Abstract
Gold nanoparticles (AuNPs) are a suitable platform for development of efficient delivery systems. AuNPs can be easily synthesized, functionalized, and are biocompatible. The tunability of the AuNP monolayer allows for complete control of surface properties for targeting and stability/release using these nanocarriers. This review will discuss several delivery strategies utilizing AuNPs.
1. Introduction
One of the greatest challenges facing chemotherapy today is developing drug delivery systems (DDSs) that are efficacious and have therapeutic selectivity [1]. Both passive and active targeting approaches have been utilized with nanocarriers such as dendrimers [2, 3], liposomes [4], metal nanoparticles [5], polymer micelles and vesicles [6, 7]. These DDSs have improved in the targeted delivery of the therapeutics for cancer treatment.
The application of gold nanoparticles (AuNPs) as a DDS is a rapidly expanding field [8, 9]. Their inherent properties make them a very promising vehicle for drug delivery. Controlled fabrication of various sized particles (1–150 nm) with limited size dispersity has been established [10], and using ligand place exchange reactions [11], multifunctional monolayers can be fabricated. This structural diversity enables particle surfaces to contain multiple targeting agents and/or chemotherapeutics. In addition the core in essence is non-toxic, biocompatible, and inert [12–14].
The diverse functional possibilities of AuNPs allows for a variety of approaches for DDS design. Hydrophobic drugs can be loaded onto AuNPs through non-covalent interactions, requiring no structural modification to the drug for drug release [15]. Likewise, covalent conjugation to the AuNP through cleavable linkages can be used to deliver prodrugs to the cell and the drug can then be released by external [16] or internal [17] stimuli. Regardless of the approach used, the tunability of the AuNP monolayer is crucial for internal or external release mechanisms.
The use of AuNPs for therapy, biosensing, and diagnostics has been reviewed [18–22]. This review will focus on the use of AuNPs as a viable DDS and the influence on the overall function provided by the monolayer.
2. Synthetic approaches for AuNP fabrication
The fabrication of AuNPs with varying core sizes makes them an appealing platform for DDSs. A variety of synthetic methods exist for the fabrication of core-shell AuNPs, as summarized in Table 1. The one-pot method of Brust and Schiffrin et al. allows for the rapid and scalable synthesis of monolayer protected AuNPs [23]. AuCl4− salts are reduced by NaBH4 in solution with the desired ligands. By changing the ligand to gold stoichiometry core sizes from 1.5 nm to 6 nm can be fabricated. To create larger particles citrate reduction of gold salts[24, 25] or ripening approaches [26] are widely used. Improved diversity of AuNPs is achieved by synthesizing a mixed monolayer by post-functionalization or directly functionalizing with appropriate ligands. A widely utilized method for the formation of mixed monolayer protected AuNPs is using a place-exchange reaction developed by Murray et al. [11]. In this method, ligands with thiol functionality exchange in equilibrium with the bound ligands of AuNPs. The tunability of the ligand structure allows for enhanced delivery applications, such as the use of poly(ethylene glycol) and oligo(ethylene glycol) moieties to create a more biocompatible particle [27–33].
Table 1.
Synthetic methods and capping agents for AuNPs of varying core sizes.
| Core | Synthetic methods | Capping agents | References |
|---|---|---|---|
| 1–2 nm | Reduction of AuCl(PPh3) with diborane of sodium borohydride | Phosphine | 10 |
| 1.5–5 nm | Biphasic reduction of thiol capping agents | Alkanethiol | 23 |
| 3.5–10 nm | Heat-induced size ripening method | Alkanethiol | 26 |
| 10–150 nm | Reduction of HAuCl4 with sodium citrate in water | Citrate | 24 |
3. Cell membrane penetration by gold nanoparticles
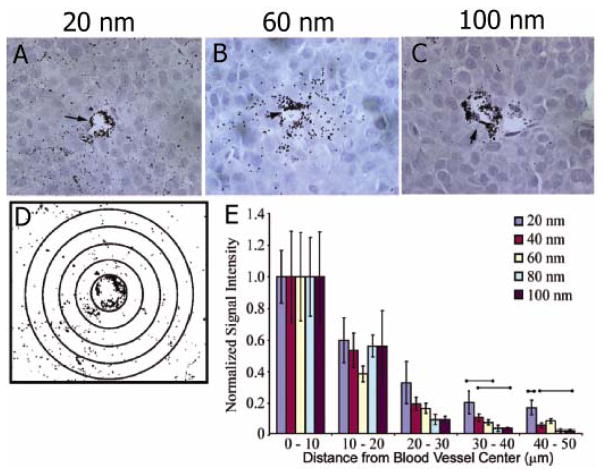
For a DDS to be effective, the interaction between cells and the delivery particles must be understood. Charge [34], size and surface functionality [35] affect the intracellular fate and cellular uptake of AuNPs. Rotello and Vachet have shown charge and hydrophobicity contributed to determining the cellular uptake of functionalized AuNPs [36]. Chan et al. have reported cellular uptake is likewise dependent on the size of nanoparticles [37]. In these studies, AuNPs ranging in size from 2–100 nm were coated with Herceptin and were tested for breast cell internalization mediated by the ErbB2 receptor. The most efficient cellular uptake was observed with particles ranging from 20–50 nm. Apoptosis was also enhanced by 40–50 nm particles. In vivo studies of passive targeting of tumors was also performed with AuNPs ranging from 10–100 nm [38]. The authors found smaller AuNPs rapidly diffused into the tumor matrix, whereas larger AuNPs stayed near the vasculature (Figure 1).
Figure 1.
Particle size-dependent permeation of the tumor interstitial space. (A–C) Histological samples were obtained for 20, 60, and 100 nm particle sizes at 8 h postinjection (HPI). (D) ImageJ software was used to generate contrast-enhanced images for densitometry analysis. (E) Densitometry signal was quantified at 10 μm distances away from blood vessel centers 8 HPI and was normalized to the signal at 0–10 _m. Reprinted with permission from Ref. 38.
