Arterial injury initiates a complex series of events including proliferation of smooth muscle cells (SMCs) that culminates in the formation of the neointima. Neointimal formation can be a clinically problematic event, significantly narrowing the vessel lumen after angioplasty, bypass vein grafting, and transplant. Numerous growth factors and cytokines trigger the complex and redundant signaling pathways that lead to cell cycle entry.1–6 Because of the redundancy of these signaling pathways, targeting individual growth factors and cytokines has failed to affect neointimal proliferation and has obviated the need to target the “final common pathway” of events.1
Growth factor–stimulated proliferation is mediated by an early upregulation in transcription of the proto-oncogenes c-fos, c-myc, c-myb, B-myb, and ras.1,7–10 The gene products then act as transcription factors that increase expression of cell cycle regulatory genes, including the cyclins, that when complexed with cyclin-dependent kinases (CDKs), coordinate cell cycle progression.7,11–14 Certain proto-oncogene gene products also have the ability to augment cyclin-associated kinase activity and to couple growth regulatory signals to second messenger pathways.15,16 Early upregulation of proliferating cell nuclear antigen (PCNA) occurs as well, stimulating DNA-polymerase-δ ability. In opposition to cell cycle progression are the cyclin-dependent kinase inhibitors (CKIs), such as p27kip1 and p21cip1. Transcription factors, such as p53, GAX, GATA-6, E2A, and Id, are expressed in the developing neointima after vascular injury and regulate the expression of the CKIs.17–20 The final common pathway, therefore, involves regulation of the cell cycle through transcription and translation of cell cycle proteins. In addition, regulation of cell cycle protein function through post-translational modifications, such as phosphorylation, is also important.
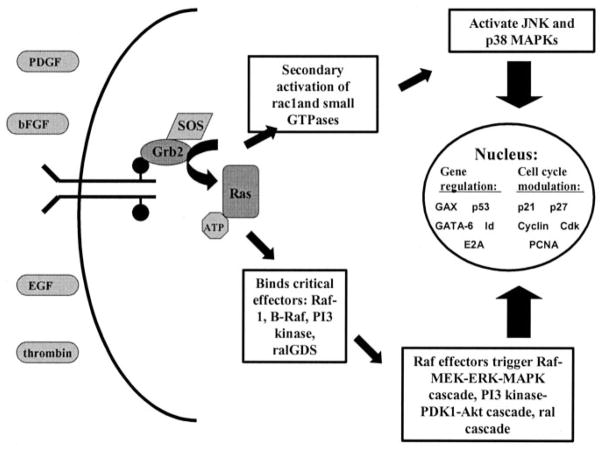
The study by Zhang et al21 in this issue of Arteriosclerosis, Thrombosis, and Vascular Biology describes the role of Grb2 in vascular neointimal formation and provides further evidence underscoring the rationale of targeting the final common pathway. The authors focus mainly on inhibiting downstream results of ras activation including activation of the Raf-MEK-ERK MAPK cascade, PI3 kinase-PDK1-Akt cascade, ral cascade, JNK, and p38 MAPKs all of which culminate in affecting gene expression, cytoskeletal regulation, metabolism, and cell cycle progression (Figure). In order to accomplish this, they focus on the protein Grb2, which facilitates ras activation in response to activation of several upstream receptors. Clearly Grb2 is important to normal development in that the knockout mice do not survive embryogenesis due to defective endoderm and inability to develop epiblast. The authors demonstrate that Grb2 is, indeed, important to SMC proliferation and neointimal development following injury. Through use of morpholino anti-sense oligodeoxynucleotides (ODNs) directed against Grb2, it is clearly shown that reducing Grb2 levels results in decreased SMC growth in culture. They further demonstrate that Grb+/− animals develop less neointima in response to injury. They nicely show that this likely occurs through decreased activation of p38, ERK and JNK, thus creating a break in the series of events involved in the final pathway leading to cellular proliferation. Grb2, therefore, represents a possibly useful target for in vivo oligonucleotide or pharmacologic therapy as it appears to have multiple effects on downstream participants in the final common pathway of events.
Figure.
