Abstract
Translation of research advances into clinical practice for at-risk communities is important to eliminate disease disparities. Adult type 2 diabetes prevalence in the US territory of American Samoa is 21.5%, but little intervention research has been carried out there. We discuss our experience with cultural translation, drawing on an emerging implementation science, which aims to build a knowledge base on adapting interventions to real-world settings. We offer examples from our behavioral intervention study, Diabetes Care in American Samoa, which was adapted from Project Sugar 2, a nurse and community health worker intervention to support diabetes self-management among urban African Americans. The challenges we experienced and solutions we used may inform adaptations of interventions in other settings.
Translating efficacious health treatments into routine clinical and public health practice to eliminate health disparities for communities at risk is an increasing public health priority. Recent significant advances in diabetes care have the potential to prevent complications from diabetes and improve quality of life, yet these evidence-based practices are not being used in real-world settings.1,2 Innovations from other cultures or from efficacy studies in academic settings may be ineffective in low-income, minority, or ethnic communities. This is attributable to barriers to care, such as limited access, health worker shortages, underfinanced health systems, and cultural and language factors, among many challenges.3 As a result, new research frameworks are emerging to help guide the adaptation process.
One such framework is translation research: applied research to help understand solutions to real-world health care delivery problems and to learn about transferability of solutions to diverse settings, while retaining effectiveness, efficiency, and sustainability.4 Another approach is implementation science, which describes the process of bridging health disparity gaps in developing countries; it also aims to create a knowledge base that can be applied across real-world settings to answer key research questions, such as how proven clinical interventions should be modified to achieve sustained health improvements.3 Both of these approaches advocate for exploration of advances in theoretical models, new methods, multilevel interventions, and multidisciplinary collaborations to accommodate different contexts.3,4
Diabetes rates are increasing in the United States and throughout the world, where 80% of people with diabetes live in low- and middle-income countries.5 Recent diabetes care advances need to be introduced in these communities, including the US territory of American Samoa, where the prevalence of type 2 diabetes in adults aged 18 years or older is 21.5%,6 double the 2007 US rate of 10.7% for adults aged 20 years and older.7 The Centers for Disease Control and Prevention launched an extensive process to build and train community coalitions to address diabetes in the Pacific Islands—including American Samoa—from 1998 to 2003,8–10 thus beginning to build an infrastructure to support diabetes interventions. Several descriptive reports of observational diabetes interventions among other Pacific Islanders have been published,11–13 as well as some comparison group studies among Samoans in New Zealand14,15 and Pacific Islanders in the Torres Strait Islands near Australia.16,17 However, no randomized controlled intervention trials among American Samoans have been conducted; studies with such a design would strengthen the science of translation.
The process of cultural adaptation brings yet another dimension to translation research, and this integrated process is termed cultural translation. We discuss our experience with cultural translation prior to and during our study, Diabetes Care in American Samoa (2004–2010). This intervention employs a primary care–based team comprising a nurse and 4 community health workers to support diabetes self-management. We describe our process of choosing an intervention approach from evidence-based models, our community partnerships, and our use of formative research and applied adaptations to design a randomized trial to test the effectiveness of the intervention in the Samoan setting. We also discuss challenges to the translation and solutions we developed, which may inform adaptations of interventions in other settings.
WHEN IS CULTURAL ADAPTATION NECESSARY?
The health disparities and cross-cultural literature has emphasized the importance of culturally salient and competent interventions, with researchers documenting a variety of strategies to achieve this.18–20 Still, it has been argued that adapting interventions to every context would be inefficient and that adaptation may compromise the fidelity of evidence-based treatments.21 Lau provided a helpful framework for considering when cultural adaptation is necessary and when it may not be.21 Cultural adaptation is warranted when there is evidence of variability across groups, that is, when cultural or contextual processes influence risk or protection from target problems or when the external validity of evidence-based interventions is jeopardized by differences in engagement (e.g., participation rates, attrition, compliance, etc.). Lau also advocated a directed approach for treatment adaptation, which uses existing or original research to enhance engagement and contextualize the intervention content to the target community.
Whaley and Davis described different approaches to cultural adaptation that are commonly used: (1) modify a standard intervention to be more inclusive, for example, by providing child care and transportation or adding educational sessions before the treatment; (2) make an intervention more culturally appropriate by incorporating generally known cultural values and experiences of the target group; (3) develop treatment guided by basic research; and (4) compare a standard and an adapted intervention (this approach has not yet been applied in randomized trials).19
Resnicow et al. operationalized 2 dimensions in the process: surface structure and deep structure.20 Surface structure refers to matching intervention materials and messages to observable social and behavioral characteristics of the target population, such as familiar faces, places, music, and foods. Deep structure reflects how cultural, psychological, social, political, environmental, and historical factors affect people differently across populations; these deeper factors should also be incorporated into interventions. Qualitative research, which incorporates such techniques as focus groups and in-depth interviews, is frequently used to gather information to learn about these key factors.22
Our approach to cultural translation relied on the following steps: (1) background research on epidemiology and culture; (2) preliminary meetings with community partners; (3) evaluation of evidence-based studies to adapt; (4) formative studies to learn about local culture and practices; (5) linguistic and cultural translation of measures; (6) adaptation of interventions, informed by formative studies and theory; (7) implementation of a randomized controlled trial; (8) follow-up qualitative studies to verify appropriateness of adaptations; and (9) interpretation of results with input of community partners. We drew many of these steps from previous research, particularly the Precede–Proceed Model for health program planning,23 which we applied in our study; however, here we emphasized steps that are involved in cultural translation of an intervention.
STEP 1—BACKGROUND RESEARCH ON EPIDEMIOLOGY AND CULTURE
An important starting point, as indicated in the Precede phase of the Precede–Proceed Model,23 is to learn about the target population, including its social and political history, its health problems, and how these problems relate to the culture and health behaviors. We started by reading the available literature.
