Abstract
Objective:
To evaluate the quality of sleep in Ménière's disease patients with the use of polysomnography.
Study Design:
Prospective study using polysomnography administered in patients diagnosed as “Definite Ménière's disease cases” according to the guidelines of the American Academy of Otolaryngology—Head and Neck Surgery.
Methods:
Thirty-five patients, 17 male and 18 female, aged 31 to 71 (58 average) years with active, unilateral, cochleovestibular Ménière's disease refractory to medical management underwent polysomnography. The results were compared with 35 healthy controls matched for age and sex. All participants underwent full-night polysomnography, and a sleep medicine physician interpreted the results.
Results:
Total sleeping time in Ménière's disease was significantly higher than in controls. Stage 2 sleep was significantly longer and stage 3+4 shorter in Ménière's disease than controls, while there was no difference of stage 1 and REM. Arousal index was significantly higher in Ménière's disease than in controls. Five cases of severe OSAS were found in Ménière's disease and 4 cases in controls; 4 cases of PLMD were found in patients and 3 in controls.
Conclusions:
Our finding of decreased deep sleep and an elevated arousal index is a striking new finding in Ménière's disease. This poor quality of sleep in Ménière's disease patients has received little attention in the past, but may cause additional stress and lead to a negative spiral of symptoms.
Citation:
Nakayama M; Suzuki M; Inagaki A; Takemura K; Watanabe N; Tanigawa T; Okamoto K; Hattori H; Brodie H; Murakami S. Impaired quality of sleep in Ménière's disease patients. J Clin Sleep Med 2010;6(5):445-449.
Keywords: Ménière's disease, sleep, OSAS, PLMD, polysomnography, stress
Ménière's disease is characterized by progressive hearing loss, tinnitus, and intermittent attacks of vertigo, an illusory sensation of movement which is caused by damage to the vestibular organ in the inner ear.1,2 Pathologically, Ménière's disease is associated with hydropic distension of the endolymphatic system, but the etiology remains unknown. Episodes of vertigo, which are often accompanied by nausea and vomiting, are the most prominent and disabling features of the disease. The presentation of Ménière's disease is highly variable and its clinical course is characterized by acute exacerbation and spontaneous remission.2–4
Emotional stress has long been known to be a precipitating factor and a psychosomatic aspect of Ménière's disease.5–8 Emotional stress may increase the risk of an attack of Ménière's disease over the subsequent 1 to 3 hours.7 Horner and Cazals8 clearly indicated that the effect of stress on Ménière's disease is not a psychologic byproduct, but that stress might very well contribute to inner ear pathology. The mechanism behind the relation between stress and Ménière's attacks might be mediated through the hypothalamus. Stress leads to increased secretion of adrenocorticotropic hormone from the anterior pituitary gland, followed by increased adrenocortical production of glucocorticoids (cortisol and corticosterone) and mineral corticoids (aldosterone).8,9 There is growing evidence that emotional stress acts as a trigger of Ménière's disease attacks.7
It is well known that insomnia is associated with increased psychological symptomatology and perceived stress, higher predisposition to arousal, and greater impairment to quality of health.10–12 The relationship between Ménière's disease and stress is well documented, but that between Ménière's disease and insomnia is unclear. Physicians often encounter Ménière's disease patients who also suffer from insomnia,13 but there are no reported studies on the quality of sleep in Ménière's patients.
BRIEF SUMMARY
Current Knowledge/Study Rationale: The relationship between Ménière's disease and stress is well documented, but that between Ménière's disease and insomnia is unclear. Physicians often encounter Ménière's disease patients who also suffer from insomnia, but there are no reported studies on the quality of sleep in Ménière's patients.
Study Impact: We found that Ménière's disease patients who were refractory to medical management might suffer from poor quality of sleep or high arousal with little deep sleep, possibly combined with OSAS or PLMD. Poor quality of sleep may cause additional stress and lead Ménière's disease patients to a negative spiral of symptoms.