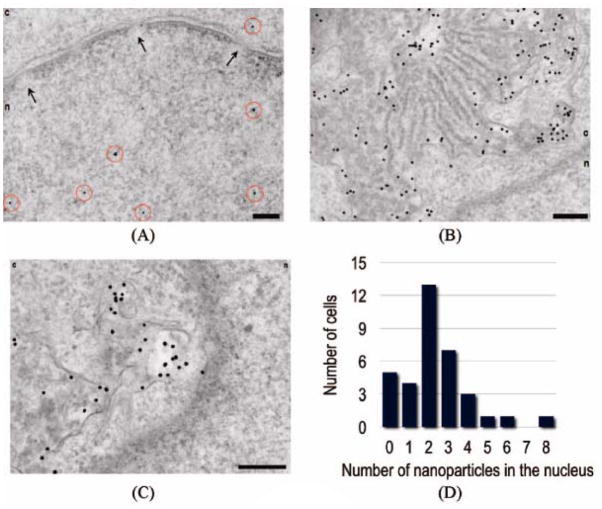
Stellacci et al. found ligand shell morphology affects cell membrane penetration of AuNPs [39]. It was shown that cytotoxic AuNPs with structured ligand shells could directly pass through the plasma membrane of cells without the creation of pores. Surface modifications to the ligand shell allow for targeting of specific organelles. Brust et al. utilized transmission electron microscopy to demonstrate that modifying the AuNP surface with cell penetrating peptides the nucleus and other organelles could be specifically targeted [40](Figure 2). Feldheim et al. have also shown nuclear targeting of AuNPs by modifying the surface with a nuclear localization sequence [41].
Figure 2.
Nuclear targeting (A) by PEG-modified nanoparticles functionalized with a combination of CPPs (2% TAT and 2% Pntn) and 2% NLS. Nanoparticles are highlighted by red circles. The nuclear envelope with nuclear pores (arrows) is clearly shown in this image. The nucleus is denoted n, and the cytosol c. Unusual perinuclear membranous structures (B and C) that are highly loaded with nanoparticles are typically also observed under these conditions. Nuclear targeting is enhanced in comparison with experiments in the absence of CPPs (D). Scale bars are 200 nm. Reprinted with permission from Ref. 40.
4. Drug delivery strategies using gold nanoparticle platforms
Drug release and transport are major factors for creating an efficient DDS. Nanocarriers can be loaded with drugs through non-covalent interactions or by covalent conjugation [42]. using a prodrug that is processed by the cell [43]. AuNPs provide an excellent platform for DDS design due to the functional versatility of their monolayers.
4-1. Photo-regulated release
Regulation of drug release is crucial for DDSs [5]. One useful approach for controlling the rate and site of release is to use an external stimulus to trigger release [44–49]. Photocleavable “cages” have been used to reduce the activity of a drug, with activation occurring upon uncaging [50, 51]. Nakanishi et al. have used this approach to develop a photoresponsive nanocarrier of amines[52]. Using near-UV irradiation, a carbamate linkage could be dissociated by the photocleavable reaction of the 2-nitrobenzyl group. They found histamine had no biological activity while caged but after irradiation it became active.
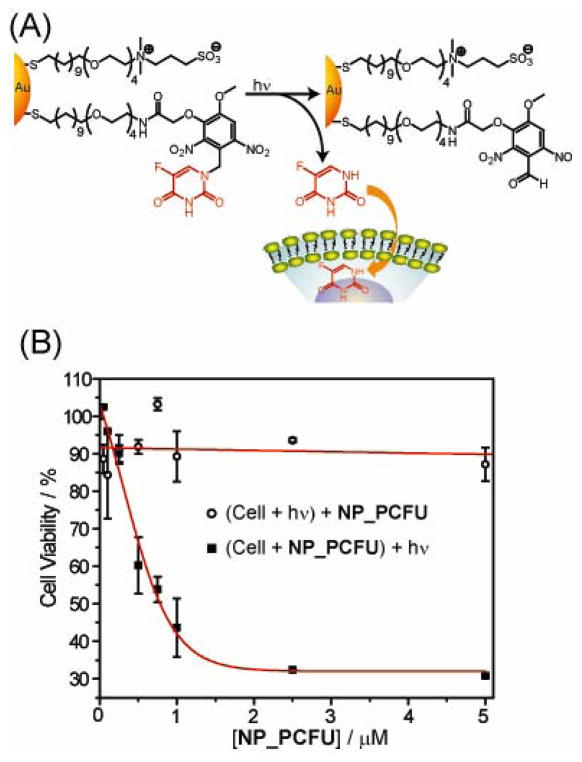
Rotello et al. have demonstrated an AuNP platform with a photo-cleavable o-nitrobenzyl ester moiety that upon light irradiation dissociates changing the surface potential to negative from positive, intracellularly releasing adsorbed DNA [16]. In further studies the authors observed light-controlled release of the anticancer drug 5-fluorouracil from AuNPs (Figure 3) [53]. The mixed monolayer of the AuNPs was composed of photocleavable moieties and zwitterionic ligands. Improved solubility and limited cellular uptake was achieved by the use of the zwitterionic ligand. Using near-UV irradiation (365 nm) the photocleavable orthonitrobenzyl group could efficiently cleave the 5-fluorouracil from the AuNP. The observed IC50 value on a per particle basis for the AuNP was 0.7 μM. No significant cell death was observed in cells treated with only light AuNPs or only light.
Figure 3.
(A) Photochemical reaction (365 nm) of Au_PCFU and delivery of payload to cell. (B) Cytotoxicity of different concentrations of Au_PCFU under uncaging and control conditions. The IC50 value was 0.7 μM per particle, 11.9 μM per drug.
4-2. Glutathione-mediated release in covalent conjugation
DDSs have been created utilizing glutathione (GSH) as an endogenous agent for drug release. These systems rely on the drastic difference between intracellular GSH concentrations (1–10 mM) [54, 55] and extracellular thiol concentrations (cysteine 8 μM, GSH 2 μM) [56, 57]. Disulfide exchange or place-exchange reactions with the intracellular GSH can release prodrugs bound to the AuNP. Also the monolayer of the AuNP limits reactivity with cysteine residues of proteins in the bloodstream [58–60].
