Abstract
The health effects of milk and dairy food consumption would best be determined in randomised controlled trials. No adequately powered trial has been reported and none is likely because of the numbers required. The best evidence comes, therefore, from prospective cohort studies with disease events and death as outcomes. Medline was searched for prospective studies of dairy food consumption and incident vascular disease and Type 2 diabetes, based on representative population samples. Reports in which evaluation was in incident disease or death were selected. Meta-analyses of the adjusted estimates of relative risk for disease outcomes in these reports were conducted. Relevant case–control retrospective studies were also identified and the results are summarised in this article. Meta-analyses suggest a reduction in risk in the subjects with the highest dairy consumption relative to those with the lowest intake: 0.87 (0.77, 0.98) for all-cause deaths, 0.92 (0.80, 0.99) for ischaemic heart disease, 0.79 (0.68, 0.91) for stroke and 0.85 (0.75, 0.96) for incident diabetes. The number of cohort studies which give evidence on individual dairy food items is very small, but, again, there is no convincing evidence of harm from consumption of the separate food items. In conclusion, there appears to be an enormous mis-match between the evidence from long-term prospective studies and perceptions of harm from the consumption of dairy food items.
Keywords: Dairy, Milk, Butter, Cheese, Heart disease, Stroke, Diabetes, Cohort studies
Introduction
Milk and dairy foods contain saturated fats, and their consumption often leads to a rise in plasma cholesterol level. This, together with the belief that milk is ‘fattening’, appears to have led to the widespread conviction that milk and dairy foods are a factor in obesity and in heart disease, and that their consumption should be limited.
At least ten hypotheses have been defined in attempts to explain the supposed harm from milk and dairy consumption [1]. The mechanism most frequently quoted is, undoubtedly, a rise in plasma cholesterol concentration following the ingestion of milk or a dairy food item. The drawing of conclusions about milk from its effect upon a single ‘intermediate’ variate, such as cholesterol level, is, however, quite unreasonable, as it ignores the fact that milk, being a complex food with a host of nutrients, is likely to affect many mechanisms relevant to the development of vascular and other diseases. The only valid basis for conclusions about a food item and health or survival comes from long-term studies of the consumption of that food and the incidence of disease or death.
Archie Cochrane was one of the first to urge that conclusions in clinical practice and in medical research are evidence-based, and that the evidence considered comes from all of the available, bias-free relevant studies [2]. The urgings of Cochrane and others have led to ‘evidence-based medicine’ within the whole field of clinical and public health practice. Alvarez-León et al. [3] have, however, pointed out that statements about the benefits and risks of dairy product consumption appear to be based on selected physio-pathological data, such as relationships with cholesterol level, and not on valid epidemiological evidence, indeed, as Alvarez-León et al. commented: “Public health nutrition should not be unaware of the need for evidence-based conclusions.”
The most convincing evidence on a food item and health would come from randomised controlled trials, but no adequately powered trials of milk or dairy consumption have been reported, nor are any likely to be conducted because of the numbers of participants required and the compliance that would be necessary from each participant. By default, the best evidence on dairy food consumption, health and survival comes, therefore, from long-term cohort studies with disease events and death as the outcomes.
We report the results of a literature search and meta-analyses of prospective cohort studies of milk and dairy food consumption as predictors, and death, vascular disease and diabetes as outcomes. We also summarise evidence from relevant retrospective case–control studies.
Experimental Procedure
As far as possible, the procedures in the review and meta-analyses which we conducted are those outlined by Egger et al. [4] and Moher et al. [5] using the statistical programmes available at http://www.systematicreviews.com.
Search Strategy
A number of searches were conducted using Medline, PubMed and ISI Web of Science, and four researchers were involved. Using the search terms for predictors: milk, dairy, dairy products, cheese, butter, cream and yoghurt, together with the terms for outcomes: death, heart disease and stroke, 138 papers were identified and limiting these to ‘adult’ gave 47 papers. The predictors together with the outcome terms diabetes and diabetes mellitus Type 2 gave 330 papers. From these, five papers were selected. Papers which used a composite of foods including dairy items as a predictor were not selected. A further three papers with relevant results, which had not been detected in the electronic searches but which had been identified by the lead author during extensive reading over the past ten and more years, were included.
In the end, a total of 38 reports of cohort studies were selected and used in the analyses presented. Five case–control retrospective studies which gave relevant data are described in what follows, but are not examined by meta-analyses. In an attempt to clarify uncertainties, and/or to obtain further data, letters were sent to 14 authors, but responses were obtained from only a very few.
Meta-Analyses
The results of a test of homogeneity between studies is given for each dairy food, together with estimates of the overall relative risk. Difficulties arose from the fact that the results of individual studies were reported in terms of relative risk, odds ratio or hazard ratio. These three measures of risk are not entirely equivalent. However, in almost all of the studies, the event rate is well below 10% and, in this situation, the odds ratio can be considered as a good approximation for the relative risk [4]. The hazard ratio is a comparison of time-to-event and, so, is not an approximation for the relative risk. However, repeating the summary calculations with and without the studies which reported a hazard ratio produced only a trivial difference in the results.
The summary statistic was calculated using the ‘meta’ command in the Stata statistical software package [4]. This uses an inverse-variance weighting to calculate fixed and random effects summary statistics. The ‘meta’ command was convenient as it calculates the variance using the confidence intervals of the risk estimate. Homogeneity was assessed using the Q statistic, which tests the null hypothesis that the variation between trials is compatible with chance. It follows a Chi-squared distribution with n − 1 degrees of freedom, where n is the number of studies being investigated. In many of our groupings, there was significant heterogeneity. The heterogeneity led to the choice of random effects models for the summary statistics. The adjusted relative risks (RR) given in each individual report were noted, and pooled estimates were obtained from these by weighting the natural logs of each reported RR by the inverse of the variance, as described by Gao et al. [6].
In addition to all of the above, data from relevant retrospective case–control studies are described in the text.
Results
Dairy Foods
Eight long-term cohort studies have reported on all-cause deaths in relation to dairy food consumption (Table 1). Unfortunately, two of the studies [7, 8] do not include sufficient data for inclusion in a meta-analysis. There is no significant heterogeneity between the results for the six studies (P = 0.427) and a meta-analysis suggests a small but significant reduction in total mortality in the subjects with the highest dairy consumption, relative to the risk in the subjects with the lowest consumption (RR) 0.87; 95% confidence limits (0.77, 0.98).
Table 1.
Dairy foods and all-cause mortality
| Study | Number in cohort (length of follow-up) | Number of deaths | Factors adjusted for | Adjusted estimate of risk (95% CI) | Predictive factor and subgroups compared |
|---|---|---|---|---|---|
|
Kahn et al. [7] An Adventists cohort |
22,033 subjects (21 years) | 6,075 | Age, sex, smoking, history of vascular disease, hypertension, diabetes | 0.98 (NS) | 3+ glasses/week vs <1 glass of whole milk |
|
van der Vijver et al. [8] Dutch Civil Servants cohort |
2,605 subjects (28 years) | Numbers not stated | Age, smoking, BMI, systolic BP, cholesterol, energy, alcohol |
1.0 (0.7–1.4) men 0.8 (0.5–1.3) women |
Top third of total calcium intake vs lowest third |
|
Kelemen et al. [45] Iowa Women’s cohort |
29,017 subjects (15 years) | 3,978 | Age, BMI, smoking, energy, education, hypertension, post-menopausal, vitamins, fat intake, fruit, vegetables, fibre | 1.10 (0.97–1.24) | A simulation study substituting a composite of milk, cream, ice cream yoghurt and cheese protein |
|
Mann et al. [46] Oxford Vegetarian cohort |
10,802 subjects (13.3 years) | 383 | Age, sex, smoking, social class | 0.87 (0.68–1.13) | More than 1/2 pint milk/day vs less than 1/2 |
|
Ness et al. [30] Scottish Men cohort |
5,765 men (25 years) | 2,350 | Age, social class, health behaviour and health status | 0.81 (0.61–1.09) | 1 pint+ milk/day vs no milk |
|
Elwood et al. [31] Caerphilly cohort |
2,512 men (20–24 years) | 811 | Age, smoking, social class, IHD, BMI, energy, alcohol, fasting cholesterol HDL cholesterol and triglycerides | 1.20 (0.80–1.80) | 1 pint+ /milk/day vs little or no milk |
|
Trichopoulou et al. [47] A Greek cohort |
1,013 diabetic subjects (4.5 years) | 80 | Age, gender, smoking, education weight and height, hip circum., insulin, hypertension, hyperchol., food groups | 0.92 (0.71–1.19) | Increase in dairy foods by 1 SD/day |
|
van der Pols et al. [48] Carnegie cohort |
4,374 subjects (66–68 years) | 1,468 | Age, sex, area, energy, fruit, vegetables, eggs, protein, fat, energy |
0.77 (0.61–0.98)a 0.77 (0.61–0.97)a |
Top vs bottom quartile dairy |
| Top vs bottom quartile milk |
Details of cohort studies in which the consumption of ‘dairy foods’ (see text) was related to the risk of death, with an estimate of homogeneity between the studies and the results of a meta-analysis
Data from Kahn et al. [7] omitted because of the absence of detailed data; van der Vijver et al. [8] omitted because it was based on the total dietary calcium; Kelemen et al. [45] omitted because it is a test of dietary substitution
0.64M person years; 5,092 deaths: heterogeneity between studies P = 0.427
Meta-analysis (random effects) RR (95% CI) for highest intake groups 0.87 (0.77–0.98)
vs = compared with, or relative to; 1 pint = 0.568 l
aIn van der Pols et al. [48], the estimate for dairy intake was included in the above meta-analysis. This is reported as a hazard ratio and if it is omitted from the meta-analysis, the heterogeneity is P = 0.470 and the overall RR = 0.91 (0.78–1.05)
Milk
Table 2 summarises data from 11 cohort studies of milk consumption and ischaemic heart disease (IHD). Again, two do not include adequate data for inclusion in a meta-analysis. The results of the other nine cohorts show no significant heterogeneity (P = 0.570) and the overall risk of incident heart disease in the subjects with the highest milk intake, relative to those within each cohort with the lowest milk intakes, is 0.92 (0.80, 0.99).
