Abstract
Depression is a disabling condition resulting in significant impairment in social functioning, involving the patient’s family, friends, work colleagues, and society at large. Although both psychologic and pharmacologic treatments generally improve many depressive symptoms, they do not always result in significant improvement in social functioning. The importance of recovery of social functioning in depressed patients is now widely appreciated, and studies are beginning to include it in evaluations of therapeutic efficacy. Among the various social adjustment evaluation rating scales, the Social Adaptation Self-Evaluation Scale, a social motivation and behavior scale, has been found to be simple to use and sensitive to change. Using this scale, the selective norepinephrine reuptake inhibitor, reboxetine, has been shown to be significantly more effective in improving social functioning than the selective serotonin reuptake inhibitor, fluoxetine. These findings are consistent with the notion that improvement in social adaptation involves functions depending primarily on noradrenergic neurotransmission. This hypothesis suggests that the serotonin and norepinephrine reuptake inhibitors, venlafaxine, duloxetine, and milnacipran, could be particularly helpful in improving social functioning. Preliminary studies with the serotonin and norepinephrine reuptake inhibitors suggest that they significantly improve social functioning. Comparative studies with selective serotonin reuptake inhibitors on the effects on social functioning should be encouraged.
Keywords: Social Adaptation Self-Evaluation Scale, social functioning, depression, serotonin and norepinephrine reuptake inhibitors, noradrenergic neurotransmission
Introduction
The importance of social relationships in clinical psychiatry is well recognized.1 Social functioning can be defined as the interaction of an individual with his/her environment and the ability to fulfill his/her role within it. An individual functions daily within several environments, ie, work, social and leisure, marital, parental, within the extended family,2 as well as with virtual networks. The major impact of depression on social functioning and the consequences of impaired social functioning on the global well-being of depressed patients has been well established.3–7 Social functioning is possibly one of the most important factors affecting the quality of life in depressed patients, although this has not yet been systematically investigated. For workers, depression has a profound effect on workplace functioning. Individuals with major depression have high rates of absenteeism and of presenteeism, a term used to describe the lost productivity a worker experiences when he is able to attend work but is not performing optimally.8
Impairment of social functioning may be substantial and long-lasting. The severity of social dysfunction is dependent on the clinical form of depression. Double depressives (those suffering simultaneously from dysthymia and major depression), for example, have been found to be significantly more impaired in overall social functioning than those with dysthymia or major depressive episodes alone.6 The main differences were in relationships with extended family and in social and leisure pursuits.6 The social dysfunction seen in patients with dysthymia is at least as severe as in patients with major depression.6 There is evidence that poor social support, maladjustment in social and leisure activities, and poor quality of relationships with extended family are strong predictors of recurrence of a major depressive episode.9 The protective effect of social contacts is undisputable, and has even been shown in a rodent model of depression.10
The difference between social functioning (or social adaptation) and social support needs to be clarified. Social adaptation is the ability of each person to “adapt” his/her behavior to make it appropriate to the social environment in which he/she finds his/herself. In contrast, “social support” refers to people who are emotionally close to the individual and who provide “understanding, encouragement and general positive feedback”. A depressive episode will not, at least in the early stages, alter the social support network of a patient. It does, however, profoundly alter his/her “social adaptation”, making him/her less socially acceptable. In the long term, this is likely to have a negative impact on the social support network of the patient. Lack of social support has been well established as a risk factor for depression.11–13
Full recovery from depression requires not only the resolution of depressive symptoms, but also an improvement in the interaction of the individual with his/her environment.3,4,6 Enhancement of social functioning or adaptation should thus be considered a therapeutic goal in the management of depression and, as such, should legitimately influence the choice of antidepressant therapy.5
This review explores the mechanisms underlying social dysfunction in depression, evaluation of its severity, and the effect of antidepressants on social functioning. Recent data for the serotonin and norepinephrine reuptake inhibitors (SNRIs) are reviewed in detail.
