Abstract
Risk assessment is a core skill in psychiatry. Risk prediction for suicide in schizophrenia is known to be complex. We undertook a systematic review of all original studies concerning suicide in schizophrenia published since 2004. We found 51 data-containing studies (from 1281 studies screened) that met our inclusion criteria, and ranked these by standardized quality criteria. Estimates of rates of suicide and risk factors associated with later suicide were identified, and the risk factors were grouped according to type and strength of association with suicide. Consensus on the lifetime risk of suicide was a rate of approximately 5%. Risk factors with a strong association with later suicide included being young, male, and with a high level of education. Illness-related risk factors were important predictors, with number of prior suicide attempts, depressive symptoms, active hallucinations and delusions, and the presence of insight all having a strong evidential basis. A family history of suicide, and comorbid substance misuse were also positively associated with later suicide. The only consistent protective factor for suicide was delivery of and adherence to effective treatment. Prevention of suicide in schizophrenia will rely on identifying those individuals at risk, and treating comorbid depression and substance misuse, as well as providing best available treatment for psychotic symptoms.
Keywords: Schizophrenia, suicide, systematic review
Introduction
People with schizophrenia are known to die much earlier (Saha et al., 2007) than expected. Up to 40% (Bushe et al., 2010) of this excess premature mortality can be attributed to suicide and unnatural deaths, with one authoritative review (Palmer et al., 2005) estimating a lifetime suicide risk of 4.9% for people with schizophrenia. Detection of those at risk is clinically important, but risk prediction is known to be imprecise (Goldney, 2000).
An earlier systematic review (Hawton et al., 2005) of risk factors for suicide in schizophrenia identified 29 high-quality data-containing studies which were analysed for individual risk factors. Hawton et al. (2005) found, perhaps unsurprisingly, that many of the important risk factors for suicide in schizophrenia were similar to those in the general population, including mood disorder, recent loss, previous suicide attempts, and drug misuse. However, some other factors they identified as associated with high suicide risk in schizophrenia, such as fear of mental disintegration, agitation or restlessness, and poor adherence with treatment, are not immediately self-evident. Interestingly, Hawton et al. (2005) also observed a reduced risk of suicide associated with the presence of hallucinations. Since that time, Tiihonen et al. (2006) have confirmed, in a nationwide follow-up of individuals discharged from hospital after a first episode of schizophrenia, that not taking any regular antipsychotic medication was associated with a 12-fold increase in the relative risk of all-cause death and a worrying 37-fold increase in death by suicide.
Risk assessment and risk management remain core skills in clinical psychiatry. Since the 2005 review of Hawton et al., which examined data published up until June 2004, a large number of studies examining the rates and correlates of suicide in schizophrenia have been produced. For example, a recent non-systematic review by Carlborg et al. (2010) found many of the risk factors listed above to be important, as well as some disease-specific factors such as high suicide risk in the first year of illness and associations with a high premorbid function and high IQ, but also noted the low predictive specificity of these factors. We undertook a systematic review of all relevant studies published after June 2004 which provided new data on risk factors for suicide in schizophrenia to better inform clinical practice. We decided to only include studies likely to provide valid estimates of risk factors, namely randomized controlled trials, prospective and retrospective cohort studies, and case-control studies. As part of our systematic review we decided to rank the quality of the evidence, and hence assessed the quality of the included studies, according to standardized criteria.
Methods
Search strategy and study eligibility
This systematic review included literature published between June 2004 and January 2010. An electronic search on the following databases were carried out – EMBASE, PsychINFO and OVID Medline (R). The subject headings used included:
Catatonic Schizophrenia or Paranoid Schizophrenia or Schizophrenia or Disorganized Schizophrenia or Childhood Schizophrenia or schizophrenia.mp., Psychotic Disorders or schizoaffective psychosis.mp., and
Suicide.mp. or Suicide, and
Risk factor.mp. or Risk Factors, and
Cohort Studies.mp. or Cohort Studies, Case Control Studies.mp. or Case-Control Studies, Cohort Analysis.mp. or Cohort Studies, Follow Up Studies.mp. or Follow-Up Studies
The results of the search were screened for suitability independently by both investigators. These studies were further screened for eligibility based on the inclusion criteria:
Literature published in English
Case-control, cohort or follow-up studies
Patient diagnosis of schizophrenia (including all subtypes), psychosis and schizoaffective disorder
Data extraction
The shortlisted studies were then analysed and the following data were extracted:
Rate of suicide
Socio-demographic information: age, gender, ethnicity, marital status, employment, education, social class, rural/urban
Genetic/biological information: genetics, family history of suicidal behaviour, biological markers
Illness-related: age of onset, duration of disease, physical illness, affective disorder, thought disorder, depression, psychopathology, insight
Life events
Previous suicide attempts/ideation
Substance misuse/abuse/dependence: alcohol, smoking, drugs
Quality of studies
The studies included in this systematic review were assessed for quality. A score was given for study design: 4, randomized controlled trials; 3, prospective cohort/follow-up study; 2, retrospective cohort study; 1, case-control study. The studies were also assessed for the following characteristics: explicit aims, definition and size of population investigated, demographic details of subjects, explicit risk factors (if study looked at risk factors), validity and reliability of methods, response and drop-out rate specified, justification of response or drop-out rate, discussion of generalizability and discussion of limitations. Each of these criteria was allocated 1 point and the total score for each article was calculated. The six studies which provided data on over 100 subjects and had the highest quality scores were extracted and analysed in more detail, in order to ascertain recurrent findings or themes.
