Abstract
Hepatic artery thrombosis is a dreadful complication of orthotopic liver transplantation. It should be suspected in cases of fulminant liver failure, delayed bile leak, or intermittent sepsis of unknown cause after liver transplantation. Accurate diagnosis is assisted by ultrasound and computerized tomography scans, but usually requires arteriography. Prompt retransplantation is required in most of the cases.
Many factors have contributed to the improved survival of recipients of liver transplants. Among the remaining causes of mortality and serious morbidity, those resulting from technical failures continue to pose serious challenges to surgeons undertaking the procedure.
The most common and potentially the most devastating of these technical failures is thrombosis of the arterial supply of the hepatic allograft.
This article describes the clinical presentation of hepatic artery thrombosis and outlines the steps taken in diagnosing and treating the disorder.
MATERIALS AND METHODS
The records of 244 patients who received 309 liver transplantations at the University of Colorado Medical Sciences Center and the University of Pittsburgh Medical Center, from March 1980 to June 1984 (liver transplantation Nos. 171–414 included), were reviewed. Of these patients, 104 were children (7 months to 18 years old) and 140 were adults (19 to 57 years old) (Table 1). There were 136 pediatric and 173 adult liver transplant recipients. All patients were treated with cyclosporine and low-dose steroids.
Table 1.
Case material (OLTx Nos. 171–414)
| Number of recipients | Number of transplants | |
|---|---|---|
| Pediatric cases | 104 | 136 |
| Adults | 140 | 173 |
| Total | 244 | 309 |
The diagnosis of hepatic artery thrombosis was made in 22 cases: by arteriography in 5 cases, digital subtraction arteriography in 1 case, exploratory laparotomy in 6, and by autopsy in 6 cases. In 4 cases, the diagnosis was made at the time of retransplantation.
RESULTS
The clinical presentation of these patients was found to follow one of three general patterns: fulminant hepatic necrosis, delayed biliary leak, and relapsing bacteremia. These will be described and a case representative of each pattern presented.
Fulminant hepatic necrosis
Eight patients with hepatic artery thrombosis experienced massive hepatic necrosis. Frank hepatic gangrene and rapid clinical deterioration were common.
Sudden and sharp rises in the serum transaminase levels were seen in all cases (average peak serum glutamic oxaloacetic transaminase (SGOT)4 level l00-fold higher than normal). The interval between transplantation and presentation was 9–33 days (mean 16.4 days). In two cases, gas bubbles were demonstrated in the right upper quadrant of the abdomen in the plain roentgenogram of the abdomen.
Case report
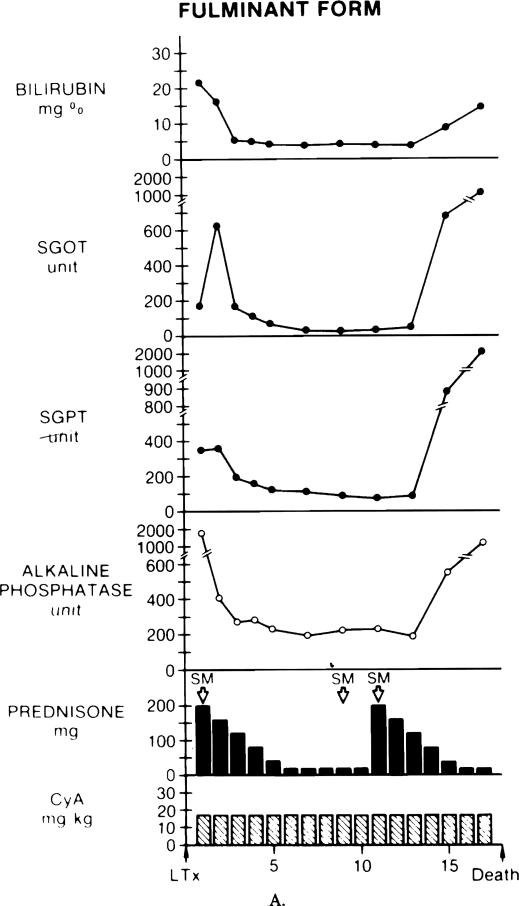
A 6-year-old girl with biliary atresia (OLTX No. 267), underwent an uneventful liver transplantation. The arterial reconstruction was an end-to-end anastomosis between the donor celiac axis and the recipient common hepatic artery. Figure 1A charts the patient's clinical course.
