Abstract
Study Objectives:
Describe the self-reported sleep quality and sleep hygiene behaviors of adolescents before diagnosis and during chemotherapy (CTX), compare their sleep quality and sleep hygiene behaviors with published normative data for healthy adolescents and adolescents with chronic pain, and explore factors that predict sleep quality.
Methods:
Subjects were 51 adolescents (10 to 19 years) receiving CTX for cancer. A questionnaire was used to assess sleep patterns prior to the adolescent's cancer diagnosis, and a 7-day sleep diary was used to assess subjective sleep-wake activity during CTX. Sleep quality was assessed using the Adolescent Sleep Wake Scale, and sleep-facilitating and sleep-inhibiting behaviors using the Adolescent Sleep Hygiene Scale.
Results:
Adolescents receiving CTX reported significantly worse sleep quality and sleep hygiene behaviors than healthy adolescents, and better sleep quality but similar sleep hygiene behaviors to adolescents with chronic pain. Significant interactions were found between bedtimes and wake-times on weekdays and weekends before diagnosis and during CTX. Sleep hygiene and demographic variables accounted for 24% of the variance in sleep quality. The cognitive and emotional subscales of the sleep hygiene scale and demographic variables accounted for 36% of the variance in sleep quality.
Conclusions:
Both the weekday and weekend sleep-wake patterns of adolescents receiving CTX resembled their weekend sleep patterns prior to diagnosis.
Citation:
Walker AJ; Johnson KP; Miaskowski C; Lee KA; Gedaly-Duff V. Sleep quality and sleep hygiene behaviors of adolescents during chemotherapy. J Clin Sleep Med 2010;6(5):439-444.
Keywords: Adolescent, cancer, sleep quality, sleep hygiene
Adolescent sleep-wake patterns result from complex interactions among four distinct processes: maturation and development, behavior, and intrinsic sleep and circadian regulatory mechanisms. Several developmental trends are evident in the sleep-wake patterns of healthy adolescents.1 First, as children progress from early to late adolescence they go to bed later. In addition, they tend to awaken later on weekends and during vacation periods. These patterns result in shortened week-day sleep durations and increased discrepancies between weekday and weekend sleep patterns. These changes in sleep-wake patterns exist within the context of an educational system that requires adolescents to start school earlier in the morning than younger children. Developmental changes in sleep patterns, coupled with earlier school start times, are associated with insufficient sleep for many adolescents.2 Adolescence proceeds through three distinct periods: early (10 to 13 years), middle (14 to 16 years), and late (17 to 19 years).3 For the purposes of this study, adolescents were defined as persons 10 to 19 years to broadly reflect the biological and psychosocial period of adolescence.
Good sleep quality can be defined as a period of restorative sleep that meets an individual's sleep-related needs and allows for optimal daily functioning.4 An adolescent with good sleep quality goes to bed easily at bedtime, transitions effortlessly from wakefulness to sleep, maintains sleep without disruptions, reinitiates sleep if aroused, and transitions easily in the morning from sleep to wakefulness.5 Sleep quality is influenced by intrinsic sleep and circadian regulatory mechanisms, as well as demographic (e.g., age, race, gender) and lifestyle factors (e.g., sleep hygiene behaviors, physical activity).
BRIEF SUMMARY
Current Knowledge/Study Rationale: Sleep is important for adolescents who are experiencing a life-threatening illness and a period of brain maturation that require adequate sleep. Self-reported sleep quality and sleep hygiene behaviors during cancer chemotherapy are likely related but have not been described.
Study Impact: The findings of this study suggest that adolescents have poor sleep quality and sleep hygiene behaviors during chemotherapy. The cognitive and emotional aspects of sleep hygiene behaviors may be particularly relevant for adolescents with cancer and warrant further study.
Sleep hygiene behaviors are lifestyle factors assumed to influence sleep quality by promoting or inhibiting better sleep. Positive sleep-promoting behaviors include following a bedtime routine; sleeping alone; sleeping in a comfortable, quiet, toxin-free environment; maintaining a regular sleep and exercise schedule,6 and decreasing the number of negative sleep-inhibiting behaviors (taking late-afternoon naps; consumption of tobacco, alcohol, and caffeine prior to bedtime; engaging in physiologically, cognitively, and emotionally stimulating activities within an hour of bedtime).5 Adolescents frequently engage in negative sleep hygiene behaviors, including keeping different sleep schedules on weekdays and weekends and engaging in stimulating activities prior to bed that result in disrupted sleep-wake patterns.7
In addition to changes in sleep-wake patterns and sleep hygiene behaviors associated with development, adolescents with cancer are subject to disease-related (e.g., symptoms, physical activity, rest) and treatment-related (e.g., CTX) insults to their sleep quality.8 While research about these factors has focused on adults with cancer, these factors may be relevant for children and adolescents with cancer. To date, no studies have described the sleep quality and sleep hygiene behaviors, or the influences of demographic, disease, treatment, and lifestyle factors on the sleep quality of adolescents receiving cancer CTX.
