Abstract
The results of 393 consecutive orthotopic liver transplants in 313 patients were reviewed to determine the incidence of primary biliary tract complications. There were 52 biliary tract complications in 393 grafts (13.2%), and 5 directly related deaths. Choledochojejunostomy over an internal stent to a Roux-en-Y limb of proximal jejunum (RYCJ-S) was the most frequently used technique (175 cases) and the most successful with only 9 technical failures (5.2%). Choledochocholedochostomy over a T tube (CC-T) was used in 159 cases and was successful in all but 20 cases (12.6%). Other methods of reconstruction were associated with high failure rates or technical complexity that do not justify their use.
Biliary leak and obstruction were the most common complications. Leakage after CC-T at the T tube exit site was usually directly repaired, but anastomotic leakage required conversion to RYCJ-S. Obstruction may be relieved by percutaneous balloon dilatation but definitive treatment also usually required conversion to RYCJ-S.
The most common complication after RYCJ-S is functional obstruction by a retained stent, which has a low morbidity but may necessitate surgical removal. Anastomotic leaks, which occurred in 2 cases, were successfully managed by revision of the choledochojejunostomy.
The use of cyclosporine-prednisone therapy and standardization of techniques of liver procurement and implantation have resulted in dramatic improvement in patient survival after orthotopic liver transplantation (1-3). Nevertheless, technical complications are still responsible for substantial morbidity and mortality.
We have previously reported our experience with biliary tract complications after orthotopic liver transplantation for 90 transplants in 78 patients (4). This report extends our experience to a consecutive series of 393 orthotopic liver transplantations in 313 patients.
MATERIALS AND METHODS
Case material
Between March 1, 1980 and December 31, 1984, 313 patients including 177 adults and 136 children received a primary orthotopic liver transplant. Fourteen operations were done at the University of Colorado Health Sciences Center in Denver, Colorado and the rest at the University Health Center of Pittsburgh, Pittsburgh, Pennsylvania. Sixty-eight patients received a second transplant and 12 patients a third liver transplant in this series.
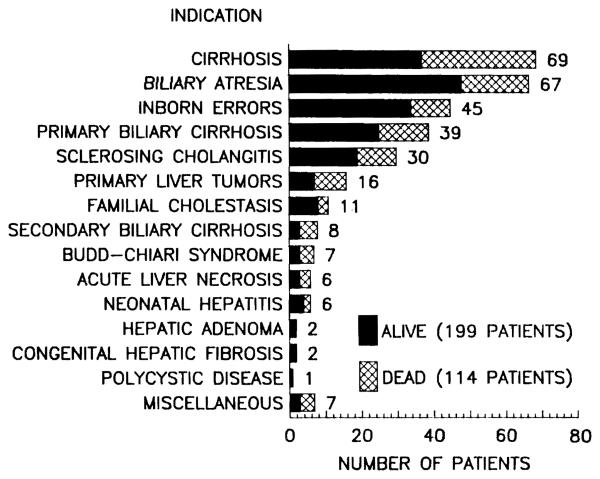
The indications for primary grafts are summarized in Figure 1. Cirrhosis was the most common indication for liver replacement. Most of these patients had chronic aggressive hepatitis, but a small number had cryptogenic cirrhosis or Laennec's cirrhosis. Biliary atresia was the second most common indication and accounted for nearly 50% of the transplantations in children. Sixty-two (45.6%) of the pediatric patients and 137 (77.4%) of the adult patients were free of primary disease of the extrahepatic biliary system.
Figure 1.
Indications for liver transplantation in 313 consecutive patients between March 1, 1980 and December 31, 1984.
Immunosuppression
All patients were treated with combination cyclosporine-prednisone therapy, as described elsewhere (1, 3, 5). In the last few months of this series, OKT3 monoclonal antibody (Ortho Pharmaceuticals, Raritan, NJ) was used for the treatment of acute steroid-resistant rejection or as temporary therapy in patients unable to tolerate therapeutic doses of cyclosporine (6).
Surgical technique
The techniques of donor hepatectomy and graft implantation have been described in detail elsewhere (5, 7, 8). We here mention only those features of the operation pertinent to biliary tract reconstruction.
During the donor hepatectomy, the common bile duct is divided as distally as possible and the biliary system is flushed with saline through an incision in the fundus of the gallbladder. This prevents damage to the bile duct epithelium from residual bile.