Results
Data extraction
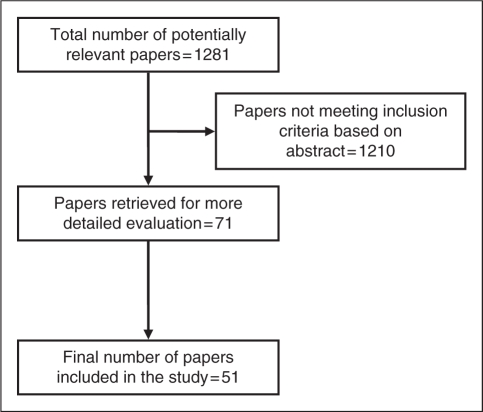
A total of 1281 articles were initially identified by the search strategy. Of the 1281 studies identified, 12 papers were not written in English and were therefore excluded from the study. Some 71 papers (out of 1269) were shortlisted for detailed analyses based on the abstracts; 20 of these papers were not included as they did not address the objectives of this study. A final total of 51 studies were identified as relevant to this study and were reviewed, as depicted in Figure 1.
Figure 1.
Flow chart showing the article-identification process.
All 51 papers were further analysed for risk factors for suicide. The risk factors were grouped into six main categories – Demographics, Illness-Related Factors, Insight, Suicide Attempt/Ideation, Life Events and Genetics.
The following studies provided new data on the rates of suicide in schizophrenia, which we have presented in Table 1.
Table 1.
Rates of suicide
| Study | Details of study | Population | Conclusion on suicide rates |
|---|---|---|---|
| Phillips et al. (2004) | Retrospective observational study in China. Data for 1995–99 were extrapolated from data obtained from 1993 | Annual estimate of 4.25 million people with schizophrenia and 284,614 total suicides – of which 28,737 suicides are by people with schizophrenia | 10.1% of all suicides had schizophrenia. Suicide rate in adults with schizophrenia was 6.8/1000 people/year. RR of suicide in those with schizophrenia vs. those without is 23.8. |
| Silverton et al. (2008) | 43 year prospective longitudinal Danish cohort study | 208 children in ‘high-risk’ group (based on mother's diagnosis of schizophrenia), 11 committed suicide | Suicide was 14 times more likely in ‘high-risk’ subjects diagnosed with schizophrenia, compared with other mental disorders or no mental disorders |
| Craig et al. (2006) | Prospective cohort study. 5- and 10-year survival; absolute and relative mortality rates among first-admission patients with psychotic disorder | 235 patients with schizophrenia, 12 deaths due to all causes (four natural deaths, seven unnatural death, one unknown) | 1.7% of all patients with schizophrenia died by suicide |
| Ran et al. (2007) | 10-year prospective follow-up study in rural China | 500 patients with schizophrenia; 21 died by suicide | Suicide rate was 477/100000 person-years. SMR was 32.0. Risk of suicide during the follow-up period was 4.5%. |
| Osborn et al. (2008) | Retrospective cohort study in general practices in UK from 1987–2002 | 46,136 patients with severe mental illness (40.2% with schizophrenia) included, matched with 300,426 controls | 48 (0.26%) patients with schizophrenia committed suicide; adjusted hazard ratio = 7.00 |
| Healy et al. (2006) | Retrospective cohort study, North Wales, UK. Compared lifetime suicide rates in treated schizophrenia between cohorts from 1875–1924 and 1994–1998 | 1875–1924: 594 patients with schizophrenia, three suicides 1994–1998: 85 patients, four suicides | 1875–1924: 16/100000 patient-years, lifetime suicide rate of 0.46% 1994–1998: 752/100000 patient-years |
| Nordentoft et al. (2004) | Case-control study using four Danish longitudinal registers from 1981–1997 | 18,744 individuals committed suicide in total, including 756 people with schizophrenia | Suicide rates were found to decline from 1981–1997 by >50%. Incidence rate ratio for suicide among patients with schizophrenia was about 20 times higher than the general population |
| Carlborg et al. (2008) | Follow-up study in Sweden from 1973–2006 | 385 inpatients (153 men, 232 women) with schizophrenia spectrum psychoses | Rate of suicide during the follow-up period was 6.8%. Incidence rate ratio for suicide was 1.01 |
| Bhatia et al. (2006) | Retrospective cohort study with Indian and American samples | 460 Indians and 424 Americans | More attempted suicides in US (205/424 in US vs. 107/460 in India cohorts) |
| Limosin et al. (2007) | 10-year prospective follow-up study in France | 3470 patients with schizophrenia, 141 suicides | Prevalence of suicide (global SMR) was 16.2. Mortality due to suicide especially high during the first 4 years of follow-up |
| Barak et al. (2004a) | 10-year case-control study in Israel | 692 elderly patients with schizophrenia, 30 patients attempted suicide | Rate of suicide attempts was ∼5%, somewhat less than that reported for younger patients |
| Laursen et al. (2007) | Retrospective cohort study using two population-based cohorts in Denmark | Schizophrenia: 17,660 first admissions and 3942 deceased. Schizoaffective: 4055 first admissions and 1261 deaths | Mortality rate ratio for suicide among male and female patients with schizophrenia was 34.51 and 58.81, respectively. Schizophrenia highest mortality rate ratio in the age groups 55–79 and 80+. |
RR, relative risk; SMR, standardised mortality ratio.
The new data on risk factors for suicide in schizophrenia were grouped into the six main themes noted above. Individual demographic characteristics identified as risk factors for suicide are depicted in Table 2.
Table 2.
Patient demographics
| Characteristic | Number of studies | Positive association | No association | Conclusion on risk factors |
|---|---|---|---|---|
| Age | 10 | 7/10 identified young age as a predisposing risk factor for increased suicide. One study noted higher risk among patients >50y/o, and another identified higher mean age of suicide among females, but not in males | Young age not replicated in one study | Young age |
| Gender | 16 | Two studies identified females having a higher risk of suicide. Eleven studies found that males have a higher risk of suicide | One study did not replicate findings on male gender as a predisposing factor for suicide. Two studies found no difference in suicide between gender | Males |
| Ethnicity | 2 | One study showed that whites have higher suicide rate, another found that being born in Sweden predisposes to suicide | – | Inconclusive |
| Marital status | 3 | Two studies found that being single predisposes to suicide | One study found that there was no difference in suicide | Single |
| Employment | 3 | Two studies found unemployment and inability to work, respectively, as increasing risk of suicide. One study identified minimal lost work potential amongst the suicide group | – | Unemployment |
| Education | 6 | All six studies identified higher levels of education as a predisposing risk factor for suicide. One of the studies only found this amongst the Americans but not Indian subjects | – | Higher levels of education |
| Social class | 4 | One study identified higher suicide rate in those from higher social class, and two studies identified homelessness and living alone, respectively, as positive risk factors | One study found no difference in economic status | Inconclusive |
| Rural/urban | 1 | Rural >urban by 3.18 times | – | Rural |
Risk factors for later suicide that were identified from systematic review and were related to the individual’s illness are shown in Table 3.