Sleep is important for these adolescents who are experiencing a life-threatening illness during normal brain maturation that requires adequate sleep. Increasing evidence suggests that natural killer cell activity is reduced with sleep deprivation and raises the possibility that sleep is important for immune defenses against tumor cells.9,10 In addition, sleep may sustain the activity of certain immune cells that are important in fighting cancer.11 Given the paucity of research and the importance of sleep for adolescents with cancer, the purposes of this study were to describe the self-reported sleep quality and sleep hygiene behaviors of adolescents before diagnosis and during CTX, and to compare their sleep quality and sleep hygiene behaviors with published data for healthy adolescents and adolescents with chronic pain. In addition, factors that predicted sleep quality were explored. It was hypothesized that adolescents with cancer would report worse sleep quality and sleep hygiene behaviors than healthy adolescents.
METHODS
This analysis is part of a larger descriptive, longitudinal study that explored nocturnal sleep, symptoms, and quality of life in adolescents with cancer. Fifty-one adolescents (10 to 19 years) receiving CTX were recruited from 2 regional children's cancer centers in the Pacific Northwest. The study was approved by the institutional review boards at both centers. Adolescents were recruited irrespective of type of cancer, phase of treatment, or whether the cancer was primary, secondary, or in relapse. Adolescents needed to read, speak, and understand English, and were excluded if they had a diagnosis of mental illness prior to cancer or cognitive impairment (e.g., developmental delay) that precluded participation. Decisions to exclude an adolescent were made by the investigator, in conjunction with chart reviews and informal discussions with physicians, parents, and adolescents. For adolescents 10 to 17 years of age, assent and written consent from a parent or legal guardian were obtained. Written consent was obtained from 18 and 19-year-old adolescents.
Data from 2 published samples of adolescents were used for comparative purposes.12 One sample of adolescents was healthy (n = 20), and the other sample had chronic pain (n = 20). The healthy sample was recruited by posted advertisements about a study exploring adolescent sleep and the pain sample was recruited from a multidisciplinary pediatric chronic pain clinic. Both samples were recruited from a metropolitan area in the Pacific Northwest.
Measures
Sleep Routines “Before You Were Sick” Questionnaire (BYWS) is a brief investigator-developed questionnaire that was used to assess baseline sleep patterns (i.e., weekday and weekend bedtimes and wake-times). The “before you were sick” period is a retrospective report of the time before they experienced symptoms related to their cancer diagnosis. Although the length of recall reflected the time since diagnosis, adolescents seemed to be able to readily recall bedtimes and wake-times on weekdays and weekends because they were in school. These data provided a comparison for self-reported sleep-wake patterns during CTX.
Sleep Week Diary is an investigator-developed, one-page, 7-day sleep diary that was used to assess subjective sleep-wake activity during CTX. Questions included bedtimes and wake-times. Content validity of the diary was supported by a review of the literature and an examination of other sleep diaries.4,13,14
Adolescent Sleep Wake Scale (Sleep Quality) is a 28-item instrument that assesses sleep quality in adolescents 12 to 18 years of age for 5 behavioral dimensions: (1) going to bed, (2) falling asleep, (3) maintaining sleep, (4) reinitiating sleep, and (5) returning to wakefulness (i.e., final awakening).5 Respondents indicate how often these sleep behaviors occurred on a 6-point Likert scale (never, once in awhile, sometimes, quite often, frequently if not always, always). For this study, the reference time was modified from past month to last week. Mean scores were calculated so that total and subscale scores ranged from 1 to 6, with higher scores indicating better sleep quality. Reliability estimates of internal consistency are reported for the full scale (Cronbach α = 0.80 to 0.86) and subscales (Cronbach α = 0.60 to 0.82).5,15 In this study, the Cronbach α for the total score was 0.83 and ranged from 0.66 to 0.78 for the 5 subscales.
