Abstract
Epidemiological evidence suggests that the incidence of amyotrophic lateral sclerosis is increased in association with head injury. Repetitive head injury is also associated with the development of chronic traumatic encephalopathy (CTE), a tauopathy characterized by neurofibrillary tangles throughout the brain in the relative absence of β-amyloid deposits. We examined 12 cases of CTE and, in 10, found a widespread TAR DNA-binding protein of approximately 43 kd (TDP-43) proteinopathy affecting the frontal and temporal cortices, medial temporal lobe, basal ganglia, diencephalon, and brainstem. Three athletes with CTE also developed a progressive motor neuron disease with profound weakness, atrophy, spasticity, and fasciculations several years before death. In these 3 cases, there were abundant TDP-43–positive inclusions and neurites in the spinal cord in addition to tau neurofibrillary changes, motor neuron loss, and corticospinal tract degeneration. The TDP-43 proteinopathy associated with CTE is similar to that found in frontotemporal lobar degeneration with TDP-43 inclusions, in that widespread regions of the brain are affected. Akin to frontotemporal lobar degeneration with TDP-43 inclusions, in some individuals with CTE, the TDP-43 proteinopathy extends to involve the spinal cord and is associated with motor neuron disease. This is the first pathological evidence that repetitive head trauma experienced in collision sports might be associated with the development of a motor neuron disease.
Keywords: Amyotrophic lateral sclerosis, Chronic brain injury, Motor neuron disease, Sports, Tau proteins, TDP-43
INTRODUCTION
Amyotrophic lateral sclerosis (ALS) is a fatal progressive degeneration of motor neurons in the brain and spinal cord. Whereas 90% to 95% of ALS cases are sporadic, gene mutations in copper/zinc superoxide dismutase 1, senataxin, dynactin, angiogenic, and TAR-DBP (the gene for transactive response DNA-binding protein of 43 kd [TDP-43] on chromosome 1) account for some familial forms of the disease (1, 2). ALS is pathologically characterized by motor neuron loss and corticospinal tract degeneration. In addition, remaining motor neurons in sporadic ALS often have ubiquitin- and TDP-43– immunoreactive inclusion bodies that appear either as rounded hyaline inclusions or as skeinlike inclusions (3–6).
Although the etiology of sporadic ALS is unknown, it has long been suspected to involve a complex interaction between multiple genetic and environmental risk factors. Many environmental risk factors have been considered as possible triggers of the neurodegenerative cascade in ALS, including a history of trauma to the brain and spinal cord (7–13), a history of participation in varsity athletics and a slim physique (14), strenuous physical activity (14–17), cigarette smoking (18–20), and exposure to heavy metals (21–28), radiation, electrical shocks (12, 29), and pesticides (8, 24, 30, 31). Yet, of all the putative environmental risk factors, trauma to the CNS emerges as one of the strongest and most consistent contenders for initiating the molecular cascades that result in ALS (9, 32), as well as other neurodegenerative processes, such as Alzheimer disease (AD) (33–39) and Parkinson disease (40, 41).
That mechanical or traumatic injury to the head, neck, or spine might be etiologically related to ALS has been suggested for more than 100 years (42, 43). More recent literature points toward a trend not only between CNS trauma and the development of ALS but also between a smaller number of years between the last injury and ALS diagnosis, and older age at the last injury and the development of ALS (9, 32). In a case-control study of 109 cases of ALS and 255 controls, Chen et al (9) found that having experienced repeated head injuries or having been injured within the 10 years before diagnosis was associated with a more than 3-fold higher risk of ALS (odds ratio [OR], 3.1; 95% confidence interval [95% CI], 1.2–8.1; and OR, 3.2; 95% CI, 1.0–10.2, respectively), with a slightly elevated risk for the interval 11 to 30 years. The authors further performed a meta-analysis of 8 previous ALS studies and estimated a pooled OR of 1.7 (95% CI, 1.3–2.2) for at least 1 previous head injury. Another case-control study, which was not included in the meta-analysis, reported an increased risk of ALS when the last head injury occurred at an older age and closer to the time of diagnosis (10). ALS incidence and mortality are also reported to be unusually high among professional soccer players in Italy (16, 17, 44). ALS mortality for Italian professional soccer players was increased 12-fold, whereas mortality from other causes was generally lower or comparable to that of the general population (17). Moreover, an incidence study involving 7,325 Italian professional soccer players showed that the incidence of ALS was 6.5 times higher than expected (16). An increased incidence of ALS has also been reported in American football players (45), and clusters of ALS have been found in Canadian and National Football League players, including 3 members of the 1970s San Francisco 49ers (46).
The risk of ALS was reported to be increased approximately 2-fold among veterans of the 1991 Gulf War during the 10 years after the war (47–49). This elevated risk was evident among deployed military personnel who were on active duty, with statistically significant elevations especially notable among those in the Air Force and Army. A second independent study involving only Gulf War veterans younger than 45 years also found an elevated risk of ALS in this population (50). Recently, Schmidt et al (32) found that military veterans who had experienced head injuries during the last 15 years had an adjusted OR for the development of ALS of 2.33 (95% CI, 1.18–4.61) relative to veterans without any head injuries, and that this association was strongest in APOE-ε4 carriers. Several specific attributes of the at-risk military veterans contributed to their higher prevalence of head injuries, including combat-related injuries during deployment to major conflicts and participation in competitive sports.
Repetitive head injury is also associated with the development of chronic traumatic encephalopathy (CTE), a progressive tauopathy clinically associated with behavioral and personality changes, parkinsonism, and dementia (51). Recently, TDP-43 immunoreactivity was found in the cerebral cortex in 3 cases of CTE associated with boxing (52). Although TDP-43 was originally thought to be a specific marker for ALS and frontotemporal lobar degeneration (FTLD) with tau-negative ubiquitin-positive TDP-43–positive inclusions (FTLD-U, recently renamed FTLD-TDP) (5, 53–57), TDP-43–positive inclusions have now been found in a variety of other neurodegenerative disorders.
Through the brain donation program for Center for the Study of Traumatic Encephalopathy at Boston University School of Medicine and the Bedford VA Medical Center, we analyzed the brains and spinal cords of 12 former athletes with CTE; 3 of the athletes with CTE also had signs and symptoms of motor neuron disease (MND). We compared the nature and distribution of tau and TDP-43 immunoreactivity in the brain and spinal cord of the 9 athletes with CTE without MND (CTE–no MND) with those of the 3 with CTE with MND (CTE + MND) and with the findings in the spinal cords of 12 normal controls and 12 individuals with sporadic ALS. We wanted to establish the extent of the TDP-43 proteinopathy in CTE, the relationship of TDP-43 immunoreactivity to symptoms of MND, and whether the TDP-43–immunoreactive pathology colocalized with tau pathology.
MATERIALS AND METHODS
Subjects
The brain and spinal cords from 11 of the 12 athletes with pathologically verified CTE were received through the brain donation program of the Boston University Alzheimer’s Disease Center (ADC) and the Center for the Study of Traumatic Encephalopathy. Brain and spinal cord tissues from the remaining athlete (Case 3) were received from the Massachusetts Alzheimer’s Disease Research Center Brain Bank. Samples of paraffin-embedded brain and spinal cord sections from 12 age- and sex-matched subjects with pathologically verified ALS and 6 of the 12 normal controls were received from the National VA ALS biorepository. Samples of formalin-fixed spinal cord from the remaining 6 age- and sex-matched control subjects who were neurologically intact at time of death were received from the Mount Sinai ADC.
