Abstract
Objectives
To describe radiation exposure from cardiac imaging procedures over time in a general population.
Background
Cardiac imaging procedures frequently expose patients to ionizing radiation, but their contribution to effective doses of radiation in the general population is unknown.
Methods
We used administrative claims to identify cardiac imaging procedures performed from 2005-2007 in 952,420 non-elderly insured adults in 5 U.S. healthcare markets. We estimated 3-year cumulative effective doses of radiation in millisieverts (mSv) from these procedures We then calculated population-based annual rates of radiation exposure to effective doses ≤3 mSv/year (background level of radiation from natural sources), >3-20 mSv/year, or >20 mSv/year (upper annual limit for occupational exposure averaged over 5 years).
Results
90,121 (9.5%) individuals underwent at least one cardiac imaging procedure using radiation. Among patients who underwent ≥1 cardiac imaging procedure, the mean cumulative effective dose over 3 years was 16.4 mSv (range 1.5-189.5 mSv). Myocardial perfusion imaging accounted for 74% of the cumulative effective dose. Overall, 47.8% of cardiac imaging procedures were performed in physician offices; this proportion was higher for myocardial perfusion imaging (74.8%) and cardiac CT studies (76.5%). The annual population-based rate of receiving an effective dose of >3-20 mSv/year was 89.0 per 1000; and 3.3 per 1000 for cumulative doses >20 mSv/year. Annual effective doses increased with age and were generally higher among men.
Conclusions
Cardiac imaging procedures lead to substantial radiation exposure and effective doses for many patients in the United States.
Keywords: radiation, imaging, epidemiology
Background
The volume of medical imaging procedures incorporating ionizing radiation has been growing rapidly in recent years, especially for evaluation of cardiovascular conditions.1 In the United States alone, the use of myocardial perfusion imaging (MPI) increased from less than 3 million in 1990 to nearly 10 million by 2002.2 From 2002 to 2006 the number of procedures in cardiac catheterization laboratories increased by 9% and now exceeds 4 million cases per year.3 The use of cardiac computed tomography (CT), an emerging imaging technology, is expected to rise dramatically over the next decade.4
Although advances in cardiac imaging procedures have improved the ability to assess and treat cardiovascular conditions, there is a dearth of patient-level data on radiation exposure over time from cardiac imaging procedures despite a rapid rise in their use. A recent study reported that cumulative radiation exposure from general medical imaging is substantial in many individuals.5 In that study MPI studies accounted for 22% of total effective dose of radiation received in the study population, but further assessment of other cardiac imaging procedures was not performed. Another study that examined radiation exposure from cardiac imaging procedures was conducted in the inpatient setting of a single hospital, thus limiting generalizability of radiation exposure over time to the overall population.6 There are also gaps in knowledge regarding the type and location of cardiac imaging services currently performed in the U.S., which is an important consideration given the increase in diagnostic imaging equipment within physician offices.7
Accordingly, we analyzed administrative claims data over a 3-year period from a large cohort of non-elderly insured adults across the U.S. to estimate mean cumulative effective doses of radiation attributable to cardiac imaging procedures. This study cohort consisted of beneficiaries aged 18 to 64 years old representing a broad spectrum of individuals from the general population. We examined the proportion of individuals that received cumulative effective doses of radiation over two thresholds: >3 millisieverts (mSv) per year, representing the background level of radiation absorbed from natural sources in the United States;8 and >20 mSv per year, representing the upper annual limit for occupational exposure for at-risk workers averaged over 5 years.9 Our overall goals were to describe radiation exposure that accumulates over time in a general population from cardiac imaging procedures and to identify patient groups at risk for high radiation exposure.
Methods
Data Source and Study Population
The study cohort consisted of non-elderly adults with healthcare benefits administered by United Healthcare (UHC), one of the largest private healthcare insurance carriers in the United States. Administrative claims data were collected related to cardiac imaging procedures for 5 major healthcare markets: Arizona, Dallas, Orlando, South Florida, and Wisconsin. These markets were specifically selected because of their size and the similarity of their insurance products, as well as to provide a degree of geographical diversity. More than three quarters of individuals were enrolled in point of service / exclusive provider organization insurance plans with health maintenance organization plans comprising ≤12% of enrollees in any market. Dallas had the largest proportion of enrollees in preferred provider organization / indemnity plans (∼23%) compared with other markets (≤2%). Within these 5 healthcare markets, all adults ages 18 to <65 years old who were alive and continuously enrolled in a health plan administered by UHC between January 1, 2005 and December 31, 2007 were identified.
Data Elements
UHC administrative data included information on the age and sex of enrollees along with type of medical services performed as classified by Current Procedural Terminology (CPT) codes and the location where services were delivered. The location of imaging services was recorded in the administrative claims, and classified into the following categories: hospital inpatient (performed during a hospital admission), hospital outpatient (performed within hospital facilities for non-hospitalized patients), and physician offices. Cardiac imaging procedures associated with radiation exposure were identified using CPT codes and classified into the following categories: 1) myocardial perfusion imaging (MPI) scans with planar imaging, single photon emission computed tomography (SPECT), or positron emission tomography (PET) imaging, 2) diagnostic cardiac catheterization and/or percutaneous coronary intervention (PCI), 3) cardiac blood pool imaging such as equilibrium radionuclide angiogram (ERNA) or multi-gated acquisition scan (MUGA), 4) electrophysiological procedures (including device implantations and arrhythmia ablation procedures), and 5) cardiac computed tomography (CT). Because CPT codes for cardiac CT became effective on January 1, 2006, the analysis only considered cardiac CT studies billed during the 2-year period from 2006-2007.
Estimates of Radiation Dose
We surveyed the published literature to obtain estimates of effective doses of radiation associated with each cardiac imaging procedure. Effective dose, reported in millisieverts (mSv), is a measure of the overall detrimental biological effect of a given radiation exposure. It is calculated by weighting the concentrations of energy deposited in each organ from a given radiation exposure, taking into account type of radiation and the potential for organ-specific damage in a reference individual.10, 11 Effective dose allows for population-level comparisons across different types of radiation exposure.9, 12 Estimates for effective dose for cardiac imaging procedures were obtained from a recent systematic review13 as well as other published sources.14-16 Estimation of the effective dose for MPI studies was a particular challenge given the wide diversity in varying protocols (e.g. single versus dual isotope) across the nation. We arrived at an estimate of 15.6 mSv for the effective dose of MPI studies after considering the dosimetry of specific radiopharmaceuticals,17 their median injected activities,18 and the distribution of imaging protocols in the U.S.19 Estimates of effective doses for the cardiac imaging procedures commonly performed in our study cohort are presented in Table 1.
