Abstract
Objectives. We compared the quality of care received by managed care Medicaid beneficiaries in counties with a choice of health plans and counties with no choice.
Methods. This cross-sectional study among California Medicaid beneficiaries was conducted during 2002. We used a multivariate Poisson model to calculate adjusted rates of hospital admissions for ambulatory care–sensitive conditions by duration of plan enrollment.
Results. Among beneficiaries with continuous Medicaid coverage, the percentage with 12 months of continuous enrollment in a health plan was significantly lower in counties with a choice of plans than in counties with no choice (79.2% vs 95.2%; P < .001). Annual ambulatory care–sensitive admission rates adjusted for age, gender, and race/ethnicity were significantly higher among beneficiaries living in counties with a choice of plans (6.58 admissions per 1000 beneficiaries; 95% confidence interval [CI] = 6.57, 6.58) than among those in counties with no choice (6.27 per 1000; 95% CI = 6.27, 6.28).
Conclusions. Potential benefits of health plan choice may be undermined by transaction costs of delayed enrollment, which may increase the probability of hospitalization for ambulatory care–sensitive conditions.
Extending consumer choice in health care is an important policy objective in a growing number of countries, reflecting recent developments in the United Kingdom1 and the Netherlands.2 This trend is occurring because choice and associated market-like competition are seen by many as an essential component of strategies to improve quality and efficiency and to increase the responsiveness of health care systems.3,4
Choice and competition are highly embedded features of the financing and delivery of health care in the United States. Many consumers of US health care are afforded a choice of health plans, medical groups, and providers as well as the ability to directly access specialist care and seek a second opinion. During the Clinton era,5 the concepts of competition and choice became synonymous with, rather than simply enablers of, efficient, high-quality health care. However, concern is increasing among health care analysts that the potential benefits of competition and choice are not being realized in practice.6 Furthermore, popular concerns about loss of choice have undermined key efforts to reform the US health care system. For example, arguments from those who opposed the expansion of managed care in the 1990s were often framed around how managed delivery systems would restrict choice of doctors and access to care.7 Similarly, opponents of recent proposals for a government-run, public plan option argued that the public option would limit, rather than expand, health plan choice by undermining the viability of commercial plans.8
The availability of choice is not uniform across the US health care system, and the poor and uninsured frequently have either no choice or limited choices. For example, Medicaid beneficiaries typically have fewer providers to choose from than do patients with commercial insurance because of low participation rates by physicians in the Medicaid program.9,10 Although approximately 60% of Medicaid beneficiaries nationwide are in managed care, the extent to which beneficiaries are able to choose a health plan varies considerably both between and within states.11,12
In California, managed care is mandatory for Temporary Assistance for Needy Families (TANF) Medicaid beneficiaries in 21 counties where approximately 90% of the state's beneficiaries reside. This group of California Medicaid beneficiaries consists mainly of children (67% are aged 18 years or younger) and younger women (66% of adult beneficiaries are women younger than 50 years). Although California beneficiaries do not have a choice about being in managed care, they may have a choice of health plans, depending on the county in which they reside. California has 3 county models of mandatory managed care: (1) County Organized Health Systems (COHS), with a single, nonprofit, county-run health plan (8 counties); (2) Two Plan counties, in which a nonprofit, county-run plan competes with a commercial plan (11 counties); and (3) Geographic Managed Care, in which multiple commercial plans compete (2 counties). In counties in which TANF beneficiaries have a choice of health plans, the beneficiaries have up to 45 days after gaining Medicaid eligibility to choose a plan. Furthermore, beneficiaries can change plans at any time while they are enrolled in California Medicaid. The difference between counties in the availability of health plan choice provides a natural experiment in which to compare differences in the quality of care delivered to the target population. In the present study, we examined the hypothesis that Medicaid beneficiaries living in counties that offer a choice of health plans receive a higher quality of care and have better health outcomes than do beneficiaries living in counties with a single health plan.
METHODS
We undertook a cross-sectional study by using a research file linking the 2002 California Medicaid Eligibility File and inpatient hospital discharge data from that year provided by the California Office of Statewide Health Planning and Development. The Medicaid Eligibility File contains data on each beneficiary's Medicaid eligibility status and health plan enrollment status on a monthly basis. Information on demographics (age, gender, and race/ethnicity), county of residence, and Medicaid eligibility criteria (TANF, disability, and Supplemental Security Income recipient) are contained in the file.
