Abstract
Background
Physician workforce projections by the Institute of Medicine require enhanced training in geriatrics for all primary care and subspecialty physicians. Defining essential geriatrics competencies for internal medicine and family medicine residents would improve training for primary care and subspecialty physicians. The objectives of this study were to (1) define essential geriatrics competencies common to internal medicine and family medicine residents that build on established national geriatrics competencies for medical students, are feasible within current residency programs, are assessable, and address the Accreditation Council for Graduate Medical Education competencies; and (2) involve key stakeholder organizations in their development and implementation.
Methods
Initial candidate competencies were defined through small group meetings and a survey of more than 100 experts, followed by detailed item review by 26 program directors and residency clinical educators from key professional organizations. Throughout, an 8-member working group made revisions to maintain consistency and compatibility among the competencies. Support and participation by key stakeholder organizations were secured throughout the project.
Results
The process identified 26 competencies in 7 domains: Medication Management; Cognitive, Affective, and Behavioral Health; Complex or Chronic Illness(es) in Older Adults; Palliative and End-of-Life Care; Hospital Patient Safety; Transitions of Care; and Ambulatory Care. The competencies map directly onto the medical student geriatric competencies and the 6 Accreditation Council for Graduate Medical Education Competencies.
Conclusions
Through a consensus-building process that included leadership and members of key stakeholder organizations, a concise set of essential geriatrics competencies for internal medicine and family medicine residencies has been developed. These competencies are well aligned with concerns for residency training raised in a recent Medicare Payment Advisory Commission report to Congress. Work is underway through stakeholder organizations to disseminate and assess the competencies among internal medicine and family medicine residency programs.
Introduction
In its landmark report Retooling for an Aging America: Building the Health Care Workforce, the Institute of Medicine (IOM) identified a critical need to expand geriatrics competence among all physicians.1 The IOM noted that older adults currently make up about 12% of the US population yet account for 26% of all physician office visits, 35% of all hospital stays, and 38% of all emergency medical service responses. Regarding physician training, the IOM report noted that although 27 types of medical residency programs (accounting for 70% of trainees) included Accreditation Council for Graduate Medical Education (ACGME) requirements for some form of geriatrics training, the content and extent of such training are highly variable.
In addition to seeing an explosion in the numbers of old and very old people, the early part of the 21st century will see the transformation of the nation's health care delivery system from an approach focused on acute illness to one that recognizes the prevalence of chronic and complex disease.
The June 2009 Medicare Payment Advisory Commission (MedPAC) report to Congress2 raised concerns that residents are not currently receiving formal instruction and experience that will allow them to function optimally in the new systems of health care delivery.
As the source of all primary care and medical subspecialty physicians who care for adults, internal medicine (IM) and family medicine (FM) residency programs play an essential role in the continuum of training physicians to care for older adults. However, in 2001, only about half of graduating FM and IM residents (48% and 52%, respectively) reported feeling very prepared to care for older adults.3 More recently, in focus groups among medical students and IM residents, trainees perceived training gaps in caring for elderly patients in the areas of (1) recognizing and addressing complex, multifactorial illness; (2) setting priorities and goals for workup and intervention; (3) communication with families and with patients with cognitive disorders; and (4) assessment of a patient for discharge from the hospital.4 These concerns parallel, remarkably, those expressed in the June 2009 MedPAC report2 related to residency training in care coordination, patient safety (including working with multidisciplinary teams), interpersonal communication with special populations, and work in nonhospital settings.
Despite the importance of expanded training in clinical care of older adults in IM and FM residencies, geriatrics training remains limited. In a 2005 survey of 3-year (IM) residency training programs, fully 30% of programs provided fewer than 4 weeks of clinical instruction specific to geriatrics; and few programs (9%) provided 6 or more weeks of instruction. The crowded 3-year residency curriculum and lack of longitudinal outpatient care were cited by program directors as the most challenging barriers to expanding geriatrics training.5 In a 2004 survey, FM program directors reported a median of only 24 (range, 0–264) half-days of required geriatrics experience.6 Although geriatrics was rated as the most important curriculum area for a successful program by 53% of program directors, other curriculum demands and faculty time were cited as the most important barriers to expanding geriatrics training.
