Abstract
Background:
Current data on bronchiectasis prevalence, trends, and risk factors are lacking; such data are needed to estimate the burden of disease and for improved medical care and public health resource allocation. The objective of the present study was to estimate the trends and burden of bronchiectasis-associated hospitalizations in the United States.
Methods:
We extracted hospital discharge records containing International Classification of Diseases, 9th Revision, Clinical Modification codes for bronchiectasis (494, 494.0, and 494.1) as any discharge diagnosis from the State Inpatient Databases from the Agency for Healthcare Research and Quality. Discharge records were extracted for 12 states with complete and continuous reporting from 1993 to 2006.
Results:
The average annual age-adjusted hospitalization rate from 1993 to 2006 was 16.5 hospitalizations per 100,000 population. From 1993 to 2006, the age-adjusted rate increased significantly, with an average annual percentage increase of 2.4% among men and 3.0% among women. Women and persons aged > 60 years had the highest rate of bronchiectasis-associated hospitalizations. The median cost for inpatient care was 7,827 US dollars (USD) (range, 13-543,914 USD).
Conclusions:
The average annual age-adjusted rate of bronchiectasis-associated hospitalizations increased from 1993 to 2006. This study furthers the understanding of the impact of bronchiectasis and demonstrates the need for further research to identify risk factors and reasons for the increasing burden.
Bronchiectasis is a potentially serious condition related to permanent and abnormal widening of the airways. Common characteristics of bronchiectasis include chronic cough, sputum production, hemoptysis, and shortness of breath.1-3 Multiple factors can contribute to bronchiectasis, including chronic lung infection, foreign objects in the airways, and inherited disorders such as cystic fibrosis and primary ciliary dyskinesia.4
The current epidemiology of bronchiectasis in the United States has not been well described. The only recent US study was a retrospective cohort design with > 56 million patients from multiple US health plans, which used International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes to estimate a prevalence of 52.3 cases of bronchiectasis per 100,000 adults.5
Previous studies have suggested that the incidence among children and the overall prevalence of bronchiectasis may be declining in areas of the United States in part because of childhood immunizations and increased use of broad-spectrum antibiotics.2,6 There is evidence of a higher prevalence among women, although comparisons are limited by study designs and populations.5,7-12 Recent studies have found that those > 50 years are most affected.5,9
Bronchiectasis may require extensive medical care and hospitalization. Based on health-care claims data from outpatient and inpatient settings, the total medical care expenditures average $5,681 more than those for nonbronchiectasis patients.5 A Finnish study found the average length of stay for bronchiectasis-associated hospitalizations to be 7 days.13 A current estimate for the length of bronchiectasis-associated hospitalizations within the United States is not available, nor is the proportion of persons hospitalized with bronchiectasis.
Population-based databases at the state level are available that allow estimation of the hospitalization rate and trends for any condition with an ICD-9-CM code. ICD-9-CM codes are used primarily for payment reimbursement purposes; however, they are used frequently in epidemiologic research to describe burden and trends. State Inpatient Databases (SID) are compiled by the US Agency for Healthcare Research and Quality (AHRQ) through the Healthcare Cost and Utilization Project.14 The SID include data beginning in 1988 and currently include 40 participating states, contributing hospital discharge information from nearly 90% of all US hospital discharges.14 Thus, the AHRQ SID databases provide an excellent resource to assess the population-based frequency and cost of hospitalization for this disease.
We believe this study represents the most comprehensive assessment of bronchiectasis-associated hospitalizations in the United States and provides insights into the overall trends and burden of bronchiectasis in the US population.