Predictor Variable
Our main predictor was whether a county offered a choice of health plans for TANF Medicaid beneficiaries. We combined Two Plan counties and Geographic Managed Care counties into a single group (counties with a choice of health plans) for the purpose of the analysis.
Outcome Variables
We compared duration of health plan enrollment and annual hospitalization rates for ambulatory care–sensitive (ACS) conditions among TANF beneficiaries continuously enrolled in Medicaid for 12 months during 2002 in 2 groups: counties with a choice of health plans and counties with no choice. We defined ACS conditions according to criteria set by the Agency for Healthcare Research and Quality.13 We identified ACS admissions among TANF beneficiaries on the basis of their primary diagnosis by use of International Classification of Diseases, Ninth Revision, codes.14 The validity of ACS admissions as indicators of primary care quality has been established previously with a clear relation being demonstrated between better access to ambulatory care and lower rates of ACS hospitalizations.15 Furthermore, beneficiaries in Medicaid managed care plans have been shown to have fewer hospitalizations for ACS conditions than do beneficiaries in fee-for-service Medicaid.16
Analysis
We aggregated hospital admissions for any ACS conditions into a single combined rate. We used a multivariate Poisson model with age, gender, race/ethnicity, and county type as covariates to calculate adjusted ACS admission rates in the choice and no-choice groups and by duration of health plan enrollment among TANF beneficiaries continuously enrolled in Medicaid. To assess whether differences in observed rates of hospitalizations for ACS conditions were likely related to better access to medical care, as a result of the availability of health insurance, we made similar comparisons between the choice and no-choice groups for a marker condition (appendicitis). Hospitalization rates for marker conditions are not influenced by access to ambulatory care and we therefore hypothesized that there would be no difference in appendicitis rates between the choice and no-choice groups even if the groups differed in their access to health plan coverage.17 To assess the effect of choice on the timing of health plan enrollment, we examined whether the pattern of monthly enrollment in health plans among new Medicaid beneficiaries differed between counties with a choice of health plans and counties with no choice. All analyses were undertaken by using the Stata 9.1 program (Stata Corporation, College Station, TX).
RESULTS
There were 3.0 million TANF Medicaid beneficiaries residing in the 21 California counties with mandatory managed care during 2002. Of these beneficiaries, 2.1 million (69%) were continuously enrolled in Medicaid during the year; 1.9 million of the continuously enrolled beneficiaries resided in 13 counties that offered a choice of health plans, and 200 000 of the continuously enrolled beneficiaries resided in 8 counties with a single plan (Table 1). There were small differences in the age and gender profile of TANF beneficiaries with continuous Medicaid enrollment in the choice and no-choice counties (mean age: 15.9 years and 15.2 years, respectively; percentage female: 56.8% and 55.9%, respectively). Counties with a choice of health plans had a smaller proportion of Hispanic beneficiaries but a higher proportion of Black beneficiaries than did counties with no choice (Table 1). Only 2.5% of beneficiaries in counties with a choice of health plans made use of their entitlement to switch health plans during the year.
TABLE 1.
Characteristics of Beneficiaries Continuously Enrolled in Medicaid by County Health Plan Model: California, 2002
| Choice Counties | No-Choice Counties | P | |
| No. | 1 864 704 | 224 176 | |
| Age, y | |||
| Mean (95% CI) | 15.9 (15.9, 15.9) | 15.3 (15.2, 15.3) | |
| Median (IQR/range) | 11 (5–24/0–64) | 10 (4–23/0–64) | |
| Gender, % female | 56.8 | 55.9 | < .001 |
| Race/ethnicity, % | < .001 | ||
| White | 20.2 | 20.8 | |
| Hispanic | 52.4 | 59.6 | |
| Black | 16.9 | 6.4 | |
| Asian/Pacific Islander | 4.8 | 3.1 | |
| Native American | 0.4 | 0.3 | |
| Other | 4.6 | 9.4 | |
| Missing | 0.8 | 0.5 |
Note. CI = confidence interval; IQR = interquartile range. P values are based on the χ2 test.