Table 2.
Milk and dairy consumption and incident ischaemic heart disease (IHD)
| Study | Number of subjects (length of follow-up) | Number of heart disease events | Factors adjusted for | Adjusted estimate of risk (95% CI) | Predictive factor |
|---|---|---|---|---|---|
|
Snowdon et al. [33] An Adventists cohort |
8,725 males 15,048 females (20 years) |
758 841 IHD deaths |
Age, smoking and other food items, weight, marital status |
0.94 1.11 |
Two glasses of milk/day vs none |
|
van der Vijver et al. [8] Dutch Civil Servants cohort |
1,340 males 1,265 females |
366 178 CHD deaths |
Age, smoking, BMI, systolic BP, cholesterol, energy, alcohol |
0.77 (0.53–1.11) 0.91 (0.55–1.50) |
Top and bottom tertile of dietary calcium intake |
|
Fraser [49] An Adventists cohort |
26,473 subjects (duration not stated) | Total CHD no. not stated | None | 1.33 (P < 0.07) | One glass or more whole milk vs none |
|
Kelemen et al. [45] Iowa Women’s cohort |
29,017 subjects (15 years) | 739 CHD deaths | Age, BMI, smoking, energy, education, hypertension, post-menopausal, vitamins, fat intake, fruit, vegetables, fibre | 1.41 (1.07–1.87) | A simulation study substituting a composite of milk, cream, ice cream yoghurt and cheese for protein |
|
Nettleton et al. [50] ARIC cohort |
14,153 subjects (13 years) | 1,140 incident heart failure | Age, sex, race, smoking, alcohol, prevalent disease, education, activity | 1.08 (1.01–1.16)a | High-fat dairy: whole milk, cheese and ice cream |
|
Shaper et al. [37] UK RHS cohort |
7,735 subjects (9.5 years) | 608 IHD events | Age, social class, smoking, cholesterol, blood pressure and diabetes | 0.88 (0.55–1.40) | Milk drunk and taken on cereals vs ‘none’ |
|
Mann et al. [46] Oxford Vegetarian cohort |
10,802 subjects (13.3 years) | 63 IHD deaths | Age, sex, smoking, social class | 1.50 (0.81–2.78) | More than 1/2 pint milk per day vs less than 1/2 pint |
|
Bostick et al. [51] Iowa women cohort |
34,486 women (8 years) | 387 IHD deaths | Age, energy, BMI, waist–hip ratio, diabetes, smoking, vit. E, saturated fat, oestrogen, alcohol, education, activity | 0.94 (0.66–1.35) | Top and bottom quartile of milk products |
|
Hu et al. [9] Health Prof. cohort |
80,082 women (14 years) | 939 total CHD | Age, BMI, menopause, HRT, smoking, alcohol, family history, hypertension, aspirin, exercise, vit. E |
1.67 (1.14–1.90)a 0.78 (0.63–0.96)a 1.04 (0.96–1.12)a 0.93 (0.85–1.02)a |
More than two glasses milk/day vs less than one/week: whole milk, skimmed milk, one serving per day high-fat dairy, one serving per day low-fat dairy |
|
Ness et al. [30] Scottish Men cohort |
5,765 men (25 years) | 892 CHD deaths | Age, social class, health behaviour and health status | 0.68 (0.40–1.13) | More than one pint milk/day vs less than one-third/day |
|
Elwood et al. [31] Caerphilly cohort |
2,512 men (20–24 years) | 493 total IHD | Age, smoking, social class, IHD, BMI, energy, alcohol, fasting cholesterol, HDL cholesterol and triglycerides | 0.71 (0.40–1.26) | One or more pint/day vs little or no milk/day |
|
Al Delaimy et al. [52] Health Prof. cohort |
39,800 subjects (12 years) | 1,458 total IHD | Age, BMI, time period, smoking, alcohol, energy and vit E intake, activity, diabetes, hyperchol, family history, aspirin |
1.03 (0.86–1.26) 1.01 (0.83–1.23) |
Top and bottom quintile of dairy calcium intake Total dairy product intake |
|
Larmarche [53] Quebec Cardiovasc. Cohort |
2,000 men (13 years) | 217 total CHD | Age, smoking, BMI, diabetes | 0.73 (0.56–0.93) | Above and below average intake of dairy products |
|
Trichopoulou et al. [47] A Greek cohort |
1,013 subjects (4.5 years) | 46 CVD deaths | Age, gender, smoking, education, weight and height, hip circum., insulin, hypertension, hyperchol., food groups | 0.95 (0.68–1.31) | 150 g (one SD) increase in dairy products |
|
Umesawa et al. [54] JACC cohort |
21,068 men 32,319 women (10 years) |
135 99 Total CHD |
Age, sex, BMI, smoking, alcohol, sodium, potassium, fatty acids, area, menopause, hyperchol., diabetes |
0.80 (0.45–1.44) 1.06 (0.50–2.25) |
Top and bottom quintile of dairy calcium intake |
|
Umesawa et al. [32] JPHC cohort |
41,526 (13 years) | 322 total CHD | Age, sex, BMI, smoking, alcohol, sodium, potassium, fatty acids, area, menopause, hyperchol., diabetes | 1.09 (0.74–1.61) | Top and bottom quintile of dairy calcium intake |
|
van der Pols et al. [48] Carnegie cohortc |
4,374 subjects (66–68 years) | 378 CHD deaths | Age, sex, area, energy, fruit, vegetables, eggs, protein, fat, energy |
0.74 (0.45–.22)a, b 1.06 (0.49 1.31)a, b |
Top and bottom quintile of dairy products Top and bottom quintile of milk |
Details of cohort studies in which the consumption milk and dairy foods was related to incident heart disease, with the results of a meta-analysis
Data from Snowdon et al. [33] and Fraser [49] omitted because of the absence of detailed data; van der Vijver et al. [8] omitted because it was based on the total dietary calcium; Kelemen et al. [45] omitted because it is a test of dietary substitution; Nettleton et al. [50] omitted because the outcome is heart failure
4.3M person years; 16,212 IHD events: heterogeneity between studies P = 0.570
Meta-analysis: risk of a heart disease event in the subjects with the highest milk/dairy intake, relative to that in the subjects with the lowest intake: 0.92 (0.80–0.99)
aIf Nettleton et al. [50] is included, the heterogeneity between studies P = 0.033; RR = 0.92 (0.82–1.03)
bAn estimate for Hu et al. [9] based on the data for milk, assuming 20% of women had been on whole milk, 80% on skimmed, the heterogeneity is P = 0.454; overall RR = 0.88 (0.80, 0.97) and when van der Pols et al. is omitted (because an HR is stated), the heterogeneity is P = 0.408; RR = 0.88 (0.80–0.98). When the estimates of Hu et al. [9] for dairy is used, P = 0.570; RR = 0.92 (0.86–0.99)
cIn van der Pols et al. [48], risk estimates which had been adjusted for calcium are not used because the inclusion of calcium may have led to over-adjustment
As indicated in a footnote to Table 2, the result reported by Hu et al. [9] for whole milk (1.67; 1.14, 1.90) shows marked heterogeneity with all the other estimates of risk for milk. We have, therefore, used the estimate of Hu et al. [9] for skimmed milk in our meta-analysis. If, however, it is assumed that 20% of women in that cohort had been drinking whole milk and 80% skimmed milk, then an overall estimate of IHD risk in the cohort studied by Hu et al. [9] is 0.96 (0.74, 1.15), and putting this estimate into the meta-analysis gives an overall estimate for milk and heart disease of 0.91 (0.77–1.07). A similar problem arose with estimates derived from the same cohort of the US Nurses Health Study by Sun et al. [10]. They used plasma pentadecanoic acid as a surrogate for dairy fat consumption, though it can also be obtained from beef, lamb and venison. The estimate of risk for heart disease that they obtained is statistically inconsistent with estimates derived from other populations in which the same surrogate approach had been used [11]. It could possibly be that the women within the Nurses’ Cohort who drank whole milk had become so highly selected with reference to a range of health-related behaviours that they may have become unrepresentative of any meaningful population group.