Materials and Methods
Data Source and Population
We extracted data from the SID, which contain record-level information on inpatient hospital discharges without patient identifiers. We extracted records for which the ICD-9-CM codes for bronchiectasis were listed as any discharge diagnosis. The ICD-9-CM codes listed as the primary discharge diagnosis code generally indicate the principal condition identified or diagnosis during hospitalization, whereas the secondary codes indicate contributing or associated (“comorbid”) conditions. These bronchiectasis codes included 494 (bronchiectasis [before October 2000]), 494.0 (bronchiectasis without acute exacerbation), and 494.1 (bronchiectasis with acute exacerbation [October 2000 forward]). In October 2000, the ICD-9-CM code for bronchiectasis was split into two codes to indicate bronchiectasis with and without acute exacerbation. We chose to include all bronchiectasis with and without exacerbation for consistency in trend analysis. Variables collected for each discharge record included year of admission, state of hospitalization, age at admission, sex, length of hospitalization, total charges from hospitalization, associated conditions as indicated by ICD-9-CM codes (primary discharge diagnosis through discharge diagnosis number 30), and whether the patient died while in hospital. Data were analyzed from states with complete and continuous reporting from 1993 through 2006 (Arizona, California, Colorado, Connecticut, Florida, Iowa, Maryland, New Jersey, New York, South Carolina, Washington, and Wisconsin), representing ∼ 40% of the total US population in 2000.
Data Analysis
Analysis was limited to records with bronchiectasis as a discharge diagnosis (ICD-9-CM: 494, 494.0, and 494.1) from the 12 states contributing data from 1993 through 2006. US census age- and sex-specific state population data were used as the denominator for all rates of hospitalization calculations. We adjusted for age to control for different age distributions among states and to make the overall estimate from the study population comparable to the US population. Age-adjusted hospitalization rates were calculated using US Census 2000 population as the reference population.
Poisson regression was used to assess the significance of trends (P < .05). Standard errors from Poisson regression were scaled using the Pearson χ2 dispersion statistic to account for overdispersion. Model fit was assessed with the Pearson χ2 statistic.
The study file was analyzed for associated conditions for two groups: (1) primary diagnoses from all records and (2) secondary diagnoses among records with bronchiectasis as a primary diagnosis. COPD and pneumonia/influenza ICD-9-CM code groupings were based on COPD and pneumonia/influenza classifications provided by AHRQ clinical classification software.15 We analyzed the total hospital costs instead of charges because cost has been shown to better represent economic impact.16-18 Total cost of hospital stay was calculated from total charges available in the SID using the cost-to-charge ratio developed by AHRQ.19 Analysis of hospital costs was limited to the 12 states from 1999 through 2006 because of the years available in the AHRQ cost-to-charge ratio files. We used the cost-to-charge ratio specific to hospital groups as defined by AHRQ cost-to-charge files.19 Total costs approximate the cost of providing the inpatient service. These estimated costs do not include physician services.19 Annual readmission information was available for five states for 2005 and 2006 from the AHRQ revisit files. We used this information to estimate the frequency of repeated admissions within the year. All analysis was completed using SAS, versions 9.1 and 9.2 (SAS Institute; Cary, NC). Because the SID were deidentified and not collected specifically for this study, institutional review board approval was not required.
Results
From 1993 to 2006, 258,947 bronchiectasis-associated hospitalizations were identified, of which 163,021 (63%) were among women. Overall, 181,456 (70%) were among persons aged ≥ 65 years. The median age of persons hospitalized with bronchiectasis was significantly higher in women than in men (women, 75 years; men, 71 years). For hospitalizations with bronchiectasis as the primary diagnosis from 2000 to 2006, 57% (14,735) were coded as bronchiectasis with acute exacerbation (494.1), 35% (9,142) were coded as bronchiectasis without acute exacerbation (494.0) and 8% (2,142) were coded as bronchiectasis (494). Among the 35% of hospitalizations with the code of bronchiectasis without acute exacerbation, there were a variety of codes as the second diagnosis, with the most frequent being hemoptysis (21%, n = 1,957). The remainder of the comorbid conditions each accounted for < 5%.