Mechanisms underlying social dysfunction in depressed patients
Human behavior is complex and rarely, if ever, the result of the action of a single neurotransmitter. However, it is possible, to define certain functions that are related more specifically to serotonergic, noradrenergic, or dopaminergic neurotransmission. Noradrenergic neurotransmission is thought to be essential to sustain or enhance vigilance, motivation, and self-perception, whereas serotonin (5-hydroxytryptamine, 5-HT) affects impulsivity and irritability, while dopamine (DA) is important in the regulation of drive.14,15
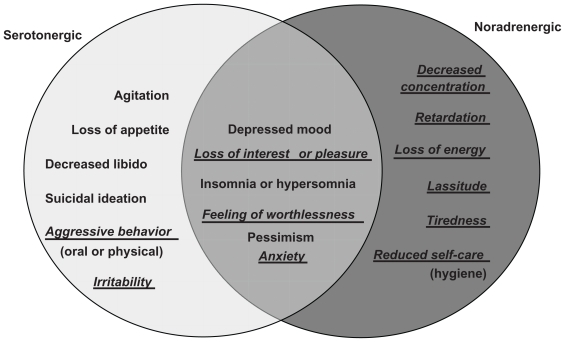
Widespread disturbances of monoamine neurotransmission occur in depression, and they are probably fundamental to its pathophysiology.16,17 More specifically, a deficiency in 5-HT, norepinephrine (NE), and possibly DA neurotransmission has been suggested in depression.18–20 A relationship exists between the different neurotransmitter deficits and the symptoms of major depressive disorder21 (Figure 1). Agitation, loss of appetite, decreased libido, suicidal ideation, aggressive behavior (verbal or physical), and irritability are symptoms related principally to the dysfunction of serotonergic neurotransmission.21,22 Decreased concentration, mental and physical slowing, loss of energy, lassitude, tiredness, and reduced self-care (hygiene) are symptoms related principally to reduced noradrenergic activity.21,22 Depressed mood, loss of interest or pleasure, sleep disturbances, feeling of worthlessness, pessimism, and anxiety are symptoms related to changes in both 5-HT and NE neurotransmission.21,22
Figure 1.
Influence of serotonergic and noradrenergic neurotransmission on the symptoms of depression. Symptoms in underlined italics are those that are directly related to social adaptation. Adapted from Nutt.21
The negative effects of depression on social functioning can be grouped into three main areas, ie, perceptual, cognitive, and performance. As shown in Figure 1, the symptoms of depression implicated in problems of social functioning (in underlined italics in Figure 1) are those resulting primarily from noradrenergic dysfunction.
The importance of noradrenergic neurotransmission in social functioning is supported by studies using the specific NE reuptake inhibitor, reboxetine, in healthy volunteers. The effects of reboxetine have been studied using a stranger-dyadic social interaction paradigm and cooperative game situations.23–25 Reboxetine was found to increase cooperative social behavior and social drive in healthy volunteers. In contrast, the selective serotonin reuptake inhibitor (SSRI), citalopram, had less effect on cooperative behavior.23 Two weeks’ enhancement of noradrenergic transmission induced by reboxetine made healthy volunteers more self-confident and assertive.25
Methods for assessing social adaptation
In the DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, 4th Edition) diagnostic criteria for major depression, the item “lack of interests” only partially covers the concept of decreased social ability. However, in addition to the simple presence of certain symptoms, the DSM-IV requires that symptoms should cause significant distress or impairment in social, occupational, or other important areas of functioning.26 Increasingly, the enhancement of social functioning is considered to be an important therapeutic target in the treatment of depression.15,26,27 The measurement of social adaptation should thus be an important part of assessment of the outcome of depression. A number of instruments have been developed to measure social functioning, each with its advantages and disadvantages.28
Although several self- or clinician-evaluated social adjustment scales are available, they are frequently complex and time-consuming, and their conceptual background is often poorly defined.29–31 The three most frequently used instruments for measuring social functioning are the 36-item Short-Form Health Survey,32 the Social Adjustment Scale Self-Report,33 and the more recently developed Social Adaptation Self-Evaluation Scale (SASS).29 It has been suggested28 that the SASS might be the most appropriate for studies exploring hypotheses about mechanisms involved in social dysfunction.
SASS instrument
The 21-item SASS was developed with two requirements, ie, simplicity of use and clear measurement of social behavior. It has been validated in a large sample of over 3000 people in the general population and in 496 depressed patients.26,27 The SASS explores social functioning in the areas of work, leisure, family and extrafamily relationships, global social attitude, and self-perception vis à vis the environment. The 21 items (Table 1) are scored from 0 to 3, (3 being maximal adjustment). Questions 1 and 2 are mutually exclusive, so that 20 questions are scored giving a total score range of 0 to 60. Normal scores are in the range 35–52.29 The test takes 5–10 minutes to complete.
Table 1.