The Samoan archipelago lies in the Pacific, midway between Hawaii and New Zealand. For centuries these islands remained in relative isolation, allowing them to maintain traditional lifestyles. However, colonization and subsequent modernization greatly affected the lifestyle and health of Samoans. Anthropological and epidemiological studies on the health of Samoans have been conducted by author S. T. M. and other colleagues over the past 30 years. Samoans residing in California, Hawaii, American Samoa, and Samoa suffer increasingly high levels of overweight, obesity, and the associated chronic noncommunicable conditions, including hypertension, type 2 diabetes, and high-risk lipid profiles.24–30 From 2002 to 2003, approximately 90% of all men and women in American Samoa had a body mass index of 26 kg/m2 or higher (the Polynesian standard of overweight).26,27 Between 1990 and 2002, the prevalence of type 2 diabetes among American Samoans aged 25 to 54 years increased from 12.9% to 17.2% in men and from 8.1% to 16.7% in women.26,27 Overall, in 2002 the prevalence of type 2 diabetes for adults aged 18 years and older was 21.5%.6
The increasing prevalence of obesity and diabetes among Samoans at the population level results from the general influences of socioeconomic modernization and specifically from the shift away from agrarian work to more sedentary jobs and an increased reliance on imported foods of low nutritional quality.26,31,32 For example, very few American Samoa adults now have subsistence farming and fishing as their main occupation,26 and traditional food staples such as taro, banana, and breadfruit have been replaced by white bread, white rice, and noodles. Imported meats of low nutritional quality, such as turkey tails and mutton flaps, and animal protein offered by an increasing number of US-based fast food restaurants, have replaced seafood as sources of protein and fat.27,31,33 These nutritional changes have been slower and less pervasive in the independent nation of Samoa.31,32
Certain cultural beliefs have complicated the changes brought on by modernization. The traditional respect for and acceptance of large body size is gradually changing, as idealization of thinner bodies spreads among Samoans; however, many individuals with large sizes still do not view themselves as overweight.34,35 At to'onai [Sunday feasts], fiafia [village celebrations], and fa'alavelave [large feasts for weddings or funerals], food is distributed by social status; matai [chiefs] and respected elders are fed first, with the largest portion sizes, followed by those with lower social status.27 Heavier labor was traditionally done by younger men, and as men aged, they shifted to a more managerial role in the family and to a more sedentary lifestyle.26,36 Until recently, when Samoan women married and raised children, they completed a large part of their social responsibility, and it became the job of their children and younger members of the village to care for them.37,38 In American Samoa today, 44% of adult women are employed in the wage and salary labor force.39
Traditionally, Samoan culture is both hierarchical and collectivist; therefore, the extended family is responsible for the support of its members, but a matai or other elder may be designated to make major health care decisions.40 Reliance on family for care may cause delays in seeking health care, especially for preventive care.41 Once in the health care system, Samoan patients regard doctors with great respect and want them to be directive and not to ask for patients' preferences for care.40 Diabetes and cancer are not viewed as Samoan illnesses because these diseases were not common in their community in the past; they have come about by not following fa'aSamoa [the traditional Samoan way of life].42
The effects of chronic illness on the island led local health care providers and public health officials in American Samoa to approach author S. T. M. and request research to address the high prevalence of diabetes. They specifically asked for an intervention to be used in their new community health center.
STEP 2—PRELIMINARY MEETINGS WITH COMMUNITY PARTNERS
Before we met with local stakeholders about formulating a research proposal, we reviewed the literature for effective diabetes interventions in primary care settings, diabetes interventions among Pacific Islanders and other ethnic minority populations, and cultural adaptation procedures. From this review, we identified a menu of ideas to present in American Samoa.
The movement for translation of evidence-based interventions calls for adaptations of specific approaches to new settings to reach populations in need.1,2,4 Our proposals emphasized approaches found to be successful, especially in the Pacific Islands or other minority communities. The parallel movement for community-based participatory research reflects a demand for greater sensitivity to local perceptions, needs, and circumstances and for inclusion of local stakeholders in formulating research questions, selecting methods, and interpreting results.43–45 By using translation research methods, we explicitly guided some intervention choices from evidence-based practices, and thus we did not use a full community-based participatory approach. Still, it is important that the adaptation be community guided.45,46 We identified several stakeholders for a series of meetings, including staff and board members from the community health center that is our main partner organization, leaders from the American Samoa Department of Health and its Diabetes Control Program, leaders from the local hospital, American Samoa Diabetes Association officers, and a local ophthalmologist. Our academic research team contributed research expertise in American Samoa and in diabetes interventions.
American Samoa is designated as a medically underserved area and health professional shortage area.46 No endocrinologist or diabetologist has established a practice on the island, although specialists visit and consult for short periods. One certified nurse diabetes educator and 1 registered dietician work at the hospital. All stakeholders recognized the need for serious attention to diabetes care. We discussed several intervention ideas, drawn from evidence-based models in primary care and other minority settings, including the use of case management, group-cluster visits, family group visits, peer outreach workers, self-management support, and peer-led support groups.16,17,47–52 Health center staff identified the need for expanded outreach to the community and to families. Health center staff suggested using a peer outreach worker to assist clinical staff with care coordination and to reach family members who influence self-care behaviors in Samoan culture. This approach would extend healthy lifestyle messages to the whole family, which is likely to include other people at risk for diabetes.
The research team advocated for the scientific strength of a randomized controlled trial, but local partners did not want to withhold care from a control group. This conflict has been common in community-based research, and alternative designs may serve both interests.45 The control group design was deemed acceptable by the community partners with the proviso that the control group be placed on a waiting list to eventually receive the experimental intervention. Local partners also appreciated outcome data provided by this design, so that if the intervention proved successful, a case could be made for extending it to other areas of the island.
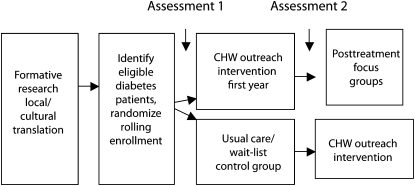
Area health professionals and health center staff welcomed the opportunity for training that our project might facilitate. Although some community members had participated in the Centers for Disease Control and Prevention Diabetes Today focus groups and coalition training,8–10 our project would specifically target a health care setting. Patient focus groups and provider interviews were important elements for our partners, to ensure that the community health worker intervention would be effectively tailored to local culture and practices. We also educated our partners about the process and time line for seeking funding and the need to collect preliminary data. Sharing research funds by way of local subcontracts was a concrete recognition of our partnership. The study design is shown in Figure 1.