During recipient hepatectomy, the proximal common bile duct is divided as high as possible. Biliary reconstruction is deferred until completion of all vascular anastomoses and until after complete hemostasis has been achieved. If both donor and recipient ducts are suitable, a primary choledochocholedochostomy over a T-tube (CC-T)* is performed with a single layer of interrupted 5–0 polyglycolic acid suture. The T tube is brought out through a stab incision in the recipient common duct at least 5 mm from the duct-to-duct anastomosis and contralateral to nearby vascular suture lines.
If preexisting biliary tract disease or inadequacies of duct size do not permit a direct duct-to-duct anastomosis, an 18-inch Roux-en-Y limb of proximal jejunum is constructed and used to perform an end to side choledocho-jejunostomy over an internal stent (RYCJ-S). The anastomosis is single-layer 5–0 or 6–0 interrupted or running polyglycolic acid suture and an infant polyethylene feeding tube, secured in place with a single 6–0 chromic catgut suture, is used for the internal stent.
The Waddell-Calne procedure (9, 10) in which the gallbladder is used as a conduit between donor and recipient biliary tract has been rarely used by us. Primary duct reconstruction over an internal stent, cholecystoenterostomy, tube cholecystostomy or choledochostomy, or simple external drainage have been used only in exceptional circumstances.
All cases were reviewed to determine the incidence, treatment, and outcome of primary surgical failures of biliary tract reconstruction. All patients have been followed for at least one year since transplantation.
RESULTS
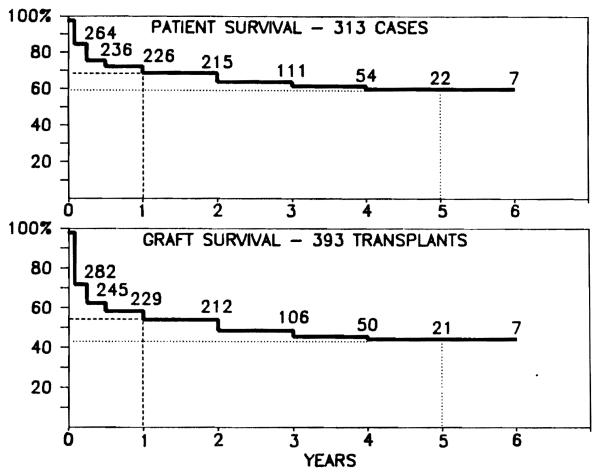
Survival for the 313 patients and 393 grafts is presented in Figure 2. There are 199 (63.6%) surviving patients. Patient survival is 68.3% at one year and 59.9% at five years. There are 189 (48.1%) surviving grafts (ten patients are surviving with retransplants done after 1984).
Figure 2.
Survival (life table method) of 313 recipients of 393 liver transplants done between March 1, 1980 and December 31, 1984. Follow-up is complete through January 31, 1986.
Technical complications, summarized in Table 1, occurred in 87 of the 393 (22.1%) grafts and were responsible for the loss of 38 grafts (9.6%) and 24 patients (7.6%). Twenty-five retransplantations were performed for technical failures of a previous graft, 14 of which were successful.
Table 1.
Technical complications in 393 orthotopic liver transplants
| Complication | Grafts (393) | Patients (313) | Retransplantations |
Deaths |
||
|---|---|---|---|---|---|---|
| Successful | Failed | Unrelated | Related | |||
| Biliary tract | 52 (13.2%) | 52 (16.6%) | 3 | 1 | 2 | 5 (9.6%) |
| Hepatic artery thrombosis | 27 (6.8%) | 25 (7.9%) | 10 | 8 | — | 16 (64.0%) |
| Portal vein thrombosis | 6 (1.5%) | 6 (1.9%) | — | 1 | 1 | 2 (40.0%) |
| Portal vein stenosis | 2 (0.5%) | 2 (0.6%) | — | — | — | — |
| Portal vein and inferior vena cava thrombosis | 1 (0.3%) | 1 (0.3%) | 1 | — | — | — |
| Inferior vena cava thrombosis | 2 (0.5%) | 2 (0.6%) | — | 1 | 1 | 1 (50.0%) |
| Total | 87 (22.1%) | 85 (27.1%) | 14 | 11 | 6 | 24 (7.6%) |
Biliary tract complications occurred in 52 of the 393 grafts (13.2%), and thus accounted for 59.8% of the 87 technical failures. There were 17 failures in pediatric grafts (10.0%) and 35 failures in adult grafts (16.2%). The incidence of biliary tract complications has declined significantly from 24.4% during 1980–1982 to 8.0% in 1984.
