Abstract
Study Objectives:
To investigate the prevalence of restless legs syndrome (RLS) in fibromyalgia (FM) and determine the presence and amount of sleep disruption in FM patients with RLS. RLS and FM have been associated in uncontrolled studies using a variety of RLS definitions. We explored this relationship using a cross-sectional study design.
Methods:
FM cases that met the American College of Rheumatology diagnostic criteria were recruited through an academic referral clinic and advertising. Pain- and fatigue-free controls were recruited from the Seattle metropolitan area. We enrolled 172 FM patients (mean age 50 years, 93% female) and 63 pain- and fatigue-free controls (mean age 41 years, 56% female). RLS was ascertained by a self-administered validated diagnostic interview.
Results:
The age- and gender-adjusted prevalence of RLS was higher in the FM group than the control group (33.0%; 95% CI: 25.9, 40.1 vs. 3.1%; 95% CI: 0.0, 7.4; p = 0.001). Likewise, the FM group was more likely to report RLS (OR = 11.7; 95% CI: 2.6, 53.0), even after adjusting for age and gender. The mean Pittsburgh Sleep Quality Index score was higher among FM patients with RLS than those without (11.8 vs. 9.9; p = 0.01) but subjective limb pain measures did not differ between these 2 groups.
Conclusions:
There is a higher prevalence and odds of RLS in those with FM compared to controls. Clinicians should routinely query FM patients regarding RLS symptoms because treatment of RLS can potentially improve sleep and quality of life in these patients.
Citation:
Viola-Saltzman M; Watson NF; Bogart A; Goldberg J; Buchwald D. High prevalence of restless legs syndrome among patients with fibromyalgia: a controlled cross-sectional study. J Clin Sleep Med 2010;6(5):423-427.
Keywords: Restless legs syndrome, fibromyalgia, pain, insomnia, sleep
Restless legs syndrome (RLS) is a sensorimotor disorder characterized by an urge for leg movement, often accompanied by an uncomfortable sensation deep within the legs.1 Leg movement relieves the discomfort. RLS can be an idiopathic condition, or occur secondary to iron deficiency, peripheral neuropathy, uremia, pregnancy, medication side-effects, and other conditions.2 The disorder has a familial component, is clinically diagnosed, more common in women, and disrupts sleep.1,2 Fibromyalgia (FM) is a chronic disorder of widespread pain lasting three or more months accompanied by at least 11 of 18 tender point sites.3 FM also clusters in families, is nine times more common in women than men,4 and is characterized by non-restorative sleep and nocturnal awakenings.5 FM is also associated with obstructive sleep apnea,6,7 periodic leg movements during sleep,6–9 and excessive daytime somnolence.6,7 Fatigue5–7 and insomnia6,7,10 are more common in patients with FM than pain-free controls.
The clinical overlap between RLS and FM has motivated researchers to search for a link between these disorders. Although the reported prevalence of RLS in FM is between 20% and 65.7%,6–8,10–12 these studies were limited by non-validated or poorly described methods for diagnosing one or both disorders6–8,10–12 or lacked a control group, obviating risk estimation.6,7,10,12 To clarify if and how FM is related to RLS, we examined adults with FM and controls with a cross-sectional study design. Our goals were to (1) investigate the prevalence of RLS in FM using a validated RLS screening tool, (2) estimate the strength of the association between RLS and FM, and (3) establish whether RLS disrupts sleep over and above the sleep disruption observed in FM patients.
BRIEF SUMMARY
Current Knowledge/Study Rationale: The clinical overlap between restless legs syndrome and fibromyalgia motivated us to investigate whether these two disorders are related. We were also interested in determining if there was a difference in the amount of sleep disruption in fibromyalgia patients with and without restless legs syndrome.
Study Impact: Restless legs syndrome was found to have a high prevalence in those with fibromyalgia and may be the cause of increased sleep disruption in these patients. Screening fibromyalgia patients for restless legs syndrome may help improve their sleep and quality of life.