Social Adaptation Self-Evaluation Scale questionnaire
| 21 questions exploring patient motivation and behavior25 |
|---|
|
As discussed above, major depressive episodes have an extensive impact on work and family functioning, and thus antidepressant treatment would be expected to lead to improved social functioning. The first comparative study to use the SASS to evaluate the effects of antidepressant treatment on social functioning was a randomized, double-blind, placebo-controlled, eight-week study comparing the selective NE reuptake inhibitor, reboxetine (8 mg/day) with the SSRI, fluoxetine (20 mg/day).34,35 At the end of the study, the mean SASS total score was significantly higher (P < 0.05) in both the reboxetine (n = 103) and fluoxetine (n = 100) groups compared with placebo (n = 99) group. The SASS total score in the reboxetine group, however, was significantly higher (P < 0.05) than in the fluoxetine group. Improvement from baseline in the three groups was reboxetine 41%, fluoxetine 31%, and placebo 14%. Correlation analysis showed that 19 out of 20 items of the SASS discriminated reboxetine from placebo, while only 12 items discriminated fluoxetine from placebo. Discrimination between the two antidepressants was maximal in the area of negative self-perception and lack of motivation towards action. In the subgroup of 91 patients in remission (Hamilton Depression Rating Scale [HAMD] ≤ 10) at the end of the study, the mean SASS total score for reboxetine was also significantly higher than that of both fluoxetine and placebo (P < 0.05). A direct comparison of reboxetine and fluoxetine showed that 14 SASS items showed a significantly greater improvement with reboxetine treatment.
Another study36 compared the effects of reboxetine 8–10 mg/day and fluoxetine 20–40 mg/day over eight weeks in 168 patients with acute major depressive episode. Both antidepressants improved scores on the HAMD to a similar extent. In patients treated for at least four weeks, the mean SASS total score was improved by 42.4% in the reboxetine group and 33.3% in the fluoxetine group, although this difference was not significantly different. In patients who achieved remission (HAMD ≤ 10), the mean SASS total score improvement in the reboxetine group was 43.5% compared with 29.37% in the fluoxetine group (P < 0.05). The quality of remission, in terms of social adjustment, was better in the reboxetine group, with greater improvement on almost all individual items compared with the fluoxetine group, and statistically significant differences for “interest in hobbies” (P = 0.02), “gregariousness” (P = 0.01), “difficulties in coping with resources” (P = 0.03), and “control of surroundings” (P = 0.04).
These studies suggest that noradrenergic agents, such as reboxetine, may be particularly effective in improving negative self-perception and lack of motivation, leading to a better quality of remission in terms of social functioning.37
A meta-analysis of nine studies (n = 2641 patients) of durations ranging over 8–24 weeks comparing reboxetine with fluoxetine, paroxetine, and citalopram38 showed comparable antidepressant response rates between reboxetine and the grouped SSRIs. However, the analysis failed to show a significant difference in improvement in psychosocial functioning, as measured by the SASS, between the reboxetine and SSRI groups, although the SASS was not used in all studies.
Effects of serotonin norepinephrine reuptake inhibitors on social adaptation
If improved social adaptation is related to increased noradrenergic activity, then SNRIs should be particularly effective in reducing social dysfunction in depressed patients. However, to date, the effects of SNRIs on social adaptation in depressed patients have been measured in only a few studies. There have been no studies using the SASS or another social adaptation scale comparing SNRIs and SSRIs.
Venlafaxine
A small study compared treatment with venlafaxine and amitriptyline on social functioning in depressed patients,39 although this study used the Self-Report Social Adjustment Scale (SAS-SR) and not the SASS. Twenty-eight outpatients, with recurrent or single major depressive episodes, took part in a double-blind, eight-week trial with amitriptyline or venlafaxine (both drugs administered at doses up to 150 mg/day), and were assessed by the SAS-SR at baseline and at the end of treatment. Both drugs showed comparable efficacy for improving depressive symptoms. Amitriptyline-treated patients showed a significant (P < 0.005) overall improved SAS-SR score and a significant improvement in several subscales (work P = 0.005; leisure time P = 0.006; economic situation P < 0.05). However, venlafaxine-treated patients showed a significantly greater improvement in social adjustment on the SAS-SR than those treated with amitriptyline (P < 0.05). Venlafaxine-treated patients showed a significant (P < 0.001) overall improved SAS-SR score and a significant improvement in all subscales except economic situation (work P < 0.001; leisure time, extended family, marital, parental, family unit P < 0.05). In addition, only venlafaxine-treated patients reached SAS-SR values in the range for normal subjects. This difference may reflect the greater noradrenergic component of venlafaxine’s mechanism of action.