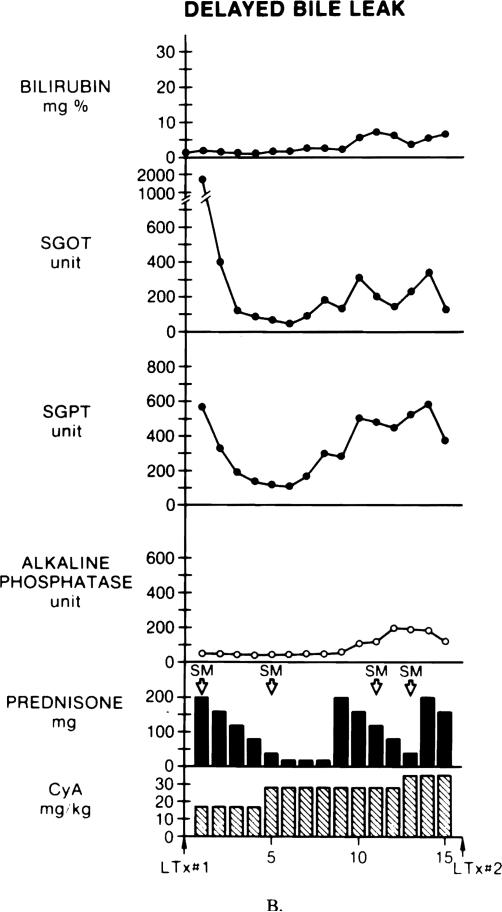
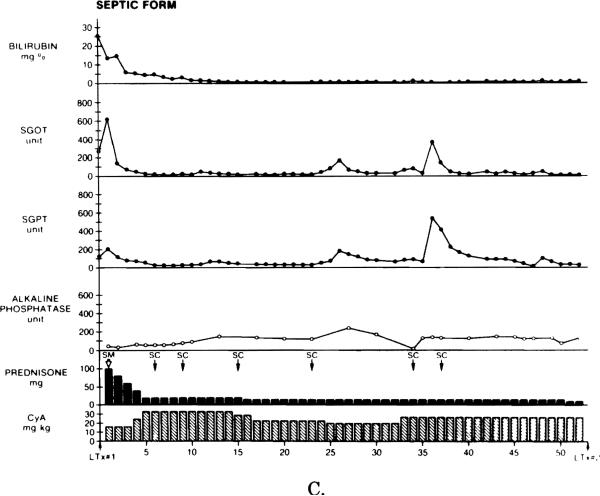
Figure 1.
(A, B, C). Graphic presentations of typical cases of (A) fulminant (OLT 267), (B) delayed-bile-leak (OLT 320a) and (C) septic (312a) hepatic artery thrombosis seen clinically after orthotopic liver transplantation. The cyclosporine dose represents both i.v. and oral cyclosporine given daily, the i.v. dose converted by a factor of 3 for simplicity.
On the 9th postoperative day, she developed a fever of 39.8°C. At the same time, the serum transaminases rose slightly. Ultrasonic examination showed no evidence of dilatation of the intrahepatic bile ducts or fluid collections. Treatment for graft rejection was begun (Fig. 1A). However, blood cultures drawn at the time grew Clostridium perfigens in 48 hr and a plain abdominal roentgenogram showed a collection of foamy gas bubbles in the region of the graft. Hepatic gangrene secondary to hepatic artery thrombosis was suspected. An organ was found within 48 hr. The patient died during the retransplantation procedure. Overzealous mobilization of the gangrenous liver resulted in the release of potassium and perhaps other toxins into the systemic circulation, leading to cardiac arrest and death.
