Abstract
Objectives:
This study seeks to identify factors for hepatectomy in the management of post-cholecystectomy bile duct injury (BDI) and outcome via a systematic review of the literature.
Methods:
Relevant literature was found by searching the PubMed database and the bibliographies of extracted articles. To avoid bias selection, factors for hepatectomy were analysed in series reporting both patients undergoing hepatectomy and patients undergoing biliary repair without hepatectomy (bimodal treatment). Relevant variables were the presence or absence of additional hepatic artery and/or portal vein injury, the level of BDI, and a previous biliary repair.
Results:
Among 460 potentially relevant publications, only 31 met the eligibility criteria. A total of 99 hepatectomies were reported among 1756 (5.6%) patients referred for post-cholecystectomy BDI. In eight series reporting bimodal treatment, including 232 patients, logistic regression multivariate analysis showed that hepatic arterial and Strasberg E4 and E5 injuries were independent factors associated with hepatectomy. Patients with combined arterial and Strasberg E4 or E5 injury were 43.3 times more likely to undergo hepatectomy (95% confidence interval 8.0–234.2) than patients without complex injury. Despite high postoperative morbidity, mortality rates were comparable with those of hepaticojejunostomy, except in urgent hepatectomies (within 2 weeks; four of nine patients died). Longterm outcome was satisfactory in 12 of 18 patients in the largest series.
Conclusions:
Hepatectomies were performed mainly in patients showing complex concurrent Strasberg E4 or E5 and hepatic arterial injury and provided satisfactory longterm outcomes despite high postoperative morbidity.
Keywords: hepatectomy, bile duct injury, laparoscopic cholecystectomy
Introduction
Post-cholecystectomy bile duct injury (BDI) remains a major health concern as its incidence has increased two-fold since the advent of laparoscopic cholecystectomy compared with that in open procedures.1,2 Despite the evident learning curve, injuries that occurred in laparoscopic surgery were shown to be more complex than those occurring during the open procedure because of the more proximal location of injury in the biliary tree and its frequent association with vascular injury.3 Although minor BDI, such as leakage from the cystic duct or common bile duct, can often be managed endoscopically, surgical reconstruction is needed for major BDI.4,5 In most patients, repair of BDI consists of immediate or delayed Roux-en-Y hepaticojejunostomy.6 In rare situations, management of these post-cholecystectomy BDIs requires hepatectomy.7 The aim of the present study was to specifically analyse, via a literature review, the factors and circumstances that led to the decision for hepatectomy in the management of post-cholecystectomy BDI. The results of such hepatectomies were further analysed in terms of postoperative morbidity and mortality and longterm outcome.
Materials and methods
A literature search was conducted for the period 1990 to July 2008 using the PubMed database, employing the search terms ‘biliary leakage and hepatectomy’, ‘bile duct injury and hepatectomy’, ‘biliary stenosis and hepatectomy’ and ‘cholecystectomy and hepatectomy’. The bibliographies of extracted articles were further cross-referenced. Both analyses by studies and by patients were performed to identify factors for hepatectomy. The aim of the analysis per study was to compare the study populations in their entirety and to search for differences in BDI features that might explain the differences between teams in the management of these BDIs. By contrast, in order to avoid selection bias, the analysis per patient focused on studies that reported on same-team treatment outcomes for patients who underwent biliary reconstruction without hepatic resection as well as patients in whom hepatic resection was required with the biliary reconstruction (bimodal treatment). Only studies providing information on the factors of interest, namely, the presence or absence of additional hepatic artery injury, portal vein injury and the level of BDI (Bismuth8 and/or Strasberg2 classification), were included. Complex BDIs were defined as proximal BDIs with disruption of the hepatic ductal confluence (Bismuth level 4 or 5; Strasberg type E4 or E5) or any BDI level with concurrent arterial injuries. When available, other data, such as the period of inclusion of patients or previous biliary reconstruction, were collected. Hepatectomies were regarded as urgent when performed within the first 2 weeks. Patients who underwent liver transplantation for post-cholecystectomy BDI or hepatectomy for BDI that was not related to cholecystectomy were excluded from this study. Likewise, partial resection of segments IV and V to allow adequate exposure of the bile duct9 was not considered as hepatectomy in this study.
Statistical analysis
Continuous variables were expressed as means (or medians when indicated) and compared using the Mann–Whitney test. Categorical variables, expressed as frequencies and percentages, were compared using chi-squared tests or Fisher exact tests, as appropriate. To identify independent factors of hepatectomy, variables identified as significant in univariate analysis were subsequently included in stepwise logistic regression analysis. The variables of interest were then compared among four groups of patients with: combined arterial and Strasberg E4 or E5 injuries; isolated hepatic arterial injury; isolated Strasberg E4 or E5 injury, or none of these injuries. For logistic regression models, odds ratios and 95% confidence intervals (CIs) were reported relative to a chosen reference group. Statistical significance was considered for P < 0.05. All analyses were performed using spss Version 13.0 (SPSS, Inc., Chicago, IL, USA).
Results
The search strategy identified 460 publications reporting various studies of which 31 met the inclusion criteria (Fig. 1). Of these 31 studies, 10 were case reports and 21 were retrospective series. For three teams, patient(s) undergoing hepatectomy were reported on twice;9–14 those patients were pooled and considered as one study for each team. Among other extracted articles that reported on only biliary repair with no hepatectomy, 31 studies that provided enough information on the factors of interest described above were used as a control group in the analysis per study.
Figure 1.