In recent years, influenced by a series of grants from the Donald W. Reynolds Foundation7 and the John A. Hartford Foundation,8–10 geriatrics training has been substantially expanded among medical students and residents at many academic institutions11 in a variety of surgical and related specialties12 and medical subspecialties.7,13
In the context of the IOM recommendations, in May 2009, the American Geriatrics Society (AGS), American Medical Association (AMA), and the Council of Medical Specialty Societies convened a conference that brought together representatives of 13 certifying boards, 21 specialty or subspecialty societies, and members of 6 Residency Review Committees. There was near unanimous agreement that defining, teaching, and assessing physician competence in the care of older adults were essential and that they should occur as a continuum.14 Basic knowledge and skills essential for all physicians would be integrated into medical student education, and competencies of increasing specificity would be developed for residents, fellows, and practicing physicians. Consistent with this recommendation, in a project beginning in 2007, 26 recommended essential geriatrics competencies that medical students should demonstrate by the beginning of residency have been defined.15
The recent activity in geriatrics education for physicians in all disciplines, the IOM recommendations, and the development of minimal competencies for medical students provide an opportunity to establish essential competencies in geriatrics for all physicians entering primary care practice or medical subspecialty training. This paper describes the process and outcome of a project to define a set of essential competencies related to the care of older adults by IM and FM residents.
Methods
In late 2007, a group of academic educators and geriatricians from IM and FM involved in geriatrics curriculum development organized to define essential competencies in geriatrics. The primary goal of the project was to define a set of competencies in the care of older adults that are minimal (ie, not intended to be comprehensive) and essential (applicable to all IM and FM residents, regardless of future career path). Although “competency” has been applied with a variety of implied or explicit definitions in medical education, competency was defined for this project as specific behaviors that are evidence based, rooted in clinical outcomes that matter for patients, observable, and can be assessed during patient care.
Specifically, the competencies would: (1) be unique to the care of older patients (ie, not general competencies), (2) be feasible within the structure of current residency programs, and (3) be endorsed and adopted by key stakeholder organizations and residency programs. Moreover, the competencies should: (1) constitute a uniform expectation for all graduating residents, (2) build on the recently established national competencies for medical students, (3) be assessable, and (4) address the ACGME competencies. To focus on performance in clinical contexts, and to be compatible with the medical student competencies, the IM/FM competencies complete the sentence: “The graduating IM or FM resident, in the context of a specific older patient scenario (real or simulated), must be able to…”
At the outset of the project, contact was made with and support solicited from a number of stakeholder organizations. Unrestricted funding support for the project (without implying organizational endorsement of the final product) was provided by the AMA, the American Board of Family Medicine Foundation, the AGS, and the Society of General Internal Medicine (SGIM). Leaders within the American Board of Internal Medicine and the Association of Program Directors of Internal Medicine (APDIM) were also supportive of the work.
The project took place in 4 stages. First, after completing a review of existing published curricula,16–20 the working group of 8 academic educators reviewed a list of 52 clinical competency content areas related to older persons that had been developed for the medical student project (eg, “malnutrition,” “sleep disorders,” “functional assessment”). The list was designed to capture all clinical areas important in caring for older patients. The 52 content areas were used as triggers to identify 7 domains that: (1) were useful as an organizing framework for defining specific competencies, (2) were directly relevant to the practice demands of graduating residents, and (3) reflected the current teaching context of IM and FM residencies.