In a report based on 27,529 Adventists, Snowdon [12] states that milk was not related to all-cause mortality, but he gives no data. Likewise, Jacobsen and Stensvold [13] refer to “a large prospective study with more than 17,000 men and women followed for 11.5 years (which) showed an inverse relationship between milk drinking (predominantly full-fat milk) and the risk of cardiovascular death.” One of the authors (BKJ) was contacted and details requested, but these are not now available.
A number of cross-sectional studies have been reported in which the past milk consumption of patients admitted to hospital with a myocardial infarct was compared with the past consumption by control subjects without evidence of vascular disease. This research strategy has uncertainties because only a proportion of patients survive an infarct and are questioned, and because the estimation of milk intake prior to the infarct is dependent upon memory. Four such studies have been reviewed elsewhere [14] and a meta-analysis yielded an overall relative risk of milk consumption and incident heart disease of 0.83 (0.66, 0.99). A further, unusual case–control study of 144 diabetic patients with peripheral vascular disease matched with 288 control diabetic patients reported an odds ratio of 0.71 (0.42, 1.19) for peripheral vascular disease in those who consumed milk more than seven times a week relative to those who took milk twice or less per week [15].
The estimates of risk for milk consumption and stroke incidence in the 11 cohorts summarised in Table 3 show significant heterogeneity, and although the overall estimate of risk is significant (0.78; 0.68, 0.91), this cannot be interpreted with confidence. However, the data on stroke in Table 3 relate, as far as is possible, to ischaemic stroke and in Table 4, reports on haemorrhagic strokes and sub-arachnoid bleeds are summarised. Five studies give evidence on haemorrhagic stroke, and, again, there is significant heterogeneity, but the overall risk in relation to dairy intake is 0.75; (0.60, 0.94). Only three studies give evidence on sub-arachnoid bleeds and, ignoring significant heterogeneity, the overall risk in those with the highest dairy intake is 0.65 (0.32, 1.31).
Table 3.
Milk and dairy consumption and incident stroke
| Study | Number of subjects (length of follow-up) | Number and type of stroke | Factors adjusted for | Predictive factor | Adjusted estimate of risk (95% CI) |
|---|---|---|---|---|---|
|
Iso et al. [19] Nurses Health cohort |
85,764 women (14 years) | 347 ischaemic | Age, smoking, time interval, BMI, alcohol, menopause, hormone use, exercise, multivitamins, fatty acid intake, history of hypertension, diabetes and cholesterol | Top and bottom quintile of dairy calcium | 0.70 (0.51–0.97) |
|
Kinjo et al. [55] A Japanese cohort |
223,170 subjects (16 years) | 3,084 thromboembolic | Age, sex, area, smoking, alcohol, occupation | Milk four or more times/week vs less than once/week | 0.85 (0.77–0.92) |
|
Ness et al. [30] Scottish Men cohort |
5,765 men (25 years) | 196 stroke deaths | Age, social class, health behaviour and health status | More than one pint/day vs less than one-third/day | 0.84 (0.31–2.30) |
|
Sauvaget et al. [56] Life span cohort |
40,349 subjects (16 years) | 1,462 stroke deaths | Sex, age, area, BMI, smoking, alcohol, education, diabetes, hypertension, radiation history | Milk almost daily vs none dairy products almost daily vs none |
0.94 (0.79–1.12)a 0.73 (0.57–0.94) |
|
He et al. [57] Health Prof. cohort |
43,732 men (14 years) | 451 ischaemic | Smoking, alcohol, BMI, activity, hyperchol., hypertension, aspirin, potassium, multivitamins, vit E, fruit and veg, energy | High-fat dairy once a day+ vs less than once a week | 1.23 (0.74–2.03) |
|
Elwood et al. [31] Caerphilly cohort |
2,512 men (22–25 years) | 185 ischaemic | Age, smoking, social class, IHD, BMI, energy, alcohol, fasting cholesterol, HDL cholesterol and triglycerides | One or more pint/day vs little or no milk | 0.66 (0.24–1.81) |
|
Abbott et al. [58] Honolulu heart cohort |
3,150 men (22 years) | 229 thromboembolic | Age, dietary K and Na, alcohol, smoking, activity, BP, glucose, cholesterol, glucose, uric acid, Hct | 16 oz/day milk drunk vs non-drinkers | 0.67 (0.45–1.00) |
|
Larsson et al. [23] ATBC cohort |
26,556 men (13.6.years) | 2,702 cerebral infarcts | Age, smoking, alcohol, BMI, education, total cholesterol, diabetes, IHD, energy intake and activity, intake of various foods and original randomisation | Top quintile of a composite of low-fat, whole and sour milk vs lowest quintile | 1.03 (0.96–1.10) |
|
Umesawa et al. [54] JACC cohort |
110,792 subjects (12.9 years) | 284 stroke deaths | Age, sex, BMI, smoking, alcohol, sodium, potassium, fatty acids, area, menopause, hyperchol., diabetes | Top and bottom quintile of dairy calcium intake | 0.53 (0.34–0.81) |
|
Umesawa et al. [32] JPHC cohort |
41,526 subjects (12.9 years) | 664 ischaemic | Age, sex, BMI, smoking, alcohol, sodium, potassium, fatty acids, area, menopause, hyperchol., diabetes | Top and bottom quintile of dairy calcium intake | 0.70 (0.52–0.94) |
|
van der Pols et al. [48] Carnegie cohort |
4,374 subjects (66–68 years) | 121 stroke deaths | Age, sex, area, energy, fruit, vegetables, eggs, protein, fat, energy |
Top and lowest quartiles of dairy Top and bottom quartile of milk |
0.61 (0.27–1.38)a 0.60 (0.28, 1.33) |
Details of cohort studies in which the consumption of milk and dairy foods was related to incident stroke events, with the results of a meta-analysis
8.4M person years; 9,725 strokes: heterogeneity between studies P < 0.000
Meta-analysis: risk of a stroke in the subjects with the highest milk/dairy intake, relative to that in the subjects with the lowest intake: 0.79 (0.68–0.91)
aFor both Sauvaget et al. [56] and van der Pols et al. [48], the results for ‘dairy’ are used in the meta-analysis
Table 4.
