Abstract
Purpose
To determine (a) changes in the Tinnitus Handicap Questionnaire (THQ) for patients using cochlear implants, (b) differences between patients who receive total or partial relief, and (c) identifiable characteristics of those who report tinnitus after implantation.
Method
Pre- and postoperatively, 244 adults were administered the THQ when they reported tinnitus.
Results
Of the 153 patients who had tinnitus preoperatively, 94 (61%) patients reported total suppression and 59 (39%) reported a partial reduction. In 91 patients who did not have tinnitus before implantation, 11 (12%) reported tinnitus postimplantation. The THQ score decreased from 41% preimplant to 30% postimplant. The largest reductions involved social handicap and hearing. Patients with a more severe hearing loss might be more likely to experience an exacerbation of their tinnitus. We were not able to clearly identify differences between patients who received total or partial relief and the characteristics of patients who reported tinnitus after implantation. Those who acquired tinnitus had the shortest duration hearing loss (5.6 years) and were the oldest (63 years). The average THQ score of patients getting tinnitus was 29%.
Conclusions
Most tinnitus patients benefit from receiving a cochlear implant.
Keywords: tinnitus, cochlear implant, Tinnitus Handicap Questionnaire, electrical tinnitus suppression
Electrical stimulation of the inner ear can effectively suppress tinnitus for many cochlear implant (CI) patients; the reported efficacy rate varies from about 46% to 93% (Demajumdar, Stoddart, Donaldson, & Proops, 1999; Di Nardo et al., 2007; Gibson, Aran, & Dauman, 1992; Ito, 1997; Miyamoto, Wynne, McKnight, & Bichey, 1997; Mo, Harris, & Lindbaek, 2002; Quaranta, Fernandez-Vega, D’elia, Filipo, & Quaranta, 2008; Tyler, 1994; Tyler & Kelsay, 1990). However, reviews by Dauman et al. (2000), Rubinstein, Tyler, Johnson, and Brown (2003), Rubinstein, Wilson, Finley, and Abbas (1999), Quaranta, Wagstaff, and Baguley (2004), and Baguley and Atlas (2007) have questioned the nature of tinnitus reduction by electrical stimulation.
Although previous studies have employed categorical ratings of the effect of CIs on perceived tinnitus severity, those data have not addressed specific aspects of benefit, nor have they provided an indication of any gradation of benefit. Other studies have provided category visual analog scales or attempted interval visual analog or magnitude estimation scales (e.g., Newman, Jacobson, & Spitzer, 1996). These metrics have the potential to distinguish between those who receive total relief of their tinnitus and those who receive partial relief. However, no study has attempted to explore differences between these two groups. It is also noteworthy that most of those studies that have used visual analog or magnitude estimation scales have been limited to questions regarding tinnitus loudness or annoyance.
There has been little attempt to explore a CI’s effect on the reactions patients can have to their tinnitus. We have characterized the handicapping nature of tinnitus in four broad categories (based on Tyler, 2006): Tinnitus can have an impact on (a) thoughts and emotions, (b) hearing, (c) sleep, and (d) concentration. CI users typically receive substantial benefit in hearing through use of their CIs. Therefore, while they might believe their tinnitus is reduced, the real effect may be a substantial improvement in their hearing.
We also think that previous studies have paid insufficient attention to those patients whose tinnitus is made worse by cochlear implantation. This group is of interest as attempts are made to develop a clinical instrument to electrically suppress tinnitus.
It has been known for many years that tinnitus involves both the peripheral and central auditory mechanism (Eggermont & Roberts, 2004; Kiang, Moson, & Levine, 1970; Salvi, Wang, & Powers, 1996; Tyler, 1981, 2006). There are several ways that tinnitus might be suppressed by peripheral electrical stimulation (see Tyler et al., 2008, for a review). For example, CI stimulation might contribute to the “reorganization” of a cortical representation of tinnitus (Giraud, Price, Graham, & Frackowiak, 2001; Kral & Tillein, 2006; Muhlnickel, Ebert, Taub, & Flor, 1998).
The aims of this study were:
to document changes in the Tinnitus Handicap Questionnaire (THQ) results for patients using CIs;
to make an initial attempt at determining what differences might exist prior to implantation between tinnitus patients who receive total or partial relief from their CI;
to determine if we could preoperatively identify any characteristics of CI users who develop tinnitus as a result of implantation.
Method
Our primary measure was the THQ (Kuk, Tyler, Russell, & Jordan, 1990; see Appendix). Specifically, we used the total THQ score, the Factor 1 (social, emotional, and behavioral effects) score, and the Factor 2 (tinnitus and hearing) score. The THQ was developed and validated with great rigor and is used widely (see Tyler, 1993). The questions evolved from the earlier work by Tyler and Baker (1983) in which tinnitus patients were asked to list the problems they felt were important. In an initial study, responses from 87 questions were evaluated on 100 patients. In a secondary study, the final 27-question version was administered to 275 patients. Its validity, factor structure, and reliability have been independently evaluated (Newman, Wharton, & Jacobson, 1995). As noted by Newman et al. (1995), “This Tinnitus Handicap Questionnaire is broad in scope” (p. 718), and “our data suggest the total questionnaire, as well as factors 1 and 2, can be used as an index of change in self-perceived tinnitus handicap following medical (e.g., drug trials), surgical (e.g., vascular decompression), or rehabilitative (e.g., tinnitus masking devices, counseling) treatment” (p. 722). Unlike some other questionnaires (e.g., The Tinnitus Handicap Inventory; Newman et al., 1996), the THQ scores each question from 0 to 100, enabling each question to be used as a sensitive ordinal scale that can be scored independently.