METHODS
Study Participants
All individuals in the present study were involved in a parent study of Chiari I malformation and FM.13 Those with FM were identified either through an academic referral clinic devoted to the evaluation of chronic pain and fatigue or local advertising in the Seattle, Washington metropolitan area. The FM group was required to (1) be ≥ 18 years of age; (2) not be pregnant; and (3) have FM by self-report or review of the medical records. A Research Coordinator trained by one of our team (DB) verified the diagnosis of FM according to the 1990 American College of Rheumatology guidelines by confirming the presence of chronic, widespread pain and ≥ 11 of 18 tender points on examination.3
Control participants, recruited through advertising at 3 medical institutions, were required to (1) be ≥ 18 years of age; (2) not be pregnant, and; (3) deny chronic, widespread pain and chronic fatigue. The Research Coordinator screened controls on the telephone for pain and FM-related symptoms using the validated London Fibromyalgia Epidemiology Study Screening Questionnaire.14
Restless Legs Syndrome Diagnosis
RLS was ascertained by a self-administered modified John Hopkins telephone diagnostic interview.15 Questions determined the (1) presence of recurrent, uncomfortable feelings or sensations in the legs (or urge to move the legs) while sitting or lying down; (2) whether the discomfort was worse when resting; (3) if the discomfort improved or resolved with walking; and (4) whether the discomfort was worst in the evening or nighttime. Only participants endorsing all 4 questions were considered to have RLS.
Sleep Measures
Sleep quality, insomnia, and sleepiness were assessed using a self-administered Pittsburgh Sleep Quality Index, Insomnia Severity Index, and Epworth Sleepiness Scale. The Pittsburgh Sleep Quality Index consists of 19 self-rated questions with high test-retest reliability and good validity in patients with primary insomnia.16 The Insomnia Severity Index is a 7-question quantitative instrument with proven reliability and validitiy.17 Lastly, the Epworth Sleepiness Scale is a commonly used 8-question measure of recent excessive daytime somnolence.18
Subjective Pain Measurement
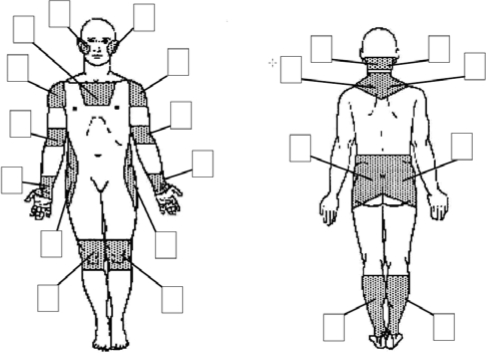
Participants were asked about their average pain intensity over the past month on a 5-point scale (0 = no pain, 5 = intolerable pain) from a diagram representing 11 anatomic areas encompassing a total of 21 separate measures (Figure 1). Total body pain was calculated from the pain intensity sum of all 21 measures, with a maximum score of 105. Distal leg pain was calculated from pain intensity scores from the knees and calves, and distal arm pain was calculated from the forearm and wrist: both have maximum scores of 20.
Figure 1.
On the diagram, subjects were asked to rate the average intensity of pain for the last month in each shaded body area
Objective Pain Measurement
Using a standard protocol, a Chattilon variable pressure dolorimeter, a spring-loaded gauge with a range of 0-12 kg, was used by a trained research assistant to apply pressure at a rate of 1 kg/sec to 9 bilateral tender points identified in the American College of Rheumatology definition of FM.3 Three additional sites tested in the same manner included the mid-forehead, dorsum of right forearm, and left thumbnail.19 Participants verbally indicated when the pain level was noticeable (threshold). Pressure was discontinued when a threshold was indicated or when a maximum pressure of 12 kg was attained, whichever came first. Threshold pressure levels were recorded for each tender point. Because RLS is predominantly a disorder of the limbs, we focused on measures from the lateral epicondyles, right forearm, left thumbnail, greater trochanters, and knees. Measures from the lateral epicondyles, greater trochanters, and knees were averaged over the left and right sides of the body.