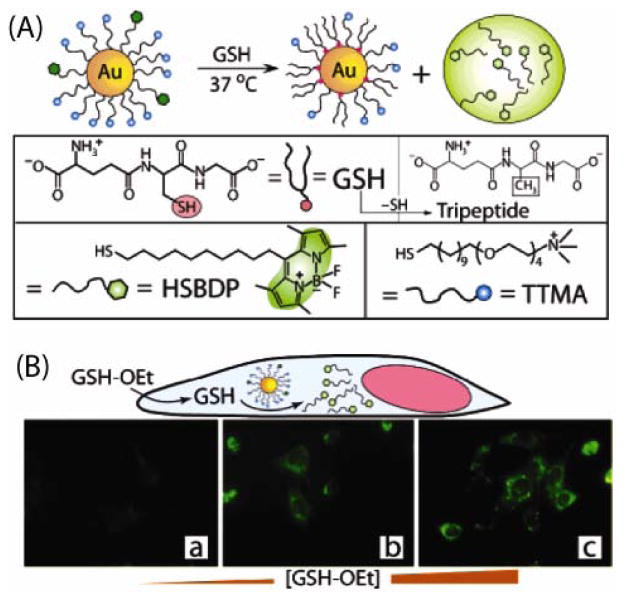
A DDS utilizing glutathione (GSH) for payload release was developed by Rotello et al. [17]. A mixed monolayer of fluorogenic ligands (HSBDP) and cationic ligands (TTMA) was attached to AuNPs with a core diameter of 2 nm (Figure 4). Cellular penetration was assisted by the TTMA ligands on the surface of the nanoparticle. When attached, the Au core quenches the fluorescence of the BODIPY moiety of the HSDBP [61, 62]. Fluorogenesis occurred after cellular uptake through the intracellular GSH in human liver cells (Hep G2) or GSH treatment in cuvette. Treatment of mouse embryonic fibroblast cells (containing greater than 50% lower intracellular GSH levels than Hep G2) with varying levels of glutathione monoester (GSH-OEt) verified GSH-mediated release of the dye. Increasing concentrations of GSH-OEt showed a dose dependent relationship in fluorescence signal. Regulation of intracellular GSH levels likewise controlled the effectiveness of AuNP-mediated DNA transfection [63].
Figure 4.
(A) Schematic illustration of GSH-mediated surface monolayer exchange reaction/payload release. (B) Fluorescence images of MEF cells displaying GSH-controlled release of the fluorophore after incubation with 0, 5, and 20 mM GSH-OEt.
The surface charge and monolayer structure of AuNPs heavily influence the rate of ligand-displacement by intracellular thiols (e.g. GSH), giving rise to a controlled release of payload [64, 65]. Kotov et al. observed the anti-proliferative effect against K-562 leukemia cells of 6-mercaptopurine-9-β-D-ribofuranoside was notably increased when attached to an AuNP in comparison to the free form drug [66]. Improved intracellular transport of the AuNPs preceding the GSH-mediated release in the lysosomes and cytoplasm was used to explain the enhancement.
4.3 Additional covalent attachment strategies
Enhanced selectivity and potency can be achieved by targeting overexpressed receptors in cancer cells. El-Sayed et al. observed selective delivery and enhanced potency of conjugated tamoxifen to their AuNPs [67]. The increased potency is attributed to an enhancement of cellular uptake of their AuNPs compared to the passive diffusion of the free drug. The binding of the estrogen receptor alpha in the plasma membrane facilitated improved selectivity for drug delivery. Alemzadeh et al. utilized the overexpressed folate-receptor in cancer cells to develop targeted delivery system for doxorubicin [68]. Folate-modified PEG ligands were conjugated to doxorubicin to comprise the monolayer of their AuNP. The AuNPs had increased cytotoxicity to cells with overexpression of folate-receptors and reduced cytotoxicity to healthy cells when compared to free doxorubicin.
Mukherjee et al. also developed a system to deliver the platinum containing drug cisplatin targeting the folate-receptor [69]. The delivery system targets cancer cells preferentially and enhances cytotoxicity. The cisplatin retains its cytotoxic effects while conjugated, and the folic acid protects healthy cells from the cisplatin. Lippard et al. combined DNA functionalized AuNPs with Pt(IV) prodrugs for a novel DDS [70]. After the Pt-DNA-AuNPs enters the cell the Pt(IV) is reduced to release cytotoxic cisplatin. The Pt(IV) species exhibit greater biological stability when compared to the more reactive Pt(II) species leading to less side effects. Wheate et. al observed enhanced cytotoxicity of oxaliplatin when tethered to AuNPs [71]. The tumor cell concentrations of oxaliplatin were greater for the AuNP delivered drug than when compared to the free drug.
4-4. Therapeutics incorporated into the monolayer of AuNPs
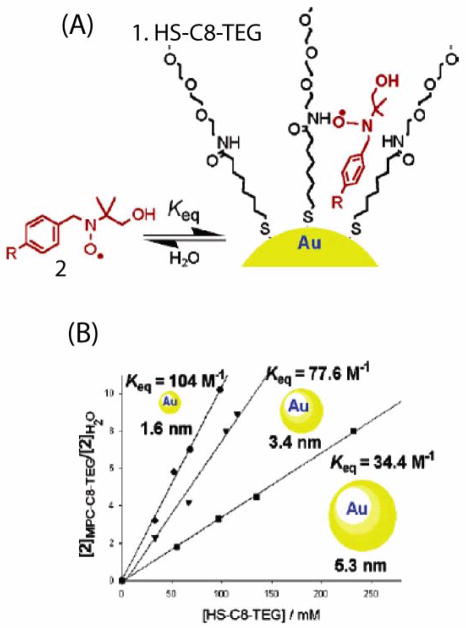
Encapsulating unmodified drugs into the monolayer of the AuNP non-covalently avoids potential issues associated with using a prodrug strategy. Using appropriate ligands, a hydrophobic environment is created to incorporate the drugs into the monolayer. The further one goes from the gold core, the smaller the ligand density becomes [72, 73]. Using EPR spectroscopy, Pasquato et al. observed the partitioning of radical, lipophilic probes between bulk water and the monolayer of an AuNP. As seen in Figure 5, they found that guest encapsulation was favored by the greater radial monolayers of smaller particle cores [74, 75].
Figure 5.
(A) Schematic representation of AuNP and the nitroxide probe inclusion. (B) Plot of the ratio between the concentration of 2 partitioned in the monolayer and that of the free species (● 1.6 nm; ▼ 3.4 nm; ■ 5.3 nm) as a function of [HS-C8-TEG] bound to the gold. Reprinted with permission from Ref. 75.
