Abstract
AIMS
The aims of the study were to assess the trend of older and newer anti-epileptic drugs (AEDs) in the elderly population and to analyze the effects of a health-policy intervention with regard to AED use in general practice in a setting in Southern Italy.
METHODS
Data were extracted from the ‘Caserta-1’ Local-Health-Unit Arianna database in the years 2004–07. Patients aged over 65 years, receiving at least one AED prescription and registered in the lists of 88 general practitioners, were selected. The use of older and newer AEDs was calculated as 1 year prevalence and incidence of use and defined daily dose (DDD) per 1000 inhabitants day−1. Sub-analyses by gender, age and indication of use were performed.
RESULTS
Most of AED users were treated because of neuropathic pain (64.8%). However, the main indication of use for older AEDs (57.8%) was epilepsy, whereas newer AEDs (79.5%) were used for neuropathic pain. Prevalence and incidence of newer AED use increased until 2006, followed by a reduction in 2007. Newer AEDs, particularly gabapentin and pregabalin, were used in the treatment of more patients than older AEDs. However phenobarbital, accounting for more than 50% of total AED volume, was the most prescribed medication during the entire study period.
CONCLUSIONS
An increasing use of AEDs has been observed during 2004–07, mostly due to the prescription of newer compounds for neuropathic pain. The fall in the use of newer AEDs during 2007 coincides with revised re-imbursement criteria for gabapentin and pregabalin. The large use of phenobarbital in the elderly should be considered in the light of a risk of adverse drug reactions.
Keywords: antiepileptic drugs, elderly, epilepsy, general practitioners database, neuropathic pain
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
In the last years there has been a growing trend in anti-epileptic drug (AED) use, particularly in elderly patients, but few data concerning indication of use are available in general practice.
Various AEDs, including newer agents, have been approved for indications other than epilepsy and are increasingly also used for unlicensed indications.
No data about the impact of re-imbursement restrictions on the choice of anti-epileptic drugs in general practice are available.
THIS STUDY ADDS
In general practice, a rapid increase of AED prescriptions in the elderly was observed, principally due to the use of newer AEDs for indications other than epilepsy.
Re-imbursement restrictions influenced newer AED use, particularly pregabalin and gabapentin prescriptions.
Phenobarbital, accounting for more than 50% of total AED volume, was the most prescribed medication during the entire study period. This finding should be considered in light of the potential risks associated with phenobarbital use in the geriatric population.
Introduction
Antiepileptic drugs (AEDs) are the mainstay of the therapy for epilepsy, despite the development in recent years of new therapeutic options, such as brain stimulation [1] or surgery [2]. In the last years, several pharmacoepidemiological studies documented a growing trend in AED use, particularly in elderly patients [3, 4] and the elderly have become the population with the highest growth for epilepsy [5, 6]. The prevalence of this disease ranges from 6.01 per 1000 in patients between 65 and 69 years to 7.73 per 1000 in patients aged over 85 years [7] and is about two-fold the prevalence among younger adults with a higher burden in nursing home residents [8, 9]. Moreover, the annual incidence of epileptic disorders rises from 90 per 100 000 in people between 65 and 69 years to more than 150 per 100 000 in people over 80 years [10, 11].
In the last 15 years, several compounds have been newly marketed. For this reason, AEDs are traditionally divided into two classes: older AEDs (marketed before 1991) and newer AEDs (marketed from 1991) [12, 13]. First and foremost, newer AEDs were developed to be used together with older AEDs as add-on therapy in epileptic patients with a suboptimal control of epilepsy [14]. Nevertheless, some of these newer agents such as lamotrigine, levetiracetam, oxcarbazepine and topiramate are also currently approved in Italy as monotherapy for the treatment of epilepsy.
More recently, various AEDs have been approved for indications other than epilepsy, such as mood disorders or neuropathic pain [15] and an increased use of these compounds has been observed in different countries [3, 4] both for labelled and unlabelled indications [16, 17]. With regard to this, valproic acid, carbamazepine and lamotrigine are approved in the treatment of various phases of bipolar disorder, while gabapentin and pregabalin are approved for neuropathic pain.
As a consequence, starting from January 2007, the Italian National Health System introduced a health-policy intervention (as reported in ‘Nota 4’) which restricted the refundability of newer AEDs pregabalin and gabapentin, in diseases other than epilepsy, only to patients affected by post-herpetic neuralgia, diabetic neuropathy and cancer related neuropathic pain, indications for which scientific evidence has been provided [18]. All the epidemiological studies previously performed, have explored the AED utilization in the general population [19–21], while few data are specifically available on the use of AEDs in elderly outpatients [22, 23]. Moreover, no data concerning the effects of the health-policy intervention regarding the use of AEDs in general practice are available. Thus, the aims of this study were a) to characterize the elderly users of older and newer AEDs during the years 2004–07 in general practice in a setting of Southern Italy, b) to evaluate the trend in the use of newer and older AEDs, both as 1 year prevalence, incidence of use and defined daily dose (DDD) per 1000 inhabitants day−1 and c) to analyze the effects of health-policy intervention with regard to AED use in general practice.