Second, in addition to the two factors recommended for use by Kuk et al. (1990; three factors were identified, but the third was deemed unreliable), we have grouped some of the questions to produce exploratory subscale scores intended to identify additional group differences. In addition to using the total, Factor 1, and Factor 2 scores, we explore some additional metrics using individual questions that are scored on a scale from 0 to 100 (0 indicating no handicap, and 100 indicating the severe handicap). This is equivalent to the approach used by previous studies employing visual analog scales or magnitude estimation. The use of individual questions from a larger questionnaire has been reported previously by others (e.g., with the Speech, Spatial and Qualities of Hearing Questionnaire; Gatehouse & Noble, 2004). One of the advantages of using the 0–100 magnitude estimation procedure is that it offers greater resolution than 3-, 5-, or 7-point scales.
In the present study, while the subscales represent secondary, exploratory variables, they might provide useful clues about the effects of CIs on tinnitus. Reliability of the three subscales among 153 patients was assessed by performing Cronbach’s alpha (α). For the Social subscale (combining Questions 1, 12, 15, and 20), α = 0.84; for the Emotional subscale (combining Questions 11, 13, 18, 22, 24, and 27), α = 0.94; and for the Physical subscale (Items 9, 14, 16, 17, and 19), α = 0.88; this indicates good reliability for each of the three subscales. We also obtained some basic tinnitus biographical data, modeled after the questionnaire administered by Stouffer and Tyler (1990) to 528 tinnitus patients.
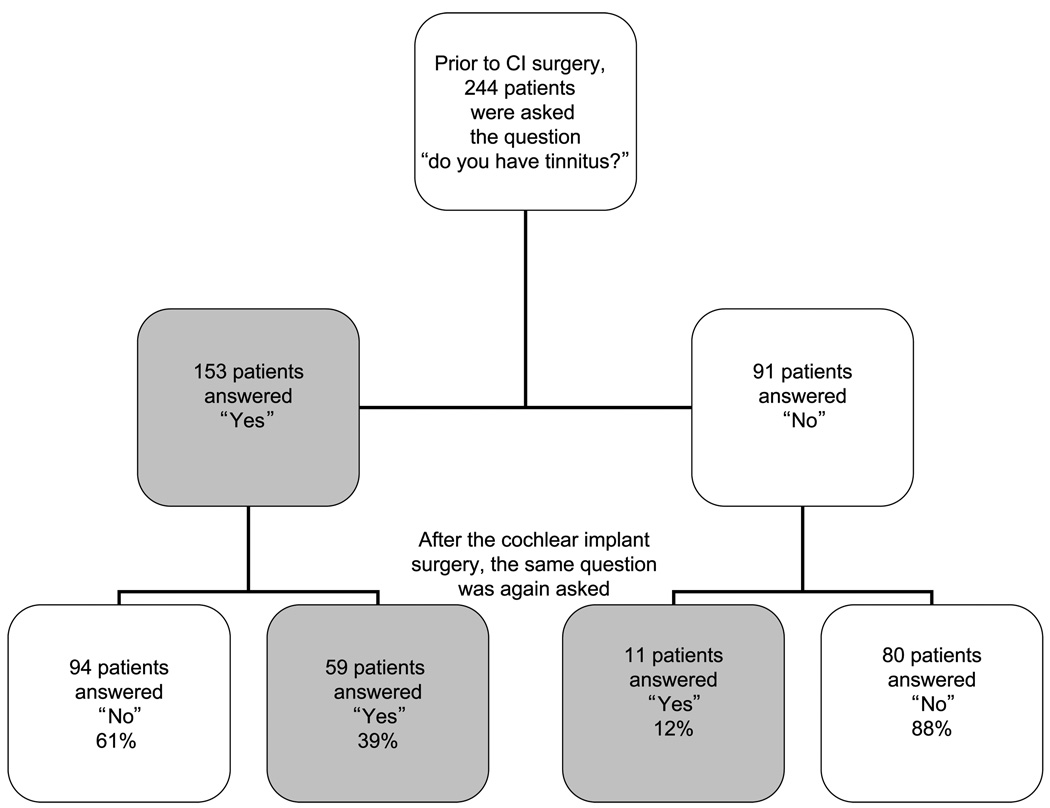
Between April 1981 and July 2007, 525 adult patients received CIs at the University of Iowa. Figure 1 shows an overall schema of the grouping of the patients and the order of questionnaire administration, and identifies the patient groups used in each of our comparisons. All patients in this population had a multichannel CI. Before cochlear implantation, 244 patients were asked the question “Do you have tinnitus?” Those who responded positively were asked to complete the THQ. Of the 244 who were asked the question “Do you have tinnitus?” 153 patients answered affirmatively (153/244 = 63%). Of those 153 patients, 94 (61%) patients reported complete suppression of tinnitus, while the remaining 59 (39%) patients continued to experience tinnitus. Fifty-eight of these patients completed the THQ pre- and postimplantation. Out of 91 patients who did not have tinnitus before their CI, 11 (12%) patients experienced tinnitus after cochlear implantation.