At a 2008 meeting involving approximately 100 geriatrics educators from 36 academic institutions and sponsored by the D. W. Reynolds Foundation (www.dwreynolds.org), 8 groups of 10 to 15 geriatrics educators defined 3 to 6 competencies for each domain. One domain (Complex and chronic illness(s) in older adults) was divided among 2 groups focusing on clinical care and communication, respectively, because of its complexity. The result was a candidate set of 46 competencies. All 100 conference attendees then rated the relative importance of and provided comments on each of the 46 competencies using a web-based survey. Based on these results, redundant or overlapping competencies were combined, and wording of several competencies was modified by the working group to increase the specificity of terms and emphasize observable behaviors, resulting in 40 competencies.
Third, an expert panel of 26 faculty members was convened, whose members had experience in teaching residents or directing IM or FM residency programs but whose career focus was not geriatrics. A total of 3 to 7 panel members were recruited from the membership and with the assistance of each of 5 organizations: the Association of Family Medicine Residency Directors, the APDIM, the Society of Teachers of Family Medicine, the SGIM, and the AGS. Using a web-based survey, each of the 40 competencies was independently rated by the panel members as either “essential,” “desirable,” or “neither” for a resident to master before the end of residency. Respondents also provided written comments on the focus, wording, and relevance of the competencies to residency training. Of the 26 faculty members, 13 identified their primary discipline as IM, 12 as FM, and 1 as geriatrics.
Based on the results of the expert panel ratings and comments, the number of competencies was reduced by the working group, with a goal of arriving at 20 to 25 competencies. Competencies rated as “essential” by 11 or more of both the 13 IM and 12 FM reviewers were accepted (18 items), and competencies rated as “essential” by fewer than 8 of both the IM and FM reviewers were eliminated (6 items) or modified to address reviewers' concerns (2 items). The remaining 14 competencies, rated as “essential” by at least 9 reviewers from one (5 items) or both (9 items) groups of reviewers, were accepted (5 items), reworded (5 items), incorporated into other competencies (1 item), or eliminated (3 items) based on reviewers' comments. Finally, the competencies were reviewed by 12 residency program directors and teaching faculty from the home institutions of working group members for sensibility and suggestions on wording to convey content.
Results
Seven domains were identified for the essential IM/FM geriatric competencies: Medication management; Cognitive, affective, and behavioral health; Palliative and end-of-life care; Hospital patient safety; Complex or chronic illness(es) in older adults; Transitions of care; and Ambulatory care. The first 4 of these relate directly to similar domains in the medical student geriatrics competencies.4 The last 3 reflect clinical areas critical to residency training, each of which builds on several of the other student domains, ie, Self-care capacity; Health care planning and promotion; Atypical presentation of disease; and Falls, balance, and gait disorders.
A total of 14 of the 40 competencies reviewed by the nongeriatrician expert panel were eliminated or combined with other competencies. Specifically, 5 competencies were combined with other, related competencies (eg, skills related to transfers to and from the hospital, or to care of hospitalized patients); 4 competencies were deemed not specific to geriatrics (eg, perioperative assessment; patient counseling skills); 2 were too advanced to be deemed minimal and essential for all residents (related to managing behavioral complications of dementia and prescribing psychotropic medications); 2 were too complex or ambiguous to be behaviorally specific and assessable (related to identifying, assessing, and managing or referring patients with substance abuse problems; and critically applying literature to older patients); and 1 was deemed not feasible in all IM programs (related to providing care in nursing homes and at home). The review of the 26 competencies by 12 program directors and residency teachers resulted in only minor wording changes.