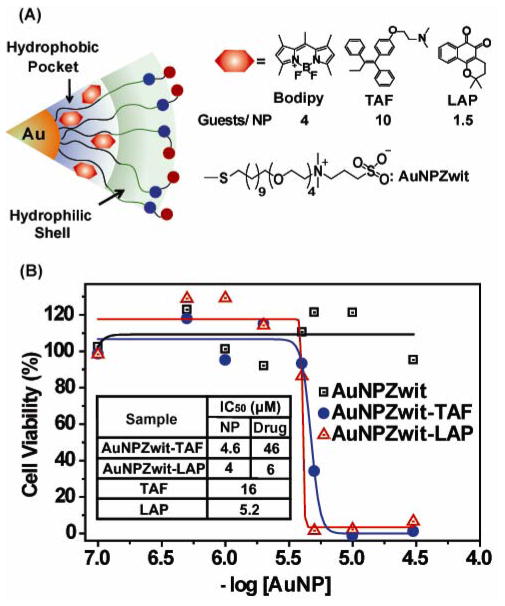
Rotello et al. fabricated a biocompatible AuNP to deliver drugs to cancer cells via their incorporation into the monolayer [76]. The 2.5 nm core AuNPs were functionalized with a hydrophobic alkanethiol interior and a tetra(ethylene glycol) (TEG) hydrophilic shell. The ligands possessed zwitterionic headgroup which minimized nonspecific binding with cell surface functionalities and biomacromolecules [77, 78] (Figure 6). Kinetically encapsulated in the monolayer, the hydrophobic payloads were stable in serum and buffer. Fluorescence microscopy, using a hydrophobic fluorophore, and drug efficacy measurements of therapeutics verified membrane-mediated diffusion into cells without cellular uptake of the particles. These DDS are great candidates for passive targeting utilizing the enhanced permeability and retention effect [79].
Figure 6.
(A) Structure of particles and guest compounds: Bodipy, TAF, and LAP, the number of encapsulated guests per particle (B) Cytotoxicity of AuNPZwit complexes measured by Alamar blue assay after 24 h incubation with MCF-7 cells. IC50 of AuNP (NP), equivalent drugs (Drug), and free drugs are shown in table.
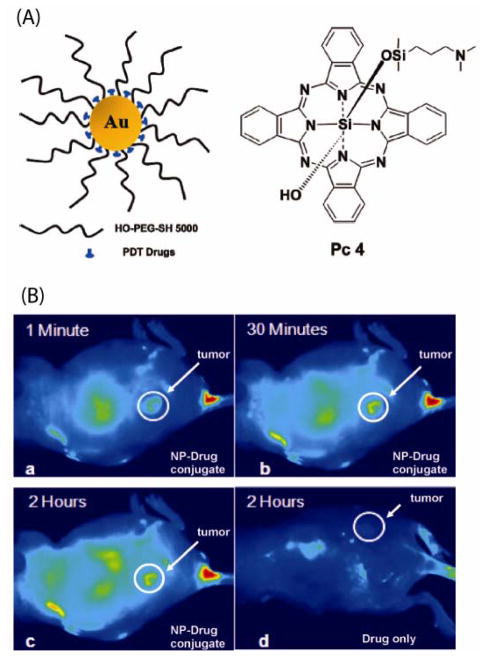
Inducing necrosis and apoptosis using reactive oxygen species is a potential strategy for therapeutics. Burda et al. utilized this strategy to develop a photodynamic therapy (PDT) with PEGylated AuNP-Pc4 (Si-phthalocyanine) [80]. The PEG ligands serve multiple purposes. First they inhibit non-specific binging to biomacromolecules and prevent colloidal aggregation. Theligands also, through Van der Waals interactions, encapsulate the phthalocyanine photosensitizing agent (Figure 7a). An efficient delivery process was verified by monitoring the release of Pc4 from the nanocarrier in vitro in a two-phase solution system and in vivo in cancer-bearing mice with enhanced accumulation of Pc4 in tumor sites. The Au NP-Pc4 conjugates decreased the time necessary for PDT from 2 days to 2 hours versus the free drug (Figure 7b).
Figure 7.
(A) Structure of the water-soluble Au NPs as a PDT drug delivery agent, Pc 4 structure (B) Fluorescence images of a tumor-bearing mouse after being injected with Au NP-Pc 4 conjugates in normal saline (0.9% NaCl, pH 7.2), (a) 1 min, (b) 30 min, and (c) 120 min after intravenous tail injection. Any bright signal is due to Pc 4 fluorescence. For comparison, a mouse that got only a Pc 4 formulation without the Au NP vector injected is shown in panel (d). No circulation of the drug in the body or into the tumor was detectable 2 h after injection without the Au NP as drug vector. Reprinted with permission from Ref. 80.
Kim et al. developed a DDS using non-covalently loaded anti-cancer drugs which are released by glutathione [15]. β-Lapachone, an anti-cancer drug, was encapsulated in the cyclodextrin moieties. Poly(ethylene glycol) was used to prevent degradation before delivery. The AuNPs were also functionalized with an anti-epidermal growth factor receptor antibody as a targeting agent. In addition to this, the targeting antibody increased the extent of apoptosis. Schoenfisch et al. have developed a pH responsive system which at acidic pHs releases nitric oxide from AuNPs [81]. This potentially gives the ability to control cellular processes such as immune response, angiogenesis, and vasodilation [82, 83]. Using a phosphate linker Hwu et al. conjugated paclitaxel to Fe3O4 particles and AuNPs [84]. Phosphodiesterase could then release the paclitaxel.