Methods
Data source
Data were extracted from the Arianna database that currently contains information about a population of almost 400 000 individuals living in the area of Caserta and registered in the lists of 289 general practitioners (GPs). Information collected included patients' demographic characteristics and drug prescriptions coded according to the Anatomical Therapeutic Chemical (ATC) classification system. Every drug prescription is linked to medical diagnoses, coded by the ninth edition of International Classification of Diseases (ICD-9). All participating GPs received extensive training in data collection techniques. Data are recorded during daily clinical practice through dedicated software and transferred monthly to the central database, in a complete and anonymous way. Routine quality checks include the analysis of several parameters such as missing patient codes, the number of daily filled prescriptions, the proportion of prescriptions correctly linked to medical diagnoses and monthly continuity of data submission. Quality and completeness of data out of the defined ranges were investigated and back-submitted to each participating GP in order to receive an immediate feedback. GPs failing to meet these standard quality criteria were excluded from the epidemiologic surveys according to the basic standards in the conduction of pharmacoepidemiological investigations [24]. This sample of physicians represented 30.4% (88/289) of total GPs, who practice in the same area. A number of previously published studies has demonstrated that the Arianna database provides accurate and reliable information on drug utilization [25, 26].
Moreover, this data source has previously been used to evaluate the effect of another health-policy intervention in Italy [26].
Study population
For this investigation, 88 GPs who continuously sent data to the Arianna database during the years 2004–07 were included. A total population of almost 140 000 individuals, registered in the lists of these GPs, was analyzed. Among individuals aged 65 years or more, patients who received at least one AED prescription (ATC: N03) during the observational years, were identified. Patients, irrespective of whether pharmacological treatment was initiated by GPs or by specialists working in the public or private sector, were included in the analysis. In fact, in Italy outpatients receive the medicines free of charge only through GP prescriptions. For each patient, data on age, gender, AED prescriptions (including product name) prescription date, number of prescribed packages and indication of use, were analyzed.
Study drugs
AEDs were divided into two groups: i) older AEDs (phenobarbital, ethosuximide, phenytoin, valproic acid, carbamazepine, clonazepam, primidone, barbexaclone, and valpromide) and ii) newer AEDs (levetiracetam, tiagabine, lamotrigine, gabapentin, topiramate, felbamate, oxcarbazepine, vigabatrin, pregabalin and zonisamide).
Data analysis
One-year prevalence of AEDs treatment was evaluated, for each year, as the ratio between the number of patients who received at least one AED prescription and the number of subjects alive and registered in the GPs' lists. Prevalence of use was calculated overall and per year, for both older and newer AEDs. In order to evaluate the incidence of AED use (cumulative incidence), we defined a ‘new user’ as a patient receiving at least one AED prescription during the observational year, without any recorded AED prescription in the previous one. For each year, the incidence was calculated as the number of ‘new users’ divided by the number of subjects free from AED prescription in the previous year. Both prevalence and incidence of use were expressed as rates per 1000 inhabitants, together with the 95% confidence interval (CI). Drug volume was expressed as defined daily dose (DDD) per 1000 inhabitants day−1, where DDD is the assumed average dose per day for a drug used, in adults, for its main indication. DDDs provide a fixed unit of measurement independent of price and formulation, enabling the researcher to assess trends in drug consumption and to perform comparisons between population groups. It does not necessarily reflect the recommended or prescribed daily dose [27].
Statistical analysis
Chi square test for categorical variables and Student's t-test for continuous variables were used to assess the differences between older and newer AED users. Significance was set at a level of P < 0.05. Statistical analyses were performed using STATA 6.0 (STATA Corporation, Texas, USA).
Results
Characteristics of AED users
Out of a total sample of 17 071 elderly patients, 1609 (9.4%) received at least one AED prescription during the study period. In particular, 467 (29.0%) and 1255 (78.0%) were older or newer AED users, respectively. Therefore, 113 patients (7.0% of users) received at least one prescription of both older and newer AEDs. Demographic characteristics and indication of use in the study population are summarized in Table 1.
Table 1.
Demographic characteristics and indication of use of AED users
| Older AEDs (n = 467) | Newer AEDs (n = 1255) | |||||
|---|---|---|---|---|---|---|
| n | % | (95% CI) | n | % | (95% CI) | |
| Age group (years) | ||||||
| 65–74 | 253 | 54.2 | (49.7, 59.7) | 744 | 59.3 | (56.6, 62.0) |
| 75–84 | 175 | 37.5 | (33.1, 41.9) | 441 | 35.1 | (32.5, 37.8) |
| ≥85 | 39 | 8.3 | (5.8, 10.9) | 70 | 5.6 | (4.3, 6.8) |
| Gender | ||||||
| Female | 252 | 54.0 | (49.4, 58.5) | 755 | 60.2 | (57.4, 62.9) |
| Male | 215 | 46.0 | (41.5, 50.6) | 500 | 39.8 | (37.1, 42.5) |
| Indication for use | ||||||
| Epilepsy | 270 | 57.8 | (53.3, 62.3) | 142 | 11.3 | (9.6, 13.1) |
| Pain | 78 | 16.7 | (13.3, 20.1) | 998 | 79.5 | (77.3, 81.7) |
| Mood disorders | 81 | 17.4 | (13.9, 20.8) | 72 | 5.8 | (4.4, 7.0) |
| Other | 38 | 8.1 | (5.7, 10.6) | 43 | 3.4 | (2.4, 4.4) |
Newer and older AED users are not mutually exclusive.
Females were more likely to receive newer AED prescriptions (P < 0.05), while no significant differences in age subgroups were shown between users of newer or older AEDs (Table 1).
With regard to indication of use, overall 354 patients (22.0%) were treated for epilepsy while 1042 patients (64.8%) were treated for neuropathic pain. In particular, a significantly higher proportion (P < 0.01) of older AED users (57.8%) were treated for epilepsy, compared with users of newer AEDs (11.3%). Neuropathic pain was the main indication of treatment for newer AED users (79.5%; P < 0.01) (Table 1).