Adolescent Sleep Hygiene Scale (Sleep Hygiene) is a 28-item instrument that assesses sleep-facilitating and sleep-inhibiting behaviors in adolescents 12 to 18 years of age in 6 conceptual domains: (1) physiological, (2) cognitive, (3) emotional, (4) sleep environment, (5) substances, and (6) sleep stability.16 In this study, the reference time was modified from past month to last week. Mean scores were calculated so that total and subscale scores ranged from 1 to 6, with higher scores indicating better sleep hygiene behaviors. Internal consistency coefficients were reported for the full scale (Cronbach α = 0.80) and subscales (Cronbach α = 0.46 to 0.74). In this study, the Cronbach α for the total score was 0.73 and ranged from 0.34 to 0.84 for the subscales. The sleep quality and sleep hygiene scales were developed for use with healthy adolescents. However, in this study they were used to evaluate for differences in sleep quality and sleep hygiene among published data from healthy adolescents and adolescents with chronic pain, and this sample of adolescents with cancer.
Study Procedures
Eligible adolescents were identified by a physician, staff nurse, nurse practitioner, or medical assistant. After screening for eligibility and obtaining consent, medical records were reviewed to confirm diagnosis, age, ethnicity, date of diagnosis, and treatment protocol. The BYWS, sleep quality, and sleep hygiene scales were completed on day one of data collection, when intravenous CTX was administered. The sleep diaries were completed on days 1 to 7 of data collection. Adolescents received a cash incentive when they completed data collection.
Data Analysis
Data were analyzed using SPSS 15.0. Descriptive statistics were used to describe the demographic and clinical characteristics of the sample, bedtimes and wake-times on weekdays and weekends before diagnosis and during CTX, and total and subscale scores for sleep quality and sleep hygiene. Self-reported bedtimes and wake-times from the diary were used to make comparisons with the retrospective self-reports of sleep patterns prior to diagnosis.
Repeated measures analyses of variance (ANOVA) with 2 within-subjects factors (weekday versus weekend and before diagnosis versus during CTX) were performed to compare differences between bedtimes and wake-times on weekdays and weekends before diagnosis and during CTX. One-sample t-tests were used to evaluate for differences in sleep quality and sleep hygiene scores between the adolescents during CTX and published normative data from healthy adolescents and adolescents with chronic pain.12 A p-value < 0.05 was considered statistically significant.
Two multiple regression analyses were performed to determine predictors of sleep quality using the sleep quality total score. In both regression analyses, age, gender, and race (i.e., white, not white) were entered as control variables because these variables have been shown to affect sleep in previous studies.17–20 In the first regression analysis, the impact of sleep hygiene (total score) on sleep quality (total score) was evaluated. In the second analysis, the impact of sleep hygiene (cognitive and emotional subscales) on sleep quality was evaluated. Because of the small sample size, the predictors were limited to those that showed significance in a prior study.5
RESULTS
Sample Characteristics
The majority of the adolescents were male (57%) and Caucasian (75%) with a mean age of 14.2 years (SD = 2.7; range 10 to 18 years) (see Table 1). The most common cancers were acute lymphocytic leukemia (ALL), lymphoma, bone tumors, and brain tumors. Other diagnoses included testicular rhabdomyosarcoma, alveolar rhabdomyosarcoma, ovarian teratoma, germ cell tumor, synovial sarcoma, and renal neuroblastoma. The mean time since diagnosis was 6.3 months (SD = 7.8; range 0 to 37 months). Treatment was for a primary cancer in 47 (92%) of the adolescents, for a relapse in 3 (6%), and for a secondary cancer in 1 (2%) adolescent.
Table 1.
Demographic and clinical characteristics of adolescents (n = 51)a
| Variable | Number | % |
|---|---|---|
| Gender | ||
| Female | 22 | 43 |
| Male | 29 | 57 |
| Race or ethnicity | ||
| Caucasian | 38 | 75 |
| Hispanic | 7 | 14 |
| More than one race | 5 | 10 |
| African American | 1 | 1 |
| Age (years) | ||
| Mean = 14.2 years, SD = 2.7 | ||
| 10-13 years | 21 | 41 |
| 14-16 years | 16 | 31 |
| 17-19 years | 14 | 28 |
| Diagnosis | ||
| Leukemia | ||
| Acute lymphocytic | 21 | 41 |
| Acute myelogenous | 2 | 4 |
| Lymphoma | ||
| Hodgkin | 4 | 8 |
| Non-Hodgkin | 4 | 8 |
| Bone tumors (osteogenic or Ewing) | 8 | 15 |
| Brain tumors | 6 | 12 |
| Other | 6 | 12 |
| Time since diagnosis (months) | ||
| Mean = 6.3, SD = 7.8, Range = 0 - 37 |
Includes 2 adolescents who started but did not complete the study.