Table 3.
Illness-related factors
| Characteristic | Number of studies | Positive association | No association | Conclusion |
|---|---|---|---|---|
| Age of illness onset | 5 | Three studies identified later age of onset as a predisposing factor to increased suicide. One study found younger age of onset associated with suicide | One study found no difference | Later age of onset |
| Duration of illness | 6 | One study: ≥ 10 years, two studies: acute/shorter duration of illness, two studies: within first 3–5 years, one study: long illness with exacerbations | – | Inconclusive |
| Physical illness | 2 | Both studies found positive correlation | – | Presence of physical illness |
| Affective disorder | 23 | Seven studies found positive correlation between affective disorders and increased suicide. Fifteen studies identified a positive relationship between the presence of depression and increased risk of suicide | Only one study found no difference in level of depression between attempters and non-attempters | Hopelessness, negative self-thoughts. Presence of depression |
| Psychotic symptoms | 16 | Ten studies identified a positive correlation between positive psychotic symptoms and suicide in schizophrenia. Low levels of negative symptoms also showed a strong relationship with increased suicide in three studies. Also positive: higher level of baseline mental suffering (one study) and mental disintegration and agitation/restlessness (one study) | One study found no relationship between suicide and lifetime occurrence of hallucinations or delusions. One study showed no difference in suicidality by mean number of negative symptoms | Increased positive symptoms, particularly auditory hallucinations and delusions, but lower levels of negative symptoms |
| Insight | 5 | Four studies showed a positive correlation between suicide and insight | One study found no difference in suicide rates between groups with insight and without | Presence of insight |
| Treatment | 11 | Two studies identified increased suicide risk with current use of antidepressants and being treated by male psychiatrists. One study identified higher number of hospitalizations amongst those with who committed suicide. Protective factors include CBT, SGAs and deinstitutionalization | One study found no difference in suicide rates between those who have been treated and those who have not. Another study identified no difference between groups treated with CBTp, supportive counselling or usual treatment | Inconclusive. Studies suggest that second-generation antipsychotics are protective |
CBT, cognitive behavioural therapy; SGA, second generation antipsychotic.
Those familial or genetic characteristics studied, and elicited by our systematic review, in individuals with schizophrenia who later committed suicide are contained in Table 4.
Table 4.
Genetics
| Characteristic | Number of studies | Positive association | No association | Conclusion |
|---|---|---|---|---|
| Family history | 4 | Three studies identified a positive correlation between family history of suicide (behaviour/attempt) and suicide | One study found no difference | Positive family history |
| Biological markers | 1 | – | No difference in CSF 5-HIAA levels and CSF HVA levels between suicide attempters and non-attempters | No association between CSF 5-HIAA and HVA levels, and suicide |
| Genetics | 2 | One study: COMT Del Allele confers susceptibility to suicide attempters. One study: difference in mean ratios, with the ‘C’ alleles showing lower cDNA levels in the suicide group; decreased total 5-HT2A receptor mRNA in suicide victims | – | Genes identified to be associated with suicide – COMT Del Allele, “C” alleles and 5-HT2A receptor |
The other three specific domains of risk factors associated with later suicide in people with schizophrenia are separated below:
Suicide attempt/ideation
Of the 51 studies, 10 evaluated history of suicide attempt/ideation as a risk factor for suicide in patients with schizophrenia. All 10 studies identified a positive correlation between suicide attempt/ideation and suicide.
Substance abuse
Of the seven studies that looked into substance misuse, four studies identified alcohol as a predisposing factor to increased suicides among patients with schizophrenia, while three studies identified substance abuse and one study identified smoking only. Only one study found no difference in current substance abuse in those who committed suicide.
Life events
Only two studies looked at life events as a risk factor for suicide. One of the studies looked at childhood trauma and found that patients who committed suicide had higher scores on the Childhood Trauma Questionnaire. Another study found that those with schizophrenia had a higher number of life events compared with a normal control group, but people with schizophrenia who were suicidal had fewer incidences of life events than those who were non-suicidal.
Our systematic quality analysis of all available included studies, using the scoring criteria noted above, yielded the following results (Table 5):
Table 5.