MATERIALS AND METHODS
Ménière's Disease Patients and Controls
Patients diagnosed with “Definite Ménière's disease” according to the guidelines for Ménière's disease by the American Academy of Otolaryngology—Head and Neck Surgery1 were recruited from the Department of Otolaryngology in Nagoya City University, Nagoya, Japan. Thirty-five patients, 17 male and 18 female, aged 31 to 71 (58 average) years with active, unilateral, cochleovestibular Ménière's disease refractory to medical management were enrolled in this study. The patients' chief complaints were vertigo attacks, dizziness, tinnitus, ear fullness, and/or hearing loss. No patient reported “sleep disturbance” as a chief complaint, until asked specifically. The patients were instructed to discontinue medications that could influence sleep (such as benzodiazepines) and medications prescribed for Ménière's disease (such as steroids and diuretics) for 2 weeks before the examination. Thirty-five normal healthy subjects matched for age and sex were used as controls. The control group did not report any sleep disturbance or other problems with vertigo attacks, dizziness, tinnitus, ear fullness, and/or hearing loss. All participants underwent full-night polysomnography, and a sleep medicine physician interpreted the results. The present study was approved by the Ethics Review Committee of Nagoya City University, and informed consent was obtained from each individual prior to the study.
Polysomnography
All study participants underwent full-night polysomnography, and a sleep medicine physician interpreted the results. A 12-channel montage was utilized, recording EEG, EOG, EKG, chin, and lower extremity EMG, naso-oral airflow, thoracic and abdominal effort, and oxygen saturation by pulse oximeter. All subjects were evaluated in an accredited sleep laboratory in sound-attenuated rooms, monitored by an infrared camera. The records were scored by the method of Rechtschaffen and Kales.14 Electroencephalogram was divided into NREM and REM sleep. NREM is conventionally subdivided into 4 stages (stage 1 to 4). Sleep stages 3 and 4 were scored together as delta sleep, and movement time was scored as an arousal (2-15 sec) or awakening (> 15 sec). The various indices of sleep architecture analyzed were total sleep time (TST), sleep efficiency (TST divided by time in bed), percentage of sleep stages, apnea index (AI), hypopnea index (HI), and apnea hypopnea index (AHI). Arousal index (ArI) was scored as described by the American Sleep Disorders Association.15 Periodic limb movement index (PLMI) was scored according to standard criteria.16 Digital videotaping with sound recording was performed throughout the night.
Statistics
Based on the level of AHI, obstructive sleep apnea syndrome (OSAS)17 was classified into 3 groups: normal (< 5), mild (5-15), and severe (> 15). PLMI was dichotomized into normal (< 15) and periodic limb movement disorder (PLMD) (≥ 15). Differences between Ménière's disease patients and controls were analyzed with the Wilcoxon matched pairs signed rank test. A value of p < 0.05 was considered statistically significant. We performed all calculations with SPSS Version 17.0 for Windows (Statistical Package for the Social Sciences, SPSS Inc., Chicago, IL), using the LOGISTIC procedures.
RESULTS
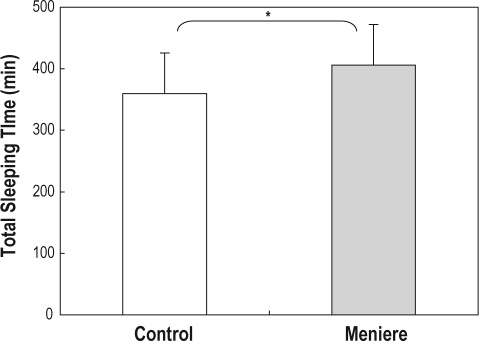
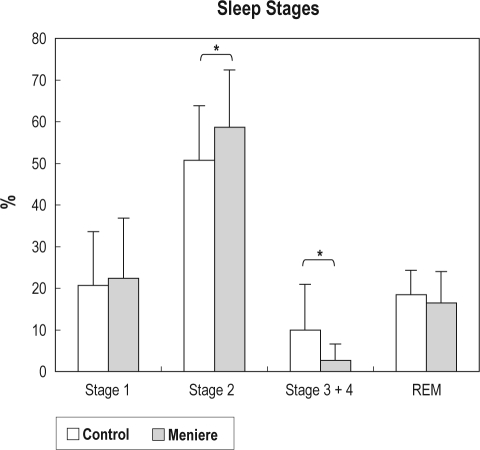
TST ranged from 252 to 509.5 min (mean 406 min) in Ménière's disease patients, and from 188 to 462 min (mean 359.6 min) in controls; this was significantly higher in Ménière's disease patients (p < 0.01; Figure 1). Sleep stages were divided into stage 1, 2, 3+4, and REM. Stage 1 ranged from 2.5% to 87.1% (mean 22.4%) of TST in Ménière's disease patients, and from 1.9% to 53.9% (mean 20.7%) in controls (difference not significant; Figure 2). Stage 2 sleep was significantly longer (p < 0.01) in Ménière's disease patients (range 14.2% to 83.2%, mean 58.7%) than in controls (23.7% to 77.6%, mean 50.7%; Figure 2). Stage 3+4 was significantly shorter in Ménière's disease patients (range 0.3% to 13.1%, mean 2.8%) than in controls (range 0.3% to 46.6%, mean 10%; Figure 2). REM was not significantly different between Ménière's disease patients (range 6.3% to 40.1%, mean 16.5%) and controls (range 7.8% to 28.9%, mean 18.5%; Figure 2).