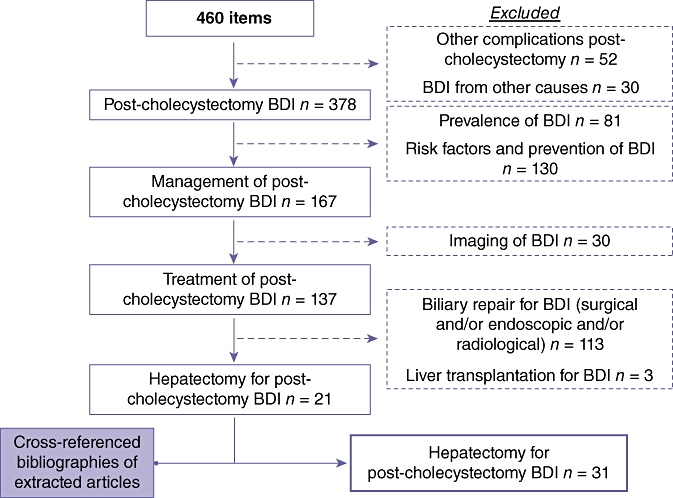
Flow chart showing details of articles selected from the PubMed database, subsequent exclusions and cross-referenced bibliographies of extracted articles. BDI, bile duct injury
Analysis per study
Study population
Altogether, 99 patients who underwent hepatectomy for post-cholecystectomy BDI (12 in case reports, 87 in the series reporting bimodal treatment) were identified in a total of 1756 patients (5.6%) and are summarized in Table 1. Overall, 91.5% (65/71 patients in 22 studies) of hepatectomies were performed after laparoscopic cholecystectomy. For anatomical reasons, right lobectomy was the most frequently performed hepatectomy (n = 79/99, 79.8%) (Table 1). In the 21 series reporting bimodal treatment, the median (range) incidence of hepatectomy was 6.1% (1–20%) of all patients referred for BDI, with a median number of three (one to 18) hepatectomies per series (Table 1). Previous biliary reconstruction had been performed in 71.2% (47/66) of patients.
Table 1.
Reported cases of hepatectomy performed for the management of bile duct injury
| Author | Year | Patients, n/totala (%) |
Vascular injury |
Complex injuriesb, n | Time of hepatectomy | Definitive treatment | |
|---|---|---|---|---|---|---|---|
| RHAI | PVI | ||||||
| Branum et al.16 | 1993 | 2/50 (4) | NS | NS | 2 | NS | Right lobectomy |
| Madariaga et al.34c | 1994 | 2/15 | 2 | 1 | 2 | 5/21 days | Right lobectomy |
| Ohtsuka et al.20 | 1999 | 10 | 0 | 0 | 1 | 4 months | Right lobectomy |
| Nishio et al.15 | 1999 | 10 | 1 | 1 | 1 | 135 days | Right lobectomy |
| Topal et al.24 | 1999 | 1/16 | 0 | 0 | 1 | NS | Left lateral sectionectomy |
| Uenishi et al.23 | 1999 | 10 | 1 | 0 | 1 | 13 months | Right lobectomy |
| Lichtenstein et al.33c | 2000 | 2/16 | 0 | 0 | 2 | 4/28 days | Segment V–VI resection |
| Nishiguchi et al.51 | 2000 | 10 | 0 | 0 | 1 | 13 months | Right lobectomy |
| Gazzaniga et al.22 | 2001 | 1/60 (1.7) | NS | NS | NS | NS | Left lateral sectionectomy |
| Kayaalp et al.48c | 2001 | 20 | 2 | 0 | 2 | 4–15 days | Right lobectomy |
| Wong et al.52 | 2001 | 1 | 1 | 1 | 1 | 5 weeks | Right lobectomy |
| Buell et al.32 | 2002 | 3/49 | 3 | 0 | 3 | NS | Right lobectomy |
| Heinrich et al.53c | 2003 | 10 | 0 | 1 | 1 | 2 weeks | Right lobectomy |
| Schmidt et al.11,12 | 2002–2004 | 3/54 (5.5) | 3 | 0 | 3 | NS, 4, 8 months | Right lobectomy |
| Frilling et al.26 | 2004 | 5/40 | 4 | 0 | 4 | NS | Right lobectomy |
| Ota et al.17 | 2004 | 10 | 0 | 0 | 1 | 144 days | Right lobectomy |
| Sekido et al.19 | 2004 | 2/10 | 2 | 0 | 2 | 2.5/5 months | Right lobectomy |
| Stewart et al.43 | 2004 | 4/261 (1.5) | 4 | 0 | 4 | NS | Partial lobectomy (3), right lobectomy (1) |
| Mercado et al.9 | 2006 | 3/285 (1.1) | NS | NS | 3 | NS | Right lobectomy |
| De Santibanes et al.27 | 2006 | 9/169 (5.3) | NS | NS | 9 | NS | Right lobectomy (7) or left hepatectomy (2) |
| Felekouras et al.54c | 2007 | 10 | 1 | 1 | 1 | 1 day | Right lobectomy |
| Yan et al.35 | 2007 | 1/8 | 1 | 0 | 1 | NS | Right lobectomy |
| Wu et al.55 | 2007 | 2/210 (1) | NS | NS | NS | NS | Right lobectomy |
| Li et al.56 | 2007 | 3/60 (5) | 3 | 0 | 3 | NS | Right lobectomy |
| Ragozzino et al.57c | 2007 | 20 | 2 | 2 | 2 | 2–3 days | Right lobectomy |
| Ortega-Deballon et al.31c | 2007 | 1/18 | 1 | 0 | 1 | NS | Right lobectomy |
| Bektas et al.28 | 2007 | 12/74 (16.2) | 6 | 3 | 7 | NS | Right lobectomy (10), segmentectomy (2) |
| Thomson et al.21 | 2007 | 8/119 (6.7) | 4 | 1 | 7 | 6–95 months | Right lobectomy (6), left lateral sectionectomy (2) |
| Alves et al.10Laurent et al.14 | 2003–2008 | 18/120 (15) | 11 | 4 | 18 | 7 days to 21 years | Right (14) or left (3) lobectomy or left trisectionectomy (1) |
| Nuzzo et al.58 | 2008 | 2/77 (2.6) | NS | NS | NS | NS | Right hepatectomy |
| Truant et al.30 | 2009 | 3/45 | 1 | 0 | 3 | 8, 18, 30 years | Right lobectomy (2) or left hepatectomy (1) |
| Total | 99/1756 (5.6) | 53/80d (66.3%) | 15/80d (18.8%) | 87/94d (92.6%) | Right lobectomy | ||
Total number of patients referred for bile duct injury
Complex injuries were defined as proximal biliary injuries with disruption of the hepatic ductal confluence (Bismuth level 4 or 5; Strasberg type E4 or E5) or any biliary level injury with concurrent arterial injuries
Urgent hepatectomy
Total including only patients for whom information was specified
RHAI, right hepatic artery injury; PVI, portal vein injury; NS, not specified