Figure 1.
Schematic representation of different participant groups.
Patients were asked at postimplantation visits about the presence of tinnitus; those who reported tinnitus completed the THQ. In the current study, the results of the most recent completion of the THQ were analyzed. The average duration between implantation and the administration of the most recent questionnaire was 57 months (n = 75). Our clinic at the University of Iowa is the primary source of tinnitus treatment in the area, and none of these patients had received treatment in the clinic. In discussion with our patients who returned yearly to the clinic for CI follow-up care, we were not aware that any of these patients received other forms of treatment. It is possible that a small number received some counseling that we were unaware of, as might also be the case in other studies.
Results
There were a total of 118 male and 126 female patients surveyed, ranging in age from 18 to 90 years (M = 58, SD = 15.5). Table 1 provides biographical and hearing data for the four groups. Since we have some missing data (incomplete answers on questionnaires) for the demographic data, the number of participants is different for some variables. In Table 2, we show that the distribution of patients in these groups was very similar for those who received either Cochlear Corporation implants or the Advanced Bionics Corporation implants.
Table 1.
Comparison of biographical and hearing characteristics of patients whose tinnitus was not eliminated, was eliminated, or was induced, or who did not have tinnitus pre- and postimplantation.
| Characteristic | Not eliminated | Eliminated | Induced | No tinnitus |
|---|---|---|---|---|
| Years of profound hearing loss | ||||
| N | 54 | 80 | 7 | 65 |
| M | 9 | 10 | 6 | 13 |
| SD | 12 | 13 | 6 | 16 |
| Age of implantation (years) | ||||
| N | 59 | 94 | 11 | 80 |
| M | 54 | 58 | 63 | 60 |
| SD | 14 | 16 | 11 | 17 |
| Left residual hearing (PTA dB HL) | ||||
| N | 58 | 67 | 8 | 71 |
| M | 99 | 97 | 99 | 96 |
| SD | 15 | 20 | 15 | 17 |
| Right residual hearing (PTA dB HL) | ||||
| N | 58 | 67 | 9 | 71 |
| M | 98 | 99 | 94 | 96 |
| SD | 16 | 17 | 14 | 17 |
| Implanted ear (excluding bilaterals) | ||||
| N | 42 | 56 | 8 | 57 |
| M | 99 | 100 | 93 | 95 |
| SD | 15 | 17 | 16 | 16 |
| Unimplanted ear (excluding bilaterals) | ||||
| N | 42 | 56 | 7 | 57 |
| M | 98 | 97 | 103 | 95 |
| SD | 16 | 20 | 10 | 19 |
Note. PTA db HL= pure-tone average of 500 Hz, 1000 Hz, and 2000 Hz in dB HL.
Table 2.
