Abstract
Objectives. I examined the association between income inequality and population health and tested whether this association was mediated by interpersonal trust or public expenditures on health.
Methods. Individual data on trust were collected from 48 641 adults in 33 countries. These data were linked to country data on income inequality, public health expenditures, healthy life expectancy, and adult mortality. Regression analyses tested for statistical mediation of the association between income inequality and population health outcomes by country differences in trust and health expenditures.
Results. Income inequality correlated with country differences in trust (r = −0.51), health expenditures (r = −0.45), life expectancy (r = −0.74), and mortality (r = 0.55). Trust correlated with life expectancy (r = 0.48) and mortality (r = −0.47) and partly mediated their relations to income inequality. Health expenditures did not correlate with life expectancy and mortality, and health expenditures did not mediate links between inequality and health.
Conclusions. Income inequality might contribute to short life expectancy and adult mortality in part because of societal differences in trust. Societies with low levels of trust may lack the capacity to create the kind of social supports and connections that promote health and successful aging.
Social inequalities in health are closely aligned with individual differences in income. At every level of socioeconomic status, health tends to be better on the level above and poorer on the level below, even among those who are not poor and enjoy equal access to health services.1,2 Research also shows that health problems that are associated with socioeconomic status are more common in societies that have wider distributions of personal income.3 It is well-documented that international differences in income inequality (i.e., size of the gap between rich and poor) are associated with rates of mortality4 and with various mental and physical health problems.5–8
Opinions are divided regarding the contextual mechanisms that might account for the association between income inequality and health. One line of research focuses on the psychosocial impact of inequality and the breakdown of “social capital,” which is defined as features of social organization—such as networks, norms, and interpersonal trust—that facilitate coordination and cooperation for mutual benefit.2,9 Wilkinson, Kawachi, and others have suggested that large income differences intensify social hierarchies and increase class conflict and feelings of relative deprivation while simultaneously reducing levels of interpersonal trust, social cohesion, and other dimensions of social capital that promote health.3,10–12 The alternative “neomaterialist” hypothesis suggests that income inequality inhibits public expenditures on important services and infrastructure that promote health.13–17 In the United States, for instance, state expenditures on public health and education negatively correlate with income inequality and adult mortality.13,16 It remains undetermined whether international differences in public expenditures account for the association between income inequality and health.
The neomaterialist and social capital hypotheses are not mutually exclusive. Kawachi and Kennedy observed that US state populations with low levels of trust are also characterized by values that support a minimal role for government in reducing health inequalities.18 Putnam's index of health and health care in the United States (which included expenditures on health care) was highly correlated with an index of social capital.9 Therefore, it could be the case that more equal, more trusting societies are also more willing to support government spending on goods and services that advance the common good, compared with less equal, less trusting societies.
It is important to understand which factors account for the association between income inequality and population health. A piecemeal evidence base shows inconsistent findings for mediation by psychosocial and neomaterial paths. Inconsistencies among studies with regard to sample selection criteria, tests of mediated effects, and measures of income inequality have made it difficult to weigh the evidence in favor of either hypothesis.11,19–21 As a result, previous claims that the relationship between income inequality and poor health is mediated by trust, social capital, or public expenditures22—or that the relation is simply a statistical artifact caused by confounding effects of individual income,23 race,24 or education25—have not all been based on rigorous tests of statistical mediation.
One issue in particular muddies the water when testing mediated effects: small changes in a regression slope or correlation coefficient that occur when a third variable is controlled can easily cause the statistic to change from significance (P < .05) to nonsignificance (P > .05), even when the third variable does not account for a significant proportion of shared variance. Negligible change from significance to nonsignificance does not, in itself, establish mediation.26 Kawachi et al. addressed this issue by using path analysis to show significant mediated effects of income inequality (via social capital) on mortality11 and births to adolescents.20 However, these studies did not include similar mediation analyses of public expenditures.
There has not been a direct comparison of psychosocial and neomaterial paths in accounting for the association between income inequality and health. Therefore, my aim in the current study was to test the association between income inequality and 2 indicators of population health—healthy life expectancy and adult mortality—and then test how much this association was mediated by differences in a proxy indicator of social capital (interpersonal trust) and by public expenditures on health. Of course, trust is just a single aspect of social capital that could mediate links between inequality and health, and expenditures on services other than health might also relate to health. But by using a consistent set of data on income inequality and population health, I explored whether their association (if significant) was better explained by a psychosocial path or a neomaterial path. In disadvantaged populations, healthy life expectancy (also referred to as “disability-free life expectancy”) represents the burden of ill health better than total life expectancy does, according to the World Health Organization,27 so I used healthy life expectancy as an indicator of population health. Adult mortality was used as a general indicator of population health.