The frequency of vascular injury, severity of biliary injury and timing of hepatectomy are shown in Table 1. In nine patients, urgent hepatectomy (within 2 weeks) was needed in cases of parenchymal necrosis caused by combined biliary and vascular injury following laparoscopic cholecystectomy (Table 1). Substantial variations existed in the indications mentioned for postponed hepatectomy, as follows: recurrent biliary sepsis;12,15 biliary strictures caused by continuous cholangitis;12,16,17 development of intrahepatic abscesses;18,19 non-visualization and/or unsuitability of the proximal stump of the injured bile duct(s) for anastomosis;9,20,21 intrahepatic injuries of an aberrant right hepatic duct;20 anastomotic strictures and intrahepatic lithiasis;21,22 right hepatic lobe atrophy with23,24 or without10,21 recurrent cholangitis; secondary biliary cirrhosis;11,12 hepatic confluence stented with metallic stents,14,25 or primary non-diagnosed Klatskin tumour.26 Such indications were related to symptoms in all patients.
Postoperative morbidity, mortality and outcome of hepatectomies
Rates of postoperative morbidity were high, mainly secondary to infectious complications14,21,27 (Table 2). In one series of 18 patients, despite the use of intermittent portal trial clamping in 14 patients (78%), 12 patients required a blood transfusion for a mean of 6 ± 3.6 units (range 2–12 units).14 Biliary fistula occurred in 25% (3/12)28 to 39% (7/18)14 of patients. One study also reported a longer hospital stay than that found among patients who underwent hepatectomy for other reasons.29 Postoperative death following hepatectomy occurred in 11.1% (9/81) of patients for whom data were available. Nevertheless, mortality was significantly lower in those undergoing non-urgent hepatectomy compared with urgent (within 2 weeks) hepatectomy (2/53 vs. 4/9 patients; P = 0.003). With regard to longterm outcome, the largest series14 reported that 13 of 18 patients who underwent hepatectomy for complex BDI had no symptoms after a median follow-up of 8 years (range 3–12 years) (Table 2).
Table 2.
Postoperative morbidity, mortality and outcome of hepatectomy in the management of post-cholecystectomy bile duct injury
| Author | Year | Patients, n | Complex injuriesa, n | Morbidityb, n | Mortalityb, n | Longterm outcome |
|---|---|---|---|---|---|---|
| Madariaga et al.34c | 1994 | 2 (1c) | 2 | – | 0 | Good at 14–16 months |
| Uenishi et al.23 | 1999 | 1 | 1 | – | 0 | Good at 22 months |
| Lichtenstein et al.33c | 2000 | 2 (1c) | 2 | – | 0 | Good at 12–13 months |
| Kayaalp et al.48c | 2001 | 2 (2c) | 2 | – | 1 | Good at 3 years (one postoperative death) |
| Buell et al.32 | 2002 | 3 | 3 | NS | 2 | NS |
| Schmidt et al.11,12 | 2002–2004 | 3 | 3 | NS | 1 | Good at 39 months/SBC at 83 months (one postoperative death) |
| Heinrich et al.53c | 2003 | 1 | 1 | – | 0 | – |
| Ota et al.17 | 2004 | 1 | 1 | – | 0 | Good at 5 years |
| Sekido et al.19 | 2004 | 2 | 2 | – | 0 | No symptoms at 16–36 months |
| Frilling et al.26 | 2004 | 5 | 4 | NS | 1 | NS |
| De Santibanes et al.27 | 2006 | 9 | 9 | 3 | 0 | NS |
| Yan et al.35 | 2007 | 1 | 1 | – | 0 | Normal postoperative liver function |
| Li et al.56 | 2007 | 3 | 3 | NS | 1 | No symptoms at >12 months (one postoperative death) |
| Felekouras et al.54c | 2007 | 1 | 1 | – | 1 | – |
| Ragozzino et al.57c | 2007 | 2 (2c) | 2 | – | 1 | – |
| Thomson et al.21 | 2007 | 8 | 7 | 5 | 0 | Good in 8/8 (time of follow-up not specified) |
| Ortega-Deballon et al.31c | 2007 | 1 | 1 | – | 1 | – |
| Alves et al.10Laurent et al.14 | 2008 | 18 | 18 | 11 | 0 | No symptoms in 13/18 patients; median (range) follow-up: 8 (3–12) years |
| Truant et al.30 | 2009 | 3 | 3 | 2 | 0 | Good at 13, 17, 63 months |
Complex injuries were defined as proximal biliary injuries with disruption of the hepatic ductal confluence (Bismuth level 4 or 5; Strasberg type E4 or E5) or any biliary level injury with concurrent arterial injuries
Number of complication(s) and death(s) are given for studies reporting at least three cases of hepatectomy
Urgent hepatectomy (when more than one hepatectomy were performed, the number of urgent hepatectomies is given in parentheses in the Patients, n column)
NS, not specified; SBC, secondary biliary cirrhosis
Comparison of patient features between series reporting bimodal treatment and control studies
When the study populations were considered in their entirety, the 21 series reporting bimodal treatment were found to be comparable with the 31 control studies in terms of laparoscopic approach (75.4% [range 23–100%] vs. 76.3% [range 0–100%], respectively; P = 0.60) and periods of inclusion (median time of inclusion before the year 2000 in 90.5% vs. 90.6%; P = 1.00). By contrast, when the 21 series reporting bimodal treatment were compared with the 31 control studies, the incidences of hepatic arterial injury (22.3% [range 0–100%] vs. 13.0% [range 0–61.1%], respectively; P < 0.001], portal vein injury (1.0% [range 0–6.7%] vs. 0.1% [range 0–3.4%], respectively; P = 0.047), complex BDI (26.5% [range 17.8–100%] vs. 21.7% [range 0–100%], respectively; P = 0.01) and previous biliary reconstruction (46.0% [range 0–100%] vs. 41.4% [range 0–100%], respectively; P = 0.042) were significantly higher.