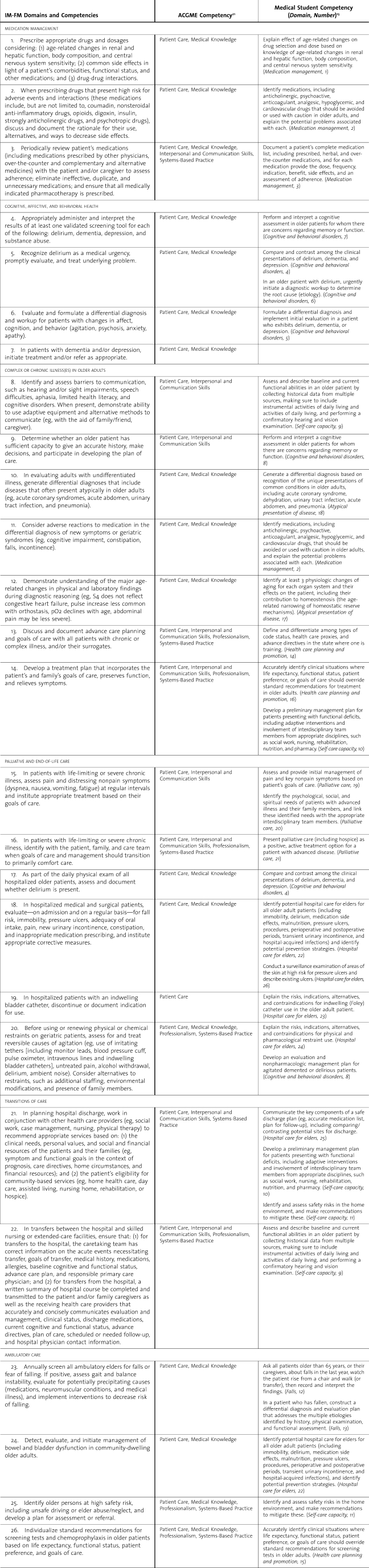
table 1 depicts the final set of 26 competencies in the first column. These have been mapped to related ACGME Core Competencies21 (second column) and to the corresponding medical student competencies4 (third column).
Table 1.
Internal Medicine (IM) and Family Medicine (FM) Resident Competencies Showing Accreditation Council for Graduate Medical Education (ACGME) Core Competencies and Related Medical Student Competencies
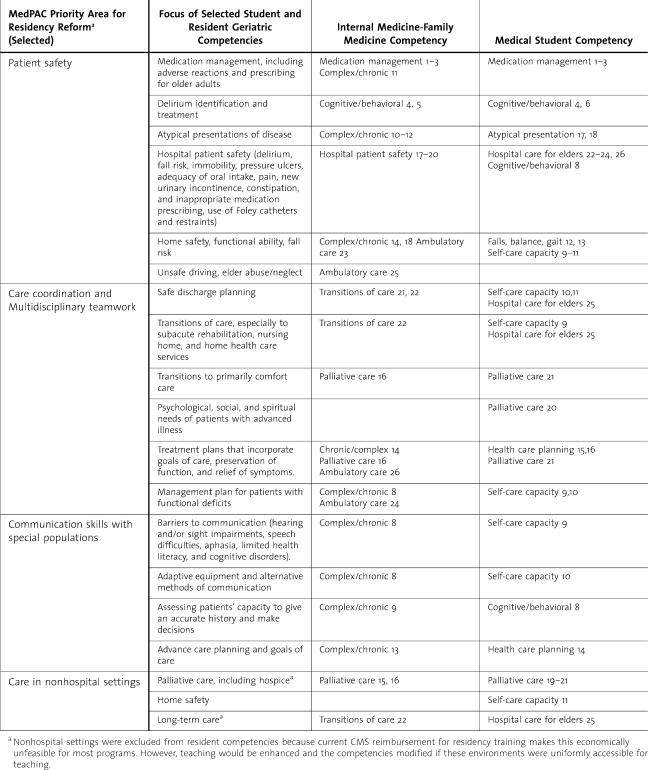
In table 2, the IM/FM resident and medical student competencies are linked to the areas of training identified in the June 2009 MedPAC report as among highest-priority areas for IM residency reform, ie, patient safety, care coordination (including working with multidisciplinary teams), interpersonal communication with special populations, and work in nonhospital and ambulatory settings.2
Table 2.
