Abstract
Objective
To examine patterns and recent trends in multi-class psychotropic treatment among youth visits to office-based physicians in the United States.
Method
Annual data from the 1996–2007 National Ambulatory Medical Care Surveys were analyzed to examine patterns and trends in multi-class psychotropic treatment within a nationally representative sample of 3466 child and adolescent visits to office-based physicians in which a psychotropic medication was prescribed.
Results
There was an increase in the percentage of child visits in which psychotropic medications were prescribed that included at least two psychotropic classes. Across the twelve year period, multi-class psychotropic treatment rose from 14.3% of child psychotropic visits (1996–1999) to 20.2% (2004–2007) (AOR: 1.89; 95% CI: 1.22–2.94, p<.01). Among medical visits in which a current mental disorder was diagnosed, the percentage with multi-class psychotropic treatment increased from 22.2% (1996–1999) to 32.2% (2004–2007) (AOR: 2.23, 95% CI: 1.42–3.52, p<.001). Over time, there were significant increases in multi-class psychotropic visits in which ADHD medications, antidepressants, or antipsychotics were prescribed, and a decrease in those visits in which mood stabilizers were prescribed. There were also specific increases in co-prescription of ADHD medications and antipsychotic medications (AOR: 6.22, 95% CI: 2.82–13.70, p<.001) and co-prescription of antidepressant and antipsychotic medications (AOR: 5.77, 95% CI: 2.88–11.60, p<.001).
Conclusions
Although little is known about the safety and efficacy of regimens that involve concomitant use of two or more psychotropic agents for children and adolescents, multi-class psychotropic pharmacy is becoming increasingly common in outpatient practice.
Keywords: National Trends, Pediatric Psychopharmacology, Polypharmacy
Psychotropic medications are recommended for the treatment of a range of child and adolescent mental disorders.1 In large-scale short-term placebo-controlled trials, 56% of youth diagnosed with attention-deficit/hyperactivity disorder (ADHD) and treated as outpatients responded to stimulant medication monotherapy,2 61% of depressed adolescents responded to antidepressant monotherapy,3,4 and 55% of youth with common anxiety disorders also responded to antidepressant monotherapy.5 Controlled trials have also evaluated antipsychotic medications for schizophrenia,6 and antipsychotics as well as mood stabilizers as monotherapies for bipolar disorder in youth.7–11 Efficacy of medication treatments in these trials has been less robust, and side effect concerns and drop out rates remain considerable.12
Community practice patterns reveal that a substantial proportion of child and adolescent mental health outpatients are treated with psychotropic medications.13–17 An estimated 85% of youth diagnosed with ADHD and treated as outpatients are prescribed stimulant medications,14 60% of youth outpatients with bipolar disorder are prescribed mood stabilizers,18 and 57% of depressed youth outpatients are treated with antidepressant medications.19
Little is known about the safety and efficacy of regimens that involve concomitant use of two or more psychotropic agents in the outpatient mental health care of children and adolescents.16 Research on this topic has been largely confined to uncontrolled, unblinded, or retrospective reports.20–29 Case reports,20–23 case series,24–26 and retrospective chart reviews,27–29 are limited in the extent to which they can systematically evaluate the safety, tolerability, and efficacy of these complex regimens. Much of the available research on complex regimens involving youth has focused on medication combinations from within the same broad class. For example, there is some empirical support for concomitant use of two mood stabilizers for pediatric bipolar disorder30 and augmentation of methylphenidate with the non-stimulant atomoxetine for youth with ADHD.31 The few controlled studies that have evaluated multi-class psychotropic treatment combinations in youth provide little evidence of improved outcomes over monotherapy regimens.32,33
Polypharmacy refers to the “administration of many drugs together” or “the administration of excessive medication.” 34 Whereas no specific number of concurrently prescribed medications can unequivocally define polypharmacy, in the present study we were interested in trends in the concurrent prescription of two or more psychotropic drugs from across medication classes. Despite a paucity of research evaluating the safety and efficacy of various forms of multi-class psychotropic treatment in youth, many children appear to be treated with multi-class psychotropic regimens.33 Estimates of multi-class treatment in child mental health care, which likely vary by treatment setting, range from 12% to 52% of those receiving at least one psychotropic medication.14,16,35–39 The most commonly reported combinations of multi-class psychotropic pharmacy appear to be co-prescription of a stimulant medication and an antidepressant medication,14,36,40 and co-prescription of an antidepressant and an antipsychotic medication.37 In some youth outpatient populations, there is evidence of increasing psychotropic polypharmacy.14,15,41,42 However, the breadth and extent of this trend remains poorly defined.
The present report examines recent national trends in multi-class youth psychotropic treatment in a large and representative sample of visits to office-based physicians across a twelve year period (1996–2007). Among visits in which a psychotropic medication was prescribed, we examine patterns of multi-class youth psychotropic pharmacy in relation to single-class psychotropic pharmacy by patient socio-demographic and clinical characteristics. We further examine time trends in multi-class psychotropic treatment overall and by medication class.
METHOD
Sample
Data were drawn from 12 consecutive years of the US National Ambulatory Medical Care Survey (NAMCS; http://www.cdc.gov/nchs/ahcd/about_ahcd.htm) from 1996 to 2007. NAMCS is a multistage probability survey of visits to office-based physicians of all medical specialties engaged primarily in direct patient care. The survey response rate varied from 62.9% to 77.1% (median=67.7%). A systematic random sample of visits to each physician was drawn during a randomly selected 1-week period (N=317,416). We limited the sample to 27,979 child (ages 6–17) patient visits in which a physician was seen. The sample for most analyses was further limited to visits in which the child was prescribed at least one of five major psychotropic medication classes: ADHD medications, antidepressants, antipsychotics, mood stabilizers, and sedative-hypnotics (N=3,466 visits). Psychiatrists comprised 24.7% of the prescribing physicians in this sample, and contributed 50.3% (N=1,754) of all psychotropic visits.
Assessments
For each visit, the physician or a member of the physician’s staff provided information about patient socio-demographic and clinical characteristics as well as psychotropic medications prescribed, supplied or administered at the visit.