One year prevalence and incidence of AED use
Overall, the annual prevalence of total AED use increased from 33.0 per 1000 (95% CI: 30.0, 35.7) in 2004 to 53.5 (50.1, 56.9) in 2006, followed by a reduction in 2007 (40.2; 37.3, 43.2). In particular, prevalence of older AED use slightly increased during the study period from 14.4 (12.6, 16.1) in 2004 to 19.8 (17.7, 21.9) in 2007, while the prevalence of use of newer AEDs rose from 22.5 (20.3, 24.7) in 2004 to 41.0 (38.0, 44.0) in 2006, followed by a marked reduction to 25.5 (23.2, 27.9) in 2007. Moreover, 113 patients (6.7; 5.4, 7.8) received at least one prescription of both older and newer AEDs with an increasing trend from 2004 (3.9; 2.9, 4.8) to 2007 (5.1; 4.0, 6.2). The prevalence of older and newer AED use per 1000 inhabitants, in patients affected by epileptic disorders or pain is reported in Figure 1.
Figure 1.
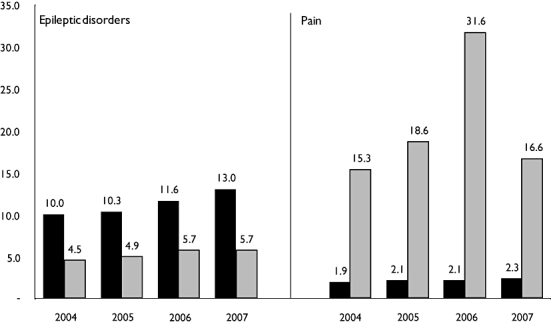
One-year prevalence of AED use per 1000 inhabitants, in patients affected by epileptic disorders or by pain, stratified by drug class and calendar year. Use of newer and older AEDs was not mutually exclusive. Older ( ); Newer (
); Newer ( )
)
Prevalence of phenobarbital, the most prescribed older AED, increased from 7.0 (5.8, 8.3) in 2004 to 9.5 (8.0, 10.9) in 2007. Among newer AEDs, gabapentin was the most prescribed drug until 2005. Pregabalin, newly marketed in Italy from July 2004, overcame gabapentin use during 2006 and 2007 with a prevalence rising from 7.3 (6.0, 8.6) in 2005 to 25.2 (22.8, 27.5) in 2006, followed by a marked reduction in 2007 (13.1; 11.4, 14.8).
The incidence of older AED use increased from 3.1 (2.3, 3.9) in 2004 to 5.3 (4.1, 6.4) in 2007, while newer AED users significantly increased from 13.4 (11.7, 15.2) in 2004 to 27.7 (25.2, 30.3) in 2006 and decreased to 11.8 (9.8, 13.0) in the last year. However, restricting the analysis to patients treated for epileptic disorders, the incidence of use of older AEDs increased slightly from 2005–07 while newer AED use remained stable during the whole study period. In patients affected by pain, the incidence of newer AED use increased from 2004 to 2006 falling to 36% in the last year (Figure 2).
Figure 2.
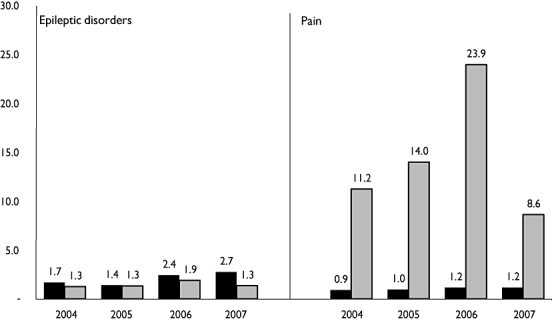
One-year incidence of AED use per 1000 inhabitants, in patients affected by epileptic disorders or by pain, stratified by drug class and calendar year. Use of newer and older AEDs was not mutually exclusive. Older ( ); Newer (
); Newer ( )
)
Concerning specific medications, gabapentin and pregabalin were the drugs mostly prescribed as initial AED treatment during the observational years (Figure 3): the incidence of gabapentin use was up to 10 times higher than that of phenobarbital (the second medication) in 2004 (data not shown). Nevertheless, the number of new users treated with gabapentin decreased from 12.5 (10.8, 14.2) in 2004 to 2.6 (1.8, 3.4) in 2007, while pregabalin rose from 5.5 (4.4, 6.6) in 2005 to 18.1 (16.1, 20.2) in 2006 and decreased to 6.7 (5.5, 8.0) in 2007. Incidence of older AED use remained stable during the study period except for phenobarbital which increased slightly from 1.0 (0.5, 1.5) in 2006 to 1.8 (1.1, 2.4) in 2007. Restricting the analysis to epileptic patients, the incidence of use of phenobarbital showed an increasing trend, ranging from 0.8 (0.4, 1.3) in 2004 to 1.5 (0.9, 2.1) in 2007. A similar trend was observed for valproic acid (2004: 0.4, 0.1, 0.7; 2007: 0.6, 0.2, 1.0) while the incidence of gabapentin use (2004: 0.6; 0.2, 1.0; 2007: 0.1; 0.0, 0.3) decreased over the years. Although gabapentin was the most prescribed drug for pain during 2004 (11.2; 6.1, 16.2) and 2005 (8.6; 7.2, 10.0), it was outnumbered by pregabalin in 2006 for the same indication (17.1; 15.2, 19.1). A marked decrease was shown in 2007 for both medications (gabapentin: 2.2; 1.5, 2.9; pregabalin: 6.4; 5.1, 7.6). Carbamazepine incidence of use slowly increased from 2004 (0.4; 0.1, 0.7) to 2007 (0.7; 0.3, 1.1). No relevant prescriptions of other AEDs were observed in the treatment of pain.