Five patients died before retransplantation could be performed. Another patient died after retransplantation from a systemic fungal infection. Two patients are in good health following a successful retransplantation.
Delayed biliary leak
Six patients (7 transplants) developed significant bile leaks 7–65 days following liver transplantation (average 29.0). Bile leak in these patients resulted from ischemic necrosis of the bile duct secondary to hepatic artery thrombosis. The signs and symptoms included frank bile peritonitis, subhepatic fluid collections, drainage of bile through the abdominal drains, and bacteremia.
The liver function tests showed changes similar to those seen in rejection (average peak SGOT level 50-fold above normal).
Case report
A 21-year-old woman with chronic, non-A, non-B hepatitis underwent a liver transplantation with arterial reconstruction involving anastomosis of the donor celiac axis to the recipient common hepatic artery.
As seen in Figure 1B, 9 days later she had an elevation of the liver enzymes that was thought to represent an acute rejection. A T-tube cholangiogram and an abdominal ultrasound were normal—however, 2 days later she developed an episode of acute shortness of breath and epigastric pain. Blood cultures drawn at the time became positive for Enterobacter. A computerized tomography (CT) scan showed a sUbhepatic collection, from which bile was percutaneously aspirated. At exploration, the hepatic artery was found to be thrombosed. Four days later, the patient was retransplanted uneventfully.
Three patients were retransplanted. Two of them are perfectly well. The third patient (OLTX No. 340) had a total of 3 grafts, all of which developed arterial thrombosis. He has survived all after a long hospital course. The first two grafts developed a biliary leak and the third was of the type described below. Three patients were not retransplanted and died of fungal infection or multiple organ failure.
Relapsing bacteremia
In 7 cases, the development of hepatic artery thrombosis was accompanied by a much less dramatic course, presenting as relapsing bacteremia. Diagnosis of hepatic artery thrombosis was made 15–45 days (average 26.7 days) after liver transplantation. Liver function tests were normal except for minor abnormalities associated with episodes of septicemia. Sepsis was usually controllable with appropriate antibiotics.
Case report
A seriously ill 4-year-old boy received a liver transplant for treatment of end-stage liver disease resulting from alpha-l-antitrypsin deficiency (OLTX No. 312) (Fig. 1C).
The donor liver arterial supply was provided by a left hepatic artery from the celiac axis and a right from the superior mesenteric artery. Arterial reconstruction required the use of the donor thoracic aorta, with the celiac and superior mesenteric arteries, end-to-side with the right common iliac artery (10).
The patient made a prompt recovery with rapid reversal of encephalopathy and coagulopathy. During the fourth week after the operation, he developed an episode of Klebsiella septicemia with mild elevation of liver function studies. He made a prompt response to treatment with i.v. antibiotics and steroids. An intensive search for the source of sepsis, including sputum and urine cultures, chest roentgenograms, and an abdominal sonogram, failed to reveal the source of sepsis.
After one week, antibiotics were discontinued and a second episode of Klebsiella sepsis occurred. An abdominal CT at this time suggested thrombus in the aortic conduit. An abdominal aortogram confirmed the diagnosis of arterial thrombosis.
Since the patient was clinically stable, a conservative approach was first taken. However, when antibiotics were discontinued, another episode of septicemia occurred, this time accompanied by GI bleeding. A suitable donor became available on the 53rd postoperative day. At the time of retransplantation, the bile ducts were impacted with inspissated bile and old blood clots. Disimpaction of this material, resulted into vigorous hemorrhage from the portobiliary fistula.
The patient developed a rupture of a mycotic aneurysm at the anastomosis between the new aortic conduit and the native abdominal aorta on the 15th postoperative day and died. Three more patients with relapsing bacteremia have been retransplanted. One of these has died and two are well.