Psychotropic medications
NAMCS recorded all medications that were ordered, supplied, administered, or continued during each visit. Up to six medications were recorded in each visit in NAMCS 1996–2002. Starting in 2003, the maximum number of medications recorded was increased to eight. To make the years comparable, we limited the maximum number of medications to six in all years. ADHD medications included amphetamine, amphetamine/dextroamphetamine combination, atomoxetine, clonidine, dexmethylphenidate, dextroamphetamine, guanfacine, methylphenidate, and pemoline. We included clonidine and guanfacine as psychotropic medications only if the patient did not have hypertension. Antidepressants included amitriptyline, amoxapine, bupropion, citalopram, clomipramine, desipramine, doxepin, duloxetine, escitalopram, fluoxetine, fluvoxamine, imipramine, isocarboxazid, maprotiline, mirtazapine, nefazodone, nortriptyline, paroxetine, phenelzine, protriptyline, selegiline, sertraline, tranylcypromine, trazodone, trimipramine, and venlafaxine. Antipsychotic medications included aripiprazole, chlorpromazine, clozapine, fluphenazine, haloperidol, loxapine, mesoridazine, molindone, olanzapine, perphenazine, pimozide, quetiapine, risperidone, thioridazine, thiothixene, trifluoperazine, triflupromazine, and ziprasidone. Prochlorperazine, promethazine, droperidol, and prochlorperazine, which are primarily used for non-psychiatric indications, were not included. Mood stabilizers included carbamazepine, lamotrigine, lithium and valproate/divalproex. We included anticonvulsants (carbamazepine, lamotrigine, valproate/divalproex) as psychotropic medications only if the patient did not have a seizure disorder diagnosis. Sedative-hypnotics included alprazolam, butabarbital, chloralhydrate, chlordiazepoxide, chlorazepate, clonazepam, diazepam, diphenhydramine, esczopiclone, estazolam, flurazepam, hydroxyzine, lorazepam, meprobamate, nitrazepam, oxazepam, phenobarbital, secobarbital, temazepam, triazolam, zaleplon, and zolpidem. We included phenobarbital as a psychotropic medication only if the patient did not have a seizure disorder diagnosis. Psychotropic visits were classified into single-class psychotropic pharmacy visits, in which the patient was prescribed psychotropic agent(s) from only one medication class (ADHD medications, antidepressants, antipsychotics, mood stabilizers and sedative-hypnotics), and multi-class psychotropic visits, in which the patient was prescribed two or more psychotropic agents from across different psychotropic medication classes.
Mental disorder diagnoses were recorded based on ICD-9-CM codes (290–319). Up to 3 diagnoses were recorded for each visit. Specific diagnoses were classified into 5 broad categories: (i) disruptive behavior disorders [ICD-9-CM: 312.0–312.2, 312.30–312.38, 312.4–312.9, 313.81, 313.89, 314.0, 314.2–314.9], (ii) mood disorders [ICD-9-CM: 296.0–296.9, 300.4, 301.13, 311], (iii) anxiety disorders [ICD-9-CM: 293.84, 300.0–300.02, 300.09, 300.2, 300.21–300.23, 300.29, 300.3, 300.7, 308.0–308.9, 309.21, 309.81, 312.39, 313.0, 313.21, 313.23], (iv) adjustment disorders [309.0–309.9, except 309.21, 309.81], and (v) pervasive developmental disorders (PDD), mental retardation (MR), and psychotic disorders [ICD-9-CM: 291.0–295.9, 297, 298.0–298.9, 299, 301.2–301.22, 314.1].
Primary source of payment was classified as private insurance, public insurance, self-pay or “other”.
Other variables used in multivariate analyses included patient’s age group (6–12 years vs. 13–17 years), sex, race-ethnicity (white vs. minority), number of mental disorder diagnoses (1 vs. ≥ 2 diagnoses), visit status (returning patient vs. new patient), and physician specialty (psychiatry and psychiatric subspecialties vs. all others).
Data Analysis
Analyses were conducted in two stages. First, we compared the patterns and clinical correlates of multi-class psychotropic visits in relation to single-class psychotropic visits. Next we assessed time trends in multi-class psychotropic treatment for all medication groups and for individual medication groups adjusting for the effects of all demographic and clinical correlates associated with multi-class psychotropic visits at p<.10 (i.e., age group, race-ethnicity, diagnostic status, comorbidity, source of payment, and physician specialty).
All analyses were adjusted for visit weights, clustering, and stratification of data using design elements provided by the National Center for Health Statistics. When adjusted for these design elements, NAMCS data represent annual visits to office-based physicians in the United States.43,44 We examined time trends in the prescription of multi-class psychotropic treatment using multivariate binary logistic models. Survey year was transformed by subtracting 1996 from the year and dividing the results by 11. Thus the transformed value was 0 for the year 1996 and 1 for the year 2007. The odds ratios associated with this transformed variable of survey year represent a change in the odds of multi-class psychotropic visits during the entire study period from 1996 to 2007. Analyses were conducted using the STATA 10 software.45
RESULTS
Overall patterns and clinical correlates of child psychotropic treatment
Between 1996 and 2007, 8.8% (N=3,466) of 27,979 youth visits to U.S. office-based physicians were associated with prescription of a psychotropic medication from the 5 classes described above. A majority of these psychotropic visits (70.7%) were associated with a mental disorder diagnosis. Among psychotropic visits, the most common current diagnostic category carried was disruptive behavior disorders, which includes ADHD (49.2%); followed by mood disorders (21.5%); anxiety disorders (5.6%); PDD, MR, and psychotic disorders (4.0%); and adjustment disorders (3.2%). Psychotropic visits, relative to non-psychotropic visits, included a larger percentage of males (61.7% vs. 49.9%, respectively) [F(1,5260)=96.17, p<.001], youth aged 13–17 years (46.3% vs. 42.7) [F(1,5260)=7.35, p<.01], white children and adolescents (78.2% vs. 72.0%) [F(1,5260)=16.72, p<.001], youth with multiple mental disorder diagnosis (78.4% vs. 0.6%) [F(1,5260)=2497.44, p<.001], and returning patients (91.4% vs. 86.6%) [F(1,5260)=31.16, p<.001]. A majority of child psychotropic visits were provided by non-psychiatrist physicians (64.0%).
