Abstract
Background
When the data from the National Resident Matching Program (NRMP) are used to analyze trends in medical students' career preferences, positions offered outside the match are omitted. The purpose of the study was to evaluate the extent and nature of out-of-match residency offers.
Methods
We obtained total resident complements and postgraduate year-1 positions offered in 7 specialties in 2007 and compared these with the 2007 NRMP match data. We compared the percentage of positions offered outside the match to “success” in matching United States medical doctors (USMDs) and to the availability of fellowship positions, using the Spearman rank order test (SROT).
Results
A total of 18 030 postgraduate year-1 positions were offered in 9 specialty areas. Of 15 205 positions offered in the match, 54% were taken by USMDs. The percentage of outside-the-match offers was found to vary by specialty, from 7% in obstetrics-gynecology to 23% in internal medicine, and was inversely correlated with the specialty's “success” in matching USMDs (SROT = −0.87). The 3 nonprocedural primary care specialties (internal medicine, family medicine, and pediatrics) accounted for 10 091 (46.2%) of the 21 845 total positions offered in the match, with 4401 (43.6%) offered almost entirely to non-USMDs. Another 2467 positions were offered outside the match, resulting in 6868 positions offered to non-USMDs (55% of all primary care positions). In internal medicine, the percentage of outside-the-match offers was significantly and inversely associated with the availability of intrainstitutional fellowship programs (P < .0001). Prematching of independent applicants was significantly higher in primary care than in procedural-lifestyle programs (P < .0001).
Conclusion
The NRMP's match data do not account for positions filled outside the match, a finding that appears to be significant. In 2007, 1 in 5 positions in primary care was offered outside the match.
Background
The National Residency Matching Program (NRMP) was introduced in 1952 to resolve the turmoil surrounding resident recruitment that existed from the inception of internships in the early 1900s.1 With a mission to “protect” medical students,2 the NRMP was created in response to concerns that some residency programs were attempting to strong-arm medical students into their training programs. It has provided much needed stability to a market that, before the program's inception, required some students to commit to offers within 12 hours.1
Currently, only students enrolled in allopathic medical schools in the United States (United States medical doctors; USMDs) are required to participate in a national matching program like the NRMP (provided that the institution uses a matching program for any of its other residency programs).3 Osteopathic medical students (OMSs), international medical graduates, and the small group of USMDs who have already graduated from medical school are allowed to take outside-the-match offers. The number of such offers is not reported by any organization, but it can be estimated. The purpose of the study was to evaluate the possible extent of out-of match-residency offers. This may create an unregulated method of residency recruitment in which tens of thousands of non-USMDs vie for several thousand positions, a situation akin to that which existed for USMDs before the matching program.
Methods
Data Sources
To analyze postgraduate year-1 (PGY-1) residency positions offered in and outside of the NRMP match, we used Results and Data: 2007 Main Residency Match,4 published by the NRMP, and 2007 data from the 2009 Association of American Medical Colleges (AAMC) Data Book.5 Additional data regarding availability of fellowships were obtained from the American Medical Association's (AMA's) FREIDA Online resource6 and the AMA's Graduate Medical Education Directory.7
We compared the number of residency positions offered, from Table F7 of the AAMC Data Book,5 to the number of positions offered in the match, from Table F2 in the AAMC Data Book,5 (these numbers are identical to the NRMP Results and Data4). The difference represents the number of outside-the-match positions offered. For added validation, we compared the total number of residents reported to be employed (Table F8 in the AAMC Data Book5) to the total positions offered (Table F7). Tables F7 and F8 were derived from data provided in the annual GME Track Census, a database jointly sponsored by the AAMC and the AMA. Combined programs (eg, internal medicine–pediatrics, internal medicine–emergency medicine, internal medicine–psychiatry, pediatrics-psychiatry) were not included in the study.
