Abstract
CD4 T cells are principal producers of IL-21 and are often required for optimal CD8 T cell responses. Therefore, we investigated the importance of IL-21 in determining the phenotypic attributes, functional quality, and maintenance of anti-viral CD8 T cells following acute infection with the prototypic mouse pathogen lymphocytic choriomeningitis virus (LCMV). Previous reports have documented an obligatory role for IL-21 in sustaining CD8 T cell responses during chronic infections. Here we show that the requirements for IL-21 are less stringent following acute infections; however, in the absence of IL-21 the capacity of CD8 T cells to attain the polyfunctional trait of IL-2 production is consistently reduced during both the effector and memory phases. This is further supported by in vitro studies showing that the addition of IL-21 promotes the differentiation of IL-2 producing CD8 T cells. Although the generation of memory CD8 T cells, which are capable of mounting protective recall responses, proceeds independently of IL-21, we demonstrate that IL-21 does function to support secondary responses, especially under competitive conditions. Collectively, these studies highlight the potential roles of IL-21 in determining the quality of CD8 T cell responses following infection.
The quality and effectiveness of pathogen-specific CD8 T cells is shaped by many factors including the presence of CD4 T cell help and the availability of cytokines. Ideally, effector CD8 T cell responses are initially elicited which elaborate the necessary arrays of effector functions, such as cytokine production and cytotoxicity, required to clear infected cells. Typically, as homeostasis is restored following the control of the pathogen, a population of memory CD8 T cells emerge that is stably maintained over time (1–3). These memory T cells serve as sentinels and respond to protect the host if the original infection is reencountered.
CD8 T cell responses are diverse and exhibit a spectrum of functional activities. The ability of effector CD8 T cells to produce IL-2 has been partially associated with their ability to form the memory pool (4, 5). In addition, CD8 T cells that produce IL-2 are generally considered to be highly polyfunctional and can often simultaneously elaborate multiple effector activities, including the co-production of IFN-γ and TNF-α (6–8). The development of T cells that can functionally multi-task is notable as this has been correlated with a greater ability to control infections (7–12).
It is now well established that optimal CD8 T cell responses can be disrupted if the levels of CD4 T cell help is insufficient. Under these “helpless” conditions reduced primary CD8 T cell responses may be elicited and atypical memory responses are often observed (13–15). Without CD4 T cell help, the pseudomemory CD8 T cells may not be maintained at steady state levels, exhibit altered responsiveness to homeostatic cytokines, display a reduced portfolio of effector functions including diminished IL-2 production, and fail to mount prominent secondary immune responses. During chronic infections the requirements for CD4 T cell help are even more stringent as under these conditions marked exhaustion of the CD8 T cell response can occur, which is characterized by the functional inactivation and subsequent deletion of the responding T cells (7, 8, 16–18).
IL-21 is a member of the common-γ chain family of cytokines, is mainly produced by CD4 T cells, and has a broad impact on the immune response (19, 20). IL-21 has been shown to limit the terminal differentiation of effector CD8 T cells, favoring the development of immature effector cells which are more effective at suppressing tumor growth (21). IL-21 has also been shown to suppress the development of T cell senescence, which is characterized by the loss of CD28 expression (22–24). In vitro studies indicate that IL-21 can act as a third signal, distinct from IFN-α and IL-12, to promote CD8 T cell effector functions (25). Recently, IL-21 has been implicated as a vital helper factor which supports CD8 T cell activities during chronic viral infections. In studies of HIV-1 infected individuals, the levels of IL-21 have been shown to positively correlate with CD4 T cell counts (26, 27). The highest amounts of IL-21 were detected in uninfected subjects and in long-term non-progressors. In the case of chronic lymphocytic choriomeningitis virus (LCMV) infections, IL-21 was shown to act directly on CD8 T cells to sustain their physical presence and functional capabilities (28–31). The absence of IL-21 resulted in severe CD8 T cell exhaustion and viral persistence, outcomes that parallel those observed in chronically infected CD4−/− mice.
Given that CD4 T cells are a principal source of IL-21 and that CD4 T cells are necessary for optimal anti-viral CD8 T cell responses, in this report we set out to determine how IL-21 influences the functional quality and memory attributes of CD8 T cells following an acute viral infection. We demonstrate that following acute LCMV infection effector and memory CD8 T cell responses develop independently of IL-21, but that IL-21 regulates the generation of IL-2-producing CD8 T cells. Although IL-21 deficiency has minimal effects on the formation of the memory pool, in the absence of IL-21 signaling secondary responses are compromised under competitive conditions.
Materials and Methods
Mice and infections
C57BL/6J (B6), B6.PL Thy1a/CyJ, B6.129S2-Cd4tm1Mak/J (CD4−/−), B6.SJL-PtprcaPepcb/BoyJ (CD45.1), B6.129S7-Rag1tm1Mom/J (RAG-1−/−) mice were purchased from Jackson Laboratory (Bar Harbor, ME). P14 TCR transgenic mice (P14) crossed onto a B6 background were originally kindly provided by Dr. R. Ahmed (Emory University, GA). B6;129S5-Il21tm1Lex (IL-21−/−) and B6;129S5-Il21rtm1Lex (IL-21R−/−) mice were obtained from the Mutant Mice Regional Resource Center (Davis, CA). IL-21−/− mice were crossed an additional 6, 10, or 12 generations onto the B6 background. IL-21R−/− mice (crossed an additional 4 generations onto the B6 background) were mated with P14 mice to generate IL-21R+/− and IL-21R−/− P14 TCR transgenics. The IL-21R−/− mice used for the bone marrow chimera studies were crossed 8 generations onto the B6 background. All mice were bred and maintained in fully accredited facilities at the University of Alabama at Birmingham. For acute infections, mice were infected by i.p. injection with 2×105 p.f.u. LCMV-Armstrong and with 2×106 p.f.u LCMV-Armstrong for rechallenge studies. In certain experiments LCMV primed mice were challenged by i.v. inoculation with 5×104−1×105 CFU recombinant Listeria monocytogenes expressing the LCMV GP33 and GP34 epitopes (rLM33), kindly provided by Dr. H. Shen (University of Pennsylvania, PA) (32).
Cell preparations
Splenocytes were prepared as previously described (6). Blood samples were collected into 4%(w/v) sodium citrate. Livers and lungs were isolated from mice that had been perfused with 20ml PBS. Livers were minced and incubated for 30 minutes with 2mg/mL of Collagenase D (Roche, Indianapolis IN) and 0.3mg/mL of DNase I (Sigma-Aldrich, St. Louis MO) in HBSS. Liver samples were then further disrupted by passage through a 70µm cell strainer. Lungs were disrupted into single cell suspension using fine wire mesh. Lymphocytes from the blood, liver, and lungs were subsequently isolated by centrifugation over a layer of Histopaque-1083 (Sigma-Aldrich, St. Louis MO).
Cellular analyses and flow cytometry
MHC tetramer staining and intracellular cytokine analyses were performed essentially as previously described (6). For the detection of IL-21, a two-step intracellular cytokine staining was performed by initially using recombinant IL-21R/Fc fusion proteins (0.1µg, R&D system, Minneapolis, MN) together with anti-IFN-γ FITC (XMG1.2) and anti-IL-2 APC (JES6-5H4) (eBioscience, San Diego, CA). After incubation, cells were washed with Perm-Wash buffer (BD, San Jose, CA) and stained with F(ab)2 PE-conjugated goat anti-human Fcγ (Jackson ImmunoResearch Laboratories, West Grove, PA) (33). Samples were acquired using FACSCalibur or LSR II flow cytometers (BD, San Jose, CA), and data was analyzed using FlowJo software (Tree Star, Ashland, OR).
In vitro cultures
Splenocytes from naïve P14 TCR transgenic mice were labeled with CFSE (Molecular Probes; Eugene, OR) and cultured in the presence of 1µg/mL GP33 (KAVYNFATM) peptide and combinations of recombinant IL-21 (50ng/mL, R&D systems, Minneapolis, MN) and IL-15 (50ng/mL, Invitrogen, Carlsbad, CA). In certain experiments, naïve (CD44lo), CD8+ T cells from IL-21R+/− and IL-21R−/− P14 TCR transgenic mice were isolated by cell sorting using a FACSAria instrument (BD, San Jose, CA). These sorted naïve CD8 T cells were labeled with CFSE and cultured together with irradiated (3000 rad) splenic feeder cells from B6.PL Thy1a/CyJ mice at a responder to feeder cell ratio of 1:5. The GP33 peptide was added to activate the responder cells, with and without the addition of IL-21, as described above. After ~5 days cultured splenocytes were re-stimulated with the GP33 peptide prior to intracellular cytokine staining.
Adoptive transfer of normalized numbers of memory CD8 T cells
Splenic CD8 T cells from LCMV primed IL-21+/+ and IL-21−/− mice (>150 days following infection) were isolated to >96% purity using mouse CD8 FlowComp Dynabeads (Invitrogen; Carlsbad, CA). The frequencies of LCMV Db(GP33)-specific CD8 T cells in the purified cell pools were then immediately determined by MHC tetramer staining. Subsequently, purified cell populations containing 5×104 Db(GP33)-specific CD8 T cells were transferred by i.p. injection into allelically marked (CD45.1) recipients. One day later recipient mice were challenged with rLM33 and the recall responses of the donor cells analyzed after 6 days.
Mixed bone marrow chimeras
Bone marrow was prepared from the tibias and femurs of control CD45.1 mice, and CD45.2 IL-21R+/+ and IL-21R−/− littermates (31). Bone marrow suspensions were depleted of T cells using anti-CD5 (Ly-1) microbeads (Miltenyi Biotec; Auburn, CA). Recipient RAG-1−/− mice were irradiated twice, 3–4 hours apart, to give a total exposure of ~1000 rads. These mice were then reconstituted by i.v. injection of T depleted bone marrow containing 5–7×106 IL-21R+/+ (CD45.1) cells mixed with equal numbers of IL-21R+/+ or IL-21R−/− (CD45.2) cells. Mice were maintained on chlorinated acidified water containing sulfamethoxazole, trimethoprim, and neomycin for 6 weeks. Chimeras were infected with LCMV-Armstrong ~8 weeks following reconstitution and subsequently rechallenged with LCMV >60 days post primary challenge.