For the athletes, the concussion history, injury history, history of cognitive, behavioral, and neurological abnormalities, motor symptoms, neurological examinations, and clinical status at the time of death were determined through review of medical records and interviews with the players’ next of kin. When available, additional informants were interviewed to obtain confirmation or the information provided. Interviews were conducted by a neuropsychologist (Robert Stern) who was blinded to the results of the neuropathologic examination at the time of the interview. Informants were interviewed before receiving information concerning the results of the neuropathologic examination. Medical records review was also conducted by a neurologist (Neil Kowall) and a neuropathologist (Ann McKee).
Neuropathologic Examination
The neuropathologic processing followed the procedures previously established for the Boston University ADC, Mount Sinai ADC, and Massachusetts Alzheimer’s Disease Research Center Brain Bank; these include a comprehensive analysis of all neurodegenerative conditions (58). Brain tissues from 3 athletes were received in fragments fixed in formalin after processing by medical examiners; brain and spinal cord tissues from the other 9 were received either fresh or fixed in formalin. Paraffin-embedded sections from at least 25 brain regions were stained with Luxol fast blue, hematoxylin and eosin, Bielschowsky silver, AT8 (a mouse monoclonal antibody directed against phosphoserine 202 and phosphothreonine 205 of PHF-tau, 1:2000; Pierce Endogen, Rockford, IL), PHF-1, a monoclonal antibody against phosphoserine 396 and phosphoserine 404 of hyperphosphorylated tau (1:1000; courtesy of Peter Davies), TDP-43 (rabbit polyclonal to TAR DNA-binding protein, 1:1000; Abcam, Cambridge, MA), LN3 (HLA-DR Class II [major histocompatibility complex], 1:2000; Zymed, San Francisco, CA), ubiquitin (rabbit polyclonal, 1:2000; Dako North America Inc, Carpinteria, CA), α-synuclein (rabbit polyclonal, 1:15,000; Chemicon, Temecula, CA), and β-amyloid (Aβ, mouse monoclonal, 1:2000, formic acid pretreatment; Dako North America Inc). In addition, multiple large coronal fragments were cut at 50 μm on a sledge microtome and stained as free-floating sections using CP13, a monoclonal antibody directed against phosphoserine 202 of tau, considered to be the initial site of tau phosphorylation in neurofibrillary tangle (NFT) formation (1:200; courtesy of Peter Davies), glial fibrillary acidic protein (mouse monoclonal, 1:2000; Chemicon), TDP-43, PHF-1, ubiquitin, Aβ, and LN3, all counterstained with cresyl violet as previously described (51). For the control and ALS subjects, 10-μm-thick sections were prepared from paraffin blocks and stained with Luxol fast blue, hematoxylin and eosin, AT8, and TDP-43.
Double immunofluorescence staining was carried out to assess colocalization by confocal imaging using a Leica SP5 laser scanning confocal microscope. Paraffin-embedded tissue sections were deparaffinized in xylene and rehydrated through alcohol before being subjected to antigen retrieval in formic acid. Sections were blocked in Super Block buffer (ScyTek, Logan, UT) containing 5% serum before avidin/biotin blocking and incubation overnight at 4°C with the initial primary antibody. Sections were then incubated for 1 hour at room temperature with a biotinylated secondary antibody followed by avidin conjugated with either Alexa Fluor 488 or Alexa Fluor 555 (Invitrogen). This protocol (beginning with blocking procedures) was repeated for secondary antigen detection.
Apolipoprotein E genotyping was conducted on 11 of the 12 athletes using restriction isotyping for determining apolipoprotein E isoforms based on brain tissue samples.
RESULTS
Clinical Data
At death, the 12 athletes who developed CTE ranged in age from 42 to 85 years (mean, 65.4 years; SD, 15.9 years) and included 7 former football players (6 of whom played professionally and 1 in college), 4 retired professional boxers, and 1 professional hockey player (Tables 1 and 2). The 3 athletes who developed clinically diagnosed MND included 2 retired professional football players and a former professional boxer. The players with CTE + MND did not differ from the 9 athletes with CTE–no MND with respect to age at death, total years of participation in the sport, age at retirement from the sport, or concussion histories (data not shown).
TABLE 1.
Clinical Data on the Athletes With Chronic Traumatic Encephalopathy and Motor Neuron Disease
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age at death, years | 66 | 49 | 67 |
| Cause of death | Respiratory insufficiency | Respiratory insufficiency | Cardiac arrhythmia |
| Sports history | |||
| Sport played | Football | Football | Boxing |
| Total years played | 27 | 16 | 10 |
| Years as a professional | 16 | 3 | 10 |
| Age at retirement from sport, years | 37 | 36 | 22 |
| Concussion history | |||
| No. reported | >10 | 3–4 | “Many” |
| Cervical spine injury history | |||
| No. reported | Multiple | 0 | 0 |
| Substance history | |||
| Alcohol abuse | 0 | 0 | + in youth |
| Illicit drug use | 0 | 0 | 0 |
| Family history | |||
| ALS | 0 | 0 | Sibling with probable ALS |
| Dementia | 0 | Paternal grandmother with AD | 0 |
| Motor neuron symptoms | |||
| Age at onset, years | 64 | 47 | 67 |
| Initial motor symptoms | Weakness of neck flexion, finger extension | Right arm and hand weakness, hyperactive DTRs, diffuse fasciculations | Hypophonic speech, drooling, severe atrophy of shoulder girdles and arms, diffuse fasciculations |
| New symptoms 6 months after onset | Slurred spastic speech, decreased walking | Slow, slurred speech, swallowing difficulty, excessive emotionality, tongue weakness, slow gait, numerous falls, respiratory difficulty | Progressive muscular atrophy and speech impairment |
| Clinical diagnosis | |||
| ALS | ALS | Atypical ALS with dementia | |
| Cognitive and behavioral changes | |||
| Cognitive symptoms | Cognitive impairment | None | Dementia |
| Age at symptom onset, years | 56 | NA | 64 |
| Depression | 0 | ++ | 0 |
| Outbursts of anger or aggression, “short fuse” | 0 | + | +++ |
| Apathy | +++ | 0 | 0 |
0, absent; +, mild; ++, moderate; +++, severe.
AD, Alzheimer disease; ALS, amyotrophic lateral sclerosis; DTR, deep tendon reflexes; NA, not applicable.
TABLE 2.
Demographic and Immunocytochemical Characteristics of the 12 Chronic Traumatic Encephalopathy Cases
| Case | Demographics |
Tau Immunoreactivity |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MND | Age, Years | Sex | Sport | Race | APOE | Spinal Cord | Brainstem | Diencephalon | Basal Ganglia | Medial Temporal Lobe | Frontal, Insular, and Temporal Cortex | Aβ | |
| 1* | Yes | 66 | M | PFB | C | 2/3 | +++ | +++ | +++ | ++ | +++ | +++ | 0 |
| 2* | Yes | 49 | M | PFB | AA | 3/4 | + | ++ | + | + | + | + | + |
| 3* | Yes | 67 | M | PB | C | 3/3 | +++ | +++ | +++ | +++ | +++ | +++ | + |
| 4† | No | 73 | M | PB | C | 3/3 | + | +++ | +++ | +++ | +++ | +++ | 0 |
| 5† | No | 82 | M | PFB | C | 3/3 | + | +++ | +++ | ++ | +++ | +++ | 0 |
| 6* | No | 75 | M | PH | C | 3/4 | ++ | +++ | ++ | ++ | ++ | ++ | ++ |
| 7* | No | 85 | M | PFB | C | 3/3 | + | + | + | + | +++ | +++ | ++ |
| 8† | No | 80 | M | PB | AA | 3/4 | + | +++ | + | + | +++ | +++ | ++ |
| 9† | No | 76 | M | PB | AA | NA | NA | +++ | + | + | +++ | ++ | ++ |
| 10‡ | No | 42 | M | PFB | C | 3/3 | NA | + | + | + | ++ | +++ | 0 |
| 11‡ | No | 45 | M | PFB | C | 4/4 | NA | + | + | + | ++ | +++ | 0 |
| 12‡ | No | 45 | M | PFB | C | 4/4 | NA | + | + | + | ++ | +++ | + |
Entire spinal cord studied.
