Abstract
The objective of this study was to compare comorbidity, functional ability, and health care utilization in veterans with total knee arthroplasty (TKA) or total hip arthroplasty (THA) versus matched control populations. A cohort of veterans using Veterans Affairs (VA) healthcare system reported limitations in six activities of daily living (ADLs; bathing, dressing, eating, walking, transferring, and using the toilet), demographics, and physician-diagnosed comorbidity. VA databases provided healthcare utilization and International Classification of Diseases-9/Common procedure terminology codes for TKA/THA. Patients were classified as: (1) primary TKA; (2) primary THA; (3) combination group (≤1 procedure); and (4) control veteran population (no THA/TKA). Multivariable regression analyses compared the risk or counts of ADL limitation and in-/out-patient visits. After multivariable adjustment, TKA, THA or combination groups had significantly higher prevalence of the following compared to veteran controls: arthritis, diabetes, or heart disease (p<0.0001 each), severe (≥3) ADL limitation (33%, 42%, 42% vs. 24%; p<0.0001), and annual hospitalization rate (24%, 19%, 26% vs. 16%, p<0.0001). Annual outpatient surgery visits were more (2.5, 2.3, 2.3 vs. 2, p=0.01) and risk of any mental health outpatient visit was lower (12%, 11%, 12% vs. 18%, p=0.0039). All ADLs, except eating, were significantly more limited in arthroplasty groups (p= 0.0009). Severe ADL limitation was more prevalent in veterans with arthroplasty than in two age-matched US cohorts: 13.4 times in ≥65 years; and 1.2-, 1.6-, and 4-fold in ≥85, 75–84, and 65–74 years. Poorer function and higher comorbidity and utilization in veterans with TKA/THA suggest that this group is appropriate for interventions targeted at improving function and decreasing utilization.
Keywords: Arthroplasty, Functional status, Healthcare utilization, Total hip arthroplasty, Total joint arthroplasty, Total knee arthroplasty, Veterans
Introduction
Total knee arthroplasty and total hip arthroplasty (TKA and THA) are among the most common orthopedic procedures performed in the USA to relieve pain and improve function and quality of life of patients with end-stage arthritis [1–3]. Osteoarthritis, the most common underlying arthritic diagnosis in patients undergoing TKA or THA, is the fifth most common condition among veterans [4, 5]. Approximately 202,500 primary TKA [6] and 402,100 primary THA surgeries were performed in the USA in 2003 [7]. The median cost for primary joint arthroplasty was $12,846 at the USA hospitals between 1997 and 2001 [8]; Medicare paid $3.2 billion for these procedures in 2000 [9]. The prevalence of TKA and THA are increasing, and it is projected that by 2030, the number of primary THAs in USA will grow 174% to 572,000 and primary TKA by 673% to 3.48 million procedures per year [7]. The public health burden of this high-volume procedure and overall societal costs are, hence, likely to increase substantially and consistently for the foreseeable future.
Most studies of post-arthroplasty functional outcomes are single-center cohorts or clinical trials, which tend to recruit healthier populations and report success rates exceeding 95%. Very few studies have assessed functional and health outcomes at a population level [10, 11] or in high-risk groups such as veterans [6, 12]. To our knowledge, none of the published studies have assessed functional or activities of daily living (ADL) limitation in a population-based veteran sample. A 6-month study of a community-based prospective cohort of 276 TKA and 228 THA reported lower physical function than age–sex-matched US population norms [10]. Similarly, a population-based cross-sectional study found that 63% of THA/TKA vs. 36% non-arthroplasty patients reported knee pain [11], a number much higher than that reported in prospective cohorts or clinical trials [13–15]. These studies demonstrate that patient outcomes differ between population-based and nonpopulation-based single-center studies or clinical trials. Population-level studies of community-dwelling patients with arthroplasty can more accurately inform us of their burden of functional limitation.
Veterans have higher comorbidity than nonveterans [16], a factor that negatively impacts arthroplasty outcomes [17–20]. Australian veterans had lower preoperative knee function score than their civilian counterparts [6]. In a small study of US veterans, compared to civilian counterparts, despite being younger veterans had more complications, longer hospital stay and reduced knee motion up to 2-year post-TKA [12]. These studies indicate that functional outcomes in veterans are perhaps less optimal than civilians. VA constitutes the largest integrated healthcare system in the USA serving 4.9 million subjects with a budget of $25 billion [21]. Many veterans eligible for Medicare use dual services [22]. Studying utilization and functional limitation in this cohort, hence, has implications for both Medicare and VA healthcare system.
In our recent study, we found profound physical health-related quality of life deficits in veterans with TKA/THA compared both to age-matched general US population and to demographic–comorbidity-matched veterans without arthroplasty [23]. The purpose of this study was to further explore comorbidity, functional status, and utilization in this cohort of veterans with TKA/THA as compared to veteran controls and to previously described US cohort populations. Our objectives were to: (1) describe comorbidity, functional status, and utilization in veterans with TKA/THA; (2) compare the functional limitations of veterans with TKA/THA to age-matched US general populations; and (3) compare comorbidity, functional status, and utilization in veterans with TKA/THA to veterans who have not undergone these procedures, in unadjusted univariate analyses and multivariable-adjusted analyses.