Devices for all patients.
| Device | Not eliminated (N = 59) |
Eliminated (N = 94) |
Induced (N = 11) |
No tinnitus (N = 80) |
|---|---|---|---|---|
| Advanced | 25/99 | 39/99 | 4/99 | 31/99 |
| Bionics (N = 99) | 25% | 39% | 4% | 31% |
| Nucleus (N = 145) | 34/145 | 55/145 | 7/145 | 49/145 |
| 23% | 38% | 5% | 34% |
Changes in THQ for Patients Using CIs
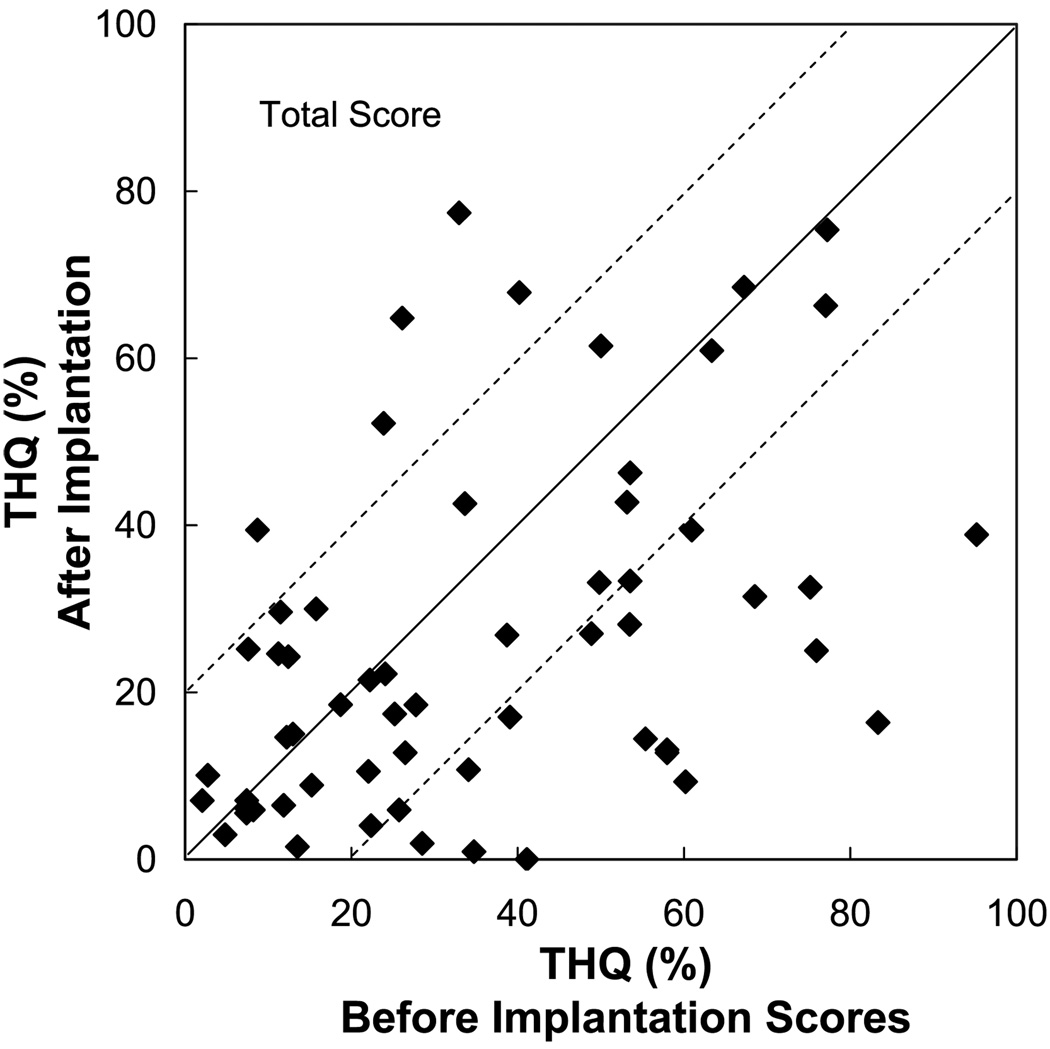
In this section, we focus on the 59 patients who had tinnitus pre- and postoperatively. Figure 2 shows a scattergram of individual THQ scores pre- and postimplantation. Out of the 59 patients, 18 had a THQ decrease of <20%, and 5 had a THQ increase of >20% (a difference score representing the preimplant THQ score minus the postimplant THQ score). Table 3 compares the average THQ scores pre- and postoperatively on total, factor, and subscale scores. A large difference—from 41% to 30%—was observed for the total score. Significant decrements were also observed for the Factor 2 hearing score, from 38% to 24%, and the Emotional subscale, from 32% to 23%.
Figure 2.
The total Tinnitus Handicap Questionnaire (THQ) score pre- and postimplantation for individual participants.
Table 3.
Average Tinnitus Handicap Questionnaire (THQ) scores pre- and postimplantation for patients whose tinnitus was not eliminated (n = 58).
| Preimplantation | Postimplantation | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Score | SD | Score | SD | Difference | t | df | P |
| THQ total score | 41.2 | 22.35 | 29.8 | 19.45 | 3.85 | 57 | .00* | |
| Factor 1—social, emotional, and behavioral effects | 29.0 | 25.61 | 22.6 | 22.94 | 6.4 | 1.93 | 57 | .06 |
| Social subscale | 29.8 | 26.87 | 23.6 | 24.13 | 6.2 | 1.75 | 57 | .09 |
| Emotional subscale | 31.7 | 28.74 | 23.4 | 23.97 | 8.3 | 2.22 | 57 | .03* |
| Physical Behaviors subscale | 25.0 | 25.49 | 20.8 | 24.62 | 4.2 | 1.19 | 57 | .24 |
| Factor 2—tinnitus and hearing | 38.3 | 34.09 | 24.0 | 23.86 | 14.3 | 3.34 | 57 | .00* |
Note. A paired t test was used to test for significance (indicated by *) at p < .05.
As an exploratory analysis, we also report those individual questions that showed a postimplant reduction of greater than 10% (see Table 4 for the difference score: the preimplant score minus the postimplant score). The largest reduction observed was on the question “My tinnitus has gotten worse over the years” (from 63% to 37%). Many of the other individual questions that showed the greatest decrement were either related to hearing improvement or social outlook.
Table 4.