In an open-label naturalistic case study, five patients with treatment-resistant severe major depressive disorder were treated with high-dose (450–600 mg/day) venlafaxine XL.40 At the end of the 24-week study, four of the five patients had a greater than 50% decrease in HAMD scores. For two of these patients, SASS scores were within the normal range at the end of the study.
Duloxetine
The only study of duloxetine using the SASS41 is a small study in seasonal affective disorder (SAD). Twenty-six patients suffering from SAD were treated in an open-label design with duloxetine (60–120 mg/day) for eight weeks. Duloxetine treatment led to a significant improvement (P < 0.001) of HAMD (SAD version) and SASS scores. Work days lost due to illness and days with reduced productivity were also significantly fewer (P < 0.001) at the end of treatment. These preliminary results suggest that duloxetine may improve the negative social consequences of SAD.
Milnacipran
Milnacipran is the most balanced of the SNRI in terms of its selectivity for the inhibition of NE and 5-HT reuptake and has the most noradrenergic potency ratio of all the SNRIs.42 As such, its effects on social adaptation would be expected to be particularly marked. Two recent studies have examined the effect of milnacipran on social adaptation as measured by the SASS. Both have been published exclusively in Japanese and will therefore be presented here in some detail because they are not otherwise available to most of the scientific community.
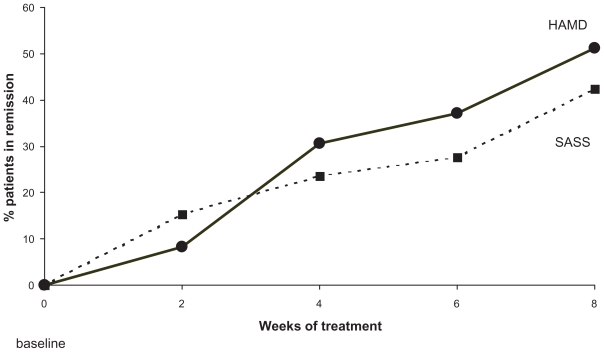
One study43 investigated 45 patients (28 men and 17 women, of mean age 46.2 years) diagnosed with major depressive disorder. Milnacipran was administered at 50 to 100 mg/day. The initial mean dose was 57.1 mg/day. The mean dose at the end of the eight-week study was 83.7 mg/day. HAMD, Beck Depression Inventory (BDI), and SASS were assessed at baseline and after 2, 4, 6, and 8 weeks treatment. Baseline scores were: HAMD 22.2; BDI 26.7; and SASS 24.4.
Significant improvements (P < 0.05) in the HAMD and BDI were seen after two weeks and in the SASS after four weeks. After eight weeks of treatment, 51.1% patients were in remission on HAMD (remission < 7) and 42.2% on SASS (remission > 35, Figure 2). Patients who did not respond to treatment (<50% reduction of baseline HAMD score after eight weeks) had no significant improvement in their SASS score at endpoint. The authors found a significant negative correlation between the reduction in HAMD score from baseline to endpoint (ΔHAMD) and the increase in SASS score from baseline to endpoint (ΔSASS, r = 0.598; P < 0.01).
Figure 2.
Patients in remission for depression and social adaptation during treatment with milnacipran. Remission for depression defined as Hamilton Depression Rating Scale < 7. Remission for social adaptation defined as Social Adaptation Self-Evaluation Scale > 35. Drawn from data.43
A second study investigated the effect of milnacipran treatment on the evolution of social adaptation using the SASS in parallel with the HAMD and the Zung Self-evaluation Depressive Rating Scale (SDS).44 A cohort of 113 patients (20–65 years), employees, or homemakers who carried out home tasks, diagnosed with major depressive episode according to the DSM-IV criteria, was recruited. Milnacipran was administered at a starting dose of 25–50 mg/day, increasing if necessary to 100 mg/day after 1–2 weeks and then continuing at this dose for 8–12 weeks. After 12 weeks the average dose was 85.4 mg/day.
Twelve of the 113 enrolled patients did not return after the first visit and were therefore excluded from the analysis. Five patients withdrew due to adverse effects within the first two weeks. Efficacy analysis, carried out on a total of 101 patients using the last observation carried forward technique, showed a significant improvement for all three scales at endpoint (P < 0.01). Mean HAMD and SDS scores were significantly reduced (P < 0.01) after two weeks whereas the SASS was only significantly increased (P < 0.01) from four weeks (Figure 3). After eight weeks, 67.4% patients were classified as responders (≥50% reduction of the baseline HAMD score), 43.0% were in remission (HAMD ≤ 7), and 33.3% patients had remission on SASS (≥35 points).