Table 1. Estimates of Effective Doses for Selected Cardiac Imaging Procedures (in mSv).
| Myocardial perfusion study with ejection fraction | 15.6 |
| Diagnostic coronary angiography | 7.0 |
| Percutaneous coronary intervention | 15.0 |
| Cardiac blood pool imaging, gated equilibrium; planar, single study at rest or stress | 7.8 |
| Cardiac CT (without contrast, for assessment of coronary calcium) | 3.0 |
| Cardiac CT (with contrast, for assessment of coronary arteries, without assessment for coronary calcium) | 16.0 |
| Pacemaker insertion | 1.5 |
| Comprehensive electrophysiologic evaluation | 5.7 |
As in a prior study5, the 3-year cumulative effective dose was calculated for each enrollee according to the type of procedure performed and pattern of claims submitted for that service. For example, if an individual had cardiac imaging procedures across multiple categories on the same day (e.g. MPI followed by PCI) the effective doses associated with each of the procedures were included in the cumulative effective dose for the individual. However, if there were multiple imaging procedures on the same day within a single imaging category, only the procedure with the highest effective dose was added to an individual's cumulative effective dose in order to avoid any overestimation. For example, accumulating radiation exposures for both diagnostic left heart catheterization and a stent implantation separately would likely overestimate the dose received due to overlapping radiation exposure during these procedures; in this example, only the higher effective dose from stent implantation would be included. This conservative approach reduced the potential risk of over-estimating radiation exposure.
Statistical Analysis
The proportion of patients who underwent any cardiac imaging procedure was calculated based on the overall denominator of enrollees, and then examined across age, sex, age-sex, and service market categories. The number of cardiac imaging procedures with radiation exposure was calculated by dividing the annual number of procedures by the denominator of enrollees across 5 procedure categories (MPI, CATH/PCI, ERNA/MUGA, cardiac CT and electrophysiologic studies) and 3 locations (hospital inpatient, hospital outpatient, and physician office) as described above.
We calculated population-based rates of receiving cumulative effective doses of radiation for 3 categories of radiation exposure based on estimates of background exposure from natural sources in the U.S. as well as categories currently recommended for radiation protection in medical occupations. The 3 categories were: ≤3 mSv per year (the background level of radiation absorbed from natural sources in the United States8); >3-20 mSv per year, and >20 mSv per year (the upper annual limit for occupational exposure for at-risk workers averaged over 5 years).9 Numerators for these rates were the number of enrollees with cumulative effective doses in these categories; denominators included the total number of eligible enrollees in the study period. Direct standardization with the overall population as a reference was used to account for differences in the distribution of age and sex across the five health care markets.20 The chi-squared test was used to assess differences across categories. All statistical analyses were carried out with the use of SAS software, version 9.1 (SAS Institute Inc., NC).
Study Oversight
This study was investigator-initiated and the authors were responsible for its design and the creation of the manuscript. The authors had complete control of the data and independently conducted the analysis. No external funding was provided for this study and there was no need to obtain approval from UHC prior to its submission for publication.
Results
The study population consisted of 952,420 non-elderly adults with continuous enrollment in health insurance programs administered by UHC from 2005 to 2007. Mean age was 35.6 years (standard deviation, 23.0) and there were 499,342 (52.4%) women. The largest number of enrollees came from the Dallas market area (298,747), while the smallest number of enrollees was located in the Orlando market area (133,561).
During the study period, a total of 90,121 (9.5%) enrollees underwent at least one cardiac imaging procedure associated with radiation exposure over the 3-year study period (Table 2). The proportion of enrollees who underwent at least one cardiac imaging procedure increased with age, ranging from 1.5% in patients 18-34 years old to 20.9% in patients 55-64 years old. A higher proportion of men underwent cardiac imaging procedures compared with women (10.5% v 8.5%, p<0.0001). The proportions of enrollees undergoing any cardiac imaging procedures were highest in the South Florida and Orlando healthcare markets compared with the 3 remaining healthcare markets.
Table 2. Number of enrollees undergoing cardiac imaging procedures with radiation exposure, 2005-2007.
| Total Patients | Patients with radiation exposure from cardiac imaging procedures | (%) | |
|---|---|---|---|
| ALL | 952420 | 90121 | 9.5% |
| Age Groups | |||
| 18-34 | 233586 | 3405 | 1.5% |
| 35-44 | 263093 | 15531 | 5.9% |
| 45-54 | 277912 | 33947 | 12.2% |
| 55-64 | 177829 | 37238 | 20.9% |
| Gender | |||
| Male | 453078 | 47467 | 10.5% |
| Female | 499342 | 42654 | 8.5% |
| Men in Age Groups | |||
| 18-34 | 110062 | 1842 | 1.7% |
| 35-44 | 125814 | 8087 | 6.4% |
| 45-54 | 131567 | 17264 | 13.1% |
| 55-64 | 85635 | 20274 | 23.7% |
| Women in Age Groups | |||
| 18-34 | 123524 | 1563 | 1.3% |
| 35-44 | 137279 | 7444 | 5.4% |
| 45-54 | 146345 | 16683 | 11.4% |
| 55-64 | 92194 | 16964 | 18.4% |
| Service Market | |||
| Arizona | 180046 | 14969 | 8.3% |
| Dallas | 298747 | 21285 | 7.1% |
| Orlando | 133561 | 17201 | 12.9% |
| South Florida | 170466 | 23962 | 14.1% |
| Wisconsin | 169600 | 12704 | 7.5% |
p<0.001 for comparisons across age, sex, age-sex and service market categories.
A total of 172,194 cardiac imaging procedures with radiation exposure were performed over the 3-year study period. Table 3 reports the number of cardiac imaging procedures performed per 1000 enrollees per year. Overall, the annual rate of use of cardiac imaging procedures was 60.3 per 1000 enrollees. MPI studies were the most common cardiac imaging procedure performed; the second most commonly performed procedure was cardiac catheterization and/or PCI. In general, annual rates for all cardiac imaging procedures were higher in men with the exception of ERNA/MUGA. Overall, approximately half of all cardiac imaging procedures took place in physician offices (47.8%) with the remainder divided between hospital inpatients (26.4%) and non-hospitalized patients who underwent imaging in hospital facilities (25.5%). The majority of MPI and cardiac CT studies were performed in physician offices — 74.8% and 76.5%, respectively.