Schematic diagram showing the results of ras activation by Grb2. Grb2 translocates from the cytosol to the cell membrane, binds to the internal portion of receptor tyrosine kinases and facilitates ras activation by delivering SOS, the guanine nucleotide exchange factor to ras. Activation of ras results in the triggering of several intra-cellular signaling cascades and the secondary activation of other kinases regulating gene expression and cell cycle progression. Grb2, critical effectors downstream (boxes) and regulators of gene expression in the nucleus are all potential therapeutic targets. PDGF indicates platelet derived growth factor; bFGF, basic fibroblast growth factor; EGF, epidermal growth factor; ATP, adenosine triphosphate; PI3 kinase, phosphatidylinositol-3′ kinase; ralGDS, ral guanine nucleotide dissociation stimulator; ERK, extracellular signal-regulated kinase; MAPK, mitogen-activated protein kinase; JNK, c-Jun-NH2-terminal kinase; PCNA, proliferating cell nuclear antigen.
Manipulation of the expression and function of these final common pathway proteins does indeed lead to reduction in neointimal formation after injury. Inhibition of membrane adherence of the small G protein p21ras with a farnesyl transferase inhibitor inhibited activation of MAPK, thus decreasing neointimal size in injured porcine coronary arteries.22 Growth factor receptor tyrosine kinases have also been shown to be useful targets as inhibitors prevent the initial phosphorylation event necessary for recruiting downstream cell cycle regulators thus decreasing cell growth.23 Cdk2 inhibitors have also been successful in inhibiting neointimal formation through their ability to block induction of cyclin D1, PCNA, and hyperphosphorylation of the retinoblastoma protein.24,25 Antisense ODNs have been used to inhibit the cell cycle regulatory genes c-myb, PCNA, c-myc, AP-I, cdc2, and cdk2, resulting in a decrease in neointimal formation after injury in rat carotid models.26–30 Trans-catheter delivery of c-myc antisense ODNs in a porcine coronary model was also effective as was the treatment of vein grafts with antisense ODN against PCNA and Cdk1.31–33 Further, multigene strategies have been shown to be more effective than targeting a single gene.26,28 ODN decoys have also been developed to prevent interaction between the transcription factor and its targeted promoter region and have been used successfully to bind the factors E2F and AP-1 in arterial balloon injury models.34–36 Conditional expression of a dominant-negative c-myb in transgenic mice, as well, provided means for decreased neointimal formation.37 Ribozymes have been used to cleave target mRNA of Cdk1 and PCNA decreasing neointimal formation in rat carotid injury models.1 Overexpression of inhibitory molecules has also been implemented via adenoviral vectors and liposome-mediated gene transfer. Overexpression of the inhibitory molecules p21cip1, p27kip1, GAX, GATA-6, and p53 have all resulted in decreased neointimal formation in animal arterial injury models.1,17,38–42
In addition to SMC proliferation, multiple other processes are involved in neointimal formation after vascular injury such as inflammation, matrix formation, migration, and loss of vasoactive responses.1,8 Indeed, similar decreases in neointimal size in vivo have been attained targeting these aspects of neointimal formation.43–49 Thus, advances in understanding the molecular mechanisms involved in neointimal formation have given us many potential targets for limiting neointimal formation in humans. Yet few of these strategies have been successfully brought to the clinical arena.
The current armamentarium for targeting the neointimal formation in humans includes pharmacologic agents and brachytherapy. Pharmacologic agents have been studied in relation to various components of the pathway. Rapamycin has been shown to inhibit down regulation of p27kip1 and block enzymatic activation of cyclin-dependent kinases and phosphorylation of the retinoblastoma gene product thus inhibiting proliferation.50–53 Paclitaxel stabilizes microtubules and indirectly upregulates p21cip1.54,55 Rapamycin- and paclitaxel-coated stents have been used successfully as directly delivered pharmacologic therapy in humans, effectively decreasing neointimal formation after stent placement.56–59 However, pharmacologic stents have failed to obliterate restenosis as initially suggested and require longer periods of anticoagulation.60,61 Brachytherapy employs beta and gamma radiation to create breaks in double stranded DNA halting cell division and successfully decreasing rates of restenosis.62–64 Edge stenosis and late total occlusion have complicated its use.65,66 Although these therapies have greatly impacted restenosis, they have clinically problematic limitations and do not address the issues of vein graft occlusion and transplant arteriopathy. Local delivery of oligonucleotides that bind the cell cycle regulatory factor E2F has successfully prevented vein graft failure in peripheral and coronary vein graft bypasses in human trials representing a unique class of therapy that may prove useful in multiple cardiovascular disease processes.67,68
It is, therefore, of extreme importance that we continue, as these authors have, to search for new mechanisms that regulate neointimal proliferation, new targets that may limit this process, and new mechanisms of therapy. Both our wealth and lack of knowledge present us with the difficult task of somehow translating this knowledge into clinically relevant and useful strategies while we still strive to further elucidate the final common pathway.