Cervical spinal cord only studied.
No spinal cord tissue available for study.
Tau immunoreactivity rated on a semiquantitative 0–3 scale: 0, absent; +, mild; ++, moderate; +++, severe; NA, data not available; Aβ, β-amyloid; M, male; MND, motor neuron disease; APOE, apolipoprotein E; PFB, professional football; PB, professional boxing; PH, professional hockey; C, white; AA, African American.
The 3 athletes with CTE + MND had clinical presentations characterized by profound muscle weakness, muscle atrophy, spasticity, and diffuse fasciculations (Table 1). Two developed motor symptoms after the development of cognitive impairment or dementia and behavioral changes; one developed parkinsonism in addition to dementia, behavioral changes, and MND; and one developed prominent symptoms of MND in the presence of behavioral changes and depression but without evidence of cognitive decline or parkinsonism. In all 3, the MND began with bilateral involvement of the shoulder girdles, neck, and arms, involved the bulbar musculature early in the disease course, and resulted in death within 2 to 3 years (see data, Supplemental Digital Content 1, http://links.lww.com/NEN/A161 for case summaries).
Pathological Aspects
Athletes With CTE Without MND
Microscopically, the brains of all 9 athletes with CTE–no MND showed the pathological changes of CTE, consisting of numerous tau-positive NFTs, neuropil neurites, and astrocytic tangles in the frontal, temporal, and insular cortices, diencephalon, basal ganglia, and brainstem (Fig. 1). Of the 5 cases with spinal cord tissue available for study, all 5 demonstrated occasional tau-immunoreactive neurites and NFTs in the posterior, lateral, and/or anterior horns of the spinal cord; 7 of the 9 also showed extensive TDP-43 immunoreactivity. The TDP-43–positive short threadlike and ring-shaped neurites (RNs), filamentous neuronal inclusions (FNIs), and ring-shaped glial inclusions (RGIs) were found in the frontal and temporal cortex and insula (Table 3, Figs. 1–3). The TDP-43–positive RNs and RGIs were frequent in the subcortical white matter, and TDP-43–positive FNIs and RNs were common in the brainstem, including the substantia nigra pars compacta, oculomotor, inferior olivary, dorsal medullary, and hypoglossal nuclei (Fig. 3). The TDP-43–positive neurites were found in the amygdala, hippocampus, caudate, putamen, thalamus, and hypothalamus (not shown). Double immunostaining and confocal microscopy showed that the great majority of the TDP-43–positive neurites and inclusions were not tau positive (Figs. 1, 2, 4). In the brain that showed the least TDP-43 immunoreactivity (Case 10), RNs were limited to the substantia nigra. Ubiquitin-positive or TDP-43–positive inclusions were not found in the dentate gyrus in any case of CTE; a few cases had rare TDP-43–positive neurites in the dentate gyrus (Table 3).
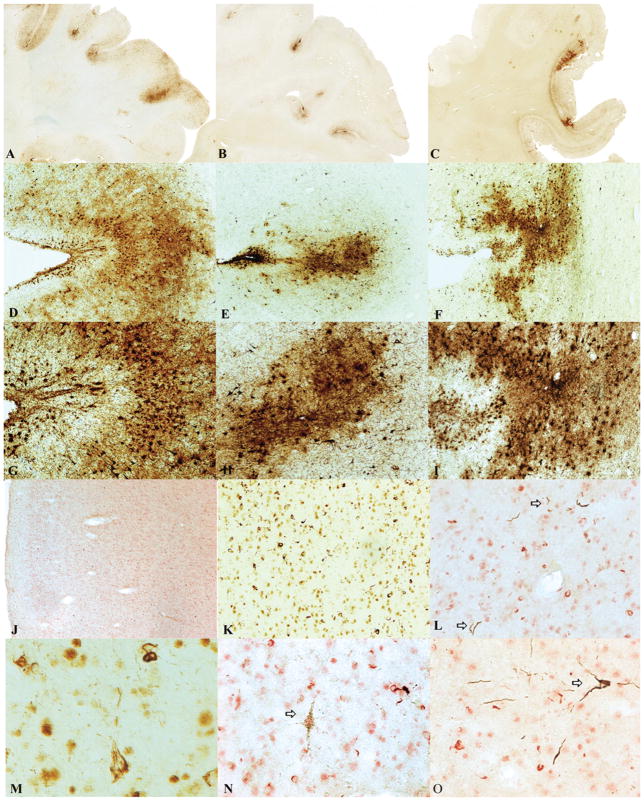
FIGURE 1.
Cases of chronic traumatic encephalopathy (CTE) with widespread TAR DNA-binding protein of approximately 43 kd (TDP-43) immunoreactivity and motor neuron disease (CTE + MND). (A–C) Tau-immunoreactive neurofibrillary degeneration in the frontal cortex of the 3 cases of CTE + MND (whole-mount 50-μm sections immunostained for CP13, original magnification: 1×). (D–I) Tau-positive neurofibrillary tangles, glial tangles, and neuropil neurites are particularly dense at the depth of the cortical sulci, CP13 immunostain, original magnification: (D–F) 50×; (G–I) 100×. (J) TDP-43 immunostaining reveals abundant TDP-positive pathology in all cortical layers in the frontal cortex of Case 1, original magnification: 50×. (K) Numerous TDP-43–positive ring-shaped neurites (RNs) and ring-shaped glial inclusions (RGIs) in the frontal cortex of Case 2, original magnification: 200×. (L) Double immunostaining shows that most TDP-43–positive RNs and RGIs (red) are not colocalized with tau-positive neurites (PHF-1 brown, arrows), original magnification: 400×. (M) TDP-43–positive filamentous neuronal inclusions, original magnification: 600×. (N) Double immunostaining shows a tau-positive pretangle (PHF-1 brown, arrow) that is not associated with TDP-43 immunoreactivity (red), original magnification: 400×. (O) Double immunostaining shows a tau-positive tangle (PHF-1, arrow) that is not associated with TDP-43 immunoreactivity (red), original magnification: 400×.
TABLE 3.
TDP-43 Immunoreactivity in the 12 Athletes With Chronic Traumatic Encephalopathy
| Case | MND | TDP-43 Immunoreactivity |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Spinal Cord | Medulla | Midbrain | Basal Ganglia | Diencephalon | Frontal Cortex | Rolandic Cortex | Insula | Temporal Cortex | Subcortical White Matter | Medial Temporal Lobe | Dentate Gyrus | ||
| 1* | Yes | +++ | ++ | +++ | + | ++ | ++ | +++ | ++ | ++ | ++ | ++ | 0 |
| 2* | Yes | +++ | ++ | +++ | + | ++ | ++ | +++ | ++ | ++ | ++ | ++ | 0 |
| 3* | Yes | ++ | + | +++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ | r |
| 4† | No | + | + | +++ | ++ | ++ | + | + | + | + | +++ | ++ | r |
| 5† | No | 0 | + | + | + | ++ | ++ | ++ | ++ | +++ | + | + | r |
| 6* | No | 0 | + | 0 | + | 0 | 0 | 0 | 0 | 0 | 0 | ++ | 0 |
| 7* | No | 0 | 0 | + | 0 | 0 | + | + | + | +++ | + | + | 0 |
| 8† | No | 0 | + | + | ++ | + | + | + | + | + | + | ++ | r |
| 9† | No | NA | ++ | ++ | + | + | 0 | 0 | 0 | 0 | 0 | + | 0 |
| 10‡ | No | NA | NA | + | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 11‡ | No | NA | NA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 12‡ | No | NA | NA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Entire spinal cord studied.