Table 3. Number of cardiac imaging procedures with radiation exposure (per 1000 enrollees per year).
| Total | MPI | CATH/PCI | ERNA/MUGA | CCT* | EP | |
|---|---|---|---|---|---|---|
| ALL | 60.3 | 34.7 | 21.6 | 1.8 | 1.0 | 1.3 |
| Age Groups | ||||||
| 18-34 | 7.1 | 4.5 | 1.6 | 0.4 | 0.1 | 0.4 |
| 35-44 | 31.6 | 19.9 | 9.2 | 1.3 | 0.6 | 0.7 |
| 45-54 | 76.4 | 44.0 | 27.6 | 2.2 | 1.3 | 1.4 |
| 55-64 | 147.3 | 81.5 | 56.8 | 3.6 | 2.1 | 3.3 |
| Gender | ||||||
| Male | 74.2 | 40.1 | 29.9 | 1.4 | 1.2 | 1.7 |
| Female | 47.7 | 29.7 | 14.1 | 2.1 | 0.8 | 0.9 |
| Men in Age Groups | ||||||
| 18-34 | 8.5 | 5.3 | 2.4 | 0.3 | 0.2 | 0.4 |
| 35-44 | 37.0 | 22.3 | 12.4 | 0.8 | 0.7 | 0.7 |
| 45-54 | 91.9 | 49.1 | 37.9 | 1.5 | 1.6 | 1.8 |
| 55-64 | 185.9 | 97.0 | 78.6 | 3.3 | 2.4 | 4.6 |
| Women in Age Groups | ||||||
| 18-34 | 5.7 | 3.8 | 0.9 | 0.5 | 0.1 | 0.4 |
| 35-44 | 26.7 | 17.8 | 6.2 | 1.7 | 0.4 | 0.6 |
| 45-54 | 62.5 | 39.3 | 18.4 | 2.8 | 1.1 | 1.0 |
| 55-64 | 111.4 | 67.2 | 36.5 | 3.9 | 1.8 | 2.0 |
| Service Market | ||||||
| Arizona | 55.4 | 29.6 | 22.7 | 1.4 | 0.2 | 1.5 |
| Dallas | 49.0 | 25.8 | 19.6 | 1.1 | 1.4 | 1.1 |
| Orlando | 81.6 | 47.6 | 30.0 | 1.5 | 1.3 | 1.3 |
| South Florida | 81.2 | 55.4 | 19.0 | 4.5 | 0.7 | 1.5 |
| Wisconsin | 47.5 | 24.4 | 20.0 | 0.9 | 0.9 | 1.3 |
Abbreviations: MPI, Myocardial perfusion imaging; CATH, cardiac catheterization; PCI, percutaneous coronary intervention; ERNA, equilibrium radionuclide angiogram; MUGA, multi-gated acquisition scan; EP, electrophysiologic procedures; CCT, cardiac computed tomography
Codes specific for cardiac computed tomography were available for two out of three years of this study (2006 and 2007).
p<0.001 for comparisons acrossage, sex, age-sex and service market categories.
The total cumulative effective dose received by the study population from cardiac imaging procedures over three years was 2,084 Sv. Among 90,121 patients undergoing at least 1 cardiac imaging procedure, the mean cumulative effective dose over the 3 years was 16.4 mSv while the median dose was 15.6 mSv, ranging from 1.5 to 189.5 mSv. There were 3173 individuals who received >20 mSv annually over the 3-year study period and 75 individuals received >50 mSv annually.
Table 4 reports on the number of cardiac imaging procedures and proportion of radiation dose, according to location. Overall, the rate of cardiac imaging procedures was highest in physician offices (28.8 per 1000 enrollees per year) compared with hospital inpatient and hospital outpatient locations (15.9 and 19.6 per 1000 enrollees per year, respectively p<0.0001). Slightly more than half of the overall radiation dose was delivered in the physician office setting (58.8%). These findings were consistent across enrollee age and sex categories. Physician office-based imaging continued to be largest contributor of procedures and radiation dose across the 5 service markets, with the exception of Wisconsin, where hospital outpatient locations had the highest procedure use and contribution to overall radiation dose.
Table 4. Number of cardiac imaging procedures (per 1000 enrollees per year) and proportion of overall radiation dose, according to location.
| Hospital Inpatient | Hospital Outpatient | Physician Office | Other / Not classified | |||||
|---|---|---|---|---|---|---|---|---|
| # | % dose | # | % dose | # | % dose | # | % dose | |
| ALL | 15.9 | 21.3% | 15.3 | 19.6% | 28.8 | 58.8% | 0.2 | 0.3% |
| Age, Groups | ||||||||
| 18-34 | 1.6 | 17.9% | 1.8 | 20.7% | 3.6 | 61.2% | 0.0 | 0.2% |
| 35-44 | 7.2 | 18.8% | 8.3 | 20.6% | 16.0 | 60.2% | 0.1 | 0.3% |
| 45-54 | 20.4 | 21.7% | 19.8 | 20.1% | 36.0 | 57.9% | 0.2 | 0.3% |
| 55-64 | 40.5 | 22.0% | 36.5 | 18.8% | 69.7 | 59.0% | 0.5 | 0.3% |
| Sex | ||||||||
| Male | 20.8 | 21.9% | 18.7 | 19.4% | 34.4 | 58.4% | 0.2 | 0.3% |
| Female | 11.5 | 20.5% | 12.3 | 19.8% | 23.7 | 59.4% | 0.2 | 0.3% |
| Men in Age Groups | ||||||||
| 18-34 | 2.0 | 18.1% | 2.2 | 21.2% | 4.3 | 60.6% | 0.0 | 0.2% |
| 35-44 | 9.0 | 19.1% | 9.6 | 20.5% | 18.3 | 60.0% | 0.1 | 0.4% |
| 45-54 | 26.5 | 22.6% | 23.3 | 19.8% | 41.8 | 57.4% | 0.2 | 0.2% |
| 55-64 | 53.4 | 22.5% | 46.2 | 18.7% | 85.7 | 58.5% | 0.6 | 0.3% |
| Women in Age Groups | ||||||||
| 18-34 | 1.2 | 17.8% | 1.5 | 20.0% | 3.1 | 62.0% | 0.0 | 0.2% |
| 35-44 | 5.6 | 18.5% | 7.1 | 20.9% | 13.9 | 60.4% | 0.1 | 0.3% |
| 45-54 | 15.0 | 20.6% | 16.6 | 20.5% | 30.7 | 58.6% | 0.2 | 0.3% |
| 55-64 | 28.4 | 21.3% | 27.6 | 18.8% | 54.9 | 59.6% | 0.4 | 0.3% |
| Service Market | ||||||||
| Arizona | 16.7 | 23.5% | 14.3 | 19.4% | 24.4 | 57.0% | 0.1 | 0.1% |
| Dallas | 11.3 | 17.3% | 13.3 | 19.2% | 24.3 | 63.4% | 0.1 | 0.1% |
| Orlando | 20.3 | 20.1% | 17.6 | 16.3% | 43.2 | 62.9% | 0.5 | 0.7% |
| South Florida | 23.3 | 25.6% | 11.9 | 10.2% | 45.6 | 63.9% | 0.4 | 0.3% |
| Wisconsin | 12.3 | 19.3% | 21.7 | 43.5% | 13.3 | 37.0% | 0.1 | 0.2% |
p<0.001 for comparisons across age, sex, age-sex and service market categories.