Dairy foods, haemorrhagic stroke and sub-arachnoid bleeds
| Study | Number of subjects (length of follow-up) | Number and type of disease event | Factors adjusted for | Adjusted RR (95% CI) | Predictive factor and subgroups compared |
|---|---|---|---|---|---|
|
Kinjo et al. [55] A Japanese cohort |
223,170 subjects (16 years) | 4,773 haemorrhagic stroke deaths | Sex, age, area, smoking, alcohol, occupation | 0.74 (0.68–0.80) | Milk four or more times/week vs once/week |
|
He et al. [57] Health Prof. cohort |
43,732 men (14 years) | 124 haemorrhagic strokes | Smoking, alcohol, BMI, activity, hyperchol., hypertension, aspirin, potassium, multivitamins, vit E, fruit and veg., energy | 1.22 (0.47–3.16) | High-fat dairy once a day or more vs less than once a week |
|
Umesawa et al. [54] JACC cohort |
21,068 men 32,319 women (10 years) |
113 haemorrhagic strokes 128 haemorrhagic strokes |
Age, sex, BMI, smoking, alcohol, sodium, potassium, fatty acids, area, menopause, hyperchol., diabetes |
0.46 (0.23–0.91) 0.51 (0.28–0.94) |
Top and bottom quintile of dairy calcium intake |
|
Umesawa et al. [32] JPHC cohort |
41,526 subjects (12.9 years) | 425 haemorrhagic strokes | Age, sex, BMI, smoking, alcohol, sodium, potassium, fatty acids, area, menopause, hyperchol., diabetes | 0.65 (0.43–0.97) | Top quintile of dairy calcium vs lowest quintile |
|
Larsson et al. [23] ATBC cohort |
26,556 men (13.6 years) | 383 haemorrhagic strokes | Age, smoking, alcohol, BMI, education, total cholesterol, diabetes, IHD, energy intake and activity, intake of various foods and original randomisation |
1.01 (0.82–1.20)a 1.32 (0.89–1.94)a |
Top quintile of a composite of low-fat, whole and sour milk vs lowest quintile Top and lowest quintile of dairy products vs lowest quintile |
|
0.36M person years: 5,946 haemorrhagic strokes: heterogeneity between studies P = 0.014 Meta-analysis (random effects) RR (95% CI) for highest intake groups 0.75 (0.60–0.94) | |||||
|
Umesawa et al. [54] JACC cohort |
21,068 men 32,319 women (10 years) |
37 sub-arachnoid bleeds 34 sub-arachnoid bleeds |
Age, sex, BMI, smoking, alcohol, sodium, potassium, fatty acids, area, menopause, hyperchol., diabetes |
0.19 (0.04–0.87) 0.41 (0.17–0.97) |
Top and bottom quintile of dairy calcium intake |
|
Umesawa et al. [32] JPHC cohort |
41,526 subjects 12.9 years |
217 sub-arachnoid bleeds | Age, sex, BMI, smoking, alcohol, sodium, potassium, fatty acids, area, menopause, hyperchol., diabetes | 0.74 (0.46–1.61) | Top quintile of dairy calcium vs lowest quintile |
|
Larsson et al. [23] ATBC cohort |
26,556 men 13.6 years |
196 sub-arachnoid bleeds | Age, smoking, alcohol, BMI, education, total cholesterol, diabetes, IHD, energy intake and activity, intake of various foods and original randomisation | 1.26 (1.00–1.52) | Top and bottom quintile: dairy products, all milks (whole + low-fat + sour) |
|
0.96M person years: 484 sub-arachnoid bleeds: heterogeneity between studies P = 0.004 Meta-analysis (random effects) RR (95% CI) for highest intake groups 0.65 (0.32–1.31) | |||||
Details of cohort studies in which the consumption of dairy food was related to the risk of haemorrhagic stroke, or a sub-arachnoid bleed, with estimates of homogeneity between the studies and the results of meta-analyses
vs = compared with, or relative to
aThe results for haemorrhagic stroke are based on Larsson et al. [23] for milk. Using Larsson et al. [23] for dairy gives P = 0.022, RR = 0.76 (0.58–1.00)
Butter and Cheese
Table 5 summarises the data from studies in which butter and cheese consumption were examined as possible predictors of vascular disease. For butter, the literature search identified only five cohort studies with incident vascular disease as the outcome. Only three of these give sufficient data to enable inclusion in a meta-analysis. The results are homogeneous, but the overall relationship between butter consumption and vascular events (0.93; 0.84, 1.02) is not statistically significant. In another early cohort study [16], 832 men were followed for 21 years. There were 267 incident CHD events and the authors commented: ‘butter intake did not predict CHD incidence,’ but no original data are given.
Table 5.
Butter, cheese, and vascular disease and death
| Study | Number of subjects (length of follow-up) | Number and type of disease event | Factors adjusted for | Adjusted estimate of risk (95% CI) | Predictive factor and subgroups compared |
|---|---|---|---|---|---|
|
Kahn et al. [7] An Adventists cohort |
22,033 subjects (21 years) | 5,627 deaths | Age, sex, smoking, history of vascular disease, hypertension, diabetes | 1.03 NS (1) | Butter daily cf less than once/week |
|
Gartside et al. [59] NHANES I |
5,811 (16 years) |
CHD events Number not stated |
Age, sex, race, poverty, region, BMI, smoking, education, activity, cholesterol |
Increase in CHD events as butter intake rose P = 0.026 |
Use of butter |
|
Shaper et al. [37] UK RHS cohort |
7,735 subjects (9.5 years) | 608 IHD events | Age, social class, smoking, cholesterol, blood pressure and diabetes | 0.87 (0.79–1.06) | Use of butter cf margarine |
|
Elwood et al. reported in Shaper et al. Caerphilly cohort |
2,187 men (20–24 years) | 605 vascular events | Age, smoking, social class, IHD, BMI, alcohol, total fat intake, systolic BP, diabetes | 0.87 (0.69–1.11) | Use of butter cf margarine use |
|
Larsson et al. [23] ATBC cohort |
26,556 men (13.6 years) |
2,702 cerebral infarcts 383 haemorrhagic 196 sub-arachnoid |
Age, smoking, alcohol, BMI, education, total cholesterol, diabetes, IHD, energy intake and activity, intake of various foods and original randomisation |
1.00 (0.87–1.14)a 1.44 (1.01–2.07) 0.98 (0.59–1.64) |
Top quintile of butter cf lowest quintile |
|
Data from Kahn et al. [7] and Gartside et al. [59] omitted because of absence of detailed data 0.36M person years: 3,310 vascular disease events: heterogeneity between studies P = 0.333 Meta-analysis (random effects) RR (95% CI) for highest intake groups 0.93 (0.84–1.02) | |||||
|
Kahn et al. [7] An Adventists cohort |
22,033 subjects (21 years) | 6,075 deaths | Age, sex, smoking, history of vascular disease, hypertension, diabetes | 0.96 NSb | Cheese on 5–7 days/week cf less than one |
|
Snowdon et al. [33] An Adventists cohort |
25,153 subjects (20 years) |
758 male IHD deaths 841 female IHD deaths |
Age, smoking and other food items, weight, marital status |
0.95 (P > 0.05)b 0.91 (P > 0.05)b |
Cheese daily cf none |
|
Fraser [49] An Adventists cohort |
26,473 (duration not stated) |
Coronary events Number not stated |
Not stated | 0.97 NS | Three or more times/week cf less than once |
|
Gartside et al. [59] NHANES I |
5,811 (16 years) | CHD events | Age, sex, race, poverty, region, BMI, smoking, education, activity, cholesterol | 0.88 (P < 0.002) | Once or more/day cf none |
|
Mann et al. [46] A vegetarian cohort |
10,802 subjects (13.3 years) | 64 IHD deaths | Age, sex, smoking, social class | 2.47 (0.97–6.26) | Cheese 5 or more times/week cf less than once |
|
Larsson et al. [23] ATBC cohort |
26,556 men (13.6 years) |
2,702 cerebr. infarcts 383 haemorrhagic 196 sub-arachnoid |
Age, smoking, alcohol, BMI, education, total cholesterol, diabetes, IHD, energy intake and activity, intake of various foods and original randomisation |
0.88 (0.77–1.01)a 1.01 (0.72–1.41) 1.07 (0.66–1.72) |
Top quintile of cheese cf lowest quintile |
|
Data from Kahn et al. [7], Snowdon et al. [33], Fraser [49] and Gartside et al. [59] omitted because of absence of detailed data 0.4M person years: 2,766 vascular disease events: heterogeneity between studies P = 0.032 Meta-analysis (random effects) RR (95% CI) for highest intake groups 1.32 (0.49–3.56) Meta-analysis (fixed effects) RR (95% CI) for highest intake groups 0.90 (0.79–1.03) | |||||
Details of cohort studies in which the consumption of cheese and of butter was related to a disease outcome or death, with estimates of homogeneity between the studies and the results of a meta-analyses
cf = compared, or, relative to
aElwood et al. here represents data from the Caerphilly Cohort Study reported in Shaper et al. [15], re-analysed by us and updated
bThe studies of cheese intake by Snowdon et al. [58], by Kahn et al. [7] and by Fraser [23] may be on the same cohort. None of these, nor Gartside et al. [20], could be included in the meta-analysis, as no estimates of error are given
cFor Larsson et al. [10], only the results for cerebral infarction were included in the meta-analysis
Several case–control studies of butter and vascular disease have been reported. In one, the previous diets of 106 patients with a myocardial infarct were compared with the diets of 105 controls, and an adjusted odds ratio of an infarct was reported as 2.80 (1.14, 6.85) for ‘butter and margarine’ [17]. In another, the use of butter by 287 women with an acute myocardial infarct was compared with that of 649 control women and an odds ratio in the upper third, adjusted for age alone, of 2.3 was reported [18]. In a study of diabetic patients, 144 with peripheral arterial disease were compared with 288 matched control patients and an odds ratio of 2.06 (1.15. 3.68) reported for the consumption of butter [15].
Evidence on cheese and vascular disease is also limited. Results have been reported from six cohort studies (Table 5), but sufficient data for a meta-analysis are given in only two. A difficulty arises here because, while random effects meta-analysis seems to be appropriate throughout the work in this paper, in the case of the two studies with cheese, there is a massive difference in the numbers of events and, hence, in the power of the two studies, with conclusions in one being based on only 64 vascular events and on 2,702 disease events in the other. It seems reasonable, therefore, for this one dairy item, to use a fixed effects model, thus, weighting the studies appropriately. This gives an overall estimate of risk from cheese of 0.90 (0.79, 1.03).
Other studies on cheese include a follow-up of 27,529 seventh-day Adventists over 20 years, in which it is stated that “…cheese… consumption (was) unrelated to stroke mortality” but no data are given [12]. In a report based on the 85,764 women in the US Nurses Health Study, the authors comment that the inverse association observed for stroke with dairy calcium was not restricted to milk, but was also observed for hard cheese [19], but, again, no data are given. Finally, in a wide-ranging review of studies of cheese consumption, Tholstrup [20] found “no convincing evidence of harm,” and wrote of the ‘neutral’ effect of cheese on coronary heart disease.