METHODS
The International Social Survey Program (ISSP) surveyed 48 641 adults from a group of 33 rich and middle-income countries from 2005 through 2008. These 33 countries provided the sample for this study: Australia, Canada, Chile, Croatia, Czech Republic, Denmark, Dominican Republic, Finland, France, Germany, Hungary, Ireland, Israel, Japan, Latvia, the Netherlands, New Zealand, Norway, the Philippines, Poland, Portugal, Russian Federation, Slovenia, South Africa, South Korea, Spain, Sweden, Switzerland, Taiwan, United Kingdom, United States, Uruguay, and Venezuela. The ISSP had no selection criteria per se for choosing countries to participate; researchers from each country elected to participate in the survey network and agreed to a common protocol for sample selection, interview methods, and survey measures. The number of survey respondents per country ranged from 910 (Canada) to 2939 (South Africa) (mean = 1471.8; SD = 542.9).
The sample was 53.5% female and ranged in age from 15 to 98 years (mean = 46.8; SD = 17.4). Surveys were administered either by mail or by telephone. Participants provided information about their age, gender, education (6-point scale ranging from 0 [no formal education] to 5 [university degree completed]; mean = 2.7; SD = 1.6), and social status (“In our society today there are groups which tend to be towards the top and groups which tend to be towards the bottom. Where would you put yourself on this scale?” Responses ranged from 1 [lowest] to 10 [highest]; mean = 5.0; SD = 1.8). Participants also indicated their level of agreement with the statement “There are only a few people I can trust completely” on a 5-point scale ranging from 1 (strongly agree) to 5 (strongly disagree; mean = 3.9; SD = 1.1). Samples were stratified and data weights were applied to best represent the adult population of each country. (Details about ISSP survey procedures are available online at www.issp.org.)
The World Health Organization Statistical Information System (http://www.who.int/whosis) provided data about these 33 countries in the following areas: total government expenditures on health in 2006 as a percentage of gross domestic product, healthy life expectancy at birth (estimated number of years a person can expect to live without disease or injury), and adult mortality (probability of death from ages 15 through 60 years per 1000 population). The World Health Organization calculated healthy life expectancy by using the Sullivan method, which uses mortality rates and age distribution in each country to estimate the number of years an individual is expected to live in a healthy state.28 Adult mortality was based on life tables and census information. Health expenditures ranged from 1.4% (the Philippines) to 8.2% (France) of gross domestic product (mean = 5.6%; SD = 2.1%). Healthy life expectancy ranged from 44 (South Africa) to 75 (Japan) years (mean = 68.0; SD = 6.2). Adult mortality ranged from 0.063 (Switzerland) to 0.564 (South Africa; mean = 0.129; SD = 0.090).
The World Bank World Development Indicators database provided data on per capita income and income inequality.29 Per capita income was estimated using gross national income per capita at 2007 purchasing parities in US dollars. I measured income inequality using the Gini index, which ranges from 0 (perfect equality, where all persons have equal income) to 1 (perfect inequality, where 1 person has all the income and the rest have none). The Gini index was calculated using data from nationally representative surveys and was adjusted for household size, and was based on consumption rather than income wherever possible.29 Per capita income ranged from $3710 (the Philippines) to $53 650 (Norway; mean = $29 777; SD = $14 033). The Gini index ranged from 0.247 (Denmark) to 0.578 (South Africa; mean = 0.363; SD = 0.769).
Per capita income shared logarithmic relations with healthy life expectancy and adult mortality (e.g., each 10-fold increase in income corresponded to 14.1 additional years of life expectancy; R2 = 0.56). Therefore, I applied log-transformed per capita income to partial correlations and linear regression models to control for country differences in average per capita income. Continuous variables were centered and scaled (mean = 0; SD = 1) to facilitate comparison of regression coefficients (B).
Because the potential for ecological fallacies was an issue that troubled previous studies on income inequality, I carried out a multilevel analysis of trust using MLwiN software, version 2.02 (Centre for Multilevel Modeling, University of Bristol, UK). These analyses tested whether the country-level associations between income inequality and trust were attributable to ISSP sample characteristics. Previous research has found that trust tended to be higher among women than among men; trust also was higher among those who were older and more educated, and among those who had higher social status.30 A 2-level linear model with variances specified at the individual level (i) and country level (j) was tested (Trustij = B0ij + B1Genderij + B2Ageij + B3Educationij + B4SocialStatusij + B5PerCapitaIncomej + B6IncomeInequalityj).
