Despite promising early results, cancer therapy aimed at selective destruction of tumor blood vessels faces several hurdles. Among these is the astronomical expense of chronic intravenous treatment with certain antiangiogenic drugs, which makes long-term therapy impractical for most patients. In this issue, Folkman and colleagues1 describe a biochemically engineered antiangiogenic compound, called Lodamin, that increases the oral availability and serum half-life of TNP-470, an antiangiogenic small molecule developed previously by this group. With this formulation, the authors have overcome a substantial obstacle to widespread clinical use of TNP-470 and offer the prospect of vastly improving the efficacy of chronic antiangiogenic treatment of tumors and metastases.
Observing that tumors fail to progress in the absence of angiogenesis, the late Judah Folkman first set forth the idea that integration with the circulatory system is a prerequisite for the advanced growth of cancers2. This phenomenon was termed the “angiogenic switch”—the point at which a tumor acquires a dedicated functional blood supply, facilitating the growth and spread of cancerous cells to other organs. This concept was initially confronted with skepticism because it was difficult to imagine how the growth of tumor endothelial cells could be selectively inhibited without compromising blood supply to other vital organs. But later studies showed that malignant transformation is associated with the upregulation of tumor-specific angiogenic factors that selectively induce the assembly of tumor vessels and are less essential for the maintenance of quiescent normal vascular beds3.
Accumulating evidence suggests that deprivation of blood supply is effective in inducing the regression of primary tumors and diminishing the frequency and extent of metastasis4,5. Ongoing clinical trials have proven the efficacy of antiangiogenic agents, such as neutralizing monoclonal antibodies or small-molecule inhibitors targeted to the vascular endothelial growth factor (VEGF-A) signaling pathway, in increasing the survival of patients with advanced, kidney, colon and possibly breast cancers4,5. However, in most advanced tumors, the response to antiangiogenic therapy, even in combination with conventional chemotherapy6, is not long lasting, and tumor cells bypass targeted signaling pathways and recruit new angiogenic pathways to become invested with blood supply7. An additional obstacle is the high cost of chronic intravenous therapy, which may be necessary to block post-treatment rebound tumor neo-angiogenesis and retard the recurrence and progression of tumors. Thus, there is a critical need to enhance the long-term bioavailability of antiangiogenic agents whose activity does not overlap with that of existing drugs.
TNP-470, a synthetic analog of fumagillin (isolated from the fungus Aspergillus fumigatus fresenius), is effective in blocking tumor neo-angiogenesis8 and was among the first antiangiogenic drugs to enter clinical trials. When given to mice alone or in combination with conventional chemotherapeutic agents, it has broad-spectrum anticancer activity. In human trials9 it slowed progression of solid tumors and, in some cases, even resulted in their regression. However, it was also neurotoxic, with side effects such as dizziness, short-term memory loss, confusion, depression and problems with motor coordination. Folkman’s group eliminated these neurological side effects by conjugating TNP-470 to a polymer that prevents passage across the blood-brain barrier10. Nevertheless, the drug still could not be effectively administered orally and had an extremely short half-life in circulation, necessitating frequent (multiple times per week) and continuous (over 1 h) intravenous infusions9. As these costly treatments result in substantial patient discomfort, an oral formulation would be of great benefit. But the relative insolubility of TNP-470 has precluded administration of a clinically effective dose by oral delivery.
Lodamin has vastly increased oral bio-availability compared with TNP-470 while retaining its antiangiogenic benefit. The authors generated Lodamin by conjugating TNP-470 to a diblock copolymer (Fig. 1). This copolymeric form of the drug is amphiphilic and, in an aqueous medium, self-assembles into micelles. In this complex, TNP-470 remains protected within the core even in highly acidic conditions like those found in the digestive system. The enhanced stability of Lodamin allows transfer into the circulation and subsequent accumulation in tumor tissue. The authors tracked the systemic distribution and accumulation of copolymeric micelles by loading them with fluorescent markers and showed rapid entry of fluorescent dyes into microvilli of the small intestines of mice. Within one hour of oral administration, high levels of the fluorescent micelles were detected in plasma, persisting for up to 72 h. Importantly, the micelles could not cross the blood-brain barrier and accumulated in the liver, and, in mouse cancer models, mostly in tumor cells.
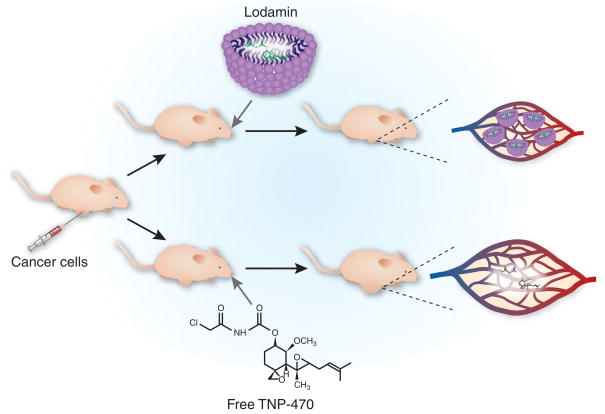
Figure 1.