The incidence of complications is summarized according to the method of biliary tract reconstruction in Table 2.
Table 2.
Primary biliary complications according to technique of reconstruction
| Type | CC-T | CC-S | RYCJ-S | Waddell- Calne |
Cholecysto- enterostomy |
External drainage |
|---|---|---|---|---|---|---|
| Number | 159 | 32 | 175 | 6 | 7 | 5 |
| Successes | 139 (87.4%) | 18 (56.2%) | 166 (94.8%) | 5 (83.4%) | 1 (14.3%) | — |
| Failures | 20 (12.6%) | 14 (43.8%) | 9 (5.2%) | 1 (16.6%) | 6 (85.7%) | 2 (40.0%) |
| Biliary leak | 15 | 7 | 3 | 1 | 1 | — |
| Obstruction | 5 | 5 | 4 | — | 5 | 1 |
| Hemobilia | — | 2 | — | — | — | 1 |
| Torsion of Roux limb | — | — | 1 | — | — | — |
| Biliary cast syndrome | — | — | 1 | — | — | — |
| Intrahepatic strictures | — | — | 1 | — | — | — |
Choledochocholedochostomy with T tube stent
Primary duct repair over a T tube stent (CC-T) was used in 159 reconstructions, including 24 children and 135 adults. Complications occurred in 20 cases (12.6%), including 4 pediatric cases (16.6%) and 16 adult cases (11.8%).
Biliary leakage, which occurred in 15 cases, was the most common complication. Eleven leaks occurred at the T tube exit site with no or minimal symptoms. Simple drainage or closure of the opening in the bile duct was sufficient treatment in most cases. One patient required conversion to RYCJ-S because the T tube exit site was too close to the primary duct anastomosis for repair.
Leakage at the biliary anastomosis, which occurred in 4 patients, was a serious complication. Two patients died of sepsis and another required retransplantation after failure of an attempt at direct repair.
Biliary tract obstruction occurred in 5 cases, four within 90 days of transplantation. In 3 patients the obstruction was caused by the T tube itself, and in 2 of these it was resolved by removal of the T tube. One patient developed obstruction at the duct anastomosis that was successfully treated by percutaneous transhepatic balloon dilatation (PTD). Ten months later the patient required endoscopic removal of common bile duct stones. The fifth patient developed a stricture of the proximal common hepatic duct which was treated by PTD but recurred within 2 years, necessitating conversion to a choledochojejunostomy.
Choledochocholedochostomy with internal stent (CC-S)
Primary duct-to-duct repair over an internal stent (CC-S) was only done in 32 cases, including 17 children and 15 adults. Complications occurred in 14 cases (43.8%), including 6 pediatric (35.3%) and 8 adult patients (53.3%). There were 7 biliary leaks, 5 obstructions, and 2 cases of hemobilia. Two patients died as a direct consequence of these complications.
All seven biliary fistulas occurred at the biliary anastomosis soon after operation. Conversion to RYCJ-S was attempted in 4 patients and was successful in 2 of them. One patient died of cytomegalovirus and Candida infection. Another patient, suspected of having inadequate vascular supply to the distal common duct, required a second RYCJ-S to correct a late anastomotic stricture with stones. Conversion to CC-T was attempted in 3 cases but was only successful in one. One patient developed a second leak and was successfully converted to RYCJ-S. Another patient died from graft failure 2 days after repair.
A fistula between the hepatic artery and common bile duct occurred as septicemia and upper gastrointestinal bleeding 2 months after transplantation in one case. Angiography demonstrated a hepatic artery aneurysm. At laparotomy, a mycotic aneurysm was resected and replaced with an arterial homograft. However, the patient re-bled and died.
One patient had hemobilia 2½ years after transplantation caused by irritation of the ampulla of Vater by a retained stent. The stent was removed at endoscopy. Two months later the patient was converted to RYCJ-S for choledocholithiasis.