Analysis per patient
Among the 21 studies reporting bimodal treatment, eight19,28,30–35 provided enough detail per patient on the variable of interest, which included: injury of the hepatic artery and/or portal vein; proximal pattern of BDI (Strasberg E4 or E5 injury), and, to a lesser extent, previous biliary reconstruction. Other potential factors, such as referral pattern, and presence or absence of sepsis or lobar atrophy, could not be assessed, as insufficient data were provided. Data were collected from these eight studies for a total of 233 patients and results are shown in Table 3. One patient was excluded from analysis as he underwent liver transplantation. Logistic regression models were performed for 182 patients for whom data on all the variables of interest were available; results are shown in Table 4.
Table 3.
Univariate analysis: comparison of patients who underwent hepatectomy with patients who underwent biliary repair in series reporting bimodal treatment
| n (%) | No hepatectomy (n = 206), n | Hepatectomy (n = 26), n | P-value | |
|---|---|---|---|---|
| Artery injury | 45 (19.3) | 29 | 16 | <0.001 |
| Portal vein injury | 5 (2.1) | 1 | 4 | 0.001 |
| Strasberg E4 or E5 injury | 25/182a (13.7) | 15/158a | 10/24a | <0.001 |
| Previous biliary reconstruction | 65/158a (41.1) | 56/144a | 9/14a | 0.06 |
Missing data for remaining patients
Table 4.
Multivariate analysis of 182 patients (hepatectomy: n = 23; biliary repair: n = 159) for whom data on all the variables of interest (hepatic artery injury, portal vein injury and Strasberg E4 or E5 injury) were available
| Factors | P-value |
Hepatectomy |
||
|---|---|---|---|---|
| OR | 95% CI for OR | |||
| Hepatic artery injury | Yes vs. no | <0.001 | 7.7 | 2.6–22.4 |
| Portal vein injury | Yes vs. no | 0.1 | 6.9 | 0.6–75.7 |
| Strasberg E4 or E5 injury | Yes vs. no | 0.003 | 5.7 | 1.8–17.9 |
| Complex injury | ||||
| No hepatic artery, no Strasberg E4 or E5 injury | 1.0 | – | ||
| Isolated artery injury | <0.001 | 14.9 | 4.3–51.6 | |
| Isolated Strasberg E4 or E5 injury | <0.001 | 11.8 | 2.9–47.2 | |
| Artery + Strasberg E4 or E5 injury | <0.001 | 43.3 | 8.0–234.2 | |
A separate logistic regression model was used to evaluate the independent effect of complex injury, (hepatic artery injury or Strasberg E4 or E5 injury, or both), in comparison with the group with neither hepatic artery nor Strasberg E4 or E5 injury
OR, odds ratio; 95% CI, 95% confidence interval
Discussion
Overall, 99 hepatectomies have been reported thus far in the management of post-cholecystectomy BDI. This review is the first to show that proximal biliary injuries with disruption of hepatic ductal confluence (Strasberg types E4 or E5) and/or concurrent arterial injuries are independent factors for hepatectomy in the management of post-cholecystectomy BDI. Among 31 studies, 92.6% of 99 patients undergoing hepatectomy had an underlying complex BDI. Patients with combined arterial and Strasberg E4 or E5 injuries were at particular risk of hepatectomy, with an odds ratio of 43.3 (95% CI 8.0–234.2) (Table 4), compared with patients with none of these complex injuries.
Overall, 91% (91/99) of hepatectomies performed for the management of post-cholecystectomy BDI were reported after the year 2000 – one decade after the advent of laparoscopic cholecystectomy – and were carried out mostly by teams specializing in hepatobiliary surgery (Table 1). This strongly contrasted with older series reported by specialist hepatobiliary surgery teams,36 but also with recent series3,37–39 reporting no hepatectomy despite concomitant vasculo-biliary injuries with or without lobar atrophy. This new indication for hepatectomy may reflect the specific complexity of laparoscopic BDI, which is considered difficult to repair with uncertain outcome. Overall, there were significant differences in the rates of concomitant vascular injuries and complex injuries between teams reporting hepatectomies performed in the management of BDI patients and those performing biliary repair exclusively by hepaticojejunostomy. The enhanced complexity of BDI has certainly impacted the decision to perform hepatectomy in this setting.