Statistical analysis
Two-tailed t-tests were used to determine statistical significance between two groups, and a one-way ANOVA test was utilized to compare three groups. p values were calculated using Prism software (Graph Pad; La Jolla, CA).
Results
Reduced IL-2-producing primary CD8 T cell responses in the absence of IL-21
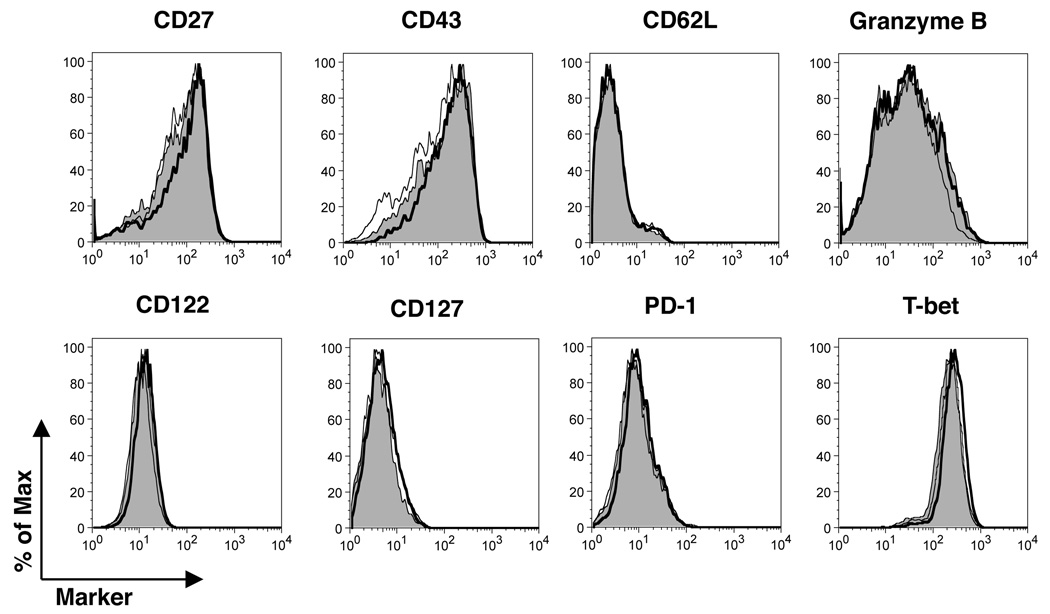
To evaluate the impact of IL-21 on the induction of anti-viral effector CD8 T cell responses during an acute viral infection, wild-type (IL-21+/+), IL-21 heterozygous (IL-21+/−), and IL-21-deficient (IL-21−/−) mice were infected with LCMV-Armstrong. As expected, by 8 days following infection, IL-21+/+ mice mounted a robust multi-epitope-specific CD8 T cell response (Fig. 1). IFN-γ production by virus-specific CD8 T cells was readily detected following a brief (5h) period of reactivation, and a subset of the responding cells displayed polyfunctional attributes as assessed by the co-production of IL-2 (Fig. 1A). By comparison with IL-21+/+ mice, the frequencies of IFN-γ+ CD8 T cells capable of producing IL-2 were reduced in IL-21+/− hosts and were even lower in IL-21−/− mice (Fig. 1, A–C). This decreased fraction of IL-2 competent effector CD8 T cells was also paralleled by a diminution in the mean-fluorescence-intensity (MFI) of IL-2 staining, indicating that the levels of IL-2 production are lower, on a per cell basis, in CD8 T cells derived from IL-21-deficient hosts (Fig. 1C). Evaluation of the overall size of the CD8 T cell pool and the numbers of MHC-tetramer binding virus-specific CD8 T cells showed no significant differences between IL-21+/+, IL-21+/− and IL-21−/− mice (Fig 1D). Enumeration of IL-2 and IFN-γ producing epitope-specific CD8 T cells revealed that the reduced percentage of IL-2 competent effector CD8 T cells was attributable to both a slight decrease in the absolute numbers of IL-2+ cells and also a modest increase in the numbers of IFN-γ+ CD8 T cells (Fig. 1E). Thus, qualitative and quantitative differences in the functionality of the virus-specific CD8 T cell response manifest in the absence of IL-21.
FIGURE 1.
Reduced IL-2-producing effector CD8 T cell responses in the absence of IL-21. IFN-γ and IL-2 production by CD8 T cells specific for four distinct viral epitopes were evaluated at 8 days following acute LCMV-Armstrong infection of IL-21+/+, IL-21+/−, IL-21−/− mice. A, Intracellular cytokine analysis for IFN-γ and IL-2 following stimulation with various antigenic peptides. Gated CD8 T cells are shown and the percentages of CD8+, IFN-γ+ cells that co-produce IL-2 are reported in parentheses. B, Composite data from individual mice showing the fraction of IFN-γ, IL-2-co-producing CD8 T cells specific for individual viral epitopes. C, The MFI of IL-2 staining by epitope-specific CD8 T cells from the various cohorts. D, The total numbers of CD8 T cells and viral-epitope-specific CD8 T cells were determined by flow cytometric analysis using a panel of MHC class I tetramers. E, Epitope-specific IFN-γ producing (black symbols) and IL-2 producing (white symbols) CD8 T cells were enumerated following intracellular cytokine analyses. Error bars are s.d. For B–E, statistical significance is represented by * p<0.05, ** p<0.01, *** p< 0.001. Results are shown from 4 independent experiments analyzing a total of 9–13 mice per group.
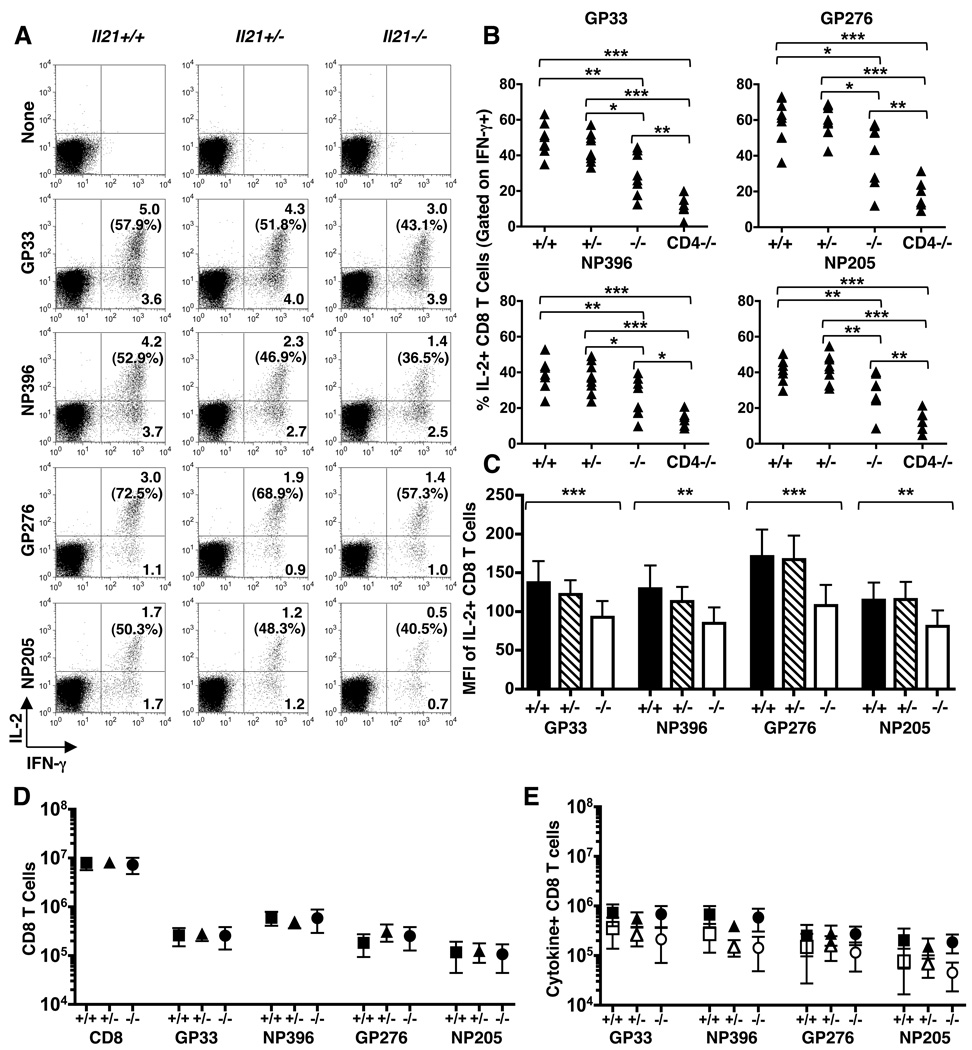
We investigated whether the functional shifts which occur in the absence of IL-21 were mirrored by other phenotypic alterations within the effector CD8 T cell pool. Analyses of the expression of a panel of molecules associated with the generation of effector CD8 T cells, including CD27, CD43, CD62L, CD122, CD127, PD-1, granzyme B, and T-bet, showed no marked differences between epitope-specific CD8 T cells induced in IL-21+/+, IL-21+/−, or IL-21−/− mice (Fig. 2). Thus, even though IL-21 selectively impacted the proportion of IL-2 producing CD8 T cells, other phenotypic attributes of the response were unaltered.
FIGURE 2.
Expression of phenotypic attributes associated with effector CD8 T cell generation is unaffected by IL-21. At 8 days following acute LCMV-Armstrong infection the expression of CD27, CD43, CD62L, CD122, CD127, PD-1, granzyme B and T-bet by LCMV- GP33-specific CD8 T cells from IL-21+/+ (shaded), IL-21+/− (thin line), and IL-21−/− (dark line) mice was determined by flow cytometry. Plots show gated GP33 tetramer+ CD8 T cells. Representative results from 4 independent experiments analyzing a total of 9–13 mice per group.