Patterns and clinical correlates in multi-class psychotropic treatment
Across the twelve year period, 863 (19%) of the 3,466 of child psychotropic visits included multi-class psychotropic treatment. Table 1 presents patterns and clinical correlates of multi-class psychotropic visits in relation to single-class psychotropic treatment. Distributions for multi-class psychotropic visits significantly differed from single-class visits with regard to age group, mental disorder diagnosis, comorbidity, source of payment, and physician specialty. As compared to single-class psychotropic visits, multi-class psychotropic visits were associated with older patient age, mental disorder diagnoses, multiple mental disorder diagnoses, and public insurance payment. Whereas mood disorders were diagnosed in less than 1 in 6 single-class psychotropic visits, almost half of multi-class psychotropic visits included a mood disorder diagnosis. The percentages of anxiety disorders; adjustment disorders; and PDD, MR, and psychotic disorder diagnoses were roughly three to four times higher among multi-class than single-class psychotropic visits. While most of single-class psychotropic visits were provided by non-psychiatrist physicians, most of the multi-class psychotropic visits were provided by psychiatrists.
Table 1.
Rates and correlates of multi-class psychotropic visitsa and single-class psychotropic visitsb in youth office-based medical visits in which a psychotropic drug is mentioned, United States 1996–2007
| Multi-Class Psychotropic Visits 1996–2007 (N=863) N (%) | Single-Class Psychotropic Visits 1996–2007 (N=2,603) N (%) | Significance test F (1, 2373) | |
|---|---|---|---|
| Age, years | |||
| 6–12 | 394 (45.39) | 1,375 (55.73) | 14.75, p<0.001 |
| 13–17 | 469 (54.61) | 1,228 (44.27) | |
| Sex | |||
| Female | 317 (38.76) | 994 (38.14) | 0.06, p=0.81 |
| Male | 546 (61.24) | 1,609 (61.86) | |
| Race/ethnicity | |||
| White | 699 (81.7) | 2,010 (77.32) | 3.36, p=0.07 |
| Minorities | 164 (18.3) | 593 (22.68) | |
| Any psychiatric disorder | 783 (88.14) | 1,895 (66.51) | 65.91, p<0.001 |
| Selected psychiatric disorders | |||
| Disruptive behavior disorders | 498 (53.7) | 1,265 (48.12) | 3.09, p=0.08 |
| Mood disorders | 398 (44.78) | 550 (15.93) | 160.16, p<0.001 |
| Anxiety disorders | 111 (11.41) | 171 (4.22) | 44.55, p<0.001 |
| Adjustment disorders | 64 (6.96) | 92 (2.24) | 37.13, p<0.001 |
| PDD, MR, and psychotic disorders | 85 (9.76) | 104 (2.56) | 54.78, p<0.001 |
| Number of psychiatric diagnoses | |||
| 1 | 311 (40.73) | 1,340 (51.07) | 147.99, p<0.001 |
| ≥2 | 472 (47.4) | 555 (15.44) | |
| Source of payment | |||
| Private insurance | 269 (46.37) | 660 (55.35) | 8.39, p<.005 |
| Public insurance | 371 (31.95) | 1,356 (24.93) | 6.86, p<0.01 |
| Self-pay or other | 189 (18.6) | 497 (16.35) | 0.59, p=0.44 |
| Visit sequence | |||
| Returning patient | 796 (92.37) | 2,344 (91.14) | 0.85, p=0.36 |
| New patient | 65 (7.63) | 252 (8.86) | |
| Physician specialty | |||
| Psychiatry | 672 (69.59) | 1,103 (27.88) | 248.53, p<0.001 |
| Other | 191 (30.41) | 1,500 (72.12) | |
Note: Data from the National Ambulatory Medical Care Survey (NAMCS). Percentages (%) are based on weighted data. Test statistics reaching statistical significance (p<.05) are in bold. MR = mental retardation; PDD = pervasive developmental disorder.
Multi-class psychotropic visits refer to visits in which patient was prescribed two or more psychotropic agents from across medication classes (see Method section for description of medications in each class).
Single-class psychotropic visits refer to visits in which patient was prescribed psychotropic agent(s) from only one medication class.
Antidepressants were the most common co-prescribed medication class in multi-class visits followed by ADHD medications, antipsychotics, mood stabilizers, and sedative-hypnotics (Table 2). The percentage of pairwise multi-class medication combinations ranged from ADHD medications and antidepressants (7.3% of psychotropic visists) to antipsychotics and sedative-hypnotics (0.6%). Only 34.6% of visits in which ADHD medications were co-prescribed with antidepressants (the most frequent pairwise between-class combination), indicated the presence of both a disruptive behavior disorder and a mood or anxiety disorder.
Table 2.
Number and percentage of drug mentions for ADHD medications, antidepressants, antipsychotics, mood stabilizers, sedative-hypnotics, and multi-class medication combinations among youth office-based medical visits in which a psychotropic drug is mentioned, United States 1996–2007
| Total number and percentage of visits in which each medication or combination is mentioned | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ADHD medications | Antidepressants | Antipsychotics | Mood stabilizers | Sedative-hypnotics | ||||||
| N | %a | N | %a | N | %a | N | %a | N | %a | |
| Any medication in the class | 1,610 | 49.75 | 1,377 | 34.14 | 630 | 13.89 | 426 | 8.58 | 497 | 17.77 |
| Medication Combinations | ||||||||||
| Any concomitant medication class | 506 | 11.37 | 586 | 13.29 | 437 | 9.47 | 278 | 5.97 | 130 | 3.39 |
| Antidepressants | 317 | 7.27 | ||||||||
| Antipsychotics | 214 | 4.65 | 222 | 5.01 | ||||||
| Mood stabilizers | 102 | 2.18 | 137 | 2.89 | 148 | 3.24 | ||||
| Sedative-hypnotics | 35 | 1.02 | 80 | 1.93 | 27 | 0.6 | 32 | 0.79 | ||
Note: Data from the National Ambulatory Medical Care Survey (NAMCS). Percentages (%) are based on weighted data. See Method section for description of medications in each class.