Indeed, in recent years, certain teams have deliberately chosen to perform hepatectomy in patients with complex laparoscopic BDI for reasons related to the excellent longterm outcome of hepatectomy.14 In the present review, rates of good or excellent (no symptoms) results of hepatectomy series, which ranged from 72% (13/18) to 100% (8/8) in the two largest series,14,21 were comparable with those obtained in most series of BDI patients treated by hepaticojejunostomy.3,36,40,41 By contrast, given the expected difficulties in dissection of such hepatectomies and their high morbidity rates, which are higher than those reported in the literature for biliary repair, it is likely that additional factors were taken into account in the choice of this treatment.
In fact, most indications for performing hepatectomy were encountered in patients displaying concurrent arterial and proximal injuries with disruption of the hilar confluence, with an odds ratio for hepatectomy of 43.3 (95% CI 8.0–234.2) (Table 4), in comparison with patients with neither arterial nor proximal Strasberg E4 or E5 injury. Indeed, over the longterm, such complex concomitant vasculo-biliary injuries were shown to compromise the viability of biliary ducts and/or parenchyma of the hemi-liver because confluence disruption impaired the development, within the hilar plate, of omega-shaped collateral arterial circulation originating from the preserved branch of the hepatic artery.10 In this setting, the justification for partial hepatectomy was based on the danger of irreversible fibrotic and atrophic parenchyma, with high risk for secondary complications such as persistent cholangitis as a result of vascular or septic lesions. In accordance with the findings of this study, one recent study of 74 BDI patients showed that the type of vascular involvement and the location of the lesion, at or above the bifurcation of the hepatic duct, had a major impact on the extent of surgical intervention for iatrogenic BDI and especially the need for hepatectomy.28
For similar reasons, the need for hepatectomy was associated, in the present study, with a higher rate of previous biliary reconstruction, with a trend towards significance when compared with patients who had biliary repair (P = 0.06) (Table 3). Each failed repair is indeed associated with some loss of bile duct length and requires more substantial dissection in the pedicle, with subsequent damage to the vascularization of the bile duct.36,42 Stewart et al.43 studied the impact of injury propagation in successive operations (i.e. the increase in the proximal extent of the BDI between initial injury and subsequent successful reconstruction) upon the incidence of hepatic arterial injury. For injuries located at or above the bifurcation of the common hepatic duct, 49% of those without injury propagation had right hepatic artery injury in comparison with 71% of those with injury propagation (P < 0.05). These authors further showed that the need for hepatectomy was more common among patients with arterial injury than among those without such injury, but only in patients in whom biliary repair had been performed by a surgeon who was inexperienced in hepatobiliary repair.43 These data underline the importance of early referral to a tertiary centre in BDI patients, as previously reported.44
By contrast, when the biliary confluence was preserved, patients with and without hepatic arterial injuries had comparable longterm outcomes, provided that high-level repair using the Hepp–Couinaud technique45 was performed to guarantee non-ischaemic bilioenteric anastomosis.10,36,38 Over one-third of patients with injuries for which Strasberg E4 or E5 classification was the only criterion of gravity underwent hepatectomy, which appears high despite the fact that the integrity of the hilar confluence was shown to be important in predicting postoperative biliary stricture.4,9,38 With respect to the Hepp–Couinaud technique, hepatectomy for Strasberg E4 or E5 BDIs should not be indicated in patients without fibrosis or significant vascular compromise except in rare cases when high-quality biliary repair is difficult or even impossible, such as when segmental bile ducts are either constricted as a result of persistent cholangitis or are unsuitable for anastomosis.9,17,20 As alternative approaches, side-to-side hepaticojejunostomy on separated right and left ducts,46 or partial resection of segments IV and V to enable adequate exposure of the left and right ducts,47 have been proposed.
Finally, indications for urgent hepatectomy may be questionable except in cases of concomitant portal vein and arterial injuries. When arterial injury is the only criterion of gravity, its hypothetical role as a factor for urgent hepatectomy should be subject to caution.48 Indeed, a delayed repair can improve local and general conditions for potentially difficult hepaticojejunostomy, given the rapid development of collateral circulation within the hilar plate10 and spontaneous improvement in hepatic infarction and abscesses in most patients.49 By contrast, a delayed repair may allow for the accurate assessment of the risk for progression of injury over several months,2 which may lead, in turn, to the decision to perform hepatectomy rather than a risky hepaticojejunostomy when duct ischaemia persists. One argument supporting this policy in the current study was the high mortality rate (4/9 patients) in patients undergoing urgent hepatectomy (within 2 weeks), which is far greater than the current near-zero mortality of cancer patients undergoing hepatectomy.50
Conclusions
In conclusion, indications for hepatectomy in the management of BDI are rare, given the high success rate of biliary repair, but have increased since 2000, possibly reflecting increases in the complexity of BDIs. This analysis of the literature suggests that hepatectomy has been required mainly in cases of concomitant vascular and proximal biliary injury. Indeed, performing hepatectomy could provide better results and longterm outcomes than repeat hepaticojejunostomy in extensive ischaemic and fibrotic biliary lesions. Mortality rates in hepatectomy seem to be comparable with those reported in the literature for hepaticojejunostomy. Except for concomitant portal vein and arterial injury, emergency hepatectomy should be avoided. Further comparative studies are needed to precisely determine the circumstances in which hepatectomy might be justified.
Conflict of interest
None declared.
