In this issue of the Journal, the Pediatrics Milestone Working Group describes an innovative and unique process for addressing the charge from the Accreditation Council for Graduate Medical Education (ACGME) and the American Board of Pediatrics to further define the 6 ACGME competencies along with performance standards for our specialty. After 18 months of intense learning, discussion, writing, and rewriting, we have a first iteration of our work. This is not the end but rather the beginning. Where do we go from here? In this brief commentary we hope to provide the background and rationale for our suggested next steps.
Background and Rationale
We are at a pivotal point in graduate medical education (GME). Currently, the stars (undergraduate medical education, GME, and Maintenance of Certification [MOC]) are aligning around the ACGME competencies, creating an unprecedented opportunity for collaboration and creation of a true educational continuum.1–3 But opportunity and challenge go hand in hand. How do we create a continuum of competency-based medical education that is meaningful?
A decade after the initiation of the Outcome Project by the ACGME,1 there is still confusion and controversy about how to integrate the competencies into training in a meaningful way.4 One barrier to implementation has been the lack of integration of the competencies across the educational continuum. However, two important decisions are breaking down this barrier: (1) the Association of American Medical Colleges2 published a document in 2006 stating that “each of the ACGME competencies is appropriate for undergraduate medical education, some in greater depth than others”; and (2) the American Board of Medical Specialties, a partner in the ACGME Outcome Project, incorporated the competencies into their conceptual framework for MOC, resulting in 4 required components of MOC in pediatrics that map to the 6 ACGME competencies.3 Integrating the competencies into the medical school curriculum and building on them during GME and throughout the MOC process improves the efficacy and perhaps the efficiency of overall education and training, and it makes the competencies more meaningful at every step.
Pediatric Milestones
A second barrier to the integration of the competencies into medical education has been the lack of understanding of how the knowledge, skills, and attitudes needed to perform these complex tasks develop over time. Thus, the ACGME embarked on the Milestone Project, designed to allow specialties to identify the behaviors and attributes that describe the competencies, with attention to performance standards, at the completion of each year of residency training. As Hicks and colleagues describe in “The Pediatrics Milestones: Conceptual Framework, Guiding Principles, and Approach to Development”5 in this issue of the Journal, the Pediatrics Milestone Working Group took a unique approach in framing the milestones in the context of a developmental continuum from the medical student to the seasoned practitioner.
Entrustable Professional Activities
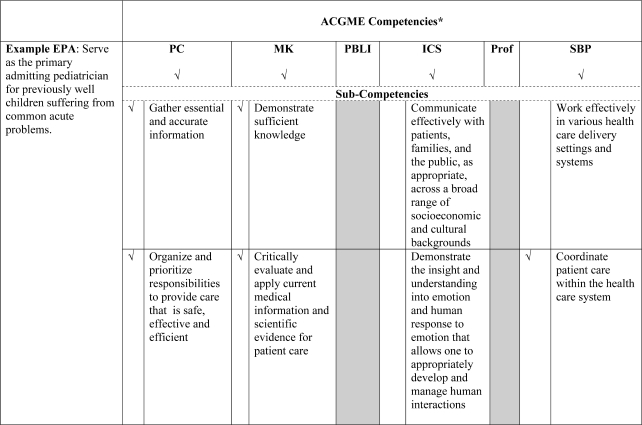
A third barrier to the integration of the competencies has been the perception of a lack of applicability to real-world practice. This barrier results from our tendency to reduce the competencies, which are complex tasks, to simple behaviors so that we can more easily assess them. This granularity does not reflect the complex integration of the competencies needed in actual day-to-day practice, and it perpetuates the view that the competencies are isolated and somewhat superficial add-ons to training requirements. The next challenge, therefore, is identifying the bridge to connect the competencies to “real world” and “real time” practice. A potential “bridge,” described in a seminal article by ten Cate and Scheele,6 is the identification of “entrustable professional activities” (EPAs). EPAs are simply the routine professional-life activities of physicians based on their specialty and subspecialty.6 For example, an EPA for a pediatric hospitalist may be to “serve as the primary admitting pediatrician for previously well children suffering from common acute problems.”4 In order to perform this professional activity, a practitioner must (1) have knowledge of the signs and symptoms of these illnesses, (2) perform a physical examination to elicit confirmatory findings, (3) search for outcomes associated with specific therapeutic interventions, (4) communicate with the patient and the family about the management plan, (5) relate to families in a way that they understand, based on cultural background and health literacy, and (6) act as a liaison to the primary care physician who will see this patient in follow-up. Framing the 6 ACGME competencies within the clinical context of an EPA takes them out of the realm of the abstract and grounds them in a way that makes them meaningful to both learners and faculty. Miller's7 pyramid, a hierarchy of competence, begins with “knows,” moves through stages of “knows how” and “shows-how,” and culminates in “does.” Assessment of an EPA aligns with “does” in Miller's pyramid. This is a critical point. “Just as trainees' scores for ‘knows’ and ‘knows how’ do not necessarily predict scores for ‘shows how,’ all these may not predict ‘does.’”8
Why “Entrustable?”