References
- 1.Braun-Dullaeus RC, Mann MJ, Dzau VJ. Cell cycle progression: new therapeutic target for vascular proliferative disease. Circulation. 1998;98:82–89. doi: 10.1161/01.cir.98.1.82. [DOI] [PubMed] [Google Scholar]
- 2.Majesky MW, Lindner V, Twardzik DR, Schwartz SM, Reidy MA. Production of transforming growth factor beta 1 during repair of arterial injury. J Clin Invest. 1991;88:904–910. doi: 10.1172/JCI115393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nabel EG, Yang Z, Liptay S, San H, Gordon D, Haudenschild CC, Nabel GJ. Recombinant platelet-derived growth factor B gene expression in porcine arteries induce intimal hyperplasia in vivo. J Clin Invest. 1993;91:1822–1829. doi: 10.1172/JCI116394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant MB, Wargovich TJ, Ellis EA, Caballero S, Mansour M, Pepine CJ. Localization of insulin-like growth factor I and inhibition of coronary smooth muscle cell growth by somatostatin analogues in human coronary smooth muscle cells: a potential treatment for restenosis? Circulation. 1994;89:1511–1517. doi: 10.1161/01.cir.89.4.1511. [DOI] [PubMed] [Google Scholar]
- 5.Dzau VJ, Gibbons GH, Pratt RE. Molecular mechanisms of vascular renin-angiotensin system in myointimal hyperplasia. Hypertension. 1991;18(Suppl-5) doi: 10.1161/01.hyp.18.4_suppl.ii100. [DOI] [PubMed] [Google Scholar]
- 6.Lindner V, Reidy MA. Proliferation of smooth muscle cells after vascular injury is inhibited by an antibody against basic fibroblast growth factor. Proc Natl Acad Sci U S A. 1991;88:3739–3743. doi: 10.1073/pnas.88.9.3739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hunter T. Oncoprotein networks. Cell. 1997;88:333–346. doi: 10.1016/s0092-8674(00)81872-3. [DOI] [PubMed] [Google Scholar]
- 8.Dzau VJ, Braun-Dullaeus RC, Sedding DG. Vascular proliferation and atherosclerosis: new perspectives and therapeutic strategies. Nat Med. 2002;8:1249–1256. doi: 10.1038/nm1102-1249. [DOI] [PubMed] [Google Scholar]
- 9.Quincoces AF, Leon J. Serum growth factors up-regulate H-ras, K-ras, and N-ras proto-oncogenes in fibroblasts. Cell Growth Differ. 1995;6:271–279. [PubMed] [Google Scholar]
- 10.Huckle WR, Earp HS. Regulation of cell proliferation and growth by angiotensin II. Progress Growth Factor Res. 1994;5:177–194. doi: 10.1016/0955-2235(94)90004-3. [DOI] [PubMed] [Google Scholar]
- 11.Phuchareon J, Tokuhisa T. Deregulated c-Fos/AP-1 modulates expression of the cyclin and the cdk gene in splenic B cells stimulated with lipopolysaccharide. Cancer Lett. 1995;92:203–208. doi: 10.1016/0304-3835(95)03780-z. [DOI] [PubMed] [Google Scholar]
- 12.Daksis JI, Lu RY, Facchini LM, Marhin WW, Penn LJ. Myc induces cyclin D1 expression in the absence of de novo protein synthesis and links mitogen-stimulated signal transduction to the cell cycle. Oncogene. 1994;9:3635–3645. [PubMed] [Google Scholar]