Generation of memory CD8 T cells in the absence of IL-21
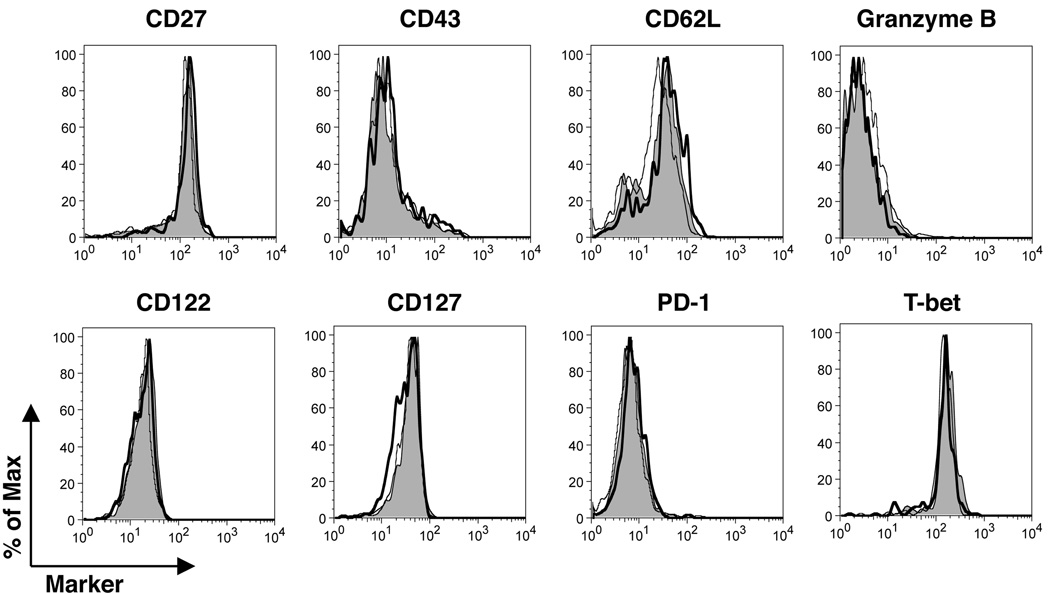
Since the loss of IL-21 negatively impacted the quality of the anti-viral CD8 T cell response during the effector phase of the response, we next checked whether differences in functional quality were maintained into the memory phase. By day 120 following acute LCMV infection, memory CD8 T cells capable of co-producing IFN-γ and IL-2 were readily detectable. Although, by comparison with the effector phase, the proportion of IL-2 producing CD8 T cells increased in IL-21+/+, IL-21+/−, and IL-21−/− mice, the fraction of IL-2-producing CD8 T cells was lower in the IL-21−/− mice compared to the IL-21+/+ mice (Fig. 3, A and B). Additionally, a significant reduction in the MFI of IL-2 production by CD8 T cells in the IL-21−/− cohort remained discernable at memory time points, paralleling the reductions observed during the effector phase (Fig. 3C cf. Fig. 1C). Despite this reduction in functional quality the numbers of virus-specific memory CD8 cells were similar in all of the groups, demonstrating that IL-21 is not required for the maintenance of these cells (Fig. 3, D and E). Further analyses of the phenotypic attributes of the virus-specific memory CD8 T cells revealed no marked differences between the IL-21+/+, IL-21+/−, and IL-21−/− cohorts (Fig. 4). Collectively, these data show that IL-21 deficiency does not inhibit memory CD8 T cell formation, and a distinct population of IL-2+ CD8 T cells does form; nevertheless, a reproducible decrease in the fraction of IL-2+ CD8 T cells in IL-21−/− mice is apparent during the memory phase of the response.
FIGURE 3.
Altered IL-2 production by CD8 T cells during the memory phase in IL-21−/− mice. IFN-γ and IL-2 production by CD8 T cells specific for four distinct viral epitopes were evaluated at days 120–273 following acute LCMV-Armstrong infection of IL-21+/+, IL-21+/−, IL-21−/− mice. A, Intracellular cytokine analysis for IFN-γ and IL-2 following stimulation with various antigenic peptides. Gated CD8 T cells are shown and the percentages of CD8+, IFN-γ+ cells that co-produce IL-2 are reported in parentheses. B, Composite data from individual mice showing the fraction of IFN-γ, IL-2-co-producing CD8 T cells specific for individual viral epitopes. C, The MFI of IL-2 staining by epitope-specific CD8 T cells from the various cohorts. D, The total numbers of CD8 T cells and viral-epitope-specific CD8 T cells were determined by flow cytometric analysis using a panel of MHC class I tetramers. E, Epitope-specific IFN-γ producing (black symbols) and IL-2 producing (white symbols) CD8 T cells were enumerated following intracellular cytokine analyses. Error bars are s.d. For B and C, statistical significance is represented by * p<0.05, **p<0.01 and ***p<0.001. Results are shown from 3 independent experiments analyzing a total of 6–9 mice per group.
FIGURE 4.
Expression of phenotypic attributes associated with memory CD8 T cell generation is unaffected by IL-21. At 120 days following acute LCMV-Armstrong infection the expression of CD27, CD43, CD62L, CD122, CD127, PD-1, and T-bet by LCMV GP33-specific CD8 T cells from IL-21+/+ (shaded), IL-21+/− (thin line), and IL-21−/− (dark line) mice was determined by flow cytometric analysis. Granzyme B levels were measured at day 44 following acute LCMV-Armstrong infection. Plots show gated GP33 tetramer+ CD8 T cells. Representative results from 2–3 independent experiments are shown for a total of 6–9 mice analyzed per group.
CD8 T cells in the liver, lungs, and circulation
It has been proposed that the inability to produce IL-2 affects the accumulation of virus-specific CD8 T cells in extralymphoid organs (34). Therefore, we compared the frequencies of IFN-γ and IL-2 producing virus-specific CD8 T cells in the liver, lungs, and circulation at days 9 (Fig. 5A and B) and 32 (Fig. 5C and D) following infection. At 9 days post infection comparable frequencies of IFN-γ+ CD8 T cells were detectable in IL-21+/+ and IL-21−/− mice following stimulation with the GP33 peptide (Fig. 5A). Consistent with the splenic analyses (Fig. 1), the fraction of the IFN-γ+ CD8 T cells capable of producing IL-2 were reduced in all of the compartments analysed in IL-21−/− mice (Fig 5, A and B). By day 32 following infection, the proportion of IL-2+ CD8 T cells had increased compared to the effector timepoint. Nevertheless, by comparison with IL-21+/+ mice, the IL-21−/− mice continued to exhibited a decrease in the frequency of IL-2 producing CD8 T cells (Fig 5, C and D). Thus, IL-21 deficiency impacts the ability of CD8 T cells to produce IL-2 in both lymphoid and non-lymphoid organs.
FIGURE 5.
Reduced frequencies of IL-2-producing CD8 T cells in the liver, lungs and circulation of IL-21−/− mice. IFN-γ and IL-2 production by LCMV-specific CD8 T cells in the liver, lungs, and blood were evaluated at day 9 (A–B) and at day 32 (C–D) following acute LCMV-Armstrong infection of IL-21+/+ and IL-21−/− mice. A and C, Intracellular cytokine analysis for IFN-γ and IL-2 following stimulation with the GP33 peptide epitope. The values represent the percentage of gated CD8 T cells present in each quadrant. B and D, Bar graphs show the fraction of virus-specific, IFN-γ producing, CD8 T cells which co-produce IL-2 in IL-21+/+ (black bars) and IL-21−/− (white bars) mice. Error bars are s.d. For B and D, statistical significance is represented by *p<0.05, **p<0.01, ***p<0.001. Representative or composite results are from two independent experiments at each timepoint analyzing a total of 8 mice per group.
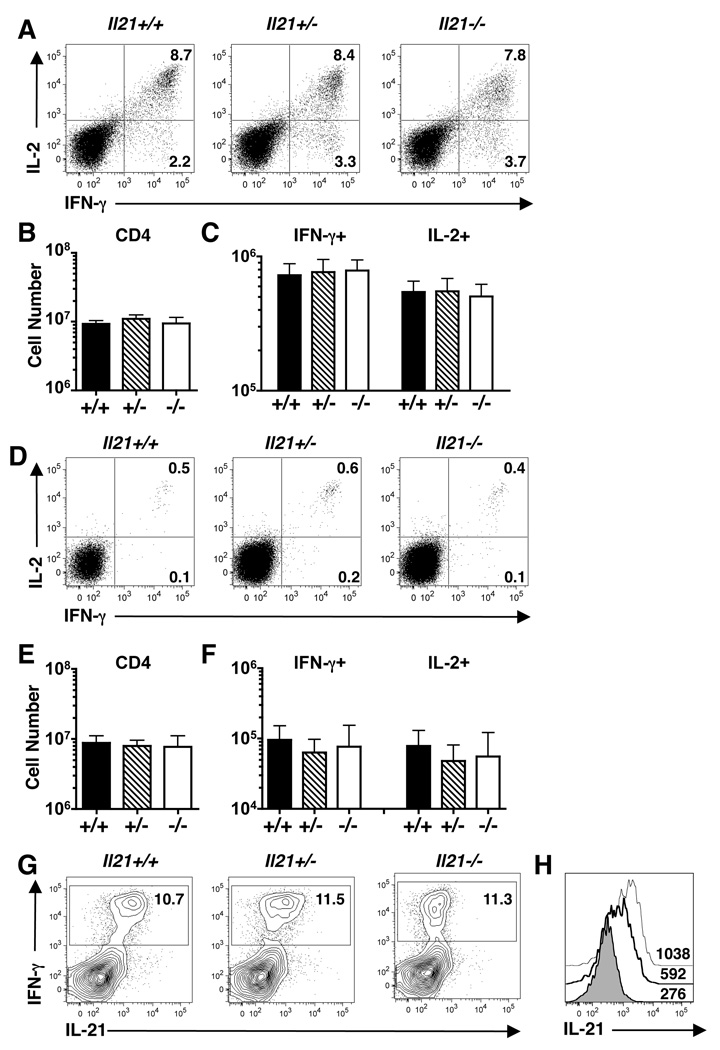
CD4 T cell responses in the absence of IL-21
CD4 T cells assist in the generation of optimal CD8 T cell responses following acute infections (13–15). Therefore, we next inspected whether the functional defects apparent in the CD8 T cell response in IL-21−/− mice were associated with altered CD4 T cell responses. Analysis at effector (day 8) (Fig. 6, A–C) and memory (≥ day 120) (Fig.6, D–F) time points revealed no marked differences in the overall virus-specific CD4 T cell response in the absence of IL-21. Thus, the altered CD8 T cell response observed in IL-21−/− mice is unlikely to be due to the failure to induce an anti-viral CD4 T cell response.