FIGURE 1.
Study design: Diabetes Care in American Samoa, 2006–2011.
Note. CHW = community health worker.
STEP 3—CHOOSING EVIDENCE-BASED STUDIES TO TRANSLATE
Drawing from Lau's framework,21 we concluded that the American Samoan cultural context required cultural adaptation of the intervention. The epidemiological studies we consulted suggested differences in risk between Samoans and other ethnic groups in the United States. Many cultural practices contributed to these risks and needed to be taken into account. We found little evidence of differences in attrition or compliance because no comparative studies between Samoans and other ethnic groups have been conducted. We chose a directed approach to adaptation, drawing on evidence-based treatments of type 2 diabetes in other ethnic minority groups to identify an outreach worker design that fit our local partners' wishes.
Community health worker interventions have been used for decades in ethnic minority communities. Many communities have used these workers in group-based approaches to diabetes self-management education,50,53–57 and community health workers clearly have enhanced the cultural competency of the interventions and improved reach and participation rates. However, individuals in groups had lower participation rates than did individuals participating in home visits provided by community health workers.56,57 Few of these trials had randomized designs, and sample sizes were small, limiting researchers' ability to detect clear differences in outcomes. Some primary care interventions successfully used community health workers in care-management approaches. A cluster-randomized trial in 21 health centers in Pacific Torres Strait Islands compared having visiting diabetes specialists available for referral in all sites with a proactive community health worker reminder system in 8 sites. Significantly greater improvement (21%) in national guidelines indicators and 40% fewer hospital admissions were observed in the intervention than in the control sites,16 with improvements sustained 3 years later.17
In one of the few well-designed randomized controlled trials with a community health worker model, Project Sugar compared 4 types of care delivery among African Americans with diabetes in a Baltimore, Maryland, managed-care setting: a nurse–community health worker team, a nurse alone, a community health worker alone, and usual care.58 The nurse–community health worker team produced the best outcomes at a 2-year follow-up. A second study, Project Sugar 2 (PS2), more intensively and successfully compared the nurse–community health worker team with usual care.59,60
The available research indicated that the nurse–community health worker team model best fit the American Samoa context. Community health workers integrated within the medical team would help support self-management and extend the reach, quantity, and quality of interventions among diabetes patients. PS2 used the Precede–Proceed Model as a theoretical framework, which appears suitable for a collectivist culture and has been extensively applied around the world in many cultures.23 Such a framework allowed for the development of culturally appropriate interventions targeted at addressing predisposing (knowledge, beliefs), enabling (skills, resources), and reinforcing (family, health care providers) factors. Outreach workers had been used in American Samoa for maternal and child health initiatives, but there had been no such interventions for diabetes care. PS2 also used many of the best-practice components that were identified in reviews, such as treatment algorithms, community outreach, one-on-one interventions, and multiple contacts over time.47,48,61,62 Formative work would identify what cultural adaptations were needed.
STEP 4—FORMATIVE STUDIES
Original qualitative research, with its well-established methodology, is a common approach to formative work to identify what cultural adaptations are needed for intervention development.22,63 Further detail on our qualitative studies is presented elsewhere.64
We conducted focus groups with diabetes patients and in-depth interviews with health center providers. In 6 focus groups, with a total of 39 persons with diabetes, we explored barriers to and facilitators of diabetes self-care in American Samoa, attitudes about stress and depression, and feedback on proposed community health worker roles and home visits. We also sought feedback on sample images and messages, drawing from standard diet and exercise messages used by the National Diabetes Education Program65 and other Pacific health care materials66 to see whether further adaptation was needed for project-specific tools. The focus groups were conducted in Samoan by trained facilitators. We explored many of the same issues with all 13 health center clinicians in individual interviews, which were conducted in English.
Group sessions and interviews were audiorecorded and transcribed, and Samoan comments were translated into English before analysis of themes, which was facilitated by use of NVivo software.67 Challenges during the focus groups included accommodating an oratorical and hierarchical culture, in which speakers often took the stage at length and facilitators could not always respectfully interrupt, redirect, or probe. Linguistic translation of focus group transcripts provided another layer of analysis. It was necessary to recheck translations against the original language and to employ multiple translators to ensure that the correct meaning was transcribed.
STEP 5—CULTURAL TRANSLATION OF MEASURES
We selected measures for the 3 phases of evaluation, according to the Precede–Proceed Model: (1) process evaluation, to determine whether the program was delivered as intended; (2) impact evaluation, to measure the changes in intermediate outcomes and changes in predisposing (knowledge, beliefs), enabling (health behaviors, standards of care), and reinforcing (support for diabetes self-management) factors; and (3) outcome evaluation, to measure changes in health status (hemoglobin A1c level, blood pressure, BMI, waist circumference). Because of the complexity of diabetes in behaviors and relevant disease outcomes, we had many relevant measures from which to choose. It was important to select measures previously used in lower-literacy populations and to limit the number of measures to reduce burden. Our outcome selections also had to take into account the remoteness of the field site, with its lack of access to standardized research laboratories. Therefore, we chose to use a point-of-care assessment tool for hemoglobin A1c: the DCA Vantage Analyzer (Siemans Healthcare Diagnostics, Inc., Malvern, PA), which uses capillary blood samples, a method used by nonmedical personnel in previous research in remote field conditions.68
Few intervention research measures had been used previously in American Samoa. When standardized measures from mainstream culture are used in other ethnic groups, they may lack cultural relevance, leading to measurement error or misinterpretation of findings.69 Therefore, we used a World Health Organization protocol for linguistic and cultural translation of instruments: (1) forward translation, (2) expert panel back-translation, and (3) pretesting and cognitive interviewing.70 Linguistic translation from English to Samoan focused on finding the right words or phrases to express medical concepts for which there were often no analogous Samoan expressions.
