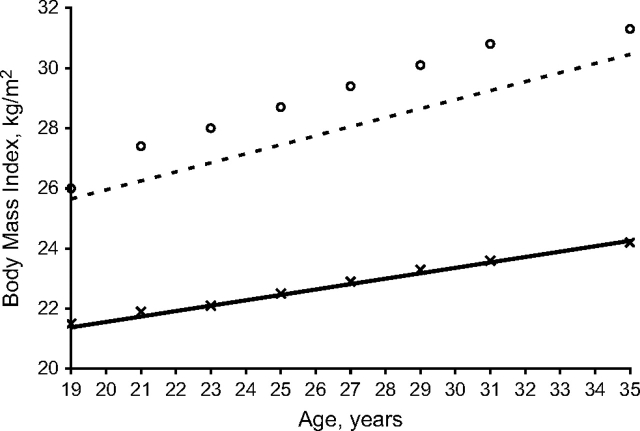
Figure 1 shows the estimated growth curves for BMI from age 19 to 35 years according to the 2-class solution (observed mean BMI scores are also plotted for each class). The 2 curves represent 2 distinct trajectories of BMI growth from early adulthood: Class 1 (with 80.9% of the sample) represents the majority of the sample, which we term the “normative class,” with an average BMI of 21.4 following high school and a steady rate of growth in BMI up to age 35 years (slope = 0.18, P < 0.001). Conversely, individuals in class 2 (19.1% of the sample) were on average overweight at high school graduation (mean BMI = 25.7) and gained weight more rapidly throughout the next 15 years (slope = 0.30, P < 0.001), whom we term the “persistently overweight class.” The model supports a class-varying factor covariance matrix, where the growth factor variances are allowed to differ across classes. Results indicate greater variance around the intercept and slope for the persistently overweight class (σ2 = 23.41 and 0.102, respectively) compared with the normative class (σ2 = 3.64 and 0.004, respectively).
Figure 1.
Trajectories of body mass index over adulthood (Monitoring the Future Study, 1986–2008): Growth mixture model showing 2-class solution. Solid line: class 1 = normative weight gain (80.9%) (x = observed mean body mass index scores for class 1).
Dashed line: class 2 = persistently overweight (19.1%) (o = observed mean body mass index scores for class 2).
Model D in Table 2 adds the covariates to the model, regressing gender, race/ethnicity, childhood SES, region, and academic performance on class membership. The model also specifies class-specific effects of the covariates on the growth factors. For ease of model interpretation, average grade in high school is centered at the mean. The fit of the model improves significantly, and the results provide insight into the underlying reasons for the different trajectory patterns. Table 3 reports the results from the logistic regression for class membership (adjusted odds ratios and 95% confidence intervals using the normative latent class as the reference class. Compared with individuals in the normative class, individuals in the persistently overweight class are more likely to be female and to come from a lower socioeconomic background. (See also descriptive statistics by latent class, Table 1.) The odds of membership in the persistently overweight class are significantly reduced among those with a higher average grade in high school (controlling for childhood SES and other covariates). There was no significant association between race/ethnicity and class membership after adjusting for gender and socioeconomic position.
Table 3.
Logistic Regression for Latent Class Membership, Monitoring the Future Study, 1986–2008 (N = 5,233)
| Latent Class 2a(Persistently Overweight) |
||
| OR | 95% CI | |
| Femaleb | 2.16 | 1.39, 3.36* |
| Blackc | 1.23 | 0.79, 1.93 |
| Hispanicc | 0.51 | 0.23, 1.09 |
| Other race/ethnicityc | 1.08 | 0.59, 1.97 |
| Low childhood SESd | 1.71 | 1.30, 2.24* |
| South regione | 1.34 | 0.94, 1.90 |
| West regione | 1.34 | 0.89, 2.03 |
| North Central regione | 0.99 | 0.69, 1.41 |
| Average grade in high school | 0.96 | 0.94, 0.98* |
Abbreviations: CI, confidence interval; OR, adjusted odds ratio; SES, socioeconomic status.
*P < 0.001 (2-tailed tests).
Latent class 1 (normative weight gain) is the reference class.
Reference group is male.
Reference group is white.
Refers to those whose parents have a high school education or less; reference group is parents with a college degree or higher.
Reference group is high school residence in the Northeast region of the United States.