Statistical Analysis
We estimated the prevalence of RLS in the groups defined by FM status. Unadjusted estimates came from simple cross tabulation of FM and RLS status. To estimate the age and gender-adjusted prevalence of RLS by FM group, we fit a logistic model of RLS status on FM status, and included linear adjustment for age and a binary indicator of female gender. We transformed the predicted log odds from this model for each participant to the probability scale, and calculated the mean predicted probability and its 95% confidence interval. We conducted t-tests to compare mean Pittsburgh Sleep Quality Index, Insomnia Severity Index, and Epworth Sleepiness Scale scores in FM participants with and without RLS. Because the self-reported pain measures and the dolorimetry threshold tended to be markedly right skewed, we compared distributions across RLS groups using the Wilcoxon Rank Sum test. We compared sleep and pain measures by RLS status in the FM group using t-tests and Rank Sum tests. For all measures, statistical significance was set at p < 0.05. Stata 10 statistical package (StataCorp LP, College Station, Texas, USA) was used for all analyses.
RESULTS
We recruited 172 participants with FM; the mean age was 50 years, and 93% were female. The control group was composed of 63 participants; the mean age was 41 years, and 56% female. The FM group was more likely to be married and less likely to be employed. Table 1 provides further demographic details. The age and gender adjusted prevalence of RLS in the FM group was 33.0% (95% CI: 25.9, 40.1), significantly higher than the control group (3.1%; 0.0, 7.4; p < 0.01), as shown in Table 2. For individuals with FM, the age and gender adjusted odds of RLS were 11.7 (2.6, 53.0; p < 0.01) times higher than for the pain- and fatigue-free controls. Likewise, the fully adjusted model, which included age, gender, ethnicity, marital status, employment, education, and income, confirmed an increased odds of RLS in FM of 11.2 (2.3, 54.6; p < 0.01) compared to controls.
Table 1.
Participant characteristics by FM status
| Characteristic | FM (n = 172) | Controls (n = 63) |
|---|---|---|
| Age (years), mean (SD) | 50 (10) | 41 (10) |
| Female % | 93 | 56 |
| Married or living as married, % | 57 | 32 |
| Education, years, % | ||
| 0 – 12 | 15 | 13 |
| 13 – 16 | 58 | 56 |
| 17 or more | 27 | 31 |
| Employed at least part time, % | 29 | 73 |
| Annual household income, % | ||
| $0 – 14,999 | 27 | 23 |
| $15,000 – 24,999 | 13 | 21 |
| $25,000 – 34,999 | 10 | 16 |
| $35,000 – 49,999 | 15 | 7 |
| $50,000 or more | 35 | 32 |
Table 2.
Sleep and pain measures by FM status
| Measure | FM (n = 172) | Controls (n = 63) | p-value |
|---|---|---|---|
| Sleep Measures | |||
| Restless legs syndrome, adjusted odds ratio | 33.0 | 3.1 | < 0.01 |
| Pittsburgh Sleep Quality Index, mean (SD)a | 10.6 (3.6) | 4.5 (3.1) | < 0.01 |
| Insomnia Severity Index, mean (SD)a | 18.9 (6.0) | 12.1 (5.8) | < 0.01 |
| Epworth Sleepiness Scale, mean (SD)a | 9.4 (4.8) | 5.7 (4.0) | < 0.01 |
| Self-rated pain measuresb | |||
| Distal arm pain, median* | 6 (6) | 0 (0) | < 0.01 |
| Distal leg pain, median* | 8 (6.5) | 0 (2) | < 0.01 |
| Total body pain, median* | 47 (24) | 4 (9) | < 0.01 |
| Dolorimetry threshold pressureb | |||
| Lateral epicondyle†, median* | 1.7 (1.45) | 3.6 (1.7) | < 0.01 |
| Dorsum right forearm, median* | 2.2 (1.9) | 4.3 (2.8) | < 0.01 |
| Left thumbnail, median* | 1.5 (1.1) | 2.5 (2.1) | < 0.01 |
| Greater trochanter†, median* | 3.1 (2.25) | 5.6 (3.4) | < 0.01 |
| Knee†, median* | 2.7 (1.9) | 4.6 (2.1) | < 0.01 |
Interquartile range;
Averaged over left and right sides of the body;
t-test;
Wilcoxon Rank Sum test
As shown in Table 2, scores were significantly higher in the FM group than in the control group on the Pittsburgh Sleep Quality Index (10.6 vs 4.5), Insomnia Severity Index (18.9 vs 12.1), and Epworth Sleepiness Scale (9.4 vs 5.7), indicating considerable sleep disruption in the FM group (all p < 0.01). Self-reported pain measures in all locations were significantly higher (p < 0.01) in FM patients than controls. Participants with FM reached their pain thresholds at significantly lower dolorimetry pressures than their pain- and fatigue-free counterparts on all 3 arm locations and both leg locations (p < 0.01).