Four of the 5 obstructions after CC-S occurred more than 3 months after transplantation. One was managed by removal of the stent at 8 months. Multiple stones were later found in the bile duct when the patient was retransplanted for chronic graft rejection. One patient was successfully treated by PTD. Three patients were successfully converted to RYCJ-S, including one patient who also had successful portal vein thrombectomy and resection of a portal vein stenosis.
Choledochojejunostomy with internal stent (RYCJ-S)
Anastomosis over an internal stent of the end of the graft common bile duct to the side of a Roux-en-Y limb of proximal jejunum was used in 175 reconstructions, including 126 children and 49 adults. Complications occurred in only 9 cases (5.1%), including 3 pediatric (2.3%) and 6 adult patients (12.2%).
There were 2 anastomotic leaks and one leak caused by a tear in the donor duct near the cystic duct that had been used to insert the stent. All were successfully repaired by revision of the choledochojejunostomy.
Three patients required laparotomy for removal of a retained stent causing functional biliary obstruction. A fourth patient with clinical signs of obstruction, including dilatation of the intrahepatic bile ducts, was explored after several attempts at PTD, but intraoperative cholangiography failed to find a site of stenosis. The anastomosis was stented with a T tube.
One patient developed torsion of the Roux-en-Y jejunal limb 3 months after transplantation. A new jejunal limb was constructed.
A 9-year old boy transplanted for Allagille's syndrome developed dilatation of the intrahepatic bile ducts with numerous casts filling the ducts. There was no obvious obstruction of the choledochojejunostomy. Lavage-drainage by a percutaneous stent failed, even after use of mono-octanoin (Capumil). Revision of the anastomosis produced no improvement. The patient was successfully given another transplant after 87 days. The resected specimen confirmed the presence of numerous bile casts in both dilated and nondilated intrahepatic bile ducts but no mechanical obstruction was identified.
There were 6 patients who developed intestinal fistulas from the Roux-en-Y jejunal limb. However, these complications were associated with other abdominal catastrophes (evisceration, electrocautery injury to the bowel, and intra-abdominal sepsis from other causes) and were not specifically related to the type of biliary reconstruction.
Other reconstructions
The Waddell-Calne gallbladder conduit was used in only 4 pediatric and 2 adult patients. Since 2 patients died of early graft failure and 2 patients had an early retransplantation using another method of reconstruction, our experience with this method is too limited for meaningful evaluation.
Cholecystoduodenostomy (1 case) or cholecystoenterostomy (6 cases) were used in 3 pediatric and 4 adult patients. Complications occurred in 6 cases. One patient died as a result of an unrecognized bile leak from a faulty ligature on the distal common bile duct. One pediatric patient developed a large fungal liver abscess 2 weeks after operation and was successfully given another graft using RYCJ-S. In four patients early obstruction of the cystic duct required conversion to RYCJ-S. One of these patients died within 3 weeks of hepatic failure and sepsis and another required retransplantation for an injury to the portal vein that occurred at reoperation.
External biliary drainage was performed in 2 pediatric and 3 adult patients who were unstable and required rapid completion of the operation. Two patients survived and required early conversion to RYCJ-S because of bleeding in the gallbladder or obstruction.
DISCUSSION
Throughout the development of orthotopic liver transplantation, the biliary tract reconstruction has always been responsible for the most technical complications (3, 4, 11-17). Many of the problems encountered in the early years of liver transplantation can be traced to the use of inappropriate techniques (16, 17) and delay in recognition and treatment of complications (15, 16). In our early experience beginning in 1963, one of every three recipients developed a biliary obstruction or fistula (15, 16). Even without these complications, there was a high incidence of bacteremia, probably caused by constant contamination of the biliary tree through the cholecystoduodenostomy, which was often used until the early 1970s.
By 1973, cholecystojejunostomy became the preferred method of reconstruction. However, narrowing and kinking of the cystic duct was frequently responsible for persistent postoperative jaundice (16). Recognition of this problem permitted successful conversion of these grafts to choledochojejunostomy (15, 16). In recent years, this procedure has been limited only to patients in whom urgency or technical difficulty do not permit direct duct-to-duct repair or cholecystojejunostomy.
Our experience with the Waddell-Calne gallbladder conduit has been limited. The complexity of the procedure and its lack of significant advantages has led us to prefer other conventional methods of reconstruction.
