Abstract
Background:
Lower extremity alignment may influence the load distribution at the knee, potentially predisposing the anterior cruciate ligament to greater stress. We examined whether lower extremity alignment predicted the magnitude of anterior knee laxity in men and women.
Hypothesis:
Greater anterior pelvic angle, hip anteversion, tibiofemoral angle, genu recurvatum, and navicular drop will predict greater anterior knee laxity.
Study Design:
Descriptive laboratory study.
Methods:
Women (n = 122) and men (n = 97) were measured for anterior knee laxity and 7 lower extremity alignment variables on their dominant stance leg. Linear regression determined the extent to which the alignment variables predicted anterior knee laxity for each sex.
Results:
Lower anterior pelvic tilt and tibiofemoral angle, and greater genu recurvatum and navicular drop were related to greater anterior knee laxity in women, explaining 28.1% of the variance (P < .001). Lower anterior pelvic tilt and greater hip anteversion, genu recurvatum and navicular drop were predictors of greater anterior knee laxity in men, explaining 26.5% of the variance (P < .001).
Conclusion:
Lower anterior pelvic tilt, greater knee hyperextension, and foot pronation predicted greater anterior knee laxity in both men and women, with genu recurvatum and navicular drop having the greatest impact on anterior knee laxity. Greater hip anteversion was also a strong predictor in men, while a lower tibiofemoral angle was a significant predictor in women.
Clinical Relevance:
The associations between lower extremity alignment and anterior knee laxity suggest that alignment of the hip, knee, and ankle may be linked to or contribute to abnormal loading patterns at the knee, potentially stressing the capsuloligamentous structures and promoting greater joint laxity.
Keywords: posture, alignment, anterior cruciate ligament, joint laxity
Anterior knee laxity (AKL) defines the amount of anterior displacement of the tibia relative to the femur, where the primary restraint is the anterior cruciate ligament (ACL). Greater AKL has been identified as a risk factor for ACL injury and has the potential to disrupt normal joint neuromechanics during weightbearing activity.† While AKL is known to vary widely among individuals and on average is greater in adult (but not adolescent) women compared to men, little is known about the collective factors that may contribute to or are associated with greater AKL and whether these factors differ between sexes.‡ Previous research suggests that sex hormones may in part explain the greater values observed in adult women compared to men due to cyclic changes in women during their menstrual cycle.10,15,39 However, even within sex there exists a broad range of knee laxity values. Therefore, it is likely that other factors also influence the magnitude of AKL.
Alignment of the hip, knee, and ankle is thought to play a key role in the load distribution at the knee36 and, thus, the tension placed on the capsuloligamentous structures. For example, a compensatory increase in internal tibial rotation is thought to accompany excessive subtalar pronation during weightbearing that creates a preloading, rotatory stress to the knee joint.1,3,8,9 In the intact knee, this rotatory force may stress the ligaments over time, promoting greater joint laxity. This is supported by in vivo work that has demonstrated an increase in ACL loads during weightbearing when an internal rotation torque is applied at the knee.11 When these internal rotation torques are applied in combination with knee hyperextension26,27 or knee valgus,19 ACL loads are reported to be substantially higher than when valgus or internal rotation torques are applied alone. Together, these findings would suggest that lower extremity alignments that promote excessive knee valgus, knee hyperextension, and tibial internal rotation during weightbearing may create tension and stretch the ACL, potentially promoting greater AKL. Moreover, many of these alignment factors (greater anterior pelvic tilt, genu recurvatum, and navicular drop) have been identified as risk factors for ACL injury in retrospective and case-control studies.3,16,22,24,32,35,50
Despite the potential association between lower extremity alignment and greater AKL, little empirical data are available to support these relationships. Coplan et al7 reported greater internal-external rotational motion at the knee at 5° of flexion in subjects with a pronated foot compared to a more neutral foot. Woodford-Rogers et al50 observed both greater navicular drop and AKL in the noninjured limb of ACL-injured subjects compared to uninjured subjects. We are aware of only 2 studies18,47 that have examined the relationship between lower extremity alignment and AKL in the healthy knee. In the sagittal plane, knee hyperextension in otherwise healthy knees was reported to impinge the ACL against the intercondylar roof at an average of 6.3° ± 3.8° of hyperextension, and the amount of knee hyperextension an individual had past this point of impingement (hyperextension laxity) was strongly correlated with their AKL as measured by maximal manual displacement.18 In contrast, Trimble et al47 examined whether clinical measures of navicular drop, thigh foot angle (as a measure of tibial torsion), and genu recurvatum were related to AKL in uninjured subjects. Using a stepwise regression analysis, only sex and navicular drop entered the model as moderate predictors of AKL, and no relationship was observed between genu recurvatum and AKL. These findings are based on relatively small samples, limited alignment variables, and with men and women examined in the same analysis.