Table 3 demonstrates that sleep outcomes in FM patients by RLS status also showed differences. FM cases with RLS scored higher than those without RLS on the Pittsburgh Sleep Quality Index (11.8 vs. 9.9; p = 0.01). The FM group with comorbid RLS also tended to have higher scores on the other 2 subjective sleep measures. Subjective and objective measures of pain did not differ between FM cases with and without RLS.
Table 3.
Sleep and pain measures in the FM group by RLS status
| Measure | FM + RLS (n = 58) | FM - RLS (n = 114) | p-value |
|---|---|---|---|
| Sleep measuresa | |||
| Pittsburgh Sleep Quality Index, mean (SD) | 11.8 (4.1) | 9.9 (3.2) | 0.01 |
| Insomnia Severity Index, mean (SD) | 20.1 (5.8) | 18.2 (6.1) | 0.07 |
| Epworth Sleepiness Scale, mean (SD) | 10.3 (5.0) | 8.9 (4.6) | 0.08 |
| Self-rated pain measures b | |||
| Distal arm pain, median* | 6 (8) | 6 (6) | 0.45 |
| Distal leg pain, median* | 8 (7) | 8 (5) | 0.87 |
| Total body pain, median* | 47 (20) | 46 (26) | 0.68 |
| Dolorimetry threshold pressureb | |||
| Lateral epicondyle†, median* | 1.9 (1.5) | 1.6 (1.4) | 0.07 |
| Dorsum right forearm, median* | 2.4 (2.2) | 2.2 (1.8) | 0.17 |
| Left thumbnail, median* | 1.5 (1.1) | 1.5 (1.1) | 0.52 |
| Greater trochanter†, median* | 3.3 (2.0) | 3.0 (2.4) | 0.42 |
| Knee†, median* | 2.8 (2.1) | 2.5 (1.9) | 0.45 |
Interquartile range;
Averaged over left and right sides of the body;
t-test;
Wilcoxon Rank Sum test
DISCUSSION
This study demonstrates FM is strongly associated with RLS. RLS was about 10 times more prevalent in the FM group than among the control group; furthermore, the odds of RLS in the FM group were over 11. We identified RLS in a third of our FM sample, consistent with other studies estimating prevalences of 20% to 65.7%.6–8,10–12 Our estimate is also consistent with other established secondary causes of RLS including peripheral neuropathy (5.2% to 54%),20–23 uremia (14% to 40%),24–26 and pregnancy (10% to 26%).27–29 The age- and sex-adjusted RLS prevalence in our control group was 3.1%, which is similar to the range of 2% to 15% observed in the general population.30–33 Our estimate was at the lower end of this range, potentially explained by the youthfulness and general health of our control group. The strict nature of our RLS definition may also have reduced RLS ascertainment in our study.
As shown previously,6,7,10 we demonstrated that FM patients have higher insomnia and daytime sleepiness ratings than controls. Importantly, in the FM sample, those with RLS scored higher on the Pittsburgh Sleep Quality Index, indicating greater sleep impairment as a function of RLS status. Therefore, at least a portion of the disturbed sleep commonly observed in FM is attributable to RLS. Because RLS is a treatable cause of sleep disruption and insomnia, it is prudent to routinely evaluate patients with FM for RLS.