Figure 3.
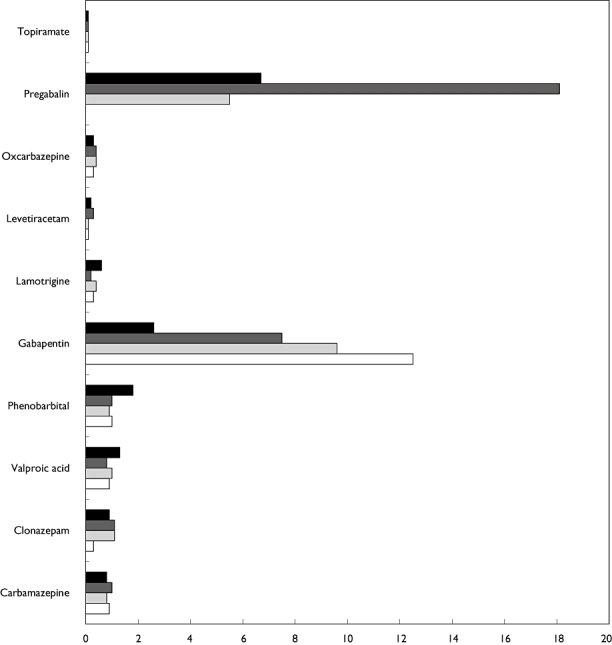
One-year incidence of the most prescribed medications per 1000 inhabitants (more than 90% on total prescriptions during 2007), irrespective of the indication use, stratified by calendar year. 2004 (□); 2005 ( );2006 (
);2006 ( ); 2007 (
); 2007 ( )
)
AED volume
Overall, AED volume, measured as DDD per 1000 inhabitants day−1, increased slightly from 2004 to 2006, remaining stable in the last year (Table 2). Older AEDs were the most used drugs and their volume increased during the whole study period, while newer AED use decreased in 2007 compared with the previous year. With regard to total AED volume, the proportion of newer AED volume rose from 24.9% in 2004 to 34.5% in 2006 followed by a fall during 2007 (29.9%).
Table 2.
Volume of AED prescriptions, measured as DDD/1000 inhabitants day−1, stratified by drug and calendar year
| AED | 2004 DDD 1000 inhabitants day−1 | % | 2005 DDD 1000 inhabitants day−1 | % | 2006 DDD 1000 inhabitants day−1 | % | 2007 DDD 1000 inhabitants day−1 | % |
|---|---|---|---|---|---|---|---|---|
| Older AEDs | ||||||||
| Phenobarbital | 5.70 | 59.8 | 5.83 | 56.7 | 6.16 | 51.7 | 6.40 | 53.8 |
| Phenytoin | 0.01 | 0.1 | 0.03 | 0.2 | ||||
| Valproic acid | 0.52 | 5.5 | 0.66 | 6.4 | 0.66 | 5.5 | 0.78 | 6.5 |
| Carbamazepine | 0.70 | 7.4 | 0.64 | 6.2 | 0.64 | 5.3 | 0.74 | 6.2 |
| Clonazepam | 0.09 | 0.9 | 0.13 | 1.2 | 0.21 | 1.7 | 0.23 | 2.0 |
| Primidone | 0.05 | 0.6 | 0.07 | 0.7 | 0.09 | 0.8 | 0.11 | 0.9 |
| Barbexaclone | 0.09 | 0.9 | 0.07 | 0.7 | 0.05 | 0.4 | 0.05 | 0.4 |
| Valpromide | 0.02 | 0.2 | ||||||
| Total | 7.18 | 75.3 | 7.39 | 72.0 | 7.81 | 65.5 | 8.34 | 70.1 |
| Newer AEDs | ||||||||
| Levetiracetam | 0.05 | 0.6 | 0.08 | 0.8 | 0.19 | 1.6 | 0.26 | 2.1 |
| Tiagabine | 0.04 | 0.4 | ||||||
| Lamotrigine | 0.41 | 4.4 | 0.47 | 4.5 | 0.47 | 3.9 | 0.63 | 5.3 |
| Gabapentin | 1.58 | 16,6 | 1.66 | 16.2 | 1.35 | 11.3 | 0.94 | 7.9 |
| Topiramate | 0.13 | 1.4 | 0.14 | 1.3 | 0.13 | 1.1 | 0.14 | 1.2 |
| Oxcarbazepine | 0.14 | 1.4 | 0.28 | 2.8 | 0.45 | 3.8 | 0.56 | 4.7 |
| Pregabalin | 0.25 | 2.4 | 1.51 | 12.7 | 1.03 | 8.6 | ||
| Total | 2.35 | 24.7 | 2.88 | 28.0 | 4.11 | 34.5 | 3.56 | 29.9 |
| Total AEDs | 9.53 | 100 | 10.27 | 100 | 11.92 | 100 | 11.89 | 100 |
Phenobarbital accounted for more than 50% of total AED volume during the study period, increasing from 5.7 in 2004 to 6.4 in 2007.