A number of studies based on retrospective case–control comparisons examined cheese consumption and vascular disease. A comparison of the past diets of 106 patients with myocardial infarction and 105 control subjects [17] gave an adjusted odds ratio for cheese and yoghurt of 0.42 (0.18–1.03). In another case–control study of 111 myocardial infarction patients and 107 controls [21], an estimated odds ratio in the highest quartile of cheese intake of 0.34 (0.13, 0.91) was reported. In yet other case–control studies, estimates of 0.77 (0.54–1.11) [22] and 1.0 (no CIs stated) [18] were made for cheese consumption. Finally, Ciccarone et al. [15] reported an odds ratio for cheese consumption in 144 diabetic patients with peripheral vascular disease compared with 288 matched control diabetic patients of 0.61 (0.26–1.45).
Other Dairy Foods
Evidence on other individual dairy food items is very sparse indeed. The large ATBS cohort of Finnish male smokers originally enlisted for a randomised trial of antioxidant prophylaxis [23] yielded adjusted odds ratios for the quintile of subjects with the largest intake of cream (0.81; 0.72–0.92 for cerebral infarction and 0.72; 0.52–1.00 for intra-cerebral haemorrhage), yoghurt (1.08; 0.95–1.24 and 1.08; 0.58–1.28) and ice cream (0.92; 0.81–1.03 and 1.21; 0.89–1.63), none of which are significant. In the report on the US Nurses Health Study, Iso et al. [19] commented that the inverse association observed for stroke with dairy calcium was not restricted to milk, but was also shown for yoghurt and for ice cream.
Evidence from cross-sectional retrospective studies of these items comes from Tavani et al. [22], who reported an odds ratio for yoghurt in a case–control study based on 507 patients with an acute myocardial infarction of 0.55 (0.32–0.95). Biong et al. [21] based a study on 111 myocardial infarction patients and 107 controls and estimated an odds ratio in the highest quartile of ice cream of 0.99 (P = 0.21, no CIs stated). Finally, a case–control study of cream consumption in 432 diabetic patients yielded an odds ratio of 2.79 (0.93–8.35) for peripheral vascular disease [15].
Dairy Foods and Diabetes
Elsewhere [24], we have reported a meta-analysis of cross-sectional studies of milk and/or dairy consumption and the metabolic syndrome (RR in the highest consumers of milk and dairy: 0.74; 0.64–0.84). Five studies have now reported on dairy consumption and incident Type 2 diabetes (Table 6). The results of these studies (Table 6) are homogeneous, and the estimated overall relative risk for diabetes is 0.85 (0.75–0.96).
Table 6.
Milk and dairy consumption and diabetes
| Study | Number of subjects (length of follow-up) | Number of new diabetes | Factors adjusted for | Adjusted estimate of risk (95% CI) | Predictive factor |
|---|---|---|---|---|---|
|
Choi et al. [60] Health Prof. Cohort |
41,254 males (12 years) | 1,243 | Age, smoking, alcohol, energy, family history, hyperchol., hypertension, energy intake and activity | 0.91 (0.85–0.97) | Increase of one serving of dairy foods/day |
|
Liu et al. [61] Women’s Health cohort |
37,183 females (10 years) | 1,603 | Age, smoking, alcohol, BMI, hypertension, hyperchol, HRT, family history, energy and activity, dietary intakes randomisation |
0.79 (0.67–0.94)a 1.04 (0.84–1.30) 0.92 (0.78–1.09) |
Top and bottom quintile of all dairy foods Whole milk twice+/week vs <1/month Skim milk twice+/week vs <1/month |
|
van Dam et al. [62] Caerphilly cohort |
41,186 females (8 years) | 1,964 | Age, BMI, smoking, alcohol, education, family history, activity, energy, coffee, sugar, meat, whole grain consumption | 0.93 (0.75–1.15) | Highest vs lowest quintile of total dairy intake |
|
Elwood et al. [24] Caerphilly cohort |
640 males (22–25 years) | 41 | Age, smoking, social class, IHD, BMI, alcohol, total fat intake, systolic BP | 0.57 (0.20–1.63) | Highest and lowest quartile of milk intake |
|
Villegas et al. [63] Shanghai women cohort |
64,191 women (6.9 years) | 2,270 | Age, BMI, smoking, alcohol, waist–hip ratio, activity, income, education, occupation, hypertension, energy | 0.60 (0.41–0.88) | >200 g milk/day vs none |
Details of cohort studies in which the consumption of milk and dairy foods was related to new cases of diabetes, with the results of a meta-analysis
1.7M person years: 7,121 new diabetic patients: heterogeneity between studies P = 0.122
Meta-analysis (fixed effects) RR (95% CI) for highest intake groups: 0.85 (0.75–0.96)
aThe result from Liu et al. [61] for dairy is used in the meta-analysis
Discussion
Much has been written on the associations between the consumption of milk and dairy products and individual vascular risk factors, and, in particular, effects on plasma cholesterol level. An evaluation based upon a single risk factor for a disease can, however, be misleading. At the same time as affecting lipid markers of heart disease, the consumption of milk and dairy produce is associated with an increase in the level of high-density lipoprotein cholesterol [25, 26] and with a reduction in blood pressure [27, 28], and, furthermore, milk and dairy food items are likely to have effects upon many other biological mechanisms and disease processes. Even studies which have examined relationships with a cluster of risk factors for disease, such as the metabolic syndrome [24], cannot possibly give a valid estimate of the overall effect of a complex food such as milk on disease incidence.
Most concern appears to focus on milk consumption and heart disease, and the evidence we present on this is substantial. The studies are homogeneous and the meta-analysis of all of the available evidence suggests that there is a small but worthwhile reduction in risk of coronary heart disease (0.92; 0.80, 0.99) in the subjects who drink the most milk. The evidence which we present on milk and the risk of stroke is also substantial and suggests a reduction in both all stroke (0.79; 0.68–0.91) and in haemorrhagic lesions in those with the highest consumption of milk. A reduction in sub-arachnoid haemorrhage was unexpected, as the aetiology of this condition is totally different to that of thrombo-embolic or haemorrhagic stroke, but benefit from a reduction in blood pressure would be common to all of these events.
All-cause mortality also shows a reduction associated with dairy food consumption (0.87; 0.77–0.98). The evidence of a reduction in diabetes is also substantial, the results of the separate studies are homogeneous (P = 0.122) and the risk reduction in the highest consumers of dairy foods is statistically significant (0.85; 0.75–0.96).
The literature on milk and dairy consumption and cancer is extensive. A detailed examination of the evidence is beyond the scope of this review, but it has been reviewed by the World Cancer Research Fund and the American Institute for Cancer Research [29]. The consumption of milk or dairy foods is associated with a significant reduction in colon cancer (the pooled RR from ten cohort studies is 0.78; 0.69–0.88 and for bladder cancer in four cohorts, the RR is 0.82; 0.67–0.99). There may, however, be an increased risk of prostate cancer, the relative risk estimated from eight cohorts being 1.05; 0.98–1.14. No relationship of importance with milk or dairy consumption was reported for any other cancer.
Apart, perhaps, from milk, no firm conclusions can, however, be drawn on the individual dairy food items. In fact, there is an extreme paucity of studies relating to individual dairy food items. We find this quite remarkable, given the strength of the beliefs about the undesirable effects of butter in particular. The disparity between the results on butter from cohort and from retrospective case–control studies is of concern. Thus, the overview of three cohort studies suggests a possible reduction in vascular disease risk (0.93; 0.84–1.02), while two cross-sectional studies suggested an increase and one an increase in peripheral arterial disease from the consumption of butter. This kind of inconsistency between evidence collected prospectively and evidence dependent upon the memory of patients is, however, not unknown in epidemiological research, and, perhaps, the main message of these data relates to the inadequacy of the evidence on butter and the other dairy items, rather than whether or not there is evidence of harm.
Unfortunately, it is not possible to estimate quantitative relationships with disease incidence for the consumption of a dairy item with any confidence. For example, within the studies reporting milk consumption, the quantity defined as ‘high’ varied in the different studies. Most studies used quartiles or quintiles of the distribution of intakes, while others defined milk intake in terms of the number of occasions on which milk or dairy foods were consumed. Nevertheless, several studies defined a ‘high’ intake as the consumption of one pint (568 ml) or more per day [30–32], in others two or more ‘glasses’ per day [19, 33], while in a study based on weighed dietary intakes [34], the mean daily consumption of milk in the subjects who showed a reduction in vascular disease and diabetes was a pint (568 ml) or more.