- 13.Steiner P, Philipp A, Lukas J, Godden-Kent D, Pagano M, Mittnacht S, Bartek J, Eilers M. Identification of a Myc-dependent step during the formation of active G1 cyclin-cdk complexes. EMBO J. 1995;14:4814–4826. doi: 10.1002/j.1460-2075.1995.tb00163.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu JJ, Chao JR, Jiang MC, Ng SY, Yen JJ, Yang-Yen HF. Ras transformation results in an elevated level of cyclin D1 and acceleration of G1 progression in NIH 3T3 cells. Mol Cell Biol. 1995;15:3654–3663. doi: 10.1128/mcb.15.7.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Avruch J, Zhang XF, Kyriakis JM. Raf meets Ras: completing the framework of a signal transduction pathway. Trends Biochem Sci. 1994;19:279–283. doi: 10.1016/0968-0004(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 16.Leone G, DeGregori J, Sears R, Jakoi L, Nevins JR. Myc and Ras collaborate in inducing accumulation of active cyclin E/Cdk2 and E2F [published erratum appears in Nature. 1997;387:932] Nature. 1997;387:422–426. doi: 10.1038/387422a0. [DOI] [PubMed] [Google Scholar]
- 17.Smith RC, Branellec D, Gorski DH, Guo K, Perlman H, Dedieu JF, Pastore C, Mahfoudi A, Denefle P, Isner JM, Walsh K. p21CIP1-mediated inhibition of cell proliferation by overexpression of the gax homeodomain gene. Genes Dev. 1997;11:1674–1689. doi: 10.1101/gad.11.13.1674. [DOI] [PubMed] [Google Scholar]
- 18.Levine AJ. p53, the cellular gatekeeper for growth and division. Cell. 1997;88:323–331. doi: 10.1016/s0092-8674(00)81871-1. [DOI] [PubMed] [Google Scholar]
- 19.Perlman H, Suzuki E, Simonson M, Smith RC, Walsh K. GATA-6 induces p21(Cip1) expression and G1 cell cycle arrest. J Biol Chem. 1998;273:13713–13718. doi: 10.1074/jbc.273.22.13713. [DOI] [PubMed] [Google Scholar]
- 20.Prabhu S, Ignatova A, Park ST, Sun XH. Regulation of the expression of cyclin-dependent kinase inhibitor p21 by E2A and Id proteins. Mol Cell Biol. 1997;17:5888–5896. doi: 10.1128/mcb.17.10.5888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang S, Ren J, Khan MF, Cheng AM, Abendschein D, Muslin AJ. Grb2 is required for the development of neointima in response to vascular injury. Arterioscler Thromb Vasc Biol. 2003;23:1788–1793. doi: 10.1161/01.ATV.0000085015.49110.85. [DOI] [PubMed] [Google Scholar]
- 22.Work LM, McPhaden AR, Pyne NJ, Pyne S, Wadsworth RM, Wainwright CL. Short-term local delivery of an inhibitor of Ras farnesyltransferase prevents neointima formation in vivo after porcine coronary balloon angioplasty. Circulation. 2001;104:1538–1543. doi: 10.1161/hc3801.095661. [DOI] [PubMed] [Google Scholar]
- 23.Dahring TK, Lu GH, Hamby JM, Batley BL, Kraker AJ, Panek RL. Inhibition of growth factor-mediated tyrosine phosphorylation in vascular smooth muscle by PD 089828, a new synthetic protein tyrosine kinase inhibitor. J Pharmacol Exp Ther. 1997;281:1446–1456. [PubMed] [Google Scholar]
- 24.Ruef J, Meshel AS, Hu Z, Horaist C, Ballinger CA, Thompson LJ, Subbarao VD, Dumont JA, Patterson C. Flavopiridol inhibits smooth muscle cell proliferation in vitro and neointimal formation in vivo after carotid injury in the rat. Circulation. 1999;100:659–665. doi: 10.1161/01.cir.100.6.659. [DOI] [PubMed] [Google Scholar]
- 25.Brooks EE, Gray NS, Joly A, Kerwar SS, Lum R, Mackman RL, Norman TC, Rosete J, Rowe M, Schow SR, Schultz PG, Wang X, Wick MM, Shiffman D. CVT-313, a specific and potent inhibitor of CDK2 that prevents neointimal proliferation. J Biol Chem. 1997;272:29207–29211. doi: 10.1074/jbc.272.46.29207. [DOI] [PubMed] [Google Scholar]