The overlap between RLS ad FM is logical for several reasons. Both patient groups have sensory abnormalities, which at times may be confused by patients and/or clinicians as representing either RLS or FM. The use of antidepressants to treat FM may predispose to the development of RLS and a similar pathophysiology of the dopamine system has been proposed for both disorders.10 Lastly, severity assessments and quality of life have both been shown to improve with exercise in patients with RLS and FM.34–36
This study has several limitations. First, RLS was defined by a self-administered questionnaire and not by personal interview. Also, we did not examine or control for the concomitant use of medications in either group. Many medications may induce RLS, including antidepressants, which may be prescribed to treat pain and depression in FM. It is possible that some cases of RLS in our FM sample may have been due to medication side effects. In addition, there was no information regarding underlying medical illnesses or other sleep disorders for either group. Our control group was simply known to be pain- and fatigue-free. The absence of fatigue in our control group may have biased the controls to a healthier sleeping group. However, we feel that this group was representative of a normal population since the prevalence of RLS found in the controls and the mean ESS score was consistent with normative values.37
Strengths of this study include the control group, adjustment for confounding variables, and use of a validated instrument for diagnosing RLS. The latter is key, as many previous efforts have not used rigorous criteria to define RLS.6–8,10,12 In addition, we collected subjective and objective pain assessments in both cases and controls. This allowed us to assess if tender point pain experienced in FM can describe the paresthesias commonly experienced in RLS.
Our study was cross-sectional; therefore inference regarding FM as a cause of RLS is not possible. Demonstration of causality requires substantial scientific evidence. The physiology of FM as described in animal models and humans would need to overlap with RLS physiology. Prospective cohort studies of FM patients demonstrating development of RLS over time and resolution of RLS with treatment of FM symptoms would also be required for causality. Indeed, our data could be used to rationalize the reverse scenario; that RLS causes FM. Severe RLS may induce sleep deprivation, which could lead to an increase in markers of inflammation and reduction in pain thresholds possibly precipitating FM.38 Further research is required to investigate causal pathways in the association between FM and RLS.
In conclusion, we found a higher prevalence and odds of RLS in FM patients than controls. Compared to those without RLS, sleep was more disturbed in the FM sample with comorbid RLS. These findings indicate a substantial portion of sleep disturbance in FM may be RLS-related and amenable to treatment with medications such as dopamine agonists. Clinicians should routinely query FM patients regarding RLS symptoms as treatment may improve sleep39 and quality of life40 in this challenging disorder. Future studies to investigate whether improvement in FM symptoms reduces RLS symptoms may be useful to further determine if FM is in fact a secondary cause of RLS.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01 AR47678-01A1) to Dr. Buchwald. Additional funding was received from the National Fibromyalgia Research Association.