References
- 1.Roslyn JJ, Binns GS, Hughes EF, Saunders-Kirkwood K, Zinner MJ, Cates JA. Open cholecystectomy. A contemporary analysis of 42 474 patients. Ann Surg. 1993;218:129–137. doi: 10.1097/00000658-199308000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–125. [PubMed] [Google Scholar]
- 3.Lillemoe KD, Melton GB, Cameron JL, Pitt HA, Campbell KA, Talamini MA, et al. Postoperative bile duct strictures: management and outcome in the 1990s. Ann Surg. 2000;232:430–441. doi: 10.1097/00000658-200009000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmidt SC, Langrehr JM, Hintze RE, Neuhaus P. Longterm results and risk factors influencing outcome of major bile duct injuries following cholecystectomy. Br J Surg. 2005;92:76–82. doi: 10.1002/bjs.4775. [DOI] [PubMed] [Google Scholar]
- 5.Vitale GC, Tran TC, Davis BR, Vitale M, Vitale D, Larson G. Endoscopic management of post-cholecystectomy bile duct strictures. J Am Coll Surg. 2008;206:918–923. doi: 10.1016/j.jamcollsurg.2008.01.064. discussion 924–925. [DOI] [PubMed] [Google Scholar]
- 6.de Reuver PR, Busch OR, Rauws EA, Lameris JS, van Gulik TM, Gouma DJ. Longterm results of a primary end-to-end anastomosis in perioperative detected bile duct injury. J Gastrointest Surg. 2007;11:296–302. doi: 10.1007/s11605-007-0087-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bismuth H, Majno PE. Biliary strictures: classification based on the principles of surgical treatment. World J Surg. 2001;25:1241–1244. doi: 10.1007/s00268-001-0102-8. [DOI] [PubMed] [Google Scholar]
- 8.Bismuth H. How to treat a postoperative stenosis? In: Bismuth H, Lazorthes F, editors. Operative Injury of the Common Bile Duct. Paris: Masson; 1981. pp. 47–107. [Google Scholar]
- 9.Mercado MA, Chan C, Orozco H, Villalta JM, Barajas-Olivas A, Erana J, et al. Longterm evaluation of biliary reconstruction after partial resection of segments IV and V in iatrogenic injuries. J Gastrointest Surg. 2006;10:77–82. doi: 10.1016/j.gassur.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 10.Alves A, Farges O, Nicolet J, Watrin T, Sauvanet A, Belghiti J. Incidence and consequence of an hepatic artery injury in patients with post-cholecystectomy bile duct strictures. Ann Surg. 2003;238:93–96. doi: 10.1097/01.sla.0000074983.39297.c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schmidt SC, Langrehr JM, Raakow R, Klupp J, Steinmuller T, Neuhaus P. Right hepatic lobectomy for recurrent cholangitis after combined bile duct and right hepatic artery injury during laparoscopic cholecystectomy: a report of two cases. Langenbecks Arch Surg. 2002;387:183–187. doi: 10.1007/s00423-002-0300-3. [DOI] [PubMed] [Google Scholar]
- 12.Schmidt SC, Settmacher U, Langrehr JM, Neuhaus P. Management and outcome of patients with combined bile duct and hepatic arterial injuries after laparoscopic cholecystectomy. Surgery. 2004;135:613–618. doi: 10.1016/j.surg.2003.11.018. [DOI] [PubMed] [Google Scholar]
- 13.Mercado MA, Chan C, Salgado-Nesme N, Lopez-Rosales F. Intrahepatic repair of bile duct injuries. A comparative study. J Gastrointest Surg. 2008;12:364–368. doi: 10.1007/s11605-007-0428-0. [DOI] [PubMed] [Google Scholar]
- 14.Laurent A, Sauvanet A, Farges O, Watrin T, Rivkine E, Belghiti J. Major hepatectomy for the treatment of complex bile duct injury. Ann Surg. 2008;248:77–83. doi: 10.1097/SLA.0b013e31817b65f2. [DOI] [PubMed] [Google Scholar]
- 15.Nishio H, Kamiya J, Nagino M, Uesaka K, Kanai M, Sano T, et al. Right hepatic lobectomy for bile duct injury associated with major vascular occlusion after laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg. 1999;6:427–430. doi: 10.1007/s005340050145. [DOI] [PubMed] [Google Scholar]
- 16.Branum G, Schmitt C, Baillie J, Suhocki P, Baker M, Davidoff A, et al. Management of major biliary complications after laparoscopic cholecystectomy. Ann Surg. 1993;217:532–540. doi: 10.1097/00000658-199305010-00014. discussion 540–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ota T, Hirai R, Tsukuda K, Murakami M, Naitou M, Shimizu N. Biliary reconstruction with right hepatic lobectomy due to delayed management of laparoscopic bile duct injuries: a case report. Acta Med Okayama. 2004;58:163–167. doi: 10.18926/AMO/32112. [DOI] [PubMed] [Google Scholar]
- 18.Majno PE, Pretre R, Mentha G, Morel P. Operative injury to the hepatic artery. Consequences of a biliary-enteric anastomosis and principles for rational management. Arch Surg. 1996;131:211–215. doi: 10.1001/archsurg.1996.01430140101025. [DOI] [PubMed] [Google Scholar]
- 19.Sekido H, Matsuo K, Morioka D, Kunihiro O, Tanaka K, Endo I, et al. Surgical strategy for the management of biliary injury in laparoscopic cholecystectomy. Hepatogastroenterology. 2004;51:357–361. [PubMed] [Google Scholar]