Quality analysis of all included original studies
| Study | Study design | Percentage of maximum quality score (%) |
|---|---|---|
| Crumlish et al. (2005) | Prospective Cohort Study | 92 |
| Fialko et al. (2006) | Randomized Controlled Trial | 92 |
| Ran et al. (2007) | Follow-Up/Cohort Study | 92 |
| Ran et al. (2009) | Prospective Cohort Study | 92 |
| Montross et al. (2008) | Randomized Controlled Trial | 92 |
| Ran et al. (2008) | Prospective Cohort Study | 92 |
| Sevincok et al. (2007) | Prospective Case-Control Study | 85 |
| Alaräisänen et al. (2006) | Retrospective Cohort Study | 85 |
| Kuo et al. (2005) | Follow-up Cohort Study | 85 |
| Pompili et al. (2009) | Retrospective Cohort Study | 85 |
| Loas et al. (2009) | Prospective Cohort Study | 85 |
| Bhatia et al. (2006) | Retrospective Cohort Study | 85 |
| Limosin et al. (2007) | Prospective Follow-up Study | 85 |
| McGirr et al. (2008) | Retrospective Cohort Study | 85 |
| Bickley et al. (2006) | Retrospective Cohort Study | 85 |
| Bateman et al. (2007) | Randomized Controlled Trial | 85 |
| Silverton et al. (2008) | Prospective Cohort Study | 77 |
| Carlborg et al. (2008) | Follow-Up/Cohort Study | 77 |
| Tidemalm et al. (2008) | Follow-Up/Cohort Study | 77 |
| Healy et al. (2006) | Retrospective Cohort Study | 77 |
| Bertelsen et al. (2007) | Randomized Controlled Trial | 77 |
| Laursen et al. (2007) | Retrospective Cohort Study | 77 |
| Kelly et al. (2004) | Retrospective Cohort Study | 77 |
| Haukka et al. (2008) | Retrospective Cohort Study | 77 |
| Barak et al. (2004a) | Retrospective Case-Control Study | 77 |
| Sinclair et al. (2004) | Retrospective Case-Control Study | 77 |
| Reutfors et al. (2009) | Retrospective Case-Control Study | 77 |
| Carlborg et al. (2009) | Prospective Cohort Study | 77 |
| Preti et al. (2009) | Prospective Cohort Study | 77 |
| Barak et al. (2004b) | Retrospective Case-Control Study | 77 |
| Tarrier et al. (2006) | Prospective Randomized Controlled Trial | 77 |
| Strauss et al. (2006) | Retrospective Cohort Study | 77 |
| Altamura et al. (2007) | Retrospective Cohort Study | 77 |
| Alaräisänen et al. (2009) | Prospective Cohort Study | 77 |
| Rantanen et al. (2009) | Follow-up Study | 77 |
| Niehaus et al. (2004) | Case-Control Study | 77 |
| Ran et al. (2005) | Retrospective Cohort Study | 77 |
| Lewine and Shriner (2009) | Retrospective Cohort Study | 69 |
| Barak et al. (2008) | Case-Control Study | 69 |
| Lee et al. (2009) | Case-Control Study | 69 |
| McGirr et al. (2006) | Case-Control Study | 69 |
| Osborn et al. (2008) | Retrospective Cohort Study | 69 |
| Harkavy-Friedman et al. (2004) | Retrospective Cohort Study | 69 |
| Roy (2005) | Retrospective Case-Control Study | 69 |
| Li et al. (2008) | Case-Control Study | 69 |
| De Luca et al. (2007) | Case-Control Study | 62 |
| Bourgeois et al. (2004) | Follow-Up/Cohort Study | 62 |
| De Luca et al. (2006) | Case-Control Study | 62 |
| Karvonen et al. (2007) | Retrospective Cohort Study | 62 |
| Phillips et al. (2004) | Retrospective Cohort Study | 62 |
| Fennig et al. (2005) | Case-Control Study | 46 |
The top six articles (percentage of maximum quality score = 92%) were extracted for more detailed analysis. Table 6 summarizes the details on methods, risk factors investigated and conclusions of each of these six studies.
Table 6.
Summary of the highest-quality studies of risk factors for suicide in schizophrenia
| Study | Title of paper | Details of participants | Conclusions re increased suicide risk |
|---|---|---|---|
| Crumlish et al. (2005) | Early insight predicts depression and attempted suicide after 4 years in first-episode schizophrenia | 101 participants, suicide attempts was used as a measurement | Insight is associated with increased risk of suicide attempts. Insight is also associated with depression |
| Fialko et al. (2006) | Understanding suicidal ideation in psychosis: findings from the Psychological Prevention of Relapse in Psychosis (PRP) trial | 290 patients | Younger age and male gender not replicated Whites Anxiety, negative beliefs and depression Auditory hallucinations Daily alcohol consumption |
| Ran et al. (2007) | Mortality in people with schizophrenia in rural China: 10-year cohort study | 500 patients | >50 y/o, male gender and inability to work associated with increased risk |
| Age of onset > 45 y/o, duration of disease ≥ 10 years, physical illness | |||
| Reduced risk with treatment | |||
| Ran et al. (2009) | Differences in mortality and suicidal behaviour between treated and never-treated people with schizophrenia in rural China | 500 patients, 132 never received antipsychotic and 368 reported having received antipsychotic treatment | Suicide rates were not significantly different between treated and non-treated schizophrenic patients. Overall mortality rates in patients are high when compared with general population (>6.5 times) |
| Montross et al. (2008) | Suicidal ideation and attempts among middle-aged and older patients with schizophrenia spectrum and concurrent subsyndromal depression. | 132 patients | Male gender Hopelessness, depression, higher PANSS general psychopathology subscale scores |
| History of suicidal ideation | |||
| Ran et al. (2008) | Mortality of geriatric and younger patients with schizophrenia in the community | 500 patients | Patients from the younger age group had higher suicide rates |
PANSS, positive and negative syndrome scale
Discussion
This systematic review included findings from 51 articles published from June 2004 to January 2010. The main findings from this review are as follows:
Suicide rate in schizophrenia
Studies so far have not come to an agreement on suicide rates amongst patients with schizophrenia. The most widely cited lifetime suicide rate is 10%, as estimated by a review by Miles (1977). However, a recent study by Palmer et al. (2005) has challenged this and has proposed that the lifetime suicide risk in schizophrenia is approximately 4.9%. The current review analysed contemporary data on suicide rates amongst patients with schizophrenia, and we conclude that an accurate estimated suicide rate is 579/100,000 person-years (477–680/100,000 person-years). However, two other studies that investigated the proportion of people who died due to suicide who also had schizophrenia reported a rate of 10.1% (Philips et al., 2004) and 22.3% (Osborn et al., 2008), but proportionate mortality should not be confused with lifetime risk.
It is perhaps not surprising that different studies, using different populations and methodologies, return varying estimates of the suicide rate in schizophrenia. Also, the ‘true’ suicide rate will fluctuate over time, depending on numerous complex variables including the period over which the studies were carried out. In addition, many suicides may be misclassified as ‘unnatural’ or ‘undetermined’ deaths. However, most studies seem to indicate that the earlier consensus figure of 10% lifetime risk is an overestimate (perhaps due to confusion with proportionate mortality), with a lifetime risk of around 5% being more representative, and compatible with various studies we analysed (Barak et al., 2004a; Carlborg et al., 2008; Ran et al., 2007; Limosin et al., 2007). This 5% figure remains significantly higher than the general population risk of suicide.