The Figure displays the contribution of cardiac imaging procedures to the cumulative effective dose of radiation, according to type of imaging procedure performed. Overall, the largest contributor to the cumulative effective dose was MPI studies, which were responsible for 74.2% of the cumulative effective dose, while diagnostic cardiac catheterization and PCI procedures contributed to 21.4%. Among women and men age 18-34 years, MPI was the largest contributor to radiation dose (81.3% and 78.4%, respectively). In contrast, among patients with annual dose >20 mSv and >50 mSv, diagnostic cardiac catheterization and PCI procedures were the largest contributors to radiation dose (66.2% and 48.4%, respectively). Of the 75 patients with annual dose >50 mSv, 73 patients underwent 5 or more diagnostic cardiac catheterization or PCI procedures, with a median of 4 MPI/PET studies performed in this subgroup. Of the 3173 patients with annual dose >20 mSv, 1,727 patients underwent 5 or more diagnostic cardiac catheterization or /PCI procedures with a median of 3 MPI/PET studies performed in this subgroup.
Figure. Contribution to cumulative effective radiation dose, by type of cardiac imaging procedure.
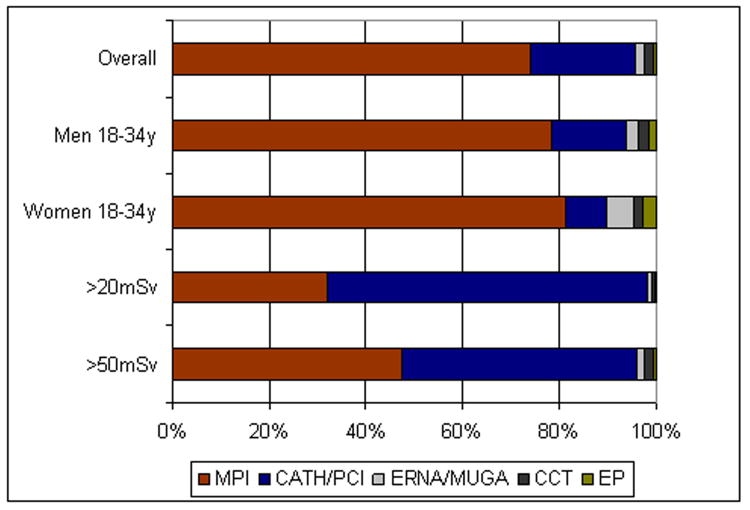
Abbreviations: MPI, Myocardial perfusion imaging; CATH, cardiac catheterization; PCI, percutaneous coronary intervention; ERNA, equilibrium radionuclide angiogram; MUGA, multi-gated acquisition scan; EP, electrophysiologic procedures; CCT, cardiac computed tomography
Table 5 reports calculated population-based rates of receiving annual effective doses of radiation across different thresholds. Overall, 89.0 per 1000 enrollees had annual effective doses of >3 to 20mSv per year and 3.3 per 1000 enrollees had doses of >20mSv per year. The rate of individuals exposed to >3-20 and >20 mSv per year rose dramatically with increasing age and were higher for men as compared with women. Adjusting for age and sex, the population-based rate of receiving annual effective doses of >3 to 20mSv and >20mSv were highest in the Orlando and South Florida healthcare markets.
Table 5. Annual rates of radiation exposure from cardiac imaging procedures, per 1000 enrollees.
| No exposure | >0-3mSv/year | >3-20mSv/year | >20mSv/year | |
|---|---|---|---|---|
| ALL | 905.4 | 2.3 | 89.0 | 3.3 |
| Age Groups | ||||
| 18-34 | 985.4 | 1.0 | 13.5 | 0.1 |
| 35-44 | 941.0 | 1.8 | 56.3 | 1.0 |
| 45-54 | 877.8 | 2.7 | 115.5 | 3.9 |
| 55-64 | 790.6 | 4.3 | 195.0 | 10.1 |
| Gender | ||||
| Male | 895.2 | 1.8 | 97.8 | 5.2 |
| Female | 914.6 | 2.8 | 81.0 | 1.7 |
| Men in Age Groups | ||||
| 18-34 | 983.3 | 0.8 | 15.8 | 0.2 |
| 35-44 | 935.7 | 1.2 | 61.6 | 1.5 |
| 45-54 | 868.8 | 1.8 | 123.3 | 6.1 |
| 55-64 | 763.3 | 4.0 | 217.2 | 15.5 |
| Women in Age Groups | ||||
| 18-34 | 987.3 | 1.1 | 11.5 | 0.1 |
| 35-44 | 945.8 | 2.3 | 51.5 | 0.5 |
| 45-54 | 886.0 | 3.5 | 108.5 | 2.0 |
| 55-64 | 816.0 | 4.5 | 174.4 | 5.1 |
| Service Market* | ||||
| Arizona | 916.9 | 2.6 | 73.0 | 3.0 |
| Dallas | 928.8 | 2.2 | 69.5 | 3.4 |
| Orlando | 871.2 | 2.4 | 118.4 | 4.1 |
| South Florida | 859.4 | 2.1 | 133.6 | 4.1 |
| Wisconsin | 925.1 | 2.3 | 71.5 | 2.2 |
Proportion adjusted for age and sex using direct standardization to the overall population
p<0.001 for comparisons across age, sex, age-sex and service market categories.
Discussion
This study provides contemporary data on the cumulative effective doses of radiation from cardiac imaging procedures in nearly 1 million non-elderly insured adults. We observed that nearly one out of ten adults underwent at least one cardiac imaging procedure with radiation exposure during the 3-year study period. The distribution of cardiac imaging procedures was skewed, with sizeable effective doses accumulating in a minority of individuals over time. For example, approximately 10% of our study population overall underwent at least one cardiac imaging procedure with radiation exposure.