Figure 1.
Total sleep time was significantly longer in Ménière's disease (range 252-509.5 min, mean 406 min) than in controls (range 188-462 min, mean 359.6 min; p < 0.01). Error bar = standard deviation.
Figure 2.
Sleep stages were divided into stages: 1, 2, 3+4, and REM. Stage 1 ranged from 2.5% to 87.1% (mean 22.4%) in Ménière's disease and 1.9% to 53.9% (mean 20.7%) in controls (not significant). Stage 2 ranged from 14.2% to 83.2% (mean 58.7%) in Ménière's disease and was significantly higher (p < 0.01) than controls (23.7% to 77.6%, mean 50.7%). Stage 3+4 ranged from 0.3% to 13.1% (mean 2.8%) in Ménière's disease and was significantly lower (p < 0.01) than controls (0.3% to 46.6%, mean 10%). REM ranged from 6.3% to 40.1% (mean 16.5%) in Ménière's disease and was not significantly different from controls (7.8% to 28.9%, mean 18.5%). Error bar = standard deviation.
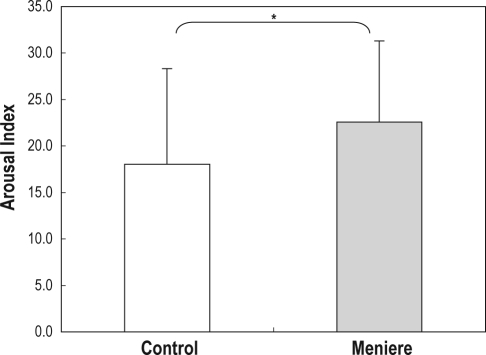
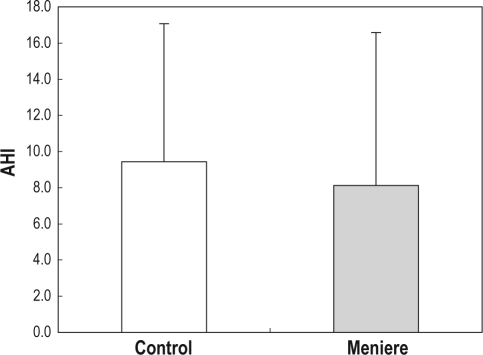
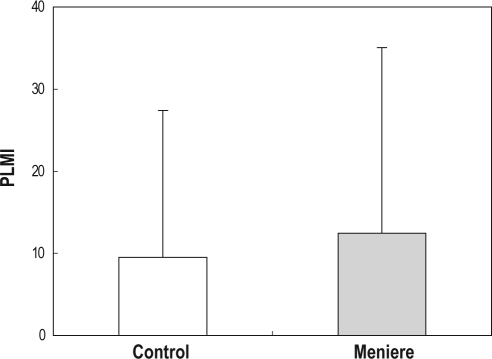
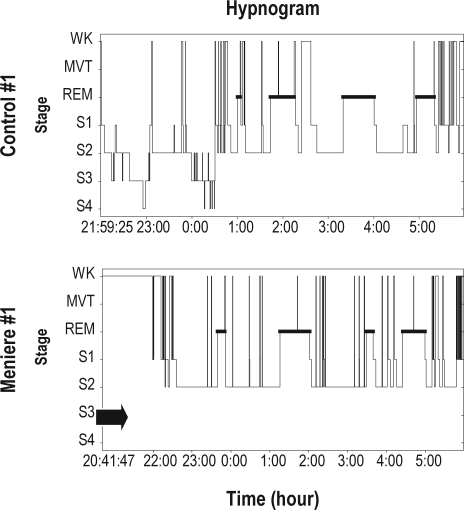
Arousal index was significantly higher (p < 0.05) in Ménière's disease patients (range 8.5-45.1, mean 22) than in controls (range 2.6-37.6, mean 18; Figure 3). AHI was not significantly different between Ménière's disease patients (range 0.5-31.9, mean 8.1) and controls (range 0.3-29.9, mean 9.4; Figure 4). Five cases of severe OSAS were found in patients and 4 cases in controls. PLMI was higher but not significantly different (p = 0.29) in Ménière's disease patients (range 0.5-81.7, mean 12.4) than in controls (range 0.7-71.5, mean 9.5; Figure 5). Four cases of PLMD were found in patients and 3 in controls. Figure 6 shows a hypnogram of a Ménière's patient and a control subject; the control subject showed all sleep stages, while the patient showed complete absence of stage 3 and stage 4 sleep.