Figure 3.
Evolution of Hamilton Depression Rating Scale and Social Adaptation Self-Evaluation Scale scores during milnacipran treatment. *P < 0.01. Drawn from data.44
After four weeks, the dose had been increased to 100 mg/day in 23 patients, with 63 patients remaining at doses of less than 100 mg/day. Patients in the high-dose group had significantly greater improvements on the HAMD and SASS scales (Table 2).
Table 2.
Change in scores on the different rating scales from baseline to endpoint for high-dose and low-dose milnacipran groups
| ΔHAMD | ΔSDS | ΔSASS | |
|---|---|---|---|
| Low-dose group* | − 12.3 ± 8.2 | − 13.8 ± 10.9 | 4.0 ± 7.3 |
| High-dose group** | − 14.5 ± 9.5 | − 17.4 ± 12.0 | 9.8 ± 8.1 |
| P | 0.011 | 0.163 | 0.049 |
Notes: Patients whose dose of milnacipran had not been raised to 100 mg/day by the end of week 4 (n = 63);
Patients whose dose of milnacipran had been raised to 100 mg/day or more by the end of week 4 (n = 23); P = difference between high and low groups.
Abbreviations: SD, standard deviation; ΔHAMD, mean (±SD) difference in scores on the Hamilton Depression Rating Scale from baseline to endpoint; ΔSDS, mean (±SD) difference in scores on the Self-evaluation Depressive Rating scale from baseline to endpoint; ΔSASS, mean (±SD) difference in scores on the Social Adaptation Self-Evaluation Scale from baseline to endpoint. Developed from data.41
Although a third of patients achieved remission on the SASS after 12 weeks, the mean SASS score after 12 weeks (31.3 ± 3.7) was still below the remission level (>35). There was a significant negative correlation between ΔSASS (baseline to endpoint difference) and ΔHAMD (−0.39, P < 0.01) although the correlation was considerably weaker than between the two depression scales (ΔHAMD and ΔSDS; 0.74, P < 0.01).
Both of these Japanese studies showed a significant improvement on the SASS scale by four weeks of treatment, whereas a significant improvement on depression scales, ie, HAMD, BDI, and SDS, occurred by two weeks. Although both studies showed a significant negative correlation between changes in the SASS and changes in the HAMD, the correlation was weaker than between the two depression rating scales.
These results suggest that social adaptation, as measured by the SASS, may be more difficult and slower to achieve than improvement in classical depressive symptoms. In addition, although there is a correlation between SASS improvement and HAMD improvement, and the dispersion is greater than when comparing two depression scales, suggesting that in spite of certain similarities, the scales do not measure the same underlying functions. Finally, higher doses appear to favor a more rapid recovery from social dysfunction and thus a rapid return to productivity in the workplace and an overall improved quality of life.
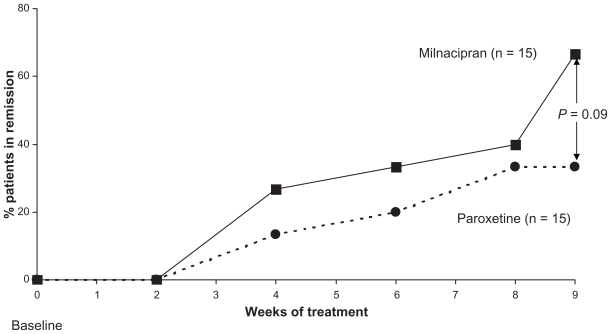
We have found mention of only a single study comparing improvement of social adaptation between SNRIs and SSRIs. A study presented orally in Japanese46 and cited in a review47 compared depressed patients (n = 15 per group) treated by milnacipran (mean dose 83 mg/day) or paroxetine (mean dose 35 mg/day). From the data presented47 (Figure 4), milnacipran treatment appears to result in a greater number of patients with social remission than paroxetine. Not surprisingly, in view of the small study population, the difference was not significant. This difference is consistent with that found in some studies between the selective NE reuptake inhibitor, reboxetine and the SSRI, fluoxetine (see above).34–36
Figure 4.