The public health and clinical implications of radiation exposure from cardiac imaging are not easily determined. Clinicians and patients must consider tradeoffs between the benefits of cardiac imaging procedures against their potential long-term risks due to radiation, mainly those of malignancy. The National Academies' seventh Biologic Effects of Ionizing Radiation (BEIR VII) report, a comprehensive assessment of the health risks from exposure to ionizing radiation, estimates that a 100 mSv radiation dose would lead to 1 additional cancer per 100 individuals over a lifetime.21 Studies have also estimated cancer risk from radiation exposures associated with specific cardiac imaging procedures. A model of CT coronary angiography suggested that the lifetime attributable risks of cancer were 1 in 284 for a 40-year old woman and 1 in 1007 for a 40-year old man.22
Although the overall proportion of enrollees experiencing high cumulative effective doses was relatively small in our study population, the absolute number individuals at risk may be considerable when our findings are extended to the U.S. population. With approximately 191 million adults age 18-64 years in the U.S.,23 annual effective doses of >20 mSv per year from cardiac imaging procedures would occur in ∼636,000 Americans, if cardiac testing patterns were similar to those in our UHC population.
Of course, radiation exposure from cardiac imaging procedures may be worth the risk for many patients. Certain procedures, such as PCI or device implantation, are performed to mitigate the risk of near-term and even life-threatening cardiac events while the potential malignancy risk from radiation exposure is a long-term stochastic consideration that may occur typically decades after exposure.24 Yet our study demonstrates that there are sizeable rates of radiation exposure for patients aged 35-54 years, many of whom will likely live long enough to potentially develop such long-term complications. Many of these younger patients may be candidates for alternative imaging modalities that do not use ionizing radiation but provide similar clinical information for informed decision-making. For example, alternatives such as stress echocardiography or in some cases exercise testing alone without imaging could serve as alternatives to MPI scans. Similarly, while cardiac blood pool studies contributed a small amount to overall radiation exposure, judicious use of echocardiography or cardiac MRI may lead to lower lifetime doses.
In cases where radiation exposure from cardiac imaging procedures is unavoidable because of clinical need, it is possible that the risks can be reduced even further. Investigators have shown that radiation exposures from cardiac imaging procedures, such as cardiac CT, differ considerably across imaging centers due to variations in equipment, protocols, and experience25, 26 and that radiation exposure can be reduced further by incorporating optimal technical practices.27-31 Given that the current expert consensus is that no level of radiation exposure exists that is not potentially harmful, physicians should guided by a principle of “as low as reasonably achievable” (ALARA) to reduce lifetime biological risk from the radiation exposure associated with cardiac imaging procedures.32
As frequent providers of record for many cardiac imaging services and procedures, cardiologists bear a particular responsibility for minimizing radiation risk to patients while achieving clinical goals, balancing potential benefits from reducing the burden of cardiac disease term in the near-term with potential harm of malignancy in the long-term. Cardiac imaging procedures account for a substantial proportion of the radiation exposure from medical testing. The mean annual effective dose for medical imaging overall in this UHC cohort was previously estimated at 2.4 mSv,5 suggesting that cardiac procedures account for ∼30% of total dose received. This proportion parallels recent findings from cross-sectional data collected by the U.S. National Council on Radiation Protection and Measurements.33
Yet despite their frequent utilization of these studies, cardiologists, like many other physician specialties, are not optimally trained in how to describe the risks of radiation to patients.34, 35 Several reports have demonstrated that patients do not receive information about the radiation dose and risk associated with MPI studies36 or CT scans37, 38 from providers, and equally concerning is that many physicians are often unable to quantify radiation risk.34, 37 Educating cardiologists on more effective methods to inform patients regarding the risks of radiation from cardiac imaging procedures and potential alternatives can help in reducing lifetime radiation exposure.35
The finding that variation in cumulative effective doses of radiation exists across the 5 service markets in our study is not unexpected. Differences in radiation exposure largely reflect regional differences in the rates of cardiac imaging procedures, a previously-established phenomenon.39 Many potential reasons exist that account for regional differences in the use of cardiac imaging procedures with radiation exposure. Differences in patient case mix potentially explain why beneficiaries in Florida were more likely to undergo cardiac imaging procedures, although cumulative radiation dose remained higher even after adjusting for age and sex. Regional differences may also occur if there were differences in the use of alternative imaging modalities that do not use ionizing radiation— factors such as geographic availability, clinical preferences, or level of reimbursement may be important explanatory factors. Lastly, our findings may reflect that cardiac imaging procedures are overused in some areas or underused in others; further research examining whether differences in the appropriateness of cardiac imaging exist across regions is needed.
The relationship between the location of cardiac imaging procedures and cumulative radiation dose is not entirely clear. South Florida and Orlando had the highest annual rates of cumulative radiation dose >3 mSv with the majority of cardiac imaging procedures taking place in physician offices. In contrast, Dallas and Wisconsin had the two lowest annual rates of cumulative radiation dose >3 mSv, but the former had most cardiac imaging procedures performed in physician offices, while the latter had most imaging procedures performed in the hospital-outpatient setting. As such, differences in location of cardiac imaging appear less important than differences in absolute rates of procedure use across service markets. However, as more than half of the radiation from cardiac imaging studies consisted of tests based in physician offices, efforts to monitor and reduce radiation exposure at these facilities may yield greater dose reductions compared with those aimed at hospital-based facilities.
We found that cardiac imaging procedures contributed an increasingly higher proportion of radiation dose with advancing age, for both men and women. This phenomenon is not unexpected as the probability of cardiovascular diseases increases with age. Yet on a population level, we also observe that many young and middle-aged patients appear to have some radiation exposure from cardiac testing. For example, 56 per 1000 beneficiaries aged 35-44 years old in our study population had a cumulative effective dose >3 mSv per year from cardiac imaging procedures; this translates into approximately 2.4 million individuals in the U.S. Because younger patients are likely to continue to be exposed to radiation over time from both cardiac and non-cardiac testing, they are particularly susceptible to higher risks of malignancy over time. Younger women are especially susceptible to the deleterious effects of radiation exposure and have higher cancer risk from a given exposure compared with older women or men.22, 26 Our findings that MPI studies contributed to approximately 80% of all radiation dose for patients age 18-34 years, suggests that alternative modalities to evaluate ischemia (such as stress echocardiography) would decrease the radiation dose substantially for these patients. Among adults with the highest doses of radiation, cardiac catheterization and PCI procedures were important contributors to overall radiation dose. Cardiologists should exercise particular caution using established techniques for minimizing exposure in the cardiac catheterization laboratory, particularly for patients undergoing repeat procedures.40
The urgency for implementing strategies for reducing radiation exposure from cardiac imaging procedures will only increase as the volume of such studies continues to grow in the U.S. For example, reimbursement for screening CT scans for coronary calcium is now mandated in one state,41 and the number of cardiac CT studies will almost certainly increase.42 The expansion of in-office imaging is also thought to be a significant contributor to increased utilization.43 Given that nearly half of all cardiac imaging procedures overall (and three-quarters of MPI and cardiac CT studies) were conducted within physician offices in our study population, increases in in-office imaging will likely continue to lead to increased imaging volume and radiation exposure. As a result, efforts to monitor and reduce the burden of radiation exposure will be progressively more important as the number of cardiac imaging procedures grows.