Summary
AuNPs show great potential for the creation of DDSs. Their stability, tunable monolayers, functional flexibility, low toxicity, and ability to control the release of drugs offer many possibilities for further development of DDSs. Additional investigations of these systems will be required to fully understand their pharmacokinetics, interactions with the immune system, and the extent of cytotoxicity due to surface and size of the AuNPs. Continued research into these nanoscale delivery vehicles will expand the understanding of the interactions of these materials with biological systems, and promoting the development of more effective DDSs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Allen TM, Cullis PR. Drug Delivery Systems: Entering the Mainstream. Science. (5665)(2004):303. 1818–1822. doi: 10.1126/science.1095833. [DOI] [PubMed] [Google Scholar]
- 2.Crampton HL, Simanek EE. Dendrimers as drug delivery vehicles: non-covalent interactions of bioactive compounds with dendrimers. Polymer International. 2007;56(4):489–496. doi: 10.1002/pi.2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee CC, MacKay JA, Frechet JMJ, Szoka FC. Designing dendrimers for biological applications. Nat Biotech. 2005;23(12):1517–1526. doi: 10.1038/nbt1171. [DOI] [PubMed] [Google Scholar]
- 4.Torchilin VP. Recent advances with liposomes as pharmaceutical carriers. Nat Rev Drug Discov. 2005;4(2):145–160. doi: 10.1038/nrd1632. [DOI] [PubMed] [Google Scholar]
- 5.Peer D, Karp JM, Hong S, Farokhzad OC, Margalit R, Langer R. Nanocarriers as an emerging platform for cancer therapy. Nat Nano. 2007;2(12):751–760. doi: 10.1038/nnano.2007.387. [DOI] [PubMed] [Google Scholar]
- 6.Davis ME, Chen Z, Shin DM. Nanoparticle therapeutics: an emerging treatment modality for cancer. Nat Rev Drug Discov. 2008;7(9):771–782. doi: 10.1038/nrd2614. [DOI] [PubMed] [Google Scholar]
- 7.Brannon-Peppas L, Blanchette JO. Nanoparticle and targeted systems for cancer therapy. Advanced Drug Delivery Reviews. 2004;56(11):1649–1659. doi: 10.1016/j.addr.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 8.Gibson JD, Khanal BP, Zubarev ER. Paclitaxel-Functionalized Gold Nanoparticles. Journal of the American Chemical Society. 2007;129(37):11653–11661. doi: 10.1021/ja075181k. [DOI] [PubMed] [Google Scholar]
- 9.Paciotti GF, Kingston DGI, Tamarkin L. Colloidal gold nanoparticles: a novel nanoparticle platform for developing multifunctional tumor-targeted drug delivery vectors. Drug Development Research. 2006;67(1):47–54. [Google Scholar]
- 10.Schmid G. Large clusters and colloids. Metals in the embryonic state. Chemical Reviews. 1992;92(8):1709–1727. [Google Scholar]
- 11.Templeton AC, Wuelfing WP, Murray RW. Monolayer-Protected Cluster Molecules. Accounts of Chemical Research. 1999;33(1):27–36. doi: 10.1021/ar9602664. [DOI] [PubMed] [Google Scholar]
- 12.Tsoli M, Kuhn H, Brandau W, Esche H, Schmid G. Cellular Uptake and Toxicity of Au55 Clusters. Small. 2005;1(8–9):841–844. doi: 10.1002/smll.200500104. [DOI] [PubMed] [Google Scholar]
- 13.Bhattacharya R, Mukherjee P. Biological properties of “naked” metal nanoparticles. Advanced Drug Delivery Reviews. 2008;60(11):1289–1306. doi: 10.1016/j.addr.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 14.Connor Ellen E, Mwamuka J, Gole A, Murphy Catherine J, Wyatt Michael D. Gold Nanoparticles Are Taken Up by Human Cells but Do Not Cause Acute Cytotoxicity 13. Small. 2005;1(3):325–327. doi: 10.1002/smll.200400093. [DOI] [PubMed] [Google Scholar]
- 15.Park C, Youn H, Kim H, Noh T, Kook YH, Oh ET, Park HJ, Kim C. Cyclodextrin-covered gold nanoparticles for targeted delivery of an anti-cancer drug. Journal of Materials Chemistry. 2009;19(16):2310–2315. [Google Scholar]
- 16.Han G, You C-C, Kim B-j, Turingan RS, Forbes NS, Martin CT, Rotello VM. Light-Regulated Release of DNA and Its Delivery to Nuclei by Means of Photolabile Gold Nanoparticles 13. Angewandte Chemie International Edition. 2006;45(19):3165–3169. doi: 10.1002/anie.200600214. [DOI] [PubMed] [Google Scholar]
- 17.Hong R, Han G, Fernández JM, Kim B-j, Forbes NS, Rotello VM. Glutathione-Mediated Delivery and Release Using Monolayer Protected Nanoparticle Carriers. Journal of the American Chemical Society. 2006;128(4):1078–1079. doi: 10.1021/ja056726i. [DOI] [PubMed] [Google Scholar]
- 18.Murphy CJ, Gole AM, Stone JW, Sisco PN, Alkilany AM, Goldsmith EC, Baxter SC. Gold Nanoparticles in Biology: Beyond Toxicity to Cellular Imaging. Accounts of Chemical Research. 2008;41(12):1721–1730. doi: 10.1021/ar800035u. [DOI] [PubMed] [Google Scholar]
- 19.Daniel MC, Astruc D. Gold Nanoparticles: Assembly, Supramolecular Chemistry, Quantum-Size-Related Properties, and Applications toward Biology, Catalysis, and Nanotechnology. Chemical Reviews. 2003;104(1):293–346. doi: 10.1021/cr030698+. [DOI] [PubMed] [Google Scholar]
- 20.Rosi NL, Mirkin CA. Nanostructures in Biodiagnostics. Chemical Reviews. 2005;105(4):1547–1562. doi: 10.1021/cr030067f. [DOI] [PubMed] [Google Scholar]
- 21.Boisselier E, Astruc D. Gold nanoparticles in nanomedicine: preparations, imaging, diagnostics, therapies and toxicity. Chemical Society Reviews. 2009;38(6):1759–1782. doi: 10.1039/b806051g. [DOI] [PubMed] [Google Scholar]
- 22.De M, Ghosh PS, Rotello VM. Applications of Nanoparticles in Biology. Advanced Materials. 2008;20(22):4225–4241. [Google Scholar]