Gabapentin, the most frequently used newer AED in 2004 (1.58), decreased to 0.94 in 2007, while pregabalin, the most used newer AED since 2006, rose from 0.25 in 2005 to 1.51 in 2006 and decreased to 1.03 in the last observational year. Newer AEDs, approved to treat epilepsy also as monotherapy, were used in smaller amounts than the previous ones. However, oxcarbazepine and levetiracetam volume rose from 0.14 and 0.05 in 2004 to 0.56 and 0.26 in 2007, respectively.
Discussion
The results of this study indicate an increase in both prevalence and incidence of AED use from 2004 to 2006, followed by a marked reduction in the last observational year in an elderly population in Southern Italy. This finding is mainly due to newer AED use and in particular to gabapentin and pregabalin, usually prescribed for neuropathic pain. Neuropathic pain was the main indication for AED use in our study. In fact 64.8% of AED users were treated because of this condition, while only 22.0% of patients were treated for epilepsy. This result is consistent with our population of elderly patients. In fact painful syndromes affect elderly patients with a prevalence rate between 40% and 80% [28] and AED efficacy in pain is well-documented [15]. The wide use of newer AEDs in indications other than epilepsy is in line with other studies that documented an increased use of newer AEDs in the last few years for the treatment of neuropathic pain [3, 4] However, users of older AEDs were significantly more affected by epilepsy compared with newer AED users (57.8% vs. 11.3%).
The increase of AED use during the years 2004–06 is in line with several European drug utilization studies that explored the trend of AED prescriptions [3, 4, 22, 29, 30]. In particular, a recent survey, performed in an Italian general population during 2000–05, showed a prevalence ranging from 11.4 to 34.8 in patients over 65 years [4].
A different trend in the prevalence of use of older and newer AEDs was observed in our study; older AED use increased slightly during the whole study period (14.4 in 2004 to 19.8 per 1000 in 2007), while newer AED use substantially increased until 2006 (41.0), with a 40% decrease in the following year (25.5). Similar trends were shown regarding the incidence of newer and older AED use. The striking decrease of newer AED use in 2007 could be ascribed to the introduction, by the Italian Drug Agency, of a restriction in the refundability for gabapentin and pregabalin (Nota 4) starting from January 2007 [18]. In detail, this health policy intervention was targeted to restrict the refundability of these medications, in diseases other than epilepsy, only to patients with severe neuropathic pain associated with post-herpetic neuralgia, diabetic neuropathy or cancer [18]. Even though this kind of health policy intervention is principally aimed at cost-containment, measures adopted for drug refundability are based on EBM principles, taking into account only proven scientific evidence. Our study showed that drug refundability restrictions may be very influential and have far reaching consequences for drug prescribing behaviour. As a consequence, it could be considered as a useful tool, not only in cost-containment, but also in improving effective and safe prescribing of new drugs. Even though these conditions are the only ones with proven scientific evidence, a large increase in gabapentin and pregabalin use has been observed for unlicensed indications in the last few years [16, 17].
The study also showed a peculiar trend of gabapentin and pregabalin use. Gabapentin, the most used AED until 2005, significantly decreased in the following years, as reported in the Italian National report on drug use (OsMed 2007) [31]. On the contrary, the use of pregabalin strongly increased starting from its introduction to the market (July 2004), becoming the most prescribed AED during 2006. This finding confirms the trend of newly marketed drugs widely prescribed in general practice after their marketing [32]. In addition, this trend in the use of pregabalin and gabapentin may reflect a change in the promotional strategies by the drug manufacturer of both medications, since gabapentin lost its patent in 2005. In line with this hypothesis, a previous paper has shown how promotional strategies influenced the use of gabapentin by physicians [16].
Although the prevalence and incidence of newer AED use strongly increased until 2006 and were consistently higher than older AED use, opposite results were shown after restricting the analysis to epileptic patients. Indeed, in this condition, older AED prevalence of use was almost twice that of newer AED use and phenobarbital emerged as the most prescribed medication. Nevertheless, no difference between older and newer AED incidence of use was observed until 2006. Gabapentin, not currently approved in Italy to treat epilepsy as monotherapy, was the most used newer AED in epileptic patients. Conversely, a very low incidence of use was reported for other newer medications approved to treat epilepsy as monotherapy, such as oxcarbazepine and levetiracetam.
Older AED volume was significantly higher with respect to newer AEDs when measured as DDD per 1000 inhabitants day−1. The reported higher volume of older AEDs could be explained by a more persistent use in chronic diseases while newer AEDs are principally used for acute conditions [3].
In particular, phenobarbital, accounting for more than 50% of total AED volume, was the most prescribed medication during the entire study period, followed by valproic acid and carbamazepine. Phenobarbital volume increased more than 10% during the study years. A recently published study, based on a US population, indicated a decreasing trend in the use of phenobarbital in older patients with new-onset epilepsy during the years 2000–04 [23]. Phenytoin, the most used AED reported in this study, is scarcely prescribed in the general practice setting in Southern Italy, as well as in the Italian general population [4]. The large use of phenobarbital observed in our research and confirmed by other studies deserves a particular consideration [23, 33]. Indeed, it disagrees with recently published international guidelines and expert consensus recommendations, suggesting the use of lamotrigine, gabapentin or carbamazepine as first line agents in the treatment of epilepsy in elderly patients [33–35]. This is because of the negative cognitive effects, sedation and potential toxicity of phenobarbital in this group of patients. This finding should be considered in the light of the potential risks associated with phenobarbital use in geriatric population [28].
Finally, an increasing trend in volume of use of oxcarbazepine and levetiracetam was observed with almost a five fold increase between 2004 and 2007. This result is in line with a US study reporting a significant increase in the use of these drugs over time [23].