We decided it would be clinically relevant and helpful to classify the data on risk factors for suicide in schizophrenia, according to the strength of the findings in the data reviewed. Thus we produced Table 7, which summarizes those risk factors which have a strong association, and those with a weaker (or negative) association for later suicide.
Table 7.
Summary of risk factors associated with suicide in schizophrenia
| Risk factor | Strong association with suicide | Weak association with suicide |
|---|---|---|
| Demographic factors | Young, male, unemployment, with higher levels of education | Single (not married), rural |
| Illness-related factors | Presence of depression, hopelessness, negative self-thoughts, anxiety, insomnia, self-devaluation, low self-esteem, guilty thoughts and PTSD | Treatment (in particular, second-generation antipsychotic) may be a protective factor against suicide |
| Increased positive symptoms, in particular auditory hallucinations and delusions; low negative symptoms; higher level of mental suffering at baseline; mental disintegration and agitation/motor restlessness | Later age of onset The impact of duration of disease on suicide risk is inconclusive | |
| Presence of insight | ||
| Presence of physical illnesses | ||
| Genetics | Positive family history | |
| Previous suicide attempt/ideation | Strong correlation with history of suicide attempt/ideation | |
| Substance abuse | Alcohol and drug abuse | Smoking |
| Life events | Potentially increased risk with history of increased childhood trauma |
PTSD, post-traumatic stress disorder
What have we learnt since 2005?
This systematic review has replicated some of the key findings found in Hawton et al. (2005), including identifying a strong association with later suicide in schizophrenia and earlier depression, history of suicide attempts, and drug misuse. Depression is one of the major risk factors for suicide among individuals with schizophrenia. A randomized controlled trial (OPUS Trial) (Bertelsen et al., 2007) investigated suicidal thoughts and plans, depressive symptoms and drug misuse in predicting suicidal attempts at 1- and 2-year follow-up. This trial has shown that suicidal thoughts and plans, previous suicide attempts and depressive symptoms are among the strongest predictors of suicidality in patients presenting with first-episode psychosis. One of our top-scoring articles (Fialko et al., 2006) used the Beck Depression Inventory as a measure of the severity of depression and its association with the risk of committing suicide. This study has shown that the likelihood of patients with scores equal or greater than 2 on Suicide Item (9) committing suicide increases by seven-fold.
A history of prior suicide attempts elevates risk of completed suicide threefold according to both Reutfors et al. (2009) and Sinclair et al. (2004), who found that individuals who were admitted for an attempted suicide had the highest risk (of all variables studied) of committing suicide (Odds Ratio (OR) = 8.10).
In addition to drug misuse, we also identified alcohol misuse as a key risk factor for suicide. The WHO Mental Health Surveys (Nock et al., 2009) aimed to identify mental disorders associated with suicidal behaviour and have shown that alcohol (OR = 2.6) and drug (OR = 2.0) abuse or dependency are strong predictive factors for suicide. However, one of the studies included in this review (McGirr and Turecki, 2008) has shown that substance abuse does not increase risk of suicide amongst patients with schizophrenia (alcohol abuse and lifetime suicide risk OR = 0.29, drug abuse and lifetime suicide risk OR = 0.94), although this study used data from interviews with family members of the deceased patients, which may not be the most accurate source of information.
Hawton et al. (2005) found that poor adherence to treatment is associated with increased risk of suicide (OR = 3.75). Some of the studies included in this review have shown that individuals who underwent treatment had a smaller risk of committing suicide (Barak et al., 2008; Preti et al., 2009; Ran et al., 2007), but one particular study (Ran et al., 2009) found no significant difference between suicide rates between the treated and non-treated group, although Ran et al. (2009) found that the non-treated group had more severe symptoms.
An interesting finding in this study is the association between the presence of positive symptoms, in particular auditory hallucinations and delusions, and an increased risk of suicide among patients with schizophrenia. This is in contrast with the findings reported by Hawton et al. (2005). This difference may be due to the heterogeneity of the data in Hawton et al. (2005) which resulted in a relatively weak association between hallucinations and reduced risk of suicide. While our study has identified a positive association, further studies are required to confirm this.
Conventional wisdom suggests that increased risk of suicide in schizophrenia is associated with young age. However, some of the studies (Fialko et al., 2006; Kuo et al. 2005; Ran et al., 2007; Reutfors et al., 2009) included in this review have challenged this association, with both Reutfors et al. (2009) and Kuo et al. (2005) finding that a later age of illness onset is associated with an increased risk of suicide. Ran et al. (2007) identified that age (>50 years old, hazard ratio = 4.8) and age at illness onset (>45 years old, hazard ratio = 9.2) are independent predictors of mortality in the population studied, but this study did not define the causes of death or investigate specific predictors of suicide. The difference in conclusions about age as a risk factor for suicide in patients with schizophrenia may be a result of the design of the study, with shorter-term studies having a tendency of identifying younger patients as a higher risk group. Further studies are needed to identify if older age and later age of onset are indeed strong predictors of suicide, and such studies should take into account the severity of psychotic symptoms, chronicity of illness, and other co-morbidities including affective disorders. Until then, the weight of evidence supports a younger age as a risk factor.
Some of the risk factors identified in this systematic review may be similar or may oppose those observed in the general population, as Agerbo (2007) has pointed out. However, for the purposes of this study, the risk factors identified are in relation to patients with schizophrenia and are not compared with risk factors in the general population. This systematic review looked at studies that identified either suicide or suicide ideation as an outcome. This may potentially affect our findings, although a history of suicide attempt or ideation has a strong positive correlation with completed suicide among patients with schizophrenia. Therefore, we feel that inclusion of studies with suicide ideation or attempt as an outcome in this study is justified.