Cervical spinal cord only studied.
No spinal cord tissue available for study.
TDP-43 immunoreactivity rated on a semiquantitative 0–4 scale: 0, absent; r, rare; +, mild; ++, moderate; +++, severe; NA, data not available; MND, motor neuron disease.
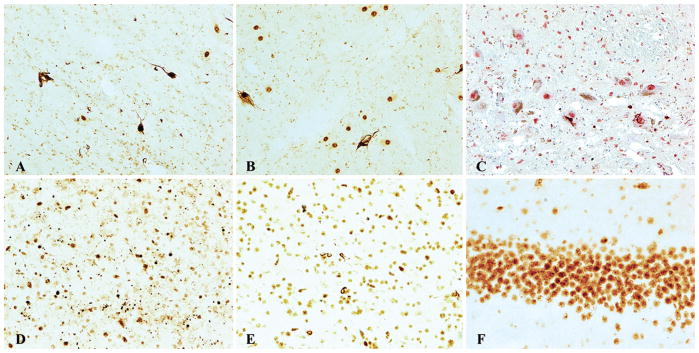
FIGURE 3.
TAR DNA-binding protein of approximately 43 kd (TDP-43) immunoreactivity in chronic traumatic encephalopathy (CTE). TDP-43 immunoreactivity is found as glial cytoplasmic inclusions (GCIs) and neuropil neurites in multiple brainstem nuclei including hypoglossal nucleus (A), oculomotor nucleus (B), substantia nigra (C) (original magnification: 200×). TDP-43 immunoreactivity in the medial temporal lobe structures consists primarily of dotlike neurites. (D) Hippocampus, CA1 (original magnification: 200×). TDP-43–positive dystrophic neurites and GCIs are also found in white matter. (E) Subcortical frontal white matter (original magnification: 200×). No ubiquitinated or TDP-43–positive inclusions are found in the dentate gyrus of the hippocampus. (F) Dentate gyrus of the hippocampus (original magnification: 400×).
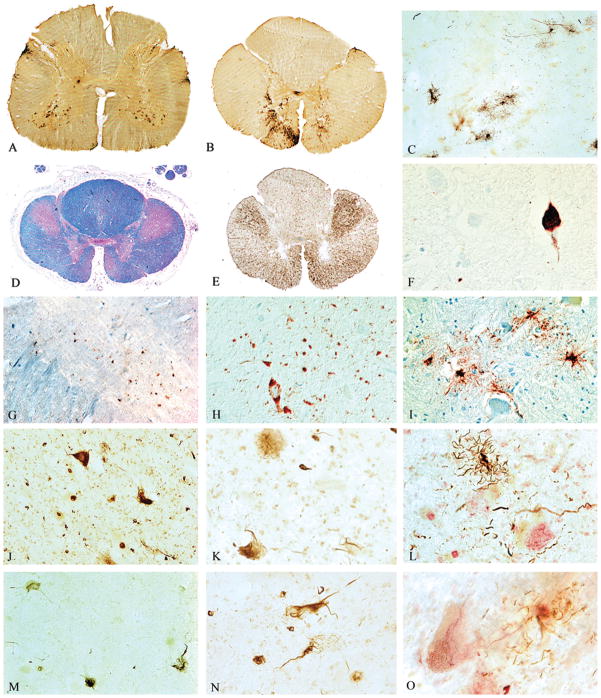
FIGURE 2.
Spinal cord pathology in chronic traumatic encephalopathy (CTE) with TAR DNA-binding protein of approximately 43 kd (TDP-43) proteinopathy, tauopathy, and motor neuron disease (CTE + MND). (A, B) Whole-mount 50-μm sections of lumbar and thoracic spinal cord immunostained with antibody AT8 showing abundant tau immunostaining in the ventral horns. (C) Tau-positive astrocytic tangles in the ventral horn of Case 1 (AT8 immunostain, original magnification: 100×). (D) Whole-mount 10-μm section through high thoracic spinal cord showing marked myelin and axonal loss in the lateral and ventral corticospinal tracts. Atrophic ventral roots are not visible. Luxol fast blue hematoxylin and eosin stain, original magnification: 1×. (E) Whole-mount 50-μm section of high thoracic cord showing intense immunoreactivity for activated microglia and macrophages in lateral and corticospinal tracts (LN-3 immunostain, original magnification: 1×). (F) Tau-positive neurofibrillary tangles in ventral horn of Case 3, AT8 immunostain, original magnification: 600×. (G) TDP-43 immunoreactivity in ventral horn, original magnification: 50×. (H) TDP-43 immunoreactive filamentous neuronal inclusions (FNIs), ring-shaped glial inclusions (RGIs), and ring-shaped neurites (RNs) in the ventral horns of the lumbar spinal cord in Case 3, original magnification: 200×. (I) Tau-positive astrocytes and their processes surrounding degenerating anterior horn cells in the thoracic spinal cord (AT8 immunostain, original magnification: 350×). (J) TDP-43–positive FNIs, RGIs, and RNs in the ventral horns of the lumbar spinal cord in Case 2, original magnification: 200×. (K) TDP-43–positive FNI in the anterior horn, original magnification: 400×.(L) Double immunostained sections show tau-positive astrocytes (brown) and their processes surrounding anterior horn neurons containing TDP-43–positive filamentous inclusions (red), PHF-1 and TDP-43 immunostains, original magnification: 400×. (M) TDP-43–positive FNIs, RGIs, and RNs in the lumbar ventral horns in Case 1, original magnification: 200×. (N) TDP-43–positive FNIs in the anterior horn, original magnification: 400×. (O) Double immunostained sections showing tau-positive astrocytes (brown) and their processes surrounding anterior horn neurons containing TDP-43–positive FNIs (red), PHF-1 and TDP-43 immunostains, original magnification: 600×.
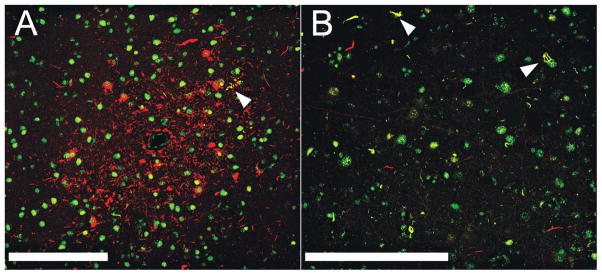
FIGURE 4.
Limited colocalization of tau and TAR DNA-binding protein of approximately 43 kd (TDP-43). (A, B) Laser scanning confocal microscopy was carried out on sections from the frontal cortex of Case 1 (A) and Case 2 (B). Sections were double immunostained for TDP-43 (green) and PHF-1 (red). Areas of colocalization appear yellow. In (A), there are abundant tau-positive neurites around a small blood vessel; white arrowhead indicates a small cluster of tau-positive neurites that seem to be colocalized with TDP-43. (B) Many TDP-43–positive neurites (green) and a few tau-positive neurites (red). Most neurites do not seem to be colocalized, but arrowheads point to occasional colocalized intraneuronal inclusions and neurites. White bars = 200 μm.