The within-class influence of the covariates on the growth factors varies significantly across class. Table 4 presents the unstandardized regression coefficients (with standard errors) for the effects of the covariates on BMI intercept and slope for each of the 2 latent classes. Within the persistently overweight class, the rate of growth in BMI is more rapid for women (although their initial status at age 19 years is somewhat lower on average than that of men). On the other hand, the rate of growth in the persistently overweight class is significantly attenuated among those residing in the North Central and South regions of the United States. Within the normative class, Hispanics have a much faster rate of growth in BMI than whites, all other factors held constant.
Table 4.
Regressing Growth Parameters on Sociodemographic Characteristics by Latent Class of BMI Trajectory: Monitoring the Future Study, 1986–2008 (N = 5,233)a
| Latent Class 1(Normative Class) |
Latent Class 2(Persistently Overweight) |
|||
| Intercept | Slope | Intercept | Slope | |
| Femaleb | −2.599*** (0.128) | −0.041*** (0.010) | −1.204* (0.532) | 0.245*** (0.031) |
| Blackc | 0.531** (0.224) | 0.032 (0.019) | 1.315 (0.873) | −0.031 (0.054) |
| Hispanicc | 0.136 (0.352) | 0.096*** (0.027) | 3.084 (1.729) | 0.061 (0.101) |
| Other race/ethnicityc | −0.919*** (0.233) | 0.021 (0.019) | −0.468 (1.128) | 0.018 (0.088) |
| Low childhood SESd | −0.167 (0.114) | 0.017 (0.009) | −0.142 (0.516) | −0.009 (0.033) |
| South regione | −0.508*** (0.154) | 0.024 (0.012) | 0.575 (0.658) | −0.092* (0.042) |
| West regione | −0.307 (0.174) | −0.008 (0.014) | −0.343 (0.770) | −0.073 (0.045) |
| North Central regione | −0.163 (0.149) | 0.003 (0.012) | 1.684* (0.718) | −0.172*** (0.048) |
| Average grade in high school | −0.002 (0.009) | −0.001 (0.001) | 0.002 (0.036) | 0.001 (0.002) |
Abbreviations: BMI, body mass index; SES, socioeconomic status.
* P < 0.05; ** P < 0.01; *** P < 0.001 (2-tailed tests).
Cell entries are unstandardized regression coefficients; standard errors are in parentheses after the parameter estimates.
Reference group is male.
Reference group is white.
Refers to those whose parents have a high school education or less; reference group is parents with a college degree or higher.
Reference group is high school residence in the Northeast region of the United States.
The next step in the modeling process adds the distal outcomes at age 40 years. In these models, membership in a particular latent trajectory class between ages 19 and 35 years predicts health and SES at age 40 years, controlling for early life sociodemographic factors. Table 5 presents the odds ratios for these midlife outcomes using the normative class as the reference class. Relative to those who leave high school with a normal BMI and gain weight gradually over adulthood, those who are persistently overweight have odds of reporting any medically diagnosed chronic health condition at age 40 years that are over 3-fold higher (odds ratio (OR) = 3.33, adjusted for baseline covariates). Part of this effect appears to operate through mediating processes that may lie on the causal pathway, including financial hardship (being on welfare or collecting unemployment compensation), a lack of further education beyond high school, and lack of a current partner (adjusted OR = 2.74), but there remains a net direct effect of persistent overweight on the risk for chronic health problems at age 40 years. There is also a net effect of persistent overweight on the absence of higher education (adjusted OR = 1.33, P < 0.05), which remains after adjusting for potential confounders and mediators.
Table 5.
Logistic Regression Results for Midlife Health and Socioeconomic Outcomes by Latent Class of BMI Trajectory, Monitoring the Future Study, 1986–2008 (N = 5,233)
| Class 2a(Persistently Overweight) |
||||
| Outcome at Age 40 years | Adjusted for Baseline Covariatesb |
Adjusted for Baseline Covariatesb and Other Outcomes at Age 40 Years |
||
| OR | 95% CI | OR | 95% CI | |
| Any chronic health problem | 3.33 | 2.44, 4.21* | 2.74 | 2.20, 3.43* |
| Receiving welfare or unemployment compensation | 1.76 | 1.49, 2.04* | 1.36 | 0.92, 1.99 |
| Home ownership | 0.66 | 0.18, 1.14 | 1.08 | 0.81, 1.44 |
| No further education | 1.46 | 1.04, 1.88* | 1.33 | 1.04, 1.69* |
| No current partner | 1.61 | 1.33, 1.89* | 1.44 | 0.97, 2.15 |
Abbreviations: BMI, body mass index; CI, confidence interval; OR, odds ratio.