Percentages refer to adjusted rates within total office-based psychotropic visits (N=3,466)
Time trends in multi-class psychotropic visits
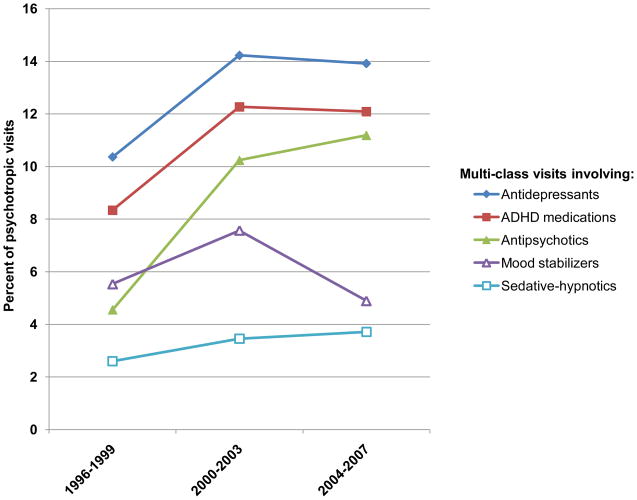
Between 1996–1999 and 2004–2007, there was an approximately 75% increase in the proportion of child and adolescent visits that mentioned a psychotropic medication (from 6.0% in 1996–1999 to 10.6% in 2004–2007). During this period, there was also a significant increase in the percentage of child psychotropic medication visits that included at least two psychotropic classes (Table 3). Across the twelve year period multi-class psychotropic visits rose from 14.3% (1996–1999) to 20.2% (2004–2007) of youth visits including a psychotropic medication. Among psychotropic visits with mental disorder diagnoses, the percentage with multi-class psychotropic visits increased from 22.2% (1996–1999) to 32.2% (2004–2007) (AOR: 2.23, 95% CI: 1.42–3.52, p<.001). Moreover, there were significant increases in multi-class psychotropic visits in which ADHD medications, antidepressants, or antipsychotics were prescribed, and a decrease in visits in which mood stabilizers were prescribed (see Figure 1, details in Table 3). Across this twelve year period, there was not a significant increase in comorbid mental disorder diagnoses among psychotropic visits: 16.5% (1996–1999) and 20.1% (2004–2007) (OR: 1.13, 95% CI: 0.71–1.79, p=0.61).
Table 3.
Trends in multi-class psychotropic visitsa among youth office-based medical visits in which a psychotropic drug is mentioned by psychotropic medication class, United States 1996–2007
| Total office-based medical visits with a psychotropic drug mention | Trend statistic | ||||||
|---|---|---|---|---|---|---|---|
| 1996–1999, (N = 742) | 2004–2007 (N = 1,483) | ||||||
| Multi-class psychotropic visits involving: | N | % | N | % | AORb | 95% CI | p |
| Any 2 or more psychotropic medication classes | 145 | 14.3 | 396 | 20.2 | 1.89 | 1.22–2.94 | .005 |
| ADHD medications | 86 | 8.34 | 246 | 12.09 | 1.94 | 1.13–3.34 | .02 |
| Antidepressants | 111 | 10.36 | 254 | 13.92 | 1.89 | 1.17–3.05 | .009 |
| Antipsychotics | 47 | 4.55 | 225 | 11.19 | 4.38 | 2.50–7.65 | <.001 |
| Sedative-hynotics | 21 | 2.60 | 65 | 3.71 | 1.85 | .77–4.48 | .17 |
| Mood stabilizers | 52 | 5.53 | 110 | 4.89 | 0.57 | .33-.99 | .05 |
Note: Data from the National Ambulatory Medical Care Survey (NAMCS). Percentages (%) are based on weighted data. See Method section for description of medications in each class. Regression coefficients different than 1 at a statistically significant (p<.05) are in bold. Percentages refer to adjusted rates within total office-based psychotropic visits in 1996–1999 (N=742) and 2004–2007 (N=1,483)
Multi-class psychotropic visits refer to visits in which patient was prescribed two or more psychotropic agents from across medication classes.
Odds ratios assocated with the transformed survey year variable: (survey year-1996)/11, adjusted for age group, ethnicity-race, diagnostic status, comorbidity, source of payment, and physician specialty.
Figure 1.
Trends in multi-class psychotropic visitsa involving antidepressants, attention-deficit/hyperactivity disorder (ADHD) medications, antipsychotics, mood stabilizers, or sedative-hypnotics among youth office-based psychiatric visits in which a psychotropic drug is mentioned, United States 1996–2007.
a. Multi-class psychotropic visits refer to visits in which patient was prescribed two or more psychotropic agents from across medication classes
Risperidone, bupropion, and methylphenidate were, respectively, the most commonly prescribed antipsychotic, antidepressant, and ADHD medications in multi-class psychotropic visits in 2004–2007 (20.1%, 13.2%, and 28.3% of multi-class visits, respectively). Risperidone was prescribed in 36.0% of multi-class psychotropic visits involving an antipsychotic medication (82 of 225 such visits), bupropion was prescribed in 19.0% of multi-class psychotropic visits involving an antidepressant medication (44 of 254 such visits), and methyphenidate was prescribed in 46.8% of multi-class psychotropic visits involving an ADHD medication (121 of 246 such visits). In addition, multi-class psychotropic prescribing occurred in 61.5% of all youth visits in which risperidone was prescribed (82 of 130 such visits), in 57.7% of all visits in which bupropion was prescribed (44 of 84 such visits), and in 19.7% of all visits in which methylphenidate was prescribed (121 of 411 such visits) (data not shown). The visits involving concomitant use of medications in years 2004–2007 were not limited to a small group of physicians—the 254 visits involving concomitant prescription of antidepressants and other psychotropic medications came from 131 unique physician practices. Similarly, the 246 visits involving concomitant prescription of ADHD medications and other psychotropic medications came from 115 unique practices, and the 225 visits involving concomitant prescription of antipsychotics with other psychotropic medications came from 92 unique practices. Overall, of the 518 unique physician practices conducting the 1,483 psychotropic visits involving children and adolescents between 2004–2007, 156 practices (30.1%) reported multi-class psychotropic visits. The proportion of physicians prescribing medications from different groups concomitantly was greater among psychiatrists than other physicians. Of 119 unique psychiatrists prescribing psychotropic medications between 2004–2007, 93 (78.2%) prescribed medications from different groups concomitantly; whereas only 63 (15.8%) of the 399 unique non-psychiatrists physicians prescribing psychotropic medications in this period prescribed medication from different groups concomitantly.