Athletes With CTE and MND
The macroscopic features of the brains and spinal cords of the athletes with CTE + MND did not differ from those with CTE–no MND, except for atrophy of the ventral roots of the spinal cord. All 3 brains showed the characteristic microscopic findings of CTE (Fig. 1). The 2 athletes with cognitive impairment or dementia and MND (Cases 1 and 3) had advanced CTE with dense NFTs throughout the medial temporal lobe structures, neocortex, olfactory bulb, substantia nigra, locus caeruleus, mammillary body, hypothalamus, and periventricular regions. Betz cells in the precentral gyrus also bore tau-immunoreactive NFTs. Case 2 displayed milder CTE, with involvement primarily limited to the frontal cortex, diencephalon, and brainstem. Abundant TDP-43–positive RNs, FNIs, and RGIs were found in widespread regions of the brain and spinal cord in all 3 CTE + MND brains, generally in a far greater density than that found in the CTE–no MND brains. In the cortex, TDP-43–positive pathology was found throughout all cortical laminae and was most prominent in the motor cortex (Fig. 1).
In Cases 1 and 2 (both of whom developed end-stage MND with severe respiratory insufficiency and muscular weakness in the final months of their lives), the medullary pyramids and lateral corticospinal tracts throughout the spinal cord showed marked myelin and axonal loss with astrocytosis. Loss of anterior horn cells was profound, and there was marked atrophy and gliosis of ventral roots (Fig. 2). In Case 3 (whose motor neuron symptoms were not as severe), there was only mild degeneration of the lateral corticospinal tracts and ventral root atrophy. Staining with LN-3 showed numerous activated microglia and macrophages throughout the brain and spinal cord, most intense in the lateral corticospinal tracts of the cord. Anterior horn cells were markedly reduced in number in Cases 1 and 2 and moderately reduced in number in Case 3. Tau-positive neurites, astrocytic tangles, and NFTs were found in the posterior, lateral, and ventral horns, most frequently in Cases 1 and 3 where numerous astrocytic tangles surrounded degenerating anterior horn cells (Fig. 2; Table 3). In the remaining anterior horn cells in all 3 cases, there were frequent TDP-43–positive tau-negative FNIs, RNs, and RGIs (Figs. 2 and 4).
Normal Control Cases
Sections from the cervical, thoracic, and lumbar spinal cord of 12 neurologically normal controls ranging in age from 53 to 84 years (mean, 66.0 years; SD, 10.6 years), 9 men and 3 women, were examined. Rare tau-positive neurites were found in the ventral horn of 4 cases, primarily in the cervical cord; no tau-positive NFTs or astrocytic tangles were observed. There was no TDP-43 immunoreactivity in any case.
Sporadic ALS Cases
Sections from cervical, thoracic, and lumbar spinal cord in 12 age-matched men with sporadic ALS, ranging in age from 45 to 77 years (mean, 64.3 years; SD, 9.5 years) were examined. Rare tau-positive neurites were found in 1 of 12 cases of sporadic ALS. Immunoreactivity for TDP-43 was present in every ALS case and ranged from TDP-43–positive threadlike and curved neurites to abundant short skeinlike inclusions or punctate neuronal cytoplasmic immunoreactivity within the remaining anterior horn cells.
DISCUSSION
We report a widespread TDP-43 proteinopathy in more than 80% of our cases of CTE that involved the brainstem, basal ganglia, diencephalon, medial temporal lobe, frontal, temporal, and insular cortices, and subcortical white matter in most cases. Moreover, in 3 athletes with CTE who developed a progressive MND several years before death, there were extensive TDP-43–positive FNIs, RGIs, and RNs in the anterior horns of the spinal cord in addition to tau-positive astrocytic tangles, neurites, and occasional NFTs. These findings suggest that a distinctive widespread TDP-43 proteinopathy is associated with CTE, and that in some individuals, the TDP-43 proteinopathy extends to involve the spinal cord and is clinically manifest as MND.
Widespread TDP-43 immunoreactivity has been previously reported in CTE (52). The shared presence of 2 aggregated phosphorylated proteins associated with neurodegeneration in the great majority of cases argues against the coincidental occurrence of CTE and sporadic ALS, suggesting instead that a common stimulus provokes the pathological accumulation of both proteins. In CTE cases with mild TDP-43 immunoreactivity, TDP-43–immunoreactive RGIs and RNs were found in the midbrain, medulla, basal ganglia, and medial temporal lobe; and in the least affected case of CTE, TDP-43–positive RNs were limited to the substantia nigra. Occasional TDP-43–positive RNs were found in the spinal cord of Case 4, a 73-year-old former professional boxer with severe end-stage CTE but with no recognized symptoms of motor neuron dysfunction, and Case 8, a former professional hockey player with advanced CTE.
Frontotemporal lobar degeneration is also associated with MND and TDP-43 immunoreactivity, although FTLD-TDP 43/MND is characterized by neuronal inclusions that are immunoreactive for ubiquitin but not tau (FTLD with tau-negative ubiquitin-positive inclusions), and there are no tau-immunoreactive NFTs, astrocytic tangles, or neurites (59). Conversely, the TDP-43 positivity found in CTE is associated with an extensive tauopathy, and none of the CTE cases bore any ubiquitin or TDP-43–positive inclusions in the dentate gyrus. Moreover, the morphology and cortical distribution of TDP-43–positive RNs, FGIs, and RGIs in CTE seem to be distinct.
In CTE + MND, tau-positive NFTs, astrocytic tangles, and neurites are also found in the spinal cord. No tau-immunoreactive NFTs were found in our cases of sporadic ALS, and none have been described in the literature (60, 61). Rare tau NFTs have been described in the spinal cord from individuals with sporadic AD, but we found none in the spinal cord from age-matched controls (60, 61).
The TDP-43 is a highly conserved protein that is widely expressed in many tissues, including the CNS. Its physiological functions are diverse and incompletely understood but likely involve the regulation of multiple biological processes via TDP-43 binding to DNA, RNA, and other proteins. Originally, TDP-43 was thought to be specific to FTLD-TDP, ALS-D/FTLD-MND, and ALS, but it is now recognized in a variety of other disorders in which it is present to a lesser degree and considered a secondary pathology. The major TDP-43 proteinopathies, FTLD-TDP, FTLD-MND/ALS-D, and ALS, once thought to be discrete clinical and pathological subtypes, have more recently been considered to represent different points on a continuous spectrum of a multisystem degeneration. The FTLD-TDP, FTLD-MND/ALS-D, and ALS all show widespread CNS TDP-43 pathology; however, the presence of MND or ALS is associated with a higher burden of inclusions in lower motor neurons, and cognitive dysfunction is related to a higher degree of cortical pathology (6, 62).
Diseases with secondary TDP-43 pathology include AD and hippocampal sclerosis (63), Guam parkinsonism-dementia complex (PDC) (64), Pick disease, corticobasal degeneration, argyrophilic grain disease, and Lewy body disease (5, 28, 65). CTE is a 3R/4R tauopathy; when TDP-43 has been reported in other 3R/4R tauopathies, such as AD and Guam PDC, it may be seen in neurons with NFTs. We also found a minor degree of colocalization of TDP-43 and tau; however, the majority of TDP-43–positive inclusions were in discrete structures. In AD, TDP-43 immunoreactivity is limited primarily to the medial temporal lobe, except in advanced stages (i.e. Braak V or VI) in which it may be found in the neocortex and basal ganglia (52).
Neuropathologically, the tau neurofibrillary degeneration of CTE most resembles that in Guam PDC (60), although the patchy irregular involvement of the cortex and the perivascular distribution of dense NFTs distinguish CTE from Guam PDC. In Guam PDC, TDP-43–positive neurites are found in the frontal subcortical white matter and cortex, and neuronal cytoplasmic inclusions are found in the dentate gyrus of the medial temporal lobe (64). Although the pathogenesis of Guam PDC is unknown, environmental factors, such as toxins in cycad seeds, minerals in the soil or drinking water, and genetic susceptibility have been implicated (66). Guam PDC might be another example of an environmentally acquired tauopathy and TDP-43 proteinopathy that is associated with cognitive impairment, parkinsonism, and, in some instances, MND.