Multilevel analysis is generally preferred when testing cross-level associations, but it does not permit country-level outcome variables (j), such as healthy life expectancy and adult mortality, to be estimated by individual-level predictors (i). Therefore, tests of mediation were based on associations at the country level. Data on trust were aggregated to country averages and then tested as mediating variables along with health expenditures. Linear regression analyses tested Baron and Kenny's 4 criteria of mediation: (1) income inequality correlates with the mediator (either trust or health expenditures; path a), (2) the mediator correlates with the outcome (either healthy life expectancy or adult mortality; path b), (3) income inequality correlates with the outcome (path c), and (4) the unique relation between income inequality and the outcome is attenuated when the mediator is included in the model (path c’).26 That is, the difference between paths c and c’ had to be statistically significant to establish mediation. I calculated these differences using the Sobel test and reported them as a z score,
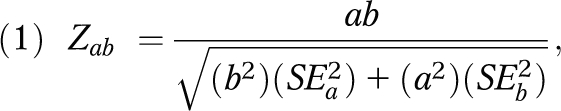 |
where a and b were the regression coefficients associated with paths a and b, respectively, and SE was the standard error associated with these coefficients. All paths accounted for any shared variance with per capita income. When aggregating data on trust to the country level, I used sampling weights from the ISSP survey. Poststratification data weights based on country population were applied so that the results would best represent the total survey population of 1.29 billion.21
RESULTS
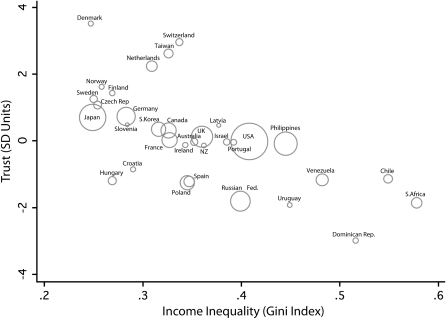
Partial correlations (controlling for per capita income) showed that income inequality negatively correlated with interpersonal trust, health expenditures, and life expectancy, and positively correlated with adult mortality (Table 1). Healthy life expectancy correlated with interpersonal trust and was marginally correlated (P = .06) with health expenditures. Adult mortality negatively correlated with trust but not with health expenditures. In none of these associations did an outlier affect the strength of the correlation. Figure 1 shows the correlation between income inequality and trust.
TABLE 1.
Correlations Among Income Inequality, Trust, Public Health Expenditures, and Population Health: 33 Countries, 2005–2008
| Income Inequality | Trust | Public Health Expenditures | Healthy Life Expectancy | Adult Mortality | |
| Income inequality | NA | ||||
| Trust | –0.51** | NA | |||
| Public health expenditures | –0.45* | 0.12 | NA | ||
| Healthy life expectancy | –0.74** | 0.48** | 0.34 | NA | |
| Adult mortality | 0.55** | –0.47** | –0.13 | –0.92 | NA |
Note. Partial correlations shown, with control for country differences in per capita income. The 33 countries that provided the sample population are Australia, Canada, Chile, Croatia, Czech Republic, Denmark, Dominican Republic, Finland, France, Germany, Hungary, Ireland, Israel, Japan, Latvia, the Netherlands, New Zealand, Norway, the Philippines, Poland, Portugal, Russian Federation, Slovenia, South Africa, South Korea, Spain, Sweden, Switzerland, Taiwan, United Kingdom, United States, Uruguay, and Venezuela.
*P < .05; **P < .01.
FIGURE 1.
Income inequality and interpersonal trust: 33 countries, 2005–2008.
Note. Circles illustrate weighting by country population.
Multilevel analysis verified that the association between country-level income inequality and individual-level trust was significant after sample characteristics were taken into account (Table 2). In a base model with no predictors (model 1), the intraclass coefficient of trust was 0.09, indicating large variation at the individual level. Model 2 reveals the source of some of these individual differences. Trust related to older age, female gender, higher education, and higher social status. With these individual differences and per capita income taken into account, income inequality still related to less trust (B = −0.12; P < .01; model 3).
TABLE 2.