Cultural translation focused on ensuring that the concepts we translated were as relevant as possible to Samoan life and culture. Cognitive interviews were an essential step in this process.71 In these interviews, translated questionnaires were administered to 10 diabetes patients. The patients answered each question and then discussed their answers and their understanding of the translated items with a research interviewer. Through this process we were able to determine that many of our questions were appropriately translated, and we corrected or adapted others before administration to participants in the randomized controlled trial.
In adapting standardized measures, it is important to strike a balance between the emic perspective (seeking equivalence within the culture) and the etic perspective (ensuring comparability across cultures).69 We sought a consensus among our investigators, who were expert in the content of the instruments, and our culture experts, who considered the work of multiple translators, because Samoan, like all languages, often has multiple ways to translate the same words. Although cognitive interviews are often used in item development,71,72 our protocol used them to confirm the effectiveness and cultural salience of our translations.
STEP 6—ADAPTATION OF INTERVENTIONS
After the qualitative studies were completed and themes were identified, we developed the intervention protocols and materials, drawing on PS2 interventions as a model.59 We were alert to the risk that our adaptation could compromise the fidelity of the original evidence-based treatments.21 Although the premise of PS2 served as an ideal intellectual backdrop, adaptations were needed to fit the more rural and isolated setting in American Samoa and to accommodate local barriers and cultural practices. Unique considerations in the American Samoa population included higher blood glucose and blood pressure levels.29,73
We adapted treatment algorithms to accommodate manageable staff workloads. We used somewhat higher cutpoints to define lower, medium, and higher risk; level of risk determined the frequency of visits for individuals. Because participants had limited access to professionally led diabetes education, we trained our community health workers to provide basic education during their home visits. To facilitate this, we developed flipcharts modeled on National Diabetes Education Program flipcharts for diabetes prevention by community health workers in other ethnic communities.65 Community health workers' pages contained their talking points and background information; participants simultaneously viewed parallel pages, with bigger images and minimal text.
Diabetes self-care is more complicated than diabetes prevention, so we developed 8 flipcharts, 1 with basic diabetes information and 7 about diabetes-related behaviors (monitoring, taking medication, healthy eating, being active, reducing risk, healthy coping, and problem solving).74 Intervention delivery was guided by patient risk, as determined by algorithm, and by self-directed patient goals from the menu of 7 health behaviors. Further, the flipcharts were organized to include strategies in the Precede–Proceed Model: predisposing factors (exploring beliefs and motivation), enabling factors (building behavior change skills), and reinforcing factors (enlisting support from family and community).23 We also incorporated local cultural features in the flipcharts, including quotes from focus groups, culturally relevant examples of healthy behaviors, local sources of stress, and effective local coping strategies. Linguistic translations of printed materials were requested by staff for themselves as well as for participants. Although staff members were bilingual, their comfort with English varied. Side-by-side translations facilitated shifting from one language to the other, reflecting the way people regularly speak.
After drafts were developed for flipcharts and visit protocols, we reviewed them with local staff and practiced with role plays. Then we made further adaptations to better fit how the materials would be used. This process of collaboration, an integral part of community-based participatory research,43–45 was invaluable; it revealed the need to scale back both the quantity and complexity of information, and it identified additional training needs for the staff. Staff members also came up with novel interactive teaching tools, such as laminated photos of locally available foods that could be sorted into red, yellow, and green categories, according to the National Diabetes Education Program red light system for foods to eat more of, eat with caution, and avoid.65
STEP 7—IMPLEMENTATION OF THE RANDOMIZED CONTROLLED TRIAL
Conducting a randomized trial in a setting where intervention research is unfamiliar required several cultural adaptations. We provided education to all health center staff about research practices, including why we do research, why we randomize, what contamination across study groups is, and how it affects study goals. Health care personnel on the island have limited opportunities for continuing education, and few can afford to seek training elsewhere. Therefore, health center clinicians specifically asked for more training on diabetes care as part of this project. This training was provided over a 4-day visit by author M. G. G. and included a review of the American Diabetes Association standards of care75; principles and elements of the chronic care model,76,77 which has been adopted by federally funded health centers throughout the United States, with several sessions on the self-management support component of the model78; and sessions on patient-centered communication skills.79
Our local project staff also received extensive training on diabetes management, assessment techniques, and study protocols, and all were certified on human participant protection. The community health worker training was geared to a lay audience with high school education. We used several hands-on learning techniques, such as role plays and daily quizzes, with prizes for correct answers or knowing where to find the correct information. Study protocols were approved by American Samoa and Brown University review boards.
The randomized trial, which is under way, will test the effectiveness of an intervention coordinated by a nurse and community health worker team to provide outreach, education, and support to type 2 diabetes patients and their families. We randomized villages instead of patients because of extensive familial and local community ties. Villages are matched by size and location in the health center catchment's area, and villages in the pairs are randomly assigned to intervention or control group. Control participants receive their usual care at the health center for 1 year, after which they will receive the intervention. Eligibility for this sample is broad, because this translational research is intended to test real-world effectiveness: participants must be aged 21 years or older, reside in the health center service area, self-identify as Samoan, have type 2 diabetes diagnosed by a physician, be mentally competent and willing to give informed consent, be unlikely to leave American Samoa for more than 4 months during the study, and have no comorbid conditions likely to lead to death in the next year (e.g., end-stage renal disease or cancer). Characteristics of the total population of health center diabetes patients will be used to assess the sample's representativeness and external validity and to ensure that this research is relevant to practicing clinicians and policymakers.80,81
Some challenges during implementation of the trial have required other adaptations. Because research funding is temporary, local staff were hired on 1-year contracts, as required by American Samoa government policy. Delays in contract approvals caused a 6-month wait before staff could start working. Further, contract renewals required special extensions by the governor because government policy allowed only 1-year nonrenewable contracts. Therefore, renewals also involved delays. These delays led to significant gaps in staff coverage, which caused us to fall behind on our time line.
Although the original research job descriptions differentiated between research assistants (who were to do assessment interviews and data entry) and community health workers (responsible for patient education and support), we decided to cross-train staff on all tasks. We found this to be more effective in building a consistent team that is able to manage all necessary tasks, especially when gaps in staff coverage occur. These accommodations have required more training, closer supervision, and additional quality control mechanisms. We could not do this work without a full-time field director, who supervises the research in American Samoa, bridging the requirements of research and local authority and policy.