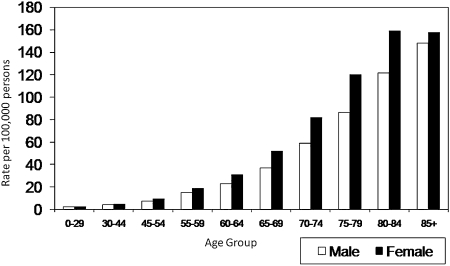
The average annual age-adjusted rate of bronchiectasis-associated hospitalizations in the 12 states with data from 1993 through 2006 was 16.5 hospitalizations per 100,000 population. The rate varied greatly by age and sex, with the highest rate among women and older persons; the relative rate for persons aged 80-84 years compared with persons aged 55-59 years was 8.5-fold higher among women (161 vs 19) and eightfold higher among men (121 vs 15) (Fig 1). The average annual age-adjusted rate of hospitalization with bronchiectasis as a primary diagnosis from 1993-2006 was 2.0 per 100,000 population.
Figure 1.
Average annual rate of bronchiectasis-associated (primary and secondary discharge diagnoses) hospitalizations by age and sex in 12 states, 1993-2006, in the United States.
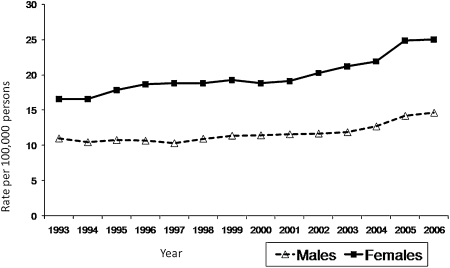
Age-adjusted rates of bronchiectasis-associated hospitalizations increased significantly among both men and women, with the highest annual percentage change (APC) among women. The APC from 1993 to 2006 was 2.4% for men and 3.0% for women (Table 1). The increasing trend was most marked from 2001 through 2006, with an APC of 5.5% for men and 5.9% for women (Fig 2). Among records with bronchiectasis as the primary diagnosis, the APC from 1993 to 2006 was 1.7% for men and 2.6% for women. The APC among records with bronchiectasis as a primary diagnosis from 2001 to 2006 was not significant for men or women. The overall APC for women significantly increased in more states than did the APC for men: of the 12 states included in the analysis from 1993 to 2006, 10 showed a significant positive APC for women, seven showed a significant positive APC for men, and seven showed a significant positive APC for both men and women (Table 1). The state with the highest annual percentage increase from 1993 to 2006 for women was Connecticut (6.2 annual percentage increase) and for men was South Carolina (7.1 annual percentage increase).
Table 1.
—Age-Adjusted Rates of Hospitalization and Annual Percentage Change for Men and Women in Each State, 1993-2006
| Men |
Women |
|||||
| State | Age-Adjusted Rate | APC | 95% CI | Age-Adjusted Rate | APC | 95% CI |
| All 12 states | 12.27 | 2.36a | (1.62-3.11) | 20.57 | 2.97a | (2.35-3.60) |
| Arizona | 15.68 | 0.53 | (–0.68-1.76) | 28.73 | 0.14 | (–1.27-1.56) |
| California | 12.40 | 3.49a | (2.42-4.57) | 22.57 | 3.63a | (3.03-4.24) |
| Colorado | 9.32 | 0.92 | (–0.44-2.31) | 18.76 | 1.92a | (0.43-3.43) |
| Connecticut | 10.26 | 4.44a | (3.06-5.82) | 18.23 | 6.21a | (5.37-7.05) |
| Florida | 13.83 | 2.05a | (1.39-2.71) | 23.95 | 3.20a | (2.65-3.76) |
| Iowa | 12.16 | –0.64 | (–2.71-1.48) | 20.52 | 2.00a | (0.94-3.07) |
| Maryland | 11.38 | 2.22 | (–0.28-4.82) | 18.36 | 1.81 | (–0.12-3.76) |
| New Jersey | 12.24 | 0.88 | (–0.09-1.88) | 19.40 | 3.18a | (2.57-3.79) |
| New York | 13.50 | 1.42a | (0.28-2.56) | 18.01 | 3.98a | (3.09-4.88) |
| South Carolina | 12.99 | 7.10a | (5.60-8.61) | 21.89 | 4.85a | (3.93-5.80) |
| Washington | 8.30 | 4.63a | (3.41-5.89) | 14.91 | 3.17a | (2.18-4.17) |
| Wisconsin | 8.36 | 3.02a | (2.04-4.02) | 13.60 | 3.11a | (2.36-3.84) |
APC = annual percentage change.