Average responses to individual questions of the THQ for patients whose tinnitus was not eliminated (n = 59).
| Question | Preimplantation | Postimplantation | Difference | |
|---|---|---|---|---|
| 2 | My tinnitus has gotten worse over the years. | 63.4 (39.38) | 37.4 (37.84) | 26.0 |
| 21 | Tinnitus has caused a reduction in my speech understanding ability. | 43.5 (40.68) | 23.5 (26.99) | 20.0 |
| 23 | Tinnitus interferes with my speech understanding when listening to the television. | 39.7 (41.16) | 21.2 (28.11) | 18.5 |
| 4 | I am unable to follow conversation during meetings because of tinnitus. | 43.5 (40.23) | 25.9 (29.93) | 17.6 |
| 6 | Tinnitus interferes with my speech understanding when talking with someone in a noisy room. | 44.4 (43.92) | 28.4 (33.58) | 16.0 |
| 3 | Tinnitus interferes with my ability to tell where sounds are coming from. | 49.7 (40.81) | 33.9 (34.55) | 15.8 |
| 7 | I feel uneasy in social situations because of tinnitus. | 34.7 (39.67) | 20.4 (27.76) | 14.3 |
| 24 | Tinnitus makes me feel anxious. | 29.5 (34.78) | 15.4 (21.68) | 14.1 |
| 22 | Tinnitus makes me feel annoyed. | 41.9 (36.39) | 28.0 (33.18) | 13.9 |
| 20 | Tinnitus affects the quality of my relationships. | 25.9 (35.05) | 13.3 (23.99) | 12.6 |
| 25 | I think I have a healthy outlook on tinnitus. | 31.0 (35.30) | 19.6 (29.84) | 11.4 |
Note. The questions are listed in descending order of largest difference for the items that showed a difference greater than 10. Numbers in parentheses represent standard deviations.
A further comparison was made between those individuals whose tinnitus got better or worse on the total THQ scores, as shown in Figure 2. Although the number of participants is small, Table 5 suggests that those whose tinnitus was improved had better preimplant thresholds in the implanted ear (pure-tone averages [PTAs] of 97 to 105 dB HL) compared with patients whose tinnitus got worse following implantation.
Table 5.
Biographical data of 18 patients whose tinnitus decreased and 5 patients whose tinnitus worsened following implantation.
| Tinnitus got better (N = 18) |
Tinnitus got worse (N = 5) |
|
|---|---|---|
| Duration of profound hearing loss (years) | ||
| M | 7 | 8 |
| SD | 12 | 13 |
| Age at implantation ( years) | ||
| M | 52 | 46 |
| SD | 13 | 8 |
| PTA left ear (dB HL) | ||
| M | 97 | 92 |
| SD | 14 | 14 |
| PTA right ear (dB HL) | ||
| M | 94 | 100 |
| SD | 16 | 16 |
| Implanted ear (excluding bilaterals) | ||
| M | 97 | 105 |
| SD | 14 | 17 |
| n | 13 | 2 |
| Unimplanted ear (excluding bilaterals) | ||
| M | 92 | 106 |
| SD | 13 | 16 |
| n | 13 | 2 |
Note. PTA included frequencies 500, 1000, and 2000 Hz.
Comparison of THQ Results Between Patients With Complete Tinnitus Suppression and Those With Partial Tinnitus Relief
We now contrast the 94 CI users whose tinnitus disappeared after cochlear implantation with the 59 CI users who still had tinnitus after implantation. We performed two different analyses to search for factors that might be important. First, we evaluated preimplantation differences between these two groups. Table 6 shows that the total THQ, factor, and subscale scores were similar for the two groups (t tests were not significant).
Table 6.
Average preimplantation responses to individual questions of the THQ in patients with partial tinnitus suppression (n = 58) or complete tinnitus suppression (n = 94, except for Emotional and Physical subscales, where n = 93), and responses in patients whose tinnitus occurred after cochlear implantation (n = 11).
| Variable | Partial tinnitus suppression or no suppression |
Complete tinnitus suppression |
Tinnitus occurred postimplantation |
|---|---|---|---|
| THQ total | 41.2 (22.35) | 39.9 (23.51) | 29.5 (18.19) |
| Factor 1—social, emotional, and behavioral effects | 29.0 (25.61) | 31.4 (29.86) | 24.5 (24.86) |
| Social subscale | 29.8 (26.87) | 31.3 (30.72) | 30.3 (25.23) |
| Emotional subscale | 31.7 (28.74) | 36.5 (34.11) | 25.5 (27.20) |
| Physical Behaviors subscale | 25.0 (25.49) | 25.7 (28.55) | 18.5 (26.11) |
| Factor 2—tinnitus and hearing | 38.3 (34.09) | 37.3 (34.65) | 20.5 (22.52) |
Note. Numbers in parentheses represent standard deviations
Another statistical approach is to determine whether preoperative scores can predict postoperative differences between the two groups with binary logistic regression (SPSS Version 15.0). The total THQ score, the two factor scores, and the Emotional subscale score were included with the model out of 12 variables (age at implantation, profound years of deafness, left ear PTA, right ear PTA, implant ear PTA, unimplanted ear PTA, preimplant Factor 1, preimplant Factor 2, preimplant Social subscale, preimplant Emotional subscale, preimplant Physical subscale, and preimplant THQ). We noted in Table 3 that decrements following implantation were obtained in the group data in the THQ total score, Emotional subscale, and Factor 2—tinnitus and hearing. The logistic regression was used to determine whether the magnitude of the preoperative scores before implantation could predict postoperative changes after CI use. Two of the variables were significant: total THQ and the Emotional subscale. A high THQ total score preimplant was a predictor for still having tinnitus following implantation (odds ratio = 1.036, 95% confidence interval [CI] = 1.004–1.068, p = .025; controlling for the Emotional subscale score). A high Emotional subscale score preimplant was a predictor for not having tinnitus following implantation (odds ratio = 0.973, 95% CI = 0.952–0.995, p = .016; controlling for the THQ total score). Both of these effects are small (and we report no difference in preimplant scores with the t tests shown in Table 6) and therefore should be interpreted with caution.