In recent years CC-T or RYCJ-S have been our preferred methods of reconstruction (3, 4, 6). Together, these methods were successful in 305 of 334 grafts (91.3%). Similar good results have been reported recently in two smaller series (11, 18). CC-T is an ideal method of reconstruction in the recipient with a normal native bile duct; the technique is simple and preserves the sphincter of Oddi. The T tube stent protects the bile duct from leakage and stricture and provides easy access for diagnostic studies. The exit site of the T tube should be at least 5 mm from the transection margin of the recipient bile duct to prevent necrosis of the intervening segment and contralateral to the neighboring vascular anastomoses to minimize the risk of biliary-vascular fistula. The T tube is clamped as soon as liver function permits (total bilirubin <2–3 mg/dl). Cyclosporine absorption usually improves with clamping of the T tube and adjustments in dosage may be required. The T tube is left in place for 2 to 3 months after the operation.
Early recognition of bile leakage or obstruction after CC-T permits prompt treatment with minimum morbidity and mortality. The T tube exit site is a frequent site of leaks and can often be managed by primary repair. Anastomotic leaks are more dangerous and are usually best treated by conversion to RYCJ-S. Obstruction is a less-frequent complication, can occur early or late, and may be caused by ischemic stricture, severe size discrepancy between donor and recipient ducts, errors in surgical technique, or functional obstruction by the T tube. Percutaneous dilatation has been of benefit in a few cases, but is often only of temporary benefit. Conversion to RYCJ-S is definitive.
If the recipient duct is diseased, absent, too short, or too small—or if the graft duct cannot accept a T tube—end-to-side RYCJ-S is the best alternative and has been, in our hands, the most reliable method of biliary reconstruction (94.8% success). The most frequent complication of this method, functional obstruction of the biliary tree by a retained stent, has little morbidity or mortality, but may necessitate surgical removal of the stent.
Duct-to-duct repair over an internal stent is a tempting alternative when the bile duct of the graft or the recipient is too small to accept a T tube. However, in our experience this method is associated with a high rate of serious complications (45.3%) and RYCJ-S should be performed instead.
Most biliary tract complications occur in the first weeks after transplantation and the differential diagnosis includes rejection, hepatic artery thrombosis with secondary biliary tract ischemic injury (19), and primary graft dysfunction. Ultrasound examinations may detect duct dilatation and intra- or extrahepatic collections, but a negative study is unreliable. T tube, ERCP, or percutaneous cholangiography can demonstrate obstruction or bile fistula (20). Even seemingly small, asymptomatic bile leaks merit prompt repair since peritonitis and infection of vascular anastomoses are significant risks.
Bile cast syndrome (15) with sludge precipitation throughout the biliary tree occurred in one case in this series. An unrecognized partial obstruction was suspected but could not be proved. During the early postoperative period there was no evidence of allograft rejection, sepsis, or drug toxicity. Retransplantation was performed successfully after 3 months. It is possible that early bile sludge is the result of an ischemic injury of the bile mucosa.
This extended review of our experience with biliary tract reconstruction confirms the findings of our earlier report (4). The biliary tract complication is no longer the “Achilles' heel” of liver transplantation. Reliance upon standardized methods of direct duct-to-duct repair or choledochojejunostomy have reduced the complication rate to less than 10%. Prompt recognition and proper treatment can markedly reduce the morbidity and mortality of complications that do occur.
Many of the patients in this series have only been followed for 12 to 18 months. Even longer follow-up will be necessary to identify significant numbers of late biliary tract complications.
Footnotes
Presented at the 12th Annual Meeting of the American Society of Transplant Surgeons, May 1986, Chicago, IL.
This work was supported by Research Project Grant AM-29961 from the National Institutes of Health, Bethesda, MD.
Abbreviations used: CC-S, choledochocholedochostomy with internal stent; CC-T, choledochocholedochostomy over a T tube; PTD, percutaneous transhepatic dilatation; RYCJ-S, choledochojejunostomy over an internal stent to a Roux-en-Y limb of proximal jejunum.