Over time, there were specific increases in the co-prescription of ADHD and antipsychotic medications (AOR=6.22, 95% CI=2.82–13.70, p<.0001) and the co-prescription of antidepressant and antipsychotic medications (AOR=5.77, 95% CI=2.88–11.60, p<.0001). The other eight possible pairwise multi-class combinations remained stable across time (data not shown).
DISCUSSION
The findings of this study should be interpreted in the context of several limitations. First, despite adjustment for several visit and patient characteristics, including diagnosis, insurance and physician speciality, we cannot exclude the possibility that the trends reflect residual confounding due to unmeasured differences among patient groups across survey years. Second, it is also not possible to determine previous clinical response to single-class psychotropic regimens or measure the effects of multi-class psychotropic pharmacy on clinical outcomes. It is also possible that some of the multi-class psychotropic treatment represents cross-tapering as part of psychotropic switching. Third, the survey underestimates the number of psychotropic medications used by patients who may be receiving mental health care from more than one physician. NAMCS does not provide population prevalence estimates but prevalence estimates of diagnoses and treatments in a representative sample of visits to office-based physicians. Fourth, because the surveys are limited to office-based practices, the results do not generalize to other treatment settings where children may receive mental health care. Fifth, limited numbers of visits preclude multi-class treatment estimates for specific diagnostic groups such as distinguishing bipolar disorder from major depressive disorder, or smaller demographic groups such as racial-ethnic minorities, as well as polypharmacy trends stratified by physician specialty. Sixth, diagnostic determinations may vary over time with changing practice patterns. Without structured diagnostic interviews, it is not possible to examine these variations. Moreover, roughly 29% of psychotropic visits were not associated with a mental disorder diagnosis. The extent to which this may have been due to underdiagnosis, failure to document diagnosed mental disorders, or non-psychiatric targets is not clear. Finally, because NAMCS records visits rather than patients, some patient duplication may occur during the 1-week sampling period. Despite these limitations, the NAMCS offers a rare national statistical portrait of multi-class psychotropic treatment trends in youth office-based medical practice.
In recent years, multi-class psychotropic treatment has become increasingly common in the office-based medical care of American children and adolescents. During the study period, the proportion of outpatient medical visits in which psychotropic medications from two or more medication classes were prescribed to children increased from one in seven visits to one in five visits. This finding extends earlier reports of increasing overall psychotropic medication treatment of children and adolescents,13–15,18 and increasing psychotropic co-prescribing.35–38,40 The results also parallel the broader literature documenting increased psychotropic co-prescribing trends in adult medical care.46–50
While it is reassuring that youth multi-class psychotropic pharmacy is concentrated among treatment provided by psychiatrists and patients with indications of more complex psychopathology, the safety and effectiveness of these regimens in youth remain poorly characterized. Despite advances in our understanding of the short-term efficacy and safety of many classes of psychotropic medications as monotherapies for youth,2–5 there are currently few controlled evaluations of multi-class psychotropic treatment regimens in this age group. Relevant research is largely limited to small or retrospective studies21,23,25–27 and these studies have yielded mixed findings regarding safety and tolerability of these regimens.
Given the frequency and increasing prevalence of multi-class psychotropic treatment in children, there is a pressing need for clinical trials to evaluate the safety and efficacy of these complex combinations. Between 1996 and 2007, antidepressant and ADHD medication combinations were the most prevalent multi-class psychotropic regimen. Accordingly, this regimen appears to be a promising candidate for controlled evaluations.
The use of antipsychotic medications in conjunction with other classes of psychotropic medication in children also appears to be on the rise. One published controlled trial evaluating the combined use of antipsychotic and stimulant medications in youth did not find that this combination offered improved clinical outcomes over psychotropic monotherapy options.32 To date no prospective clinical trials have evaluated use of second generation antipsychotoics in conjunction with other psychotropic medication classes in youth. Several antipsychotics used as monotherapies have FDA approved indications in children and adolescents. However, evaluations of these medications used as monotherapies in child populations have produced somewhat mixed efficacy findings and adverse metabolic effects of second-generation antipsychotic medications appear to pose a particular challenge.51–55
Several possible factors may have contributed to the recent increase in multi-class psychotropic treatment in children’s outpatient care. First, greater patient, parent, or physician emphasis on symptom reduction with diminishing concern regarding polypharmacy may have contributed to the trend.56 Second, an increasing number of psychiatrists are specializing in pharmacotherapy, to the exclusion of psychosocial treatments.57 Limitations in the availability and accessibility of psychosocial interventions may place heavy clinical demands on the pharmacological dimensions of child and adolescent mental health care. Third, some physicians may generalize to children and adolescents psychotropic prescribing practices that have been evaluated in adult populations.58–60 Fourth, changes in patient characteristics, including increasing severity of illnesses or comorbidities61–63 might play a role in the trend toward multi-class treatment, though the overall trend in our study persisted after adjusting for psychiatric diagnosis and comorbidity. Finally, the availability of new psychotropic medications during the study period and the presumably large number of patients who exhibit only partial symptomatic responses to monotherapy likely contributed to the increased use of complex pharmacological regimens.
While the contributions of the above factors to the observed trends in multi-class psychotropic treatment remain to be elucidated in future research, a number of physician training programs, quality improvement initiatives, and explicit criteria have been developed in an effort to restrain the growth of polypharmacy in mental health care.46,49,64–66 Yet despite these efforts, the overall rate of multi-class psychotropic treatment in child outpatient practice has increased significantly in recent years. The increasing share of mental health care costs attributable to pharmaceutical expenditures that accompanies this practice risks increasing administrative mandates and coverage restrictions by third party payors.67 To guide optimal medication management, a new generation of research is needed to identify the clinical circumstances in which psychotropic regimens with multiple classes yield outcomes that are superior to optimized single class regimens.
Acknowledgments
This work was supported by AHRQ U18 HS016097 and NIH T32 MH016434.