The published healthy adolescent (n = 20) and chronic pain (n = 20) samples had mean ages of 14.6 years (SD = 2.0; range 12 to 17) and 15 years (SD = 1.4; range 12 to 17), and were 85% and 95% Caucasian, respectively. Among the adolescents with chronic pain, primary diagnoses were chronic headaches (40%), functional abdominal pain (10%), myofascial pain (40%), and complex regional pain syndrome (10%).12
Sleep Quality
Although this study was not powered to detect differences in sleep quality based on race or gender, exploratory analyses revealed no significant differences in sleep quality by race or gender for these adolescents with cancer. As shown in Table 2, adolescents receiving CTX (M = 4.2; SD = 0.6) reported significantly worse sleep quality based on sleep quality total scores than healthy adolescents (M = 4.4; SD = 0.6). Adolescents receiving CTX reported more problems with going to bed, falling asleep, maintaining sleep, and reinitiating sleep than healthy adolescents. No difference was found between the 2 groups on returning to wakefulness (i.e., final awakening).
Table 2.
Total and subscale scores for the Adolescent Sleep Wake Scale (ASWS) and Adolescent Sleep Hygiene Scale (ASHS) for adolescents receiving CTX compared to healthy adolescentsa
| Scale | Adolescents CTX N = 46 | Healthy Adolescents N = 20 | One-Sample t-test |
|---|---|---|---|
| Sleep Quality | Mean ± SD | Mean ± SD | |
| Going to bed subscale | 4.2 ± 1.0 | 3.9 ± 1.2 | 2.10* |
| Falling asleep subscale | 4.2 ± 0.8 | 4.5 ± 0.7 | 2.78** |
| Maintaining sleep subscale | 4.3 ± 0.9 | 4.7 ± 0.8 | 2.94** |
| Reinitiating sleep subscale | 4.8 ± 0.7 | 5.2 ± 0.5 | 3.54** |
| Return to wakefulness subscale | 3.4 ± 0.9 | 3.4 ± 1.2 | 0.01 |
| ASWS Total Score | 4.2 ± 0.6 | 4.4 ± 0.6 | 2.71** |
| Sleep Hygiene | |||
| Physiological subscale | 4.7 ± 0.7 | 4.9 ± 0.8 | 1.75 |
| Cognitive subscale | 3.9 ± 0.8 | 4.4 ± 0.6 | 4.07*** |
| Emotional subscale | 4.7 ± 1.1 | 4.8 ± 1.1 | 0.70 |
| Sleep environment subscale | 5.0 ± 0.9 | 5.5 ± 0.6 | 4.07*** |
| Substances subscale | 5.9 ± 0.5 | 6.0 ± 0.1 | 1.71 |
| Sleep stability subscale | 3.7 ± 1.1 | 4.3 ± 0.7 | 3.80*** |
| ASHS Total Score | 4.7 ± 0.5 | 5.0 ± 0.4 | 4.84*** |
Sample from Palmero, 2007;
p ≤ 0.05;
p ≤ 0.01;
p ≤ 0.001
As shown in Table 3, adolescents receiving CTX (M = 4.2, SD = 0.6) reported better sleep quality based on the sleep quality total score than adolescents with chronic pain (M = 3.5, SD = 0.7). Adolescents with chronic pain had more problems with going to bed, falling asleep, maintaining sleep, reinitiating sleep, and returning to wakefulness than adolescents receiving CTX.
Table 3.