FIGURE 6.
Th1-associated virus-specific CD4 T cell responses are IL-21 independent. CD4 T cell responses were evaluated at 8 days (A–C and G–H) and at days 120–273 (D–F) following acute (LCMV-Armstrong) infection. A and D, The production of IFN-γ and IL-2 was determined by intracellular cytokine staining following a brief period of stimulation with the GP61 peptide epitope. The values represent the percentage of gated CD4 T cells present in each quadrant. B and E, Enumeration of total splenic CD4 T cells, and (C and F) IFN-γ+ and IL-2+ GP61-specific CD4 T cells, following infection of IL-21+/+ (black bars), IL-21+/− (striped bars), IL-21−/− (white bars) mice. G, IL-21 and IFN-γ production by GP61-specific CD4 T cells and (H) histograms depicting the MFI of IL-21 staining on gated IFN-γ+ CD4 T cells following GP61 peptide stimulation from a representative IL-21+/+ (thin line), IL-21+/− (dark line), IL-21−/− (shaded) mouse. Mean values ± s.d are shown from 3–4 independent experiments analyzing a total of 6–13 mice per group.
Comparative analyses of CD8 T cells consistently shows the most pronounced IL-2+ response in IL-21+/+ mice, an intermediate response in IL-21+/− mice, and the lowest response in IL-21−/− mice (Figs. 1 and 3). We predicted that these changes in the quality of CD8 T cell responses would be paralleled by decreases in the levels of IL-21 production by the virus-specific CD4 T cells. Therefore, we measured the ability of anti-viral CD4 T cells from each group of mice to produce IL-21 following stimulation with the LCMV GP61–80 peptide epitope. IL-21 production was clearly discernable by CD4 T cells from IL-21+/+ mice, with intermediate levels produced by IL-21+/− CD4 T cells and, as expected, was not synthesized by IL-21−/− CD4 T cells (Fig. 6, G and H).
IL-21 promotes the generation of IL-2+ CD8 T cells
The results showing that the generation of IL-2 producing anti-viral CD8 T cells was reduced without IL-21 prompted us to determine whether the addition of IL-21 enhanced the functional quality of CD8 T cells. In a series of in vitro studies, CD8 T cells from P14 TCR transgenic mice, which are specific for the LCMV GP33 epitope, were activated by addition of the cognate GP33 peptide and co-cultured with combinations of IL-15 and IL-21. To determine whether the functional attributes of the responses were altered by the addition of IL-21, intracellular cytokine analyses for IL-2 (Fig. 7A) and IFN-γ (Fig. 7B) were performed. After 18 hours of culture no pronounced differences in the fraction of IL-2 producing CD8 T cells were observed (data not shown). By ~5 days of culture, the responding cells had undergone 6–8 divisions, and notably, initial activation in the presence of exogenous IL-21 increased the fraction of IL-2 producing CD8 T cells (11.8±4.9%) compared to cells cultured without cytokine (4.6±3.1%; p=0.0245) (Fig. 7A). Examination of the impact of IL-21 on IFN-γ production showed no significant differences between the IL-21 cultured cells (21.9±10.5%) and cells cultured without the addition of IL-21 (18.1±7.2; p=0.5293) (Fig. 7B).
FIGURE 7.
IL-21 promotes IL-2+ CD8 T cell generation in vitro. A and B, CFSE labeled splenocytes from naïve P14 (LCMV-specific) TCR transgenic mice were activated in vitro with GP33 peptide and co-cultured with: IL-15, IL-21, or IL-21 together with IL-15. C–F, Sorted naïve (CD44lo) CD8 T cells from IL-21R+/− [(C) and (E)] or IL-21R−/− [(D) and (F)] P14 TCR transgenic mice were CFSE labeled and co-cultured together with GP33 peptide and irradiated feeder cells in the absence or presence of exogenous IL-21. After ~5 days of culture, responder cells were briefly restimulated and the production of cytokines by CD8 T cells analyzed by intracellular cytokine staining. The percentage of gated CD8 T cells which produce the indicated cytokines are reported. For each series of studies representative results from three independent experiments are shown.
We next examined whether IL-21 was acting directly on the responding CD8 T cells to configure their functional traits (Fig. 7, C–F). Naïve (CD44lo) CD8 T cells sorted from P14 TCR transgenic IL-21 receptor-deficient (IL-21R−/−) and IL-21R+/− mice were similarly activated in vitro using the GP33 peptide, with and without the addition of IL-21. After ~5 days, culture in the presence of IL-21 increased the proportion of IL-2 producing IL-21R+/− CD8 T cells but did not augment the responses of IL-21R−/− CD8 T cells (Fig. 7, C and D). Since IL-21 has been proposed to influence the induction of IL-17 producing T cells, we also checked whether antigen-activated CD8 T cells exposed to IL-21 gained the ability to produce IL-17 (Fig. 7, E and F) (33, 35). No significant fraction of IL-17+ CD8 T cells were detectable following the culture period. These in vitro studies indicate that IL-21 acts directly on CD8 T cells to influence their differentiation and acquisition of functional traits.
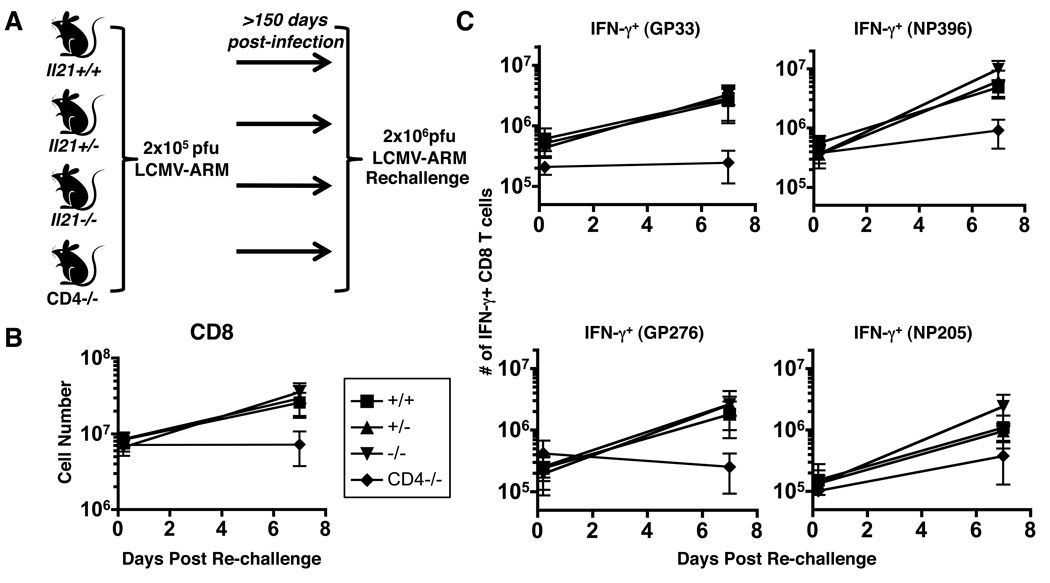
CD8 T cells primed in the absence of IL-21 mount recall responses
Since functional discrepancies were detected in anti-viral CD8 T cells generated in the presence or absence of IL-21, we next evaluated whether these “IL-21-less” memory CD8 T cells could elicit secondary recall responses. In an initial series of studies IL-21+/+, IL-21+/−, IL-21−/−, and CD4−/− mice, which had been infected with LCMV-Armstrong at least 150 days earlier, were rechallenged with a high dose of LCMV (Fig. 8A). As shown previously, CD8 T cells primed in CD4−/− mice mount severely blunted recall responses (13–15), as demonstrated by the minimal increase in the numbers of total CD8 T cells present in the spleen at 7 days post-rechallenge (Fig 8B). By contrast, the absence of IL-21 had no effect on the overall magnitude of the CD8 T cell response, as similar secondary responses were detected in IL-21+/+, IL-21+/−, and IL-21−/− mice (Fig. 8B). Further evaluation of viral-epitope-specific CD8 T cells confirmed that secondary CD8 T cell responses are impaired in CD4−/− hosts but are unaffected by the absence of IL-21 (Fig. 8C). Thus, the requirements for CD4 T cell help in generating memory CD8 T cells that can mount robust recall responses is far more stringent than the specific requirement for IL-21.
FIGURE 8.
Intact secondary CD8 T cell responses in the absence of IL-21. IL-21+/+ (squares), IL-21+/− (triangles), IL-21−/− (inverted triangles), and CD4−/− (diamonds) mice, which had undergone primary acute LCMV infection at least 150 days previously, were rechallenged and secondary responses analyzed 7 days later. A, Schematic of the experimental set-up. B, The number of total splenic CD8 T cells and (C) the number IFN-γ producing virus-specific CD8 T cells were determined by intracellular cytokine staining following peptide stimulation. The number of cells at day 0 represents the mean value in control cohorts that were not given a secondary challenge. Mean values ± s.d are shown for four independent experiments analyzing a total of 9–12 per group.
To further evaluate recall responses we performed a series of adoptive transfer studies. Normalized numbers (5×104) of memory LCMV GP33-epitope specific CD8 T cells from IL-21+/+ and IL-21−/− mice were transferred into congenic, allelically marked, naïve CD45.1 recipient mice (Fig. 9A). Subsequently, the recall potential of these donor populations was compared following challenge of the recipients with recombinant Listeria monocytogenes expressing the LCMV GP33/GP34 epitopes (rLM33) (32). Both IL-21+/+ and IL-21−/− donor CD8 T cells were readily detectable by 6 days following rLM33 challenge (Fig. 9B). Similar numbers of IFN-γ producing GP33/GP34-specific donor cells were present in both groups of recipients; however, the number of IL-2 producing IL-21−/− donor cells was lower, which is consistent with the impaired functional CD8 T cells responses detected at acute and memory timepoints (Fig. 9C cf. Fig 1 and 3). Analysis of the endogenous listeriolysin O (LLO)-specific CD4 T cell responses in the recipient mice demonstrated the presence of IL-21 producing CD4 T cells (Fig. 9E). Nevertheless, this production of IL-21 did not enable the memory CD8 T cells generated in the absence of IL-21 to recover their ability to produce IL-2 and match the functional responsiveness of IL-21+/+ memory CD8 T cells.