Methods
A cohort of veterans utilizing Upper Midwest Veterans Integrated Service Network (VISN-13: Minnesota, North Dakota, and South Dakota, and selected counties in Iowa, Nebraska, Wisconsin, and Wyoming) for healthcare services between 10/1/1996 and 3/31/1998 with valid mailing addresses was identified. We conducted a cross-sectional survey by mail: querying demographics, and performance of ADLs and HRQOL using the Short Form-36 for veterans (SF-36 V; details previously published as VISN 13 Veterans Quality-QOL Study [24]). Nonresponders received the same survey 10 weeks after the first mailing. Overall, 58% responded to the survey (40,508 of the 70,334 population).
Demographic questions included: education level, race or ethnicity, and current use of cigarettes. ADL questions asked about performance of six activities: bathing, dressing, eating, walking, transferring, and using the toilet—a validated measure of ADL ability [25] commonly used [26, 27]. Survey data were supplemented by data obtained from the national VA database included age, International Classification of Diseases-9 codes for TKA/THA and comorbid conditions, marital and employment status, and inpatient and outpatient healthcare utilization.
Gender, age, race, marital status, employment status, service connection, health care utilization, and site use (single- vs. multisite use) were obtained from the administrative databases. Education level, self-reported physician diagnosis of six common diseases—arthritis, asthma/chronic obstructive pulmonary disease (COPD), diabetes, depression, heart disease and hypertension, ADL limitation, and HRQoL were obtained from the survey.
Study outcomes
Outcomes of this current study included:
Comorbidity: measured by self-report of physician diagnosis of six diseases;
ADL limitation: percent of subjects with limitations in each ADL, overall ADL limitation (none, moderate (one to two ADL limitation)) or severe (≥3 ADLs with limitation) categorized as in previous studies [26, 28] and number of ADLs with limitations per subject; and
Healthcare utilization for the year after the survey: outpatient visits as a continuous variable (primary care, medical subspecialty, surgery clinic) and inpatient and mental health visits as categorical variables (none vs. one or more), due to a right-skewed distribution.
Healthcare utilization data were obtained from in- and out-patient VA datasets, shown reliable for demographics and valid for most common [29] and specific diagnoses [30, 31].
Covariates/predictor variables
We obtained both unadjusted univariate and multivariable-adjusted estimates of ADL limitation and health care utilization. All multivariable regression models adjusted for the following covariates or confounders:
Socio-demographic: age (in years), employment status (employed, unemployed, retired, unknown), marital status (married, not married; all database-derived); gender (male, female), race (White, non-White), education level (less than 8th grade, some high school, high school graduate, college and beyond; all survey derived);
Comorbidity: Patient report of six, common physician-diagnosed comorbidities: arthritis, asthma/COPD, diabetes, depression, hypertension, heart disease (database-derived); current smoking status: current smoker vs. nonsmoker (survey-derived);
Healthcare access: single vs. multiple VA site use; percent service connection—veterans get service connection ranging from 0% to 100% for health conditions due to or diagnosed during active duty and veterans with >50% service connection get priority in health care access.
Prior healthcare utilization: since prior utilization has strong association with future utilization, we adjusted the models for utilization outcomes for the respective prior year utilization (for example for future primary care visit model was adjusted for prior year primary care visits) in addition to the above variables.
Models for mortality were additionally adjusted for in-and out-patient utilization in the pre-survey year and the physical and mental component summary scores of the SF-36 V. Database derived variables were available for most of the sample (~70,000); survey derived variables for ~35,000–40,000 responders to the questionnaire.
Statistical analyses
Continuous and categorical variables, between subjects with and without TKA/THA, were compared between survey responders and nonresponders using Student’s t test and chi-square test. Individual and overall ADL limitation rates in veterans with arthroplasty were compared to two age-matched US populations: the 1998 Health and Retirement Survey (HRS, a national probability sample of adults ≥65 years) [26] and the San Luis Valley Health and Aging study that used stratified sampling on age and ethnicity of residents ≥60 years from two rural Southern Colorado counties [27].
Multiple logistic regression analyses modeled the prevalence of any hospitalization, any mental health care visit, limitation of each ADL, and overall ADL limitation comparing veterans with THA, TKA, combination, and veterans without arthroplasty model estimated probabilities were calculated using average values of the additional covariates. Odds ratios (OR) and 95% confidence intervals (CI) are presented. To test whether TKA/THA status is independently associated with severe overall ADL limitation, we performed a multivariable logistic regression analysis with all variables listed above plus the TKA/THA status variable as predictor and severe ADL limitation as an outcome. Multiple linear regression analyses using least squares means were used to obtain the number of primary care, specialty, and surgical care visits in post-survey year. All analyses were performed using SPSS, version 11.5 (Chicago IL) and SAS, version 9.0 (Cary, NC). Due to multiple comparisons performed, comparison-wise p values <0.01 were considered statistically significant. The large sample size, however, somewhat mitigates the importance of statistical significance, and so the focus of the results and interpretation is based on the effect size of the observed differences.