Total and subscale scores for the Adolescent Sleep Wake Scale (ASWS) and Adolescent Sleep Hygiene Scale (ASHS) for adolescents receiving CTX compared to adolescents with chronic paina
| Scale | Adolescents CTX N = 46 | Adolescents with Chronic Pain N = 20 | One-Sample t-test |
|---|---|---|---|
| Sleep Quality | Mean ± SD | Mean ± SD | |
| Going to bed subscale | 4.2 ± 1.0 | 3.4 ± 0.9 | 5.44*** |
| Falling asleep subscale | 4.2 ± 0.8 | 3.3 ± 1.0 | 7.07*** |
| Maintaining sleep subscale | 4.3 ± 0.9 | 3.5 ± 1.0 | 5.71*** |
| Reinitiating sleep subscale | 4.8 ± 0.7 | 4.5 ± 0.7 | 3.23** |
| Return to wakefulness subscale | 3.4 ± 0.9 | 2.5 ± 1.0 | 6.50*** |
| ASWS Total Score | 4.2 ± 0.6 | 3.5 ± 0.7 | 8.24*** |
| Sleep Hygiene | |||
| Physiological subscale | 4.7 ± 0.7 | 4.6 ± 0.8 | 1.03 |
| Cognitive subscale | 3.9 ± 0.8 | 3.9 ± 0.9 | 0.33 |
| Emotional subscale | 4.7 ± 1.1 | 4.4 ± 1.1 | 1.90 |
| Sleep environment subscale | 5.0 ± 0.9 | 5.1 ± 0.7 | 0.95 |
| Substances subscale | 5.9 ± 0.5 | 6.0 ± 0.0 | 1.71 |
| Sleep stability subscale | 3.7 ± 1.1 | 3.8 ± 1.2 | 0.70 |
| ASHS Total Score | 4.7 ± 0.5 | 4.6 ± 0.6 | 0.83 |
Sample from Palmero, 2007;
p ≤ 0.01;
p ≤ 0.001
Sleep Hygiene
Although this study was not powered to detect differences in sleep hygiene based on race or gender, exploratory analyses revealed no significant differences in sleep hygiene by race or gender for these adolescents with cancer. As shown in Table 2, the adolescents receiving CTX (M = 4.7, SD = 0.5) reported significantly lower total sleep hygiene scores (i.e., worse sleep hygiene behaviors) than healthy adolescents (M = 5.0, SD = 0.4). In addition, adolescents receiving CTX reported worse sleep hygiene behaviors on the cognitive, sleep environment, and sleep stability subscales than healthy adolescents. As shown in Table 3, no significant differences in total sleep hygiene or any of the subscales (physiological, cognitive, emotional, sleep environment, substances, or sleep stability) scores were found between the adolescents receiving CTX and adolescents with chronic pain.
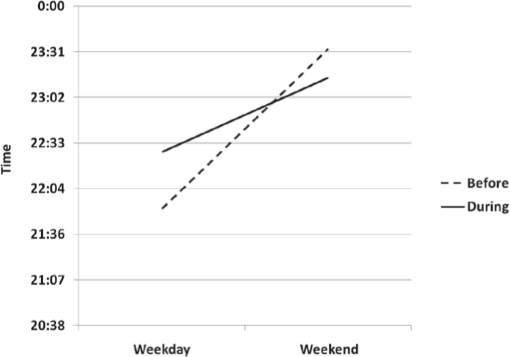
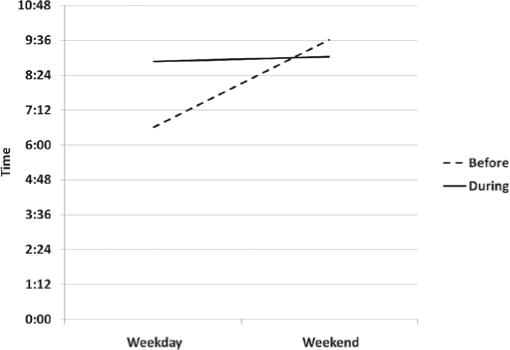
Mean bedtimes and wake-times for adolescents prior to and during CTX are summarized in Table 4. The effect for weekend versus weekday (F1,38 = 70.09, p < 0.001) was significant, but the effect for before versus during CTX (F1,38 = 1.09), p = 0.30) was not significant. For bedtimes, a significant interaction was found between bedtimes on weekdays and weekends before diagnosis and during CTX (F1,38 = 9.54; p < 0.01). As illustrated in Figure 1, a larger discrepancy between bedtimes on weekdays and weekends occurred before diagnosis than during CTX. For wake-times, a significant interaction was found between wake-times on weekdays and weekends before diagnosis and during CTX (F1,38 = 93.54; p < 0.01). As illustrated in Figure 2, a larger discrepancy occurred between wake-times on weekdays and weekends before diagnosis than during CTX.
Table 4.
Descriptive statistics for bedtimes and wake-times before diagnosis and during CTX
| Variable | N | Mean | SD | Range |
|---|---|---|---|---|
| Bedtime weekdays | ||||
| Before diagnosis | 43 | 21:52 | 1:08 | 20:00–02:30 |
| During CTX | 43 | 22:28 | 1:26 | 20:30–02:00 |
| Bedtime weekends | ||||
| Before diagnosis | 44 | 23:33 | 1:34 | 21:30–05:00 |
| During CTX | 43 | 23:15 | 1:11 | 00:30–02:00 |
| Wake-time weekdays | ||||
| Before diagnosis | 43 | 06:36 | 0:34 | 05:30–08:00 |
| During CTX | 43 | 08:52 | 1:16 | 06:30–11:26 |
| Wake time weekends | ||||
| Before diagnosis | 44 | 09:37 | 1:33 | 07:00–1400 |
| During CTX | 43 | 09:02 | 1:36 | 04:30–12:15 |
Figure 1.