For programs with multiple tracks (eg, surgery and internal medicine), the following assumptions were made. In surgery, preliminary PGY-1 positions (Pre S), were assumed to make up all the outside-the-match surgery offers, since these positions do not directly lead to surgical careers with the same ease as do categorical surgery positions. Preliminary internal medicine positions (leading to careers in radiology, ophthalmology, anesthesiology, dermatology, neurology, etc), matching with more than 75% USMDs, were not assumed to make up any of the internal medicine positions offered outside the match. Outside-the-match offers in internal medicine were assumed to be for categorical or primary care PGY-1 residency positions.
We hypothesized that availability of fellowship programs would obviate or lessen the need for prematching in internal medicine and identified the number of institutions with 2 or more sponsored internal medicine fellowship programs with FREIDA Online database6 and the AMA's Graduate Medical Education Directory.7 Core internal medicine subspecialties including geriatrics, infectious diseases, cardiology, pulmonary, critical care, hematology, oncology, nephrology, endocrinology, rheumatology, and gastroenterology, as well as the aforementioned combined programs, were used for the count. Prematch data were calculated for each internal medicine program and grouped together in a state-by-state analysis.
Statistical Analysis
The Spearman rank order test (SROT) was used to compare the calculated percentage of outside-the-match offers in internal medicine programs by state with the percentage of programs with 2 or more internal medicine fellowships. An SROT was used to evaluate the strength of the relationship between the percentage of positions filled outside the match to the percentage of positions filled by USMDs in the match by specialty. The Pearson χ2 test was used to compare prematching in primary care to procedural/lifestyle programs.
Results
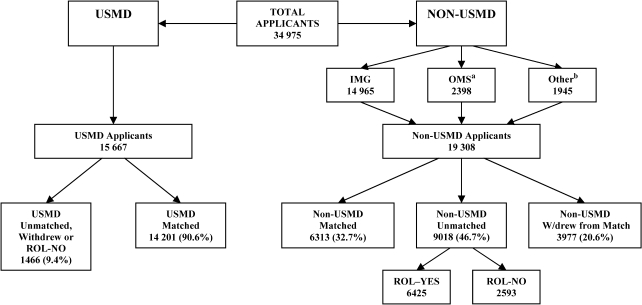
In 2007, a total of 21 845 PGY-1 positions were offered through the NRMP (figure 1). Applying for these positions were 15 667 USMDs and 19 308 non-USMDs (although a small percentage withdrew their applications or did not submit rank order lists). Only 6313 (32.7%) of non-USMDs matched to a position. Also, 2593 non-USMDs (13.4%) “participated” in the match, but did not submit a rank order list, making them eligible to participate in the postmatch “scramble” for unmatched positions. Postmatch “scramble” offers are not included in the final match data published by the NRMP.
Figure 1.
Breakdown of Applicants Applying for 21 845 Postgraduate Year-1 Positions in the 2007 Match
Abbreviations: IMG, international medical graduate; OMS, osteopathic medical student; ROL-NO, rank order list was not submitted; ROL-YES, rank order list was submitted; USMD, United States medical doctor from allopathic medical school; W/drew, withdrew. Non-USMD applicants are also known as independent applicants.
a For this study, OMSs were included with non-USMDs because only allopathic medical students are required (see text) to use the match system.
b Other includes Canadian physicians, US physicians, and Fifth Pathway graduates.