FIGURE 9.
Diminished IL-2 production by memory IL-21−/− CD8 T cells following adoptive transfer. Populations of purified CD8 T cells normalized to contain 5×104 Db(GP33)-specific memory IL-21+/+ or IL-21−/− CD8 T cells were transferred into CD45.1 mice and splenic secondary responses in the recipients were analyzed 6 days following rLM33 challenge. A, Schematic of the experimental set-up. B, Detection of IFN-γ production by donor (CD45.2+) and endogenous (CD45.2−) CD8 T cells following GP33 peptide stimulation. Gated CD8 T cells are shown and the values represent the percentages of CD8 T cells present within the indicated regions. C, Enumeration of IFN-γ and IL-2 producing donor memory CD8 T cells. D, The recoveries of donor GP33 and GP34 tetramer+ CD8 T cells from the challenged mice (IL-21+/+ donor cells: black bars; IL-21−/− donor cells: white bars). E, The production of IL-21 by the recipient LLO-specific CD4 T cells (bold line and thin line: the endogenous CD4 T cell response in the recipients receiving donor CD8 T cells from IL-21+/+ and IL-21−/− mice, respectively; the shaded line shows the control staining profile using α-Fc PE only. For C and D, statistical significance is represented by * p<0.05 and **p<0.01. Results are shown from 3 independent experiments analyzing a total of 5–16 mice per group.
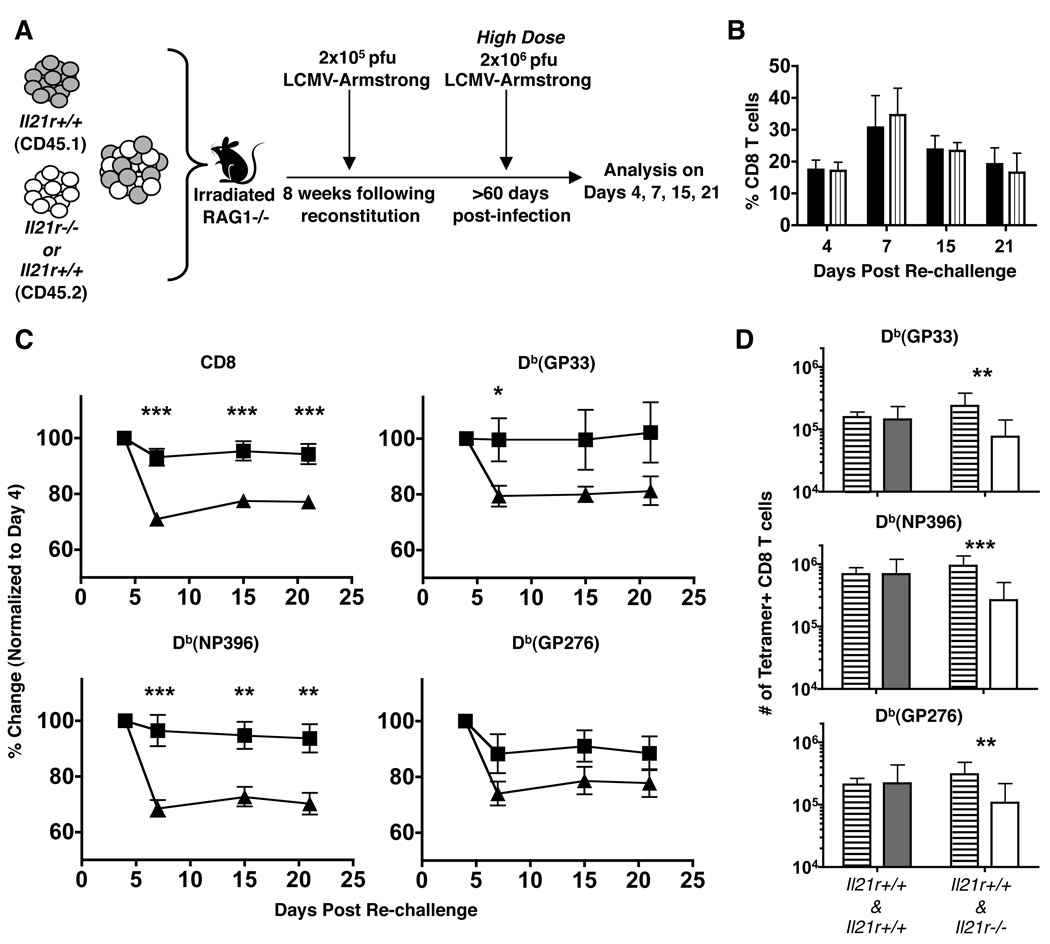
IL-21 helps recall CD8 T cell responses under competitive conditions
To provide a more stringent readout of the potential roles of IL-21 in helping recall CD8 T cell responses we directly compared the secondary responses of IL-21R+/+ and IL-21R−/− memory CD8 T cells in the same host. To accomplish this a series of chimeras were generated by reconstituting lethally irradiated RAG-1−/− mice with a mixture of allelically distinguishable bone marrow from IL-21R+/+ and IL-21R−/− mice. In this way the recipient mice are reconstituted with populations of CD8 T cells which could (IL-21R+/+) and could not (IL-21R−/−) perceive IL-21 signals. For control purposes we also generated mixed chimeras using two populations of allelically marked IL-21R+/+ cells. The reconstitution efficiency was checked 6 weeks following transfer, and the chimeric mice were primed by LCMV-Armstrong infection at 8 weeks post-transfer. To determine whether IL-21 is required for optimal recall responses, the mixed chimeras were rechallenged with a high dose of LCMV-Armstrong after at least 60 days following the primary acute infection (Fig. 10A). Collectively, in the control chimeras, the median percentage of IL-21R+/+ (CD45.2) CD8 T cells prior to rechallenge was 44.3 with a range of 29.2–65. By comparison, in the experimental cohorts the median percentage of IL-21R−/− (CD45.2) CD8 T cells was 41.45 with a range of 24–49.4.
FIGURE 10.
A requirement for IL-21 during secondary CD8 T cell responses under competitive conditions. Mixed bone marrow chimeras were generated using combinations of IL-21R+/+ and IL-21R−/− cells or IL-21R+/+ and IL-21R+/+ cells as controls. Chimeras were rechallenged with LCMV at least 60 days following primary infection. Recall responses were subsequently analyzed. A, Schematic of the experimental set-up. B, The percentages of total CD8 T cells in the circulation at various times following secondary challenge of the control (IL-21R+/+ | IL-21R+/+) (black bars) and experimental (IL-21R+/+ | IL-21R−/−) chimeras (vertically striped bars). C, The fraction of CD45.2 IL-21R+/+ CD8 T cells in the control chimeras (squares) and of CD45.2 IL-21R−/− in the experimental chimeras (triangles) were evaluated in the circulation over time following secondary challenge. The proportion of total and epitope-specific CD8 T cells were normalized (100%) to the recovery at day 4 following rechallenge. D, Enumeration of splenic virus-specific CD8 T cells in the control and experimental chimeras at day 21 after secondary challenge. CD45.1 (IL-21R+/+): horizontal striped bars. CD45.2 (IL-21R+/+) in the control chimeras: gray bars. CD45.2 (IL-21R−/−) in the experimental chimeras: white bars. Statistical significance is represented by * p<0.05, **p<0.01 and ***p<0.001; error bars are s.e.m. Results are shown from 4 experiments analyzing a total of 12–18 mice per group.
Analysis of the blood on days 4, 7, 15, and 21 following secondary challenge showed similar overall CD8 T cell levels in the control and experimental chimeras (Fig. 10B). Comparison of the IL-21R+/+ and IL-21R−/− CD8 T cells did, however, reveal a selective defect in the recall responses of IL-21R−/− CD8 T cells (Fig. 10C). The recoveries of total and viral-epitope-specific CD45.2 IL-21R+/+ CD8 T cells in the control cohorts (Fig. 10C, squares), as well as the fraction of total and viral epitope-specific CD45.2 IL-21R−/− CD8 T cells in the experimental cohorts (Fig. 10C, triangles) were normalized to 100% at day 4 following rechallenge. By day 7 following challenge, the proportion of the IL-21R−/− CD8 T cells clearly dropped in the experimental cohort. This impediment of the IL-21R−/− CD8 T cells is most dramatic for the NP396-specific response, which typically dominates following a secondary challenge with LCMV (36, 37). Enumeration of the virus-specific CD8 T cells in the spleen at day 21 following a secondary challenge shows similar magnitudes of CD45.1 IL-21R+/+ and CD45.2 IL-21R+/+ CD8 T cells in the control chimeras (Fig. 10D). In the experimental groups the numbers of GP33, NP396, and GP276-specific IL-21R−/− CD8 T cells were significantly lower than their IL-21R+/+ counterparts, mirroring the findings from the blood analyses (Fig. 10D cf. 10B). Thus, the IL-21R−/− virus-specific memory CD8 T cells mount a less vigorous recall response and are outcompeted by their IL-21R+/+ counterparts in this mixed environment.
Discussion
CD4 T cells have been proposed to help CD8 T cell responses in several ways, including by the licensing of dendritic cells, the production of chemokines and cytokines which promote T cell migration to the sites of priming and areas of infection, and by the secretion of cytokines such as IL-2 and IL-21 (28, 29, 31, 38–43). Previous studies have emphasized the critical role of IL-21 in supporting CD8 T cell responses in the context of chronic viral infections (28, 29, 31). In this report we demonstrate that IL-21 has a subtle but significant role in structuring the functional attributes of anti-viral CD8 T cells in acutely infected hosts as well as a potential impact on recall responses, especially under competitive conditions.