The structure of Lodamin enhances its bioavailability and stability in circulation and inhibits tumor growth and metastasis. Combining TNP-470 with a co-polymer generates Lodamin, an amphiphilic molecule that forms micelles in aqueous solution. Orally administered Lodamin shows rapid entry into circulation and maintains high levels in serum relative to free TNP-470. In mouse tumor models, Lodamin accumulates in tumor tissue and, by abrogating tumor vasculature, reduces primary tumor growth and liver metastasis.
Oral administration of Lodamin showed a striking ability to inhibit growth of both primary and metastatic tumors compared with free TNP-470. With daily oral doses of both compounds, tumor growth was significantly inhibited only in Lodamin-treated animals, and failed development of tumor vessels resulted in apoptosis of cancer cells. Lodamin also dramatically affected the development of liver metastasis: twenty days after injection of cancer cells, 100% of Lodamin-treated mice were alive, whereas more than half of the mice treated with TNP-470 alone had died. The marked ability of Lodamin to prevent liver metastasis fulfills a major promise of antiangiogenesis therapy and may provide a substantial benefit in suppressing the progression of malignant cancer cells within the liver.
The copolymer structure of Lodamin was designed to preclude transfer across the blood-brain barrier, but this formulation comes at the expense of the drug’s therapeutic potential. The authors showed accumulation of Lodamin mainly in the liver, which makes it effective for prevention of primary and metastatic growth within that organ, but may limit its action in the brain and perhaps other organs. Although the antiangiogenic properties of Lodamin in animals are exciting, the drug’s efficacy in human trials has yet to be determined. Other angiogenesis inhibitors, such as bevacizumab (Avastin), originally manifested minor toxicities when delivered in mice11. Unexpectedly, however, in a clinical setting Avastin caused significant side effects in a small subset of patients, including hypertension and increased risk of bleeding11. It is possible that Lodamin, despite its low toxicity profile in mouse tumor models, may also cause more severe side effects, particularly if used in a chronic treatment regimen. Before instituting human trials, it may be prudent to interrogate the potential toxicities associated with acute and chronic use of Lodamin in nonhuman primates or other in vivo models.
A major unresolved issue surrounding Lodamin is the mechanism of its antiangiogenic effect. Proposed molecular targets include methionine aminopeptidase, p21, p53 and Rac1. Defining the mechanism of action of Lodamin is important because effective treatment of certain tumors is achieved only by combining multiple chemotherapeutic agents that presumably act on nonoverlapping aspects of tumor cell growth and survival. Thus, a combination of antiangiogenic agents, including Lodamin and Avastin, may be effective in blocking tumor neo-angiogenesis and preventing the ‘angiogenic escape’ phenomenon, whereby tumors recruit alternate angiogenic pathways to support neo-vessel formation.
Advanced locally invasive or metastatic cancers are particularly refractory to treatment because they are able to evade treatment and/or exploit the vascular system to colonize distant sites. Ultimately, complete systemic eradication of cancer cells using chemotherapy may not be feasible; however, a combination of antiangiogenic agents may abrogate vascular-mediated advance or angiogenic escape of tumor cells. Indeed, long-term antiangiogenic treatment with drugs like Lodamin may turn certain cancers into a chronic disease by preventing the formation of new blood vessels and thus enforcing tumor dormancy.
Nearly four decades after their ground-breaking proposal of an “angiogenic switch,” Folkman’s group has taken yet another step toward realizing the therapeutic potential of drugs based on this model. The innovative concepts pioneered by Folkman have transformed the cancer therapeutic landscape and may continue to improve the life expectancy of patients with devastating advanced cancers for which there are no other therapies.
References
- 1.Benny O. Nat Biotechnol. 2008;26:799–807. doi: 10.1038/nbt1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Folkman J. N Engl J Med. 1971;285:1182–1186. doi: 10.1056/NEJM197111182852108. [DOI] [PubMed] [Google Scholar]
- 3.Hanahan D, Folkman J. Cell. 1996;86:353–364. doi: 10.1016/s0092-8674(00)80108-7. [DOI] [PubMed] [Google Scholar]
- 4.Folkman J. Nat Rev Drug Discov. 2007;6:273–286. doi: 10.1038/nrd2115. [DOI] [PubMed] [Google Scholar]
- 5.Jain RK, Duda DG, Clark JW, Loeffler JS. Nat Clin Pract Oncol. 2006;3:24–40. doi: 10.1038/ncponc0403. [DOI] [PubMed] [Google Scholar]
- 6.Gasparini G, Longo R, Fanelli M, Teicher BA. J Clin Oncol. 2005;23:1295–1311. doi: 10.1200/JCO.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 7.Thurston G, Noguera-Troise I, Yancopoulos GD. Nat Rev Cancer. 2007;7:327–331. doi: 10.1038/nrc2130. [DOI] [PubMed] [Google Scholar]
- 8.Ingber D, et al. Nature. 1990;348:555–557. doi: 10.1038/348555a0. [DOI] [PubMed] [Google Scholar]
- 9.Bhargava P, et al. Clin Cancer Res. 1999;5:1989–1995. [PubMed] [Google Scholar]
- 10.Satchi-Fainaro R, et al. Nat Med. 2004;10:255–261. doi: 10.1038/nm1002. [DOI] [PubMed] [Google Scholar]
- 11.Ferrara N, Kerbel RS. Nature. 2005;438:967–974. doi: 10.1038/nature04483. [DOI] [PubMed] [Google Scholar]