Bedtimes on weekdays and weekends before and during chemotherapy
Values are plotted as means.
Figure 2.
Wake-times on weekdays and weekends before and during chemotherapy
Values are plotted as means.
Correlations between Sleep Quality and Sleep Hygiene
As shown in Table 5, sleep quality total score was correlated with sleep hygiene (total and subscales). Demographic variables (age, gender, race) and sleep hygiene (total) accounted for 30% of the variance in sleep quality (r2 = 0.305; p = 0.004), whereas demographic variables and sleep hygiene (cognitive and emotional subscales) accounted for 36% of the variance in sleep quality (r2 = 0.359; p = 0.002). The cognitive and emotional subscale uniquely explained 14% and 6% of the variance in sleep quality, respectively.
Table 5.
Multiple regressions for effects of control variables, sleep hygiene (ASHS) total scores and sleep hygiene (ASHS) cognitive and emotional subscale scores on sleep quality (ASWS) total scores for adolescents with cancer
| Variable | Sleep Quality (ASWS Total) |
|||
|---|---|---|---|---|
| R2 | F(p) | ß | (sp2) | |
| Age | 0.013 | 0.003 | ||
| Gender | 0.266 | 0.054 | ||
| Race | −0.192 | 0.019 | ||
| ASHS Total | 0.305 | 4.498 (p = 0.004 ) | ||
| Model 2 | ||||
| Age | 0.047 | 0.029 | ||
| Gender | 0.217 | 0.036 | ||
| Race | −0.239 | 0.029 | ||
| ASHS Cognitive & Emotional Subscales | 0.359 | 4.480 (p = 0.002) | ||
| Cognitive | 0.346 | 0.140 | ||
| Emotional | 0.146 | 0.063 | ||
sp2 (semi-partial correlation) refers to the unique contribution of a variable to the explained variance
DISCUSSION
Both the weekday and weekend sleep-wake patterns of adolescents receiving CTX resembled their weekend sleep patterns prior to diagnosis. Adolescents receiving CTX had worse sleep quality than healthy adolescents and better sleep quality than adolescents with chronic pain. For sleep hygiene behaviors, healthy adolescents had better sleep hygiene behaviors than adolescents receiving CTX and similar sleep hygiene behaviors to adolescents with chronic pain. These findings suggest that these instruments are sensitive enough to detect differences in sleep quality and sleep hygiene behaviors in adolescents who are healthy compared to adolescents with acute and chronic diseases. Future studies with larger sample sizes are needed to confirm these findings.
Prior to their cancer diagnosis, adolescents reported a delayed timing of sleep and concomitant early wake-time on schooldays. On weekends, a delayed timing occurred for sleep and wake-times. These findings are consistent with previous findings of delayed timing of sleep in healthy adolescents.2,6 Their weekend sleep-wake pattern (i.e., later bedtimes and wake-times) prior to diagnosis persisted during CTX. The most likely explanation for this pattern is that many of these adolescents were not attending school and so weekday sleep patterns were not restricted by school start times. They went to bed later and awakened later. While this finding suggests that their sleep time was adequate when compared to the estimated sleep need for healthy adolescents, the actual sleep need of adolescents on CTX is unknown. Additional research is warranted to determine the total sleep time needed by adolescents on CTX to enhance their immune system, as well as their physical and psychological recovery. An assessment of adolescent's knowledge about sleep need, positive and negative sleep hygiene behaviors, and relationships between sleep, brain maturation, and the immune system would help drive efforts toward development of effective measures and interventions that include patient and family education materials.