Figure 3.
Arousal index ranged from 8.5-45.1 (mean 22) in Ménière's disease; it was significantly higher (p < 0.05) than controls (range 2.6-37.6, mean 18). Error bar = standard deviation.
Figure 4.
AHI ranged from 0.5-31.9 (mean 8.1) in Ménière's disease and was not significantly different than controls (0.3-29.9, mean 9.4). Severe OSAS was found in 5 patients and 4 controls. Error bar = standard deviation.
Figure 5.
PLMI ranged from 0.5-81.7 (mean 12.4) in Ménière's disease; this was higher than controls (0.7-71.5, mean 9.5), but the difference was not significant (p = 0.29). PLMD was found in 4 patients and 3 controls. Error bar = standard deviation.
Figure 6.
A hypnogram of a control and patient. While the control (above) shows all sleep stages (S1-S4 and REM sleep), there is a complete deficit (arrow) of S3 and S4 in the patient (below). wk = wake, mvt = movement time, S1 = sleep stage 1, S2 = sleep stage 2, S3 = sleep stage 3, S4 = sleep stage 4.
DISCUSSION
The effect of sleep deprivation on the vestibular function is largely unknown. Several reports mention that sleep restriction degrades vestibular function. Wolfe and Brown18 found no significant difference in vestibulo-ocular reflex (VOR) after 25-28 h of sleep deprivation. Collins19 reported that the VOR velocity and duration remained unchanged after 24 hours of sleep deprivation and was decreased following 48 to 52 hours of sleep deprivation. In contrast, Quarck20 found that sleep deprivation induced a significant increase in VOR gain after 26 to 29 hours of sleep deprivation. Although findings differ, sleep deprivation obviously may influence vestibular function in some way.
Recent reports suggest that insomnia is not a state of sleep loss, but a disorder of hyperarousal present both during the night and daytime.12 It has been reported that approximately 40% of Ménière's disease patients suffer from inadequate sleep.13 In this study, we found that a significant percentage of Ménière's patients suffered from a very poor quality of sleep, which consisted of a low frequency of deep sleep, high arousal index, and occasional severe OSAS and PLMD. Decreased deep sleep with a significantly high arousal index is a striking new finding in Ménière's disease. The results suggest that remarkable arousal without deep sleep may be one reason that people feel their sleep is inadequate.
Why, then, do Ménière's patients or physicians not often report this poor quality of sleep? NREM sleep, associated with stage 1-4, and REM sleep continue to alternate through the night in cyclical fashion. REM sleep episodes generally become longer across the night. Stage 3 and 4 sleep occupies less time in the second cycle and may disappear altogether from later cycles, as stage 2 sleep expands to occupy the NREM portion of the cycle.21 The proportion of NREM and REM, which is important in managing normal sleep,22,23 was normal in the present Ménière's patients and no different from the controls. Their significantly higher stage 2 and TST in may be a physical response to compensate for the lack of stage 3 and 4 sleep, and higher arousal. This physical compensation may mask the effects of poor quality of sleep but induce “silent insomnia” in Ménière's patients.
It has been proposed that chronic insomniacs suffer from a more general disorder of hyperarousal that may be responsible for both their daytime symptoms and poor nocturnal sleep.24 Attacks of Ménière's disease during daytime may cause insomnia, and insomnia may cause further attacks. Many Ménière's patients complain of lightheadedness, even during periods free from active vertigo attack. It seems possible, then, that the dizziness experienced by these patients is associated with and increased by their poor quality of sleep. Poor quality of sleep may cause additional stress, leading to a vicious cycle with Ménière's symptoms.