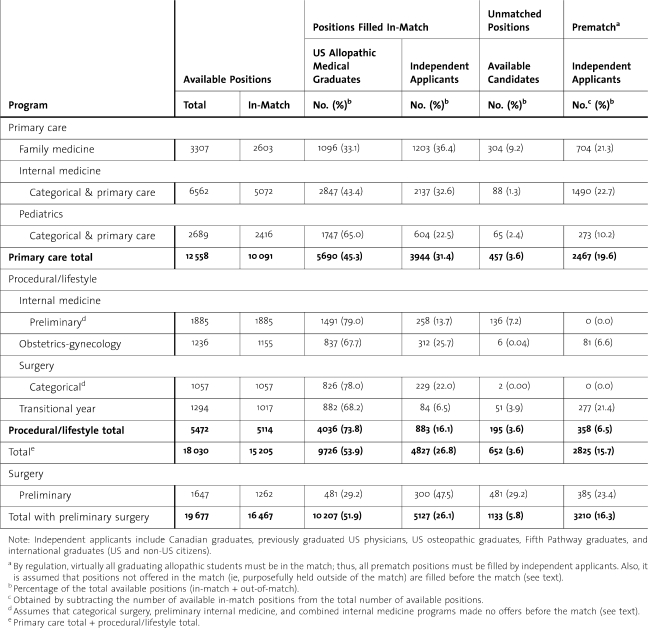
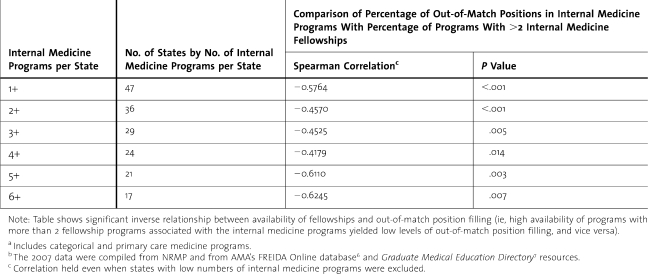
The 3 nonprocedural primary care specialties (internal medicine, family medicine, and pediatrics) accounted for 10 091 (46.2%) of the NRMP-offered PGY-1 residency positions (table 1). The 7 disciplines (primary care plus procedural/lifestyle) analyzed in this study represented 15 205 (69.6%) of the PGY-1 positions offered through the match (table 1). Of these, 64% were filled by USMDs and 31.7% matched with non-USMDs (4.3% went unmatched). An additional 1262 Pre S positions (not included in either the primary care or the procedural/lifestyle groups) were offered in the match, and only 38.1% matched with USMDs (table 1).
Table 1.
Comparison of Total Available Positions Versus National Resident Matching Program–Offered Positions in 2007 (Prematch Calculations)
The total number of PGY-1 positions available, in the 3 primary care and 4 procedural and/or lifestyle-oriented specialties studied, was 18 030, with 2825 (15.7%) of these positions being offered outside the match (table 1). Practically all USMDs are required to take residency offers through the match (in fact in 2007, 91% of the available 15 667 USMDs were recruited via the match); thus, virtually all outside-the-match offers are made to non-USMDs. Variation in percentages for outside-the-match offers was found by specialty and ranged from 7% in obstetrics-gynecology to 23% in internal medicine. Four specialties—family medicine, internal medicine, transitional year, and Pre S—appear to be prematching more than 20% of their total available positions (table 1). The percentage of NRMP-offered positions taken by USMDs ranged from 87% in transitional year to 42% in family medicine (38% in Pre S). The percentage of outside-the-match offers was highly inversely correlated with the specialty's “success” in matching USMDs (SROT = −0.87) (figure 2).
Figure 2.
Percentage Breakdown of Positions Offered by Studied Disciplines
Abbreviations: Ob/Gyn, obstetrics/gynecology; Prelim, preliminary; USMD, United States medical doctor of an allopathic medical school
* Figure shows inverse relationship between “successfully” matching USMDs and out-of-match position filling (ie, high USMD matching percentage yields low levels of out-of-match position filling and vice versa).
A total of 8304 (46.1%) of all PGY-1 positions (in the specialties studied) in 2007 were offered to non-USMDs in and out of the match (table 1). Most of these offers were made in the 3 nonprocedural primary care specialties (internal medicine, family medicine, and pediatrics) and they represent 54.7% of the total 12 558 primary care positions offered (table 1). Fully 19.6% (2467) of these positions were offered outside the match and they represent 35.9% of all primary care offers to non-USMDs (table 1). The procedure-oriented/lifestyle-oriented specialties (obstetrics-gynecology, categorical surgery, preliminary internal medicine positions, and transitional year) matched with an average of 78.9% USMDs and offered only 358 of their total positions outside the match (table 1). The percentage of the total PGY-1 positions in these specialties accepted by non-USMDs was 26.2% (with 6.5% offered outside the match) (table 1).