Characteristics of CI Users Who Developed Tinnitus as a Result of Cochlear Implantation
In this section, we focus on the 11 patients who did not have tinnitus preoperatively but did postoperatively. We compare this group with CI users (a) whose tinnitus was not eliminated, (b) whose tinnitus was eliminated completely, and (c) who did not have tinnitus pre- or postoperatively. In Table 1, implant age, years of hearing loss, and hearing levels as defined by PTAs in the right and left ears across four different groups are listed. A one-way analysis of variance was used to compare results from the four groups with the following demographic variables: years of profound hearing loss; implant age; and preimplant PTA including the left ear alone, right ear alone, the implanted ear alone, and the unimplanted ear alone. Results showed no significant difference between the four groups for any of the demographic variables tested: years of profound hearing loss, F(3, 202) = 1.27, p > .05; implant age, F(3, 240) = 2.12, p > .05; preimplant left ear PTA, F(3, 200) = 0.32, p > .05; preimplant right ear PTA, F(3, 201) = 0.53, p > .05; preimplant implanted ear PTA, F(3, 159) = 1.52, p > .05; preimplant unimplanted ear PTA, F(3, 158) = 0.52, p > .05.
The average THQ score of patients who developed tinnitus was 30%, as shown in Table 6. This was lower than preimplant scores of both patients who had tinnitus (41%) and those who experienced complete suppression (40%). The scores from the patients who got tinnitus are similar to the THQ scores of patients who had tinnitus pre- and postimplantation (30%; compare to Table 3). The hearing loss characteristics and THQ scores were not different between CI users who got tinnitus as a result of cochlear implantation compared to other CI users. The average results for those individuals who developed tinnitus following implantation indicated a shorter duration of profound hearing loss (5.6 years) and more advanced age (63.0 years), although these differences were small and lacked significance.
Discussion
In this study, data from 244 CI users were studied. Preoperatively, 153 patients had tinnitus, and after cochlear implantation, 94 (61%) patients’ tinnitus was fully suppressed, and 59 (39%) patients still had tinnitus. Comparing changes before and after cochlear implantation, the THQ showed that scores were often reduced dramatically even in those patients whose tinnitus remained.
Reduction in Tinnitus Hearing Handicap Achieved by Tinnitus Sufferers Using CIs
For many patients (with or without CIs), it can be difficult to distinguish whether hearing difficulties are a result of tinnitus or of the concomitant hearing loss. Patients who are candidates for CIs obviously have a significant hearing loss and show dramatic improvements in their hearing ability postimplantation.
If a portion of a patient’s hearing handicap is produced by tinnitus, then electrical stimulation with a CI can improve hearing by reducing the magnitude of tinnitus disruption. As Souliere, Kileny, Zwolan, and Kemink (1992) reported, approximately 50% of patients with tinnitus prior to implantation experienced a reduction of tinnitus loudness of 30% or more. If the tinnitus is having a negative impact on hearing, then reduction of tinnitus loudness should improve hearing as well.
In future studies it will be useful to obtain estimates of the magnitude of the tinnitus preimplantation and to determine whether reductions in the tinnitus magnitude relate to improvements in hearing.
Differences Between CI Patients Who Showed Total Versus Partial Suppression of Tinnitus
We attempted to find differences between patients who benefited from electrical stimulation and those who did not benefit from electrical stimulation. We found no clear distinction. Years of profound hearing loss, implant age, and preimplant hearing thresholds between these two groups were not significantly different. There were also no THQ differences between CI users without tinnitus suppression and CI users with tinnitus suppression.
It appeared that the patients who were sensitive to noisy situations were generally more likely to have their tinnitus suppressed. Additionally, the patients whose localization ability was influenced by their tinnitus were less likely to benefit from electrical stimulation. But these effects were not large.
The reason that electrical stimulation reduced tinnitus disruption in only a portion of the patients is unclear. Ruckenstein, Hedgepeth, Rafter, Montes, and Bigelow (2001) reported that the implanted device (Clarion or Nucleus) and gender have no influence on the efficacy of electrical suppression of tinnitus. Souliere et al. (1992) reported that there may be a relation between loudness and annoyance values prior to implantation with the amount of tinnitus reduction after implantation. We found no relation between the magnitude of the handicap and the benefit from the CI.