REFERENCES
- 1.American Academy of Sleep Medicine. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. The international classification of sleep disorders: diagnostic and coding manual. [Google Scholar]
- 2.Kryger MH, Roth T, Dement WC. 4th ed. Philadelphia, PA: Elsevier/Saunders; 2005. Principles and practice of sleep medicine. [Google Scholar]
- 3.Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 Criteria for the classification of fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33:160–72. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 4.Firestein GS, Kelley WN. 8th ed. Philadelphia, PA: Saunders/Elsevier; 2009. Kelley's textbook of rheumatology. [Google Scholar]
- 5.Drewes AM. Pain and sleep disturbances with special reference to fibromyalgia and rheumatoid arthritis. Rheumatology (Oxford) 1999;38:1035–8. doi: 10.1093/rheumatology/38.11.1035. [DOI] [PubMed] [Google Scholar]
- 6.Delgado J, Murali G, Goldberg R. Sleep disorders in fibromyalgia. Sleep. 2004;27:A339. [Google Scholar]
- 7.Khan S, Goldberg R, Haber A. Sleep disorders in fibromyalgia. Sleep. 2005;28:A290. [Google Scholar]
- 8.Shaver JL, Wilbur J, Robinson FP, Wang E, Buntin MS. Women's health issues with fibromyalgia syndrome. J Womens Health (Larchmt) 2006;15:1035–45. doi: 10.1089/jwh.2006.15.1035. [DOI] [PubMed] [Google Scholar]
- 9.Tayag-Kier CE, Keenan GF, Scalzi LV, et al. Sleep and periodic limb movement in sleep in juvenile fibromyalgia. Pediatrics. 2000;106:E70. doi: 10.1542/peds.106.5.e70. [DOI] [PubMed] [Google Scholar]
- 10.Stehlik R, Arvidsson L, Ulfberg J. Restless legs syndrome is common among female patients with fibromyalgia. Eur Neurol. 2009;61:107–11. doi: 10.1159/000180313. [DOI] [PubMed] [Google Scholar]
- 11.Yunus MB, Aldag JC. Restless legs syndrome and leg cramps in fibromyalgia syndrome: a controlled study. BMJ. 1996;312:1339. doi: 10.1136/bmj.312.7042.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zoppi M, Maresca M. Symptoms accompanying fibromyalgia. Reumatismo. 2008;60:217–20. doi: 10.4081/reumatismo.2008.217. [DOI] [PubMed] [Google Scholar]
- 13.Watson NF, Buchwald D, Goldberg J, Noonan C, Ellenbogen RG. Neurological signs and symptoms in fibromyalgia. Arthritis Rheum. 2009;60:2839–44. doi: 10.1002/art.24772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.White KP, Harth M, Speechley M, Ostbye T. Testing an instrument to screen for fibromyalgia syndrome in general population studies: the London Fibromyalgia Epidemiology Study Screening Questionnaire. J Rheumatol. 1999;26:880–4. [PubMed] [Google Scholar]
- 15.Hening WA, Allen RP, Thanner S, et al. The Johns Hopkins telephone diagnostic interview for the restless legs syndrome: preliminary investigation for validation in a multi-center patient and control population. Sleep Med. 2003;4:137–41. doi: 10.1016/s1389-9457(03)00006-6. [DOI] [PubMed] [Google Scholar]
- 16.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–40. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 17.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 18.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 19.Fischer AA. Pressure algometry over normal muscles Standard values, validity and reproducibility of pressure threshold. Pain. 1987;30:115–26. doi: 10.1016/0304-3959(87)90089-3. [DOI] [PubMed] [Google Scholar]
- 20.Gemignani F, Brindani F, Negrotti A, Vitetta F, Alfieri S, Marbini A. Restless legs syndrome and polyneuropathy. Mov Disord. 2006;21:1254–7. doi: 10.1002/mds.20928. [DOI] [PubMed] [Google Scholar]
- 21.Hattan E, Chalk C, Postuma RB. Is there a higher risk of restless legs syndrome in peripheral neuropathy? Neurology. 2009;72:955–60. doi: 10.1212/01.wnl.0000336341.72621.db. [DOI] [PubMed] [Google Scholar]