Three patients are surviving with the existing grafts at 5, 5½, and 6 months after discharge from the hospital. Two of them (OLTX Nos. 332 and 340) are doing well and have normal liver function. The third is developing jaundice and ascites. A recent liver biopsy showed evidence of cirrhosis and plans have been made for retransplantation.
Incidence
Hepatic artery thrombosis occurred in 22 of the 309 grafts reviewed in this series (7.1%) (20 recipients). Fourteen were children (16 grafts, 11.8% of the children's liver transplants), 6 were adults (6 grafts, 3.4% of the adult liver transplants) (Table 2). Mortality was 50% overall, 37.5% in children, and 83.3% in adults. Mortality was 27.3% after retransplantation and 72.7% without retransplantation.
Table 2.
Incidence of hepatic artery thrombosis in liver transplantation
| No. Cases | Hepatic artery thrombosis | Incidence | |
|---|---|---|---|
| Pediatric group | 136 | 16 | 11.8% |
| Adult group | 173 | 6 | 3.4% |
| Overall | 309 | 22 | 7.1% |
The pathoanatomical cause was an intimal dissection of the recipient common hepatic artery in 2 cases. In 1 case, the thrombosis was due to medial necrosis and intramural hemorrhage in the celiac axis of the previous graft, which was left in place and was used for arterial inflow. In the remaining cases, no pathoanatomical cause was found.
Technical considerations
The arterial reconstruction of the grafts followed the principles previously reported (1, 6, 10, 13). The anatomical variations of the arterial blood supply of the donor and recipient livers and the reconstructions performed are shown in Tables 3 and 4. Table 5 describes cases in which donor arterial allografts were used.
Table 3.
Arterial anatomy of recipient livers (OLTx Nos. 171–414)
| Total | Hepatic artery thrombosis | Incidence | |
|---|---|---|---|
| Single arterya | 217 | 19 | 8.8% |
| A or CA branch used | 257 | 12 | 4.7% |
| Aortic graft | 11 | 2 | 18.2% |
| Iliac graft | 12 | 5 | 41.7% |
| Double artery | 25 | 3 | 12.0% |
| CA or CA branch used | 8 | 2 | 25.0% |
| SMA branch used | 9 | 0 | 0% |
| Aortic graft | 2 | 1 | 50.0% |
| Iliac graft | 8 | 0 | 0% |
| No Hep. art identified | 2 | 0 | 0% |
| Aortic graft | 0 | 0 | 0% |
| Iliac graft | 2 | 0 | 0% |
Including anomalous branch from the left gastric artery.
Table 4.
Arterial anatomy of donor livers (OLTx Nos. 171–414)
| Total | Hepatic artery thrombosis | Incidence | |
|---|---|---|---|
| Single arterya | 280 | 15 | 5.4% |
| CA | 251 | 9 | 3.6% |
| SMA | 2 | 0 | 0% |
| Aortic graft | 6 | 1 | 16.7% |
| Iliac graft | 21 | 5 | 23.8% |
| Double artery | 29 | 7 | 24.1% |
| SMA after black table anastomosis | 21 | 5 | 23.8% |
| Aortic graft | 7 | 2 | 28.6% |
| Iliac graft to SMA after back table anastomosis | 1 | 0 | 0% |
Including anomalous branch from the left gastric artery.
Table 5.
Grafts used for arterial reconstruction
| Total | Hepatic artery thrombosis | Incidence | |
|---|---|---|---|
| Iliac artery: | 22 | 5 | 22.7% |
| Aorta: | 13 | 3 | 23.1% |
Diagnostic considerations
Abdominal plain roentgenograms were useful in 3 cases in which air was demonstrated in the liver. A CT scan showed a clot within the aortic conduit in one case, and this finding was confirmed both by ultrasound and arteriography.
Nuclear liver scans can demonstrate filling defects in the liver in cases complicated by hepatic necrosis of abscess, but have not by themselves confirmed the diagnosis of hepatic artery thrombosis. False-negative scans are frequent and rejection may cause a false-positive scan. Liver biopsy was not helpful. Rejection was found by needle biopsy, or in the hepatectomy specimen (in 3 cases). Focal or diffuse necrosis was identified in 8 cases. Necrosis of the common bile duct was identified in all patients with a delayed bile leak.