P < 0.05 (2-tailed tests).
Class 1 (normative weight gain) is the reference class.
Baseline covariates include gender, race/ethnicity, childhood socioeconomic status, region of residence, average grade in high school.
When adjusted for baseline sociodemographic characteristics, the odds of reporting socioeconomic hardship at age 40 years in the form of receiving welfare or unemployment compensation are over 50% greater for those who remain persistently overweight compared with those in the normative class (OR = 1.76). However, most of this effect operates through intervening statuses, including the onset of health problems and the lack of further education and a current partner (adjusted OR = 1.36). Thus, it is the elevated risk for socioeconomic hardship and health problems associated with persistent overweight that increases the risk for receiving welfare or unemployment compensation at age 40 years, not the history of persistent overweight per se. Similarly, some of the effect of persistent overweight on having no current partner in midlife operates through intervening mechanisms such as health problems and socioeconomic hardship. However, there remains a moderate (marginally statistically significant) net effect of persistent overweight on having no current partner at age 40 years (OR = 1.44, P < 0.10). Home ownership in midlife is not associated with being persistently overweight after adjusting for potential confounders and mediators.
DISCUSSION
This paper considers the long-term consequences of young adult weight gain for health and socioeconomic attainment in midlife. We found 2 distinct patterns of BMI growth over early adulthood (ages 19–35 years) in a national sample of Americans followed over a 22-year period. One pattern is slow, steady growth following a normal BMI in high school. The other represents people who started out with a high BMI in high school (BMI >25) and remained persistently overweight throughout early adulthood. We found notable health and socioeconomic consequences of being in the persistently overweight class. Those who were persistently overweight were more likely to have a medically diagnosed chronic health problem at age 40 years. These include nontrivial medical conditions surfacing at a relatively young age. Compared with those experiencing more gradual weight gain, the persistently overweight were also more likely to have pursued no further education beyond high school and to have no current partner. Persistent overweight was also associated with higher odds of receiving welfare or unemployment compensation at age 40 years, which was found to operate partly through health and socioeconomic pathways.
Early life disadvantage is a critical factor in membership in these 2 trajectories. Persons from low SESs were more likely to be in the persistently overweight class, controlling for gender, race/ethnicity, and geographic region of the United States. As early life socioeconomic disadvantage increases exposure to risk and as socioeconomic advantage increases exposure to opportunity (29), the “Matthew effect” comes into play (48). Referring to the Gospel of St. Matthew—“For unto every one that hath shall be given and he shall have abundance: but from him that hath not shall be taken away even that which he hath”—the Matthew effect describes how those in advantaged social circumstances are better able to reinforce their position by accruing better jobs and income and more education and health benefits over the course of their lives, thereby reducing their exposure to risk factors and lifestyles that typically compromise health. Conversely, those with fewer resources are at increased risk for health and socioeconomic decline as exposure to disadvantage multiplies over the life course in the form of cumulative inequality that reinforces their position of social and economic disadvantage (27, 29, 30).
However, we also found that the odds of membership in the persistently overweight class were significantly reduced among those with a higher average grade in high school (controlling for childhood SES), suggesting that individual resources and other collective social capital operating in the school setting can attenuate the risk for obesity and overweight even among those from a lower SES. These findings suggest that strategies aimed at supporting socially disadvantaged youth in the school context may hold promise for altering their trajectory of weight gain and subsequent health and socioeconomic challenges. Consistent with findings that suggest that reducing educational disengagement and increasing academic performance can contribute to less cigarette and other drug use (49), our results here suggest that academic performance in high school, to the extent that it can be fostered and promoted in socially disadvantaged youth, has the potential to alter the trajectory of adult weight gain and subsequent midlife outcomes.
Regarding limitations, we cannot be certain of the causal associations assumed in these analyses, although the use of longitudinal data identifies the temporal sequence consistent with the assumed casual sequence. Ideally we would have liked to include a control for early life health status, but such a measure is not available in these data. However, we endeavored to account for early life health and social risk by including measures of childhood SES and race/ethnicity, which are highly correlated with early life health status (50, 51). Another limitation includes nonrandom attrition in the panel data, but this was to some degree statistically adjusted for in the analyses. Self-reported measures of weight tend to be underestimated (52), and this varies by education, gender, and race/ethnicity. However, if this underreporting is consistent over time, the slope estimates for the growth trajectories should not be affected.