Social adaptation for patients in remission during treatment with milnacipran and paroxetine. Remission for social adaptation defined as Social Adaptation Self- Evaluation Scale > 35. Milnacipran was administered at a mean dose of 83 mg/day (n = 15) and paroxetine at 35 mg/day (n = 15). Drawn from data.46
Conclusions
Social dysfunction is a common feature in depressed patients and has important implications for quality of life. Because the level of social functioning may be significant in determining the course of the illness and risk of relapse,37 this aspect of depression merits particular attention. The role of antidepressants in alleviating social impairment is poorly studied, and it is unknown whether antidepressants act directly to affect mechanisms that mediate social functioning, or indirectly via clinical improvement of the core symptoms of depression. The effects of depression on social functioning fit into the monoamine hypothesis of depression through the improvement of symptoms related to noradrenergic function.21,22,45 The important implication of NE in social dysfunction in depression is supported by studies with antidepressants acting specifically on the noradrenergic system, such as reboxetine, both in healthy volunteers and in depressed patients.
There is a suggestion that antidepressants activating noradrenergic neurotransmission may improve social functioning more rapidly and/or to a greater extent than those acting exclusively on serotonergic function. If this is indeed true, SNRIs would also be expected to be particularly effective in improving social functioning.
The studies currently available are all small and many of them are not comparative. This is a clear limitation of support for the hypothesis. From these preliminary data, SNRIs do appear to improve social functioning, with possibly a slower time course than for the improvement of depressive symptoms. Although there is a first indication that milnacipran may possibly produce a greater effect on social adaptation than the SSRI, paroxetine, this interesting question is still open. We hope that this review will stimulate the curiosity of investigators and encourage then to include the SASS in future trials comparing SNRIs and SSRIs.
Footnotes
Disclosure
CM reports no conflict of interest in this work. MB is a consultant for Pierre Fabre Médicament, Asahi Kasei Pharma, Germania Pharmaceutica, Janssen Pharmaceutica, and Cypress BioScience.
References
- 1.Henderson S. A development in social psychiatry. The systematic study of social bonds. J Nerv Ment Dis. 1980;168(2):63–69. doi: 10.1097/00005053-198002000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Weissman MM. The assessment of social functioning. A review of techniques. Arch Gen Psychiatry. 1975;32(3):357–365. doi: 10.1001/archpsyc.1975.01760210091006. [DOI] [PubMed] [Google Scholar]
- 3.Weissman MM, Klerman GL, Paykel ES, et al. Treatment effects on the social adjustment of depressed patients. Arch Gen Psychiatry. 1974;30(6):771–778. doi: 10.1001/archpsyc.1974.01760120033006. [DOI] [PubMed] [Google Scholar]
- 4.Paykel ES, Weissman MM, Prusoff BA. Social maladjustment and severity of depression. Compr Psychiatry. 1978;19(2):121–128. doi: 10.1016/0010-440x(78)90056-1. [DOI] [PubMed] [Google Scholar]
- 5.Hays RD, Wells KB, Sherboume CD, et al. Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry. 1995;52(1):11–19. doi: 10.1001/archpsyc.1995.03950130011002. [DOI] [PubMed] [Google Scholar]
- 6.Leader JB, Klein DN. Social adjustment in dysthymia, double depression and episodic major depression. J Affect Disord. 1996;37:2–3. 91–101. doi: 10.1016/0165-0327(95)00076-3. [DOI] [PubMed] [Google Scholar]
- 7.Tse WS, Bond AJ. The impact of depression on social skills. J Nerv Ment Dis. 2004;192(4):260–268. doi: 10.1097/01.nmd.0000120884.60002.2b. [DOI] [PubMed] [Google Scholar]
- 8.Katon W. The impact of depression on workplace functioning and disability costs. Am J Manag Care. 2009;15(Suppl 11):S322–S327. [PubMed] [Google Scholar]