Since the results from unadjusted analyses did not differ from the multivariable-adjusted regression analyses, we present both but discuss only the multivariable-adjusted regression estimates.
Results
Demographic characteristics
Unadjusted healthcare utilization data were available for 70,334 patients. This population cohort included 740 patients with TKA, 374 had THA, and 639 constituted the combination group. The remaining 69,238 patients constituted the control group. Data on comorbidity and ADL limitations were gathered from 40,508 survey respondents (58% of the 70,334 patients). The sample included 531 patients (1.3%) with TKA, 254 (0.6%) had THA, and 461 (1%) constituted the combination group. The remaining 39,262 (97%) formed the control group.
The 29,826 patients who provided healthcare utilization data but did not respond to the survey were similar to responders in most characteristics except that they were significantly younger (56.3 vs. 64.5 years), less likely to be married (47% vs. 64.9%), and less likely to be retired (26.7% vs. 43.9%).
Veterans with TKA, THA, and combination group had their index (of first) surgery 2.3±2.6, 2.3±2.5, and 3.0± 2.8 years prior to the survey, respectively. Veterans with TKA (n=531) or THA (n=254) were 9–11 years older than the control population, were more likely married, had higher service connection, were less likely to be smokers or employed, and were less educated (Table 1). Veterans with TKA/THA were more likely to report physician-diagnosed arthritis, diabetes and heart disease but had a similar prevalence of asthma/COPD, depression, and hypertension, with an overall higher comorbidity load (Table 2). Minor differences in race and gender were noted among the groups.
Table 1.
Demographic characteristics of the study population
| Control (n=36,978–70,991) | Primary TKA (n=516–531) | Primary THA (n=247–254) | Combination group (n=447–461) | P value | |
|---|---|---|---|---|---|
| Age in years | 60.7±15.4 | 71.6±9 | 69.4±11.2 | 72.2±9.1 | <0.001 |
| % Male | 95% | 97% | 97% | 97% | 0.003 |
| % White | 94% | 96% | 99% | 98% | <0.001 |
| % Married | 52% | 70% | 60% | 67% | <0.001 |
| % Currently smokea | 24% | 11% | 16% | 13% | <0.001 |
| % Employed | 34% | 19% | 21% | 15% | <0.001 |
| % Educated college and beyonda | 36% | 21% | 27% | 25% | <0.001 |
| % Service connection | |||||
| None or 0% | 61% | 49% | 63% | 54% | <0.001 |
| 1–49% | 25% | 26% | 18% | 20% | |
| 50–100% | 14% | 25% | 19% | 26% | |
Survey-derived measures were available for 36,978–39,297 subjects; race data were available for 41,954 patients; all other measures were available for administrative database ~70,542–70,991 subjects
p-values represent the differences between the four groups of patients
Table 2.
Prevalence of comorbid conditions in population cohorts
| Control (n=33,404–38,688) | Primary TKA (n=420–529) | Primary THA (n=209–248) | Combination group (n=377–454) | P value | |
|---|---|---|---|---|---|
| Arthritis | 53% | 86% | 84% | 84% | <0.001 |
| Asthma/COPD | 26% | 27% | 24% | 25% | 0.72 |
| Depression | 28% | 31% | 26% | 31% | 0.31 |
| Diabetes | 18% | 26% | 16% | 22% | <0.001 |
| Hypertension | 35% | 36% | 39% | 40% | 0.056 |
| Heart disease | 34% | 42% | 33% | 42% | <0.001 |
| # of comorbid conditions | 1.7±1.2 | 2.1±1.2 | 1.9±1.2 | 2.1±1.2 | <0.001 |
| % with ≥2 comorbidities | 52% | 65% | 56% | 67% | <0.001 |
More ADL limitation in veterans with arthroplasty compared to general US population
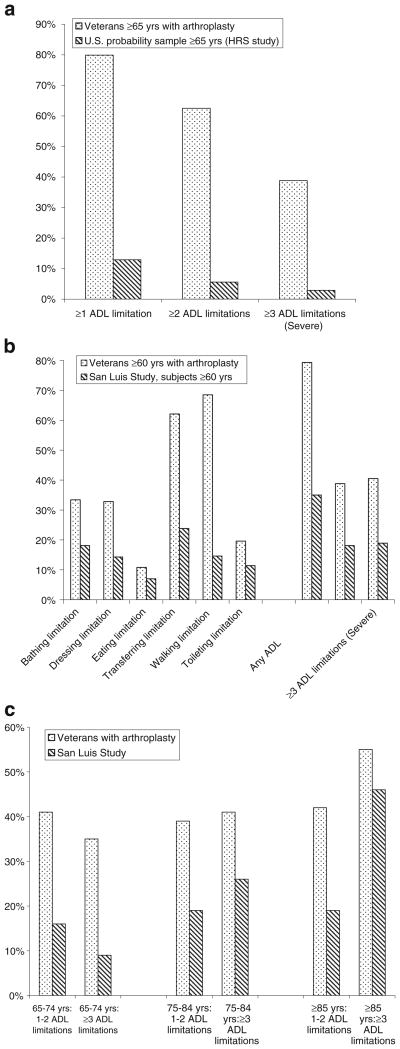
Comparing the ADL limitation rates of our veterans with arthroplasty to age-matched US populations revealed huge differences. Veterans with arthroplasty ≥65 years were 6.2, 11.2, and 13.4 times as likely as the age-matched HRS respondents with arthritis to have ≥1, ≥2, and ≥3 ADL limitations, respectively (Fig. 1a). Compared to age-matched San Luis Valley cohort aged ≥60 years, veterans with arthroplasty were 1.5–2.6 times as likely to report limitation in each of the five ADLs and 4.7 times to have limitation in walking (Fig. 1b). In each age-group (65–74, 75–84, and ≥85), moderate limitation (limitation of one to two ADLs) was twice as likely in veterans with arthroplasty compared to San Luis cohort. Severe ADL limitation was 3.9, 1.6, and 1.2 times as likely in the 65–74-, 75–84-, and ≥85-year-old veterans with arthroplasty, as compared to San Luis cohort in the same age groups (Fig. 1c).