OSAS17,25,26 is characterized by repetitive episodes of complete (apnea) or partial (hypopnea) upper airway obstruction during sleep. These events often result in a reduction in blood oxygen saturation and are usually terminated by brief arousals from sleep. PLMD17,27,28 is characterized by periodic episodes of repetitive, highly stereotyped, limb movements that occur during sleep and by clinical sleep disturbance. Typically, the patient is unaware of the limb movements or the frequent sleep disruption. An arousal may precede, coincide with, or follow the limb movement. The prevalence of OSAS or PLMD is reported to be highest among people aged 40-65 years, at 4% to 10%.25–28 Similar morbidity rates for OSAS or PLMD are seen in Ménière's patients from our study. However, Ménière's patients frequently receive benzodiazepines or other drugs that have hypnotic, muscle relaxing, anti-anxiety, and anticonvulsant properties. These properties may have the effect of aggravating OSAS or PLMD symptoms. Ménière's patients who are refractory to medication may find themselves in a vicious cycle combining disease, quality of sleep, and stress. When prescribing hypnotic drugs to Ménière's patients, the possibility should be kept in mind that such drugs could have the effect of increasing the severity of sleep disturbances.
CONCLUSION
Ménière's disease patients who are refractory to medical management may suffer from poor quality of sleep; high arousal with little deep sleep, possibly combined with OSAS or PLMD. Poor quality of sleep may cause additional stress and lead Ménière's disease patients to a negative spiral of symptoms. Furthermore, it may result in being refractory to medical management. Ménière's disease patients are often prescribed benzodiazepines to manage their vertigo. However, these medications may aggravate underlying contributing factors for sleep disturbance, which may, in turn, exacerbate the Ménière's disease. Based on our current findings, we would recommend that sleep studies be obtained prior to initiation of benzodiazepines for the treatment of Ménière's disease.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Monsell EM. New and revised reporting guidelines from the Committee on Hearing and Equilibrium. American Academy of Otolaryngology-Head and Neck Surgery Foundation, Inc. Otolaryngol Head Neck Surg. 1995;113:176–8. doi: 10.1016/S0194-5998(95)70100-1. [DOI] [PubMed] [Google Scholar]
- 2.Sajjadi H, Paparella MM. Ménière's disease. Lancet. 2008;372:406–14. doi: 10.1016/S0140-6736(08)61161-7. [DOI] [PubMed] [Google Scholar]
- 3.Coelho DH, Lalwani AK. Medical management of Ménière's disease. Laryngoscope. 2008;118:1099–108. doi: 10.1097/MLG.0b013e31816927f0. [DOI] [PubMed] [Google Scholar]
- 4.Green JD, Jr, Verrall A, Gates GA. Quality of life instruments in Ménière's disease. Laryngoscope. 2007;117:1622–8. doi: 10.1097/MLG.0b013e3180caa14f. [DOI] [PubMed] [Google Scholar]
- 5.Horner KC, Guieu R, Magnan J, Chays A, Cazals Y. Prolactinoma in some Ménière's patients–is stress involved? Neuropsychopharmacology. 2002;26:135–8. doi: 10.1016/S0893-133X(01)00356-6. [DOI] [PubMed] [Google Scholar]
- 6.Fowler EP, Jr, Zeckel A. Psychosomatic aspects of Ménière's disease. JAMA. 1952;148:1265–8. doi: 10.1001/jama.1952.02930150001001. [DOI] [PubMed] [Google Scholar]
- 7.Söderman AC, Möller J, Bagger- Sjöbäck D, Bergenius J, Hallqvist J. Stress as a trigger of attacks in Ménière's disease. A case-crossover study. Laryngoscope. 2004;114:1843–8. doi: 10.1097/00005537-200410000-00031. [DOI] [PubMed] [Google Scholar]