A number of systematic reviews of dairy foods have already been published and are consistent with what we present. Gibson et al. [35] identified 12 cohort studies and, from them, drew the conclusion that their review showed “no consistent findings to support the concept that dairy food consumption is associated with a higher risk of coronary heart disease.” Mente et al. [36] looked at a number of foods, including milk. Their conclusion, based on five cohort studies, was that milk has “no significant association with coronary heart disease” (0.91; 0.73–1.00). Two earlier overview studies by us [14, 31] examined associations with milk, and, although based on smaller numbers of cohorts, the results of both are in close agreement with those which we now report.
There are, of course, serious limitations in the evidence we present. The cohort strategy is powerful, but it still has uncertainties and possible biases. In particular, estimates of risk for one item can be confounded by the effects of dietary and other factors apart from milk and dairy consumption. Then, there are differences in social class, smoking and other factors between subjects who drink milk and those who drink little or none, and some of the studies comment upon these [31, 37]. While all of the estimates upon which we have based our overall meta-analyses have each been adjusted for a number of confounding factors, as listed in the tables (age, social class, smoking, alcohol, activity etc.), residual confounding by unknown factors is still possible. While it is possible that this could possibly explain the observed reductions in vascular disease, diabetes and all-cause mortality, it seems highly unlikely that a true harmful effect of milk/dairy consumption on the diseases considered could have been missed simply because of some important, but as yet unknown, confounding factor(s). It is also possible, but again extremely unlikely, that publication bias has led to studies which showed harm from dairy consumption have been preferentially withheld from publication.
The issue of fat-reduced, skimmed milk and other fat-reduced dairy products remains. Despite the widespread beliefs that whole milk increases the risk of vascular disease, and is ‘fattening’, the appropriate question to ask is: do fat-reduced milks provide any advantage further to the benefits conferred by the consumption of whole dairy foods or milk, or does the removal of fat reduce the benefit of the whole items? Low-fat milks were not widely used in the US until about 1989 and about 2000 in the UK, and a large part of the follow-up periods of most of the cohort studies which we have included in the meta-analyses relate, therefore, to times when the milk and dairy items consumed were the full-fat items. Epidemiological studies are of necessity long term and, therefore, the data which we have summarised and the conclusion we have drawn relate overwhelmingly to whole milk and full-fat dairy items.
Given the promotion of fat-reduced milks by many authorities and the large increase in the consumption of fat-reduced milks and dairy items throughout the Western world, this is an area requiring critical study. A number of reports do give evidence on the incidence of disease events in subjects within the same cohort who drank whole milk and others who drank fat-reduced milk, and we have summarised some of these data elsewhere [14]. However, it is most important to accept that persons who choose to drink fat-reduced milks will almost certainly have adopted other ‘healthy’ behaviours, and these will confound any differences in disease outcome within groups of persons defined by the type of milk consumed. It has to be accepted that these other confounding factors cannot all be known, but they will be responsible for biases which cannot possibly be estimated or allowed for. In the absence of evidence from large long-term randomised trials, the statement of German and Dillard [38] is, therefore, most apposite: “Such hypotheses (about fat-reduced milks) are the basis of sound scientific debate; however they are not the basis of sound public health policy.”
On a priori grounds, milk would be expected to be beneficial to health. Calcium has many biological actions, including a reduction in fat absorption through the forming of soaps in the intestine and the binding of cholesterol and bile acids in the gut [39]. Of greater importance is a reduction of blood pressure by dietary calcium, and in a 6-year study of 2,245 older subjects in the Rotterdam Cohort Study, a 20% reduction in incident hypertension was attributed to dairy food consumption [40]. While calcium, magnesium and potassium are all required to prevent hypertension, dairy products are unique in providing a balanced supply of these elements [3, 41]. This may be why milk appears to have a greater effect on blood pressure than dietary calcium supplements [27]. Furthermore, in addition to the minerals provided by milk, certain peptides released on the digestion of milk proteins may have a beneficial effect on blood pressure by inhibiting the angiotension-1-converting enzyme, thus, modulating endothelial function [42].
Renaud et al. [43] described further effects of dietary calcium on thrombo-embolic mechanisms. They fed butter to rabbits and to half, they also gave high levels of calcium. The calcium led to a reduction in platelet aggregation, and a reduction in the severity of atherosclerosis. However, an examination of extensive platelet-related tests in 1,433 older men in the Caerphilly Cohort Study [44] gave no confirmatory evidence in terms of an association between milk consumption and platelet aggregation to adenosine phosphate (P = 0.41), or stressed template bleeding times (P = 0.91) (unpublished data).
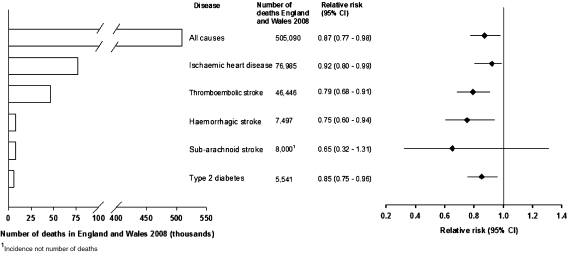
The results of the literature search and meta-analyses presented here are summarised in Table 7 and in Fig. 1. The similarity of the estimates of risk is remarkable and, although conclusions have to be tentative, it seems not unreasonable to conclude that there is no evidence that dairy foods as a total group are associated with harm to health either in terms of death, heart disease, stroke or diabetes, but are probably beneficial in relation to these disease outcomes.
Table 7.
Summary of the relative risk for milk and/or dairy food consumption and various diseases, together with the total numbers of deaths in England and Wales in 2008 from those causes
| Cause of deatha | Number of cohort studies (no. in analyses) | Estimate of the risk ratio for milk or dairy food consumptionb (significance of heterogeneity between studies) | Number of deaths in England and Wales in 2008 |
|---|---|---|---|
| All-cause deaths | 8 (5) | 0.87; 0.77–0.98 (P = 0.427) | 509,090 |
| Ischaemic heart disease (I20–I25)a | 17 (13) | 0.92; 0.80–0.99 (P = 0.570) | 76,985 |
| Stroke (I60–I69)a | |||
| Thrombo-embolic | 11 (11) | 0.79; 0.68–0.91 (P < 0.000) | 46,446 |
| Haemorrhagic | 5 (3) | 0.75; 0.60–0.94 (P = 0.014) | 7,497 |
| Sub-arachnoid | 3 (3) | 0.65; 0.32–1.31 (P = 0.004) | 8,000c |
| Type 2 diabetes (E10-15)a | 5 (5) | 0.85; 0.75–0.96 (P = 0.122) | 5,541 |
aCauses of death as defined in the short list used in the classification of causes of death by the Office of National Statistics UK (Office for National Statistics: mortality statistics: cause (series DH2 No.32). London: The Stationery Office, 2008)
bEstimate of the risk of each disease in subjects with the highest consumption of milk/dairy, relative to the risk in the subjects with the lowest risk (usually the top and the bottom fifths in subjects ranked by consumption)
cThis is an estimate of the total incidence and not the number of deaths
Fig. 1.
The numbers of deaths in England and Wales in 2008 from various causes, and the risks for these causes in the subjects with the highest milk/dairy consumption, relative to the risk in the subjects with the lowest milk/dairy consumption
Apart from their effects on plasma lipids and on blood pressure, very little is known about the biological mechanisms likely to be involved in the relationships of milk and dairy foods with human diseases or, indeed, whether milk can be modified to provide increased health advantages. Clearly, more work should be done.
Due to a focus on the small rise in blood cholesterol with milk drinking, the debate on milk has never achieved a reasonable balance in the evaluation of risks and benefits. We believe that the debate about the health risks and benefits of milk and dairy consumption in Western communities should focus on evidence of direct relevance to health and survival, such as we have presented in this review, and this would benefit greatly if it were supported by a concerted and targeted research effort to understand the underlying mechanisms.
Acknowledgements
Janie Hughes, research assistant, gave considerable help in the literature searches.