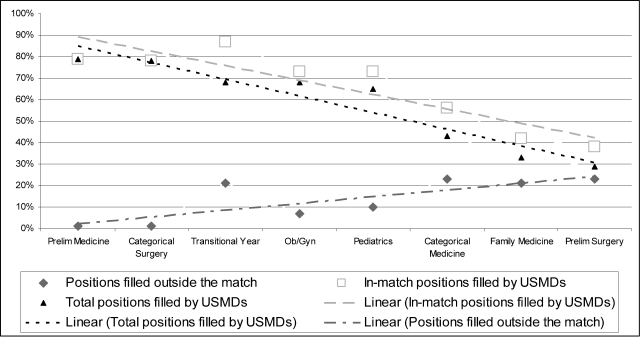
In internal medicine, the percentage of outside-the-match offers was significantly and inversely associated with the number of fellowship programs (P < .0001) offered by these internal medicine programs (table 2). After excluding data from states with few internal medicine programs, the association remained significant (table 2).
Table 2.
Percentage of Out-of-Match Positions in Internal Medicinea Compared to Availability of Fellowship Programs for 2007b
Discussion
The NRMP data show that a higher percentage of USMDs are filling positions in procedure-oriented/lifestyle-oriented specialties than in primary care. However, this does not consider the added outside-the-match offers we explored in our analysis. When the total number of available positions (obtained from the AAMC) is used as the denominator instead of the total number of NRMP-offered positions, USMDs appear to fill an even smaller percentage of primary care positions (5690 of 12 558, 45.3% versus 5690 of 10 091, 56.3%) than reported by the NRMP. Likewise, the disparity in USMD choice between primary care and procedural/lifestyle programs is underestimated if the NRMP data only are used as the total number of positions for a given specialty. Alternatively, the actual number (not a percentage of positions) of USMDs entering the primary care specialty is greater than that entering the procedural/lifestyle residencies (5690 versus 4036). The authors recommend that AAMC data should be formally coupled with the NRMP results when examining USMDs' residency choices. It is not clear if our findings are representative of the crisis in primary care in the United States, which may contribute to USMDs choosing procedure-oriented/lifestyle-oriented specialties over primary care.
About 1 in 5 positions in nonprocedural, primary care specialties are offered outside the match. Also, 54.7% of all primary care PGY-1 positions were offered to non-USMDs, of whom 35.9% took positions outside the match, whereas 3977 non-USMDs who registered for the match withdrew before the match. While around 1200 offers (Mona Signer, MPH, E-mail communication, December 15, 2009) were withdrawn for candidates' failure to meet Educational Commission for Foreign Medical Graduates testing requirements, the remaining candidates (2777) are presumed to have been offered and to have accepted outside-the-match offers, closely approximating the 2825 outside-the-match offers made in the specialties studied. This observation suggests that most (70%) of the withdrawals were to take offers outside and before the match, though proof of this is lacking. In procedure-oriented/lifestyle-oriented specialties, only 26.2% of all positions are filled by non-USMDs and only 6.5% of all such positions are estimated to be offered outside the match.
The possible effect of the current unregulated system of offering outside-the-match residency positions has been to create a recruitment method in graduate medical education (predominantly in primary care specialties) characterized by program directors “giving” positions primarily to non-USMDs who are eager to secure a position rather than take their chances in the match. This situation is similar to that which existed for USMDs before the match (before 1952) and needs to be addressed. Our estimates suggest that outside-the-match offers occur to an extent previously unrecognized, especially in 4 specialties (family medicine, internal medicine, Pre S, and transitional year). Furthermore, the amount of prematching in internal medicine may be linked to the lack of availability of fellowship positions.