- 8.Horner KC, Cazals Y. Stress hormones in Ménière's disease and acoustic neuroma. Brain Res Bull. 2005;15:1–8. doi: 10.1016/j.brainresbull.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 9.Cruijsen NV, Dullaart RP, Wit HP, Albers FW. Analysis of cortisol and other stress-related hormones in patients with Ménière's disease. Otol Neurotol. 2005;26:1214–9. doi: 10.1097/01.mao.0000179528.24909.ba. [DOI] [PubMed] [Google Scholar]
- 10.LeBlanc M, Beaulieu-Bonneau S, Mérette C, Savard J, Ivers H, Morin CM. Psychological and health-related quality of life factors associated with insomnia in a population-based sample. J Psychosom Res. 2007;63:157–66. doi: 10.1016/j.jpsychores.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Partinen M. Sleep disorders and stress. J Psychosom Res. 1994;38(suppl):89–91. doi: 10.1016/0022-3999(94)90139-2. [DOI] [PubMed] [Google Scholar]
- 12.Basta M, Chrousos GP, Vela-Bueno A, et al. Chronic insomnia and stress system. Sleep Med Clin. 2007;2:279–91. doi: 10.1016/j.jsmc.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Takahashi M, Odagiri K, Sato R, Wada R, Onuki J. Personal factors involved in onset or progression of Ménière's disease and low-tone sensorineural hearing loss. ORL J Otorhinolaryngol Relat Spec. 2005;67:300–4. doi: 10.1159/000089412. [DOI] [PubMed] [Google Scholar]
- 14.Rechtschaffen A, Kales A. Los Angeles: Brain Information Service/Brain Research Institute; 1968. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. [Google Scholar]
- 15.American Sleep Disorders Association Report. EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep. 1992;15:173–84. [PubMed] [Google Scholar]
- 16.American Sleep Disorders Association Report. EEG arousals: atlas and scoring rules. Recording and scoring leg movements. Sleep. 1993;16:749–59. [Google Scholar]
- 17.American Academy of sleep Medicine. ICSD-2. International classification of sleep disorders, 2nd Ed. (ICSD-2): Diagnostic and coding manual. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 18.Wolfe JW, Brown JH. Effects of sleep deprivation on the vestibulo-ocular reflex. Aerosp Med. 1968;39:947–9. [PubMed] [Google Scholar]
- 19.Collins WE. Some effects of sleep loss on vestibular responses. Aviat Space Environ Med. 1988;59:523–9. [PubMed] [Google Scholar]
- 20.Quarck G, Ventre J, Etard O, Denise P. Total sleep deprivation can increase vestibulo-ocular responses. J Sleep Res. 2006;15:369–75. doi: 10.1111/j.1365-2869.2006.00550.x. [DOI] [PubMed] [Google Scholar]
- 21.Kryger MH, Roth T, Dement WC. Philadelphia, PA: W.B. Saunders Company; 2000. Sleep Medicine; pp. 15–25. [Google Scholar]
- 22.Zisapel N. Sleep and sleep disturbances: biological basis and clinical implications. Cell Mol Life Sci. 2007;64:1174–86. doi: 10.1007/s00018-007-6529-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mahowald MW, Schenck CH. Insights from studying human sleep disorders. Nature. 2005;437:1279–85. doi: 10.1038/nature04287. [DOI] [PubMed] [Google Scholar]
- 24.Stepanski E, Zorick F, Roehrs T, Young D, Roth T. Daytime alertness in patients with chronic insomnia compared with asymptomatic control subjects. Sleep. 1998;11:54–60. doi: 10.1093/sleep/11.1.54. [DOI] [PubMed] [Google Scholar]
- 25.Partinen M, Telakivi T. Epidemiology of obstructive sleep apnea syndrome. Sleep. 1992;15:1–4. doi: 10.1093/sleep/15.suppl_6.s1. [DOI] [PubMed] [Google Scholar]
- 26.Akomro RP, Kryger MH. Clinical presentations of obstructive sleep apnea syndrome. Prog Cardiovasc Dis. 1999;41:331–40. doi: 10.1053/pcad.1999.0410331. [DOI] [PubMed] [Google Scholar]
- 27.Ohayon MM, Roth T. Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. J Psychosom Res. 2002;53:547–54. doi: 10.1016/s0022-3999(02)00443-9. [DOI] [PubMed] [Google Scholar]
- 28.Hornyak M, Trenkwalder C. Restless legs syndrome and periodic limb movement disorder in the elderly. J Psychosom Res. 2004;56:543–8. doi: 10.1016/S0022-3999(04)00020-0. [DOI] [PubMed] [Google Scholar]