Geriatrics Competencies Aligned With Residency Reform Priority Areas From the Medicare Payment Advisory Commission (MedPAC)
Discussion
Through a consensus-building process based on expert panels and direct involvement of key stakeholder organizations, a set of 26 geriatrics competencies essential for mastery by the end of FM and IM residency has been defined. The competencies are designed to be context specific, performance oriented, and limited in number to promote acceptance, integration into residency curricula, and assessment. The IM/FM geriatrics competencies build on similarly developed medical student competencies in content and focus, and they comprise a critical step in the continuum of geriatrics competencies for all physicians who care for older adults.
The IM/FM geriatric competencies identify recommended essential skills and expertise needed when caring for older, rather than middle-aged, adults. They emphasize clinical areas of high morbidity and high prevalence among older patients for which current practice is often inadequate or inappropriate, as well as underemphasized in residency training—eg, identifying or avoiding adverse drug events; early recognition of delirium; and subtle presentations of common, serious disorders. Many address deficiencies in current residency training raised in the June 2009 MedPAC report, including care coordination, multidisciplinary teamwork, patient safety, interpersonal communication with special populations, and work in nonhospital settings.2
Several features of the IM/FM geriatrics competencies are worth highlighting. Although the content areas covered in the IM/FM competencies are nearly identical to the content areas in the medical student geriatrics competencies,4 the competencies themselves reflect a movement from knowledge-oriented to performance-oriented competencies. For example, under the medication management domain, although medical students are expected to “(i)dentify medications…that should be avoided or used with caution in older adults and explain the potential problems associated with each,” residents are expected to apply this knowledge “(w)hen prescribing drugs which present high risk for adverse events and interactions…”. Similarly, under the complex or chronic illness domain, although medical students are expected to “generate a differential diagnosis based on recognition of the unique presentations of common conditions in older adults…”, residents are expected to apply this knowledge “in evaluating adults with undifferentiated illness…”.
Each competency maps readily onto 1 or more of the 6 ACGME competencies. Because the IM/FM competencies focus on clinical care of individual patients, most relate directly to Patient Care, Medical Knowledge, and/or Interpersonal and Communication Skills. However, many competencies also relate to defining the professional scope of responsibilities and behaviors (Professionalism) and/or to practicing in and improving health care settings to best meet the needs of older patients (Systems-Based Practice). Implicit to the achievement of these competencies is the recognition that the optimal care of older adults requires that physicians learn to use the skills of other health professionals (Interpersonal and Communication Skills).
Many of the proposed competencies are best taught outside the hospital—in the office, nursing home, or community settings—and both FM and IM residency programs are encouraged to expose trainees to the full range of sites of care for older adults. However, as noted in the recent MedPAC report,2 the Centers for Medicare and Medicaid Services currently requires that teaching hospitals incur “all or substantially all” of the costs borne by nonhospital settings for teaching residents, including the cost of supervision. The importance of shifting incentives to increase training in nonhospital settings was emphasized in the MedPAC report.
Although the goal of this project was to develop a common set of minimum competencies for FM and IM residencies, some differences between FM and IM programs are relevant. For example, in recent surveys, 97% of FM residency programs require training in the nursing home, compared with 65% of IM residency programs, and 88% of FM programs require home visits, compared with only 33% of IM programs.7,8 Yet many of the IM reviewers felt that competencies related to providing care in nursing homes and at home could not be implemented in most current IM programs. To accommodate both disciplines within these common minimum competencies, specific requirements for using home or nursing home settings for training are not emphasized.
The IM/FM geriatrics competencies were developed in the context of a growing mandate for residency programs to directly assess residents' clinical competence. The competencies are phrased as observable behaviors that in principle can be assessed. As framed by Miller,22 the goal is to measure residents' ability to “show how” or “do” clinical care, rather than merely “know” or “know how” to care for patients. Assessment methods best able to meet this challenge include standardized direct observation, detailed review of clinical cases, or live simulations of clinical encounters, rather than written examinations or global assessments with little direct observation (the current norm). The best methods to assess the IM/FM geriatrics competencies, where “best” is an optimal mix of reliability, validity, and feasibility, need to be defined. A multi-institutional project is underway to critically review existing learner assessment tools and methods in the context of the developed competencies, and to make recommendations regarding further development and/or implementation.