Duration of Health Plan Enrollment
Data on the duration of health plan enrollment among TANF beneficiaries by county model are presented in Table 2. Among beneficiaries with continuous Medicaid coverage in 2002, the percentage with 12 months of continuous enrollment in a health plan was significantly lower in counties with a choice of health plans than in those with no choice (79.2% vs 95.2%; P < .001). A total of 11.2% of beneficiaries in counties with a choice of health plans were in a health plan for less than 9 months compared with 2.0% in no-choice counties. The best performing county in the choice group had a lower percentage of beneficiaries with 12 months of continuous health plan enrollment than did the worst performing county in the no-choice group (85.6% vs 89.5%; P < .001). The worst performing county in the choice group had 1 in 7 beneficiaries (14.2%) enrolled in a health plan for less than 3 months.
TABLE 2.
Duration of Medicaid Health Plan Enrollment by County Health Plan Model: California, 2002
| No-Choice Counties |
Choice Counties |
|||
| Mean % | % Rangea (Minimum, Maximum) | Mean % | % Rangea (Minimum, Maximum) | |
| 12 months | 95.2 | 6.5 (89.5, 96.0) | 79.2 | 18.0 (67.6, 85.6) |
| 9–11 months | 2.9 | 3.4 (2.5, 5.9) | 9.6 | 3.7 (7.5, 11.2) |
| 6–8 months | 1.0 | 0.7 (0.8, 1.5) | 4.0 | 2.4 (2.8, 5.2) |
| 3–5 months | 0.5 | 0.8 (0.3, 1.1) | 1.4 | 0.7 (1.1, 1.8) |
| < 3 months | 0.5 | 1.7 (0.4, 2.1) | 5.8 | 11.2 (3.0, 14.2) |
Note. Percentages were calculated for mean county performance and range among beneficiaries with 12 months of continuous Medicaid coverage. P < .001 for difference in mean percentage of beneficiaries enrolled for 12 months by the χ2 test.
The range is the difference between the lowest and the highest values.
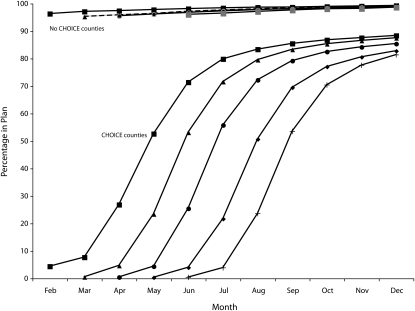
The calendar month of health plan enrollment among beneficiaries newly enrolled in Medicaid in the choice and no-choice counties between February and June 2002 is compared in Figure 1. More than 95% of new Medicaid beneficiaries in counties with no choice of health plan were enrolled in a health plan during their first month of becoming eligible for Medicaid. In comparison, fewer than 1% of beneficiaries living in counties with a choice of health plans were enrolled in a health plan during the first month, and only half of beneficiaries (51%–56%) were enrolled in a health plan 3 months after becoming eligible for Medicaid. One in 6 beneficiaries (15%–17%) in counties with a choice of health plans were not enrolled in a health plan 7 months after becoming eligible for Medicaid.
FIGURE 1.
Percentage of new Medicaid beneficiaries enrolled in a health plan, by month, in counties with a choice or no choice of health plans: California, 2002.
Note. Data are based on a subsample of 239,821 beneficiaries newly enrolled in Medicaid in February, March, April, May, and June 2002.
Admission Rates for Ambulatory Care–Sensitive Conditions
Among beneficiaries continuously enrolled in Medicaid, annual ACS admission rates adjusted for age, gender, and race/ethnicity were significantly higher (indicating worse quality of care) for beneficiaries living in counties with a choice of health plans (6.58 admissions per 1000 beneficiaries; 95% confidence interval [CI] = 6.57, 6.58) than for beneficiaries living in no-choice counties (6.27 admissions per 1000 beneficiaries; 95% CI = 6.27, 6.28). Adjusted admission rates for a marker condition (appendicitis) were the same in choice counties and no-choice counties (1.02 and 1.01 per 1000 beneficiaries, respectively).