As naïve CD8 T cells become initially activated, a burst of IL-2 synthesis is induced which subsides as the primed cells proliferate and differentiate into effector T cells (44, 45). During the effector phase only a fraction of the antigen-specific CD8 T cells are capable of producing IL-2 (7, 8) (Figs. 1 and 3). The ability of the effector CD8 T cells to produce IL-2 tends to be associated with a preferential ability to form the memory CD8 T cell pool; however, clearly not all memory T cells are competent at producing IL-2 following antigenic activation. The emergence of effector and memory CD8 T cells following acute infections has been reported to occur independently of IL-21, which is generally consistent with our observations (28, 29). Nevertheless, we now show that IL-21 appears to shape the functional quality of effector and memory CD8 T cells which do develop, as our analyses of IL-21−/− mice demonstrate a selective impairment in the ability of anti-viral CD8 T cells, primed by acute LCMV infection, to produce IL-2. Additionally, in vitro priming studies further show that elevating the levels of IL-21 favors the development of IL-2 producing CD8 T cells, and these effects are predominately mediated by the direct actions of IL-21 on the responding T cells.
IL-21 has the potential to regulate IL-2 synthesis in CD8 T cells at several levels including by epigenetic changes, by direct effects on master transcriptional regulators, and by an overall skewing of T cell differentiation. IL-2 and IL-21 are closely genetically linked and in mice these genes are encoded 98 Kb apart on chromosome 3 (46). This tight association may influence expression as chromatin remodeling at one locus may have regional effects on gene accessibility and activation. The transcription factor Blimp-1 (Prdm1) is a negative regulator of IL-2 production. Blimp-1 deficiency during viral infections results in increased levels of IL-2 producing CD8 T cells and favors the differentiation of KLRG-1loIL-7hi memory precursor/memory T cells (47–51). It is well documented that IL-21 induces Blimp-1 expression in B cells, and more recent results show that IL-21 also induces the expression of this transcription factor in antigen activated CD8 T cells (52, 53). Nevertheless, Blimp-1 induction in T cells is associated with downregulation of IL-2. Consequently, the lower IL-2+ CD8 T cell response in IL-21−/− mice cannot be due to IL-21 induced increases in Blimp-1 levels. In B cells and CD4 T cells IL-21 has also been shown to drive the expression of Bcl-6, which can act antagonistically on Blimp-1 (54–57). Thus, it is plausible that one way in which IL-21 dictates the expression of IL-2 by CD8 T cells is in part by shifting the balance of Blimp-1 and Bcl-6 expression.
Several studies have now implicated exogenous IL-2 in inducing CD25 expression on CD8 T cells and driving the development of activated effector cells which are less competent at producing their own IL-2 and forming the memory compartment (44, 58, 59). IL-21 has also been shown to skew the differentiation of naive CD8 T cells, but the outcomes are distinct from those observed following IL-2 exposure. Activation of CD8 T cells in the presence of IL-21 allows the responding cells to attain an immature effector-like phenotype (21), and as illustrated in figure 7, IL-21 favors the development of IL-2 competent CD8 T cells. Thus, IL-21 may arrest the development and terminal differentiation of potent effector CD8 T cells and instead may favor the generation of T cell subsets which are more likely to be maintained over time. The potential role of IL-21 in promoting CD8 T cell responses which are sustainable is further supported by studies showing that CD8 T cells activated in the presence of IL-21 are more effective at eradicating tumors in vivo, and that IL-21 deficiency can result in severe T cell exhaustion and loss of anti-viral CD8 T cells in chronically infected hosts (21, 28, 29, 31).
Our findings indicate that IL-21 can influence the developmental fate of responding CD8 T cells and one signature of this may be enhanced IL-2 expression. Notably, in the absence of IL-21, virus-specific CD8 T cells from all compartments examined, including the spleen, liver, lungs, and circulation, show a decreased intrinsic ability to produce IL-2. This reduction in IL-2 production is more pronounced during the effector phase than at memory timepoints. Thus, IL-21 deficiency does not preclude memory CD8 T cell development and a prominent, albeit reduced, population of CD8 T cells capable of producing IL-2 develops under these conditions. It has been previously shown that CD8 T cell frequencies are altered in extralymphoid organs if the T cells cannot produce autonomous IL-2 (34). Thus, the level of IL-2 production by “IL-21-less” CD8 T cells may be sufficient to account for the comparable frequencies observed in non-lymphoid organs of IL-21+/+ and IL-21−/− mice (Fig. 5).
In the current study we show that autocrine production of IL-2 by CD8 T cells is impacted by IL-21. The ability of memory CD8 T cells to synthesize IL-2 is generally associated with polyfunctional attributes, which is characterized by the simultaneous elaboration of multiple effector functions by an individual cell (6, 7, 9, 60, 61). Preferential IL-2 production is also a signature of central memory CD8 T cells and can correlate with greater proliferative potential (62, 63). Thus detection of IL-2 serves as a useful surrogate marker of phenotypically and functionally distinct CD8 T cell subsets. The functional significance of IL-2 production by CD8 T cells is intriguing. Memory CD8 T cell development and maintenance has been shown to be independent of autocrine IL-2 (34, 42). The requirements for intrinsic IL-2 production may also vary depending upon the anatomical location of the memory cells, where it may dictate both expansion and apoptosis of the CD8 T cell population (64). It is also possible that the ability to produce IL-2 preferentially influences the fate of the CD8 T cell population during distinct phases of the immune response.
Although the direct effects of IL-21 on CD8 T cells may shape these responses, IL-21 impacts many immunological functions. Consequently, the indirect actions of IL-21,on other cells of the immune system may also influence the outcome of the CD8 T cell response. IL-21 restricts the maturation of dendritic cells by reducing the expression of MHC class II complexes, CCR7, CD80, CD86 and cytokines including IL-6, IL-12, IL-1α and TNF-α (65, 66). Therefore, in the absence of IL-21 enhanced antigen-presentation, costimulation, and the production of innate cytokines may contribute to altered CD8 T cell activities. IL-21 also has a profound impact on B cell responses by prolonging germinal center reactions and promoting Ig class switching (52, 56, 57, 67–69). Although marked changes in antibody responses have not been detected at early timepoints following acute LCMV infections, lower antibody titers are present during the memory phase (28, 31). Thus, it is possible that underlying changes in B cell activation and antibody levels could indirectly feed back on the CD8 T cell response.
One of the most striking features of CD8 T cells primed in the absence of CD4 T cells is often severely reduced secondary responses (13–15). Therefore, it was important to carefully evaluate whether IL-21 similarly influenced the development of memory CD8 T cell responses which are capable of mounting vigorous recall responses. As shown in figure 8, IL-21 deficient mice are not phenocopies of CD4 T cell deficient hosts. Thus, CD4 T cells must utilize distinct mechanisms in addition to IL-21 production to support secondary CD8 T cell responses. Nevertheless, although not as pronounced as CD4 T cell deficiency, IL-21 can have at least some influence on recall responses. The analyses of mixed bone marrow chimeras revealed a “fitness” difference in the secondary responses of IL-21R−/− CD8 T cells. The kinetics of secondary CD8 T cell responses to LCMV are well characterized, and the responding cells proliferate very rapidly between days 4 and 7 following rechallenge (36, 37). In the rechallenged mixed chimeras the IL-21R−/− cells are outcompeted during this proliferative phase. Therefore, the ability to perceive IL-21 can play some role in shaping recall CD8 T cell responses even though other CD4 T cell-dependent functions must be required. Interestingly, during chronic LCMV infections the direct actions of IL-21 are obligatory for sustaining CD8 T cell responses (28, 29, 31). These discordant outcomes in acute and chronically infected IL-21−/− mice indicate that the precise roles and requirements for IL-21 likely varies with antigen load and the differentiation state of the responding cells. Important next steps will be to dissect how IL-21 integrates with other activatory and suppressive cytokines to influence the development of CD8 T cells capable of producing IL-2 and sustaining responses under conditions of more repetitive or continuous antigenic stimulation.
Acknowledgements
We wish to thank Laurie Harrington and all of the members of the Zajac laboratory for their advice and critical reading of this manuscript. We also thank the University of Alabama at Birmingham CFAR flow cytometry core facility for their services.
This work was supported by grants R01 AI049360, R01 AI067993 and U01 AI082966 (to A.J.Z.) and T32 AI007051 (to J.S.Y) from the National Institutes of Health.
Abbreviations used in this paper
- LCMV
lymphocytic choriomeningitis virus
- LLO
Listeriolysin O
- MFI
mean-fluorescence-intensity
- rLM33
Listeria monocytogenes expressing the LCMV GP33/GP34 epitopes
Footnotes
Publisher's Disclaimer: This is an author-produced version of a manuscript accepted for publication in The Journal of Immunology (The JI). The American Association of Immunologists, Inc. (AAI), publisher of The JI, holds the copyright to this manuscript. This version of the manuscript has not yet been copyedited or subjected to editorial proofreading by The JI; hence, it may differ from the final version published in The JI (online and in print). AAI (The JI) is not liable for errors or omissions in this author-produced version of the manuscript or in any version derived from it by the U.S. National Institutes of Health or any other third party. The final, citable version of record can be found at www.jimmunol.org.