Statistical significance at P < .001.
Figure 2.
Age-adjusted rate of bronchiectasis-associated (primary and secondary discharge diagnoses) hospitalizations by year in 12 states, 1993-2006, in the United States.
Among all records with a bronchiectasis discharge diagnosis, the most frequent primary diagnosis was pneumonia and influenza, with 25% of hospitalizations (62,799) receiving this as a primary discharge diagnosis. Eighteen percent of hospitalizations (45,883) had bronchiectasis as the primary discharge diagnosis (Table 2). Among hospitalizations with bronchiectasis as a primary diagnosis, the most frequent secondary diagnoses were hemoptysis (21%; n = 9749), Pseudomonas infection (16%; n = 7344), and COPD (16%; n = 7360) (Table 3).
Table 2.
—Primary Diagnoses for Bronchiectasis-Associated Hospitalizations, 1993-2006, Healthcare Cost and Utilization Project, State Inpatient Database
| ICD-9-CM | Primary Diagnosis | Frequency | Percentage |
| 494, 494.0, 494.1 | Bronchiectasis | 45,883 | 17.97 |
| 490, 491.0, 491.1, 491.20, 491.21 491.22, 491.8, 491.9, 492.0, 492.8, 496 | COPDa,b | 18,235 | 7.14 |
| Multiple codes and ranges as defined by AHRQ CCSa,c | Pneumonia and influenzaa,c | 62,799 | 24.60 |
| 428.0 | Congestive heart failure | 6,929 | 2.71 |
| 277.00, 277.01, 277.02, 277.03, 277.09 | Cystic fibrosis | 3,513 | 1.38 |
| 515 | Postinflammatory pulmonary fibrosis | 3,238 | 1.27 |
| 031.0 | Pulmonary non-TB mycobacteria | 1,714 | 0.67 |
| Other primary diagnosis | 103,705 | 44.26 | |
| E or V codes | 3,635 | 1.40 | |
| Missing | 6 | 0.0023 | |
| Total | 258,947 | 100 |
AHRQ = Agency for Healthcare Research and Quality; CCS = Clinical Classification Software; ICD-9-CM = International Classification of Diseases, 9th Revision, Clinical Modification.
Classified using AHRQ CCS for ICD-9 codes.
Excluding bronchiectasis.
Excluding pulmonary mycobacteria.
Table 3.
—Secondary Diagnoses When Bronchiectasis Is the Primary Diagnosis During Hospitalization, 1993-2006, Healthcare Cost and Utilization Project, State Inpatient Database
| Secondary Diagnosis | Hospitalizations Ending in Deatha (n = 1,099), No. (%) | Hospitalizations Not Ending in Deatha (n = 44,771), No. (%) | Totala (N = 45,883), No. (%) | |
| 490, 491.0, 491.1, 491.20,491.21, 491.22, 491.8, 491.9, 492.0, 492.8, 496, 491, 491.2 | COPDb,c | 190 (17.28) | 4,804 (16.01) | 7,360 (16.04) |
| 786.3 | Hemoptysis | 181 (16.5) | 9,565 (21.4) | 9,749 (21.2) |
| 041.7 | Pseudomonas infection | 108 (9.8) | 7,234 (16.2) | 7,344 (16.0) |
| 428.0 | Congestive heart failure | 255 (23.2) | 3,876 (8.7) | 4,132 (9.0) |
| 427.31 | Atrial fibrillation | 229 (20.8) | 3,716 (8.3) | 3,945 (8.6) |
| 515 | Postinflammatory pulmonary fibrosis | 120 (10.9) | 3,354 (7.5) | 3,474 (7.6) |
| 277.00, 277.01, 277.02, 277.03, 277.09 | Cystic fibrosis total | 44 (4.0) | 3,074 (6.9) | 3,115 (6.8) |
| Multiple codes and ranges as defined by AHRQ CCSb,d | Pneumonia and influenzab,d | 344 (31.3) | 4,524 (10.1) | 4,876 (10.6) |
| 031.0 | Pulmonary non-TB mycobacteria | 24 (2.2) | 686 (1.5) | 711 (1.5) |
Overall, 4.6% of patients did not survive to discharge, but survival did not vary by whether bronchiectasis was a primary or secondary discharge diagnosis. Among men, 5.3% did not survive, compared with 4.1% among women. Among all patients with bronchiectasis, those aged 80 to 84 years were 1.8-fold more likely to die during hospitalization than those aged 55 to 59 years (5.5 vs 3.0 deaths per 100 hospitalizations with bronchiectasis). Among hospitalizations for patients who died during their hospital stay, 31.3% had pneumonia and influenza as a secondary discharge diagnosis (n = 344) compared with only 10.1% (n = 4,524) of hospitalizations in which the patient did not die (Table 3).