REFERENCES
- 1.Starzl TE, Iwatsuki SI, Shaw BW, Jr, Gordon RD. Orthotopic liver transplantation in 1984. Transplant Proc. 1985;17:250. [PMC free article] [PubMed] [Google Scholar]
- 2.Gordon RD, Shaw BW, Jr, Iwatsuki SI, Esquivel CO, Starzl TE. Indications for liver transplantation in the cyclosporine era. In: Roberts AJ, Painvin GA, editors. Surgical clinics of North America. Vol. 66. Saunders; Philadelphia: 1986. p. 541. [DOI] [PubMed] [Google Scholar]
- 3.Starzl TE, Iwatsuki SI, Van Thiel DH, et al. Evolution of liver transplantation. Hepatology. 1982;2:614. doi: 10.1002/hep.1840020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iwatsuki SI, Shaw BW, Jr, Starzl TE. Biliary tract complications in liver transplantation under cyclosporine-steroid therapy. Transplant Proc. 1983;15:1288. [PMC free article] [PubMed] [Google Scholar]
- 5.Starzl TE, Iwatsuki SI, Shaw BW, Jr, et al. Factors in the development of liver transplantation. Transplant Proc. 1985;17:107. [PMC free article] [PubMed] [Google Scholar]
- 6.Fung JJ, Demetris AJ, Porter KA, et al. Use of OKT3 with cyclosporine and steroids for reversal of acute kidney and liver allograft rejection. Nephron. doi: 10.1159/000184431. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Starzl TE, Iwatsuki SI, Esquivel CO, et al. Refinements in the surgical technique of liver transplantation. Semin Liver Dis. 1985;5:349. doi: 10.1055/s-2008-1040632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Starzl TE, Hakala TR, Shaw BW, Jr, et al. A flexible procedure for multiple cadaveric organ procurement. Surg Gynecol Obstet. 1984:223. [PMC free article] [PubMed] [Google Scholar]
- 9.Waddell WR, Grover FL. The gallbladder as a conduit between the liver and intestine. Surgery. 1973;74:524. [PubMed] [Google Scholar]
- 10.Calne RY. A new technique for biliary drainage in orthotopic liver transplantation utilizing the gallbladder as a pedicle graft conduit between the donor and recipient bile ducts. Ann Surg. 1976;184:605. doi: 10.1097/00000658-197611000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krom RAF, Kingma LM, Haagsma EB, Wesenhagen H, Sloof MJH, Gips CH. Choledocho-eholedochochostomy, a relatively safe procedure in orthotopic liver transplantation. Surgery. 1985;97:522. [PubMed] [Google Scholar]
- 12.Neuhaus P, Brolsch CR, Ringe B, Lauchart W, Pichylmayr R. Results of biliary reconstruction after liver transplantation. Transplant Proc. 1984;16:1225. [PubMed] [Google Scholar]
- 13.Rolles K. Early biliary tract complications. In: Calne RY, editor. Liver transplantation. Grune & Stratton; London: 1983. p. 319. [Google Scholar]
- 14.Scudamore CH. Late biliary tract complications. In: Cane RY, editor. Liver transplantation. Grune & Stratton; London: 1983. p. 327. [Google Scholar]
- 15.Starzl TE, Putnam CW, Hansbrough JF, Porter KA, Reid HAS. Biliary complications after liver transplantation: with special reference to the biliary cast syndrome and techniques of secondary duct repair. Surgery. 1977;81:212. [PubMed] [Google Scholar]
- 16.Starzl TE, Ishikawa M, Putnam CW, et al. Progress in and deterrents to orthotopic liver transplantation, with special reference to survival, resistance to hyperacute rejection, and bile duct reconstruction. Transplant Proc. 1974;6:129. [PMC free article] [PubMed] [Google Scholar]
- 17.Martineau G, Porter KA, Gorman J, et al. Delayed biliary duct obstruction after orthotopic liver transplantation. Surgery. 1972;72:604. [PMC free article] [PubMed] [Google Scholar]
- 18.Wolff H, Otto G, David H. Biliary tract reconstruction in liver transplantation. Transplant Proc. 1985;17:274. [Google Scholar]
- 19.Tzakis AG, Gordon RD, Shaw BW, Jr, Iwatsuki S, Starzl TE. Clinical presentation of hepatic artery thrombosis after liver transplantation in the cyclosporine era. Transplantation. 1985;40:667. doi: 10.1097/00007890-198512000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zajko AB, Campbell WL, Brons KM, et al. Cholangiography and interventional biliary radiology in adult liver transplantation. Am J Radiology. 1985;144:127. doi: 10.2214/ajr.144.1.127. [DOI] [PMC free article] [PubMed] [Google Scholar]