- 9.Stefos G, Bauwens F, Staner L, et al. Psychosocial predictors of major affective recurrences in bipolar disorder: A 4-year longitudinal study of patients on prophylactic treatment. Acta Psychiatr Scand. 1996;93(6):420–426. doi: 10.1111/j.1600-0447.1996.tb10672.x. [DOI] [PubMed] [Google Scholar]
- 10.Dourish CT, Gorka Z, Williams AR, Iversen SD. Potential influence of social support in a rodent model of depression. J Psychopharmacol. 1989:38. [Google Scholar]
- 11.Jenks Kettmann JD, Altmaier EM. Social support and depression among bone marrow transplant patients. J Health Psychol. 2008;13(1):39–46. doi: 10.1177/1359105307084310. [DOI] [PubMed] [Google Scholar]
- 12.Symister P, Friend R. The influence of social support and problematic support on optimism and depression in chronic illness: A prospective study evaluating self-esteem as a mediator. Health Psychol. 2003;22(2):123–129. doi: 10.1037//0278-6133.22.2.123. [DOI] [PubMed] [Google Scholar]
- 13.Gao Y, MacDonald D, Collins KD, Alaghehbandan R, Chen Y. Role of social support in the relationship between sexually transmitted infection and depression among young women in Canada. J Epidemiol. 2010;20(4):313–318. doi: 10.2188/jea.JE20090133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carlsson A, Corrodi H, Fuxe K, Hökfelt T. Effect of antidepressant drugs on the depletion of intraneuronal brain 5-hydroxytryptamine stores caused by 4-methyl-alpha-ethyl-meta-tyramine. Eur J Pharmacol. 1969;5(4):357–366. doi: 10.1016/0014-2999(69)90113-7. [DOI] [PubMed] [Google Scholar]
- 15.Healy D, McMonagle T. The enhancement of social functioning as a therapeutic principle in the management of depression. J Psychopharmacol. 1997;11(Suppl 4):S25–S31. [PubMed] [Google Scholar]
- 16.Charney DS. Monoamine dysfunction and the pathophysiology and treatment of depression. J Clin Psychiatry. 1998;59(Suppl 14):11–14. [PubMed] [Google Scholar]
- 17.Leonard BE. Noradrenaline in basic models of depression. Eur Neuropsychopharmacol. 1997;7(Suppl 1):S11–S16. doi: 10.1016/s0924-977x(97)00415-x. [DOI] [PubMed] [Google Scholar]
- 18.Bymaster FP, McNamara RK, Tran PV. New approaches to developing antidepressants by enhancing monoaminergic neurotransmission. Expert Opin Investig Drugs. 2003;12(4):531–543. doi: 10.1517/13543784.12.4.531. [DOI] [PubMed] [Google Scholar]
- 19.Neumeister A. Tryptophan depletion, serotonin, and depression: Where do we stand? Psychopharmacol Bull. 2003;37(4):99–115. [PubMed] [Google Scholar]
- 20.Klimek V, Schenck JE, Han H, et al. Dopaminergic abnormalities in amygdaloid nuclei in major depression: A postmortem study. Biol Psychiatry. 2002;52(7):740–748. doi: 10.1016/s0006-3223(02)01383-5. [DOI] [PubMed] [Google Scholar]
- 21.Nutt DJ. Relationship of neurotransmitters to the symptoms of major depressive disorder. J Clin Psychiatry. 2008;69(Suppl E1):4–7. [PubMed] [Google Scholar]
- 22.Kasper S, Pail G. Milnacipran: A unique antidepressant? Neuropsychiatr Dis Treat. 2010;6(Suppl 1):23–31. doi: 10.2147/NDT.S11777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tse WS, Bond AJ. Difference in serotonergic and noradrenergic regulation of human social behaviours. Psychopharmacology (Berl) 2002;159(2):216–221. doi: 10.1007/s00213-001-0926-9. [DOI] [PubMed] [Google Scholar]
- 24.Tse WS, Bond AJ. Reboxetine promotes social bonding in healthy volunteers. J Psychopharmacol. 2003;17(2):189–195. doi: 10.1177/0269881103017002007. [DOI] [PubMed] [Google Scholar]
- 25.Tse WS, Bond AJ. Noradrenaline might enhance assertive human social behaviours: An investigation in a flatmate relationship. Pharmacopsychiatry. 2006;39(5):175–179. doi: 10.1055/s-2006-948328. [DOI] [PubMed] [Google Scholar]
- 26.Bech P. Social functioning: Should it become an endpoint in trials of antidepressants? CNS Drugs. 2005;19(4):313–324. doi: 10.2165/00023210-200519040-00004. [DOI] [PubMed] [Google Scholar]
- 27.Daly EJ, Trivedi MH, Wisniewski SR, et al. Health-related quality of life in depression: A STAR*D report. Ann Clin Psychiatry. 2010;22(1):43–55. [PubMed] [Google Scholar]
- 28.Weissman MM, Olfson M, Gameroff MJ, et al. A comparison of three scales for assessing social functioning in primary care. Am J Psychiatry. 2001;158(3):460–466. doi: 10.1176/appi.ajp.158.3.460. [DOI] [PubMed] [Google Scholar]