By explicitly articulating the IM/FM competencies with a parallel set of geriatrics competencies for medical students, we envision better coordination of teaching content and clinical experiences related to the care of older adults among medical schools and residency programs. In the context of numerous ongoing projects to define geriatrics competencies among surgical and related specialties14 and medical subspecialties,15 there is an opportunity to identify common and related competencies for all residents who care for older adults. Most immediately, the IM/FM geriatrics competencies can be used as a basis for defining competencies for medical subspecialty fellows, including geriatrics fellows. Eventually, an articulated set of essential geriatrics competencies can be developed for all residents and practitioners who care for older adults, as envisioned at a recent meeting of representatives of nearly two dozen specialty or subspecialty societies, certifying boards, and members of Residency Review Committees.3 To this end, significant progress has been made in coordinating the IM/FM resident competencies with recently developed parallel competencies in emergency medicine.23
Work is currently underway to secure formal support for the competencies by organizations of teachers, program directors, and the certifying boards of FM and IM, and to work with those organizations to help disseminate and implement the competencies. For example, the competencies are being compared to, and integrated with, the work of the American Board of Internal Medicine Milestones project, whose purpose is to identify a comprehensive set of competencies in each of the 6 ACGME competencies for IM residents at early and interim points in residency.24
By design, the IM/FM geriatrics competencies reflect the nexus among gaps in current physician training, patient needs, and the current and near-term structure of residency education and health care. They therefore possess some inherent limitations. They are not comprehensive, and so they inevitably underrepresent some important areas in the clinical care of older adults. They are also likely time limited, inevitably growing outdated as training programs and the health care system change to meet the demands of the 21st century. For example, if residency training and health care systems change to enhance the care of patients at hospital discharge, the role and essential competencies for physicians may be redefined. However, we believe the competencies are compatible with, and able to facilitate, the most fundamental near-term health system changes, such as improved care for chronic illness through the implementation of the Chronic Care Model25 and the Patient Centered Medical Home.26,27
Conclusions
The context and content of care for older patients are two of the major driving forces in near-term reforms to physician education and health care organization and financing. This relatively limited set of recommended essential competencies for IM and FM residents provides educators, policy makers, regulators, and payers with a roadmap to improve the clinical care that older people receive from IM and FM physicians.
Footnotes
Brent C. Williams, MD, MPH, is Associate Professor of Medicine in the Divisions of General Medicine and Geriatric Medicine, University of Michigan; Gregg Warshaw, MD, is Martha Betty Semmons Professor of Geriatric Medicine and Professor of Family Medicine at University of Cincinnati; Anne Rebecca Fabiny, MD, is Assistant Professor at Harvard Medical School; Nancy Lundebjerg, MPA, is Deputy Executive Vice President and Chief Operating Officer of the American Geriatrics Society; Annette Medina-Walpole, MD, is Associate Professor of Medicine in the Division of Geriatrics and Aging, University of Rochester Medical Center; Karen Sauvigne, MA, is Deputy Director of the Education Division, Brookdale Department of Geriatrics Palliative Medicine, Mount Sinai School of Medicine; Joanne G. Schwartzberg, MD, is Director of Aging and Health, American Medical Association; and Rosanne M. Leipzig, MD, PhD, is Gerald and May Ellen Ritter Professor in the Brookdale Department of Geriatrics Palliative Medicine, Mount Sinai School of Medicine.
Funding for this study was provided by the American Geriatrics Society, the American Medical Association, the American Board of Family Medicine Foundation, and the Society of General Internal Medicine.