Clinical experience and findings from three studies21–23 suggest that cancer and CTX has a negative impact on sleep quality and sleep hygiene behaviors. Multiple chemotherapeutic agents are used to treat adolescents with cancer, each with its own set of side-effects. For example, corticosteroids are associated with mood changes, depression, increased appetite, weight gain, and sleep disturbance. Methotrexate is associated with nausea and vomiting, mucositis, diarrhea, increased risk of sunburn, and loss of appetite; and vincristine is associated with constipation, hair loss, and numbness/tingling in hands and feet related to peripheral nerve irritation.24 These physical and psychological symptoms may contribute to sleep disturbances. In addition, the side effects of weight gain and hair loss affect body image, which is exceedingly important to adolescents, and may be sources of rumination that make it difficult for them to fall asleep at night or reinitiate sleep after nocturnal awakenings. Other aspects of cancer treatment that may contribute to sleep disturbances include symptom management medications, changes in routines for appointments, hospitalizations, surgery, and radiation therapy.25 Future research is needed to explore how these factors affect sleep quality and sleep hygiene behaviors of adolescents with cancer. Interestingly, adolescents receiving CTX had better sleep quality than adolescents with chronic pain. The reasons for the poor sleep quality of adolescents with chronic pain need to be determined in future studies. However, findings from previous studies support connections between pain, sleep, depression, and worry.12,26,27 The exact nature and direction of these relationships are not known. Differences in psychological symptoms between adolescents receiving CTX and adolescents with chronic pain may account for differences in sleep quality. Additional research is warranted that compares these groups to better understand sleep quality and guide interventions to improve sleep in both groups.The positive relationship between sleep hygiene behaviors and sleep quality is consistent with previous research with healthy adolescents5 and warrants further investigation in adolescents with cancer. Special attention should be given to cognitive and emotional aspects of sleep hygiene behaviors because the exploratory findings of this study suggest these aspects may be particularly relevant for adolescents with cancer.
Limitations
Some study limitations need to be acknowledged. The sample size was small and cross-sectional, which limits the generalizability of the study's findings. The sample was not powered to detect changes in sleep parameters between early, middle, and late adolescence. The “Before You Were Sick” questionnaire was not validated and requires additional evaluation in future studies. The comparison of sleep-wake patterns from retrospective reports of bedtimes and wake-times before treatment to current diary reports during treatment may be problematic and limit validity of the comparisons because of recall bias. The length of recall was based on the time since diagnosis, with a mean of 6.3 months and a range of 0 to 37 months. The comparisons among healthy adolescents, adolescents receiving CTX, and adolescents with chronic pain are limited by small sample sizes. The findings are also limited by lack of objective sleep data to support the subjective data. Additional studies with larger sample sizes are needed to explore predictors of sleep quality, the actual sleep needs of adolescents during cancer treatment, as well as the effectiveness of cognitive behavioral therapies to improve sleep quality.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGEMENTS
Research was conducted at Oregon Health – Science University
Funding: NINR 2 T32 NRO7061, 1 F31 NR010047-01A1, 2 T32 NR07088-13
REFERENCES
- 1.Carskadon MA, Acebo C. Regulation of sleepiness in adolescents: update, insights, and speculation. Sleep. 2002;25:606–14. doi: 10.1093/sleep/25.6.606. [DOI] [PubMed] [Google Scholar]
- 2.Carskadon M, Acebo C, Jenni OG. Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004:1021. doi: 10.1196/annals.1308.032. [DOI] [PubMed] [Google Scholar]
- 3.Marcell AV. Adolescence. In: Kliegman RM, Behrman RE, Jenson HB, Stanton BF, editors. Nelson Textbook of Pediatrics. 18th ed. Philadelphia: Saunders; 2007. [Google Scholar]
- 4.Berger AM, Parker KP, Young-McCaughan S, et al. Sleep wake disturbances in people with cancer and their caregivers: state of the science. Oncol Nurs Forum. 2005;32:E98–126. doi: 10.1188/05.ONF.E98-E126. [DOI] [PubMed] [Google Scholar]