Strength and limitations of the study
To our knowledge, this is the first drug-utilization study that provides information about both prevalence and incidence of AED use in elderly outpatients. Another strength of this study is the availability of clinical information, such as indication of AED use, in the data source. However, several limitations of this study need to be considered. First, diagnoses made by GPs may not be highly accurate and for this reason we decided not to evaluate the AED use in the treatment of different subtypes of epilepsy. Second, we used outpatient prescription data and we had no information about actual filling and use of the medications. However, this study was primarily aimed at exploring the prescribing pattern of AEDs without considering any clinical outcome. In addition, such an investigation was performed using data collected from a restricted area of Southern Italy. It is therefore possible that these findings could not be fully generalized to the whole Italian general practice. However, the comparison with the Italian national report on drug consumption supported the reliability of this database in providing information about AED utilization in Italy. Finally, the generalizability of the results is restricted to the outpatient setting, since data on elderly inpatients and those residing in nursing homes were missing. As a consequence, the prevalence rates might have underestimated the use of these agents, especially in certain age groups, such as very old people, who are more likely to be admitted to these facilities. To avoid an additional underestimation, only GPs who continuously provided data to the Arianna database, during the whole observation period, were included in the study. Sensitivity analysis did not show any significant difference in prescribing behaviour between GPs enrolled in the study and the others.
In conclusion, a different prescribing pattern of newer and older AEDs in elderly patients was observed in the last years in a general practice setting in Southern Italy; older AED use increased slightly during the study years, while a strong increase in the use of newer AEDs was reported until 2006, followed by a striking reduction in 2007. Phenobarbital has been increasingly used in the treatment of epileptic disorders in elderly patients, while newer AEDs, mainly gabapentin and pregabalin, were largely prescribed for neuropathic pain. The increased use of pregabalin instead of gabapentin, since its introduction on the market, could be justified by a change in the promotional strategies by the drug manufacturer of both medications. The health policy intervention, introduced in 2007 to restrict the use of gabapentin and pregabalin only for the indications supported by scientific evidence, led to a significant reduction in the use of both medications.
Competing interests
The authors have no conflict of interest to disclose related to this article. Vincenzo Arcoraci had full access to all the data in the study and had final responsibility for the decision to submit for publication. This study was not supported by any grant.
The authors thank the general practitioners from Caserta-1 Local Health Unit, who actively participated in this investigation by sending data continuously to the Arianna database in the years 2004–07: Serrao Luigi, Consoli Angelo, Corbisiero Carmine, Gammardella Gerardo, Betti Antonio, Marrocco Angelo, Pellegrino Pasquale, Zeppetelli, Giovanni, Nocera Pasquale, Zitiello Vincenzo, Ferrucci Carlo Eugenio, Letizia Giuseppe, Pulcino Lupo Giacomo, Correra Alessandro, Di Muccio Marcellino, Greco Agostino, Iuliano Maurizio, Iannelli Fernando, Marino Antonio, Failli Gianfranco, Iorio Enrico, Canzano Silvestro, Pontillo Maria Giovanna, Lauritano Gennaro, Coscione Margherita, Pascarella Andrea, Anastasio Antonio, De Sire Giustino, Moretti Salvatore, Di Zazzo Cesare, Barbato Domenico, Del Forno Massimo, Cavallo Pasquale, Ferrucci Francesco, Ceniccola Marianna, Della Rocca Giacinto, De Lucia Vincenzo, Castellano Maria Carmela, Porciello Aldo, Giarrusso Giovanni Alfonso, Costarella Attilio, Cicala Ferdinando, De Matteis Ornella, Abussi Maria Carmela, Nunziata Sergio, Buono Nicola, Bernardo Giuseppe, Lombardi Innocenzo, Affinita Ciro Natale, Salzillo Girolamo, Bernardi Guido, Chirico Maria Teresa, Sibillo Antonio, Ragucci Luigi, Bove Mario, Ambrosio Luigi, Vozza Giacomo, Porfidia Giovanni, Tartaglione Giacomo, Sirignano Rodolfo Aniello, Valentino Maria, Bianco Pasquale, Cesare Augusto, Moriello Pasquale, Pascarella Giuseppe, Zaccaria Francesco, De Rosa Marcantonio, Cioffi Angelo, Addeo Petronilla Maria, Trovato Francesco, Santangelo Domenico, Sagnelli Clemente, Roberti Michele, Pascarella Silvio, Massara Giorgio, Di Sorbo Stefano, Scalzitti Fausto, Morra Vittoria, Improta Bruno Vincenzo, Giordano Stefano, Gigliofiorito Arturo, Ferraiolo Nicolina, De Cesare Giovanni, Rossi Carmine, La Vedova Michele, De Cesare Gabriella, Leone Renato, Barone Michele.