References
- 1.Lau LL, Jamieson BD, Somasundaram T, Ahmed R. Cytotoxic T-cell memory without antigen. Nature. 1994;369:648–652. [PubMed] [Google Scholar]
- 2.Murali-Krishna K, Altman JD, Suresh M, Sourdive DJ, Zajac AJ, Miller JD, Slansky J, Ahmed R. Counting antigen-specific CD8 T cells: a reevaluation of bystander activation during viral infection. Immunity. 1998;8:177–187. doi: 10.1016/s1074-7613(00)80470-7. [DOI] [PubMed] [Google Scholar]
- 3.Homann D, Teyton L, Oldstone MB. Differential regulation of antiviral T-cell immunity results in stable CD8+ but declining CD4+ T-cell memory. Nat Med. 2001;7:913–919. doi: 10.1038/90950. [DOI] [PubMed] [Google Scholar]
- 4.Kristensen NN, Christensen JP, Thomsen AR. High numbers of IL-2-producing CD8+ T cells during viral infection: correlation with stable memory development. J Gen Virol. 2002;83:2123–2133. doi: 10.1099/0022-1317-83-9-2123. [DOI] [PubMed] [Google Scholar]
- 5.Sarkar S, Kalia V, Haining WN, Konieczny BT, Subramaniam S, Ahmed R. Functional and genomic profiling of effector CD8 T cell subsets with distinct memory fates. J Exp Med. 2008;205:625–640. doi: 10.1084/jem.20071641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fuller MJ, Zajac AJ. Ablation of CD8 and CD4 T cell responses by high viral loads. J Immunol. 2003;170:477–486. doi: 10.4049/jimmunol.170.1.477. [DOI] [PubMed] [Google Scholar]
- 7.Wherry EJ, Blattman JN, Murali-Krishna K, van der Most R, Ahmed R. Viral persistence alters CD8 T-cell immunodominance and tissue distribution and results in distinct stages of functional impairment. J Virol. 2003;77:4911–4927. doi: 10.1128/JVI.77.8.4911-4927.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fuller MJ, Khanolkar A, Tebo AE, Zajac AJ. Maintenance, loss, and resurgence of T cell responses during acute, protracted, and chronic viral infections. J Immunol. 2004;172:4204–4214. doi: 10.4049/jimmunol.172.7.4204. [DOI] [PubMed] [Google Scholar]
- 9.Betts MR, Nason MC, West SM, De Rosa SC, Migueles SA, Abraham J, Lederman MM, Benito JM, Goepfert PA, Connors M, Roederer M, Koup RA. HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood. 2006;107:4781–4789. doi: 10.1182/blood-2005-12-4818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harari A, Dutoit V, Cellerai C, Bart PA, Du Pasquier RA, Pantaleo G. Functional signatures of protective antiviral T-cell immunity in human virus infections. Immunol Rev. 2006;211:236–254. doi: 10.1111/j.0105-2896.2006.00395.x. [DOI] [PubMed] [Google Scholar]
- 11.Darrah PA, Patel DT, De Luca PM, Lindsay RW, Davey DF, Flynn BJ, Hoff ST, Andersen P, Reed SG, Morris SL, Roederer M, Seder RA. Multifunctional TH1 cells define a correlate of vaccine-mediated protection against Leishmania major. Nat Med. 2007;13:843–850. doi: 10.1038/nm1592. [DOI] [PubMed] [Google Scholar]
- 12.Seder RA, Darrah PA, Roederer M. T-cell quality in memory and protection: implications for vaccine design. Nat Rev Immunol. 2008;8:247–258. doi: 10.1038/nri2274. [DOI] [PubMed] [Google Scholar]
- 13.Northrop JK, Shen H. CD8+ T-cell memory: only the good ones last. Curr Opin Immunol. 2004;16:451–455. doi: 10.1016/j.coi.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Williams MA, Holmes BJ, Sun JC, Bevan MJ. Developing and maintaining protective CD8+ memory T cells. Immunol Rev. 2006;211:146–153. doi: 10.1111/j.0105-2896.2006.00389.x. [DOI] [PubMed] [Google Scholar]
- 15.Harty JT, Badovinac VP. Shaping and reshaping CD8+ T-cell memory. Nat Rev Immunol. 2008;8:107–119. doi: 10.1038/nri2251. [DOI] [PubMed] [Google Scholar]
- 16.Zajac AJ, Blattman JN, Murali-Krishna K, Sourdive DJ, Suresh M, Altman JD, Ahmed R. Viral immune evasion due to persistence of activated T cells without effector function. J Exp Med. 1998;188:2205–2213. doi: 10.1084/jem.188.12.2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou S, Ou R, Huang L, Price GE, Moskophidis D. Differential tissue-specific regulation of antiviral CD8+ T-cell immune responses during chronic viral infection. J Virol. 2004;78:3578–3600. doi: 10.1128/JVI.78.7.3578-3600.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yi JS, Cox MA, Zajac AJ. T-cell exhaustion: characteristics, causes and conversion. Immunology. 2010 doi: 10.1111/j.1365-2567.2010.03255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parrish-Novak J, Dillon SR, Nelson A, Hammond A, Sprecher C, Gross JA, Johnston J, Madden K, Xu W, West J, Schrader S, Burkhead S, Heipel M, Brandt C, Kuijper JL, Kramer J, Conklin D, Presnell SR, Berry J, Shiota F, Bort S, Hambly K, Mudri S, Clegg C, Moore M, Grant FJ, Lofton-Day C, Gilbert T, Rayond F, Ching A, Yao L, Smith D, Webster P, Whitmore T, Maurer M, Kaushansky K, Holly RD, Foster D. Interleukin 21 and its receptor are involved in NK cell expansion and regulation of lymphocyte function. Nature. 2000;408:57–63. doi: 10.1038/35040504. [DOI] [PubMed] [Google Scholar]
- 20.Spolski R, Leonard WJ. Interleukin-21: basic biology and implications for cancer and autoimmunity. Annu Rev Immunol. 2008;26:57–79. doi: 10.1146/annurev.immunol.26.021607.090316. [DOI] [PubMed] [Google Scholar]
- 21.Hinrichs CS, Spolski R, Paulos CM, Gattinoni L, Kerstann KW, Palmer DC, Klebanoff CA, Rosenberg SA, Leonard WJ, Restifo NP. IL-2 and IL-21 confer opposing differentiation programs to CD8+ T cells for adoptive immunotherapy. Blood. 2008;111:5326–5333. doi: 10.1182/blood-2007-09-113050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alves NL, Arosa FA, van Lier RA. IL-21 sustains CD28 expression on IL-15-activated human naive CD8+ T cells. J Immunol. 2005;175:755–762. doi: 10.4049/jimmunol.175.2.755. [DOI] [PubMed] [Google Scholar]
- 23.Li Y, Bleakley M, Yee C. IL-21 influences the frequency, phenotype, and affinity of the antigen-specific CD8 T cell response. J Immunol. 2005;175:2261–2269. doi: 10.4049/jimmunol.175.4.2261. [DOI] [PubMed] [Google Scholar]
- 24.Nguyen H, Weng NP. IL-21 preferentially enhances IL-15-mediated homeostatic proliferation of human CD28+ CD8 memory T cells throughout the adult age span. J Leukoc Biol. 2010;87:43–49. doi: 10.1189/jlb.0209086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Casey KA, Mescher MF. IL-21 promotes differentiation of naive CD8 T cells to a unique effector phenotype. J Immunol. 2007;178:7640–7648. doi: 10.4049/jimmunol.178.12.7640. [DOI] [PubMed] [Google Scholar]
- 26.Iannello A, Tremblay C, Routy JP, Boulassel MR, Toma E, Ahmad A. Decreased levels of circulating IL-21 in HIV-infected AIDS patients: correlation with CD4+ T-cell counts. Viral Immunol. 2008;21:385–388. doi: 10.1089/vim.2008.0025. [DOI] [PubMed] [Google Scholar]
- 27.Iannello A, Boulassel MR, Samarani S, Debbeche O, Tremblay C, Toma E, Routy JP, Ahmad A. Dynamics and consequences of IL-21 production in HIV-infected individuals: a longitudinal and cross-sectional study. J Immunol. 2010;184:114–126. doi: 10.4049/jimmunol.0901967. [DOI] [PubMed] [Google Scholar]
- 28.Elsaesser H, Sauer K, Brooks DG. IL-21 is required to control chronic viral infection. Science. 2009;324:1569–1572. doi: 10.1126/science.1174182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Frohlich A, Kisielow J, Schmitz I, Freigang S, Shamshiev AT, Weber J, Marsland BJ, Oxenius A, Kopf M. IL-21R on T cells is critical for sustained functionality and control of chronic viral infection. Science. 2009;324:1576–1580. doi: 10.1126/science.1172815. [DOI] [PubMed] [Google Scholar]
- 30.Johnson LD, Jameson SC. Immunology. A chronic need for IL-21. Science. 2009;324:1525–1526. doi: 10.1126/science.1176487. [DOI] [PubMed] [Google Scholar]
- 31.Yi JS, Du M, Zajac AJ. A vital role for interleukin-21 in the control of a chronic viral infection. Science. 2009;324:1572–1576. doi: 10.1126/science.1175194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shedlock DJ, Whitmire JK, Tan J, MacDonald AS, Ahmed R, Shen H. Role of CD4 T cell help and costimulation in CD8 T cell responses during Listeria monocytogenes infection. J Immunol. 2003;170:2053–2063. doi: 10.4049/jimmunol.170.4.2053. [DOI] [PubMed] [Google Scholar]
- 33.Suto A, Kashiwakuma D, Kagami S, Hirose K, Watanabe N, Yokote K, Saito Y, Nakayama T, Grusby MJ, Iwamoto I, Nakajima H. Development and characterization of IL-21-producing CD4+ T cells. J Exp Med. 2008;205:1369–1379. doi: 10.1084/jem.20072057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.D'Souza WN, Schluns KS, Masopust D, Lefrancois L. Essential role for IL-2 in the regulation of antiviral extralymphoid CD8 T cell responses. J Immunol. 2002;168:5566–5572. doi: 10.4049/jimmunol.168.11.5566. [DOI] [PubMed] [Google Scholar]
- 35.Zhou L, Ivanov R, II, Spolski R, Min K, Shenderov T, Egawa DE, Levy W, Leonard J, Littman DR. IL-6 programs T(H)-17 cell differentiation by promoting sequential engagement of the IL-21 and IL-23 pathways. Nat Immunol. 2007;8:967–974. doi: 10.1038/ni1488. [DOI] [PubMed] [Google Scholar]
- 36.Probst HC, Tschannen K, Gallimore A, Martinic M, Basler M, Dumrese T, Jones E, van den Broek MF. Immunodominance of an antiviral cytotoxic T cell response is shaped by the kinetics of viral protein expression. J Immunol. 2003;171:5415–5422. doi: 10.4049/jimmunol.171.10.5415. [DOI] [PubMed] [Google Scholar]