In sum, these results highlight the importance of understanding midlife health and socioeconomic attainment from a life course perspective, where early life disadvantage manifests in more rapid weight gain throughout early adulthood, with adverse consequences for midlife outcomes. Tailoring policies and interventions to the needs and circumstances of the poorest population groups is therefore critical for stemming the cycle of cumulative disadvantage.
Acknowledgments
Author affiliations: Institute for Social Research, University of Michigan, Ann Arbor (Philippa J. Clarke, Patrick M. O'Malley, John E. Schulenberg, Lloyd D. Johnston); and Department of Psychology, University of Michigan, Ann Arbor (John E. Schulenberg).
This work was supported by the Robert Wood Johnson Foundation, as part of the Youth, Education, and Society (YES) Project (64703). YES is an integral part of a larger research initiative of the Robert Wood Johnson Foundation entitled Bridging the Gap: Research Informing Practice and Policy for Healthy Youth Behavior. “Bridging the Gap” utilizes data from the Monitoring the Future study, funded by the National Institute on Drug Abuse, one of the National Institutes of Health.
The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the sponsors.
Conflict of interest: none declared.
Glossary
Abbreviations
- BMI
body mass index
- CI
confidence interval
- MTF
- OR
odds ratio
- SES
socioeconomic status
References
- 1.Flegal KM, Carroll MD, Kuczmarski RJ, et al. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord. 1988;22(1):39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 2.Hedley AA, Ogden CL, Johnson CL, et al. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291(23):2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 3.Lewis CE, Jacobs DR, Jr, McCreath H. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA Study. Coronary Artery Risk Development in Young Adults. Am J Epidemiol. 2000;151(12):1172–1181. doi: 10.1093/oxfordjournals.aje.a010167. [DOI] [PubMed] [Google Scholar]
- 4.Mokdad AH, Bowman BA, Ford ES, et al. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286(10):1195–1200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 5.Maillard G, Charles MA, Thibult N. Trends in the prevalence of obesity in the French adult population between 1980 and 1991. Int J Obes Relat Metab Disord. 1999;23(4):389–394. doi: 10.1038/sj.ijo.0800831. [DOI] [PubMed] [Google Scholar]
- 6.Kuczmarski RJ, Flegal KM, Campbell SM, et al. Increasing prevalence of overweight among US adults. The National Health and Nutrition Examination Surveys, 1960 to 1991. JAMA. 1994;272(3):205–211. doi: 10.1001/jama.272.3.205. [DOI] [PubMed] [Google Scholar]
- 7.Reilly JJ, Methven E, McDowell ZC, et al. Health consequences of obesity. Arch Dis Child. 2003;88(9):748–752. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(3):518–525. [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services. The Surgeon General's Call to Action to Prevent and Decrease Overweight and Obesity. Rockville, MD: Public Health Service, Office of the Surgeon General; 2001. [PubMed] [Google Scholar]
- 10.Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs: obesity outranks both smoking and drinking in its deleterious effects on health and health costs. Health Aff. 2002;21(2):245–253. doi: 10.1377/hlthaff.21.2.245. [DOI] [PubMed] [Google Scholar]
- 11.Field AE, Coakley EH, Must A, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med. 2001;161(3):1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- 12.Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 13.Houston DK, Ding J, Nicklas BJ, et al. Overweight and obesity over the adult life course and incident mobility limitation in older adults: the Health, Aging and Body Composition Study. Am J Epidemiol. 2009;169(8):927–936. doi: 10.1093/aje/kwp007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Troiano RP, Frongillo EA, Jr, Sobal J, et al. The relationship between body weight and mortality: a quantitative analysis of combined information from existing studies. Int J Obes Relat Metab Disord. 1996;20(1):63–75. [PubMed] [Google Scholar]