Funding
The authors have no vested interest and no special funding was received for the work described. The author has the right to grant, and does grant, an exclusive licence on a worldwide basis, to permit this article to be published and to exploit all subsidiary rights as set out in the appropriate license.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Elwood PC. Milk, coronary disease and mortality. J Epidemiol Community Health. 2001;55:375. doi: 10.1136/jech.55.6.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cochrane AL. Effectiveness and efficiency. Random reflections on health services. London: Nuffield Provincial Hospitals Trust; 1972. [DOI] [PubMed] [Google Scholar]
- 3.Alvarez-León E-E, Román-Viñas B, Serra-Majem LS. Dairy products and health: a review of the epidemiological evidence. Br J Nutr. 2006;96:S94–S99. doi: 10.1079/bjn20061709. [DOI] [PubMed] [Google Scholar]
- 4.Egger M, Davey Smith G, Altman DG. Systematic reviews in health care: meta-analysis in context. London: BMJ Books; 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gao X, LaValley MP, Tucker KL. Prospective studies of dairy product and calcium intakes and prostate cancer risk: a meta-analysis. J Natl Cancer Inst. 2005;97:1769–1777. doi: 10.1093/jnci/dji402. [DOI] [PubMed] [Google Scholar]
- 7.Kahn HA, Phillips RL, Snowdon DA, Choi W. Association between reported diet and all-cause mortality. Twenty-one-year follow-up on 27,530 adult Seventh-Day Adventists. Am J Epidemiol. 1984;119:775–787. doi: 10.1093/oxfordjournals.aje.a113798. [DOI] [PubMed] [Google Scholar]
- 8.van der Vijver LPL, van der Waal MAE, Weterings KGC, Dekker JM, Schouten EG, Kok F. Calcium intake and 28-year cardiovascular and coronary heart disease mortality in Dutch civil servants. Int J Epidemiol. 1992;21:36–39. doi: 10.1093/ije/21.1.36. [DOI] [PubMed] [Google Scholar]
- 9.Hu FB, Stampfer MJ, Manson JE, Ascherio A, Colditz GA, Speizer FE, Hennekens CH, Willett WC. Dietary saturated fats and their food sources in relation to the risk of coronary heart disease in women. Am J Clin Nutr. 1999;70:1001–1008. doi: 10.1093/ajcn/70.6.1001. [DOI] [PubMed] [Google Scholar]
- 10.Sun Q, Ma J, Campos H, Hu FB. Plasma and erythrocyte biomarkers of dairy fat intake and risk of ischemic heart disease. Am J Clin Nutr. 2007;86:929–937. doi: 10.1093/ajcn/86.4.929. [DOI] [PubMed] [Google Scholar]
- 11.Elwood P, Fehily A, Pickering J, Givens I. Pentadecanoic acid (15:0), milk, and ischemic heart disease. Am J Clin Nutr. 2008;87:1540–1541. doi: 10.1093/ajcn/87.5.1540. [DOI] [PubMed] [Google Scholar]
- 12.Snowdon DA. Animal product consumption and mortality because of all causes combined, coronary heart disease, stroke, diabetes, and cancer in Seventh-day Adventists. Am J Clin Nutr. 1998;48:739–748. doi: 10.1093/ajcn/48.3.739. [DOI] [PubMed] [Google Scholar]
- 13.Jacobsen BK, Stensvold I. Milk—a better drink? Relationships with total serum cholesterol in a cross-sectional survey. The Nordland Health Study. Scand J Soc Med. 1992;20:204–208. doi: 10.1177/140349489202000403. [DOI] [PubMed] [Google Scholar]
- 14.Elwood PC, Givens DI, Beswick AD, Fehily AM, Pickering JE, Gallacher JE. The survival advantage of milk and dairy consumption: an overview of evidence from cohort studies of vascular diseases, diabetes and cancer. J Am Coll Nutr. 2008;27:723S–734S. doi: 10.1080/07315724.2008.10719750. [DOI] [PubMed] [Google Scholar]
- 15.Ciccarone E, Di Castelnuovo A, Salcuni M, Siani A, Giacco A, Donati MB, de Gaetano G, Capani F, Iacoviello L. A high-score Mediterranean dietary pattern is associated with a reduced risk of peripheral arterial disease in Italian patients with Type 2 diabetes. J Thromb Haemost. 2003;1:1744–1752. doi: 10.1046/j.1538-7836.2003.00323.x. [DOI] [PubMed] [Google Scholar]
- 16.Gillman MW, Cupples LA, Gagnon D, Millen BE, Ellison RC, Castelli WP. Margarine intake and subsequent coronary heart disease in men. Epidemiology. 1997;8:144–149. doi: 10.1097/00001648-199703000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Lockheart MSK, Steffen LM, Rebnord HM, Fimreite RL, Ringstad J, Thelle DS, Pedersen JI, Jacobs DR. Dietary patterns, food groups and myocardial infarction: a case–control study. Br J Nutr. 2007;98:380–387. doi: 10.1017/S0007114507701654. [DOI] [PubMed] [Google Scholar]
- 18.Gramenzi A, Gentile A, Fasoli M, Negri E, Parazzini F, La Vecchia C. Association between certain foods and risk of acute myocardial infarction in women. BMJ. 1990;300:771–773. doi: 10.1136/bmj.300.6727.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iso H, Stampfer MJ, Manson JE, Rexrode K, Hennekens CH, Colditz GA, Speizer FE, Willett WC. Prospective study of calcium, potassium, and magnesium intake and risk of stroke in women. Stroke. 1999;30:1772–1779. doi: 10.1161/01.str.30.9.1772. [DOI] [PubMed] [Google Scholar]
- 20.Tholstrup T. Dairy products and cardiovascular disease. Curr Opin Lipidol. 2006;17:1–10. doi: 10.1097/01.mol.0000199813.08602.58. [DOI] [PubMed] [Google Scholar]
- 21.Biong AS, Rebnord HM, Fimreite RL, Trygg KU, Ringstad J, Thelle DS, Pedersen JI. Intake of dairy fat and dairy products, and risk of myocardial infarction: a case–control study. Int J Food Sci Nutr. 2008;59:155–165. doi: 10.1080/09637480701532521. [DOI] [PubMed] [Google Scholar]
- 22.Tavani A, Gallus S, Negri E, La Vecchia C. Milk, dairy products, and coronary heart disease. J Epidemiol Com Health. 2002;56:471–472. doi: 10.1136/jech.56.6.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Larsson SC, Männistö S, Virtanen MJ, Kontto J, Albanes D, Virtamo J. Dairy foods and risk of stroke. Epidemiology. 2009;20:355–360. doi: 10.1097/EDE.0b013e3181935dd5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elwood PC, Pickering JE, Fehily AM. Milk and dairy consumption, diabetes and the metabolic syndrome: the Caerphilly prospective study. J Epidemiol Community Health. 2007;61(8):695–698. doi: 10.1136/jech.2006.053157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Temme EHM, Mensink RP, Hornstra G. Comparison of the effects of diets enriched in lauric, palmitic, or oleic acids on serum lipids and lipoproteins in healthy women and men. Am J Clin Nutr. 1996;63:897–903. doi: 10.1093/ajcn/63.6.897. [DOI] [PubMed] [Google Scholar]
- 26.Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146–1155. doi: 10.1093/ajcn/77.5.1146. [DOI] [PubMed] [Google Scholar]
- 27.Griffith LE, Guyatt GH, Cook RJ, Bucher HC, Cook DJ. The influence of dietary and nondietary calcium supplementation on blood pressure: an updated metaanalysis of randomized controlled trials. Am J Hypertens. 1999;12:84–92. doi: 10.1016/S0895-7061(98)00224-6. [DOI] [PubMed] [Google Scholar]
- 28.Garcia-Palmieri MR, Costas R, Jr, Cruz-Vidal M, Sorlie PD, Tillotson J, Havlik RJ. Milk consumption, calcium intake, and decreased hypertension in Puerto Rico. Puerto Rico Heart Health Program study. Hypertension. 1984;6:322–328. doi: 10.1161/01.hyp.6.3.322. [DOI] [PubMed] [Google Scholar]
- 29.World Cancer Research Fund/American Institute for Cancer Research . Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington: American Institute of Cancer Research (AICR); 2007. pp. 129–132. [Google Scholar]
- 30.Ness AR, Davey Smith G, Hart C. Milk, coronary heart disease and mortality. J Epidemiol Community Health. 2001;55:379–382. doi: 10.1136/jech.55.6.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elwood PC, Pickering JE, Fehily AM, Hughes J, Ness AR. Milk drinking, ischaemic heart disease and ischaemic stroke I. Evidence from the Caerphilly cohort. Eur J Clin Nutr. 2004;58:711–717. doi: 10.1038/sj.ejcn.1601868. [DOI] [PubMed] [Google Scholar]
- 32.Umesawa M, Iso H, Ishihara J, Saito I, Kokubo Y, Inoue M, Tsugane S, JPHC Study Group Dietary calcium intake and risks of stroke, its subtypes, and coronary heart disease in Japanese: the JPHC Study Cohort I. Stroke. 2008;39:2449–2456. doi: 10.1161/STROKEAHA.107.512236. [DOI] [PubMed] [Google Scholar]
