Abstract
Background
Like their counterparts in many other nations, physicians in Singapore are tasked with providing care, conducting research, and teaching and providing leadership to junior doctors. In this paper, we describe our experience implementing the first chief residency program in Singapore.
Initiative
A pilot of a chief residency program was initiated in the Department of Medicine at National University Hospital in July 2008, with 1 chief resident (CR) and 2 associate CR positions. The pilot used the US model for CR training as the initial framework. CRs would assist in the orientation and integration of new residents, teach residents, promote camaraderie among residents, help resolve issues, function as a liaison to senior staff, and would be developed as potential health care leaders and physician role models.
Results
The CRs performed a host of administrative duties and initiated several improvements in the residency, including better practices for leave scheduling, call roster planning, and a night float system. CRs attended monthly meetings with division heads and participated in departmental strategic planning as well as professional development and leadership courses. The CR position was well regarded by the other residents, and this resulted in increased interest in identifying and addressing opportunities for improvement. The introduction of a chief residency also made the department a more attractive posting for residents and contributed to a significant increase in the number of applicants for residency rotations.
Conclusions
A chief residency program can benefit residents' morale and a CR's development as a leader, and it can facilitate linkage between junior and senior hospital management that promotes active involvement in problem solving and clinical and education improvement. Support from hospital administrators and senior clinicians is essential, and mentoring and succession planning are important to ensure the program's continued success.
Introduction
During the past 4 decades, practicing medicine in the hospital setting has become more complex in Singapore. Physicians strive to balance the goals of providing high-quality and affordable clinical care while pursuing academic research and training medical students and junior doctors. Achieving these multiple goals is challenging, making the role of strong health care leadership increasingly pertinent. For new residents, the many activities in a large clinical department contribute to a sense of role disorientation, and a common complaint is lack of communication and feedback between the junior and senior staff regarding service and training policies. This may be partly due to the lack of representation of junior staff in the senior management group.
Physician training has traditionally focused on the acquisition of clinical skills, with little or no formal education aimed at developing leadership skills. A junior health care leadership position for residents may contribute to resolving the disparity between institutional goals and the needs of junior doctors, and concurrently offer opportunities for the development of leadership skills.
In this paper, we share our experience in formulating and implementing a chief residency program in the department of medicine at National University Hospital (NUH) in Singapore.
Aims of a Chief Residency Program
The US model for chief resident (CR) training served as our initial framework. The first chief residency was instituted at Johns Hopkins Hospital in 1889.1 Like CRs in the United States and Canada (CRs do not exist in other countries), the CRs at NUH would assist in the orientation and integration of new residents into the department. They would also promote camaraderie among the residents, help resolve issues, and function as a liaison to senior staff. The CRs would be developed as potential health care leaders and future physician role models.2
In our program, CRs would hold their position for 1 year and would perform 4 specific roles: (1) faculty-resident liaison, (2) resident teacher, (3) resident leader, and (4) resident role model, in keeping with the classic model of chief residency.1 Other responsibilities included organizing social events, conducting and generating interest in research, and leading departmental rounds or conferences. Interested candidates had to meet the following qualifications to be selected, as well as complete an interview with the head of the department and the team:
Six months or more of experience in the NUH Department of Medicine.
Membership in the Royal College of Physicians Part I or higher.
Good clinical skills and knowledge as assessed by the attending physicians.
Leadership qualities.
Good interpersonal relationships as perceived by peers, attending physicians, and allied health care workers.
Implementation of the Program
The pilot of the CR program in the NUH Department of Medicine was initiated in July 2008 with 1 CR position and 2 associate CR positions.
The primary administrative duties of the CRs included:
Planning the ward roster, night duty roster, and clinic roster (the 3 CRs took turns organizing the weekly teaching and distributed the remaining work evenly among themselves).
Assigning training requirements and resident requests to meet the needs of the various subspecialties and general medicine teams.
Organizing and teaching at the weekly resident meetings.
These duties were divided among the 3 pilot participants to ensure no CR would be overwhelmed by administrative work.3 Shortly after being appointed, the CRs were tasked with developing systematic changes to the night call schedule in response to the growing concern about the increasing patient load of the on-call residents.
In the system prior to the intervention, each on-call medical officer admitted an average of 20 new patients per call in addition to providing care for existing inpatients. The existing on-call practice is often called the “29-hour shift,” with the on-call medical officer beginning the day ward duties at 8 am and starting call after 5 pm until 8 am the following day. The resident then works until 1 pm before getting a half-day off. In the proposed night float system, on-call residents would stay only until 8:30 pm after their day ward duties, and a dedicated night float team would cover the following 12-hour (8 pm–8 am) shift. Each night float team would work 5 consecutive nights with no daytime ward duties. In NUH, most new patients are admitted between 6 pm and 10 pm, allowing new admissions to be distributed among the on-call team and the night-float team.
After developing the night float system, residents, senior staff, and hospital administration reviewed duty hours, patient load, handovers between shifts, and remuneration, with the CRs as facilitators. Senior staff initially expressed concern about the night float system because this was the first time in Singapore that this scheduling approach was used. The CRs acted as the bridge between the junior and senior staff in the planning process and collected feedback from both sides. After the successful completion of the pilot phase, they were actively involved in incorporating modifications to the new call system, which was successfully implemented 6 months after its conception.
The CRs also helped negotiate better practices for leave scheduling and call roster planning. In the past, leave applications were approved on an ad-hoc, first-come, first-served basis, and this led to unhappiness and many disagreements among the residents. With the feedback the CRs received from the residents, a clear system of priority ranking of leave eligibility was developed. This new leave scheduling and call roster planning were able to better match residents' preferences. In this aspect, the CRs were mediators in work-related interpersonal conflicts and discontent among residents.