- 23.Mathias Brust MW, Bethell Donald, Schiffrin David J, Whyman Robin. Synthesis of thiol-derivatised gold nanoparticles in a two-phase Liquid–Liquid system. J Chem Soc, Chem Commun. 1994:801–802. [Google Scholar]
- 24.Turkevich J, Stevenson PC, Hillier J. A study of the nucleation and growth processes in the synthesis of colloidal gold. Discuss Faraday Soc. 1951:55–75. [Google Scholar]
- 25.Grabar KC, Freeman RG, Hommer MB, Natan MJ. Preparation and Characterization of Au Colloid Monolayers. Analytical Chemistry. 1995;67(4):735–743. [Google Scholar]
- 26.Teranishi T, Hasegawa S, Shimizu T, Miyake M. Heat-Induced Size Evolution of Gold Nanoparticles in the Solid State. Advanced Materials. 2001;13(22):1699–1701. [Google Scholar]
- 27.Khalil H, Mahajan D, Rafailovich M, Gelfer M, Pandya K. Synthesis of Zerovalent Nanophase Metal Particles Stabilized with Poly(ethylene glycol) Langmuir. 2004;20(16):6896–6903. doi: 10.1021/la0497402. [DOI] [PubMed] [Google Scholar]
- 28.Otsuka H, Nagasaki Y, Kataoka K. PEGylated nanoparticles for biological and pharmaceutical applications. Advanced Drug Delivery Reviews. 2003;55(3):403–419. doi: 10.1016/s0169-409x(02)00226-0. [DOI] [PubMed] [Google Scholar]
- 29.Otsuka H, Akiyama Y, Nagasaki Y, Kataoka K. Quantitative and Reversible Lectin-Induced Association of Gold Nanoparticles Modified with _-Lactosyl-_-mercapto-poly(ethylene glycol) Journal of the American Chemical Society. 2001;123(34):8226–8230. doi: 10.1021/ja010437m. [DOI] [PubMed] [Google Scholar]
- 30.Takae S, Akiyama Y, Otsuka H, Nakamura T, Nagasaki Y, Kataoka K. Ligand Density Effect on Biorecognition by PEGylated Gold Nanoparticles: Regulated Interaction of RCA120 Lectin with Lactose Installed to the Distal End of Tethered PEG Strands on Gold Surface. Biomacromolecules. 2005;6(2):818–824. doi: 10.1021/bm049427e. [DOI] [PubMed] [Google Scholar]
- 31.Ishii T, Otsuka H, Kataoka K, Nagasaki Y. Preparation of Functionally PEGylated Gold Nanoparticles with Narrow Distribution through Autoreduction of Auric Cation by _-Biotinyl-PEG-block-[poly(2-(N, N-dimethylamino)ethyl methacrylate)] Langmuir. 2003;20(3):561–564. doi: 10.1021/la035653i. [DOI] [PubMed] [Google Scholar]
- 32.Olivier JC, Huertas R, Lee HJ, Calon F, Pardridge WM. Synthesis of Pegylated Immunonanoparticles. Pharmaceutical Research. 2002;19(8):1137–1143. doi: 10.1023/a:1019842024814. [DOI] [PubMed] [Google Scholar]
- 33.Shimmin RG, Schoch AB, Braun PV. Polymer Size and Concentration Effects on the Size of Gold Nanoparticles Capped by Polymeric Thiols. Langmuir. 2004;20(13):5613–5620. doi: 10.1021/la036365p. [DOI] [PubMed] [Google Scholar]
- 34.Cho EC, Xie J, Wurm PA, Xia Y. Understanding the Role of Surface Charges in Cellular Adsorption versus Internalization by Selectively Removing Gold Nanoparticles on the Cell Surface with a I2/KI Etchant. Nano Letters. 2009;9(3):1080–1084. doi: 10.1021/nl803487r. [DOI] [PubMed] [Google Scholar]
- 35.Ferrari M. Nanogeometry: Beyond drug delivery. Nat Nano. 2008;3(3):131–132. doi: 10.1038/nnano.2008.46. [DOI] [PubMed] [Google Scholar]
- 36.Zhu ZJ, Ghosh PS, Miranda OR, Vachet RW, Rotello VM. Multiplexed Screening of Cellular Uptake of Gold Nanoparticles Using Laser Desorption/Ionization Mass Spectrometry. Journal of the American Chemical Society. 2008;130(43):14139–14143. doi: 10.1021/ja805392f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jiang W, KimBetty YS, Rutka JT, ChanWarren CW. Nanoparticle-mediated cellular response is size-dependent. Nat Nano. 2008;3(3):145–150. doi: 10.1038/nnano.2008.30. [DOI] [PubMed] [Google Scholar]
- 38.Perrault SD, Walkey C, Jennings T, Fischer HC, Chan WCW. Mediating Tumor Targeting Efficiency of Nanoparticles Through Design. Nano Letters. 2009;9(5):1909–1915. doi: 10.1021/nl900031y. [DOI] [PubMed] [Google Scholar]
- 39.Verma A, Uzun O, Hu Y, Hu Y, Han HS, Watson N, Chen S, Irvine DJ, Stellacci F. Surface-structure-regulated cell-membrane penetration by monolayer-protected nanoparticles. Nat Mater. 2008;7(7):588–595. doi: 10.1038/nmat2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nativo P, Prior IA, Brust M. Uptake and Intracellular Fate of Surface-Modified Gold Nanoparticles. ACS Nano. 2008;2(8):1639–1644. doi: 10.1021/nn800330a. [DOI] [PubMed] [Google Scholar]
- 41.Tkachenko AG, Xie H, Coleman D, Glomm W, Ryan J, Anderson MF, Franzen S, Feldheim DL. Multifunctional Gold Nanoparticle-Peptide Complexes for Nuclear Targeting. Journal of the American Chemical Society. 2003;125(16):4700–4701. doi: 10.1021/ja0296935. [DOI] [PubMed] [Google Scholar]
- 42.Torchilin VP. Structure and design of polymeric surfactant-based drug delivery systems. Journal of Controlled Release. 2001;73(2–3):137–172. doi: 10.1016/s0168-3659(01)00299-1. [DOI] [PubMed] [Google Scholar]
- 43.Morgan MT, Nakanishi Y, Kroll DJ, Griset AP, Carnahan MA, Wathier M, Oberlies NH, Manikumar G, Wani MC, Grinstaff MW. Dendrimer-Encapsulated Camptothecins: Increased Solubility, Cellular Uptake, and Cellular Retention Affords Enhanced Anticancer Activity In vitro. Cancer Res. 2006;66(24):11913–11921. doi: 10.1158/0008-5472.CAN-06-2066. [DOI] [PubMed] [Google Scholar]