- 26.Morishita R, Gibbons GH, Ellison KE, Nakajima M, von der LH, Zhang L, Kaneda Y, Ogihara T, Dzau VJ. Intimal hyperplasia after vascular injury is inhibited by antisense cdk 2 kinase oligonucleotides. J Clin Invest. 1994;93:1458–1464. doi: 10.1172/JCI117123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morishita R, Gibbons GH, Ellison KE, Nakajima M, Zhang L, Kaneda Y, Ogihara T, Dzau VJ. Single intraluminal delivery of antisense cdc2 kinase and proliferating-cell nuclear antigen oligonucleotides results in chronic inhibition of neointimal hyperplasia. Proc Natl Acad Sci U S A. 1993;90:8474–8478. doi: 10.1073/pnas.90.18.8474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abe J, Zhou W, Taguchi J, Takuwa N, Miki K, Okazaki H, Kurokawa K, Kumada M, Takuwa Y. Suppression of neointimal smooth muscle cell accumulation in vivo by antisense cdc2 and cdk2 oligonucleotides in rat carotid artery. Bioch Biophys Res Comm. 1994;198:16–24. doi: 10.1006/bbrc.1994.1003. [DOI] [PubMed] [Google Scholar]
- 29.Simons M, Edelman ER, DeKeyser JL, Langer R, Rosenberg RD. Antisense c-myb oligonucleotides inhibit intimal arterial smooth muscle cell accumulation in vivo. Nature. 1992;359:67–70. doi: 10.1038/359067a0. [DOI] [PubMed] [Google Scholar]
- 30.Simons M, Edelman ER, Rosenberg RD. Antisense proliferating cell nuclear antigen oligonucleotides inhibit intimal hyperplasia in a rat carotid artery injury model. J Clin Invest. 1994;93:2351–2356. doi: 10.1172/JCI117240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shi Y, Fard A, Galeo A, Hutchinson HG, Vermani P, Dodge GR, Hall DJ, Shaheen F, Zalewski A. Transcatheter delivery of c-myc antisense oligomers reduces neointimal formation in a porcine model of coronary artery balloon injury. Circulation. 1994;90:944–951. doi: 10.1161/01.cir.90.2.944. [DOI] [PubMed] [Google Scholar]
- 32.Mann MJ, Gibbons GH, Kernoff RS, Diet FP, Tsao PS, Cooke JP, Kaneda Y, Dzau VJ. Genetic engineering of vein grafts resistant to atherosclerosis. Proc Natl Acad Sci U S A. 1995;92:4502–4506. doi: 10.1073/pnas.92.10.4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mann MJ, Gibbons GH, Tsao PS, der Leyen HE, Cooke JP, Buitrago R, Kernoff R, Dzau VJ. Cell cycle inhibition preserves endothelial function in genetically engineered rabbit vein grafts. J Clin Invest. 1997;99:1295–1301. doi: 10.1172/JCI119288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morishita R, Gibbons GH, Horiuchi M, Ellison KE, Nakama M, Zhang L, Kaneda Y, Ogihara T, Dzau VJ. A gene therapy strategy using a transcription factor decoy of the E2F binding site inhibits smooth muscle proliferation in vivo. Proc Natl Acad Sci U S A. 1995;92:5855–5859. doi: 10.1073/pnas.92.13.5855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morishita R, Higaki J, Tomita N, Ogihara T. Application of transcription factor “decoy” strategy as means of gene therapy and study of gene expression in cardiovascular disease. Circ Res. 1998;82:1023–1028. doi: 10.1161/01.res.82.10.1023. [DOI] [PubMed] [Google Scholar]
- 36.Kume M, Komori K, Matsumoto T, Onohara T, Takeuchi K, Yonemitsu Y, Sugimachi K. Administration of a decoy against the activator protein-1 binding site suppresses neointimal thickening in rabbit balloon-injured arteries. Circulation. 2002;105:1226–1232. doi: 10.1161/hc1002.104903. [DOI] [PubMed] [Google Scholar]