- 5.LeBourgeois MK, Giannotti F, Cortesi F, Wolfson AR, Harsh J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics. 2005;115:257–65. doi: 10.1542/peds.2004-0815H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolfson AR. Bridging the gap between research and practice: What will adolescents' sleep-wake patterns look like in the 21st century. In: Carskadon M, editor. Adolescent sleep patterns: Biological, social, and psychological influences. Cambridge: Cambridge University Press; 2002. pp. 198–219. [Google Scholar]
- 7.Carskadon M, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21:871–81. doi: 10.1093/sleep/21.8.871. [DOI] [PubMed] [Google Scholar]
- 8.Vena C, Parker K, Cunningham M, Clark J, McMillan S. Sleep-wake disturbances in people with cancer part I: an overview of sleep, sleep regulation, and effects of disease and treatment. Oncol Nurs Forum. 2004;31:735–46. doi: 10.1188/04.ONF.735-746. [DOI] [PubMed] [Google Scholar]
- 9.Shakhar K, Valdimarsdottir HB, Guevarra JS, Bovbjerg DH. Sleep, fatigue, and NK cell activity in healthy volunteers: significant relationships revealed by within subject analyses. Brain Behav Immunol. 2007;21:180–4. doi: 10.1016/j.bbi.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Irwin M, Mascovich A, Gillin JC, Willoughby R, Pike J, Smith TL. Partial sleep deprivation reduces natural killer cell activity in humans. Psychosom Med. 1994;56:493–8. doi: 10.1097/00006842-199411000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Bryant PA, Trinder J, Curtis N. Sick and tired: Does sleep have a vital role in the immune system? Nat Rev Immunol. 2004;4:457–67. doi: 10.1038/nri1369. [DOI] [PubMed] [Google Scholar]
- 12.Palermo TM, Toliver-Sokol M, Fonareva I, Koh JL. Objective and subjective assessment of sleep in adolescents with chronic pain compared to healthy adolescents. Clin J Pain. 2007;23:812–20. doi: 10.1097/AJP.0b013e318156ca63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee K, Ward TM. Critical components of a sleep assessment for clinical practice settings. Issues Ment Health Nurs. 2005;26:739–50. doi: 10.1080/01612840591008320. [DOI] [PubMed] [Google Scholar]
- 14.Manber R, Bootzin RR, Acebo C, Carskadon MA. The effects of regularizing sleep-wake schedules on daytime sleepiness. Sleep. 1996;19:432–41. doi: 10.1093/sleep/19.5.432. [DOI] [PubMed] [Google Scholar]
- 15.LeBourgeois MK. [Accessed 6-14-2002];Children's sleep wake scale. 2001 Vol 2002 [Google Scholar]
- 16.LeBourgeois MK, Giannotti F, Cortesi F, Wolfson A, Harsh J. Sleep hygiene and sleep quality in Italian and American adolescents. Annals N Y Acad Sci. 2004;1021:352–4. doi: 10.1196/annals.1308.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roberts RE, Roberts CR, Chan W. Ethnic differences in symptoms of insomnia among adolescents. Sleep. 2006;29:359–65. doi: 10.1093/sleep/29.3.359. [DOI] [PubMed] [Google Scholar]
- 18.Roberts RE, Lee ES, Hemandez M, Solari AC. Symptoms of insomnia among adolescents in the lower Rio Grande Valley of Texas. Sleep. 2004;27:751–60. doi: 10.1093/sleep/27.4.751. [DOI] [PubMed] [Google Scholar]
- 19.Roberts RE, Roberts CR, Chen IG. Ethnocultural differences in sleep complaints among adolescents. J Nerv Ment Dis. 2000;188:222–9. doi: 10.1097/00005053-200004000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Lee K, McEnany G, Weekes D. Gender differences in sleep patterns for early adolescents. J Adolesc Health. 1999;24:16–20. doi: 10.1016/s1054-139x(98)00074-3. [DOI] [PubMed] [Google Scholar]
- 21.Hinds PS, Hockenberry M, Rai SN, et al. Nocturnal awakenings, sleep environment interruptions, and fatigue in hospitalized children with cancer. Oncol Nurs Forum. 2007;34:393–402. doi: 10.1188/07.ONF.393-402. [DOI] [PubMed] [Google Scholar]
- 22.Hinds PS, Hockenberry M, Rai SN, et al. Clinical field testing of an enhanced-activity intervention in hospitalized children with cancer. J Pain Symptom Manage. 2007;33:686–97. doi: 10.1016/j.jpainsymman.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 23.Docherty SL, Sandelowski M, Preisser JS. Three months in the symptom life of a teenage girl undergoing treatment for cancer. Res Nurs Health. 2006;29:294–310. doi: 10.1002/nur.20143. [DOI] [PubMed] [Google Scholar]
- 24.American Cancer Society. Consumer's Guide to Cancer Drugs. Vol 2004. Boston: Jones and Bartlett Publishers; 2004. [Accessed April 3, 2004]. [Google Scholar]
- 25.Lee K, Cho M, Miaskowski C, Dodd M. Impaired sleep and rhythms in persons with cancer. Sleep Med Rev. 2004;8:199–212. doi: 10.1016/j.smrv.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 26.Palermo TM, Kiska R. Subjective sleep disturbances in adolescents with chronic pain: relationship to daily functioning and quality of life. J Pain. 2005;6:201–7. doi: 10.1016/j.jpain.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 27.Smith MT, Perlis ML, Smith MS, Giles DE, Carmody TP. Sleep quality and presleep arousal in chronic pain. J Behav Med. 2000;23:1–13. doi: 10.1023/a:1005444719169. [DOI] [PubMed] [Google Scholar]