The authors wish to thank the Association of Program Directors of Internal Medicine, the Association of Family Medicine Residency Directors, the American Geriatrics Society, the Society of General Internal Medicine, and the Society of Teachers of Family Medicine for recommending expert reviewers; the Donald W. Reynolds Foundation for sponsoring the national meeting at which key portions of the project were carried out; the John A. Hartford Foundation for sponsoring the initial meeting from which this project emanated; Cheryl Irmiter (American Medical Association) for participating in conference calls and reviewing the manuscript; and Yevgeniya Yarkikova-Hurd and Jared Rejeski (Mount Sinai School of Medicine, Portal of Online Geriatrics Education) for administrative support critical to the project.
Editor's Note: The online version (43.5KB, doc) of this article contains a list of the 52 geriatrics clinical content areas and the rationale and data (120.5KB, xls) for reducing 40 competencies to 26.
References
- 1.Institute of Medicine. Retooling for an Aging America: Building the Health Care Workforce. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- 2.Medicare Payment Advisory Commission. Report to the Congress. Improving incentives in the Medicare program. June 2009. Available at: http://www.medpac.gov/documents/Jun09_EntireReport.pdf. Accessed July 30, 2009.
- 3.Blumenthal D., Gokhale M., Campbell E. G., Weissman J. S. Preparedness for clinical practice: reports of graduating residents at academic health centers. JAMA. 2001;286(9):1027–1034. doi: 10.1001/jama.286.9.1027. [DOI] [PubMed] [Google Scholar]
- 4.Drickamer M. A., Levy B., Irwin K. S., Rohrbaugh R. M. Perceived needs for geriatric education by medical students, internal medicine residents, and faculty. J Gen Intern Med. 2006;21(12):1230–1234. doi: 10.1111/j.1525-1497.2006.00585.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warshaw G. A., Bragg E. J., Thomas D. C., Ho M. L., Brewer D. E. Are internal medicine residency programs adequately preparing physicians to care for the baby boomers? A national survey from the Association of Directors of Geriatric Academic Programs Status of Geriatrics Workforce Study. J Am Ger Soc. 2006;54(10):1603–1609. doi: 10.1111/j.1532-5415.2006.00895.x. [DOI] [PubMed] [Google Scholar]
- 6.Bragg E. J., Warshaw G. A., Arenson C. A., Ho M. L., Brewer D. E. A national survey of family medicine residency education in geriatric medicine: comparing findings in 2004 to 2001. Fam Med. 2006;38(4):258–264. [PubMed] [Google Scholar]
- 7.Reuben D. B., Bachrach P. S., McCreath H., et al. Changing the course of geriatrics education: an evaluation of the first cohort of Reynolds Geriatrics Education Programs. Acad Med. 2009;84(5):619–626. doi: 10.1097/ACM.0b013e31819fb89d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.John A. Hartford Foundation Centers of Excellence in Geriatric Medicine and Training Program Description. Available at: http://www.jhartfound.org/program/physicians.htm. Accessed May 25, 2009.
- 9.Williams B. C., Weber V., Babbott S. F., et al. Faculty development for the 21st century: lessons from the Society of General Internal Medicine-Hartford Collaborative Centers for the Care of Older Adults. J Am Ger Soc. 2007;55(6):941–947. doi: 10.1111/j.1532-5415.2007.01197.x. [DOI] [PubMed] [Google Scholar]
- 10.The AAMC-Hartford Geriatric Curriculum Program: reports from 50 schools. Anderson M. B., editor. Acad Med. 2004;79(suppl 7):S1–S226. ed. [Google Scholar]
- 11.Eleazer G. P., Brummel-Smith K. Commentary: aging America: meeting the needs of older Americans and the crisis in geriatrics. Acad Med. 2009;84(5):542–544. doi: 10.1097/ACM.0b013e31819f8da9. [DOI] [PubMed] [Google Scholar]
- 12.Potter J., Burton J., Drach G., et al. Geriatrics for residents in the surgical and medical specialties: implementation of curricula and training experiences. J Am Geriatr Soc. 2005;53(3):511–515. doi: 10.1111/j.1532-5415.2005.53173.x. [DOI] [PubMed] [Google Scholar]
- 13.Hazzard W. R., Woolard N., Regenstreif D. I. Integrating geriatrics into the subspecialties of internal medicine: the Hartford Foundation/American Geriatrics Society/Wake Forest University Bowman Gray School of Medicine Initiative. J Am Geriatr Soc. 1997;45(5):638–640. doi: 10.1111/j.1532-5415.1997.tb03102.x. [DOI] [PubMed] [Google Scholar]
- 14.American Geriatrics Society, the American Medical Association, and the Council of Medical Specialty Societies. Retooling for an Aging America: Building the Health Care Workforce. A “White Paper” regarding implementation of recommendation 4.2 of this Institute of Medicine report of April 14, 2008, that “All licensure, certification and maintenance of certification for health care professionals should include demonstration of competence in care of older adults as a criterion.” Available at: http://www.americangeriatrics.org/files/documents/white_paper.pdf. Accessed July 26, 2010.