REFERENCES
- 1.Theodore WH, Fisher RS. Brain stimulation for epilepsy. Lancet Neurol. 2004;3:111–18. doi: 10.1016/s1474-4422(03)00664-1. [DOI] [PubMed] [Google Scholar]
- 2.Engel J, Jr, Wiebe S, French J, Sperling M, Williamson P, Spencer D, Gumnit R, Zahn C, Westbrook E, Enos B Quality Standards Subcommittee of the American Academy of Neurology; American Epilepsy Society; American Association of Neurological Surgeons. Practice parameter: temporal lobe and localized neocortical resections for epilepsy: report of the Quality Standards Subcommittee of the American Academy of Neurology, in association with the American Epilepsy Society and the American Association of Neurological Surgeons. Neurology. 2003;60:538–47. doi: 10.1212/01.wnl.0000055086.35806.2d. [DOI] [PubMed] [Google Scholar]
- 3.Tsiropoulos I, Gichangi A, Andersen M, Bjerrum L, Gaist D, Hallas J. Trends in utilization of antiepileptic drugs in Denmark. Acta Neurol Scand. 2006;113:405–11. doi: 10.1111/j.1600-0404.2006.00639.x. Erratum in: Acta Neurol Scand 2006; 114: 70. [DOI] [PubMed] [Google Scholar]
- 4.Savica R, Beghi E, Mazzaglia G, Innocenti F, Brignoli O, Cricelli C, Caputi AP, Musolino R, Spina E, Trifirò G. Prescribing patterns of antiepileptic drugs in Italy: a nationwide population-based study in the years 2000–2005. Eur J Neurol. 2007;14:1317–21. doi: 10.1111/j.1468-1331.2007.01970.x. [DOI] [PubMed] [Google Scholar]
- 5.Perucca E, Berlowitz D, Birnbaum A, Cloyd JC, Garrard J, Hanlon JT, Levy RH, Pugh MJ. Pharmacological and clinical aspects of antiepileptic drug use in the elderly. Epilepsy Res. 2006;68(Suppl. 1):S49–63. doi: 10.1016/j.eplepsyres.2005.07.017. [DOI] [PubMed] [Google Scholar]
- 6.Forcadas MI, Peña Mayor P, Salas Puig J. Special situations in epilepsy: women and the elderly. Neurologist. 2007;6(Suppl. 1):S52–61. doi: 10.1097/NRL.0b013e31815c613d. [DOI] [PubMed] [Google Scholar]
- 7.Wallace H, Shorvon S, Tallis R. Age-specific incidence and prevalence rates of treated epilepsy in an unselected population of 2,052,922 and age-specific fertility rates of women with epilepsy. Lancet. 1998;352:1970–3. doi: 10.1016/S0140-6736(98)04512-7. [DOI] [PubMed] [Google Scholar]
- 8.Sheorajpanday RV, De Deyn PP. Epileptic fits and epilepsy in the elderly: general reflections, specific issues and therapeutic implications. Clin Neurol Neurosurg. 2007;109:727–43. doi: 10.1016/j.clineuro.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Waterhouse EJ, DeLorenzo RJ. Status epilepticus in older patients: epidemiology and treatment options. Drugs Aging. 2001;18:133–42. doi: 10.2165/00002512-200118020-00006. [DOI] [PubMed] [Google Scholar]
- 10.Brodie MJ, Kwan P. Epilepsy in elderly people. BMJ. 2005;331:1317–22. doi: 10.1136/bmj.331.7528.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cloyd J, Hauser W, Towne A, Ramsay R, Mattson R, Gilliam F, Walczak T. Epidemiological and medical aspects of epilepsy in the elderly. Epilepsy Res. 2006;68(Suppl. 1):S39–48. doi: 10.1016/j.eplepsyres.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 12.Glauser T, Ben-Menachem E, Bourgeois B, Cnaan A, Chadwick D, Guerreiro C, Kalviainen R, Mattson R, Perucca E, Tomson T. ILAE treatment guidelines: evidence based analysis of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 2006;47:1094–120. doi: 10.1111/j.1528-1167.2006.00585.x. [DOI] [PubMed] [Google Scholar]
- 13.French JA, Kanner AM, Bautista J, Abou-Khalil B, Browne T, Harden CL, Theodore WH, Bazil C, Stern J, Schachter SC, Bergen D, Hirtz D, Montouris GD, Nespeca M, Gidal B, Marks WJ, Jr, Turk WR, Fischer JH, Bourgeois B, Wilner A, Faught RE, Jr, Sachdeo RC, Beydoun A, Glauser TA Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology; Quality Standards Subcommittee of the American Academy of Neurology; American Epilepsy Society. Efficacy and tolerability of the newer antiepileptic drugs I: treatment of newer onset epilepsy: report of the Therapeutics and Technology Assessment Subcommittee and Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Epilepsia. 2004;45:401–9. doi: 10.1111/j.0013-9580.2004.06204.x. [DOI] [PubMed] [Google Scholar]
- 14.French JA, Kanner AM, Bautista J, Abou-Khalil B, Browne T, Harden CL, Theodore WH, Bazil C, Stern J, Schachter SC, Bergen D, Hirtz D, Montouris GD, Nespeca M, Gidal B, Marks WJ, Jr, Turk WR, Fischer JH, Bourgeois B, Wilner A, Faught RE, Jr, Sachdeo RC, Beydoun A, Glauser TA Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology; Quality Standards Subcommittee of the American Academy of Neurology; American Epilepsy Society. Efficacy and tolerability of the new antiepileptic drugs II: treatment of refractory epilepsy: report of the Therapeutics and Technology Assessment Subcommittee and Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2004;62:1261–73. doi: 10.1212/01.wnl.0000123695.22623.32. [DOI] [PubMed] [Google Scholar]