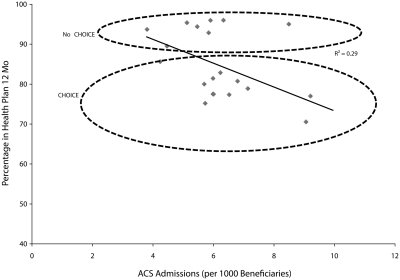
The association between the percentage of beneficiaries in a health plan for 12 months and adjusted ACS condition admission rates at the county level are presented in Figure 2. Among beneficiaries continuously enrolled in a health plan for 12 months, the adjusted admission rate for ACS conditions was significantly higher in no-choice counties (6.20 per 1000 beneficiaries; 95% CI = 6.19, 6.20) than in counties with a choice of health plans (6.02 per 1000 beneficiaries; 95% CI= 6.01, 6.03). However, consistent with previous research demonstrating lower hospitalization rates for ACS conditions among Medicaid beneficiaries in managed care rather than in fee-for-service plans, the fitted trend line suggested that adjusted ACS admissions rose in association with a decline in the percentage of beneficiaries in a health plan for 12 months; 29% of the variation in the ACS condition admission rate was attributable to variations in the mean duration of health plan enrollment at the county level. Among counties with a choice of health plans, 63% of the county-level variation in adjusted ACS admissions was attributable to variations in mean duration of health plan enrollment.
FIGURE 2.
Percentage of Medicaid beneficiaries with 12 months of continuous health plan enrollment and ambulatory care–sensitive admissions at the county level: California, 2002.
Consistent with these findings, we identified at the individual level a dose-response relation between adjusted ACS admissions and duration of plan enrollment among beneficiaries with continuous Medicaid coverage. ACS admission rates increased with shorter duration of health plan enrollment. The adjusted ACS admission rates (per 1000 beneficiaries) were 6.01, 8.54, 9.95, 11.50, and 13.41 among beneficiaries with 12, 9 to 11, 6 to 8, 3 to 5, and less than 3 months of continuous enrollment in a health plan, respectively.
DISCUSSION
Our findings indicate that the potential benefits of offering choice in California Medicaid managed care were undermined by beneficiaries delaying health plan enrollment and that these delays were strongly associated with higher adjusted admission rates for ACS conditions.
Existing Literature
Research literature examining the impact of health plan choice and competition on the quality of care remains sparse.18,19 However, 2 recently published studies found that health plan competition had a negative impact on quality within a public insurance program for children and had no effect on quality when examined among health plans nationwide. Liu and Phelps examined county-level associations between health plan competition (measured by number of plans) and quality of care in New York's Children's Health Insurance Program.20 They found that greater competition was negatively associated with quality scores for provider communication, preventative care visits, use of appropriate medication for asthma, and child immunization. In a study of all plans submitting data to the National Committee for Quality Assurance, Scanlon et al. found no association between the intensity of health plan competition and quality scores on both the Healthcare Effectiveness Data and Information Set (HEDIS) and Consumer Assessment of Health Plans Survey measures.21
An early evaluation of a competitive consumer choice model pilot within Florida Medicaid offers some important insights into why Medicaid beneficiaries may delay enrollment in health plans when provided a choice.12 The evaluation found that almost 1 in 2 Medicaid beneficiaries (43%–49%) in the 2 pilot counties were assigned to a health plan by the state because the beneficiaries did not choose a health plan within a 30-day deadline. Additionally, 30% of enrollees reported not being aware that they were being asked to choose a plan, and the majority of enrollees who chose a plan reported experiencing difficulty in understanding the plan information and making a choice.
Study Limitations
Our study had several limitations that should be considered when interpreting our findings. First, our use of cross-sectional data means that caution should be exercised concerning whether the associations found between the county model (choice or no choice), duration of plan enrollment, and adjusted ACS admission rates were causal. Nonetheless, the presence of a strong dose-response relationship between duration of health plan enrollment and ACS admission rates provides some support for a causal relationship. Second, an ACS admission is the end product of an accumulation of risk factors and interactions with the health care system, or lack thereof, over time. Although our study was restricted to TANF Medicaid beneficiaries (mainly young, female, and poor) and we adjusted for variations in age, gender, and race/ethnicity among beneficiaries living in choice and no-choice counties, there may have been some residual systematic differences in health status that we were unable to account for. However, such differences were likely to have been minimal because we excluded from consideration those Medicaid beneficiaries who were eligible on the basis of disability or other health-related conditions. Unfortunately, we were unable to adjust for potentially important health service factors, such as access to providers and wait times to see a provider for acute, urgent, or emergency visits, which may have differed between counties. Third, the data used for this study were from 2002 and may not reflect current patterns of health plan enrollment and ACS admissions in California Medicaid managed care. Finally, with only 2 counties delivering choice through Geographic Managed Care, we were unable to compare the relative difference in the quality of care between the 2 types of choice counties: those with multiple competing commercial plans and those in which a commercial plan competed with a public plan. Nonetheless, we were able to exploit county-level variation in the organization of Medicaid managed care to provide empirical evidence on whether having a choice of health plans is associated with quality of care.