- 15.Leipzig R. M., Granville L., Simpson D., Anderson M. B., Sauvigne K., Soriano R. P. Keeping Granny safe on July 1: a consensus on minimum geriatrics competencies for graduating medical students. Acad Med. 2009;84(4):604–610. doi: 10.1097/ACM.0b013e31819fab70. [DOI] [PubMed] [Google Scholar]
- 16.Abboud F. M., Ende J., Kelley M. A., et al. FCIM Internal Medicine Curriculum: A Resource Guide to Curriculum Development. Chapter 6. 2nd ed. Available at: http://www.acponline.org/education_recertification/education/training/fcim/. Accessed July 26, 2010.
- 17.Education Committee of the American Geriatrics Society. Curriculum guidelines on the care of the elderly for internal medicine residency training programs. Am J Med. 1997;103(4):260–262. [PubMed] [Google Scholar]
- 18.Sullivan G., Boling P., Ritchie C., Levine S. Curriculum recommendations for resident training in home care. J Am Geriatr Soc. 1998;46:910–912. doi: 10.1111/j.1532-5415.1998.tb02728.x. [DOI] [PubMed] [Google Scholar]
- 19.Warshaw G. A., Murphy J., Buehler J., Singleton S. Geriatric medicine training for family practice residents in the 21st century: a report from the Residency Assistance Program/Hartford Geriatrics Initiative. Fam Med. 2003;35(1):24–29. [PubMed] [Google Scholar]
- 20.Counsell S., Sullivan G. Curriculum recommendations for resident training in nursing home care. J Am Geriatr Soc. 1994;42(11):1200–1201. doi: 10.1111/j.1532-5415.1994.tb06989.x. [DOI] [PubMed] [Google Scholar]
- 21.Accreditation Council for Graduate Medical Education. ACGME Outcome Project. Available at: http://www.acgme.org/outcome/. Accessed July 26, 2010.
- 22.Miller G. E. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(suppl 9):S63–S67. doi: 10.1097/00001888-199009000-00045. [DOI] [PubMed] [Google Scholar]
- 23.Hogan T., Losman E., Carpenter C., et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med. 2010;17(3):316–324. doi: 10.1111/j.1553-2712.2010.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Green M. L., Aagaard E., Caverzagie K., et al. Charting the road to competence: developmental milestones for internal medicine residency training. J Grad Med Educ. 2009;1(1):5–20. doi: 10.4300/01.01.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wagner E. H., Austin B. T., Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511–544. [PubMed] [Google Scholar]
- 26.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Joint principles of the patient-centered medical home. March 2007. Available at: http://www.medicalhomeinfo.org/downloads/pdfs/jointstatement.pdf. Accessed May 30, 2009.
- 27.Boult C., Christmas C., Durso S. C., Leff B., Boult L. B., Fried L. P. Perspective: transforming chronic care for older persons. Acad Med. 2008;83(7):627–631. doi: 10.1097/ACM.0b013e3181782b14. [DOI] [PubMed] [Google Scholar]