Our study has a number of limitations. First, our approach to quantifying radiation is based on estimates of effective dose, rather than on a patient-specific measure. These estimates of effective dose rely on a number of assumptions such as the radiosensitivity of specific organs and tissues, specific imaging techniques and protocols, and radionuclide distribution and elimination kinetics.44 These estimates also are limited as they apply to a “reference” individual that represents an age- and sex-averaged person. However, while imperfect, effective dose is the only readily-available measure that reflects the overall potential biological harm across different types of radiation exposure.10, 45 As the focus of our study was to evaluate population-level radiation exposure, the precision of patient-specific radiation dosages is less of a concern compared with the overall patterns of imaging use and radiation burden.
Second, we are unable to determine the appropriate use of these cardiac imaging procedures. Administrative data is inherently limited in its ability to assess the clinical context under which a procedure was used. For example, determination of risk factors such as family history or diabetes mellitus are not available in our data and indications for testing based on ICD-9 diagnostic codes are non-specific, frequently referring to tests ordered to “rule-out” particular conditions. We therefore could not determine whether any of these cardiac imaging procedures could have been substituted with another test or even whether they should have been used at all. However, the focus of this study was to describe the longitudinal radiation exposure currently delivered in actual clinical practice rather than the exposure that would result under optimal conditions.
Third, we are unable to consider operator or facility factors which may affect the dose received. As noted earlier, radiation exposure from cardiac imaging procedures often vary significantly across institutions and equipment vendors.25 Similarly, we did not account for continuing technological advances that lower radiation exposure, such as those that have occurred in cardiac CT.46, 47
Fourth, our study is based on patterns that were observed during 2005-2007. While these data are fairly contemporary, the development of new technologies and protocols for cardiac imaging procedures could have a substantial impact on reducing radiation exposure in the future.48-51 Extrapolation to subsequent years is challenging since advances in cardiac imaging procedures – e.g., complex arrhythmia ablations or percutaneous stent valves – will change patterns of radiation exposure in the general population in unforeseen ways. As an example, while the impact of cardiac CT on overall radiation exposure is small currently, its future impact may be substantial.
Fifth, as the study sample is limited to those continuously enrolled, UHC enrollees who died during the study period may have incurred cardiac imaging procedures with radiation exposure that are not included in our study, underestimating the cumulative rate of exposure. Subjects who leave UHC health insurance plans during this time were also not included; the effect on the cumulative rate of exposure is unknown and depends on whether they were more or less healthy than subjects who remained insured.
Lastly, our study was limited to 5 major healthcare markets with private insurance, and the use of cardiac imaging procedures with radiation outside of those areas may differ in other areas of the United States. Although we included nearly 1 million non-elderly adults, the extent to which our findings can be extrapolated to the elderly or the uninsured is unknown. In addition, studies and procedures performed out of the UHC insurance network that were not reimbursed, in whole or part, would not appear in our data. However, given the substantial cost associated with cardiac testing and procedures, such out-of-pocket services are unlikely to be a major contributor.
In conclusion, cardiac imaging procedures represent an important source of ionizing radiation in the U.S. The overall distribution of cumulative effective doses is skewed and can lead to sizable radiation exposures for many individuals. Better strategies to minimize the radiation exposure from cardiac imaging procedures should be encouraged.
Acknowledgments
We are grateful to Matthew J. Drawz, Tri C. Tong, James C. Dahl, and Neil C. Jensen from UnitedHealthcare for their assistance with the initial preparation of data.
Sources of funding
Dr. Chen is supported in part by an American Heart Association Clinical Research Program Award (AHA 10CRP2640075) and an Agency for Healthcare Research and Quality Career Development Award (1K08HS018781-01). Dr. Ross is supported by the National Institute on Aging (K08 AG032886) and by the American Federation of Aging Research through the Paul B. Beeson Career Development Award Program. Dr Einstein is supported in part by a National Institutes of Health K12 Institutional Career Development Award (5 KL2 RR024157-03).