Recent work using in vitro and in vivo animal models indicates that overexpression of wild-type human TDP-43 and its dislocation from the neuronal nucleus to the cytoplasm are associated with neurodegeneration and cell death (67). Injections of viral wild-type human TDP-43 constructs in the substantia nigra of rats caused loss of substantia nigra neurons, gliosis, and altered behavior (68). Transgenic Drosophila overexpressing human TDP-43 in motor neurons developed axonal swelling, reduction in axonal branches, and motor neuron loss. Similarly, transgenic mice overexpressing TDP-43 in spinal and cortical motor neurons were reported to develop a dose-dependent degeneration of cortical and spinal motor neurons, nonmotor cortical and subcortical neurons, and spastic quadriplegia reminiscent of ALS (69).
During a traumatic brain injury, the brain and spinal cord undergo shear deformation, producing a transient elongation or stretch of axons. Traumatic axonal injury also perturbs the cytoskeleton, causing dissolution of microtubules and neurofilaments and pathological reorganization of neurofilament proteins (70). By virtue of its capacity to bind to neurofilament mRNA and stabilize the mRNA transcript (71), TDP -43 plays a critical role in mediating the response of the neuronal cytoskeleton to axonal injury. Models of traumatic brain injury in rodents show the accumulation of many key proteins that form pathological aggregates in human neurodegenerative diseases, including neurofilament proteins, amyloid precursor protein, α-synuclein, and tau (72). The TDP-43 is intrinsically prone to aggregation, and TDP-43 expression is upregulated after experimental axotomy in spinal motor neurons of the mouse (73). Conceivably, traumatic axonal injury may also accelerate TDP-43 accumulation, aggregation, and dislocation to the cytoplasm and thereby enhance its neurotoxicity.
There are multiple other biological mechanisms by which repetitive head injury trauma may trigger the molecular pathways leading to neuronal degeneration in CTE and CTE + MND, including inflammation, glutamate excitotoxicity, and oxidative stress. Their contributions to the molecular cascades in CTE remain to be explored. Additional studies are clearly necessary to understand the specific additional risk factors (including genetic), pathogenesis, and potential for therapeutic intervention in CTE and CTE + MND. The existence of a long period of latency between the traumatic injury and the onset of CTE or MND increases the window for implementing therapeutic measures to dampen or block the neurodegenerative cascade triggered by such injuries.
This report suggests that the play of contact sports, including boxing, football, and hockey, might be associated with a widespread TDP-43 proteinopathy that, in some individuals, is manifest as MND. The accumulation of TDP-43 as well as tau in the neocortex, medal temporal lobes, and deeper brain structures likely contributes to the overall clinical manifestations of cognitive and memory loss, behavioral changes, and parkinsonism. Whether repetitive head trauma alone provokes these neurodegenerative cascades or only in association with certain genetic constellations remains to be determined.
Supplementary Material
Acknowledgments
The authors thank the families for their generous participation in this study.
This study was supported by the Boston University Alzheimer’s Disease Center NIA P30 AG13846, supplement 0572063345-5; the Mount Sinai Alzheimer’s Disease Research Center Grants P50AG05138 and P01AG02219; the Massachusetts Alzheimer’s Disease Research Center Grant P50AG05134; the VA Biorepository (CSP 501), funded by the Department of Veterans Affairs; the Sports Legacy Institute; the National Operating Committee on Standards for Athletic Equipment; and by an unrestricted gift from the National Football League. The authors acknowledge the use of resources and facilities at the Edith Nourse Rogers Memorial Veterans Hospital in Bedford, Massachusetts.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.jneuropath.com).
References
- 1.Bruijn LI, Miller TM, Cleveland DW. Unraveling the mechanisms involved in motor neuron degeneration in ALS. Annu Rev Neurosci. 2004;27:723–49. doi: 10.1146/annurev.neuro.27.070203.144244. [DOI] [PubMed] [Google Scholar]
- 2.Mulder DW, Kurland LT, Offord KP, et al. Familial adult motor neuron disease: Amyotrophic lateral sclerosis. Neurology. 1986;36:511–17. doi: 10.1212/wnl.36.4.511. [DOI] [PubMed] [Google Scholar]
- 3.Okamoto K, Murakami N, Kusaka H, et al. Ubiquitin-positive intraneuronal inclusions in the extramotor cortices of presenile dementia patients with motor neuron disease. J Neurol. 1992;239:426–30. doi: 10.1007/BF00856806. [DOI] [PubMed] [Google Scholar]
- 4.Wightman G, Anderson VE, Martin J, et al. Hippocampal and neocortical ubiquitin-immunoreactive inclusions in amyotrophic lateral sclerosis with dementia. Neurosci Lett. 1992;139:269–74. doi: 10.1016/0304-3940(92)90569-s. [DOI] [PubMed] [Google Scholar]
- 5.Dickson DW. Neuropathology of non-Alzheimer degenerative disorders. Int J Clin Exp Pathol. 2009;3:1–23. [PMC free article] [PubMed] [Google Scholar]
- 6.Geser F, Martinez-Lage M, Kwong LK, et al. Amyotrophic lateral sclerosis, frontotemporal dementia and beyond: The TDP-43 diseases. J Neurol. 2009;256:1205–14. doi: 10.1007/s00415-009-5069-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kondo K, Tsubaki T. Case-control studies of motor neuron disease: Association with mechanical injuries. Arch Neurol. 1981;38:220–26. doi: 10.1001/archneur.1981.00510040046007. [DOI] [PubMed] [Google Scholar]
- 8.Deapen DM, Henderson BE. A case-control study of amyotrophic lateral sclerosis. Am J Epidemiol. 1986;123:790–99. doi: 10.1093/oxfordjournals.aje.a114308. [DOI] [PubMed] [Google Scholar]
- 9.Chen H, Richard M, Sandler DP, et al. Head injury and amyotrophic lateral sclerosis. Am J Epidemiol. 2007;166:810–16. doi: 10.1093/aje/kwm153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Binazzi A, Belli S, Uccelli R, et al. An exploratory case-control study on spinal and bulbar forms of amyotrophic lateral sclerosis in the province of Rome. Amyotroph Lateral Scler. 2009;10:361–69. doi: 10.3109/17482960802382313. [DOI] [PubMed] [Google Scholar]
- 11.Kurtzke JF, Beebe GW. Epidemiology of amyotrophic lateral sclerosis: 1. A case-control comparison based on ALS deaths. Neurology. 1980;30:453–62. doi: 10.1212/wnl.30.5.453. [DOI] [PubMed] [Google Scholar]
- 12.Gawel M, Zaiwalla Z, Rose FC. Antecedent events in motor neuron disease. J Neurol Neurosurg Psychiatry. 1983;46:1041–43. doi: 10.1136/jnnp.46.11.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Strickland D, Smith SA, Dolliff G, et al. Physical activity, trauma, and ALS: A case-control study. Acta Neurol Scand. 1996;94:45–50. doi: 10.1111/j.1600-0404.1996.tb00038.x. [DOI] [PubMed] [Google Scholar]