Fig. 1.
Age-matched comparisons of ADL limitation in veterans3 (current study) to the 1998 Health and Retirement Survey (≥65 years) from AHEAD Study (a) [28] and the San Luis Valley Health and Aging Study (≥60 years; b, c) [29]. (a) Y-axis represents percent of patients with limitation in each category. Veterans with arthroplasty ≥65 years were compared to an age-matched US Cohort from the 1998 Health and Retirement Survey (≥65 years) from the AHEAD Study, a population-based cohort. Veterans were 6.2, 11.2 and 13.4 times as likely as the age-matched HRS respondents with arthritis to have ≥1, ≥2 and ≥3 ADL limitations, respectively. (b) The figure shows limitation of each ADL as well as overall number of ADLs with limitation comparing veterans to an age-matched San Luis Valley cohort aged ≥60 years, a population-based cohort. Veterans with arthroplasty reported limitation in each of the five ADLs 1.5–2.6 times as often as the San Luis Valley cohort and 4.7 times to have limitation in walking. Any ADL limitation, 1–2 ADL limitation and ≥3 ADL limitation were each twice as frequent in veterans as in age-matched San Luis cohort. (c) Veterans with arthroplasty were twice as likely as the San Luis cohort to report moderate limitation (limitation of 1–2 ADLs) in each age group (65–74, 75–84, and ≥85). Compared to San Luis cohort in the same age groups, veterans with arthroplasty reported severe ADL limitation 3.9 times in the 65–74 year group, 1.6 times in 75–84 year group, and 1.2 times in the ≥85 year group
ADL limitation is greater in veteran arthroplasty cohorts compared to veteran controls
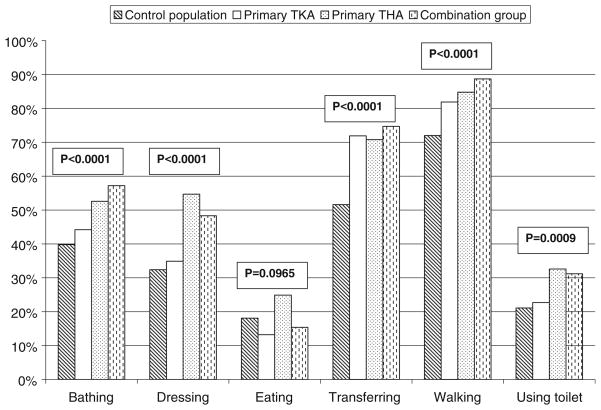
Multivariable-adjusted estimates of limitation in each ADL are shown in Table 3 (univariate estimates were similar and therefore not shown). Compared to the control veteran population, 4–17% more veterans with arthroplasty had limitations in bathing; 2–22% with dressing; 19–23% with transferring from chair; 10–17% more with walking; and 2–11% more with using the toilet. All differences were clinically and statistically significant (p≤0.0009; Table 3 and Fig. 3).
Table 3.
Multivariable-adjusted estimates of ADL limitations (N=15,385–15,853)
| Control population (%) | Primary TKA (%) | Primary THA (%) | Combination group (%) | P value | |
|---|---|---|---|---|---|
| Limitation in | |||||
| Bathing | 39.8 | 44.2 | 52.6 | 57.2 | <0.0001 |
| Dressing | 32.4 | 34.9 | 54.7 | 48.3 | <0.0001 |
| Eating | 18.1 | 13.2 | 24.9 | 15.4 | 0.0965 |
| Transferring | 51.6 | 71.9 | 70.8 | 74.7 | <0.0001 |
| Walking | 72 | 81.9 | 84.8 | 88.7 | <0.0001 |
| Using toilet | 21.1 | 22.7 | 32.6 | 31.2 | 0.0009 |
| Overall ADL limitation | <0.0001 | ||||
| None | 38.5 | 29.1 | 21.7 | 21.7 | |
| Moderate | 37.3 | 38.1 | 36.4 | 36.4 | |
| Severe | 24.2 | 32.8 | 41.8 | 41.8 | |
Adjusted for age, gender, race, education level, employment status, marital status, smoking status, self-report of six physician-diagnosed comorbidities (asthma/COPD, arthritis, depression, diabetes, heart disease, hypertension, percent service connection and single vs. multiple-site use); univariate results not presented since results were similar
Fig. 3.