- 37.You XM, Mungrue IN, Kalair W, Afroze T, Ravi B, Sadi AM, Gros R, Husain M. Conditional expression of a dominant-negative c-Myb in vascular smooth muscle cells inhibits arterial remodeling after injury. Circ Res. 2003;92:314–321. doi: 10.1161/01.res.0000056758.73215.5a. [DOI] [PubMed] [Google Scholar]
- 38.Yonemitsu Y, Kaneda Y, Hata Y, Nakashima Y, Sueishi K. Wild-type p53 gene transfer: a novel therapeutic strategy for neointimal hyperplasia after arterial injury. Ann NY Acad Sci. 1997;811:395–400. doi: 10.1111/j.1749-6632.1997.tb52019.x. [DOI] [PubMed] [Google Scholar]
- 39.Yonemitsu Y, Kaneda Y, Tanaka S, Nakashima Y, Komori K, Sugimachi K, Sueishi K. Transfer of wild-type p53 gene effectively inhibits vascular smooth muscle cell proliferation in vitro and in vivo. Circ Res. 1998;82:147–156. doi: 10.1161/01.res.82.2.147. [DOI] [PubMed] [Google Scholar]
- 40.Chen D, Krasinski K, Sylvester A, Chen J, Nisen PD, Andres V. Downregulation of cyclin-dependent kinase 2 activity and cyclin A promoter activity in vascular smooth muscle cells by p27(KIP1), an inhibitor of neointima formation in the rat carotid artery. J Clin Invest. 1997;99:2334–2341. doi: 10.1172/JCI119414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mano T, Luo Z, Malendowicz SL, Evans T, Walsh K. Reversal of GATA-6 downregulation promotes smooth muscle differentiation and inhibits intimal hyperplasia in balloon-injured rat carotid artery. Circ Res. 1999;84:647–654. doi: 10.1161/01.res.84.6.647. [DOI] [PubMed] [Google Scholar]
- 42.Tsui LV, Camrud A, Mondesire J, Carlson P, Zayek N, Camrud L, Donahue B, Bauer S, Lin A, Frey D, Rivkin M, Subramanian A, Falotico R, Gyuris J, Schwartz R, McArthur JG. p27-p16 fusion gene inhibits angioplasty-induced neointimal hyperplasia and coronary artery occlusion. Circ Res. 2001;89:323–328. doi: 10.1161/hh1601.094482. [DOI] [PubMed] [Google Scholar]
- 43.Cavusoglu E, Chen I, Rappaport J, Marmur JD. Inhibition of tissue factor gene induction and activity using a hairpin ribozyme. Circulation. 2002;105:2282–2287. doi: 10.1161/01.cir.0000015701.59498.57. [DOI] [PubMed] [Google Scholar]
- 44.Feil R, Gappa N, Rutz M, Schlossmann J, Rose CR, Konnerth A, Brummer S, Kuhbandner S, Hofmann F. Functional reconstitution of vascular smooth muscle cells with cGMP-dependent protein kinase I isoforms. Circ Res. 2002;90:1080–1086. doi: 10.1161/01.res.0000019586.95768.40. [DOI] [PubMed] [Google Scholar]
- 45.Sinnaeve P, Chiche JD, Gillijns H, Van Pelt N, Wirthlin D, Van De WF, Collen D, Bloch KD, Janssens S. Overexpression of a constitutively active protein kinase G mutant reduces neointima formation and in-stent restenosis. Circulation. 2002;105:2911–2916. doi: 10.1161/01.cir.0000018169.59205.ca. [DOI] [PubMed] [Google Scholar]
- 46.de Waard V, Arkenbout EK, Carmeliet P, Lindner V, Pannekoek H. Plasminogen activator inhibitor 1 and vitronectin protect against stenosis in a murine carotid artery ligation model. Arterioscler Thromb Vasc Biol. 2002;22:1978–1983. doi: 10.1161/01.atv.0000042231.04318.e6. [DOI] [PubMed] [Google Scholar]
- 47.Meiners S, Laule M, Rother W, Guenther C, Prauka I, Muschick P, Baumann G, Kloetzel PM, Stangl K. Ubiquitin-proteasome pathway as a new target for the prevention of restenosis. Circulation. 2002;105:483–489. doi: 10.1161/hc0402.102951. [DOI] [PubMed] [Google Scholar]