Limitations
We did not attempt to perform a meta-analysis, which would allow a quantitative analysis of predictors of suicide for schizophrenia. However, differing study designs of studies included in this systematic review mean that not all data are amenable to meta-analysis. We only reviewed papers that were published in English.
Conclusions
Since an earlier systematic review conducted by Hawton et al. (2005), there have been numerous studies published concerning suicide in schizophrenia. We included 51 new data-containing studies in this critical systematic review, and found that the factors with the strongest association with later suicide (in schizophrenia) included being young and male, with a higher level of education. Illness-related factors were also important predictors, namely depressive symptoms, a history of suicide attempts, active hallucinations (contrary to Hawton et al., 2005) and delusions, the presence of insight, and comorbid chronic physical illness. Lastly, a family history of suicide and co-existing alcohol and drug misuse were also factors with a strong association with later suicide. Adequate treatment for schizophrenia and related comorbid problems was the only protective factor identified.
Prevention of suicide in schizophrenia would thus rely on identifying those individuals with the risk factors noted above, and actively treating any comorbid depressive illness and positive psychotic symptoms, as well as addressing any co-existent substance misuse. However, suicide prediction in those with schizophrenia is complex, and efforts at prevention should also focus on optimizing adherence to medication, and possible earlier use of clozapine, as the only antipsychotic medication with demonstrated efficacy (and a licence in the USA) for the management of suicidality in schizophrenia.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Agerbo E. (2007) High income, employment, postgraduate education, and marriage: a suicidal cocktail among psychiatric patients. Arch Gen Psychiatry 64: 1377–1384, Erratum appears in Arch Gen Psychiatry (2008) 65: 144). [DOI] [PubMed] [Google Scholar]
- Alaräisänen A, Miettunen J, Lauronen E, Räsänen P, Isohanni M. (2006) Good school performance is a risk factor of suicide in psychoses: A 35-year f/u of Northern Finland 1966 Birth Cohort. Acta Psychiatr Scand 114: 357–362 [DOI] [PubMed] [Google Scholar]
- Alaräisänen A, Miettunen K, Räsänen P, Fenton W, Koivumaa-Honkanen HTJ, Isohanni M. (2009) Suicide rate in schizophrenia in the Northern Finland 1966 Birth Cohort. Soc Psychiatry Psychiatr Epidemiol 44: 1107–1110 [DOI] [PubMed] [Google Scholar]
- Altamura AC, Mundo E, Bassetti R, Green A, Lindenmayer JP, Alphs L, et al. (2007) Transcultural differences in suicide attempters: Analysis on a high-risk population of patients with schizophrenia or schizoaffective disorder. Schizophr Res 89: 140–146 [DOI] [PubMed] [Google Scholar]
- Barak Y, Baruch Y, Achiron A, Aizenberg D. (2008) Suicide attempts of schizophrenia patients: A case-controlled study in tertiary care. J Psychiatr Res 42: 822–826 [DOI] [PubMed] [Google Scholar]
- Barak Y, Knobler CY, Aizenberg D. (2004a) Suicide attempts amongst elderly schizophrenia patients: A 10-year case-control study. Schizophr Res 71: 77–81 [DOI] [PubMed] [Google Scholar]
- Barak Y, Mirecki I, Knobler HY, Natan Z, Aizenberg D. (2004b) Suicidality and second generation antipsychotics in schizophrenia patients: A case-controlled retrospective study during a 5-year period. Psychopharmacology 175: 215–219 [DOI] [PubMed] [Google Scholar]
- Bateman K, Hansen L, Turkington D, Kingdon D. (2007) Cognitive behavioural therapy reduces suicidal ideation in schizophrenia: Results from a RCT. Suicide Life Threat Behav 37: 284–290 [DOI] [PubMed] [Google Scholar]
- Bertelsen M, Jeppesen P, Petersen L, Thorup A, Øhlenschlæger J, Quach PL, et al. (2007) Suicidal behaviour and mortality in first-episode psychosis; The OPUS Trial. Br J Psychiatry 191(Suppl 51): s140–s146 [DOI] [PubMed] [Google Scholar]
- Bhatia T, Thomas P, Semwal P, Thelma BK, Nimgoankar VL, Deshpande SN. (2006) Differing correlates for suicide attempts among patients with schizophrenia or schizoaffective disorder in India and USA. Schizophr Res 86: 208–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickley H, Kapur N, Hunt IM, Robinson J, Meehan J, Parsons R, et al. (2006) Suicide in the homeless within 12 months of contact with mental health services. Soc Psychiatry Psychiatr Epidemiol 31: 686–691 [DOI] [PubMed] [Google Scholar]
- Bourgeois M, Swendsen K, Young F, Amador X, Pini S, Cassano GB, et al. (2004) Awareness of disorder and suicide risk in the treatment of schizophrenia: Results of the International Suicide Prevention Trial. Am J Psychiatry 161: 1494–1496 [DOI] [PubMed] [Google Scholar]
- Bushe C, Taylor M and Haukka J (2010) Mortality in schizophrenia – A measurable clinical endpoint. J Psychopharmacol 24(Suppl 4): 17–25. [DOI] [PMC free article] [PubMed]
- Carlborg A, Jokinen J, Jönsson EG, Nordström AL, Nordström P. (2008) Long-term suicide risk in schizophrenia spectrum psychoses: Survival analysis by gender. Arch Suicide Res 12: 347–351 [DOI] [PubMed] [Google Scholar]
- Carlborg A, Jokinen J, Nordström AL, Jönsson EG, Nordström P. (2009) CSF 5-HIAA, attempted suicide and suicide risk in schizophrenia spectrum psychosis. Schizophr Res 112: 80–85 [DOI] [PubMed] [Google Scholar]