Multivariable-adjusteda estimates of limitation of the six activities of daily living (ADLs). aAdjusted for age, gender, race, education level, employment status, marital status, smoking status, self-report of six physician-diagnosed comorbidities (asthma/COPD, arthritis, depression, diabetes, heart disease, hypertension), percent service connection and single vs. multiple-site use
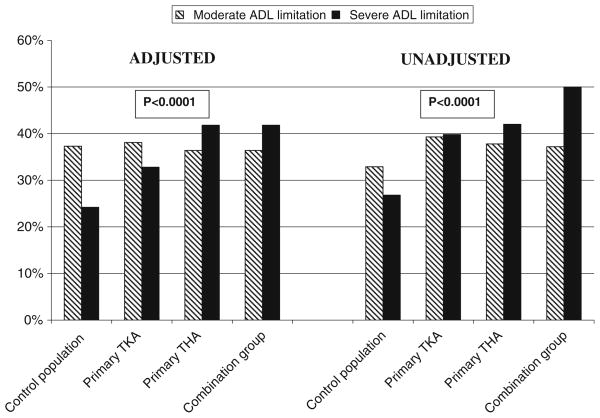
Overall ADL limitation was greater among the arthroplasty groups (primary TKA, primary THA, and combination group) compared to the control group via an unadjusted analysis. Specifically, there was much higher prevalence of severe ADL limitation (40%, 42%, 50% vs. 27%) and higher prevalence of moderate ADL limitation (39%, 37%, 38% vs. 32%), respectively (p<0.0001; Table 3). These differences attenuated slightly after multivariable adjustment, but results remained basically the same in terms of interpretation (Fig. 2).
Fig. 2.
Multivariable-adjusteda and unadjusted estimates of proportion of patients with moderate [1, 2] ADL and severe (≥3) ADL limitation. TKA total knee arthroplasty; THA total hip arthroplasty. aAdjusted for age, gender, race, education level, employment status, marital status, smoking status, self-report of six physician-diagnosed comorbidities (asthma/COPD, arthritis, depression, diabetes, heart disease, hypertension), percent service connection, and single vs. multiple-site use
Presence of arthroplasty was significantly independently associated with severe ADL limitation in a multivariable-adjusted regression (p<0.001). Patients with TKA had the increased odds of severe ADL limitation (OR=1.59, 95% CI, 1.21, 2.09), followed by THA with an OR of 2.1 (95% CI, 1.43, 3.08) and the combination group with an OR of 2.3 (95% CI, 1.73, 3.05), relative to the control group.
Higher inpatient, outpatient surgery clinic, but lower mental health clinic use in TKA/THA groups compared to veteran controls
Multivariable-adjusted analyses revealed that veterans in primary TKA, primary THA, and combination group had significantly higher utilization than control population. There was a higher risk of one or more inpatient admission in the post-survey year (24%, 19%, 26% vs. 16%, respectively; p<0.0001); higher number of annual surgery outpatient stops (2.5, 2.3, 2.3 vs. 2; p=0.01); and lower prevalence of any annual mental health clinic stops (12%, 11%, 12% vs. 18%, p=0.0039; Table 4). Annual primary care and medical subspecialty stop rates were similar. Adjusted annual mortality was similar across all groups.
Table 4.