- 48.Cho A, Reidy MA. Matrix metalloproteinase-9 is necessary for the regulation of smooth muscle cell replication and migration after arterial injury. Circ Res. 2002;91:845–851. doi: 10.1161/01.res.0000040420.17366.2e. [DOI] [PubMed] [Google Scholar]
- 49.Smyth SS, Reis ED, Zhang W, Fallon JT, Gordon RE, Coller BS. Beta(3)-integrin-deficient mice but not P-selectin-deficient mice develop intimal hyperplasia after vascular injury: correlation with leukocyte recruitment to adherent platelets 1 hour after injury. Circulation. 2001;103:2501–2507. doi: 10.1161/01.cir.103.20.2501. [DOI] [PubMed] [Google Scholar]
- 50.Nourse J, Firpo E, Flanagan WM, Coats S, Polyak K, Lee MH, Massague J, Crabtree GR, Roberts JM. Interleukin-2-mediated elimination of the p27Kip1 cyclin-dependent kinase inhibitor prevented by rapamycin. Nature. 1994;372:570–573. doi: 10.1038/372570a0. [DOI] [PubMed] [Google Scholar]
- 51.Morice WG, Wiederrecht G, Brunn GJ, Siekierka JJ, Abraham RT. Rapamycin inhibition of interleukin-2-dependent p33cdk2 and p34cdc2 kinase activation in T lymphocytes. J Biol Chem. 1993;268:22737–22745. [PubMed] [Google Scholar]
- 52.Marx SO, Jayaraman T, Go LO, Marks AR. Rapamycin-FKBP inhibits cell cycle regulators of proliferation in vascular smooth muscle cells. Circ Res. 1995;76:412–417. doi: 10.1161/01.res.76.3.412. [DOI] [PubMed] [Google Scholar]
- 53.Cao W, Mohacsi P, Shorthouse R, Pratt R, Morris RE. Effects of rapamycin on growth factor-stimulated vascular smooth muscle cell DNA synthesis: inhibition of basic fibroblast growth factor and platelet-derived growth factor action and antagonism of rapamycin by FK506. Transplantation. 1995;59:390–395. [PubMed] [Google Scholar]
- 54.Abal M, Andreu JM, Barasoain I. Taxanes: microtubule and centrosome targets, and cell cycle dependent mechanisms of action. Curr Cancer Drug Targets. 2003;3:193–203. doi: 10.2174/1568009033481967. [DOI] [PubMed] [Google Scholar]
- 55.Heliez C, Baricault L, Barboule N, Valette A. Paclitaxel increases p21 synthesis and accumulation of its AKT-phosphorylated form in the cytoplasm of cancer cells. Oncogene. 2003;22:3260–3268. doi: 10.1038/sj.onc.1206409. [DOI] [PubMed] [Google Scholar]
- 56.Duda SH, Poerner TC, Wiesinger B, Rundback JH, Tepe G, Wiskirchen J, Haase KK. Drug-eluting stents: potential applications for peripheral arterial occlusive disease. J Vasc Intervent Radiol. 2003;14:291–301. doi: 10.1097/01.rvi.0000058423.01661.57. [DOI] [PubMed] [Google Scholar]
- 57.Sousa JE, Costa MA, Abizaid AC, Rensing BJ, Abizaid AS, Tanajura LF, Kozuma K, Van Langenhove G, Sousa AG, Falotico R, Jaeger J, Popma JJ, Serruys PW. Sustained suppression of neointimal proliferation by sirolimus-eluting stents: one-year angiographic and intravascular ultrasound follow-up. Circulation. 2001;104:2007–2011. doi: 10.1161/hc4201.098056. [DOI] [PubMed] [Google Scholar]
- 58.Hong MK, Mintz GS, Lee CW, Song JM, Han KH, Kang DH, Song JK, Kim JJ, Weissman NJ, Fearnot NE, Park SW, Park SJ. Asian Paclitaxel-Eluting Stent Clinical Trial: paclitaxel coating reduces in-stent intimal hyperplasia in human coronary arteries: a serial volumetric intravascular ultrasound analysis from the Asian Paclitaxel-Eluting Stent Clinical Trial (ASPECT) Circulation. 2003;107:517–520. doi: 10.1161/01.cir.0000054163.42072.d4. [DOI] [PubMed] [Google Scholar]