Multilevel Regression Analysis of Associations Between Country-Level Income Inequality and Individual-Level Trust: 33 Countries, 2005–2008
| Variable | Model 1, B (SE) | Model 2, B (SE) | Model 3, B (SE) |
| Constant | 0.07** (0.06) | 0.01 (0.06) | 0.00 (0.06) |
| Individual characteristics (n = 48 641) | |||
| Age | 0.07** (0.02) | 0.07** (0.02) | |
| Gender (female) | 0.06** (0.02) | 0.06** (0.02) | |
| Education | 0.11** (0.03) | 0.11** (0.03) | |
| Social status | 0.06** (0.02) | 0.06** (0.06) | |
| Country characteristics (n = 33) | |||
| Per capita income | 0.08** (0.07) | ||
| Income inequality | –0.12** (0.05) | ||
| Level 1 variance | 0.96 (0.27) | 0.94 (0.26) | 0.94 (0.26) |
| Level 2 variance | 0.10 (0.02) | 0.08 (0.02) | 0.05 (0.01) |
| Model statistics | |||
| Intraclass coefficient | 0.09 | 0.08 | 0.05 |
| –2 log-likelihood | 174 463.20 | 173 568.20 | 173 551.40 |
Note. The 33 countries that provided the sample population are Australia, Canada, Chile, Croatia, Czech Republic, Denmark, Dominican Republic, Finland, France, Germany, Hungary, Ireland, Israel, Japan, Latvia, the Netherlands, New Zealand, Norway, the Philippines, Poland, Portugal, Russian Federation, Slovenia, South Africa, South Korea, Spain, Sweden, Switzerland, Taiwan, United Kingdom, United States, Uruguay, and Venezuela.
**P < 0.01.
Table 3 shows the regression analysis of healthy life expectancy and adult mortality including tests of mediation by trust and health expenditures. Income inequality related to trust and health expenditures (both relations are path a). Trust related to life expectancy and adult mortality (both relations are path b); each standard-deviation increase in trust corresponded to 2.3 additional years of life expectancy and 3.7% lower probability of adult death. Health expenditures did not relate to life expectancy and mortality and were therefore ruled out as a potential mediator. Income inequality also related to healthy life expectancy and adult mortality (both relations are path c); each standard-deviation increase in income inequality corresponded with 3.4 fewer years of life expectancy and 4.1% greater probability of adult death. Trust partly mediated the association between income inequality and healthy life expectancy (Sobel Zab = −2.71; P < .01) and between income inequality and adult mortality (Sobel Zab = −2.20; P < .01). However, these associations were not completely mediated by trust because income inequality still predicted both outcomes after differences in trust were controlled (paths c’). Variance inflation factors in these models were low (1.1–3.7), indicating that collinearity between variables did not bias the results.31
TABLE 3.
Analysis of Trust and Public Health Expenditures as Mediators Between Income Inequality and Population Health: 33 Countries, 2005–2008
| Mediating Variable: Trust |
Mediating Variable: Public Health Expenditures |
|||
| Path | B (SE) | t | B (SE) | t |
| Healthy life expectancy | ||||
| a | −0.48 (0.15) | 3.22** | −0.25 (0.09) | 2.73* |
| b | 0.38 (0.13) | 2.98** | 0.46 (0.23) | 1.96 |
| c | −0.56 (0.11) | 6.05** | −0.56 (0.11) | 6.05** |
| c’ | −0.51 (0.11) | 4.72** | −0.56 (0.11) | 5.29** |
| Sobel Zab | –2.71** | –1.62 | ||
| Adult mortality | ||||
| a | −0.48 (0.15) | 3.22** | −0.25 (0.09) | 2.73* |
| b | −0.41 (0.14) | 2.91** | −0.19 (0.27) | –0.70 |
| c | 0.46 (0.13) | 3.57** | 0.46 (0.13) | 3.57** |
| c’ | 0.35 (0.15) | 2.39* | 0.51 (0.14) | 3.56** |
| Sobel Zab | 2.20** | 0.68 | ||
Note. Path a runs between income inequality and the mediator (X→M). Path b runs between the mediator and the dependent variable (M→Y). Path c is the unmediated path between income inequality and the dependent variable (X→Y). Path c’ is the mediated path between income inequality and the dependent variable (X→M→Y). All models were adjusted for country differences in per capita income. The 33 countries that provided the sample population are Australia, Canada, Chile, Croatia, Czech Republic, Denmark, Dominican Republic, Finland, France, Germany, Hungary, Ireland, Israel, Japan, Latvia, the Netherlands, New Zealand, Norway, the Philippines, Poland, Portugal, Russian Federation, Slovenia, South Africa, South Korea, Spain, Sweden, Switzerland, Taiwan, United Kingdom, United States, Uruguay, and Venezuela.