DISCUSSION
Hepatic artery thrombosis after orthotopic liver transplantation has long been thought to be an infrequent, but devastating, complication requiring urgent retransplantation (8).
Our experience shows that although a large number of patients have a fulminant clinical course, there are also patients in whom the course is subtle and indolent. Regardless of the presentation, recognition of the cause is important to patient survival.
The proposed classification into three clinical types should not be considered as a rigid one. However, most cases will fall predominantly into 1 of 3 types. Differential diagnosis in the fulminant presentation of hepatic artery thrombosis includes primary graft nonfunction and acute severe rejection. For delayed biliary leak, the main differential is primary biliary technical failure. Disruption of the biliary anastomosis has also been seen in cases of herpetic hepatitis.
Other causes of relapsing bacteremia include intraabdominal abscess, biliary stricture, or some other undetected and persistent source of infection. This problem, when suspected, should be pursued with arteriography (12). Digital subtraction angiography could be valuable, but substantial experience with it is lacking.
Exploratory laparotomy may mean a diagnosis at a particularly high cost. Manipulation of a necrotic liver is hazardous and dissection of the delicate hilar reconstructions is tedious. Palpation of the hepatic artery can be misleading. An artery with a palpable pulse may be thrombosed at a more distal level or a transmitted pulse may be present in an occluded vessel.
Interruption of arterial blood supply has different implications in the native (3) and transplanted liver. The liver transplant is at a disadvantage because: (A) rejection, in addition to its effects on the function of the graft and the general condition of the host, renders the graft ischemic and vulnerable to invasion by intestinal microorganisms even in the presence of a patent hepatic artery (4, 5). Clinical observations (8) confirm the findings in animal models. Poorly controlled rejection has been implicated in the pathogenesis of arterial thrombosis (8); and (B) it lacks natural attachments and preformed arterial collaterals. The bile duct is completely dependent on the hepatic artery (usually the right) for its blood supply. It is evident (Figs. 2 and 3) that, given the opportunity, life-saving hepatopedal arterial collaterals can develop. Donor arterial grafts may be required to arterialize hepatic allografts (10). Reuse of such arterial grafts at retransplantation has been associated with necrosis in the vessel wall, causing thrombosis or rupture (14). We have abandoned this practice. Intimal dissection (10) must be recognized and reconstructed promptly.
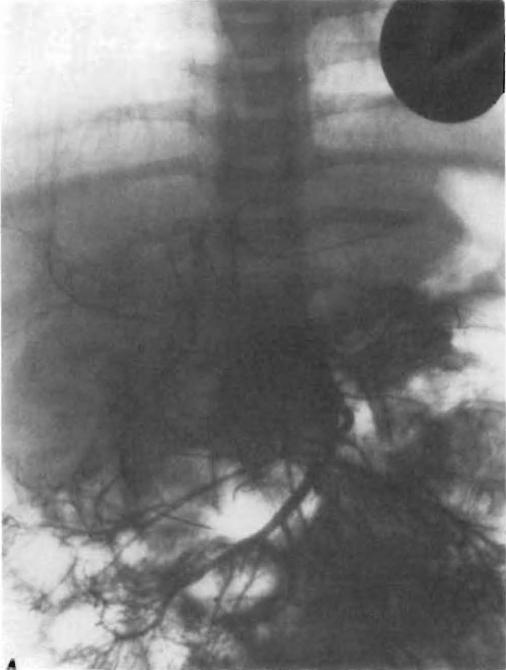
Figure 2.
Arteriogram obtained two weeks after transplantation showing thrombosed aortic conduit.
Figure 3.
Follow-up arteriogram, obtained six weeks after the arteriogram in Figure 4, showing arterial collaterals from the superior mesenteric artery filling the right and left hepatic arteries.