Another key adaptation involves working with the limited access to medical supplies that is common in low-income communities and island economies. Blood glucose–testing equipment and supplies are too costly for most island residents, and they do not have individual medical insurance to cover these costs; therefore, most patients only have access to blood sugar testing at the medical clinic. It is also common for the medical clinic to be without these crucial supplies for varying periods because of funding shortages. Our study was not funded to provide blood-testing supplies for individuals. We therefore had to redefine the role of blood glucose monitoring to include problem solving within families to increase access to meters and supplies. Community health workers also provide regular testing during their visits.
STEP 8—POSTTREATMENT QUALITATIVE STUDIES
We plan to do additional qualitative studies with participants in the intervention group and with study staff and clinicians at the health center, after the posttreatment assessments at the 1-year follow-up. These qualitative studies will examine the salient features of the intervention in the view of participants and providers, such as perceived efficacy, burden, facilitators and barriers, and potential for sustainability and wider spread. For example, we will ask about the extent to which community health workers were fully integrated into the health care system, how confident patients became in self-care, and how both of these factors could be improved. These data will be used to complement quantitative data outcomes and provide a qualitative thick description of the experiences participants and staff had with the intervention.
Posttreatment qualitative data are especially important in this first intervention study in American Samoa because they will provide in-depth feedback on the intervention and research procedures to guide future research. We are deliberately collecting qualitative data from the perspective of both participants and the staff who delivered the intervention, to determine whether future adaptations are needed to meet either group's needs.
STEP 9—INTERPRETATION OF STUDY RESULTS WITH COMMUNITY PARTNERS
Participation of community partners in interpreting results is encouraged in all community-based research.43–45 It is especially important in cross-cultural research to enlist the perspectives of the local culture experts, and it is ethically important to avoid potential harm from bias and stereotypes in interpretations.82,83 We have used our health center executive and medical director, our project staff, and the health center board, which includes business leaders and lay members, as advisers during the project. Our multidisciplinary research team, consisting of anthropologists, health psychologists, a physician, and a nurse diabetes educator, have also provided different perspectives that have been valuable throughout the process.
When posttreatment data are available, we will seek these partners' input as well to help interpret our findings. Also at that juncture, our community partners will help us consider next steps if community health worker services prove to be valuable to find ways to sustain and further disseminate community health worker services for diabetes care.
INSIGHTS
Although many efficacious interventions exist to improve diabetes care, including examples in ethnic minority populations,49,50,61,62 evidence-based treatments are needed by many underserved ethnic groups and communities to further reduce health disparities in diabetes. Our approach to cultural translation drew from the emerging science of translation research and cultural adaptation to bring strong scientific methods to American Samoa. Cultural adaptation was necessary in this context because diabetes risk on the island is much higher than in the general US population, and cultural practices contribute to this risk. Our community partners selected an approach coordinated by community health workers and primary care providers. Previous adaptations of community health worker interventions in other ethnic groups have improved cultural competency, reach, and participation rates, but few of these trials used randomized designs, and sample sizes were often small, yielding few clear differences in outcomes. Previous studies on diabetes interventions in Pacific Island populations also lacked randomized designs and produced little data specific to American Samoans.
We chose to adapt the community health worker–nurse team intervention from PS2,59,60 which was conducted in an African American population, because it was evidence based, had proved successful in a randomized controlled trial, and incorporated features found in other successful diabetes interventions. The PS2 interventions were integrated with primary care, providing a good model for the primary care context in American Samoa.
We have found many of our practical and cultural adaptations to be beneficial. Conducting qualitative research was important to our community partners to ensure cultural competency of the community health worker approach in the local primary care setting. The patient focus groups and provider interviews offered practical advice about community health worker roles and job duties, such as ways of showing respect while visiting patients' homes and discussing sensitive medical topics. Focus group participants also reported that images from materials produced for other Pacific Islands were not acceptable because they wanted to see their own people, their own foods, and local examples of physical activities. The adapted flipcharts included these local images for teaching diabetes self-management; these flipcharts continue to be a valued resource for both community health workers and patients in our ongoing trial. Other adaptations included higher cutpoints on treatment algorithms to accommodate the higher-risk population in American Samoa and flexible teaching on glucose monitoring to accommodate patients' limited access to meters. These adaptations appear to be feasible for this setting.
The more challenging situations have involved delays in hiring staff and renewing contracts through the local government and delays in purchasing and shipping supplies. These issues have been further complicated by tight research timelines and limited funds. Yet such challenges are common in real-world settings, and practical interventions must be flexible enough to accommodate them. It is helpful to be mindful of multiple layers of cultural translation, bridging not only ethnic cultures but also research and medical cultures, and to be respectful of each. We have tried to find solutions at each juncture that are guided by the values inherent in local cultural practices, best medical practices, and sound principles of research methods and human participant protection. When these different values have not appeared to be compatible, we have tried to find common ground and to retain the most salient features of each value system.
Although cultural translation is necessary to ensure cultural competency and practical implementation in real-world settings, each adaptation risks diminishing the validity of the evidence-based treatment on which it is modeled. Translation research brings new questions to be considered by researchers and in future analyses. How far can we adapt an intervention before it becomes a different intervention altogether and we have lost fidelity with the original treatment? We have used core components identified as successful in systematic reviews and meta-analyses—treatment algorithms, community outreach, one-on-one interventions, and multiple contacts over time.49,50,61,62 Will these key components from previous reviews be the salient components for success in this community? Can we retain the salient components? It is helpful if we consider and document our challenges and lessons learned as key findings of this work rather than as mere disruptions of the randomized trial's implementation.
Effective interventions should be developed that go beyond a static view of cultural competence and have a chance of being sustained and further improved by local health care and public health organizations. Cultural competency is also best viewed as a lifelong process and not an end result.82 Moreover, this process takes place in cultures that are themselves in constant transition, as are the communities and health systems in which we embed our interventions. So too is research and intervention science, because we are constantly seeking to improve on our experience in these ever-changing systems.