A fourth barrier to integration of the competencies is the challenge of assessing them in a meaningful way due to their complexity and our limited repertoire of reliable and valid tools. The concept of “entrustment” will help us meet this challenge. The word entrustable designates that “a practitioner has demonstrated the necessary knowledge, skills and attitudes to be trusted to independently perform this activity.”5 Faculty attending on the wards can articulate the level of supervision required of a given resident to perform the example EPA for a hospitalist. Provided that there is the opportunity to develop a relationship with a resident over time, the attending will know when to “entrust” the resident with this EPA, meaning the resident is capable of performing the EPA independently or, in ACGME parlance, “without direct supervision.” Thus, faculty will be able to provide more meaningful feedback and assessment when the competencies are framed in the clinical context of an EPA.
Competencies, Milestones, and EPAs
The milestones provide a developmental roadmap for the competencies and subcompetencies. They are behavioral descriptions of the developmental progression of the knowledge, skills, and attitudes that define each of the subcompetencies within the broader competency domain. They therefore serve to inform learners of where they are and the necessary knowledge, skills, and attitudes to progress to the next level(s). Entrustable professional activities represent the core clinical activities of a specialist, subspecialist, resident, or medical student, appropriately scaled to level of experience. Performing these core clinical activities requires one to integrate the competencies and subcompetencies. Since the milestones map directly to the subcompetencies, they help to pinpoint at what level in the developmental progression a resident is performing and to address any specific subcompetencies that may be barriers to entrustment. Specific milestones must be reached for entrustment to occur.
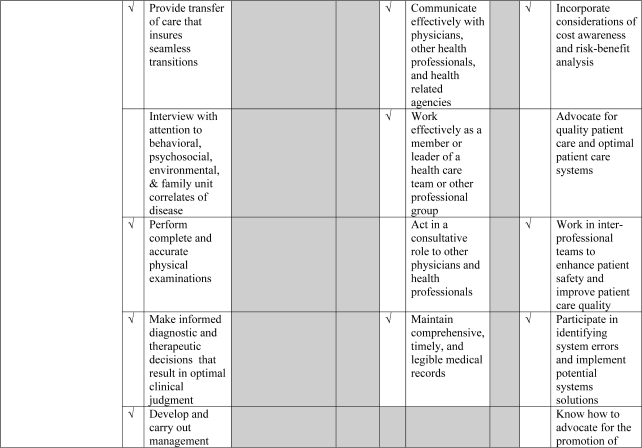
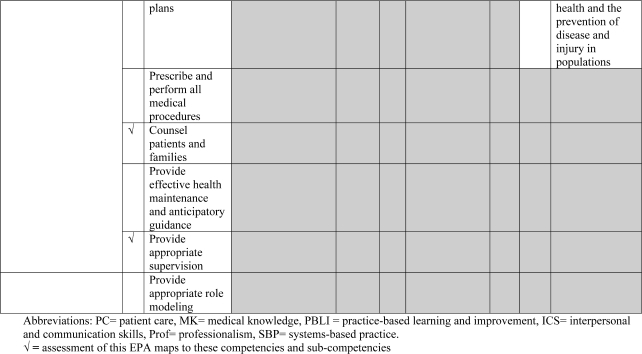
The previous example of the EPA for the hospitalist can be mapped to all of the competencies; however, some competencies are more important than others for assessing this EPA (likely patient care, medical knowledge, interpersonal and communication skills, and systems-based practice; see the figure). Additionally, the local context will be important in prioritizing which additional competencies and which subcompetencies are highlighted.
Figure.