- 29.Bosc M, Dubini A, Polin V. Development and validation of a social functioning scale, the Social Adaptation Self-evaluation Scale. Eur Neuropsychopharmacol. 1997;7(Suppl 1):S57–S70. doi: 10.1016/s0924-977x(97)00420-3. [DOI] [PubMed] [Google Scholar]
- 30.Bosc M. Assessment of social functioning in depression. Compr Psychiatry. 2000;41(1):63–69. doi: 10.1016/s0010-440x(00)90133-0. [DOI] [PubMed] [Google Scholar]
- 31.Healy D. Reboxetine: Its effects as measured by the Social Adaptation Self-evaluation Scale. Acta Psychiatr Scand. 2000;402(Suppl):45–51. doi: 10.1034/j.1600-0447.2000.02608.x. [DOI] [PubMed] [Google Scholar]
- 32.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 33.Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiatry. 1976;33(9):1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 34.Dubini A, Bosc M, Polin V. Do noradrenaline and serotonin differentially affect social motivation and behaviour? Eur Neuropsychopharmacol. 1997;7(Suppl 1):S49–S55. doi: 10.1016/s0924-977x(97)00419-7. [DOI] [PubMed] [Google Scholar]
- 35.Dubini A, Bosc M, Polin V. Noradrenaline-selective versus serotonin- selective antidepressant therapy: Differential effects on social functioning. J Psychopharmacol. 1997;11(Suppl 4):S17–S23. [PubMed] [Google Scholar]
- 36.Massana J, Möller HJ, Burrows GD, Montenegro RM. Reboxetine: A double-blind comparison with fluoxetine in major depressive disorder. Int Clin Psychopharmacol. 1999;14(2):73–80. doi: 10.1097/00004850-199903000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Keller M. Role of serotonin and noradrenaline in social dysfunction: A review of data on reboxetine and the Social Adaptation Self-evaluation Scale (SASS) Gen Hosp Psychiatry. 2001;23(1):15–19. doi: 10.1016/s0163-8343(00)00115-8. [DOI] [PubMed] [Google Scholar]
- 38.Papakostas GI, Nelson JC, Kasper S, Möller HJ. A meta-analysis of clinical trials comparing reboxetine, a norepinephrine reuptake inhibitor, with selective serotonin reuptake inhibitors for the treatment of major depressive disorder. Eur Neuropsychopharmacol. 2008;18(2):122–127. doi: 10.1016/j.euroneuro.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 39.Gorenstein C, Andrade L, Moreno RA, Artes R. Social adjustment in depressed patients treated with venlafaxine and amitriptyline. Int Clin Psychopharmacol. 2002;17(4):171–175. doi: 10.1097/00004850-200207000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Mbaya P. Safety and efficacy of high dose of venlafaxine XL in treatment resistant major depression. Hum Psychopharmacol. 2002;17(7):335–339. doi: 10.1002/hup.419. [DOI] [PubMed] [Google Scholar]
- 41.Pjrek E, Willeit M, Praschak-Rieder N, et al. Treatment of seasonal affective disorder with duloxetine: An open-label study. Pharmacopsychiatry. 2008;41(3):100–105. doi: 10.1055/s-2008-1058103. [DOI] [PubMed] [Google Scholar]
- 42.Stahl SM, Grady MM, Moret C, Briley M. SNRIs: Their pharmacology, clinical efficacy, and tolerability in comparison with other classes of antidepressants. CNS Spectr. 2005;10(9):732–747. doi: 10.1017/s1092852900019726. [DOI] [PubMed] [Google Scholar]
- 43.Ueda N, Yoshimura R, Houjo T, et al. Effects of milnacipran on social adaptation in patients with depression. Rinshyo Seisin Yakuri. 2008;11(2):273–279. [Google Scholar]
- 44.Ishida T, Inada Y, Kudo M, et al. Study on the clinical efficacy of milnacipran by using the Social Adaptation Self-evaluation Scale. Jpn J Clin Psychopharmacol. 2010;13:77–83. [Google Scholar]
- 45.Möller HJ. Are all antidepressants the same? J Clin Psychiatry. 2000;61(Suppl 6):24–28. [PubMed] [Google Scholar]
- 46.Ueda H, Takashi H, Mayumi K. Effect of paroxetine and milnacipran on social adaptation in depressed patients (in Japanese). Presented at the 15th Japan Society for Clinical and Neuropsychiatric Pharmacology meeting; 2005; Tokyo. [Google Scholar]
- 47.Yoshimura R. Treatment in depression for achieving remission – from drug selection to returning to workplace. Jpn J Clin Psychopharmacol. 2008;11(6):213–220. [Google Scholar]