The existing program for resident teaching was revamped prior to the conception of the CR program. The CRs complemented the teaching program by providing a practical clinical approach to the medical conditions discussed and by offering advice on any administrative problems that the residents may have encountered in the management of their cases. Other than administrative duties, the CRs strived to increase morale and camaraderie among the junior doctors by organizing resident outings.
Acting as a bridge between the junior staff and senior management, the CRs attended monthly meetings with division heads to provide a resident's perspective. Prior to the development of the CR role, residents were not asked to attend or given the opportunity to give any feedback.
In an effort to gain more experience with leadership and management, the CRs were invited to participate in the department's planning and strategizing retreat (an annual meeting in which all of the heads of division and senior hospital management meet). This was the first time any junior doctors attended such meetings. The CRs were also allowed to participate in professional development/leadership courses.
Over the next 6 months, the residents welcomed the idea of having senior peers look after their needs and help address their concerns. Although no formal poll was conducted, it was anecdotally apparent that there was a closer camaraderie among the residents and a sense of identification with the institution. Whereas before, residents were traditionally passive and apathetic about clinical work practices, there was a new increased interest in identifying and addressing opportunities for improvement. This increased interest culminated in the creation of a Junior Unit against InEfficiency (JUIcE) committee composed of residents and chaired by one of the CRs. Its main aim was to address resident concerns about identifying and resolving work inefficiencies, which resulted in greater cooperation between nurses and doctors, as well as the development of more user-friendly admission clerking notes.
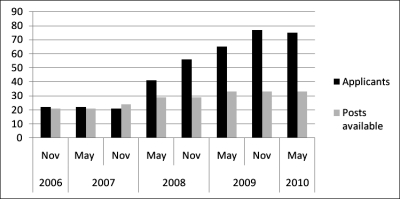
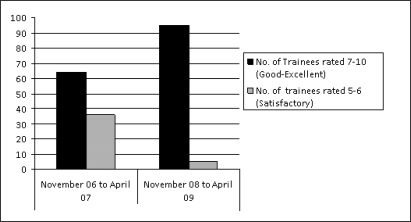
Ultimately, the introduction of the CR made the department a more attractive post for residents and contributed to a significant increase in the number of applicants for resident rotation to our department, which is significant because residents rotate through various departments and hospitals on a 6-month basis in Singapore; this differs from US residency programs, where residents remain in the same program for the duration of their residency. Therefore, each clinical department seeks to attract the top residents. Before the implementation of the CR program, the number of applicants to NUH often barely met the number of available posts. Six months after the implementation of the CR program, the institution experienced a significant increase in the number of residents indicating the NUH Department of Medicine as their first choice (figure 1). Additionally, in a comparison of preimplementation and postimplementation feedback data, the number of residents who rated the training in NUH as “good-excellent” rose from 64% to 95% (figure 2), an almost 50% rise in our ratings.
Figure 1.
Graph of Numbers of Medical Officers Applying to the Department of Medicine, National University Hospital
Figure 2.
Rating of Medical Officers on the Training Program in National University Hospital Before and After the Chief Resident Program
Before leaving their posts, the CRs had to identify their successors. At the writing of this paper, the second group of CRs/associate CRs have been identified and have started their duties. The first 3 CRs/associate CRs have moved on to respective advanced specialist training, but they continue to act as mentors to the new CRs. The CR role developed the residents' interpersonal skills and problem-solving abilities. Looking ahead, the CR role will be helpful in transitioning the graduate medical education of our residents from a British system to one modeled on the American system.
Lessons Learned
The CRs learned many lessons over the year's appointment, and the experience at NUH may also help other hospitals interested in setting up a similar program:
The strong support of hospital administrators and senior clinicians for the program is essential.
Good liaisons between junior and senior hospital management can promote an active involvement in problem solving.
Mentoring and succession planning are important to ensure continuity to the program.
Our newly introduced CR system will evolve to suit needs. The core role will likely remain as a liaison between junior and senior staff, teaching, and work schedule administration and leadership development. The leadership-training objective must balance the administrative objective. CRs require good mentorship and nurturing, and like medical training, leadership training requires mentorship and the ability to practice.
Footnotes
All authors are at National University Hospital, Singapore. Yap Eng Soo, MBBS (Int Med), is Registrar in the Department of Haematology-Oncology; Goh Wei-Ping, MBBS, is Resident Physician in the Department of Medicine; Adrian C. L. Kee, MBBS, M Med(Int Med), is Registrar in the Department of Medicine; and Chan Yee Cheun, MBBS, is a Consultant in the Department of Medicine.
The authors would like to thank Professor Khek-Yu Ho and the staff of the Department of Medicine, National University Hospital, for helping with the survey and providing some of the data.
References
- 1.Parrino T. A., Steel K. The medical chief residency and its relation to academic sections of general medicine. Am J Med. 1983;75:839–842. doi: 10.1016/0002-9343(83)90415-1. [DOI] [PubMed] [Google Scholar]
- 2.Wright S. M., Kern D. E., Kolodner K., Howard D. M., Brancati F. L. Attributes of excellent attending-physician role models. N Engl J Med. 1998;339:1986–1993. doi: 10.1056/NEJM199812313392706. [DOI] [PubMed] [Google Scholar]
- 3.La Delfa I., Wilson D. B., Kopplin P. A. The chief medical residency in Canada: comparison of opinions between physicians-in-charge and chief medical residents. CMAJ. 1988;139:203–208. [PMC free article] [PubMed] [Google Scholar]