- 15.Hoffmans MD, Kromhout D, de Lezenne Coulander C. The impact of body mass index of 78,612 18-year old Dutch men on 32-year mortality from all causes. J Clin Epidemiol. 1988;41(8):749–756. doi: 10.1016/0895-4356(88)90161-8. [DOI] [PubMed] [Google Scholar]
- 16.Engeland A, Bjørge T, Søgaard AJ, et al. Body mass index in adolescence in relation to total mortality: 32-year follow-up of 227,000 Norwegian boys and girls. Am J Epidemiol. 2003;157(6):517–523. doi: 10.1093/aje/kwf219. [DOI] [PubMed] [Google Scholar]
- 17.Ferraro KF, Kelley-Moore JA. Cumulative disadvantage and health: long-term consequences of obesity? Am Sociol Rev. 2003;68(5):707–729. [PMC free article] [PubMed] [Google Scholar]
- 18.Strauss RS. Childhood obesity and self-esteem. Pediatrics. 2000;105(1):e15. doi: 10.1542/peds.105.1.e15. (doi:10.1542/peds.105.1.e15) [DOI] [PubMed] [Google Scholar]
- 19.Stunkard A, Burt V. Obesity and the body image. II. Age at onset of disturbances in the body image. Am J Psychiatry. 1967;123(11):1443–1447. doi: 10.1176/ajp.123.11.1443. [DOI] [PubMed] [Google Scholar]
- 20.Register CA, Williams DR. Wage effects of obesity among young workers. Soc Sci Q. 1990;71(1):130–141. [Google Scholar]
- 21.Gortmaker SL, Must A, Perrin JM, et al. Social and economic consequences of overweight in adolescence and young adulthood. N Engl J Med. 1993;329(14):1008–1012. doi: 10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- 22.Viner RM, Cole TJ. Adult socioeconomic, educational, social, and psychological outcomes of childhood obesity: a National Birth Cohort Study. BMJ. 2005;330(7504):1354. doi: 10.1136/bmj.38453.422049.E0. (doi:10.1136/bmj.38453.422049.E0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31(2):285–293. [PubMed] [Google Scholar]
- 24.Elder GH., Jr Time, human agency, and social change: perspectives on the life course. Soc Psychol Q. 1994;57(1):4–15. [Google Scholar]
- 25.Dannefer D. Aging as intracohort differentiation: accentuation, the Matthew effect, and the life course. Sociol Forum. 1987;2(2):211–236. [Google Scholar]
- 26.Dannefer D. Cumulative advantage/disadvantage and the life course: cross-fertilizing age and social science theory. J Gerontol B Psychol Sci Soc Sci. 2003;58(6):S327–S337. doi: 10.1093/geronb/58.6.s327. [DOI] [PubMed] [Google Scholar]
- 27.O'Rand AM. The precious and the precocious: understanding cumulative disadvantage and cumulative advantage over the life course. Gerontologist. 1996;36(2):230–238. doi: 10.1093/geront/36.2.230. [DOI] [PubMed] [Google Scholar]
- 28.O'Rand AM. Cumulative advantage theory in life course research. In: Crystal S, Shea DF, editors. Annual Review of Gerontology and Geriatrics: Focus on Economic Outcomes in Later Life. New York, NY: Springer; 2003. pp. 14–30. [Google Scholar]
- 29.Ferraro KF, Shippee TP. Aging and cumulative inequality: how does inequality get under the skin? Gerontologist. 2009;49(3):333–343. doi: 10.1093/geront/gnp034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferraro KF, Shippee TP, Schafer MH. Cumulative inequality theory for research on aging and the life course. In: Bengston VL, Silverstein M, Putney NM, et al., editors. Handbook of Theories of Aging. New York, NY: Springer; 2009. pp. 573–593. [Google Scholar]
- 31.Greenlund KJ, Liu K, Dyer AR, et al. Body mass index in young adults: associations with parental body size and education in the CARDIA Study. Am J Public Health. 1996;86(4):480–485. doi: 10.2105/ajph.86.4.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lawlor DA, Ebrahim S, Davey Smith G. Socioeconomic position in childhood and adulthood and insulin resistance: cross sectional survey using data from British Women's Heart and Health study. BMJ. 2002;325(7369):805. doi: 10.1136/bmj.325.7368.805. (doi:10.1136/bmj.325.7368.805) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Godfrey KM, Barker DJ. Fetal nutrition and adult disease. Am J Clin Nutr. 2000;71(5 suppl) doi: 10.1093/ajcn/71.5.1344s. 1344S–1352S. [DOI] [PubMed] [Google Scholar]