- 20.Ohtsuka T, Chijiiwa K, Yamaguchi K, Akashi Y, Matsunaga H, Miyoshi A. Posterior hepatic duct injury during laparoscopic cholecystectomy finally necessitating hepatic resection: case report. JSLS. 1999;3:323–326. [PMC free article] [PubMed] [Google Scholar]
- 21.Thomson BN, Parks RW, Madhavan KK, Garden OJ. Liver resection and transplantation in the management of iatrogenic biliary injury. World J Surg. 2007;31:2363–2369. doi: 10.1007/s00268-007-9234-9. [DOI] [PubMed] [Google Scholar]
- 22.Gazzaniga GM, Filauro M, Mori L. Surgical treatment of iatrogenic lesions of the proximal common bile duct. World J Surg. 2001;25:1254–1259. doi: 10.1007/s00268-001-0105-5. [DOI] [PubMed] [Google Scholar]
- 23.Uenishi T, Hirohashi K, Tanaka H, Fujio N, Kubo S, Kinoshita H. Right hepatic lobectomy for recurrent cholangitis after bile duct and hepatic artery injury during laparoscopic cholecystectomy: report of a case. Hepatogastroenterology. 1999;46:2296–2298. [PubMed] [Google Scholar]
- 24.Topal B, Aerts R, Penninckx F. The outcome of major biliary tract injury with leakage in laparoscopic cholecystectomy. Surg Endosc. 1999;13:53–56. doi: 10.1007/s004649900897. [DOI] [PubMed] [Google Scholar]
- 25.Vibert E, Farges O, Regimbeau JM, Belghiti J. Benign hilar biliary strictures stented with metallic stents can be resected by using an oncologic approach. Surgery. 2005;137:506–510. doi: 10.1016/j.surg.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 26.Frilling A, Li J, Weber F, Fruhauf NR, Engel J, Beckebaum S, et al. Major bile duct injuries after laparoscopic cholecystectomy: a tertiary centre experience. J Gastrointest Surg. 2004;8:679–685. doi: 10.1016/j.gassur.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 27.de Santibanes E, Palavecino M, Ardiles V, Pekolj J. Bile duct injuries: management of late complications. Surg Endosc. 2006;20:1648–1653. doi: 10.1007/s00464-006-0491-8. [DOI] [PubMed] [Google Scholar]
- 28.Bektas H, Schrem H, Winny M, Klempnauer J. Surgical treatment and outcome of iatrogenic bile duct lesions after cholecystectomy and the impact of different clinical classification systems. Br J Surg. 2007;94:1119–1127. doi: 10.1002/bjs.5752. [DOI] [PubMed] [Google Scholar]
- 29.Sauvanet A, Watrin T, Nicolet J, Sa Cunha A, Farges O, Belghiti J. Major hepatectomy for bile duct injuries after cholecystectomy. IHPBA. 2000;2:171–172. [Google Scholar]
- 30.Truant SC, Boleslawski E, Sergent G, Gambiez L, Pruvot FR. Predictive factors of hepatectomy in the management of post-cholecystectomy biliary injury. HPB. 2009;11(Suppl 2):68–69. [Google Scholar]
- 31.Ortega-Deballon P, Cheynel N, Benoit L, Di Giacomo G, Favre JP, Rat P. [Iatrogenic biliary injuries during cholecystectomy.] J Chir (Paris) 2007;144:409–413. doi: 10.1016/s0021-7697(07)73996-0. [DOI] [PubMed] [Google Scholar]
- 32.Buell JF, Cronin DC, Funaki B, Koffron A, Yoshida A, Lo A, et al. Devastating and fatal complications associated with combined vascular and bile duct injuries during cholecystectomy. Arch Surg. 2002;137:703–708. doi: 10.1001/archsurg.137.6.703. discussion 708–710. [DOI] [PubMed] [Google Scholar]
- 33.Lichtenstein S, Moorman DW, Malatesta JQ, Martin MF. The role of hepatic resection in the management of bile duct injuries following laparoscopic cholecystectomy. Am Surg. 2000;66:372–376. discussion 377. [PubMed] [Google Scholar]
- 34.Madariaga JR, Dodson SF, Selby R, Todo S, Iwatsuki S, Starzl TE. Corrective treatment and anatomic considerations for laparoscopic cholecystectomy injuries. J Am Coll Surg. 1994;179:321–325. [PMC free article] [PubMed] [Google Scholar]
- 35.Yan JQ, Peng CH, Ding JZ, Yang WP, Zhou GW, Chen YJ, et al. Surgical management in biliary restricture after Roux-en-Y hepaticojejunostomy for bile duct injury. World J Gastroenterol. 2007;13:6598–6602. doi: 10.3748/wjg.v13.i48.6598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chapman WC, Halevy A, Blumgart LH, Benjamin IS. Post-cholecystectomy bile duct strictures. Management and outcome in 130 patients. Arch Surg. 1995;130:597–602. doi: 10.1001/archsurg.1995.01430060035007. discussion 602–604. [DOI] [PubMed] [Google Scholar]
- 37.Bilge O, Bozkiran S, Ozden I, Tekant Y, Acarli K, Alper A, et al. The effect of concomitant vascular disruption in patients with iatrogenic biliary injuries. Langenbecks Arch Surg. 2003;388:265–269. doi: 10.1007/s00423-003-0382-6. [DOI] [PubMed] [Google Scholar]
- 38.Walsh RM, Henderson JM, Vogt DP, Brown N. Longterm outcome of biliary reconstruction for bile duct injuries from laparoscopic cholecystectomies. Surgery. 2007;142:450–456. doi: 10.1016/j.surg.2007.07.008. discussion 456–457. [DOI] [PubMed] [Google Scholar]
- 39.Sicklick JK, Camp MS, Lillemoe KD, Melton GB, Yeo CJ, Campbell KA, et al. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg. 2005;241:786–792. doi: 10.1097/01.sla.0000161029.27410.71. discussion 793–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mercado MA. [From Langenbuch to Strasberg: the spectrum of bile duct injuries.] Rev Invest Clin. 2004;56:649–664. [PubMed] [Google Scholar]