- 14.Scarmeas N, Shih T, Stern Y, et al. Premorbid weight, body mass, and varsity athletics in ALS. Neurology. 2002;59:773–75. doi: 10.1212/wnl.59.5.773. [DOI] [PubMed] [Google Scholar]
- 15.Longstreth WT, McGuire V, Koepsell TD, et al. Risk of amyotrophic lateral sclerosis and history of physical activity: A population-based case-control study. Arch Neurol. 1998;55:201–6. doi: 10.1001/archneur.55.2.201. [DOI] [PubMed] [Google Scholar]
- 16.Chiò A, Benzi G, Dossena M, et al. Severely increased risk of amyotrophic lateral sclerosis among Italian professional football players. Brain. 2005;128:472–76. doi: 10.1093/brain/awh373. [DOI] [PubMed] [Google Scholar]
- 17.Belli S, Vanacore N. Proportionate mortality of Italian soccer players: Is amyotrophic lateral sclerosis an occupational disease? Eur J Epidemiol. 2005;20:237–42. doi: 10.1007/s10654-004-6879-7. [DOI] [PubMed] [Google Scholar]
- 18.Kamel F, Umbach DM, Munsat TL, et al. Association of cigarette smoking with amyotrophic lateral sclerosis. Neuroepidemiology. 1999;18:194–202. doi: 10.1159/000026211. [DOI] [PubMed] [Google Scholar]
- 19.Nelson LM, McGuire V, Longstreth WT, et al. Population-based case-control study of amyotrophic lateral sclerosis in western Washington state. I. Cigarette smoking and alcohol consumption. Am J Epidemiol. 2000;151:156–63. doi: 10.1093/oxfordjournals.aje.a010183. [DOI] [PubMed] [Google Scholar]
- 20.Weisskopf MG, McCullough ML, Calle EE, et al. Prospective study of cigarette smoking and amyotrophic lateral sclerosis. Am J Epidemiol. 2004;160:26–33. doi: 10.1093/aje/kwh179. [DOI] [PubMed] [Google Scholar]
- 21.Campbell AM, Williams ER, Barltrop D. Motor neurone disease and exposure to lead. J Neurol Neurosurg Psychiatry. 1970;33:877–85. doi: 10.1136/jnnp.33.6.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Armon C, Kurland LT, Daube JR, et al. Epidemiologic correlates of sporadic amyotrophic lateral sclerosis. Neurology. 1991;41:1077–84. doi: 10.1212/wnl.41.7.1077. [DOI] [PubMed] [Google Scholar]
- 23.Chancellor AM, Slattery JM, Fraser H, et al. Risk factors for motor neuron disease: A case-control study based on patients from the Scottish Motor Neuron Disease Register. J Neurol Neurosurg Psychiatry. 1993;56:1200–6. doi: 10.1136/jnnp.56.11.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McGuire V, Longstreth WT, Nelson LM, et al. Occupational exposures and amyotrophic lateral sclerosis. A population-based case-control study. Am J Epidemiol. 1997;145:1076–88. doi: 10.1093/oxfordjournals.aje.a009070. [DOI] [PubMed] [Google Scholar]
- 25.Kamel F, Umbach DM, Munsat TL, et al. Lead exposure and amyotrophic lateral sclerosis. Epidemiology. 2002;13:311–19. doi: 10.1097/00001648-200205000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Felmus MT, Patten BM, Swanke L. Antecedent events in amyotrophic lateral sclerosis. Neurology. 1976;26:167–72. doi: 10.1212/wnl.26.2.167. [DOI] [PubMed] [Google Scholar]
- 27.Pierce-Ruhland R, Patten BM. Repeat study of antecedent events in motor neuron disease. Ann Clin Res. 1981;13:102–7. [PubMed] [Google Scholar]
- 28.Gresham LS, Molgaard CA, Golbeck AL, et al. Amyotrophic lateral sclerosis and occupational heavy metal exposure: A case-control study. Neuroepidemiology. 1986;5:29–38. doi: 10.1159/000110810. [DOI] [PubMed] [Google Scholar]
- 29.Haynal A, Regli F. Amyotrophic lateral sclerosis associated with accumulated electric injury [In German] Confin Neurol. 1964;24:189–98. [PubMed] [Google Scholar]
- 30.Savettieri G, Salemi G, Arcara A, et al. A case-control study of amyotrophic lateral sclerosis. Neuroepidemiology. 1991;10:242–45. doi: 10.1159/000110279. [DOI] [PubMed] [Google Scholar]
- 31.Majoor-Krakauer D, Willems PJ, Hofman A. Genetic epidemiology of amyotrophic lateral sclerosis. Clin Genet. 2003;63:83–101. doi: 10.1046/j.0009-9163.2002.00001.x. [DOI] [PubMed] [Google Scholar]
- 32.Schmidt S, Kwee LC, Allen KD, et al. Association of ALS with head injury, cigarette smoking and APOE genotypes. J Neurol Sci. 2010;291:22–29. doi: 10.1016/j.jns.2010.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fleminger S, Oliver DL, Lovestone S, et al. Head injury as a risk factor for Alzheimer’s disease: The evidence 10 years on; a partial replication. J Neurol Neurosurg Psychiatry. 2003;74:857–62. doi: 10.1136/jnnp.74.7.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mortimer JA, French LR, Hutton JT, et al. Head injury as a risk factor for Alzheimer’s disease. Neurology. 1985;35:264–67. doi: 10.1212/wnl.35.2.264. [DOI] [PubMed] [Google Scholar]
- 35.O’Meara ES, Kukull WA, Sheppard L, et al. Head injury and risk of Alzheimer’s disease by apolipoprotein E genotype. Am J Epidemiol. 1997;146:373–84. doi: 10.1093/oxfordjournals.aje.a009290. [DOI] [PubMed] [Google Scholar]
- 36.Mehta KM, Ott A, Kalmijn S, et al. Head trauma and risk of dementia and Alzheimer’s disease: The Rotterdam Study. Neurology. 1999;53:1959–62. doi: 10.1212/wnl.53.9.1959. [DOI] [PubMed] [Google Scholar]
- 37.Katzman R, Galasko DR, Saitoh T, et al. Apolipoprotein-epsilon4 and head trauma: Synergistic or additive risks? Neurology. 1996;46:889–91. [PubMed] [Google Scholar]
- 38.Mayeux R, Ottman R, Maestre G, et al. Synergistic effects of traumatic head injury and apolipoprotein-epsilon 4 in patients with Alzheimer’s disease. Neurology. 1995;45:555–57. doi: 10.1212/wnl.45.3.555. [DOI] [PubMed] [Google Scholar]
- 39.Plassman BL, Havlik RJ, Steffens DC, et al. Documented head injury in early adulthood and risk of Alzheimer’s disease and other dementias. Neurology. 2000;55:1158–66. doi: 10.1212/wnl.55.8.1158. [DOI] [PubMed] [Google Scholar]
- 40.Bower JH, Maraganore DM, Peterson BJ, et al. Head trauma preceding PD: A case-control study. Neurology. 2003;60:1610–15. doi: 10.1212/01.wnl.0000068008.78394.2c. [DOI] [PubMed] [Google Scholar]
- 41.Goldman SM, Tanner CM, Oakes D, et al. Head injury and Parkinson’s disease risk in twins. Ann Neurol. 2006;60:65–72. doi: 10.1002/ana.20882. [DOI] [PubMed] [Google Scholar]
- 42.Erb W. Zur Casuistik der bulbären Lähmungen: Über einen neuen wahrscheinlich bulbären Lähmungscomplex. Eur Arch Psychiatry Clin Neurosci. 1879;9:325–50. [Google Scholar]
- 43.Hanisch R, Dworsky RL, Henderson BE. Letter: A search for clues to the cause of amyotrophic lateral sclerosis. Arch Neurol. 1976;33:456–57. doi: 10.1001/archneur.1976.00500060062015. [DOI] [PubMed] [Google Scholar]
- 44.Al-Chalabi A, Leigh PN. Trouble on the pitch: Are professional football players at increased risk of developing amyotrophic lateral sclerosis? Brain. 2005;128:451–53. doi: 10.1093/brain/awh426. [DOI] [PubMed] [Google Scholar]
- 45.Abel EL. Football increases the risk for Lou Gehrig’s disease, amyotrophic lateral sclerosis. Percept Mot Skills. 2007;104:1251–54. doi: 10.2466/pms.104.4.1251-1254. [DOI] [PubMed] [Google Scholar]
- 46.Wallis C, Dorfman A. Medicine: Probing A Mysterious Cluster. [Accessed September 28, 2008];TIME.com [Web site] 1987 February 23; Available at: http://www.time.com/time/magazine/article/0,9171,963607-1,00.html.