- 34.Singhal A, Lucas A. Early origins of cardiovascular disease: is there a unifying hypothesis? Lancet. 2004;363(9421):1642–1645. doi: 10.1016/S0140-6736(04)16210-7. [DOI] [PubMed] [Google Scholar]
- 35.Power C, Manor O, Matthews S. Child to adult socioeconomic conditions and obesity in a national cohort. Int J Obes Relat Metab Disord. 2003;27(9):1081–1086. doi: 10.1038/sj.ijo.0802323. [DOI] [PubMed] [Google Scholar]
- 36.Ziol-Guest KM, Duncan GJ, Kalil A. Early childhood poverty and adult body mass index. Am J Public Health. 2009;99(3):527–532. doi: 10.2105/AJPH.2007.130575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scharoun-Lee M, Kaufman JS, Popkin BM, et al. Obesity, race/ethnicity and life course socioeconomic status across the transition from adolescence to adulthood. J Epidemiol Community Health. 2009;63(2):133–139. doi: 10.1136/jech.2008.075721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johnston LD, O'Malley PM, Bachman JG, et al. Monitoring the Future National Survey Results on Drug Use, 1975–2008: Volume 1, Secondary School Students. Bethesda, MD: National Institute on Drug Abuse; 2008. (NIH publication no. 07-6205) [Google Scholar]
- 39.Bachman JG, Johnston LD, O'Malley PM, Schulenberg . The Monitoring the Future Project After Thirty-Two Years: Design and Procedures. (Occasional Paper No. 64) Ann Arbor, MI: Institute for Social Research; 2006. [Google Scholar]
- 40.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the Evidence Report. National Institutes of Health. Obes Res. 1998;6(suppl 2) 51S–209S. [PubMed] [Google Scholar]
- 41.Levi J, Vinter S, Richardson L, et al. F as in Fat: How Obesity Policies are Failing in America. Washington, DC: Trust for America's Health; 2009. [Google Scholar]
- 42.Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24(6):882–891. [PubMed] [Google Scholar]
- 43.Muthén BO. Latent variable analysis: growth mixture modelling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of Quantitative Methodology for the Social Sciences. Newbury Park, CA: Sage; 2004. pp. 345–368. [Google Scholar]
- 44.Muthén BO, Muthén LK. MPlus User's Guide. Los Angeles, CA: Muthén & Muthén; 1998. [Google Scholar]
- 45.Cnaan A, Laird NM, Slasor P. Using the general linear mixed model to analyse unbalanced repeated measures and longitudinal data. Stat Med. 1997;16(20):2349–2380. doi: 10.1002/(sici)1097-0258(19971030)16:20<2349::aid-sim667>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 46.McArdle JJ, Hamagami F. Modeling incomplete longitudinal and cross-sectional data using latent growth structural models. Exp Aging Res. 1992;18(3-4):145–166. doi: 10.1080/03610739208253917. [DOI] [PubMed] [Google Scholar]
- 47.Feng D, Silverstein M, Giarrusso R, et al. Attrition of older adults in longitudinal surveys: detection and correction of sample selection bias using multigenerational data. J Gerontol B Psychol Sci Soc Sci. 2006;61(6):S323–S328. doi: 10.1093/geronb/61.6.s323. [DOI] [PubMed] [Google Scholar]
- 48.Merton RK. The Matthew effect in science: theoretical and empirical investigations. Science. 1968;159(3810):56–63. [PubMed] [Google Scholar]
- 49.Bachman JG, O'Malley PM, Schulenberg JE, et al. The Education-Drug Use Connection: How Successes and Failures in School Relate to Adolescent Smoking, Drinking, Drug Use, and Delinquency. New York, NY: Lawrence Erlbaum Associates/Taylor & Francis; 2008. [Google Scholar]
- 50.Bradley RH, Corwyn RF. Socioeconomic status and child development. Annu Rev Psychol. 2002;53:371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- 51.Aber JL, Bennett NG, Conley DC, et al. The effects of poverty on child health and development. Annu Rev Public Health. 1997;18:463–483. doi: 10.1146/annurev.publhealth.18.1.463. [DOI] [PubMed] [Google Scholar]
- 52.Stewart AW, Jackson RT, Ford MA, et al. Underestimation of relative weight by use of self-reported height and weight. Am J Epidemiol. 1987;125(1):122–126. doi: 10.1093/oxfordjournals.aje.a114494. [DOI] [PubMed] [Google Scholar]