The overall median length of hospital stay was 6 days and did not vary by sex. However, the median length of hospital stay was greater for patients who did not survive to discharge compared with patients who did survive to discharge (died, 8 days; survived, 6 days). The median cost for inpatient care among the 12 states from 1999 to 2006 was 7,827 US dollars (USD) (range, 13-543,914 USD). The median cost varied slightly by sex (men, 8,345 USD; women, 7,550 USD) but varied greatly by the survival status of the patient (died, 15,524 USD; survived, 7,688 USD).
Data on readmission were limited. In the five states with readmission information, 81% of patients had only one hospital admission in 2005 and 82% had only one hospitalization in 2006. Thirteen percent of patients with bronchiectasis-associated hospitalizations had exactly two hospitalizations in 2005 and 12% in 2006. In 2005, 6.6% of patients, and in 2006, 5.7% of patients, had three or more hospital visits.
Discussion
To our knowledge, this is the first population-based, representative analysis of bronchiectasis-associated hospitalizations in the United States. We identified a significant increase in bronchiectasis-associated hospitalizations from 1993 to 2006 across 12 states, with the highest average annual increase of 5.7% for the period from 2001 through 2006. The overall rate of 16.5 hospitalizations per 100,000 population is very similar to the rate in Hong Kong, of 16.4 hospitalizations per 100,000 population.20 This newly identified increase in bronchiectasis-associated hospitalizations supports the observation of an increased prevalence among persons > 60 years and among women, as found by Weycker et al.5
No single condition was associated with all bronchiectasis hospitalizations. Bronchiectasis as a primary diagnosis contributed to less than one-fifth of the total hospitalizations associated with bronchiectasis, indicating that patients may be entering the hospital because of a more emergent and acute condition, such as pneumonia, and bronchiectasis may be discovered during diagnostic testing. However, the clinical significance of bronchiectasis as a secondary diagnosis is unknown. The median hospital stay and total cost of hospitalization for patients who died before discharge were significantly higher than for those who survived hospitalization, suggesting more severe disease at admission.
Although the increase in the rate of bronchiectasis-associated hospitalizations may reflect an actual increase in the prevalence of the condition, the increased use of CT scans is likely also an important contributor to the increased detection of this condition. CT scans have become more available and display better resolution, allowing bronchiectasis to be identified in more patients. Increased clinical recognition and identification of bronchiectasis could result in a higher rate of bronchiectasis-associated hospitalization, even if the actual incidence and prevalence of bronchiectasis in the population have not changed. This possibility is supported by the fact that most patients entered the hospital because of a condition other than bronchiectasis. The greater availability and better resolution of CT scans makes bronchiectasis more likely to be recognized during a hospitalization.
Limitations inherent in these data should be considered while interpreting the results. The data were extracted from the SID based on ICD-9-CM codes. Although this may identify hospitalizations of interest, it may lead to under- or overestimates of disease prevalence because these codes are used primarily for purposes of billing, and only secondarily for epidemiologic research.21 Billing practices such as unbundling to obtain higher reimbursement may lead to inconsistencies in ICD-9-CM coding at the hospital level.21 Moreover, the use of ICD-9-CM codes for this analysis has not been validated previously, so some misclassification of bronchiectasis status could exist; the database could include hospitalizations not correctly associated with bronchiectasis or, more likely, miss hospitalizations that should be associated with bronchiectasis, further underestimating the prevalence.