Acknowledgments
This study was funded by the National Institute of Diabetes, Digestive and Kidney Disorders (grant R18-DK075371).
We appreciate the contributions of Pasa Turituri, Diabetes Control Program, American Samoan Department of Health. We also appreciate the contributions of our collaborators Ray Niaura and Samuel Holzman, Brown University, to the early phases of this work.
Human Participant Protection
All study protocols for the qualitative phases and intervention trial were approved by the American Samoan and Brown University institutional review boards.
References
- 1.Narayan KM, Gregg EW, Engelgau MM, et al. Translation research for chronic disease: the case of diabetes. Diabetes Care. 2000;23(12):1794–1798 [DOI] [PubMed] [Google Scholar]
- 2.Garfield SA, Malozowski S, Chin MH, et al. Considerations for diabetes translational research in real-world settings. Diabetes Care. 2003;26(9):2670–2674 [DOI] [PubMed] [Google Scholar]
- 3.Madon T, Hofman KJ, Kupfer L, Glass RI. Public health. Implementation science. Science. 2007;318(5857):1728–1729 [DOI] [PubMed] [Google Scholar]
- 4.Narayan KM, Benjamin E, Gregg EW, Norris SL, Engelgau MM. Diabetes translation research: where are we and where do we want to be? Ann Intern Med. 2004;140(11):958–963 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organiziation World Health Organization diabetes programme. Available at: http://www.who.int/diabetes/en. Accessed April 11, 2009
- 6.DiBello JR, Baylin A, Viali S, Tuitele J, Bausserman L, McGarvey ST. Adiponectin and type 2 diabetes in Samoan Adults. Am J Hum Biol. 2009;21(3):389–391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Institutes of Health National diabetes statistics, 2007. Available at: http://diabetes.niddk.nih.gov//dm/pubs/statistics/index.htm. Accessed April 11, 2009
- 8.Braun KL, Kuhaulua RL, Ichiho HM, Aitaoto NT. Listening to the community: a first step in adapting Diabetes Today to the Pacific. Pac Health Dialog. 2002;9(2):321–328 [PubMed] [Google Scholar]
- 9.Braun KL, Ichiho HM, Kuhaullua RL, et al. Empowerment through community building: Diabetes Today in the Pacific. J Public Health Manag Pract. 2003;Nov(suppl):S19–S25 [PubMed] [Google Scholar]
- 10.Aitaoto NT, Braun KL, Ichiho HM, Kuhau RL. Diabetes Today in the Pacific: reports from the field. Pac Health Dialog. 2005;12(1):124–131 [PubMed] [Google Scholar]
- 11.Humphry J, Jameson LM, Beckham S. Overcoming social and cultural barriers to care for patients with diabetes. West J Med. 1997;167(3):138–144 [PMC free article] [PubMed] [Google Scholar]
- 12.Beckham S, Bradley S, Washburn A, Taumua T. Diabetes management: utilizing community health workers in a Hawaiian/Samoan population. J Health Care Poor Underserved. 2008;19(2):416–427 [DOI] [PubMed] [Google Scholar]
- 13.Mau MK, Glanz K, Severino R, Grove JS, Johnson B, Curb JD. Mediators of lifestyle behavior change in Native Hawaiians: initial findings from the Native Hawaiian Diabetes Intervention Program. Diabetes Care. 2001;24(10):1770–1775 [DOI] [PubMed] [Google Scholar]
- 14.Bell AC, Swinburn BA, Amosa H, Scragg RK. A nutrition and exercise intervention program for controlling weight in Samoan communities in New Zealand. Int J Obes Relat Metab Disord. 2001;25(6):920–927 [DOI] [PubMed] [Google Scholar]
- 15.Simmons D, Fleming C, Voyle J, Fou F, Feo S, Gatland B. A pilot urban church-based programme to reduce risk factors for diabetes among Western Samoans in New Zealand. Diabet Med. 1998;15(2):136–142 [DOI] [PubMed] [Google Scholar]
- 16.McDermott RA, Schmidt BA, Sinha A, Millis P. Improving diabetes care in the primary healthcare setting: a randomized cluster trial in remote indigenous communities. Med J Aust. 2001;174(10):497–502 [DOI] [PubMed] [Google Scholar]
- 17.McDermott R, Tulip F, Schmidt B, Sinha A. Sustaining better diabetes care in remote indigenous Australian communities. BMJ. 2003;327(7412):428–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown SA, Garcia AA, Winchell M. Reaching underserved populations and cultural competence in diabetes education. Curr Diab Rep. 2002;2(2):166–176 [DOI] [PubMed] [Google Scholar]
- 19.Whaley AL, Davis KE. Cultural competence and evidence-based practice in mental health services: a complementary perspective. Am Psychol. 2007;62(6):563–574 [DOI] [PubMed] [Google Scholar]
- 20.Resnicow K, Jackson A, Blissett D, et al. Results of the Healthy Body Healthy Spirit trial. Health Psychol. 2005;24(4):339–348 [DOI] [PubMed] [Google Scholar]
- 21.Lau AS. Making the case for selective and directed cultural adaptations of evidence-based treatments: examples from parent training. Clin Psychol Sci Pract. 2006;13(4):295–310 [Google Scholar]
- 22.Halcomb EJ, Gholizadeh L, DiGiacomo M, Phillips J, Davidson PM. Literature review: considerations in undertaking focus group research with culturally and linguistically diverse groups. J Clin Nurs. 2007;16(6):1000–1011 [DOI] [PubMed] [Google Scholar]
- 23.Green LW, Kreuter MW. Health Program Planning: An Educational and Ecological Approach. 4th ed.New York, NY: McGraw-Hill; 2005 [Google Scholar]
- 24.Collins VR, Dowse GK, Toelupe PM, et al. Increasing prevalence of NIDDM in the Pacific island population of Western Samoa over a 13-year period. Diabetes Care. 1994;17(4):288–296 [DOI] [PubMed] [Google Scholar]
- 25.Roberts ST, McGarvey ST, Viali S, Quested C. Youth blood pressure levels in Samoa in 1979 and 1991–93. Am J Human Biol. 2004;16(2):158–167 [DOI] [PubMed] [Google Scholar]