Footnotes
The authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosure: Dr. Olfson, in the past five years, has received investigator initiated grants from AstraZeneca, Bristol-Myers Squibb, and Eli Lilly and Co. He has served on the speakers’ bureau for Janssen Pharmaceutica, and as a consultant to Pfizer, AstraZeneca, Eli Lilly and Co., and Bristol-Myers Squibb. Dr. Mojtabai has received research funding and consulting fees from Bristol-Myers Squibb. Dr. Comer reports no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Jonathan S. Comer, College of Physicians and Surgeons, Columbia University and the New York State Psychiatric Institute, New York, New York.
Dr. Mark Olfson, College of Physicians and Surgeons, Columbia University and the New York State Psychiatric Institute, New York, New York.
Dr. Ramin Mojtabai, Bloomberg School of Public Health and Johns Hopkins University, Baltimore, Maryland.
References
- 1.AACAP Work Group on Quality Issues. Practice parameter on the use of psychotropic medication in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2009;48:961–973. doi: 10.1097/CHI.0b013e3181ae0a08. [DOI] [PubMed] [Google Scholar]
- 2.Swanson JM, Kraemer HC, Hinshaw SP, et al. Clinical relevance of the primary findings of the MTA: Success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry. 2002;40:168–179. doi: 10.1097/00004583-200102000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Bridge JA, Iyengar S, Salary CB, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007;297:1683–1696. doi: 10.1001/jama.297.15.1683. [DOI] [PubMed] [Google Scholar]
- 4.TADS Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescetns with Depression Study (TADS) randomized controlled trial. JAMA. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- 5.Walkup JT, Albano AM, Piacentini J, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Eng J Med. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sikich L, Frazier JA, McClellan J, et al. Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizoaffective disorder: Findings from the Treatment of Early-Onset Schizophrenia Spectrum disorders (TEOSS) study. Am J Psychiatry. 2008;165:1420–1431. doi: 10.1176/appi.ajp.2008.08050756. [DOI] [PubMed] [Google Scholar]
- 7.Findling RL, McNamara NK, Branicky LA, Schluchter MD, Lemon E, Blumer JL. A double-blind pilot study of risperidone in the treatment of conduct disorder. J Am Acad Child Adolesc Psychiatry. 2000;39:509–516. doi: 10.1097/00004583-200004000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Findling RL, Robb A, Nyilas M, et al. A multiple-center, randomized, double-blind, placebo-controlled study of oral aripiprazole for treatment of adolescents with schizophrenia. Am J Psychiatry. 2008;165:1432–1441. doi: 10.1176/appi.ajp.2008.07061035. [DOI] [PubMed] [Google Scholar]
- 9.Pavuluri MN, Henry DB, Moss M, Mohammed T, Carbray JA, Sweeney JA. Effectiveness of lamotrigine in maintaining symptom control in pediatric bipolar disorder. J Child Adolesc Psychopharm. 2009;19:75–82. doi: 10.1089/cap.2008.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wagner KD, Kowatch RA, Emslie G, et al. A double-blind, randomized, placebo-controlled trial of oxcarbazepine in the treatment of bipolar disorder in children and adolescents. Am J Psychiatry. 2006;163:1179–1186. doi: 10.1176/ajp.2006.163.7.1179. [DOI] [PubMed] [Google Scholar]
- 11.Wagner KD, Redden L, Kowatch RA, et al. A double-blind, randomized, placebo-controlled trial of divalproex extended-release in the treatment of bipolar disorder in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2009;48:519–532. doi: 10.1097/CHI.0b013e31819c55ec. [DOI] [PubMed] [Google Scholar]
- 12.Correll CU, Manu P, Olshanskiy V, Napolitano B, Kane JM, Malhotra AK. Cardiometabolic risk of second-generation antipsychotic medications during first-time use in children and adolescents. JAMA. 2009;302:1765–1773. doi: 10.1001/jama.2009.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olfson M, Blanco C, Liu L, Moreno C, Laje G. National trends in the outpatient treatment of children and adolescents with antipsychotic drugs. Arch Gen Psychiatry. 2006;63:679–685. doi: 10.1001/archpsyc.63.6.679. [DOI] [PubMed] [Google Scholar]
- 14.Olfson M, Gameroff MJ, Marcus SC, Jensen PS. National trends in the treatment of attention deficit hyperactivity disorder. Am J Psychiatry. 2003;160:1071–1077. doi: 10.1176/appi.ajp.160.6.1071. [DOI] [PubMed] [Google Scholar]
- 15.Olfson M, Marcus SC, Weissman MM, Jensen PS. National trends in the use of psychotropic medications by children. J Am Acad Child Adolesc Psychiatry. 2002;41:514–521. doi: 10.1097/00004583-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Zito JM, Safer DJ, dosReis S. Psychotropic practice patterns for youth: a 10-year perspective. Arch Pediatr Adolesc Med. 2003;157:17–25. doi: 10.1001/archpedi.157.1.17. [DOI] [PubMed] [Google Scholar]
- 17.Zito JM, Safer DJ, dosReis S, Gardner JF, Boles M, Lynch F. Trends in the prescribing of psychotropic medications to preschoolers. JAMA. 2000;283:1025–1030. doi: 10.1001/jama.283.8.1025. [DOI] [PubMed] [Google Scholar]
- 18.Moreno C, Laje G, Blanco C, Jiang H, Schmidt AB, Olfson M. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64:1032–1039. doi: 10.1001/archpsyc.64.9.1032. [DOI] [PubMed] [Google Scholar]