Footnotes
Disclosures
Dr. Krumholz reports consulting fees for serving on the United Healthcare Cardiac Scientific Advisory Board. He received no fees related to this project. Dr Einstein reports having received research support from Spectrum Dynamics. No other potential conflicts of interest relevant to this article were reported by any of the authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lucas FL, DeLorenzo MA, Siewers AE, Wennberg DE. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993-2001. Circulation. 2006;113(3):374–379. doi: 10.1161/CIRCULATIONAHA.105.560433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.IMV. IMV 2003 Nuclear Medicine Census Market Summary Report. Des Plaines, IL: IMV Medical Information Division; 2003. [Google Scholar]
- 3.IMV. IMV 2006 Cardiac Catheterization Lab Census Market Summary Report. Des Plaines, IL: IMV Medical Information Division; 2006. [Google Scholar]
- 4.IMV. IMV 2008. Present Practices & Future Directions in Cardiac Imaging, The Cardiologist's Perspective 2008-2011. Des Plaines, IL: IMV Medical Information Division; 2008. [Google Scholar]
- 5.Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, Shah ND, Nasir K, Einstein AJ, Nallamothu BK. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009;361(9):849–857. doi: 10.1056/NEJMoa0901249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bedetti G, Botto N, Andreassi MG, Traino C, Vano E, Picano E. Cumulative patient effective dose in cardiology. Br J Radiol. 2008;81(969):699–705. doi: 10.1259/bjr/29507259. [DOI] [PubMed] [Google Scholar]
- 7.United States Government Accountability Office. Medicare Part B Imaging Services. Rapid spending growth and shift to physician offices indicate need for CMS to consider additional management practices. Washington DC: United States Government Accountability Office; 2006. [Google Scholar]
- 8.Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, Lubin JH, Preston DL, Preston RJ, Puskin JS, Ron E, Sachs RK, Samet JM, Setlow RB, Zaider M. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci U S A. 2003;100(24):13761–13766. doi: 10.1073/pnas.2235592100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.International Commission on Radiological Protection. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37(2-4):1–332. doi: 10.1016/j.icrp.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 10.Martin CJ. Effective dose: how should it be applied to medical exposures? Br J Radiol. 2007;80(956):639–647. doi: 10.1259/bjr/25922439. [DOI] [PubMed] [Google Scholar]
- 11.Martin CJ. The application of effective dose to medical exposures. Radiat Prot Dosimetry. 2008;128(1):1–4. doi: 10.1093/rpd/ncm425. [DOI] [PubMed] [Google Scholar]
- 12.International Commission on Radiological Protection. Radiation protection in medicine. ICRP publication 105. Ann ICRP. 2007;37(6):1–63. doi: 10.1016/j.icrp.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Mettler FA, Jr, Huda W, Yoshizumi TT, Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology. 2008;248(1):254–263. doi: 10.1148/radiol.2481071451. [DOI] [PubMed] [Google Scholar]
- 14.Buls N, Pages J, de Mey J, Osteaux M. Evaluation of patient and staff doses during various CT fluoroscopy guided interventions. Health Phys. 2003;85(2):165–173. doi: 10.1097/00004032-200308000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Perisinakis K, Theocharopoulos N, Damilakis J, Manios E, Vardas P, Gourtsoyiannis N. Fluoroscopically guided implantation of modern cardiac resynchronization devices: radiation burden to the patient and associated risks. J Am Coll Cardiol. 2005;46(12):2335–2339. doi: 10.1016/j.jacc.2005.01.070. [DOI] [PubMed] [Google Scholar]
- 16.Perisinakis K, Damilakis J, Theocharopoulos N, Manios E, Vardas P, Gourtsoyiannis N. Accurate assessment of patient effective radiation dose and associated detriment risk from radiofrequency catheter ablation procedures. Circulation. 2001;104(1):58–62. doi: 10.1161/hc2601.091710. [DOI] [PubMed] [Google Scholar]
- 17.Einstein AJ, Moser KW, Thompson RC, Cerqueira MD, Henzlova MJ. Radiation dose to patients from cardiac diagnostic imaging. Circulation. 2007;116(11):1290–1305. doi: 10.1161/CIRCULATIONAHA.107.688101. [DOI] [PubMed] [Google Scholar]
- 18.Henzlova M, Cerqueria MD, Hansen CL, Taillefer R, Yao S. ASNC Imaging Guidelines for Nuclear Cardiology Procedures: Stress Protocols and Tracers. Journal of Nuclear Cardiology. 2009;16(2):331. [Google Scholar]
- 19.IMV. IMV 2005 Nuclear Medicine Census Market Summary Report. Des Plaines, IL: IMV Medical Information Division; 2005. [Google Scholar]
- 20.Friis RH, Selles TA. Epidemiology for Public Health Practice, chapter 3. Sudbury, MA: Jones and Bartlett Publishers; 2009. [Google Scholar]
- 21.National Research Council. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII - Phase 2. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 22.Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. Jama. 2007;298(3):317–323. doi: 10.1001/jama.298.3.317. [DOI] [PubMed] [Google Scholar]
- 23.Population Division U.S. Census Bureau. Table 1: Annual Estimates of the Resident Population by Sex and Five-Year Age Groups for the United States: April 1, 2000 to July 1, 2008 (NC-EST2008-01) [July 20,2009];2009 available at http://www.census.gov/popest/national/asrh/NC-EST2008-sa.html.
- 24.Amis ES, Jr, Butler PF, Applegate KE, Birnbaum SB, Brateman LF, Hevezi JM, Mettler FA, Morin RL, Pentecost MJ, Smith GG, Strauss KJ, Zeman RK. American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol. 2007;4(5):272–284. doi: 10.1016/j.jacr.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Hausleiter J, Meyer T, Hermann F, Hadamitzky M, Krebs M, Gerber TC, McCollough C, Martinoff S, Kastrati A, Schomig A, Achenbach S. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301(5):500–507. doi: 10.1001/jama.2009.54. [DOI] [PubMed] [Google Scholar]
- 26.Kim KP, Einstein AJ, Berrington de Gonzalez A. Coronary artery calcification screening: estimated radiation dose and cancer risk. Arch Intern Med. 2009;169(13):1188–1194. doi: 10.1001/archinternmed.2009.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stephen B. Radiation safety in the cardiac catheterization laboratory: Operational radiation safety. Catheterization and Cardiovascular Interventions. 1999;47(3):347–353. doi: 10.1002/(sici)1522-726x(199907)47:3<347::aid-ccd23>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 28.Jakobs TF, Becker CR, Ohnesorge B, Flohr T, Suess C, Schoepf UJ, Reiser MF. Multislice helical CT of the heart with retrospective ECG gating: reduction of radiation exposure by ECG-controlled tube current modulation. Eur Radiol. 2002;12(5):1081–1086. doi: 10.1007/s00330-001-1278-x. [DOI] [PubMed] [Google Scholar]
- 29.Ficaro EP, Zanzonico P, Stabin MG, Raff GL, Thompson RC, Einstein AJ, Henzlova MJ, Budoff MJ, Dilsizian V, Laskey WK, Lima J, Roti Roti JL, Bateman TM ASNC Information Statement. Variability in radiation dose estimates from nuclear and computed tomography diagnostic imaging. [August 8, 2009];2008 Available at http://www.asnc.org/imageuploads/InformationStatementRadiationDosimetry2009.pdf.