The importance of technical perfection cannot be overemphasized. Simplified methods of reconstruction (13) should help in avoiding technical errors. Patients at highest risk are pediatric patients and those requiring complex vascular reconstructions (double donor artery, iliac and aortic conduits).
When the diagnosis of hepatic arterial thrombosis is established, prompt retransplantation should be performed in most cases (14). A decision to delay retransplantation can only be considered in patients with stable liver function who have relapsing bacteremia that can be controlled with antibiotics. A small number of patients develop sufficient collaterals to survive without retransplantation.
Footnotes
Presented at the 11th Annual Meeting of the American Society of Transplant Surgeons, May 1985, Chicago, IL.
This work was supported by Research Grants from the Veterans Administration and by Project Grant AM-29961 from the National Institutes of Health, Bethesda, MD.
Abbreviations used: CT, computerized tomography; SGOT, serum glutamic oxaloacetic transaminase.
REFERENCES
- 1.Starzl TE, Kaupp HA, Brock DR, et al. Reconstructive problems in canine liver homotransplantation with special reference to the postoperative role of heaptic venous flow. Surg Gynecol Obstet. 1961;11:733. [PMC free article] [PubMed] [Google Scholar]
- 2.Starzl TE, Marchioro TL, von Kaulla KN, et al. Homotransplantation of liver in humans. Surg Gynecol Obstet. 1963;117:659. [PMC free article] [PubMed] [Google Scholar]
- 3.Brittain RS, Marchioro TL, Hermann G, et al. Accidental hepatic artery ligation in humans. Am J Surg. 1964;107:822. doi: 10.1016/0002-9610(64)90169-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Groth CG, Porter KA, Otte JB, et al. Studies of blood flow and ultrastructural changes in rejecting and non-rejecting canine orthotopic liver homografts. Surgery. 1968;63:658. [PMC free article] [PubMed] [Google Scholar]
- 5.Brettschneider L, Tong J, Boose DS, et al. Specific bacteriologic problems with canine orthotopic liver transplantation. Arch Surg. 1968;97:313. doi: 10.1001/archsurg.1968.01340020177021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lilly JR, Starzl TE. Liver transplantation in children with biliary atresia and vascular anomalies. J Pediatr Surg. 1974;9:707. doi: 10.1016/0022-3468(74)90109-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iwatsuki S, Shaw BW, Jr, Starzl TE. Biliary tract complications in liver transplantation under cyclosporine-steroid therapy. Transplant Proc. 1983;15:1288. [PMC free article] [PubMed] [Google Scholar]
- 8.Starzl TE, Iwatsuki S, Van Thiel DH, et al. Evolution of liver transplantation. Hepatology. 1982;2:614. doi: 10.1002/hep.1840020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krom RA, Kingma LM, Wesenhagen H, et al. Choledochocholedochostomy is successful in orthotopic liver transplantation. Transplant Proc. 1984;16:1228. [PubMed] [Google Scholar]
- 10.Shaw BW, Jr, Iwatsuki S, Starzl TE. Alternative methods of hepatic graft arterialization. Surg Gynecol Obstet. 1984;159:265. [PMC free article] [PubMed] [Google Scholar]
- 11.Cienfuegos D, Tamelhoff, et al. Surgical complications in the postoperative period of liver transplantation in children. Transplant Proc. 1984;16:1230. [PubMed] [Google Scholar]
- 12.Zajko AB, Bron KM, Starzl TE, et al. Angiographic evaluation in liver transplantation. Radiology. submitted. [Google Scholar]
- 13.Gordon RD, Shaw BW, Jr, Iwatsuki S, et al. A simplified technique for revascularization of liver homografts with a variant right hepatic artery from the superior mesenteric artery. Surg Gynecol Obstet. submitted. [PMC free article] [PubMed] [Google Scholar]
- 14.Shaw BW, Jr, Gordon RD, Iwatsuki S, Starzl TE. Hepatic retransplantation. submitted. [PMC free article] [PubMed]