*P < .05; **P < .01.
DISCUSSION
Understanding how international differences in population health are affected by socioeconomic conditions is important to public health policy.2 This study found that income inequality related to population health in a sample of 33 middle- and high-income countries.3,18 Previous research intuited the mediation of links between income inequality and health by psychosocial and neomaterial paths, but few studies actually tested that mediation. This study tested 2 hypotheses regarding the association between income inequality and population health. I found that interpersonal trust partially mediated the association. No mediation was found involving public health expenditures.
Strengths of the study include a multilevel analysis of the association between income inequality and trust, which helped reduce the risk of ecological fallacies.23 Another strength was the diverse group of countries included in the analyses. Most previous ecological studies of income inequality used data from select groups of rich countries and disregarded income differences on the basis that average per capita income is unrelated to health among rich countries.3 However, as Lynch et al. demonstrated, average per capita income correlates with life expectancy within groups of high-income countries and should be controlled when exploring additional effects of income inequality.21 I found that links between income inequality and population health were highly significant after differences in per capita income were controlled. In short, the more egalitarian countries had better health.
Limitations of the study should also be noted. First, the cross-sectional design prevented conclusions about causal paths (i.e., from inequality to low trust to poor health). Longitudinal and time-series studies would better expose how inequality, trust, and public expenditures relate over time, and whether trust is an antecedent or consequence of income inequality, public expenditures, or other dimensions of social capital. For instance, Putnam and Uslaner both documented downward trends in social trust in the United States from the 1950s to the 1990s and this trend's relation to decreasing community involvement and increasing income inequality.9,30 Second, an ecological analysis of healthy life expectancy does not address the determinants of individual health. Conclusions drawn from these results pertain to healthy societies, not healthy individuals. Multilevel models of individual health can better control for potential confounding variables at the individual level and shed light on how differences in income, gender, education, and race/ethnicity interact in their contributions to health and illness.22
These findings are consistent with the notion that income inequality harms public health through the psychosocial impact of relative deprivation, class conflict, or the lack of social capital,3,18 and not primarily through the lack of government investment.15 Previous research showed that health gradients related to socioeconomic status and links between income inequality and health are partially attributable to the negative impact of inequality on social resources that support health.1–3 As social class differences widen, class conflict, hostility, violence, and psychological stress increase, whereas moderators of stress (e.g., social support and cohesion) decrease.7,18 Further research is needed involving more data on psychosocial environments and public and private investments in health, education, and other public goods to better explain why income inequality correlates with stress-related disease and mortality.
This study is certainly not the last word on the “psychosocial versus neomaterialist” debate in income inequality research. In fact, interpersonal trust might be neither the most evident signature of equal societies nor the most powerful determinant of population health, but interpersonal trust does appear to carry an association from income inequality to health. These findings suggest that societies with large income differences and low levels of trust may lack the capacity to create the kind of social supports and connections that promote health and successful aging.
Acknowledgments
This research was funded in part by the Canadian Institutes of Health Research and the Social Sciences and Humanities Research Council of Canada.
The author thanks Richard Wilkinson, Kate Pickett, and Christopher G. Davis for their helpful suggestions on an earlier draft of this article.
Human Participant Protection
No protocol approval was needed because data were obtained from secondary sources.