- 47.Horner RD, Kamins KG, Feussner JR, et al. Occurrence of amyotrophic lateral sclerosis among Gulf War veterans. Neurology. 2003;61:742–49. doi: 10.1212/01.wnl.0000069922.32557.ca. [DOI] [PubMed] [Google Scholar]
- 48.Coffman CJ, Horner RD, Grambow SC, et al. Estimating the occurrence of amyotrophic lateral sclerosis among Gulf War (1990–1991) veterans using capture-recapture methods. Neuroepidemiology. 2005;24:141–50. doi: 10.1159/000083297. [DOI] [PubMed] [Google Scholar]
- 49.Weisskopf MG, O’Reilly EJ, McCullough ML, et al. Prospective study of military service and mortality from ALS. Neurology. 2005;64:32–37. doi: 10.1212/01.WNL.0000148649.17706.D9. [DOI] [PubMed] [Google Scholar]
- 50.Haley RW. Excess incidence of ALS in young Gulf War veterans. Neurology. 2003;61:750–56. doi: 10.1212/wnl.61.6.750. [DOI] [PubMed] [Google Scholar]
- 51.McKee A, Cantu R, Nowinski C, et al. Chronic traumatic encephalopathy in athletes: Progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68:709–35. doi: 10.1097/NEN.0b013e3181a9d503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.King A, Sweeney F, Bodi I, et al. Abnormal TDP-43 expression is identified in the neocortex in cases of dementia pugilistica, but is mainly confined to the limbic system when identified in high and moderate stages of Alzheimer’s disease. Neuropathology. 2010 doi: 10.1111/j.1440-1789.2009.01085.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 53.Arai T, Hasegawa M, Akiyama H, et al. TDP-43 is a component of ubiquitin-positive tau-negative inclusions in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Biochem Biophys Res Commun. 2006;351:602–11. doi: 10.1016/j.bbrc.2006.10.093. [DOI] [PubMed] [Google Scholar]
- 54.Neumann M, Sampathu DM, Kwong LK, et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314:130–33. doi: 10.1126/science.1134108. [DOI] [PubMed] [Google Scholar]
- 55.Hu WT, Josephs KA, Knopman DS, et al. Temporal lobar predominance of TDP-43 neuronal cytoplasmic inclusions in Alzheimer disease. Acta Neuropathol. 2008;116:215–20. doi: 10.1007/s00401-008-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mackenzie IR, Baborie A, Pickering-Brown S, et al. Heterogeneity of ubiquitin pathology in frontotemporal lobar degeneration. Acta Neuropathol. 2006;112:539–49. doi: 10.1007/s00401-006-0138-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sampathu DM, Neumann M, Kwong LK, et al. Pathological heterogeneity of frontotemporal lobar degeneration with ubiquitin-positive inclusions delineated by ubiquitin immunohistochemistry and novel monoclonal antibodies. Am J Pathol. 2006;169:1343–52. doi: 10.2353/ajpath.2006.060438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vonsattel JP, Aizawa H, Ge P, et al. An improved approach to prepare human brains for research. J Neuropathol Exp Neurol. 1995;54:42–56. doi: 10.1097/00005072-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 59.Cairns NJ, Bigio EH, Mackenzie IRA, et al. Neuropathologic diagnostic and nosologic criteria for frontotemporal lobar degeneration: Consensus of the Consortium for Frontotemporal Lobar Degeneration. Acta Neuropathol. 2007;114:5–22. doi: 10.1007/s00401-007-0237-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schmidt ML, Zhukareva V, Perl DP, et al. Spinal cord neurofibrillary pathology in Alzheimer disease and Guam parkinsonism-dementia complex. J Neuropathol Exp Neurol. 2001;60:1075–86. doi: 10.1093/jnen/60.11.1075. [DOI] [PubMed] [Google Scholar]
- 61.Umahara T, Hirano A, Kato S, et al. Demonstration of neurofibrillary tangles and neuropil thread-like structures in spinal cord white matter in parkinsonism-dementia complex on Guam and in Guamanian amyotrophic lateral sclerosis. Acta Neuropathol. 1994;88:180–84. doi: 10.1007/BF00294512. [DOI] [PubMed] [Google Scholar]
- 62.Geser F, Martinez-Lage M, Robinson J, et al. Clinical and pathological continuum of multisystem TDP-43 proteinopathies. Arch Neurol. 2009;66:180–89. doi: 10.1001/archneurol.2008.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Amador-Ortiz C, Lin WL, Ahmed Z, et al. TDP-43 immunoreactivity in hippocampal sclerosis and Alzheimer’s disease. Ann Neurol. 2007;61:435–45. doi: 10.1002/ana.21154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hasegawa M, Arai T, Akiyama H, et al. TDP-43 is deposited in the Guam parkinsonism-dementia complex brains. Brain. 2007;130:1386–94. doi: 10.1093/brain/awm065. [DOI] [PubMed] [Google Scholar]
- 65.Nakashima-Yasuda H, Uryu K, Robinson J, et al. Co-morbidity of TDP-43 proteinopathy in Lewy body–related diseases. Acta Neuropathol. 2007;114:221–29. doi: 10.1007/s00401-007-0261-2. [DOI] [PubMed] [Google Scholar]
- 66.Sieh W, Choi Y, Chapman NH, et al. Identification of novel susceptibility loci for Guam neurodegenerative disease: Challenges of genome scans in genetic isolates. Hum Mol Genet. 2009;18:3725–38. doi: 10.1093/hmg/ddp300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Barmada SJ, Skibinski G, Korb E, et al. Cytoplasmic mislocalization of TDP-43 is toxic to neurons and enhanced by a mutation associated with familial amyotrophic lateral sclerosis. J Neurosci. 2010;30:639–49. doi: 10.1523/JNEUROSCI.4988-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tatom JB, Wang D, Dayton R, et al. Mimicking aspects of frontotemporal lobar degeneration and Lou Gehrig’s disease in rats via TDP-43 overexpression. Mol Ther. 2009;17:607–13. doi: 10.1038/mt.2009.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wils H, Kleinberger G, Janssens J, et al. TDP-43 transgenic mice develop spastic paralysis and neuronal inclusions characteristic of ALS and frontotemporal lobar degeneration. Proc Natl Acad Sci U S A. 2010;107:3858–63. doi: 10.1073/pnas.0912417107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Serbest G, Burkhardt M, Siman R, et al. Temporal profiles of cytoskeletal protein loss following traumatic axonal injury in mice. Neurochem Res. 2007;32:2006–14. doi: 10.1007/s11064-007-9318-9. [DOI] [PubMed] [Google Scholar]
- 71.Strong MJ, Volkening K, Hammond R, et al. TDP43 is a human low molecular weight neurofilament (hNFL) mRNA-binding protein. Mol Cell Neurosci. 2007;35:320–27. doi: 10.1016/j.mcn.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 72.Uryu K, Chen XH, Martinez D, et al. Multiple proteins implicated in neurodegenerative diseases accumulate in axons after brain trauma in humans. Exp Neurol. 2007;208:185–92. doi: 10.1016/j.expneurol.2007.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Moisse K, Mepham J, Volkening K, et al. Cytosolic TDP-43 expression following axotomy is associated with caspase 3 activation in NFL−/− mice: Support for a role for TDP-43 in the physiological response to neuronal injury. Brain Res. 2009;1296:176–86. doi: 10.1016/j.brainres.2009.07.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.