- 30.Raff GL, Chinnaiyan KM, Share DA, Goraya TY, Kazerooni EA, Moscucci M, Gentry RE, Abidov A Advanced Cardiovascular Imaging Consortium C-I. Radiation Dose From Cardiac Computed Tomography Before and After Implementation of Radiation Dose-Reduction Techniques. JAMA. 2009;301(22):2340–2348. doi: 10.1001/jama.2009.814. [DOI] [PubMed] [Google Scholar]
- 31.Hausleiter J, Meyer T, Hermann F, Hadamitzky M, Krebs M, Gerber TC, McCollough C, Martinoff S, Kastrati A, Schomig A, Achenbach S. Estimated Radiation Dose Associated With Cardiac CT Angiography. JAMA. 2009;301(5):500–507. doi: 10.1001/jama.2009.54. [DOI] [PubMed] [Google Scholar]
- 32.Prasad KN, Cole WC, Haase GM. Radiation protection in humans: extending the concept of as low as reasonably achievable (ALARA) from dose to biological damage. Br J Radiol. 2004;77(914):97–99. doi: 10.1259/bjr/88081058. [DOI] [PubMed] [Google Scholar]
- 33.Mettler FA, Bhargavan M, Faulkner K, Gilley DB, Gray JE, Ibbott GS, Lipoti JA, Mahesh M, McCrohan JL, Stabin MG, Thomadsen BR, Yoshizumi TT. Radiologic and Nuclear Medicine Studies in the United States and Worldwide: Frequency, Radiation Dose, and Comparison with Other Radiation Sources-”1950-2007. Radiology. 2009;253(2):520–531. doi: 10.1148/radiol.2532082010. [DOI] [PubMed] [Google Scholar]
- 34.Correia MJ, Hellies A, Andreassi MG, Ghelarducci B, Picano E. Lack of radiological awareness among physicians working in a tertiary-care cardiological centre. Int J Cardiol. 2005;103(3):307–311. doi: 10.1016/j.ijcard.2004.08.070. [DOI] [PubMed] [Google Scholar]
- 35.Picano E, Vano E, Semelka R, Regulla D. The American College of Radiology white paper on radiation dose in medicine:deep impact on the practice of cardiovascular imaging. Cardiovasc Ultrasound. 2007;5:37. doi: 10.1186/1476-7120-5-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bedetti G, Pizzi C, Gavaruzzi G, Lugaresi F, Cicognani A, Picano E. Suboptimal awareness of radiologic dose among patients undergoing cardiac stress scintigraphy. J Am Coll Radiol. 2008;5(2):126–131. doi: 10.1016/j.jacr.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 37.Lee CI, Haims AH, Monico EP, Brink JA, Forman HP. Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology. 2004;231(2):393–398. doi: 10.1148/radiol.2312030767. [DOI] [PubMed] [Google Scholar]
- 38.Caoili EM, Cohan RH, Ellis JH, Dillman J, Schipper MJ, Francis IR. Medical Decision Making Regarding Computed Tomographic Radiation Dose and Associated Risk: The Patient's Perspective. Arch Intern Med. 2009;169(11):1069–1071. doi: 10.1001/archinternmed.2009.139. [DOI] [PubMed] [Google Scholar]
- 39.Wennberg D. The Dartmouth Atlas of Cardiovascular Health Care. Chicago: AHA Press; 1999. [Google Scholar]
- 40.Kuon E, Glaser C, Dahm JB. Effective techniques for reduction of radiation dosage to patients undergoing invasive cardiac procedures. Br J Radiol. 2003;76(906):406–413. doi: 10.1259/bjr/82051842. [DOI] [PubMed] [Google Scholar]
- 41.Beller GA. The Texas Heart Attack Prevention Bill mandating coverage for CAD screening tests. J Nucl Cardiol. 2009 doi: 10.1007/s12350-009-9139-0. [DOI] [PubMed] [Google Scholar]
- 42.Ladapo JA, Horwitz JR, Weinstein MC, Gazelle GS, Cutler DM. Adoption And Spread Of New Imaging Technology: A Case Study. Health Aff. 2009;28(6):w1122–1132. doi: 10.1377/hlthaff.28.6.w1122. [DOI] [PubMed] [Google Scholar]
- 43.Medicare Payment Advisory Commission (MEDPAC) Report to Congress: Improving incentives in the Medicare program, chapter 4. Washington, D.C.: Jun, 2009. [Google Scholar]
- 44.Gerber TC, Carr JJ, Arai AE, Dixon RL, Ferrari VA, Gomes AS, Heller GV, McCollough CH, McNitt-Gray MF, Mettler FA, Mieres JH, Morin RL, Yester MV. Ionizing Radiation in Cardiac Imaging. A Science Advisory From the American Heart Association Committee on Cardiac Imaging of the Council on Clinical Cardiology and Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention. Circulation. 2009;119(7):1056–1065. doi: 10.1161/CIRCULATIONAHA.108.191650. [DOI] [PubMed] [Google Scholar]
- 45.Dietze G, Harrison JD, Menzel HG. Effective dose: a flawed concept that could and should be replaced. Comments on a paper by D J Brenner (Br J Radiol 2008;81:521-3) Br J Radiol. 2009;82(976):348–350. doi: 10.1259/bjr/91937653. author reply 350-341. [DOI] [PubMed] [Google Scholar]
- 46.McCollough CH. CT dose: how to measure, how to reduce. Health Phys. 2008;95(5):508–517. doi: 10.1097/01.HP.0000326343.35884.03. [DOI] [PubMed] [Google Scholar]
- 47.Earls JP, Berman EL, Urban BA, Curry CA, Lane JL, Jennings RS, McCulloch CC, Hsieh J, Londt JH. Prospectively gated transverse coronary CT angiography versus retrospectively gated helical technique: improved image quality and reduced radiation dose. Radiology. 2008;246(3):742–753. doi: 10.1148/radiol.2463070989. [DOI] [PubMed] [Google Scholar]
- 48.Berman DS, Kang X, Tamarappoo B, Wolak A, Hayes SW, Nakazato R, Thomson LE, Kite F, Cohen I, Slomka PJ, Einstein AJ, Friedman JD. Stress thallium-201/rest technetium-99m sequential dual isotope high-speed myocardial perfusion imaging. JACC Cardiovasc Imaging. 2009;2(3):273–282. doi: 10.1016/j.jcmg.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 49.Sharir T, Ben-Haim S, Merzon K, Prochorov V, Dickman D, Berman DS. High-speed myocardial perfusion imaging initial clinical comparison with conventional dual detector anger camera imaging. JACC Cardiovasc Imaging. 2008;1(2):156–163. doi: 10.1016/j.jcmg.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 50.Esteves FP, Raggi P, Folks RD, Keidar Z, Wells Askew J, Rispler S, O'Connor MK, Verdes L, Garcia EV. Novel solid-state-detector dedicated cardiac camera for fast myocardial perfusion imaging: multicenter comparison with standard dual detector cameras. J Nucl Cardiol. 2009 doi: 10.1007/s12350-009-9137-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Slomka PJ, Patton JA, Berman DS, Germano G. Advances in technical aspects of myocardial perfusion SPECT imaging. J Nucl Cardiol. 2009;16(2):255–276. doi: 10.1007/s12350-009-9052-6. [DOI] [PubMed] [Google Scholar]