Annual healthcare utilization and mortality (mean ± standard error of mean; N=15,073–15,107)
| Adjusteda |
Unadjusted |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Control group | Primary TKA | Primary THA | Combination group | P value | Control group | Primary TKA | Primary THA | Combination group | P value | |
| Primary care clinic | 3.1±0.02 | 3.3±0.2 | 3.0±0.2 | 3.3±0.2 | 0.2805 | 3.1±0.02 | 4±0.2 | 3±0.3 | 3.8±0.2 | <0.0001 |
| Medical subspecialty clinic | 1.7±0.03 | 1.7±0.2 | 2.1±0.3 | 1.8±0.2 | 0.5930 | 1.7±0.04 | 2±0.3 | 2.4±0.5 | 3±0.4 | 0.0012 |
| Surgery clinic | 2±0.02 | 2.5±0.2 | 2.3±0.2 | 2.3±0.2 | 0.0100 | 1.9±0.03 | 4±0.2 | 4.2±0.3 | 5.1±0.2 | <0.0001 |
| ≥1 mental health clinic visits | 17.5% | 11.6% | 10.9% | 12.3% | 0.0039 | 8.4% | 8.3% | 10.3% | 10.2% | 0.8714 |
| ≥1 hospitalizations | 15.7% | 24.1% | 19.1% | 25.6% | <0.0001 | 22.0% | 25.2% | 21.7% | 23.4% | 0.7385 |
| 1-year mortalityb | 2.8% | 1.9% | 0.6% | 2.7% | 0.1736 | 3.8% | 3.6% | 0.9% | 5.9% | 0.1242 |
Adjusted for age, gender, race, education level, employment status, marital status; smoking status, self-report of six physician-diagnosed comorbidities (asthma/COPD, arthritis, depression, diabetes, heart disease, hypertension); percent service connection and single vs. multiple-site use; and respective prior utilization in the pre-survey year
models adjusted for variables listed above plus all pre-survey year inpatient and outpatient utilization and physical and mental component summary scores of the SF-36 V
Discussion
The results of this population-based study of veterans provide strong and consistent evidence across multiple analytical approaches that arthroplasty status in veterans is a marker of poorer ADL ability. The differences between the arthroplasty and control group in terms of severe ADL limitation (7–18% difference in absolute numbers) and health care utilization (20% and 25%) are clinically meaningful in that patients with arthroplasty will require substantially more care to address the ADL deficits. These differences also have significant cost and health outcomes impact, considering that one million arthroplasty procedures are done in the USA every year, and the number will increase by 2-fold for hip and 7-fold for knee arthroplasty by the year 2030 [7].
The prevalence (adjusted) of ADL limitation in veterans with arthroplasty was up to 12 times higher compared to age–gender–comorbidity-matched veteran controls without arthroplasty and to two age-matched US cohorts (one with arthritis and one general). This is a new finding to our knowledge. The only previous population-based study of outcomes in Australian veterans vs. civilians used short-form 36, a health status or health-related quality-of-life measure, and Knee Society Score, a physician-administered pain/function scale (6)—neither is a validated measure of ADL limitation. Our study provides convincing evidence that arthroplasty status in veterans is, in fact, a strong surrogate for significant ADL limitation. ADL limitation, in turn, is a significant predictor of healthcare services utilization [32, 33], use of nursing homes [34], and mortality [35, 36].
These results have important implications. If ADL limitation and/or its progression were even partially preventable, healthcare costs, and health outcomes can be positively impacted by improving ADL ability. Studies are needed to investigate the causes of ADL limitation and to design interventions to prevent ADL limitations and/or improve ADL ability.
The differences in ADL limitations are not due to veteran status only because of the inclusion of control veteran populations in our study. These differences may be due to more severe contralateral hip/knee arthritis, more severe medical comorbidity, higher prevalence of unmeasured comorbidity (renal failure, post-traumatic stress disorder, alcohol use, or metabolic syndrome), and higher complication rate and reduced knee range of motion post-TKA in veterans compared to civilians [12]. Regardless of the underlying cause of these severe ADL limitations, arthroplasty status in veterans is a surrogate for high risk for dependence in activities of daily living.
Our observation of slightly higher ADL limitation in THA vs. TKA is somewhat in contrast to better outcomes reported in THA in nonveteran populations. This finding needs to be confirmed in other veteran populations. We speculate that the veterans may have had more severe hip arthritis and or higher prevalence of hip fracture as the indication for THA than nonveterans; veterans and non-veterans differ in comorbidities and many other factors that could also explain these differences.
Higher surgery clinic utilization in veterans with THA/TKA compared to veteran controls may be due to higher orthopedics clinic utilization and/or to more severe medical comorbidities. Higher inpatient utilization may be due to more severe comorbidity. There are no prior studies of VA-healthcare utilization in veterans with arthroplasty; therefore, no comparisons can be made. Further studies should investigate whether severity of arthritis and comorbidity severity are associated with these outcomes and whether better management of these conditions can improve functional status and decrease utilization.
There are limitations to our study. The findings may not be generalizable to nonveterans, females, or to other VA service networks. Nonresponders were younger subjects likely to have better functional status which could have led to slight overestimation of ADL limitation. However, this bias is unlikely to explain 2–10-fold higher ADL limitation in ours vs. age-matched US controls or age–gender–comorbidity-matched veteran controls. Due to the observational nature of the study, residual confounding due to unmeasured variables such as other comorbidities (alcohol use, post-traumatic stress disorder, metabolic syndrome, renal failure, etc.) is possible. We did not have any measure of severity of arthritis, and more importantly, any way to assess if patients with THA/TKA were more likely to have arthritis in the opposite knee and/or hip or other joints, which may have contributed to the poorer functional status in this group. Utilization assessment was limited to VA, and since many veterans use Medicare and VA for their healthcare needs [22], we likely underestimated the overall utilization by veterans. Future studies should examine other activities of living and/or vocational activities in these cohorts.
Our population-based study had a reasonable sample size that provided >1,000 patients with arthroplasty. We controlled for a variety of patient, clinical, healthcare access characteristics. Our findings were robust across univariate and multivariable comparisons and across different comparison groups, veteran, or nonveteran US general population. Finally, to our knowledge, this is the first study in US veterans with arthroplasty that provides a comprehensive assessment of ADL ability and healthcare utilization.