An Example EPA Mapped to the Most Relevant ACGME Competencies, With Further Mapping to the Most Relevant Subcompetencies
Figure.
(Continued)
Figure.
(Continued)
Coming full circle, the “bridge” function of EPAs is well illustrated in the example EPA for a hospitalist. The experiential learning begins in medical school during core clerkships and subinternships and continues to be practiced on inpatient ward months during residency, both for the junior resident functioning as a primary caretaker and the senior resident functioning as a team leader. More-targeted and developmentally appropriate EPAs could be created for medical students from the broader EPAs written for residents (O. ten Cate, written communication, May 2010), fostering the importance of a continuum for learning. If this were the case, GME directors could expect incoming interns to start with a consistent skill set, and efforts during residency could be directed at building upon an established baseline, taking the resident further along the developmental continuum.
EPAs and Milestones in a Broader Context: The Carnegie Report
A recent report commissioned by the Carnegie Foundation9 to study the current state of affairs in medical education and to make recommendations outlines 4 goals: (1) standardization of learning outcomes and individualization of the learning process, (2) integration of formal knowledge and clinical experience, (3) development of habits of inquiry and innovation, and (4) focus on professional-identity formation. Essentially 3 of these 4 goals may be met by implementing the Milestone Project across the continuum of education, training, and practice. By definition, the milestones standardize the learning outcomes and provide a developmental continuum for their progression, thus addressing the first half of goal 1. In addition, if the pediatrics community can come to consensus on identifying the core EPAs for our specialty, we can map the competencies, subcompetencies, and milestones to them, thereby addressing goal 2. The EPA framework incorporates knowledge, skills, and attitudes across the continuum of education, connecting undergraduate medical education, GME, and MOC and thus facilitating the integration of formal knowledge and clinical experience. Finally, in approaching the Milestone Project, the pediatric community, led by the Association of Pediatric Program Directors, also identified a need to focus on professional-identity formation and thus developed milestones to specifically address this core area of competence, as highlighted in goal 4 of the Carnegie report. As a community, pediatrics is poised to take the next important step of creating a true medical education continuum, using the common framework of competencies developmentally framed within milestones and made meaningful through real-world application in EPAs. It is a step that has the potential to transform pediatric medical education, with the ultimate hope of improving the care of children.
Footnotes
Carol Carraccio, MD, is Associate Chair for Education at University of Maryland Hospital for Children; and Ann E. Burke, MD, is Pediatric Program Director at Dayton Children's Medical Center and Wright State University Boonshoft School of Medicine.
The authors have no conflicts of interest to disclose.
References
- 1.Accreditation Council for Graduate Medical Education. Outcome Project. Available at: http://www.acgme.org/outcome. Accessed July 8, 2010. [DOI] [PubMed]
- 2.Ad Hoc Committee of Deans. Educating Doctors to Provide High Quality Medical Care. Washington, DC: Association of American Medical Colleges; 2006. [Google Scholar]
- 3.American Board of Pediatrics. Understanding Maintenance of Certification—MOC. Available at: https://www.abp.org/ABPWebStatic/#murl%3Dresfellows.htm. Accessed July 9, 2010.
- 4.Jones M. D., Rosenberg A., Gilhooly J., Carraccio C. Competencies, outcomes and controversy. Acad Med. In press. [DOI] [PubMed]
- 5.Hicks P. Pediatrics Milestones Project: the approach to and progress in construction of developmentally anchored milestones. J Grad Med Educ. 2010;2(3):410–418. doi: 10.4300/JGME-D-10-00126.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ten Cate O., Scheele F. Competency-based postgraduate training: can we bridge the gap between theory and clinical practice? Acad Med. 2007;82(6):542–547. doi: 10.1097/ACM.0b013e31805559c7. [DOI] [PubMed] [Google Scholar]
- 7.Miller G. The assessment of clinical skills, competence, and performance. Acad Med. 1990;65(suppl 9):S63–S67. doi: 10.1097/00001888-199009000-00045. [DOI] [PubMed] [Google Scholar]
- 8.Ten Cate O. Trust, competence, and the supervisor's role in postgraduate training. BMJ. 2006;333(7571):748–751. doi: 10.1136/bmj.38938.407569.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooke M., Irby D. M., O'Brien B. C. Educating Physicians—A Call for Reform of Medical School and Residency. San Francisco, CA: Jossey-Bass; 2010. [Google Scholar]