References
- 1.Adler NE, Boyce T, Chesney MA, et al. Socioeconomic status and health: the challenge of the gradient. Am Psychol. 1994;49(1):15–24 [DOI] [PubMed] [Google Scholar]
- 2.Marmot MG. Status Syndrome: How Your Social Standing Directly Affects Your Health and Life Expectancy. London, England: Bloomsbury; 2004 [Google Scholar]
- 3.Wilkinson RG, Pickett K. The Spirit Level: Why More Equal Societies Almost Always Do Better. London, England: Allen Lane; 2009 [Google Scholar]
- 4.Wilkinson RG. Income distribution and life expectancy. BMJ. 1992;304(6820):165–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Babones SJ. Income inequality and population health: correlation and causality. Soc Sci Med. 2008;66(7):1614–1626 [DOI] [PubMed] [Google Scholar]
- 6.Ross NA, Wolfson MC, Dunn JR, Berthelot JM, Kaplan GA, Lynch JW. Relation between income inequality and mortality in Canada and in the United States: cross sectional assessment using census data and vital statistics. BMJ. 2000;320(7239):898–902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kondo N, Sembajwe G, Kawachi I, van Dam RM, Subramanian SV, Yamagata Z. Income inequality, mortality, and self rated health: meta-analysis of multilevel studies. BMJ. 2009;339:b4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilkinson RG, Pickett KE. Income inequality and population health: a review and explanation of the evidence. Soc Sci Med. 2006;62(7):1768–1784 [DOI] [PubMed] [Google Scholar]
- 9.Putnam RD. Bowling Alone: The Collapse and Revival of American Community. New York, NY: Simon and Schuster; 2000 [Google Scholar]
- 10.Kawachi I, Kennedy BP. Health and social cohesion: Why care about income inequality? BMJ. 1997;314(7086):1037–1040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87(9):1491–1498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marmot MG, Wilkinson RG, Social Determinants of Health. 2nd ed New York, NY: Oxford University Press; 2006 [Google Scholar]
- 13.Dunn JR, Burgess B, Ross NA. Income distribution, public services expenditures, and all cause mortality in US States. J Epidemiol Community Health. 2005;59(9):768–774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kawachi I, Kennedy BP. Income inequality and health: pathways and mechanisms. Health Serv Res. 1999;34(1, pt 2):215–227 [PMC free article] [PubMed] [Google Scholar]
- 15.Lynch JW, Smith GD, Kaplan GA, House JS. Income inequality and mortality: importance to health of individual income, psychosocial environment, or material conditions. BMJ. 2000;320(7243):1200–1204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ronzio CR, Pamuk E, Squires GD. The politics of preventable deaths: local spending, income inequality, and premature mortality in US cities. J Epidemiol Community Health. 2004;58(3):175–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwabish J, Smeeding TM, Osberg L. Income Distribution and Social Expenditures: A Cross-National Perspective. Syracuse, NY: Syracuse University Maxwell School of Citizenship and Public Affairs; 2004 [Google Scholar]
- 18.Kawachi I, Kennedy BP. The Health of Nations: Why Inequality Is Harmful to Your Health. New York, NY: New Press; 2002 [Google Scholar]
- 19.Beckfield J. Does income inequality harm health? New cross-national evidence. J Health Soc Behav. 2004;45(3):231–248 [DOI] [PubMed] [Google Scholar]
- 20.Gold R, Kennedy B, Connell F, Kawachi I. Teen births, income inequality, and social capital: developing an understanding of the causal pathway. Health Place. 2002;8(2):77–83 [DOI] [PubMed] [Google Scholar]
- 21.Lynch J, Smith GD, Hillemeier M, Shaw M, Raghunathan T, Kaplan G. Income inequality, the psychosocial environment, and health: comparisons of wealthy nations. Lancet. 2001;358(9277):194–200 [DOI] [PubMed] [Google Scholar]
- 22.Kawachi I. Income inequality and health. : Berkman LF, Kawachi I, Social Epidemiology. New York, NY: Oxford University Press; 2000:76–94 [Google Scholar]
- 23.Gravelle H. How much of the relation between population mortality and unequal distribution of income is a statistical artefact? BMJ. 1998;316(7128):382–385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deaton A, Lubotsky D. Mortality, inequality and race in American cities and states. Soc Sci Med. 2003;56(6):1139–1153 [DOI] [PubMed] [Google Scholar]
- 25.Messias E. Income inequality, illiteracy rate, and life expectancy in Brazil. Am J Public Health. 2003;93(8):1294–1296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182 [DOI] [PubMed] [Google Scholar]
- 27.Mathers CD, Murray CJ, Lopez AD, Sadana R, Salomon JA. Global patterns of healthy life expectancy for older women. J Women Aging. 2002;14(1–2):99–117 [DOI] [PubMed] [Google Scholar]
- 28.Jagger C, Cox B, Le Roy S, the EHEMU team Health Expectancy Calculation by the Sullivan Method: A Practical Guide. 3rd ed.Montpellier, France: European Health Expectancy Monitoring Unit; 2006 [Google Scholar]
- 29.World Bank World Development Indicators. Available at: http://data.worldbank.org. Accessed February 14, 2010
- 30.Uslaner EM. The Moral Foundations of Trust. Cambridge, England: Cambridge University Press; 2002 [Google Scholar]
- 31.Kutner MH. Applied Linear Statistical Models. 5th ed.Boston, MA: McGraw-Hill Irwin; 2005 [Google Scholar]