- 26.Keighley ED, McGarvey ST, Turituri P, Viali S. Farming and adiposity in Samoan adults. Am J Hum Biol. 2006;18(1):112–122 [DOI] [PubMed] [Google Scholar]
- 27.Keighley ED, McGarvey ST, Quested C, McCuddin C, Viali S, Maga UA. Nutrition and health in modernizing Samoans: temporal trends and adaptive perspectives. : Ohtsuka R, Ulijaszek SJ, Health Change in the Asia-Pacific Region. New York, NY: Cambridge University Press; 2007:142–191 [Google Scholar]
- 28.McGarvey ST. Obesity in Samoans and a perspective on its etiology in Polynesians. Am J Clin Nutr. 1991;53(suppl 6):1586S–1594S [DOI] [PubMed] [Google Scholar]
- 29.McGarvey ST. Cardiovascular disease (CVD) risk factors in Samoa and American Samoa, 1990–95. Pac Health Dialog. 2001;8(1):157–162 [PubMed] [Google Scholar]
- 30.McGarvey ST. Interdisciplinary translational research in anthropology, nutrition, and public health. Annu Rev Anthropol 2009;38:233–249 [Google Scholar]
- 31.Galanis DJ, McGarvey ST, Quested C, Sio B, Afele-Fa'amuli SA. Dietary intake of modernizing Samoans: implications for risk of cardiovascular disease. J Am Diet Assoc. 1999;99(2):184–190 [DOI] [PubMed] [Google Scholar]
- 32.DiBello JR, McGarvey ST, Kraft P, et al. Dietary patterns are associated with metabolic syndrome in adult Samoans. J Nutr. 2009;139(10):1933–1943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hughes RG, Lawrence MA. Globalization, food and health in Pacific Island countries. Asia Pac J Clin Nutr. 2005;14(4):298–306 [PubMed] [Google Scholar]
- 34.Brewis AA, McGarvey ST, Jones J, Swinburn BA. Perceptions of body size in Pacific Islanders. Int J Obes Relat Metab Disord. 1998;22(2):185–189 [DOI] [PubMed] [Google Scholar]
- 35.Brewis AA, McGarvey ST. Body image, body size, and Samoan ecological and individual modernization. Ecol Food Nutr. 2000;39(2):105–120 [Google Scholar]
- 36.Baker PT, Hanna JM, Baker TS. The Changing Samoans: Behavior and Health in Transition. New York, NY: Oxford University Press; 1986 [Google Scholar]
- 37.Holmes LD, Holmes ED. Samoan Village Then and Now. Fort Worth, TX: Harcort Brace; 1992 [Google Scholar]
- 38.O'Meara T. Samoan Planters: Tradition and Economic Development in Polynesia. Orlando, FL: Rinehart and Winston; 1990 [Google Scholar]
- 39.US Census Population and housing profile, American Samoa. Available at: http://www.census.gov/prod/cen2000/island/ASprofile.pdf. Accessed, April 27, 2009
- 40.McLaughlin LA, Braun KL. Asian and Pacific Islander cultural values: considerations for health care decision making. Health Soc Work. 1998;23(2):116–126 [DOI] [PubMed] [Google Scholar]
- 41.Puaina S, Aga DF, Pouesi D, Hubbell FA. Impact of traditional Samoan lifestyle (fa'aSamoa) on cancer screening practices. Cancer Detect Prev. 2008;32(suppl 1):S23–S28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hubbell FA, Luce PH, McMullin JM. Exploring beliefs about cancer among American Samoans: focus group findings. Cancer Detect Prev. 2005;29(2):109–115 [DOI] [PubMed] [Google Scholar]
- 43.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202 [DOI] [PubMed] [Google Scholar]
- 44.Chen DT, Jones L, Gelberg L. Ethics of clinical research within a community-academic partnered participatory framework. Ethn Dis. 2006;16(1 suppl 1):S118–S135 [PubMed] [Google Scholar]
- 45.Bogart LM, Uyeda K. Community-based participatory research: partnering with communities for effective and sustainable behavioral health interventions. Health Psychol. 2009;28(4):391–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Health Services and Resource Administration Designated health professional shortage areas (health statistics) 2009. Available at: http://ers.hrsa.gov. Accessed November 16, 2009
- 47.Norris SL, Engelgau MM, Narayan KMV. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24(3):561–587 [DOI] [PubMed] [Google Scholar]
- 48.Norris SL, Nichols PJ, Caspersen CJ, et al. The effectiveness of disease and case management for people with diabetes. A systematic review. Am J Prev Med. 2002;22(suppl 4):S15–S38 [DOI] [PubMed] [Google Scholar]
- 49.Norris SL, Chowdhury FM, Van Le K, et al. Effectiveness of community health workers in the care of people with diabetes. Diabet Med. 2006;23(5):544–556 [DOI] [PubMed] [Google Scholar]
- 50.Philis-Tsimikas A, Walker C, Rivard L, et al. Improvement in diabetes care of underinsured patients enrolled in Project Dulce: a community-based, culturally appropriate, nurse case management and peer education diabetes care model. Diabetes Care. 2004;27(1):110–115 [DOI] [PubMed] [Google Scholar]
- 51.Sarkisian CA, Brown AF, Norris KC, Wintz RL, Mangione CM. A systematic review of diabetes self-care interventions for older, African American, or Latino adults. Diabetes Educ. 2003;29(3):467–479 [DOI] [PubMed] [Google Scholar]
- 52.Satterfield D, Burd C, Valdez L, Hosey G, Eagle Shield J. The “in-between people”: participation of community health representatives in diabetes prevention and care in American Indian and Alaska Native communities. Health Promot Pract. 2002;3(2):166–175 [Google Scholar]
- 53.Brown SA, Garcia AA, Kouzekanani D, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans: the Starr County border health initiative. Diabetes Care. 2002;25(2):259–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Teufel-Shone NI, Drummond R, Rawiel U. Developing and adapting a family-based diabetes program at the U.S.–Mexico border. Prev Chronic Dis [serial online]. Published January 2005. Available at: http://www.cdc.gov/pcd/issues/2005/jan/04_0083.htm. Accessed July 1, 2005 [PMC free article] [PubMed]