Implications for Policy
Our study has several implications for health care policy and practice. First, our findings suggest that policymakers need to be mindful that providing choice in health care settings may produce unintended and potentially harmful consequences. Consideration should therefore be given to whether the potential benefits of providing greater choice in health care outweigh potential drawbacks. Second, our study suggests that the recent health care reform proposal to introduce a government-run, public plan option nationally may not have conferred all anticipated improvements in efficiency. In this study, the predominant county model of Medicaid managed care included a commercial plan competing with a public plan. Although we could not test whether this form of choice was more efficient than a model of only competing commercial plans, we found that competitive health plan models were less efficient in getting beneficiaries into plans and that the competitive models delivered lower quality of care as measured by hospitalizations for ACS conditions than did single-plan (payer) approaches. Third, interventions to mitigate the potential negative impacts of providing choice should be considered in health care systems in which choice is offered. For example, our findings highlight the need for more effective outreach within state Medicaid programs to minimize undue delays in health plan enrollment among beneficiaries living in choice environments. Several states have sought to address this problem by linking the Medicaid application and plan enrollment processes.22 Another promising approach involves the use of default options that, although preserving choice, could automatically assign beneficiaries who have not enrolled in a health plan after a fixed time period.23 Fourth, our findings suggest that there may be considerable bias in the assessment of health plan performance because lower percentages of beneficiaries living in choice environments are subject to public reporting compared with beneficiaries in no-choice environments. This difference arises because health plans are only required to report achievement of HEDIS indicators for beneficiaries with 12 months of continuous plan enrollment, for which California's choice counties show lower percentages of Medicaid beneficiaries.24 Our findings build on previous research that has identified considerable state-level variation in continuous plan enrollment among Medicaid managed care beneficiaries.25 Fifth, we found that the rate of plan switching, in which beneficiaries are able to switch health plans at any time without penalty, was low (2.5% during 2002) among this population. This finding is similar to that from a previous study conducted among Medicaid beneficiaries in North Carolina26 and could mean that California beneficiaries are satisfied with their health plans, are unaware that they can switch plans, or are unwilling to do so. In any case, plan switching does not appear to be a major driver of improvement in Medicaid health plan performance.
Conclusions
The provision of choice in managed care in California Medicaid was associated with delays in health plan enrollment, and these delays were strongly associated with poorer health outcomes. Health care planners in the United States and other countries considering using competition and choice as a means of improving the efficiency and quality of their health care systems should consider the potential for unintended consequences, particularly among underserved populations.
Acknowledgments
Support for this research was provided by The Commonwealth Fund.
Note. The views presented here are those of the authors and should not be attributed to The Commonwealth Fund or its directors, officers, or staff.
Human Participant Protection
The protocol for this data analysis was reviewed and approved by the University of California, San Francisco, institutional review board and the California Committee for the Protection of Human Subjects.