- 59.Tanabe K, Serruys PW, Grube E, Smits PC, Selbach G, van der Giessen WJ, Staberock M, de Feyter P, Muller R, Regar E, Degertekin M, Ligthart JM, Disco C, Backx B, Russell ME. TAXUS III Trial: in-stent restenosis treated with stent-based delivery of paclitaxel incorporated in a slow-release polymer formulation. Circulation. 2003;107:559–564. doi: 10.1161/01.cir.0000048184.96491.8a. [DOI] [PubMed] [Google Scholar]
- 60.Lemos PA, Lee CH, Degertekin M, Saia F, Tanabe K, Arampatzis CA, Hoye A, van Duuren M, Sianos G, Smits PC, de Feyter P, van der Giessen WJ, van Domburg RT, Serruys PW. Early outcome after sirolimus-eluting stent implantation in patients with acute coronary syndromes: insights from the Rapamycin-Eluting Stent Evaluated At Rotterdam Cardiology Hospital (RESEARCH) registry. J Am Coll Cardiol. 2003;41:2093–2099. doi: 10.1016/s0735-1097(03)00429-7. [DOI] [PubMed] [Google Scholar]
- 61.Lemos PA, Saia F, Ligthart JM, Arampatzis CA, Sianos G, Tanabe K, Hoye A, Degertekin M, Daemen J, McFadden EP, Hofma S, Smits PC, Feyter P, Giessen WJ, Domburg RT, Serruys PW. Coronary restenosis after sirolimus-eluting stent implantation: morphological description and mechanistic analysis from a consecutive series of cases. Circulation. 108:257–260. doi: 10.1161/01.CIR.0000083366.33686.11. [DOI] [PubMed] [Google Scholar]
- 62.Rubin P, Soni A, Williams JP. The molecular and cellular biologic basis for the radiation treatment of benign proliferative diseases. Sem Radiat Oncol. 1999;9:203–214. doi: 10.1016/s1053-4296(99)80010-1. [DOI] [PubMed] [Google Scholar]
- 63.Teirstein PS, Massullo V, Jani S, Popma JJ, Russo RJ, Schatz RA, Guarneri EM, Steuterman S, Sirkin K, Cloutier DA, Leon MB, Tripuraneni P. Three-year clinical and angiographic follow-up after intra-coronary radiation : results of a randomized clinical trial. Circulation. 2000;101:360–365. doi: 10.1161/01.cir.101.4.360. [DOI] [PubMed] [Google Scholar]
- 64.Waksman R, Bhargava B, White L, Chan RC, Mehran R, Lansky AJ, Mintz GS, Satler LF, Pichard AD, Leon MB, Kent KK. Intracoronary beta-radiation therapy inhibits recurrence of in-stent restenosis. Circulation. 2000;101:1895–1898. doi: 10.1161/01.cir.101.16.1895. [DOI] [PubMed] [Google Scholar]
- 65.Waksman R, Bhargava B, Mintz GS, Mehran R, Lansky AJ, Satler LF, Pichard AD, Kent KM, Leon MB. Late total occlusion after intracoronary brachytherapy for patients with in-stent restenosis. J Am Coll Cardiol. 2000;36:65–68. doi: 10.1016/s0735-1097(00)00681-1. [DOI] [PubMed] [Google Scholar]
- 66.Kim HS, Waksman R, Cottin Y, Kollum M, Bhargava B, Mehran R, Chan RC, Mintz GS. Edge stenosis and geographical miss following intracoronary gamma radiation therapy for in-stent restenosis. J Am Coll Cardiol. 2001;37:1026–1030. doi: 10.1016/s0735-1097(01)01112-3. [DOI] [PubMed] [Google Scholar]
- 67.Freedman SB. Clinical trials of gene therapy for atherosclerotic cardiovascular disease. Curr Opin Lipidol. 2002;13:653–661. doi: 10.1097/00041433-200212000-00009. [DOI] [PubMed] [Google Scholar]
- 68.Mann MJ, Whittemore AD, Donaldson MC, Belkin M, Conte MS, Polak JF, Orav EJ, Ehsan A, Dell’Acqua G, Dzau VJ. Ex-vivo gene therapy of human vascular bypass grafts with E2F decoy: the PREVENT single-centre, randomised, controlled trial. Lancet. 1999;354:1493–1498. doi: 10.1016/S0140-6736(99)09405-2. [DOI] [PubMed] [Google Scholar]