- 22.Nineb A, Rosso C, Dumurgier J, Nordine T, Lefaucheur JP, Creange A. Restless legs syndrome is frequently overlooked in patients being evaluated for polyneuropathies. Eur J Neurol. 2007;14:788–92. doi: 10.1111/j.1468-1331.2007.01856.x. [DOI] [PubMed] [Google Scholar]
- 23.Rutkove SB, Matheson JK, Logigian EL. Restless legs syndrome in patients with polyneuropathy. Muscle Nerve. 1996;19:670–2. doi: 10.1002/(SICI)1097-4598(199605)19:5<670::AID-MUS20>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 24.Callaghan N. Restless legs syndrome in uremic neuropathy. Neurology. 1966;16:359–61. doi: 10.1212/wnl.16.4.359. [DOI] [PubMed] [Google Scholar]
- 25.Merlino G, Piani A, Dolso P, et al. Sleep disorders in patients with end-stage renal disease undergoing dialysis therapy. Nephrol Dial Transplant. 2006;21:184–90. doi: 10.1093/ndt/gfi144. [DOI] [PubMed] [Google Scholar]
- 26.Mucsi I, Molnar MZ, Rethelyi J, et al. Sleep disorders and illness intrusiveness in patients on chronic dialysis. Nephrol Dial Transplant. 2004;19:1815–22. doi: 10.1093/ndt/gfh130. [DOI] [PubMed] [Google Scholar]
- 27.Ekbom KA. Restless legs syndrome. Neurology. 1960;10:868–73. doi: 10.1212/wnl.10.9.868. [DOI] [PubMed] [Google Scholar]
- 28.Goodman JD, Brodie C, Ayida GA. Restless leg syndrome in pregnancy. BMJ. 1988;297:1101–2. doi: 10.1136/bmj.297.6656.1101-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Manconi M, Govoni V, De Vito A, et al. Restless legs syndrome and pregnancy. Neurology. 2004;63:1065–9. doi: 10.1212/01.wnl.0000138427.83574.a6. [DOI] [PubMed] [Google Scholar]
- 30.Bjorvatn B, Leissner L, Ulfberg J, et al. Prevalence, severity and risk factors of restless legs syndrome in the general adult population in two Scandinavian countries. Sleep Med. 2005;6:307–12. doi: 10.1016/j.sleep.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 31.Ohayon MM, Roth T. Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. J Psychosom Res. 2002;53:547–54. doi: 10.1016/s0022-3999(02)00443-9. [DOI] [PubMed] [Google Scholar]
- 32.Tison F, Crochard A, Leger D, Bouee S, Lainey E, El Hasnaoui A. Epidemiology of restless legs syndrome in French adults: a nationwide survey: the INSTANT Study. Neurology. 2005;65:239–46. doi: 10.1212/01.wnl.0000168910.48309.4a. [DOI] [PubMed] [Google Scholar]
- 33.Ulfberg J, Nystrom B, Carter N, Edling C. Restless Legs Syndrome among working-aged women. Eur Neurol. 2001;46:17–9. doi: 10.1159/000050750. [DOI] [PubMed] [Google Scholar]
- 34.Aukerman MM, Aukerman D, Bayard M, Tudiver F, Thorp L, Bailey B. Exercise and restless legs syndrome: a randomized controlled trial. J Am Board Fam Med. 2006;19:487–93. doi: 10.3122/jabfm.19.5.487. [DOI] [PubMed] [Google Scholar]
- 35.Jones KD, Adams D, Winters-Stone K, Burckhardt CS. A comprehensive review of 46 exercise treatment studies in fibromyalgia (1988-2005) Health Qual Life Outcomes. 2006;4:67. doi: 10.1186/1477-7525-4-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lakasing E. Exercise beneficial for restless legs syndrome. Practitioner. 2008;252:43–5. [PubMed] [Google Scholar]
- 37.Johns M, Hocking B. Daytime sleepiness and sleep habits of Australian workers. Sleep. 1997;20:844–9. doi: 10.1093/sleep/20.10.844. [DOI] [PubMed] [Google Scholar]
- 38.Lautenbacher S, Kundermann B, Krieg JC. Sleep deprivation and pain perception. Sleep Med Rev. 2006;10:357–69. doi: 10.1016/j.smrv.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 39.Trenkwalder C, Hening WA, Montagna P, et al. Treatment of restless legs syndrome: an evidence-based review and implications for clinical practice. Mov Disord. 2008;23:2267–302. doi: 10.1002/mds.22254. [DOI] [PubMed] [Google Scholar]
- 40.Reinhold T, Muller-Riemenschneider F, Willich SN, Bruggenjurgen B. Economic and human costs of restless legs syndrome. Pharmacoeconomics. 2009;27:267–79. doi: 10.2165/00019053-200927040-00001. [DOI] [PubMed] [Google Scholar]