Characteristics of CI Users Who Developed Tinnitus as a Result of Cochlear Implantation
In our study, 91 patients did not have tinnitus before cochlear implantation, but 11 of them suffered from tinnitus after implantation (12%). The incidence of our report was higher than previous studies, which ranged from 0% to 4% (e.g., McKerrow, Schreiner, Snyder, Merzenich, & Toner, 1991). Tyler (1995) reported that the tinnitus increased in 3 of 22 (13.6%) CI users after 2 years of CI use. In the present study, the CI users who acquired tinnitus had a shorter duration of profound hearing loss and tended to be older, but these average differences were not large. Because of the small number of patients who developed tinnitus (N = 11), it is difficult to determine their unique characteristics.
There are several shortcomings to our study, which we will try to correct in further work. It would be helpful to know whether patients had unilateral or bilateral tinnitus, and concurrently whether the CI influenced auditory behaviors more in the tinnitus ear or nontinnitus ear. We did not separate the effects of the CI surgery on the tinnitus perception from those related to CI activation. An investigation that focused on those effects could contribute to the establishment of guidelines for fitting protocols in CI recipients who report tinnitus preoperatively.
Acknowledgments
This research was supported by National Institutes of Health Grant R01 DC005972-01A1 and the American Tinnitus Association.
Appendix
Tinnitus Handicap Questionnaire
|
Footnotes
Copyright of American Journal of Audiology is the property of American Speech-Language-Hearing Association and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
Contributor Information
Tao Pan, University of Iowa, Iowa City, and Peking University Third Hospital, Beijing, People’s Republic of China.
Richard S. Tyler, University of Iowa, Iowa City
Haihong Ji, University of Iowa, Iowa City.
Claudia Coelho, University of Iowa, Iowa City.
Anne K. Gehringer, University of Iowa, Iowa City
Stephanie A. Gogel, University of Iowa, Iowa City
References
- Baguley DM, Atlas MD. Cochlear implants and tinnitus. Progress in Brain Research. 2007;166:347–355. doi: 10.1016/S0079-6123(07)66033-6. [DOI] [PubMed] [Google Scholar]
- Dauman R, Daubech Q, Gavilan I, Colmet L, Delaroche M, Michas N, et al. Long-term outcome of childhood hearing deficiency. Acta Otolaryngologica. 2000;120:205–208. doi: 10.1080/000164800750000928. [DOI] [PubMed] [Google Scholar]
- Demajumdar R, Stoddart R, Donaldson I, Proops DW. Tinnitus, cochlear implants and how they affect patients. Journal of Laryngology & Otology. 1999;113:24–26. [PubMed] [Google Scholar]
- Di Nardo W, Cantore I, Cianfrone F, Melillo P, Scorpecci A, Paludetti G. Tinnitus modifications after cochlear implantation. European Archives of Oto-rhino-laryngology. 2007;264:1145–1149. doi: 10.1007/s00405-007-0352-7. [DOI] [PubMed] [Google Scholar]
- Eggermont JJ, Roberts LE. The neuroscience of tinnitus. Trends in Neuroscience. 2004;27:676–682. doi: 10.1016/j.tins.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Gatehouse S, Noble W. The Speech, Spatial and Qualities of Hearing Scale (SSQ) International Journal of Audiology. 2004;43(2):85–99. doi: 10.1080/14992020400050014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson WPR, Aran JM, Dauman R. The effect of electrical stimulation and cochlear implantation on tinnitus. Tinnitus 91: Proceedings of the Fourth International Tinnitus Seminar; Kugler; Amsterdam. 1992. pp. 403–408. [Google Scholar]
- Giraud AL, Price CJ, Graham JM, Frackowiak RS. Functional plasticity of language-related brain areas after cochlear implantation. Brain. 2001;124:1307–1316. doi: 10.1093/brain/124.7.1307. [DOI] [PubMed] [Google Scholar]
- Ito J. Tinnitus suppression in cochlear implant patients. Otolaryngology—Head and Neck Surgery. 1997;117:701–703. doi: 10.1016/S0194-59989770056-1. [DOI] [PubMed] [Google Scholar]
- Kiang NYS, Moson EC, Levine RA. Auditorynerve activity in cats with normal and abnormal cochleas. In: Wolstenholme GEW, editor. Sensorineural hearing loss. London: Churchill; 1970. pp. 241–268. [DOI] [PubMed] [Google Scholar]
- Kral A, Tillein J. Brain plasticity under cochlear implant stimulation. Advances in Otorhinolaryngology. 2006;64:89–108. doi: 10.1159/000094647. [DOI] [PubMed] [Google Scholar]
- Kuk FK, Tyler RS, Russell D, Jordan H. The psychometric properties of a tinnitus handicap questionnaire. Ear and Hearing. 1990;11:434–445. doi: 10.1097/00003446-199012000-00005. [DOI] [PubMed] [Google Scholar]