- 19.Olfson M, Gameroff MJ, Marcus SC, Waslick BD. Outpatient treatment of child and adolescent depression in the United States. Arch Gen Psychiatry. 2003;60:1236–1242. doi: 10.1001/archpsyc.60.12.1236. [DOI] [PubMed] [Google Scholar]
- 20.Feeney DJ, Klykylo W. Risperidone and tardive dyskinesia. J Am Acad Child Adolesc Psychiatry. 1996;35:1421–1422. doi: 10.1097/00004583-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 21.George AK, Kunwar AR, Awasthi A. Acute myocardial infarction in a young male on methyphenidate, bupropion, and erythromycin. J Child Adolesc Psychopharm. 2005;15:693–695. doi: 10.1089/cap.2005.15.693. [DOI] [PubMed] [Google Scholar]
- 22.Jaworowski S, Benarroch F, Gross-Tsur V. Concomitant use of atomoxetine and OROS methylphenidate in a 10-year-old child suffering from attention-deficit/hyperactivity disorder with comorbid bipolar disorder and Tourette syndrome. J Child Adolesc Psychopharm. 2006;16:365–370. doi: 10.1089/cap.2006.16.365. [DOI] [PubMed] [Google Scholar]
- 23.Schertz M, Steinberg T. Seizures induced by the combination treatment of methylphenidate and sertraline. J Child Adolesc Psychopharm. 2006;18:301–303. doi: 10.1089/cap.2007.0141. [DOI] [PubMed] [Google Scholar]
- 24.Carlson GA, Rapport MD, Kelly KL, Pataki CS. The effects of methylphenidate and lithium on attention and activity level. J Am Acad Child Adolesc Psychiatry. 1992;31:262–270. doi: 10.1097/00004583-199203000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Emiroglu FN, Neslihan I, Gencer O, Ozbek A. Adjunctive olanzapine treatment in bipolar adolescents responding insufficiently to mood stabilizers. Four case reports. Eur Child Adolesc Psychiatry. 2006;15:500–503. doi: 10.1007/s00787-006-0552-5. [DOI] [PubMed] [Google Scholar]
- 26.Pathak S, Johns ES, Kowatch RA. Adjunctive quetiapine for treatment-resistent adolescent major depressive disorder: A case series. J Child Adolesc Psychopharm. 2005;15:696–702. doi: 10.1089/cap.2005.15.696. [DOI] [PubMed] [Google Scholar]
- 27.Gonzalez-Heydrich J, Raches D, Wilens TE, Leichtner A, Mezzacappa E. Retrospective study of hepatic enzyme elevations in children treated with olanzapine, divalproex, and their combination. J Am Acad Child Adolesc Psychiatry. 2003;42:1227–1233. doi: 10.1097/00004583-200310000-00014. [DOI] [PubMed] [Google Scholar]
- 28.Kafantaris V, Coletti D, Dicker R, Gina P, Kane J. Adjunctive antipsychotic treatment of adolescents with bipolar psychosis. J Am Acad Child Adolesc Psychiatry. 2001;40:1448–1456. doi: 10.1097/00004583-200112000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Marchand WR, Wirth L, Simon C. Quetiapine adjunctive and monotherapy for pediatric bipolar disorder: A retrospective chart review. J Child Adolesc Psychopharm. 2004;14:405–411. doi: 10.1089/cap.2004.14.405. [DOI] [PubMed] [Google Scholar]
- 30.Findling RL, McNamara NK, Stansbrey R, et al. Combination lithium and divalproex sodium in pediatric bipolar symptom restabilization. J Am Acad Child Adolesc Psychiatry. 2006;45:142–148. doi: 10.1097/01.chi.0000189135.05060.8a. [DOI] [PubMed] [Google Scholar]
- 31.Carlson GA, Dunn D, Kelsey D, et al. A pilot study for augmenting atomoxetine with methylphenidate: Safety of concomitant therapy in children with attention-deficit/hyperactivity disorder. Child Adolesc Psychiatry Mental Health. 2007;2:ArtID 10. doi: 10.1186/1753-2000-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gittelman-Klein R, Klein D. Comparative effects of methylphenidate and thioridazine in hyperkinetic children: I. Clinical results. Arch Gen Psychiatry. 1976;33:1217–1231. doi: 10.1001/archpsyc.1976.01770100079008. [DOI] [PubMed] [Google Scholar]
- 33.Safer DJ, Zito JM, dosReis S. Concomitant psychotropic medication for youths. Am J Psychiatry. 2003;160:438–449. doi: 10.1176/appi.ajp.160.3.438. [DOI] [PubMed] [Google Scholar]
- 34.Dorland’s illustrated medical dictionary. 31. Philadelphia, PA: Saunders; 2007. [Google Scholar]
- 35.Dean AJ, McDermott BM, Marshall R. Psychotropic medication utilization in a child and adolescent mental health service. J Child Adolesc Psychopharm. 2006;16(3):273–285. doi: 10.1089/cap.2006.16.273. [DOI] [PubMed] [Google Scholar]
- 36.Duffy FF, Narrow WE, Rae DS, et al. Concomitant pharmacotherapy among youths treated in routine psychiatric practice. J Child Adolesc Psychopharm. 2005;15:12–24. doi: 10.1089/cap.2005.15.12. [DOI] [PubMed] [Google Scholar]
- 37.Martin A, Van Hoof T, Stubbe D, Sherwin T, Scahill L. Multiple psychotropic pharmacotherapy among child and adolescent enrollees in Connecticut Medicaid managed care. Psychiatr Serv. 2003;54:72–77. doi: 10.1176/appi.ps.54.1.72. [DOI] [PubMed] [Google Scholar]
- 38.Safer DJ. Changing patterns of psychotropic medications prescribed by child psychiatrists in the 1990s. J Child Adolesc Psychopharm. 1997;7:267–274. doi: 10.1089/cap.1997.7.267. [DOI] [PubMed] [Google Scholar]
- 39.Sevilla-Dedieu C, Kovess-Masfety V. Psychotropic medication use in children and adolescents: a study from France. J Child Adolesc Psychopharm. 2008;18:281–289. doi: 10.1089/cap.2007.0091. [DOI] [PubMed] [Google Scholar]
- 40.dosReis S, Zito JM, Safer DJ, Gardner JF, Puccia KB, Owens PL. Multiple psychotropic medication use for youths: A two-state comparison. J Child Adolesc Psychopharm. 2005;15:68–77. doi: 10.1089/cap.2005.15.68. [DOI] [PubMed] [Google Scholar]