- 15.Spina E, Perugi G. Antiepileptic drugs: indications other than epilepsy. Epileptic Disord. 2004;6:57–75. [PubMed] [Google Scholar]
- 16.Steinman MA, Bero LA, Chren MM, Landefeld CS. Narrative review: the promotion of gabapentin: an analysis of internal industry documents. Ann Intern Med. 2006;145:284–93. doi: 10.7326/0003-4819-145-4-200608150-00008. [DOI] [PubMed] [Google Scholar]
- 17.Steinman MA, Harper GM, Chren MM, Landefeld CS, Bero LA. Characteristics and impact of drug detailing for gabapentin. PLoS Med. 2007;4:e134. doi: 10.1371/journal.pmed.0040134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agenzia Italiana del Farmaco. Le note AIFA 2006–2007 per l'uso appropriato dei farmaci. Available at http://www.agenziafarmaco.it/wscs_render_attachment_by_id/111.90291.1168607405163575e.pdf?id = 111.88204.1168596628882 (last accessed 25 September 2008)
- 19.Rochat P, Hallas J, Gaist D, Friis ML. Antiepileptic drug utilization: a Danish prescription database analysis. Acta Neurol Scand. 2001;104:6–11. doi: 10.1034/j.1600-0404.2001.00197.x. [DOI] [PubMed] [Google Scholar]
- 20.Miketek G, Matek P. Prevalence of epilepsy in Croatia: a population-based survey. Acta Neurol Scand. 2007;116:361–7. doi: 10.1111/j.1600-0404.2007.00881.x. [DOI] [PubMed] [Google Scholar]
- 21.Oun A, Haldre S, Mägi M. Use of antiepileptic drugs in Estonia: an epidemiologic study of adult epilepsy. Eur J Neurol. 2006;13:465–70. doi: 10.1111/j.1468-1331.2006.01268.x. [DOI] [PubMed] [Google Scholar]
- 22.Oles KS, Gal P, Penry JK, Tapscott WK. Use of antiepileptic drugs in elderly population. Public Health Reports. 1987;102:335–7. [PMC free article] [PubMed] [Google Scholar]
- 23.Pugh MJ, Van Cott AC, Cramer JA, Knoefel JE, Amuan ME, Tabares J, Ramsay RE, Berlowitz DR Treatment In Geriatric Epilepsy Research (TIGER) Team. Trends in antiepileptic drug prescribing for older patients with new onset epilepsy: 2000–2004. Neurology. 2008;70:2171–8. doi: 10.1212/01.wnl.0000313157.15089.e6. [DOI] [PubMed] [Google Scholar]
- 24.Lawrenson R, Williams T, Farmer R. Clinical information for research: the use of general practice databases. J Pub Health Med. 1999;21:299–304. doi: 10.1093/pubmed/21.3.299. [DOI] [PubMed] [Google Scholar]
- 25.Piacentini N, Trifiró G, Tari M, Moretti S, Arcoraci V. Statin-macrolide interaction risk: a population based study throughout a general practice database. Eur J Clin Pharmacol. 2005;61:615–20. doi: 10.1007/s00228-005-0972-z. [DOI] [PubMed] [Google Scholar]
- 26.Trifirò G, Alacqua M, Corrao S, Tari M, Arcoraci V. Statins for the primary prevention of cardiovascular events in elderly patients: a picture from clinical practice without strong evidence from clinical trials. J Am Geriatr Soc. 2008;56:175–7. doi: 10.1111/j.1532-5415.2007.01486.x. [DOI] [PubMed] [Google Scholar]
- 27.WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC Classification and DDD Assignment. Oslo: WHO Collaborating Centre for Drug Statistics and Methodology; 2001. [Google Scholar]
- 28.Ferrell BA. Pain management in elderly people. J Am Geriatr Soc. 1991;39:64–73. doi: 10.1111/j.1532-5415.1991.tb05908.x. [DOI] [PubMed] [Google Scholar]
- 29.Galimberti CA, Magri F, Magnani B, Arbasino C, Cravello L, Marchioni E, Tartara A. Antiepileptic drug use and epileptic seizures in elderly nursing home residents: a survey in the province of Pavia, Northern Italy. Epilepsy Res. 2006;68:1–8. doi: 10.1016/j.eplepsyres.2005.09.031. [DOI] [PubMed] [Google Scholar]
- 30.Banfi R, Borselli G, Marinai C, Borgheresi A, Cavalieri A. Epidemiological study of epilepsy by monitoring prescriptions of antiepileptic drugs. Pharm World Sci. 1995;17:138–40. doi: 10.1007/BF01872391. [DOI] [PubMed] [Google Scholar]
- 31.Agenzia Italiana del Farmaco. L'uso dei farmaci in Italia. Rapporto OsMed 2007. Available at http://www.agenziafarmaco.it/allegati/rapporto_osmed_2007.pdf (last accessed 25 September 2008)
- 32.Garrison GD, Levin GM. Factors affecting prescribing of the newer antidepressants. Ann Pharmacother. 2000;34:10–4. doi: 10.1345/aph.19079. [DOI] [PubMed] [Google Scholar]
- 33.Scottish Intercollegiate Guidelines Network. Diagnosis and management of epilepsy in adults. 2003. Scottish Intercollegiate Guidelines Network. Available at http://www.sign.ac.uk/pdf/sign70.pdf (last accessed 25/09/2008)
- 34.Patsalos PN, Perucca E. Clinically important drug interactions in epilepsy: interactions between antiepileptic drugs and other drugs. Lancet Neurol. 2003;2:473–81. doi: 10.1016/s1474-4422(03)00483-6. [DOI] [PubMed] [Google Scholar]
- 35.National Collaborating Center for Primary Care. The Epilepsies: the Diagnosis and Management of the Epilepsies in Adults and Children in Primary and Secondary Care. London: National Institute for Clinical Excellence; 2004. [Google Scholar]