- 55.Carter JS, Pugh JA, Monterrosa A. Non-insulin dependent diabetes mellitus in minorities in the United States. Ann Intern Med. 1996;125(3):221–232 [DOI] [PubMed] [Google Scholar]
- 56.Gilliland SS, Azen SP, Perez GE, Carter JS. Strong in body and spirit, lifestyle intervention for Native American adults with diabetes in New Mexico. Diabetes Care. 2002;25(1):78–83 [DOI] [PubMed] [Google Scholar]
- 57.Fedder DO, Chang RJ, Curry S, Nichols G. The effectiveness of a community health worker outreach program on healthcare utilization of West Baltimore City Medicaid patients with diabetes, with or without hypertension. Ethn Dis. 2003;13(1):22–27 [PubMed] [Google Scholar]
- 58.Gary TL, Bone L, Yeh HC, et al. Randomized clinical trial of the effects of nurse case manager and community health worker team interventions on risk factors for diabetes-related complications in urban African Americans. Prev Med. 2003;37(1):23–32 [DOI] [PubMed] [Google Scholar]
- 59.Gary TL, Batts-Turner M, Bone L, et al. A randomized clinical trial of the effects of nurse case manager and community health worker team interventions in urban African Americans with type 2 diabetes. Control Clin Trials. 2004;25(1):53–66 [DOI] [PubMed] [Google Scholar]
- 60.Gary TL, Hill-Briggs F, Batts-Turner M, Brancati FL. Translational research principles of an effectiveness trial for diabetes care in an urban African American population. Diabetes Educ. 2005;31(6):880–889 [DOI] [PubMed] [Google Scholar]
- 61.Goldstein MG, Whitlock EP, DePue JD, Planning Committee of the Addressing Multiple Behavioral Risk Factors in Primary Care Project. Multiple behavioral risk factor interventions in primary care. Summary of research evidence. Am J Prev Med. 2004;27(suppl 2):61–79 [DOI] [PubMed] [Google Scholar]
- 62.Glazier RH, Kennie NR, Bajcar J, Wilson K. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care. 2006;29(7):1675–1688 [DOI] [PubMed] [Google Scholar]
- 63.Ulin PR, Robinson ET, Tolley EE. Qualitative Methods in Public Health: A Field Guide for Applied Research. San Francisco, CA: Jossey-Bass; 2005 [Google Scholar]
- 64.Rosen RK, DePue J, McGarvey ST. Overweight and diabetes in American Samoa: the cultural translation of research into health care practice. Med Health R I. 2008;91(12):372–373, 376–377 [PubMed] [Google Scholar]
- 65.Rodriguez B, Kelly J. The road to health toolkit. National Diabetes Education Program, Centers for Disease Control and Prevention. Available at: http://www.ced.gov/diabetes/NDEP/CE_RoadtoHealth.htm. Accessed April 16, 2009
- 66.Pacific Diabetes Education Program. Available at: http://www.pdep.org. Accessed November 16, 2009.
- 67.NVivo Qualitative Data Analysis Software [computer program]. Version 8. Melbourne, Australia: QSR International; 2008 [Google Scholar]
- 68.Carter JS, Houston CA, Gilliland SS, et al. Rapid HbA1c testing in a community setting. Diabetes Care. 1996;19(7):764–767 [DOI] [PubMed] [Google Scholar]
- 69.Alegria M, Vila D, Woo M, et al. Cultural relevance and equivalence in the NLAAS instrument: integrating the etic an emic in the development of cross-cultural measures for psychiatric epidemiology and services study of Latinos. Int J Methods Psychiatr Res. 2004;13(4):270–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.World Health Organization Process of translation and adaptation of instruments. Available at: http://www.who.int/substance_abuse/research_tools/translation/en. Accessed April 11, 2009
- 71.Nápoles-Springer AM, Santoyo-Olsson J, O'Brien H, Stewart AL. Using cognitive interviews to develop surveys in diverse populations. Med Care. 2006;44(11 suppl 3):S21–S30 [DOI] [PubMed] [Google Scholar]
- 72.Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA: Sage; 2004 [Google Scholar]
- 73.World Health Organization and American Samoa Government American Samoa NCD risk factors, STEPS report. Published 2007. Available at: http://www.who.int/chp/steps/AmericanSamoaSTEPSReport.pdf. Accessed April 20, 2009
- 74.American Association of Diabetes Educators AADE7 self-care behaviors. Diabetes Educ. 2008;34(3):445–449 [DOI] [PubMed] [Google Scholar]
- 75.American Diabetes Association Standards of medical care in diabetes—2009. Diabetes Care. 2009;32(suppl 1):S13–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–1779 [DOI] [PubMed] [Google Scholar]
- 77.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002;288(15):1909–1914 [DOI] [PubMed] [Google Scholar]
- 78.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475 [DOI] [PubMed] [Google Scholar]
- 79.Goldstein MG, DePue J, Kazura A. Models of provider-patient interaction and shared decision making. : Shumaker SA, Ockene JK, Riekert KA, Handbook of Health Behavior Change. 3rd ed New York, NY: Springer Publishing; 2008:107–126 [Google Scholar]
- 80.Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA. 2003;290(12):1624–1632 [DOI] [PubMed] [Google Scholar]
- 81.Glasgow RE, Magid DJ, Beck A, Ritzwoller D, Estabrooks PA. Practical clinical trials for translating research to practice: design and measurement recommendations. Med Care. 2005;43(6):551–557 [DOI] [PubMed] [Google Scholar]
- 82.American Psychological Association Guidelines on multicultural education, training, research, practice, and organizational change for psychologists. Am Psychol. 2003;58(5):377–402 [DOI] [PubMed] [Google Scholar]
- 83.Public Health Leadership Society Principles of the ethical practice of public health. Version 2.2. Published 2002. Available at: http://www.apha.org/NR/rdonlyres/1CED3CEA-287E-4185-9CBD-BD405FC60856/0/ethicsbrochure.pdf. Accessed April 27, 2009