These findings have clinical implications for resource planning relating to utilization and, as such, might be an appropriate target group for improved or preventive care management. Occupational therapy alternatives and greater availability of rehabilitative services and aids are two potentially simple and achievable management interventions that may alleviate the functional limitations of this vulnerable, and likely expanding, population.
Key messages.
Higher adjusted ADL limitation in veterans with arthroplasty compared to age-matched US cohorts identifies a group with high disability.
Veterans with arthroplasty have higher surgery clinic utilization compared to veterans without arthroplasty.
Veterans with arthroplasty also have higher inpatient utilization, which may be due to more severe comorbidity.
Acknowledgments
Supported by NIH CTSA Award 1 KL2 RR024151-01 (Mayo Clinic Center for Clinical and Translational Research)
Footnotes
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Contributor Information
Jasvinder A. Singh, Email: Jasvinder.md@gmail.com, Rheumatology Section, Medicine Service, VA Medical Center, One Veteran’s Drive, Minneapolis, MN 55417, USA, Departments of Orthopaedic Surgery and Health Sciences, Mayo Clinic College of Medicine, Rochester, MN, USA. Division of Rheumatology, Department of Medicine, University of Minnesota, Minneapolis, MN, USA
Jeffrey Sloan, Biostatistics, Mayo Clinic School of Medicine, Rochester, MN, USA.
References
- 1.Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement. A meta-analysis. Jama. 1994;271(17):1349–1357. [PubMed] [Google Scholar]
- 2.Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A(5):963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Hakkinen A, Ylinen J, Rinta-Keturi M, Talvitie U, Kautiainen H, Rissanen A. Decreased neck muscle strength is highly associated with pain in cervical dystonia patients treated with botulinum toxin injections. Arch Phys Med Rehabil. 2004;85(10):1684–1688. doi: 10.1016/j.apmr.2003.12.039. [DOI] [PubMed] [Google Scholar]
- 4.Kazis LE, Miller DR, Clark J, Skinner K, Lee A, Rogers W, et al. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998;158(6):626–632. doi: 10.1001/archinte.158.6.626. [DOI] [PubMed] [Google Scholar]
- 5.Kou B, Perner K, Yuan Y. Primary Zweymuller total hip arthroplasty for osteoarthritis secondary to congenital acetabular dysplasia. Zhonghua Wai Ke Za Zhi. 2001;39(8):623–625. [PubMed] [Google Scholar]
- 6.Wells V, Hearn T, Heard A, Lange K, Rankin W, Graves S. Incidence and outcomes of knee and hip joint replacement in veterans and civilians. ANZ J Surg. 2006;76(5):295–299. doi: 10.1111/j.1445-2197.2006.03716.x. [DOI] [PubMed] [Google Scholar]
- 7.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 8.Antoniou J, Martineau PA, Filion KB, Haider S, Zukor DJ, Huk OL, et al. In-hospital cost of total hip arthroplasty in Canada and the United States. J Bone Joint Surg Am. 2004;86-A(11):2435–2439. doi: 10.2106/00004623-200411000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The functional outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2005;87 (8):1719–1724. doi: 10.2106/JBJS.D.02714. [DOI] [PubMed] [Google Scholar]
- 10.Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. Health related quality of life outcomes after total hip and knee arthroplasties in a community based population. J Rheumatol. 2000;27(7):1745–1752. [PubMed] [Google Scholar]
- 11.Linsell L, Dawson J, Zondervan K, Rose P, Carr A, Randall T, et al. Pain and overall health status in older people with hip and knee replacement: a population perspective. J Public Health (Oxf) 2006;28(3):267–273. doi: 10.1093/pubmed/fdl020. [DOI] [PubMed] [Google Scholar]
- 12.Heck DA, Maar DC, Lowdermilk GA, Kalasinski LA, Mesko JW. Comparative analysis of total knee arthroplasty in two health care delivery systems. J Arthroplasty. 1992;7(1):93–100. doi: 10.1016/0883-5403(92)90038-r. [DOI] [PubMed] [Google Scholar]
- 13.Brander VA, Stulberg SD, Adams AD, Harden RN, Bruehl S, Stanos SP, et al. Predicting total knee replacement pain: a prospective, observational study. Clin Orthop Relat Res. 2003;416:27–36. doi: 10.1097/01.blo.0000092983.12414.e9. [DOI] [PubMed] [Google Scholar]
- 14.Elson DW, Brenkel IJ. Predicting pain after total knee arthroplasty. J Arthroplasty. 2006;21(7):1047–1053. doi: 10.1016/j.arth.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 15.Lingard EA, Katz JN, Wright EA, Sledge CB. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004;86-A:10–2186. doi: 10.2106/00004623-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252–3257. doi: 10.1001/archinte.160.21.3252. [DOI] [PubMed] [Google Scholar]