A second limitation results from the anonymized nature of this data set, such that multiple hospitalizations for a given person could not be linked across all years when estimating the rate of hospitalization with bronchiectasis. If persons had multiple hospitalizations within a given year, we could have overestimated the burden of bronchiectasis in the population by using bronchiectasis-assiociated hospitalizations. However, using the AHRQ revisit database, we were able to get estimates for the number of admissions per patient for 2005 and 2006 in five of the states in our study. Although this information is limited, most patients with bronchiectasis-associated admissions had only a single admission in either 2005 or 2006 (81% and 82%, respectively).
Because most patients with bronchiectasis are not hospitalized, the rate of bronchiectasis-associated hospitalization will underestimate the prevalence of bronchiectasis in the US population. With hospitalization data, we are more likely to be describing severe bronchiectasis or bronchiectasis as a secondary condition, because patients would only be in this database if they were admitted to the hospital for bronchiectasis or if bronchiectasis were diagnosed during the admission. Illnesses seen only as outpatient visits would have been missed in this analysis, resulting in additional underestimation of the prevalence of bronchiectasis. In addition, we were not able to find published data regarding the percentage of people with bronchiectasis requiring hospitalization.
Conclusions
Bronchiectasis-associated hospitalizations increased from 1993 to 2006. The rate of bronchiectasis-associated hospitalizations increased markedly, starting around age 50, with the highest rate in the oldest age groups and in older women in particular. The increasing trend in bronchiectasis-associated hospitalizations highlights the need for further research to determine the full burden and risk factors for occurrence and progression of this debilitating disease.
Acknowledgments
Author contributions: Ms Seitz: contributed to the design of the study, data collection, and analysis of the data, and was the primary author of the manuscript.
Dr Olivier: contributed to the design of the study, analysis of the data, and editing of the manuscript.
Dr Steiner: contributed to the access to the data, data collection, and editing of the manuscript.
Mr Montes de Oca: contributed to the data collection, data management, and analysis.
Dr Holland: contributed to the design of the study and editing of the manuscript.
Dr Prevots: contributed to the design of the study, data collection, analysis of the data, and writing of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The views expressed in this article are those of the authors and do not necessarily reflect those of the AHRQ or the US Department of Health and Human Services.
Other contributions: The authors thank Pamela A. Shaw for her valuable statistical support and Cecile Viboud for her indispensable support and advice. The authors acknowledge the state data organizations that participated in the Healthcare Cost and Utilization Project SID, 1993-2006.
Abbreviations
- AHRQ
Agency for Healthcare Research and Quality
- APC
annual percentage change
- ICD-9-CM
International Classification of Diseases, 9th Revision, Clinical Modification
- SID
State Inpatient Databases
- USD
US dollars
Funding/Support: This research was supported by the Intramural Research Program of the National Institutes of Health, National Institute of Allergy and Infectious Diseases.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (http://www.chestpubs.org/site/misc/reprints.xhtml).