It may be useful to consider why program directors choose to offer and candidates choose to accept positions outside the match. Program directors may do so to address 2 recruitment issues: (1) to prevent losing interested, non-USMD candidates to other programs offering outside-the-match contracts and (2) to avoid the “scramble.” Offering positions outside the match reduces a program's match quota, thereby limiting the number of unmatched positions. The “scramble” has been likened to college basketball's “March Madness,”8 and candidates taken in the postmatch period seem to perform less favorably when compared to those accepted in the match.9
The potential situation for candidates is similar. Non-USMDs, correctly perceiving their generally less competitive status relative to USMDs, may, if they wish to compete in the match, choose to apply to more programs and risk needing to “scramble” if they fail to match. Reginald Fitz, at Boston University, summarized a student's perspective in 1939: “… there are very few men who have the conceit to pass up a very good appointment in 1 locality offered early simply on the gamble of competing for a somewhat more desirable appointment made later in another locality.”10 Non-USMDs also may be disadvantaged in the “scramble,” as they may not receive the dean's office assistance with phone calls and paperwork; additionally, they may experience difficulty getting through to program directors who hope to fill their unfilled position(s) with USMDs. Also, the timeline for obtaining a visa is shorter the longer one waits for a position, making a prior-to-the-match offer additionally enticing for foreign citizens.
The literature11–14 indicates perceived match violations, including promises to applicants before the match, thus putting in question the ethics and morals of program directors and candidates alike. The NRMP has considered proposals to limit outside-the-match offers15 and to conduct a second match for unmatched candidates.16 Neither has been adopted, in part because of concerns expressed by program directors “dependent” on international medical graduates, who might have difficulty getting visas in time for their July start dates. Our study represents a preliminary attempt to elucidate the amount of prematching occurring in the United States. Since prematching data are not officially reported anywhere, our calculations may be overestimating or even underestimating the extent of out-of-match offers. If, however, it is confirmed that primary care programs (particularly internal medicine and family medicine) need to consistently, year after year, recruit 1 of 5 applicants outside of the match, then this negative finding should be further examined. These proposals should be reconsidered in the context of our study findings. We advise the community against drawing strong conclusions from these initial results, which analyze only a fraction of 1 academic year's match. Further research, by independent groups and spanning multiple academic years, is needed to confirm or disprove our findings and to analyze prematching trends in all specialty areas.
One limitation of this study is that the AAMC Data Book5 provides only the programs' reporting of both the total number of residents working in each specialty (without a breakdown by year of training) and the number of positions offered in total and in the PGY-1 year. When the total number of positions offered (Table F7 of AAMC Data Book5) is compared to the total number of residents reported (Table F8 of AAMC Data Book5), there is a 3% difference in nonprocedural primary care specialties and a 1% difference in procedure-oriented specialties. This difference between positions offered and filled should have little effect on the study, as it probably is evenly distributed over all years of residency training. Since preliminary internal medicine positions and Pre S positions are a part of—but much different than (with regards to a career)—the overall internal medicine and surgery program of a given institution, respectively, we analyzed them separately from their categorical counterparts. In doing so, we had to assume that no prematching occurs in preliminary internal medicine or categorical surgery positions. The actual number is likely a small percentage, and the assumption does not significantly affect the results of this study. Also, we assumed that all available postmatch positions were given to non-USMDs. Since 9% of all graduating allopathic students are theoretically available in the postmatch period, it is reasonable to assume that some postmatch positions are being filled by USMDs. For a given specialty, this would probably represent a very small percentage of their positions; this assumption also does not alter the prematch findings of this study. Finally, the data in the AAMC Data Book5 are entered online by the training programs through GME Track Census and may overstate or understate the number of positions offered and/or filled. It is the official source of the data used by the AMA and the AAMC, and it is unlikely that programs would willingly provide inaccurate information.
Despite these limitations, our study is the first to estimate the potential extent of outside-the-match offers of graduate residency positions. About 1 in every 5 positions in nonprocedural primary care specialties appears to be filled outside of the match, effectively circumventing the intent of having a matching program. As a result, USMDs are more limited in the number of open positions in the match and non-USMDs are subjected to the pre-1952 recruitment conditions that the NRMP was designed to alleviate.