- 44.Kim HJ, Matsuda H, Zhou H, Honma I. Ultrasound-Triggered Smart Drug Release from a Poly(dimethylsiloxane)- Mesoporous Silica Composite. Advanced Materials. 2006;18(23):3083–3088. [Google Scholar]
- 45.Park C, Lim J, Yun M, Kim C. Photoinduced Release of Guest Molecules by Supramolecular Transformation of Self-Assembled Aggregates Derived from Dendrons 13. Angewandte Chemie International Edition. 2008;47(16):2959–2963. doi: 10.1002/anie.200705271. [DOI] [PubMed] [Google Scholar]
- 46.Park H, Yang J, Seo S, Kim K, Suh J, Kim D, Haam S, Yoo KH. Multifunctional Nanoparticles for Photothermally Controlled Drug Delivery and Magnetic Resonance Imaging Enhancement 13. Small. 2008;4(2):192–196. doi: 10.1002/smll.200700807. [DOI] [PubMed] [Google Scholar]
- 47.Giri S, Trewyn BG, Stellmaker MP, Lin VSY. Stimuli-Responsive Controlled-Release Delivery System Based on Mesoporous Silica Nanorods Capped with Magnetic Nanoparticles 13. Angewandte Chemie International Edition. 2005;44(32):5038–5044. doi: 10.1002/anie.200501819. [DOI] [PubMed] [Google Scholar]
- 48.Rooseboom M, Commandeur JNM, Vermeulen NPE. Enzyme-Catalyzed Activation of Anticancer Prodrugs. Pharmacological Reviews. 2004;56(1):53–102. doi: 10.1124/pr.56.1.3. [DOI] [PubMed] [Google Scholar]
- 49.Kam NWS, Liu Z, Dai H. Functionalization of Carbon Nanotubes via Cleavable Disulfide Bonds for Efficient Intracellular Delivery of siRNA and Potent Gene Silencing. Journal of the American Chemical Society. 2005;127(36):12492–12493. doi: 10.1021/ja053962k. [DOI] [PubMed] [Google Scholar]
- 50.Mayer G, Heckel A. Biologically Active Molecules with a “Light Switch”. Angewandte Chemie International Edition. 2006;45(30):4900–4921. doi: 10.1002/anie.200600387. [DOI] [PubMed] [Google Scholar]
- 51.McCoy CP, Rooney C, Edwards CR, Jones DS, Gorman SP. Light-Triggered Molecule-Scale Drug Dosing Devices. Journal of the American Chemical Society. 2007;129(31):9572–9573. doi: 10.1021/ja073053q. [DOI] [PubMed] [Google Scholar]
- 52.Nakanishi J, Nakayama H, Shimizu T, Ishida H, Kikuchi Y, Yamaguchi K, Horiike Y. Light-Regulated Activation of Cellular Signaling by Gold Nanoparticles That Capture and Release Amines. Journal of the American Chemical Society. 2009;131(11):3822–3823. doi: 10.1021/ja809236a. [DOI] [PubMed] [Google Scholar]
- 53.Agasti SS, Chompoosor A, You CC, Ghosh P, Kim CK, Rotello VM. Photoregulated Release of Caged Anticancer Drugs from Gold Nanoparticles. Journal of the American Chemical Society. 2009;131(16):5728–5729. doi: 10.1021/ja900591t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Anderson ME. Glutathione: an overview of biosynthesis and modulation. Chemico-Biological Interactions. 1998;111–112:1–14. doi: 10.1016/s0009-2797(97)00146-4. [DOI] [PubMed] [Google Scholar]
- 55.Sies H. Glutathione and its role in cellular functions. Free Radical Biology and Medicine. 1999;27(9–10):916–921. doi: 10.1016/s0891-5849(99)00177-x. [DOI] [PubMed] [Google Scholar]
- 56.Jones DP, Carlson JL, Samiec PS, Sternberg P, Mody VC, Reed RL, Brown LAS. Glutathione measurement in human plasma: Evaluation of sample collection, storage and derivatization conditions for analysis of dansyl derivatives by HPLC. Clinica Chimica Acta. 1998;275(2):175–184. doi: 10.1016/s0009-8981(98)00089-8. [DOI] [PubMed] [Google Scholar]
- 57.Jones DP, Carlson JL, Mody VC, Cai J, Lynn MJ, Sternberg P. Redox state of glutathione in human plasma. Free Radical Biology and Medicine. 2000;28(4):625–635. doi: 10.1016/s0891-5849(99)00275-0. [DOI] [PubMed] [Google Scholar]
- 58.McIntosh CM, Esposito EA, Boal AK, Simard JM, Martin CT, Rotello VM. Inhibition of DNA Transcription Using Cationic Mixed Monolayer Protected Gold Clusters. Journal of the American Chemical Society. 2001;123(31):7626–7629. doi: 10.1021/ja015556g. [DOI] [PubMed] [Google Scholar]
- 59.Verma A, Simard JM, Worrall JWE, Rotello VM. Tunable Reactivation of Nanoparticle-Inhibited b-Galactosidase by Glutathione at Intracellular Concentrations. Journal of the American Chemical Society. 2004;126(43):13987–13991. doi: 10.1021/ja046572r. [DOI] [PubMed] [Google Scholar]
- 60.Ghosh P, Han G, De M, Kim CK, Rotello VM. Gold nanoparticles in delivery applications. Advanced Drug Delivery Reviews. 2008;60(11):1307–1315. doi: 10.1016/j.addr.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 61.Dulkeith E, Morteani AC, Niedereichholz T, Klar TA, Feldmann J, Levi SA, van Veggel FCJM, Reinhoudt DN, Möller M, Gittins DI. Fluorescence Quenching of Dye Molecules near Gold Nanoparticles: Radiative and Nonradiative Effects. Physical Review Letters. 2002;89(20):203002. doi: 10.1103/PhysRevLett.89.203002. [DOI] [PubMed] [Google Scholar]
- 62.Sapsford KE, Berti L, Medintz IL. Materials for Fluorescence Resonance Energy Transfer Analysis: Beyond Traditional Donor-Acceptor Combinations. Angewandte Chemie International Edition. 2006;45(28):4562–4589. doi: 10.1002/anie.200503873. [DOI] [PubMed] [Google Scholar]
- 63.Ghosh PS, Kim CK, Han G, Forbes NS, Rotello VM. Efficient Gene Delivery Vectors by Tuning the Surface Charge Density of Amino Acid-Functionalized Gold Nanoparticles. ACS Nano. 2008;2(11):2213–2218. doi: 10.1021/nn800507t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Agasti SS, You CC, Arumugam P, Rotello VM. Structural control of the monolayer stability of water-soluble gold nanoparticles. Journal of Materials Chemistry. 2008;18(1):70–73. [Google Scholar]