- McKerrow WS, Schreiner CE, Snyder RL, Merzenich MM, Toner JG. Tinnitus suppression by cochlear implants. Annals of Otology, Rhinology and Laryngology. 1991;100:552–558. doi: 10.1177/000348949110000706. [DOI] [PubMed] [Google Scholar]
- Miyamoto RT, Wynne MK, McKnight C, Bichey B. Electrical suppression of tinnitus via cochlear implants. International Tinnitus Journal. 1997;3:35–38. [PubMed] [Google Scholar]
- Mo B, Harris S, Lindbaek M. Tinnitus in cochlear implant patients—a comparison with other hearing-impaired patients. International Journal of Audiology. 2002;41:527–534. doi: 10.3109/14992020209056073. [DOI] [PubMed] [Google Scholar]
- Muhlnickel W, Elbert T, Taub E, Flor H. Reorganization of auditory cortex in tinnitus. Proceedings of the National Academy of Sciences, USA. 1998;95:10340–10343. doi: 10.1073/pnas.95.17.10340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Archives of Otolaryngology—Head Neck Surgery. 1996;122:143–148. doi: 10.1001/archotol.1996.01890140029007. [DOI] [PubMed] [Google Scholar]
- Newman CW, Wharton JA, Jacobson GP. Retest stability of the tinnitus handicap questionnaire. Annals of Otology, Rhinology and Laryngology. 1995;104:718–723. doi: 10.1177/000348949510400910. [DOI] [PubMed] [Google Scholar]
- Quaranta N, Fernandez-Vega S, D’elia C, Filipo R, Quaranta A. The effect of unilateral multichannel cochlear implant on bilaterally perceived tinnitus. Acta Otolaryngologica. 2008;128:159–163. doi: 10.1080/00016480701387173. [DOI] [PubMed] [Google Scholar]
- Quaranta N, Wagstaff S, Baguley DM. Tinnitus and cochlear implantation. International Journal of Audiology. 2004;43:245–251. doi: 10.1080/14992020400050033. [DOI] [PubMed] [Google Scholar]
- Rubinstein JT, Tyler RS, Johnson A, Brown CJ. Electrical suppression of tinnitus with high-rate pulse trains. Otology and Neurotology. 2003;24:478–485. doi: 10.1097/00129492-200305000-00021. [DOI] [PubMed] [Google Scholar]
- Rubinstein JT, Wilson BS, Finley CC, Abbas PJ. Pseudospontaneous activity: Stochastic independence of auditory nerve fibers with electrical stimulation. Hearing Research. 1999;127:108–118. doi: 10.1016/s0378-5955(98)00185-3. [DOI] [PubMed] [Google Scholar]
- Ruckenstein MJ, Hedgepeth C, Rafter KO, Montes ML, Bigelow DC. Tinnitus suppression in patients with cochlear implants. Otology and Neurotology. 2001;22:200–204. doi: 10.1097/00129492-200103000-00014. [DOI] [PubMed] [Google Scholar]
- Salvi RJ, Wang J, Powers NJ. Plasticity and reorganization in the auditory brainstem: Implications for tinnitus. In: Reich GE, Vernon JA, editors. Proceedings of the 5th International Tinnitus Seminar; American Tinnitus Association; Portland, OR. 1996. pp. 457–466. [Google Scholar]
- Souliere CRJ, Kileny PR, Zwolan TA, Kemink JL. Tinnitus suppression following cochlear implantation. A multifactorial investigation. Archives of Otolaryngology—Head & Neck Surgery. 1992;118:1291–1297. doi: 10.1001/archotol.1992.01880120017004. [DOI] [PubMed] [Google Scholar]
- Stouffer JL, Tyler RS. Characterization of tinnitus by tinnitus patients. Journal of Speech and Hearing Disorders. 1990;55:439–453. doi: 10.1044/jshd.5503.439. [DOI] [PubMed] [Google Scholar]
- Tyler RS. Tinnitus. In: Evered D, Lawrenson G, editors. Tinnitus. London: Pitman; 1981. pp. 136–137. [Google Scholar]
- Tyler RS. Tinnitus disability and handicap questionnaires. Seminars in Hearing. 1993;14:377–384. [Google Scholar]
- Tyler RS. Advantages and disadvantages expected and reported by cochlear implant patients. American Journal of Otology. 1994;15:523–531. [PubMed] [Google Scholar]
- Tyler RS. Tinnitus in the profoundly hearing-impaired and the effects of cochlear implants. Annals of Otology, Rhinology & Laryngology. 1995;104 Suppl. 165:25–30. [PubMed] [Google Scholar]
- Tyler RS. Neurophysiological models, psychological models, and treatments for tinnitus. In: Tyler RS, editor. Tinnitus treatment: Clinical protocols. New York: Thieme; 2006. pp. 1–22. [Google Scholar]
- Tyler RS, Baker LJ. Difficulties experienced by tinnitus sufferers. Journal of Speech and Hearing Disorders. 1983;48:150–154. doi: 10.1044/jshd.4802.150. [DOI] [PubMed] [Google Scholar]
- Tyler RS, Kelsay D. Advantages and disadvantages reported by some of the better cochlear-implant patients. American Journal of Otology. 1990;11(4):282–289. [PubMed] [Google Scholar]
- Tyler RS, Rubinstein J, Pan T, Chang S-A, Gogel SA, Gehringer A, Coelho C. Electrical stimulation of the cochlea to reduce tinnitus. Seminars in Hearing. 2008;29:326–332. doi: 10.1055/s-0028-1095892. [DOI] [PMC free article] [PubMed] [Google Scholar]