- Carlborg A, Winnerback K, Jonsson EG, Jokinen J, Nordstrom P. (2010) Suicide in schizophrenia. Expert Rev Neurother 10: 1153–1164 [DOI] [PubMed] [Google Scholar]
- Craig TJ, Ye Q, Bromet EJ. (2006) Mortality among first-admission patients with psychosis. Compr Psychiatry 47: 246–251 [DOI] [PubMed] [Google Scholar]
- Crumlish N, Whitty P, Kamali M, Clarke M, Browne S, McTigue O, et al. (2005) Early insight predicts depression and attempted suicide after 4 years in first-episode schizophrenia and schizophreniform disorder. Acta Psychiatrica Scand 112: 449–455 [DOI] [PubMed] [Google Scholar]
- De Luca V, Likhodi O, Kennedy JL, Wong AHC. (2007) Differential expression and parent-of-origin effect of the 5-HT2A receptor gene C102T polymorphism: Analysis of suicidality in schisophrenia and bipolar disorder. Am J Med Genet B Neuropsychiatr Genet 144B: 370–374 [DOI] [PubMed] [Google Scholar]
- De Luca V, Tharmalingam S, Müller DJ, Wong G, de Bartolomeis A, Kennedy JL. (2006) Gene-gene interaction between MAOA and COMT in suicidal behaviour: Analysis in schizophrenia. Brain Res 1097: 26–30 [DOI] [PubMed] [Google Scholar]
- Fennig S, Horesh N, Aloni D, Apter A, Weizman A, Fennig S. (2005) Life Events and suicidality in adolescents with schizophrenia. Eur Child Adolesc Psychiatry 14: 454–460 [DOI] [PubMed] [Google Scholar]
- Fialko L, Freeman D, Bebbington PE, Kuipers E, Garety PA, Dunn G, et al. (2006) Understanding suicidal ideation in psychosis: Findings from the Psychological Prevention of Relapse in Psychosis (PRP) Trial. Acta Psychiatr Scand 114: 117–186 [DOI] [PubMed] [Google Scholar]
- Goldney RD. (2000) Prediction of suicide and attempted suicide. In: Hawton K, van Heeringen K. (eds) The International Handbook of Suicide and Attempted Suicide Chichester: Wiley; 585–596 [Google Scholar]
- Harkavy-Friedman JM, Nelson EA, Venarde DF and Mann JJ (2004) Suicidal behaviour in schizophrenia and schizoaffective disorder: examining the role of depression. Suicide Life-Threat 34: 66–76. [DOI] [PubMed]
- Haukka J, Tiihonen K, Härkänen T, Lönnqvist J. (2008) Associated between medication and risk of suicide, attempted suicide and death in nationwide cohort of suicidal patients with schizophrenia. Pharmacoepidemiol Drug Saf 17: 686–696 [DOI] [PubMed] [Google Scholar]
- Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ. (2005) Schizophrenia and suicide: Systematic review of risk factors. Br J Psychiatry 187: 9–20 [DOI] [PubMed] [Google Scholar]
- Healy D, Harris M, Tranter R, Gutting P, Austin R, Jones-Edwards G, et al. (2006) Lifetime suicide rates in treated schizophrenia: 1875–1924 and 1994–1998 cohorts compared. Br J Psychiatry 188: 223–228 [DOI] [PubMed] [Google Scholar]
- Karvonen K, Sammela HL, Rahikkala H, Hakko H, Särkioja T, Meyer-Rochow B, et al. (2007) Sex, timing and depression among suicide victims with schizophrenia. Compr Psychiatry 48: 319–322 [DOI] [PubMed] [Google Scholar]
- Kelly DL, Shim JC, Feldman SM, Yu Y, Conley RR. (2004) Lifetime psychiatric symptoms in persons with schizophrenia who died by suicide compared to other means of death. J Psychiatr Res 38: 531–536 [DOI] [PubMed] [Google Scholar]
- Kuo CJ, Tsai SY, Lo CH, Wang YP, Chen CC. (2005) Risk factors for completed suicide in schizophrenia. J Clin Psychiatry 66: 579–585 [DOI] [PubMed] [Google Scholar]
- Laursen TM, Munk-Olsen T, Nordentoft M, Mortensen PB. (2007) Increased mortality among patients admitted with major psychiatric disorders: A register-based study comparing mortality in unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder and schizophrenia. J Clin Psychiatry 68: 899–907 [DOI] [PubMed] [Google Scholar]
- Lee HC, Lin HC. (2009) Are psychiatrist characteristics associated with post-discharge suicide of schizophrenia patients? Schizophr Bull 35: 760–765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewine R, Shriner B. (2009) Work expectation, cultural sensitivity, schizophrenia and suicide risk in male patients. J Nerv Ment Dis 197: 239–243 [DOI] [PubMed] [Google Scholar]
- Li J, Ran MS, Hao Y, Zhao Z, Guo Y, Su J, et al. (2008) Inpatient suicide in a Chinese psychiatric hospital. Suicide Life Threat Behav 38: 449–455 [DOI] [PubMed] [Google Scholar]
- Limosin F, Loze JY, Philippe A, Casadebaig F, Rouillon F. (2007) Ten-year prospective follow-up study on the mortality by suicide in schizophrenic patients. Schizophr Res 94: 23–28 [DOI] [PubMed] [Google Scholar]
- Loas G, Azi A, Noisette C, Legrand A, Yon V. (2009) Fourteen-year prospective follow-up study of positive and negative symptoms in chronic schizophrenic patients dying from suicide compared to other causes of death. Psychopathology 42: 185–189 [DOI] [PubMed] [Google Scholar]
- McGirr A, Turecki G. (2008) What is specific to suicide in schizophrenia disorder? Demographic, clinical and behavioural dimensions. Schizophr Res 98: 217–224 [DOI] [PubMed] [Google Scholar]
- McGirr A, Tousignant M, Routhier D, Pouliot L, Chawky N, Margolese HC, et al. (2006) Risk factors for completed suicide in schizophrenia and other chronic psychotic disorders: A case-control study. Schizophr Res 84: 132–143 [DOI] [PubMed] [Google Scholar]
- Miles CP. (1977) Conditions predisposing to suicide: A review. J Nerv Ment Dis 164: 231–246 [DOI] [PubMed] [Google Scholar]