- 65.Chompoosor A, Han G, Rotello VM. Charge Dependence of Ligand Release and Monolayer Stability of Gold Nanoparticles by Biogenic Thiols. Bioconjugate Chemistry. 2008;19(7):1342–1345. doi: 10.1021/bc8000694. [DOI] [PubMed] [Google Scholar]
- 66.Podsiadlo P, Sinani VA, Bahng JH, Kam NWS, Lee J, Kotov NA. Gold Nanoparticles Enhance the Anti-Leukemia Action of a 6-Mercaptopurine Chemotherapeutic Agent. Langmuir. 2007;24(2):568–574. doi: 10.1021/la702782k. [DOI] [PubMed] [Google Scholar]
- 67.Dreaden EC, Mwakwari SC, Sodji QH, Oyelere AK, El-Sayed MA. Tamoxifen-Poly(ethylene glycol)-Thiol Gold Nanoparticle Conjugates: Enhanced Potency and Selective Delivery for Breast Cancer Treatment. Bioconjugate Chemistry. 2009;20(12):2247–2253. doi: 10.1021/bc9002212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Asadishad B, Vossoughi M, Alemzadeh I. Folate-Receptor-Targeted Delivery of Doxorubicin Using Polyethylene Glycol-Functionalized Gold Nanoparticles. Industrial & Engineering Chemistry Research. 49(4):1958–1963. [Google Scholar]
- 69.Patra CR, Bhattacharya R, Mukherjee P. Fabrication and functional characterization of goldnanoconjugates for potential application in ovarian cancer. Journal of Materials Chemistry. 20(3):547–554. doi: 10.1039/b913224d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dhar S, Daniel WL, Giljohann DA, Mirkin CA, Lippard SJ. Polyvalent Oligonucleotide Gold Nanoparticle Conjugates as Delivery Vehicles for Platinum(IV) Warheads. Journal of the American Chemical Society. 2009;131(41):14652–14653. doi: 10.1021/ja9071282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brown SD, Nativo P, Smith J-A, Stirling D, Edwards PR, Venugopal B, Flint DJ, Plumb JA, Graham D, Wheate NJ. Gold Nanoparticles for the Improved Anticancer Drug Delivery of the Active Component of Oxaliplatin. Journal of the American Chemical Society. 132(13):4678–4684. doi: 10.1021/ja908117a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Love JC, Estroff LA, Kriebel JK, Nuzzo RG, Whitesides GM. Self-Assembled Monolayers of Thiolates on Metals as a Form of Nanotechnology. Chemical Reviews. 2005;105(4):1103–1170. doi: 10.1021/cr0300789. [DOI] [PubMed] [Google Scholar]
- 73.Hostetler MJ, Stokes JJ, Murray RW. Infrared Spectroscopy of Three-Dimensional Self-Assembled Monolayers: N-Alkanethiolate Monolayers on Gold Cluster Compounds. Langmuir. 1996;12(15):3604–3612. [Google Scholar]
- 74.Lucarini M, Franchi P, Pedulli GF, Pengo P, Scrimin P, Pasquato L. EPR Study of Dialkyl Nitroxides as Probes to Investigate the Exchange of Solutes between the Ligand Shell of Monolayers of Protected Gold Nanoparticles and Aqueous Solutions. Journal of the American Chemical Society. 2004;126(30):9326–9329. doi: 10.1021/ja048554f. [DOI] [PubMed] [Google Scholar]
- 75.Lucarini M, Franchi P, Pedulli GF, Gentilini C, Polizzi S, Pengo P, Scrimin P, Pasquato L. Effect of Core Size on the Partition of Organic Solutes in the Monolayer of Water-Soluble Nanoparticles: An ESR Investigation. Journal of the American Chemical Society. 2005;127(47):16384–16385. doi: 10.1021/ja0560534. [DOI] [PubMed] [Google Scholar]
- 76.Kim CK, Ghosh P, Pagliuca C, Zhu ZJ, Menichetti S, Rotello VM. Entrapment of Hydrophobic Drugs in Nanoparticle Monolayers with Efficient Release into Cancer Cells. Journal of the American Chemical Society. 2009;131(4):1360–1361. doi: 10.1021/ja808137c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jin Q, Xu JP, Ji J, Shen JC. Zwitterionic phosphorylcholine as a better ligand for stabilizing large biocompatible gold nanoparticles. Chemical Communications. 2008;(26):3058–3060. doi: 10.1039/b801959b. [DOI] [PubMed] [Google Scholar]
- 78.Rouhana LL, Jaber JA, Schlenoff JB. Aggregation-Resistant Water-Soluble Gold Nanoparticles. Langmuir. 2007;23(26):12799–12801. doi: 10.1021/la702151q. [DOI] [PubMed] [Google Scholar]
- 79.D’Emanuele A, Attwood D. Dendrimer-drug interactions. Advanced Drug Delivery Reviews. 2005;57(15):2147–2162. doi: 10.1016/j.addr.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 80.Cheng Y, Samia AC, Meyers JD, Panagopoulos I, Fei B, Burda C. Highly Efficient Drug Delivery with Gold Nanoparticle Vectors for in Vivo Photodynamic Therapy of Cancer. Journal of the American Chemical Society. 2008;130(32):10643–10647. doi: 10.1021/ja801631c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Polizzi MA, Stasko NA, Schoenfisch MH. Water-Soluble Nitric Oxide-Releasing Gold Nanoparticles. Langmuir. 2007;23(9):4938–4943. doi: 10.1021/la0633841. [DOI] [PubMed] [Google Scholar]
- 82.Yang Q, Wang S, Fan P, Wang L, Di Y, Lin K, Xiao FS. pH-Responsive Carrier System Based on Carboxylic Acid Modified Mesoporous Silica and Polyelectrolyte for Drug Delivery. Chemistry of Materials. 2005;17(24):5999–6003. [Google Scholar]
- 83.Mocellin S, Bronte V, Nitti D. Nitric oxide, a double edged sword in cancer biology: Searching for therapeutic opportunities. Medicinal Research Reviews. 2007;27(3):317–352. doi: 10.1002/med.20092. [DOI] [PubMed] [Google Scholar]
- 84.Hwu JR, Lin YS, Josephrajan T, Hsu MH, Cheng FY, Yeh CS, Su WC, Shieh DB. Targeted Paclitaxel by Conjugation to Iron Oxide and Gold Nanoparticles. Journal of the American Chemical Society. 2008;131(1):66–68. doi: 10.1021/ja804947u. [DOI] [PubMed] [Google Scholar]