- 41.Stewart L, Way LW. Bile duct injuries during laparoscopic cholecystectomy. Factors that influence the results of treatment. Arch Surg. 1995;130:1123–1128. doi: 10.1001/archsurg.1995.01430100101019. discussion 1129. [DOI] [PubMed] [Google Scholar]
- 42.Heise M, Schmidt SC, Adler A, Hintze RE, Langrehr JM, Neuhaus P. [Management of bile duct injuries following laparoscopic cholecystectomy.] Zentralbl Chir. 2003;128:944–951. doi: 10.1055/s-2003-44802. [DOI] [PubMed] [Google Scholar]
- 43.Stewart L, Robinson TN, Lee CM, Liu K, Whang K, Way LW. Right hepatic artery injury associated with laparoscopic bile duct injury: incidence, mechanism, and consequences. J Gastrointest Surg. 2004;8:523–530. doi: 10.1016/j.gassur.2004.02.010. discussion 530–531. [DOI] [PubMed] [Google Scholar]
- 44.de Reuver PR, Grossmann I, Busch OR, Obertop H, van Gulik TM, Gouma DJ. Referral pattern and timing of repair are risk factors for complications after reconstructive surgery for bile duct injury. Ann Surg. 2007;245:763–770. doi: 10.1097/01.sla.0000252442.91839.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hepp J, Couinaud C. L'abord et l'utilisation du canal hépatique gauche dans les réparations de la voie biliaire principale. Presse Med. 1956:947–948. [PubMed] [Google Scholar]
- 46.Winslow ER, Fialkowski EA, Linehan DC, Hawkins WG, Picus DD, Strasberg SM. ‘Sideways’: results of repair of biliary injuries using a policy of side-to-side hepatico-jejunostomy. Ann Surg. 2009;249:426–434. doi: 10.1097/SLA.0b013e31819a6b2e. [DOI] [PubMed] [Google Scholar]
- 47.Strasberg SM, Picus DD, Drebin JA. Results of a new strategy for reconstruction of biliary injuries having an isolated right-sided component. J Gastrointest Surg. 2001;5:266–274. doi: 10.1016/s1091-255x(01)80047-0. [DOI] [PubMed] [Google Scholar]
- 48.Kayaalp C, Nessar G, Kaman S, Akoglu M. Right liver necrosis: complication of laparoscopic cholecystectomy. Hepatogastroenterology. 2001;48:1727–1729. [PubMed] [Google Scholar]
- 49.Holbert BL, Baron RL, Dodd GD., III. Hepatic infarction caused by arterial insufficiency: spectrum and evolution of CT findings. AJR Am J Roentgenol. 1996;166:815–820. doi: 10.2214/ajr.166.4.8610556. [DOI] [PubMed] [Google Scholar]
- 50.Imamura H, Seyama Y, Kokudo N, Maema A, Sugawara Y, Sano K, et al. One thousand fifty-six hepatectomies without mortality in 8 years. Arch Surg. 2003;138:1198–1206. doi: 10.1001/archsurg.138.11.1198. discussion 1206. [DOI] [PubMed] [Google Scholar]
- 51.Nishiguchi S, Shiomi S, Sasaki N, Iwata Y, Tanaka H, Kubo S, et al. A case of recurrent cholangitis after bile duct injury during laparoscopic cholecystectomy: value of scintigraphy with Tc-99m GSA and hepatobiliary scintigraphy for indication of lobectomy. Ann Nucl Med. 2000;14:383–386. doi: 10.1007/BF02988702. [DOI] [PubMed] [Google Scholar]
- 52.Wong MD, Lucas CE. Liver infarction after laparoscopic cholecystectomy injury to the right hepatic artery and portal vein. Am Surg. 2001;67:410–411. [PubMed] [Google Scholar]
- 53.Heinrich S, Seifert H, Krahenbuhl L, Fellbaum C, Lorenz M. Right hemihepatectomy for bile duct injury following laparoscopic cholecystectomy. Surg Endosc. 2003;17:1494–1495. doi: 10.1007/s00464-002-4278-2. [DOI] [PubMed] [Google Scholar]
- 54.Felekouras E, Megas T, Michail OP, Papaconstantinou I, Nikiteas N, Dimitroulis D, et al. Emergency liver resection for combined biliary and vascular injury following laparoscopic cholecystectomy: case report and review of the literature. South Med J. 2007;100:317–320. doi: 10.1097/01.smj.0000242793.15923.1a. [DOI] [PubMed] [Google Scholar]
- 55.Wu JS, Peng C, Mao XH, Lv P. Bile duct injuries associated with laparoscopic and open cholecystectomy: sixteen-year experience. World J Gastroenterol. 2007;13:2374–2378. doi: 10.3748/wjg.v13.i16.2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li J, Frilling A, Nadalin S, Paul A, Malago M, Broelsch CE. Management of concomitant hepatic artery injury in patients with iatrogenic major bile duct injury after laparoscopic cholecystectomy. Br J Surg. 2008;95:460–465. doi: 10.1002/bjs.6022. [DOI] [PubMed] [Google Scholar]
- 57.Ragozzino A, Lassandro F, De Ritis R, Imbriaco M. Value of MRI in three patients with major vascular injuries after laparoscopic cholecystectomy. Emerg Radiol. 2007;14:443–447. doi: 10.1007/s10140-007-0617-x. [DOI] [PubMed] [Google Scholar]
- 58.Nuzzo G, Giuliante F, Giovannini I, Murazio M, D'Acapito F, Ardito F, et al. Advantages of multidisciplinary management of bile duct injuries occurring during cholecystectomy. Am J Surg. 2008;195:763–769. doi: 10.1016/j.amjsurg.2007.05.046. [DOI] [PubMed] [Google Scholar]