References
- 1.Rosen MJ. Chronic cough due to bronchiectasis: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):122S–131S. doi: 10.1378/chest.129.1_suppl.122S. [DOI] [PubMed] [Google Scholar]
- 2.Barker AF. Bronchiectasis. N Engl J Med. 2002;346(18):1383–1393. doi: 10.1056/NEJMra012519. [DOI] [PubMed] [Google Scholar]
- 3.Wynn-Williams N. Bronchiectasis: a study centred on Bedford and its environs. BMJ. 1953;1(4821):1194–1199. doi: 10.1136/bmj.1.4821.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barker AF, Bardana EJ., Jr Bronchiectasis: update of an orphan disease. Am Rev Respir Dis. 1988;137(4):969–978. doi: 10.1164/ajrccm/137.4.969. [DOI] [PubMed] [Google Scholar]
- 5.Weycker D, Edelsberg J, Oster G, Tino G. Prevalence and economic burden of bronchiectasis. Clin Pulm Med. 2005;12(4):205–209. [Google Scholar]
- 6.Glauser E, Cook C, Harris G. Bronchiectasis: a review of 187 cases in children with follow-up pulmonary function studies in 58. Acta Paediatr Scand. 1966;55(Suppl 165):3–16. doi: 10.1111/j.1651-2227.1966.tb14958.x. [DOI] [PubMed] [Google Scholar]
- 7.Davis MB, Jr, Hopkins WA, Wansker WC. The present status of the treatment of bronchiectasis. Am Rev Respir Dis. 1962;85:816–820. doi: 10.1164/arrd.1962.85.6.816. [DOI] [PubMed] [Google Scholar]
- 8.Keistinen T, Säynäjäkangas O, Tuuponen T, Kivelä SL. Bronchiectasis: an orphan disease with a poorly-understood prognosis. Eur Respir J. 1997;10(12):2784–2787. doi: 10.1183/09031936.97.10122784. [DOI] [PubMed] [Google Scholar]
- 9.Nicotra MB, Rivera M, Dale AM, Shepherd R, Carter R. Clinical, pathophysiologic, and microbiologic characterization of bronchiectasis in an aging cohort. Chest. 1995;108(4):955–961. doi: 10.1378/chest.108.4.955. [DOI] [PubMed] [Google Scholar]
- 10.Pasteur MC, Helliwell SM, Houghton SJ, et al. An investigation into causative factors in patients with bronchiectasis. Am J Respir Crit Care Med. 2000;162(4 Pt 1):1277–1284. doi: 10.1164/ajrccm.162.4.9906120. [DOI] [PubMed] [Google Scholar]
- 11.O’Donnell AE, Barker AF, Ilowite JS, Fick RB, et al. Treatment of idiopathic bronchiectasis with Aerosolized recombinant human DNase I. Chest. 1998;113(5):1329–1334. doi: 10.1378/chest.113.5.1329. [DOI] [PubMed] [Google Scholar]
- 12.Morrissey BM, Harper RW. Bronchiectasis: sex and gender considerations. Clin Chest Med. 2004;25(2):361–372. doi: 10.1016/j.ccm.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Säynäjäkangas O, Keistinen T, Tuuponen T, Kivelä SL. Bronchiectasis in Finland: trends in hospital treatment. Respir Med. 1997;91(7):395–398. doi: 10.1016/s0954-6111(97)90251-1. [DOI] [PubMed] [Google Scholar]
- 14.State Inpatient Databases HCUP. (SID) Healthcare Cost and Utilization Project (HCUP) 1993-2006. www.hcup-us.ahrq.gov/sidoverview.jspAccessed October 21, 2009.
- 15.Elixhauser A, Steiner C, Palmer L Clinical Classification Software (CCS) US Agency for Healthcare Research and Quality. 2008. http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed July 13, 2009.
- 16.Finkler SA. The distinction between cost and charges. Ann Intern Med. 1982;96(1):102–109. doi: 10.7326/0003-4819-96-1-102. [DOI] [PubMed] [Google Scholar]
- 17.Tompkins C, Altman S, Eilat E. The precarious pricing system for hospital services. Health Aff. 2006;25(1):45–56. doi: 10.1377/hlthaff.25.1.45. [DOI] [PubMed] [Google Scholar]
- 18.Russell RB, Green NS, Steiner CA, et al. Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics. 2007;120(1):e1–e9. doi: 10.1542/peds.2006-2386. [DOI] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research and Quality HCUP cost-to-charge ratio files. http://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed July 14, 2009. [DOI] [PubMed]
- 20.Tsang KW, Tipoe GL. Bronchiectasis: not an orphan disease in the East. Int J Tuberc Lung Dis. 2004;8(6):691–702. [PubMed] [Google Scholar]
- 21.O’Malley KJ, Cook KF, Price MD, Wildes KR, Hurdle JF, Ashton CM. Measuring diagnoses: ICD code accuracy. Health Serv Res. 2005;40(5 Pt 2):1620–1639. doi: 10.1111/j.1475-6773.2005.00444.x. [DOI] [PMC free article] [PubMed] [Google Scholar]