- 17.Weaver F, Hynes D, Hopkinson W, Wixson R, Khuri S, Daley J, et al. Preoperative risks and outcomes of hip and knee arthroplasty in the Veterans Health Administration. J Arthroplasty. 2003;18(6):693–708. doi: 10.1016/s0883-5403(03)00259-6. [DOI] [PubMed] [Google Scholar]
- 18.Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42(8):1722–1728. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 19.Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch Intern Med. 2001;161(3):454–460. doi: 10.1001/archinte.161.3.454. [DOI] [PubMed] [Google Scholar]
- 20.MacWilliam CH, Yood MU, Verner JJ, McCarthy BD, Ward RE. Patient-related risk factors that predict poor outcome after total hip replacement. Health Serv Res. 1996;31(5):623–638. [PMC free article] [PubMed] [Google Scholar]
- 21.Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: quality, value, accountability, and information as transforming strategies for patient-centered care. Am J Manag Care. 2004;10(11 Pt 2):828–836. [PubMed] [Google Scholar]
- 22.Fleming C, Fisher ES, Chang CH, Bubolz TA, Malenka DJ. Studying outcomes and hospital utilization in the elderly. The advantages of a merged data base for Medicare and Veterans Affairs hospitals. Med Care. 1992;30(5):377–391. doi: 10.1097/00005650-199205000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Singh JA, Sloan JA. Health-related quality of life in veterans with prevalent total knee arthroplasty and total hip arthroplasty. Rheumatology (Oxford) 2008;47(12):1826–1831. doi: 10.1093/rheumatology/ken381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singh JA, Borowsky SJ, Nugent S, Murdoch M, Zhao Y, Nelson DB, et al. Health-related quality of life, functional impairment, and healthcare utilization by veterans: veterans’ quality of life study. J Am Geriatr Soc. 2005;53(1):108–113. doi: 10.1111/j.1532-5415.2005.53020.x. [DOI] [PubMed] [Google Scholar]
- 25.Katz S, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in aged: The index of ADL: A standard measure of biological and psychological function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 26.Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, Chang RW. Risk factors for functional decline in older adults with arthritis. Arthritis Rheum. 2005;52(4):1274–1282. doi: 10.1002/art.20968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamman RF, Mulgrew CL, Baxter J, Shetterly SM, Swenson C, Morgenstern NE. Methods and prevalence of ADL limitations in Hispanic and non-Hispanic white subjects in rural Colorado: the San Luis Valley Health and Aging Study. Ann Epidemiol. 1999;9(4):225–235. doi: 10.1016/s1047-2797(98)00036-2. [DOI] [PubMed] [Google Scholar]
- 28.Dunlop DD, Manheim LM, Sohn MW, Liu X, Chang RW. Incidence of functional limitation in older adults: the impact of gender, race, and chronic conditions. Arch Phys Med Rehabil. 2002;83 (7):964–971. doi: 10.1053/apmr.2002.32817. [DOI] [PubMed] [Google Scholar]
- 29.Kashner TM. Agreement between administrative files and written medical records: a case of the Department of Veterans Affairs. Med Care. 1998;36(9):1324–1336. doi: 10.1097/00005650-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Szeto HC, Coleman RK, Gholami P, Hoffman BB, Goldstein MK. Accuracy of computerized outpatient diagnoses in a Veterans Affairs general medicine clinic. Am J Manag Care. 2002;8 (1):37–43. [PubMed] [Google Scholar]
- 31.Weidner C, Klede M, Rukwied R, Lischetzki G, Neisius U, Skov PS, et al. Acute effects of substance P and calcitonin gene-related peptide in human skin–a microdialysis study. J Invest Dermatol. 2000;115(6):1015–1020. doi: 10.1046/j.1523-1747.2000.00142.x. [DOI] [PubMed] [Google Scholar]
- 32.Mor V, Wilcox V, Rakowski W, Hiris J. Functional transitions among the elderly: patterns, predictors, and related hospital use. Am J Public Health. 1994;84(8):1274–1280. doi: 10.2105/ajph.84.8.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stump TE, Dexter PR, Tierney WM, Wolinsky FD. Measuring patient satisfaction with physicians among older and diseased adults in a primary care municipal outpatient setting. An examination of three instruments. Med Care. 1995;33(9):958–972. [PubMed] [Google Scholar]
- 34.Severson MA, Smith GE, Tangalos EG, Petersen RC, Kokmen E, Ivnik RJ, et al. Patterns and predictors of institutionalization in community-based dementia patients. J Am Geriatr Soc. 1994;42 (2):181–185. doi: 10.1111/j.1532-5415.1994.tb04949.x. [DOI] [PubMed] [Google Scholar]
- 35.Keller BK, Potter JF. Predictors of mortality in outpatient geriatric evaluation and management clinic patients. J Gerontol. 1994;49 (6):M246–M251. doi: 10.1093/geronj/49.6.m246. [DOI] [PubMed] [Google Scholar]
- 36.Reuben DB, Rubenstein LV, Hirsch SH, Hays RD. Value of functional status as a predictor of mortality: results of a prospective study. Am J Med. 1992;93(6):663–669. doi: 10.1016/0002-9343(92)90200-u. [DOI] [PubMed] [Google Scholar]