- Montross LP, Kasckow J, Golshan S, Solorzano E, Lehman D, Zisook S. (2008) Suicidal ideation and suicide attempts among middle-aged and older patients with schizophrenia spectrum disorders and concurrent subsyndromal depression. J Nerv Ment Dis 196: 884–890 [DOI] [PubMed] [Google Scholar]
- Niehaus DJH, Laurent C, Jordaan E, Koen L, Oosthuizen P, Keyter N, et al. (2004) Suicide attempts in an African schizophrenia population: An assessment of demographic risk factors. Suicide Life Threat Behav 34: 320. [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Laursen TM, Agerbo E, Qin P, Høyer EH, Mortensen PB. (2004) Change in suicide rates for patients with schizophrenia in Denmark, 1981–97: Nested case-control study. Br Med J 329: 261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, et al. (2009) Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Medicine 6(8): e1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn D, Levy G, Nazareth I, King M. (2008) Suicide and severe mental illnesses. Cohort study within the UK General Practice Research Database. Schizophr Res 99: 134–138 [DOI] [PubMed] [Google Scholar]
- Palmer BA, Pankratz VS, Bostwick JM. (2005) The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry 62: 247–253 [DOI] [PubMed] [Google Scholar]
- Phillips MR, Yang G, Li S, Yue L. (2004) Suicide and the unique prevalence pattern of schizophrenia in mainland China: A retrospective observational study. Lancet 364: 1062–1068 [DOI] [PubMed] [Google Scholar]
- Pompili M, Lester D, Grispini A, Innamorati M, Calandro F, Iliceto P, et al. (2009) Completed suicide in schizophrenia: evidence from a case-control study. Psychiatry Res 167: 251–257 [DOI] [PubMed] [Google Scholar]
- Preti A, Meneghelli A, Pisano A, Cocchi A. (2009) Risk of suicide and suicidal ideation in psychosis: Results from and Italian multi-modal pilot program on early intervention in psychosis. Schizophr Res 113: 145–150 [DOI] [PubMed] [Google Scholar]
- Ran MS, Chan CLW, Chen EYH, Mao WJ, Hu SH, Yang CP, et al. (2009) Differences in mortality and suicidal behaviour between treated and never-treated people with schizophrenia in rural China. Br J Psychiatry 195: 126–131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ran MS, Chan CLW, Chen EYH, Yang CP, Lin FR, Li L, et al. (2008) Mortality of geriatric and younger patients with schizophrenia in the community. Suicide Life Threat Behav 38: 143–151 [DOI] [PubMed] [Google Scholar]
- Ran MS, Chen EYH, Conwell Y, Chan CLW, Yip PSF, Ziang MZ, et al. (2007) Mortality in people with schizophrenia in rural China. Br J Psychiatry 190: 237–242 [DOI] [PubMed] [Google Scholar]
- Ran MS, Xiang MZ, Mao WJ, Hou ZJ, Tang MN, Chen EYH, et al. (2005) Characteristics of suicide attempters and nonattempters with schizophrenia in a rural community. Suicide Life Threat Behav 35: 694–701 [DOI] [PubMed] [Google Scholar]
- Rantanen H, Koivisto AM, Salokangas RKR, Helminen M, Pirkola HOS, Wahlbeck K, et al. (2009) Five-year mortality of Finnish schizophrenia patients in the era of deinstitutionalisation. Soc Psychiatry Psychiatr Epidemiol 44: 135–142 [DOI] [PubMed] [Google Scholar]
- Reutfors J, Brandt L, Jönsson EG, Ekbom A, Sparén P, Ösby U. (2009) Risk factors for suicide in schizophrenia: Findings from a Swedish population-based case-control study. Schizophr Res 108: 231–237 [DOI] [PubMed] [Google Scholar]
- Roy A. (2005) Reported childhood trauma and suicide attempts in schizophrenic patients. Suicide Life Threat Behav 35: 690–693 [DOI] [PubMed] [Google Scholar]
- Saha S, Chant D, McGrath J. (2007) A systematic review of mortality in schizophrenia: Is the differential mortality gap worsening over time? Arch Gen Psychiatry 64: 1123–1131 [DOI] [PubMed] [Google Scholar]
- Sevincok L, Akoglu A, Kokcu F. (2007) Suicidality in schizophrenic patients with and without obsessive-compulsive disorder. Schizophr Res 90: 198–202 [DOI] [PubMed] [Google Scholar]
- Silverton L, Mednick SA, Holst C, John R. (2008) High social class and suicide in persons at risk of schizophrenia. Acta Psychiatr Scand 117: 192–197 [DOI] [PubMed] [Google Scholar]
- Sinclair JMA, Mullee MA, King EA, Baldwin DS. (2004) Suicide in schizophrenia: A retrospective case-control study of 51 suicides. Schizophr Bull 30: 803–812 [DOI] [PubMed] [Google Scholar]
- Strauss JL, Calhoun PS, Marx CE, Stechuchak KM, Oddone EZ, Swartz MS, et al. (2006) Comorbid post-traumatic stress disorder is associated with suicidality in male veterans with schizophrenia of schizoaffective disorder. Schizophr Res 84: 165–169 [DOI] [PubMed] [Google Scholar]
- Tarrier N, Haddock G, Lewis S, Drake R, Gregg L. (2006) Suicide behaviour over 18 months in recent onset schizophrenic patients: The effects of CBT. Schizophr Res 83: 15–27 [DOI] [PubMed] [Google Scholar]
- Tidemalm D, Långström N, Lichtenstein P, Runeson B. (2008) Risk of suicide after suicide attempt according to coexisting psychiatric disorder: Swedish cohort study with long-term follow-up. Br Med J 337: a2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiihonen J, Wahlbeck K, Lonnqvist J, et al. (2006) Effectiveness of antipsychotic treatments in a nationwide cohort of 2230 patients in community care after first hospitalisation due to schizophrenia and schizoaffective disorder: Observational follow up study. Br Med J 333: 224. [DOI] [PMC free article] [PubMed] [Google Scholar]