References
- 1.“Choose & Book.” Patient's Choice of Hospital and Booked Appointment Policy Framework for Choice and Booking at the Point of Referral. Available at: http://www.dh.gov.uk. Accessed June 22, 2009
- 2.Enthoven AC, van de Ven WP. Going Dutch–managed-competition health insurance in the Netherlands. N Engl J Med. 2007;357(24):2421–2423 [DOI] [PubMed] [Google Scholar]
- 3.Enthoven AC. The history and principles of managed competition. Health Aff. 1993;12(suppl 1):24–48 [DOI] [PubMed] [Google Scholar]
- 4.Le Grand J. Motivation, Agency, and Public Policy: Of Knights & Knaves, Pawns & Queens. Oxford, United Kingdom: Oxford University Press; 2003 [Google Scholar]
- 5.Emanuel EJ, Brett AS. Managed competition and the patient-physician relationship. N Engl J Med. 1993;329(12):879–882 [DOI] [PubMed] [Google Scholar]
- 6.Nichols LM, Ginsburg PB, Berenson RA, Christianson J, Hurley RE. Are market forces strong enough to deliver efficient health care systems? Confidence is waning. Health Aff (Millwood). 2004;23(2):8–21 [DOI] [PubMed] [Google Scholar]
- 7.Mechanic D. The managed care backlash: perceptions and rhetoric in health care policy and the potential for health care reform. Milbank Q. 2001;79(1):35–54III-IV [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.America's Health Insurance Plans AHIP Statement on House Health Care Reform Discussion Draft. Available at: http://www.ahip.org/content/pressrelease.aspx?docid=27496. Accessed July 2, 2009
- 9.Cunningham PJ, Hadley J. Effects of changes in incomes and practice circumstances on physicians’ decisions to treat charity and Medicaid patients. Milbank Q. 2008;86(1):91–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cunningham PJ, May JH. Medicaid Patients Increasingly Concentrated Among Physicians. Washington, DC: Center for Studying Health System Change; 2006. Tracking Report no. 16 [PubMed] [Google Scholar]
- 11.Centers for Medicare & Medicaid Services Medicaid Managed Care. Available at: http://www.cms.hhs.gov/MedicaidManagCare. Accessed June 22, 2009
- 12.Coughlin TA, Long SK, Triplett T, et al. Florida's Medicaid reform: informed consumer choice? Health Aff (Millwood). 2008;27(6):w523–w532 [DOI] [PubMed] [Google Scholar]
- 13.AHRQ Quality Indicators Prevention Quality Indicators Overview. Rockville, MD: Agency for Healthcare Research and Quality; 2004. Available at: http://www.qualityindicators.ahrq.gov/pqi_overview.htm. Accessed June 22, 2009 [Google Scholar]
- 14.International Classification of Diseases (ICD). World Health Organisation. Available at: http://www.who.int/classifications/icd/en/index.html. Accessed September 10, 2010.
- 15.Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA. 1995;274(4):305–311 [PubMed] [Google Scholar]
- 16.Bindman AB, Chattopadhyay A, Osmond DH, Huen W, Bacchetti P. The impact of Medicaid managed care on hospitalizations for ambulatory care sensitive conditions. Health Serv Res. 2005;40(1):19–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weissman JS, Gatsonis C, Epstein AM. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. JAMA. 1992;268(17):2388–2394 [PubMed] [Google Scholar]
- 18.Gaynor M. What do we know about competition and quality in health care markets? Cambridge, MA: National Bureau of Economic Research; 2006. NBER Working Paper no. 12301. Available at: http://www.nber.org/papers/w12301. Accessed August 4, 2010 [Google Scholar]
- 19.Morrisey MA. Competition in hospital and health insurance markets: a review and research agenda. Health Serv Res. 2001;36(1, part 2):191–222 [PMC free article] [PubMed] [Google Scholar]
- 20.Liu H, Phelps CE. Nonprice competition and quality of care in managed care: the New York SCHIP market. Health Serv Res. 2008;43(3):971–987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scanlon DP, Swaminathan S, Lee W, Chernew M. Does competition improve health care quality? Health Serv Res. 2008;43(6):1931–1951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fraser I, Chait E, Brach C. Promoting choice: lessons from managed Medicaid. Health Aff (Millwood). 1998;17(5):165–174 [DOI] [PubMed] [Google Scholar]
- 23.Halpern SD, Ubel PA, Asch DA. Harnessing the power of default options to improve health care. N Engl J Med. 2007;357(13):1340–1344 [DOI] [PubMed] [Google Scholar]
- 24.National Committee for Quality Assurance HEDIS: Healthcare effectiveness data and information set. Available at: http://www.ncqa.org/tabid/78/Default.aspx. Accessed July 16, 2009
- 25.Fairbrother G, Jain A, Park HL, Massoudi MS, Haidery A, Gray BH. Churning in Medicaid managed care and its effect on accountability. J Health Care Poor Underserved. 2004;15(1):30–41 [DOI] [PubMed] [Google Scholar]
- 26.Brandon WP, Troyer JL, Sundaram R, Schoeps N, Sun Y, Walsh BJ. Medicaid enrollee switching among managed care plans. J Health Care Poor Underserved. 2005;16(4):760–779 [DOI] [PubMed] [Google Scholar]