Footnotes
Robert V. Wetz, MD, is Associate Chairman of Medicine and Residency Program Director for the Department of Medicine at Staten Island University Hospital; Charles B. Seelig, MD, MS, is Director of Medical Education and Internal Medicine Residency Program Director at Greenwich Hospital; Georges Khoueiry, MD, is Assistant Director of Student Education for the Department of Medicine at Staten Island University Hospital; and Kera F. Weiserbs, MHS, PhD, is Biostatistician and Epidemiologist for the Department of Medicine at Staten Island University Hospital.
The authors have no financial support or conflicts of interest to disclose.
References
- 1.Roth A. E. The origins, history, and design of the resident match. JAMA. 2003;289(7):909–12. doi: 10.1001/jama.289.7.909. [DOI] [PubMed] [Google Scholar]
- 2.Chae S. H. Is the match illegal? N Engl J Med. 2003;348(4):352–356. doi: 10.1056/NEJMsb021241. [DOI] [PubMed] [Google Scholar]
- 3.National Resident Matching Program. Match Participation Agreement for applicants & programs for the 2009 Main Residency Match: 1.0, introduction to the matching program. 2007. Available at: http://www.nrmp.org/res_match/policies/map_main.html#applicants. Accessed July 10,
- 4.NRMP Board of Directors. Results and data: 2007 Main Residency Match. 2010. National Residency Matching Program, April, 2007. Available at: http://www.nrmp.org/data/resultsanddata2007.pdf. Accessed July 14,
- 5.Geraci W., Vasev P. AAMC Data Book: Medical Schools and Teaching Hospitals by the Numbers, AAMC Section for Medical School and Faculty Studies, April 2009. Washington, DC: AAMC; 2009. [Google Scholar]
- 6.American Medical Association. FREIDA Online: fellowship and residency electronic interactive database. Available at: http://www.ama-assn.org/ama/pub/category/2997.html. Multiply accessed July–August 2007.
- 7.Donini-Lenhoff F., editor. Graduate Medical Education Directory. 92nd ed. Chicago, IL: American Medical Association; 2007–2008. [Google Scholar]
- 8.Ziegelstein R. C. “Rocking the match”: applying and getting into residency. J Natl Med Assoc. 2007;99(9):994–999. [PMC free article] [PubMed] [Google Scholar]
- 9.Blonski J., Rahm S. The relationship of residency performance to match status and US versus international graduate status. Fam Med. 2003;35(2):100–104. [PubMed] [Google Scholar]
- 10.Fitz R. Concerning interns and internships. J Assoc Am Med Coll. 1939;14(2):101–104. [Google Scholar]
- 11.Anderson K. D., Jacobs D. M. General surgery program directors' perceptions of the match. Curr Surg. 2000;57(5):460–465. doi: 10.1016/s0149-7944(00)00309-3. [DOI] [PubMed] [Google Scholar]
- 12.Anderson K. D., Jacobs D. M., Blue A. V. Is match ethics an oxymoron? Am J Surg. 1999;177(3):237–239. doi: 10.1016/s0002-9610(99)00019-7. [DOI] [PubMed] [Google Scholar]
- 13.Carek P. J., Anderson K. D., Blue A. V., Mavis B. E. Recruitment behavior and program directors: how ethical are their perspectives about the match process? Fam Med. 2000;32(4):258–260. [PubMed] [Google Scholar]
- 14.Parmley W. W. The fellowship match selection process: where has collegiality gone? J Am Coll Cardiol. 2000;36(1):294. doi: 10.1016/s0735-1097(00)00807-x. [DOI] [PubMed] [Google Scholar]
- 15.Miller F. H., Greaney T. L. The National Resident Matching Program and antitrust law. JAMA. 2003;289(7):913–918. doi: 10.1001/jama.289.7.913. [DOI] [PubMed] [Google Scholar]
- 16.Howell W. L. J. Proposed second match defeated. 2007. AAMC Reporter [serial online]. June 2005. Available at: http://www.aamc.org/newsroom/reporter/june05/proposed.htm. Accessed July 15,