- 41.Bhatara V, Feil M, Hoagwood K, Vitiello B, Zima B. National trends in concomitant psychotropic medication with stimulants in pediatric visits: practice versus knowledge. J Atten Disord. 2004;7:217–226. doi: 10.1177/108705470400700404. [DOI] [PubMed] [Google Scholar]
- 42.McIntyre RS, Jerrell JM. Polypharmacy in children and adolescents treated for major depressive disorder: a claims database study. J Clin Psychiatry. 2009;70:240–246. doi: 10.4088/jcp.08m04212. [DOI] [PubMed] [Google Scholar]
- 43.Cherry DK, Hing E, Woodwell DA, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2006 summary. Natl Health Stat Report. 2008:1–39. [PubMed] [Google Scholar]
- 44.Woodwell DA. National Ambulatory Medical Care Survey: 1996 summary. Adv Data. 1997:1–25. [PubMed] [Google Scholar]
- 45.Stata Statistical Software. Release 10 [computer program] Version. College Station, TX: Stata Corporation; 2008. [Google Scholar]
- 46.Ghaemi SN. Polypharmacy in psychiatry. New York: Dekker; 2002. [Google Scholar]
- 47.Haider SI, Johnell K, Thorslund M, Fastbom J. Trends in polypharmacy and potential drug-drug interactions across educational groups in elderly patients in Sweden for the period 1992–2002. Int J Clin Pharm Ther. 2007;45:643–653. doi: 10.5414/cpp45643. [DOI] [PubMed] [Google Scholar]
- 48.Mojtabai R, Olfson M. National trends in psychotropic medication polypharmacy in office-based psychiatry. Arch Gen Psychiatry. 2010;67:17–24. doi: 10.1001/archgenpsychiatry.2009.175. [DOI] [PubMed] [Google Scholar]
- 49.Preskorn SH, Lacey RL. Polypharmacy: when is it rational? J Psychiatr Pract. 2007;13:97–105. doi: 10.1097/01.pra.0000265766.25495.3b. [DOI] [PubMed] [Google Scholar]
- 50.Trivedi MH, Fava M, Wisniewski SR, et al. Medication augmentation after the failure of SSRIs for depression. N Engl J Med. 2006;354:1243–1252. doi: 10.1056/NEJMoa052964. [DOI] [PubMed] [Google Scholar]
- 51.Toren P, Ratner S, Laor N, Weeizman A. Benefit-risk assessment of atypical antipsychotics in the treatment of schizophrenia and comorbid disorders in children and adolescents. Drug Saf. 2004;27:1135–1156. doi: 10.2165/00002018-200427140-00005. [DOI] [PubMed] [Google Scholar]
- 52.Pappagallo M, Silva R. The effect of atypical antipsychotic agents on prolactin levels in children and adolescents. J Child Adolesc Psychopharmacol. 2004;14:359–371. doi: 10.1089/cap.2004.14.359. [DOI] [PubMed] [Google Scholar]
- 53.Findling RL, McNamara NK. Atypical antipsychotics in the treatment of children and adolescents: Clinical applications. J Clin Psychiatry. 2004;65(suppl6):30–44. [PubMed] [Google Scholar]
- 54.Sikich L, Hamer RM, Bashford RA, Sheitman BB, Leiberman JA. A pilot study of risperidone, olanzapine, and haloperidol in psychotic youth: a double-blind, randomized 8-week trial. Neuropsychopharmacology. 2004;29:133–145. doi: 10.1038/sj.npp.1300327. [DOI] [PubMed] [Google Scholar]
- 55.King B, Zwi K, Nonn K, Longworth J, Dossetor D. Use of risperidone in a paediatric population: an observational study. J Paediatr Child Health. 2003;39:523–527. doi: 10.1046/j.1440-1754.2003.00205.x. [DOI] [PubMed] [Google Scholar]
- 56.Stahl SM. Stahl’s essential pschopharmacology: Neuroscientific basis and practical applications. 3. New York: Cambridge University Press; 2008. [Google Scholar]
- 57.Mojtabai R, Olfson M. National trends in psychotherapy by office-based psychiatrists. Arch Gen Psychiatry. 2008;65:962–970. doi: 10.1001/archpsyc.65.8.962. [DOI] [PubMed] [Google Scholar]
- 58.American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder. Am J Psychiatry. 2000;157(suppl 4):1–45. [PubMed] [Google Scholar]
- 59.American Psychiatric Association. Practice guideline for the treatment of patients with bipolar disorder. Am J Psychiatry. 2002;159:1–50. [PubMed] [Google Scholar]
- 60.Wijkstra J, Lijmer J, Balk F, Geddes J, Nolen WA. Pharmacological treatment for psychotic depression. Cochrane Database Syst Rev. 2005:CD004044. doi: 10.1002/14651858.CD004044.pub2. [DOI] [PubMed] [Google Scholar]
- 61.Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 2009;40:57–87. [PubMed] [Google Scholar]
- 62.Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: phenomenology, prevalence, and comorbidity. Child Adolesc Psychiatr Clin N Am. 2005;14:631–648. doi: 10.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 63.Drabick DAG, Gadow KD, Loney J. Source-specific oppositional defiant disorder: comorbidity and risk factors in referred elementary schoolboys. J Am Acad Child Adolesc Psychiatry. 2007;46:92–101. doi: 10.1097/01.chi.0000242245.00174.90. [DOI] [PubMed] [Google Scholar]
- 64.Goren JL, Parks JJ, Ghinassi FA, et al. When is antipsychotic polypharmacy supported by research evidence? Implications for QI. Jt Comm J Qual Patient Saf. 2008;34:571–582. doi: 10.1016/s1553-7250(08)34072-0. [DOI] [PubMed] [Google Scholar]
- 65.Meyer TJ, Van Kooten D, Marsh S, Prochazka AV. Reduction of polypharmacy by feedback to clinicians. J Gen Intern Med. 1991;6:133–136. doi: 10.1007/BF02598309. [DOI] [PubMed] [Google Scholar]
- 66.Thompson A, Sullivan SA, Barley M, et al. The DEBIT trial: an intervention to reduce antipsychotic polypharmacy prescribing in adult psychiatry wards – a cluster randomized controlled trial. Psychol Med. 2008;38(5):705–715. doi: 10.1017/S003329170700147X. [DOI] [PubMed] [Google Scholar]
- 67.Frank RG, Goldman HH, McGuire TG. Trends in mental health cost growth: an expanded role for management? Health Affairs. 2009;28:649–659. doi: 10.1377/hlthaff.28.3.649. [DOI] [PubMed] [Google Scholar]