- 33.Snowdon DA, Phillips RL, Fraser GE. Meat consumption and fatal ischemic heart disease. Prev Med. 1984;13:490–500. doi: 10.1016/0091-7435(84)90017-3. [DOI] [PubMed] [Google Scholar]
- 34.Elwood PC, Strain JJ, Robson PJ, Fehily AM, Hughes J, Pickering J, Ness A. Milk consumption, stroke, and heart attack risk: evidence from the Caerphilly cohort of older men. J Epidemiol Com Health. 2005;59:502–505. doi: 10.1136/jech.2004.027904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gibson RA, Makrides M, Smithers LG, Voevodin M, Sinclair AJ. The effect of dairy foods on CHD: a systematic review of prospective cohort studies. Br J Nutr. 2009;102:1267–1275. doi: 10.1017/S0007114509371664. [DOI] [PubMed] [Google Scholar]
- 36.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169:659–669. doi: 10.1001/archinternmed.2009.38. [DOI] [PubMed] [Google Scholar]
- 37.Shaper AG, Wannamethee G, Walker M. Milk, butter, and heart disease. Br Med J. 1991;302:785–786. doi: 10.1136/bmj.302.6779.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.German JB, Dillard CJ. Saturated fats: what dietary intake? Am J Clin Nutr. 2004;80:550–559. doi: 10.1093/ajcn/80.3.550. [DOI] [PubMed] [Google Scholar]
- 39.Ditscheid B, Keller S, Jahreis G. Cholesterol metabolism is affected by calcium phosphate supplementation in humans. J Nutr. 2005;135:1678–1682. doi: 10.1093/jn/135.7.1678. [DOI] [PubMed] [Google Scholar]
- 40.Engberink MF, Hendriksen MA, Schouten EG, van Rooij FJA, Hofman A, Witteman JC, Geleijnse JM. Inverse association between dairy intake and hypertension: the Rotterdam Study. Am J Clin Nutr. 2009;89:1877–1883. doi: 10.3945/ajcn.2008.27064. [DOI] [PubMed] [Google Scholar]
- 41.Massey LK. Dairy food consumption, blood pressure and stroke. J Nutr. 2001;131:1875–1878. doi: 10.1093/jn/131.7.1875. [DOI] [PubMed] [Google Scholar]
- 42.Clare DA, Swaisgood HE. Bioactive milk peptides: a prospectus. J Dairy Sci. 2000;83:1187–1195. doi: 10.3168/jds.S0022-0302(00)74983-6. [DOI] [PubMed] [Google Scholar]
- 43.Renaud S, Ciavatti M, Thevenon C, Ripoll JP. Protective effects of dietary calcium and magnesium on platelet function and atherosclerosis in rabbits fed saturated fat. Atherosclerosis. 1983;47:187–198. doi: 10.1016/0021-9150(83)90154-5. [DOI] [PubMed] [Google Scholar]
- 44.Elwood PC, Beswick A, Pickering J, McCarron P, O’Brien JR, Renaud SR, Flower RJ. Platelet tests in the prediction of myocardial infarction and ischaemic stroke: evidence from the Caerphilly Prospective study. Br J Haematol. 2001;113:514–520. doi: 10.1046/j.1365-2141.2001.02728.x. [DOI] [PubMed] [Google Scholar]
- 45.Kelemen LE, Kushi LH, Jacobs DR, Jr, Cerhan JR. Associations of dietary protein with disease and mortality in a prospective study of postmenopausal women. Am J Epidemiol. 2005;161:239–249. doi: 10.1093/aje/kwi038. [DOI] [PubMed] [Google Scholar]
- 46.Mann JI, Appleby PN, Key TJ, Thorogood M. Dietary determinants of ischaemic heart disease in health conscious individuals. Heart. 1997;78:450–455. doi: 10.1136/hrt.78.5.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Trichopoulou A, Psaltopoulou T, Orfanos P, Trichopoulos D. Diet and physical activity in relation to overall mortality amongst adult diabetics in a general population cohort. J Intern Med. 2006;259:583–591. doi: 10.1111/j.1365-2796.2006.01638.x. [DOI] [PubMed] [Google Scholar]
- 48.van der Pols JC, Gunnell D, Williams GM, Holly JM, Bain C, Martin RM. Childhood dairy and calcium intake and cardiovascular mortality in adulthood: 65-year follow-up of the Boyd Orr cohort. Heart. 2009;19:1600–1606. doi: 10.1136/hrt.2009.168716. [DOI] [PubMed] [Google Scholar]
- 49.Fraser GE. Diet and coronary heart disease: beyond dietary fats and low-density-lipoprotein cholesterol. Am J Clin Nutr. 1994;59:1117S–1123S. doi: 10.1093/ajcn/59.5.1117S. [DOI] [PubMed] [Google Scholar]
- 50.Nettleton JA, Steffen LM, Loehr LR, Rosamond WD, Folsom AR. Incident heart failure is associated with lower whole-grain intake and greater high-fat dairy and egg intake in the Atherosclerosis Risk in Communities (ARIC) study. J Am Diet Assoc. 2008;108:1881–1887. doi: 10.1016/j.jada.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bostick RM, Kushi LH, Wu Y, Meyer KA, Sellers TA, Folsom AR. Relation of calcium, vitamin D, and dairy food intake to ischemic heart disease mortality among postmenopausal women. Am J Epidemiol. 1999;149:151–161. doi: 10.1093/oxfordjournals.aje.a009781. [DOI] [PubMed] [Google Scholar]
- 52.Al-Delaimy WK, Rimm E, Willett WC, Stampfer MJ, Hu FB. A prospective study of calcium intake from diet and supplements and risk of ischemic heart disease among men. Am J Clin Nutr. 2003;77:814–818. doi: 10.1093/ajcn/77.4.814. [DOI] [PubMed] [Google Scholar]
- 53.Larmarche B (2004) Dairy products—the metabolic syndrome and cardiovascular disease: lessons from Canada. Paper given at the World Dairy Summit, Melbourne, Australia, November 2004
- 54.Umesawa M, Iso H, Date C, Yamamoto A, Toyoshima H, Watanabe Y, Kikuchi S, Koizumi A, Kondo T, Inaba Y, Tanabe N, Tamakoshi A. Dietary intake of calcium in relation to mortality from cardiovascular disease: the JACC study. Stroke. 2006;37:20–26. doi: 10.1161/01.STR.0000195155.21143.38. [DOI] [PubMed] [Google Scholar]
- 55.Kinjo Y, Beral V, Akiba S, Key T, Mizuno S, Appleby P, Yamaguchi N, Watanabe S, Doll R. Possible protective effect of milk, meat and fish for cerebrovascular disease mortality in Japan. J Epidemiol. 1999;9:268–274. doi: 10.2188/jea.9.268. [DOI] [PubMed] [Google Scholar]
- 56.Sauvaget C, Nagano J, Allen N, Grant EJ, Beral V. Intake of animal products and stroke mortality in the Hiroshima/Nagasaki Life Span Study. Int J Epidemiol. 2003;32:536–543. doi: 10.1093/ije/dyg151. [DOI] [PubMed] [Google Scholar]
- 57.He K, Merchant A, Rimm EB, Rosner BA, Stampfer MJ, Willett WC, Ascherio A. Dietary fat intake and risk of stroke in male US healthcare professionals: 14 year prospective cohort study. BMJ. 2003;327:777–782. doi: 10.1136/bmj.327.7418.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Abbott RD, Curb JD, Rodriguez BL, Sharp DS, Burchfiel CM, Yano K. Effect of dietary calcium and milk consumption on risk of thromboembolic stroke in older middle-aged men. The Honolulu Heart Program. Stroke. 1996;27:813–818. doi: 10.1161/01.str.27.5.813. [DOI] [PubMed] [Google Scholar]
- 59.Gartside PS, Wang P, Glueck CJ. Prospective assessment of coronary heart disease risk factors: the NHANES I epidemiologic follow-up study (NHEFS) 16-year follow-up. J Am Coll Nutr. 1998;17:263–269. doi: 10.1080/07315724.1998.10718757. [DOI] [PubMed] [Google Scholar]
- 60.Choi HK, Willett WC, Stampfer MJ, Rimm E, Hu FB. Dairy consumption and risk of type 2 diabetes mellitus in men: a prospective study. Arch Intern Med. 2005;165:997–1003. doi: 10.1001/archinte.165.9.997. [DOI] [PubMed] [Google Scholar]
- 61.Liu S, Song Y, Ford ES, Manson JE, Buring JE, Ridker PM. Dietary calcium, vitamin D, and the prevalence of metabolic syndrome in middle-aged and older U.S. women. Diabetes Care. 2005;28:2926–2932. doi: 10.2337/diacare.28.12.2926. [DOI] [PubMed] [Google Scholar]
- 62.van Dam RM, Hu FB, Rosenberg L, Krishnan S, Palmer JR. Dietary calcium and magnesium, major food sources, and risk of type 2 diabetes in U.S. black women. Diabetes Care. 2006;29:2238–2243. doi: 10.2337/dc06-1014. [DOI] [PubMed] [Google Scholar]
- 63.Villegas R, Gao Y-T, Dai Q, Yang G, Cai H, Li H, Zheng W, Shu XO. Dietary calcium and magnesium intakes and the risk of type 2 diabetes: the Shanghai Women’s Health Study. Am J Clin Nutr. 2009;89:1059–1067. doi: 10.3945/ajcn.2008.27182. [DOI] [PMC free article] [PubMed] [Google Scholar]