- 37.Tebo AE, Fuller MJ, Gaddis DE, Kojima K, Rehani K, Zajac AJ. Rapid recruitment of virus-specific CD8 T cells restructures immunodominance during protective secondary responses. J Virol. 2005;79:12703–12713. doi: 10.1128/JVI.79.20.12703-12713.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bennett SR, Carbone FR, Karamalis F, Flavell RA, Miller JF, Heath WR. Help for cytotoxic-T-cell responses is mediated by CD40 signalling. Nature. 1998;393:478–480. doi: 10.1038/30996. [DOI] [PubMed] [Google Scholar]
- 39.Ridge JP, Di Rosa F, Matzinger P. A conditioned dendritic cell can be a temporal bridge between a CD4+ T-helper and a T-killer cell. Nature. 1998;393:474–478. doi: 10.1038/30989. [DOI] [PubMed] [Google Scholar]
- 40.Schoenberger SP, Toes RE, van der Voort EI, Offringa R, Melief CJ. T-cell help for cytotoxic T lymphocytes is mediated by CD40-CD40L interactions. Nature. 1998;393:480–483. doi: 10.1038/31002. [DOI] [PubMed] [Google Scholar]
- 41.Castellino F, Huang AY, Altan-Bonnet G, Stoll S, Scheinecker C, Germain RN. Chemokines enhance immunity by guiding naive CD8+ T cells to sites of CD4+ T cell-dendritic cell interaction. Nature. 2006;440:890–895. doi: 10.1038/nature04651. [DOI] [PubMed] [Google Scholar]
- 42.Williams MA, Tyznik AJ, Bevan MJ. Interleukin-2 signals during priming are required for secondary expansion of CD8+ memory T cells. Nature. 2006;441:890–893. doi: 10.1038/nature04790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nakanishi Y, Lu B, Gerard C, Iwasaki A. CD8(+) T lymphocyte mobilization to virus-infected tissue requires CD4(+) T-cell help. Nature. 2009;462:510–513. doi: 10.1038/nature08511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.D'Souza WN, Lefrancois L. Frontline: An in-depth evaluation of the production of IL-2 by antigen-specific CD8 T cells in vivo. Eur J Immunol. 2004;34:2977–2985. doi: 10.1002/eji.200425485. [DOI] [PubMed] [Google Scholar]
- 45.Malek TR. The biology of interleukin-2. Annu Rev Immunol. 2008;26:453–479. doi: 10.1146/annurev.immunol.26.021607.090357. [DOI] [PubMed] [Google Scholar]
- 46.McGuire HM, Vogelzang A, Hill N, Flodstrom-Tullberg M, Sprent J, King C. Loss of parity between IL-2 and IL-21 in the NOD Idd3 locus. Proc Natl Acad Sci U S A. 2009;106:19438–19443. doi: 10.1073/pnas.0903561106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martins G, Calame K. Regulation and functions of Blimp-1 in T and B lymphocytes. Annu Rev Immunol. 2008;26:133–169. doi: 10.1146/annurev.immunol.26.021607.090241. [DOI] [PubMed] [Google Scholar]
- 48.Kallies A, Xin A, Belz GT, Nutt SL. Blimp-1 transcription factor is required for the differentiation of effector CD8(+) T cells and memory responses. Immunity. 2009;31:283–295. doi: 10.1016/j.immuni.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 49.Rutishauser RL, Martins GA, Kalachikov S, Chandele A, Parish IA, Meffre E, Jacob J, Calame K, Kaech SM. Transcriptional repressor Blimp-1 promotes CD8(+) T cell terminal differentiation and represses the acquisition of central memory T cell properties. Immunity. 2009;31:296–308. doi: 10.1016/j.immuni.2009.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shin H, Blackburn SD, Intlekofer AM, Kao C, Angelosanto JM, Reiner SL, Wherry EJ. A role for the transcriptional repressor Blimp-1 in CD8(+) T cell exhaustion during chronic viral infection. Immunity. 2009;31:309–320. doi: 10.1016/j.immuni.2009.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Crotty S, Johnston RJ, Schoenberger SP. Effectors and memories: Bcl-6 and Blimp-1 in T and B lymphocyte differentiation. Nat Immunol. 2010;11:114–120. doi: 10.1038/ni.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ozaki K, Spolski R, Ettinger R, Kim HP, Wang G, Qi CF, Hwu P, Shaffer DJ, Akilesh S, Roopenian DC, Morse HC, 3rd, Lipsky PE, Leonard WJ. Regulation of B cell differentiation and plasma cell generation by IL-21, a novel inducer of Blimp-1 and Bcl-6. J Immunol. 2004;173:5361–5371. doi: 10.4049/jimmunol.173.9.5361. [DOI] [PubMed] [Google Scholar]
- 53.Kwon H, Thierry-Mieg D, Thierry-Mieg J, Kim HP, Oh J, Tunyaplin C, Carotta S, Donovan CE, Goldman ML, Tailor P, Ozato K, Levy DE, Nutt SL, Calame K, Leonard WJ. Analysis of interleukin-21-induced Prdm1 gene regulation reveals functional cooperation of STAT3 and IRF4 transcription factors. Immunity. 2009;31:941–952. doi: 10.1016/j.immuni.2009.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Johnston RJ, Poholek AC, DiToro D, Yusuf I, Eto D, Barnett B, Dent AL, Craft J, Crotty S. Bcl6 and Blimp-1 are reciprocal and antagonistic regulators of T follicular helper cell differentiation. Science. 2009;325:1006–1010. doi: 10.1126/science.1175870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nurieva RI, Chung Y, Martinez GJ, Yang XO, Tanaka S, Matskevitch TD, Wang YH, Dong C. Bcl6 mediates the development of T follicular helper cells. Science. 2009;325:1001–1005. doi: 10.1126/science.1176676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Linterman MA, Beaton L, Yu D, Ramiscal RR, Srivastava M, Hogan JJ, Verma NK, Smyth MJ, Rigby RJ, Vinuesa CG. IL-21 acts directly on B cells to regulate Bcl-6 expression and germinal center responses. J Exp Med. 2010;207:353–363. doi: 10.1084/jem.20091738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zotos D, Coquet JM, Zhang Y, Light A, D'Costa K, Kallies A, Corcoran LM, Godfrey DI, Toellner KM, Smyth MJ, Nutt SL, Tarlinton DM. IL-21 regulates germinal center B cell differentiation and proliferation through a B cell-intrinsic mechanism. J Exp Med. 2010;207:365–378. doi: 10.1084/jem.20091777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kalia V, Sarkar S, Subramaniam S, Haining WN, Smith KA, Ahmed R. Prolonged interleukin-2Ralpha expression on virus-specific CD8+ T cells favors terminal-effector differentiation in vivo. Immunity. 2010;32:91–103. doi: 10.1016/j.immuni.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 59.Pipkin ME, Sacks JA, Cruz-Guilloty F, Lichtenheld MG, Bevan MJ, Rao A. Interleukin-2 and inflammation induce distinct transcriptional programs that promote the differentiation of effector cytolytic T cells. Immunity. 2010;32:79–90. doi: 10.1016/j.immuni.2009.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.La Gruta NL, Turner SJ, Doherty PC. Hierarchies in cytokine expression profiles for acute and resolving influenza virus-specific CD8+ T cell responses: correlation of cytokine profile and TCR avidity. J Immunol. 2004;172:5553–5560. doi: 10.4049/jimmunol.172.9.5553. [DOI] [PubMed] [Google Scholar]
- 61.Makedonas G, Hutnick N, Haney D, Amick AC, Gardner J, Cosma G, Hersperger AR, Dolfi D, Wherry EJ, Ferrari G, Betts MR. Perforin and IL-2 upregulation define qualitative differences among highly functional virus-specific human CD8 T cells. PLoS Pathog. 2010;6:e1000798. doi: 10.1371/journal.ppat.1000798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wherry EJ, Teichgraber V, Becker TC, Masopust D, Kaech SM, Antia R, von Andrian UH, Ahmed R. Lineage relationship and protective immunity of memory CD8 T cell subsets. Nat Immunol. 2003;4:225–234. doi: 10.1038/ni889. [DOI] [PubMed] [Google Scholar]
- 63.Bachmann MF, Wolint P, Schwarz K, Jager P, Oxenius A. Functional properties and lineage relationship of CD8+ T cell subsets identified by expression of IL-7 receptor alpha and CD62L. J Immunol. 2005;175:4686–4696. doi: 10.4049/jimmunol.175.7.4686. [DOI] [PubMed] [Google Scholar]
- 64.D'Souza WN, Lefrancois L. IL-2 is not required for the initiation of CD8 T cell cycling but sustains expansion. J Immunol. 2003;171:5727–5735. doi: 10.4049/jimmunol.171.11.5727. [DOI] [PubMed] [Google Scholar]
- 65.Brandt K, Bulfone-Paus S, Foster DC, Ruckert R. Interleukin-21 inhibits dendritic cell activation and maturation. Blood. 2003;102:4090–4098. doi: 10.1182/blood-2003-03-0669. [DOI] [PubMed] [Google Scholar]
- 66.Strengell M, Lehtonen A, Matikainen S, Julkunen I. IL-21 enhances SOCS gene expression and inhibits LPS-induced cytokine production in human monocyte-derived dendritic cells. J Leukoc Biol. 2006;79:1279–1285. doi: 10.1189/jlb.0905503. [DOI] [PubMed] [Google Scholar]
- 67.Pene J, Gauchat JF, Lecart S, Drouet E, Guglielmi P, Boulay V, Delwail A, Foster D, Lecron JC, Yssel H. Cutting edge: IL-21 is a switch factor for the production of IgG1 and IgG3 by human B cells. J Immunol. 2004;172:5154–5157. doi: 10.4049/jimmunol.172.9.5154. [DOI] [PubMed] [Google Scholar]
- 68.Nurieva RI, Chung Y, Hwang D, Yang XO, Kang HS, Ma L, Wang YH, Watowich SS, Jetten AM, Tian Q, Dong C. Generation of T follicular helper cells is mediated by interleukin-21 but independent of T helper 1, 2, or 17 cell lineages. Immunity. 2008;29:138–149. doi: 10.1016/j.immuni.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vogelzang A, McGuire HM, Yu D, Sprent J, Mackay CR, King C. A fundamental role for interleukin-21 in the generation of T follicular helper cells. Immunity. 2008;29:127–137. doi: 10.1016/j.immuni.2008.06.001. [DOI] [PubMed] [Google Scholar]