Because alignment of the pelvis, hip, and knee can be very different in men and women,30 it may not be appropriate to include both sexes in the same analysis and simply “adjust” for sex. Further, understanding the impact of one variable on AKL may be dependent on what other alignments are present, and therefore the hip and pelvis should also be considered for their potential to modify alignment and joint stresses at the knee and foot.17,20 To that end, our purpose was to examine the relationship between the collective alignment of the lower extremity and the magnitude of AKL in men and women. Based on previous literature and existing clinical theory, our expectation was that individuals who have greater amounts of anterior pelvic angle, hip anteversion, tibiofemoral angle, genu recurvatum, and navicular drop values would have a greater magnitude of AKL, regardless of sex.
Materials and Methods
The stance limb (support leg when kicking a ball) of 122 women (21.6 ± 2.5 years, 63.8 ± 12.3 kg, 163.5 ± 6.8 cm) and 97 men (23.1 ± 3.2 years, 80.7 ± 13.1 kg, 177.4 ± 8.5 cm) were measured for AKL and 7 lower extremity alignment variables: pelvic angle, hip anteversion, tibiofemoral angle, genu recurvatum, tibial torsion, navicular drop, and femur to tibia length ratio, using established clinical measurement techniques as detailed below. The population represents a combined sample of 100 subjects (50 men, 50 women) from a previous study where we reported on sex differences and bilateral asymmetries30,40 and 119 subjects from an ongoing project examining the effects of hormone-mediated knee laxity on knee stability (72 women, 47 men). A single investigator with excellent measurement reliability on all measures (intraclass correlation coefficient [ICC]2,3 > .87)30,42 collected the anatomical variables from all 219 subjects. With the exception of genu recurvatum, all variables were measured using identical measurement techniques across the 2 samples. The measurement procedures, validity, and reliability of these measurement methods have been previously described30,41,42 and illustrated30 in detail, and the measurements are briefly defined here. All standing measurements were taken with the subject barefoot, feet placed biacromial width apart, arms across their chest, and looking straight ahead.42
Anterior knee laxity was measured supine and the knee flexed to 25° (± 5°) over a thigh bolster and recorded in millimeters (mm) as the amount of anterior displacement of the tibia on the femur while applying a 133-N anterior load to the posterior tibia using a knee arthrometer (KT2000; MedMetric Corp, San Diego, California). Pelvic angle was measured while standing as the angle in degrees formed by intersecting lines between the horizontal plane and a line from the anterior superior iliac spine to the posterior iliac spine using an inclinometer (Performance Attainment Associates, St. Paul, Minnesota).13,42 Hip anteversion was measured with the subject prone and the knee flexed to 90° using the Craig’s test.25 Tibiofemoral angle (frontal plane knee angle) was measured standing using the anatomical axis of the femur and tibia.29 With the goniometer axis positioned over the knee center (midpoint between the medial and lateral joint line in the frontal plane), tibiofemoral angle was recorded as the angle formed between intersecting lines from the knee joint center to a landmark midway between the anterior superior iliac spine (ASIS) and greater trochanter, and from the knee joint center to the ankle center.
Genu recurvatum was measured supine, with the distal tibia supported on a bolster, as the angle formed between the line of the femur (lateral femoral epicondyle to the greater trochanter) and the line of the tibia (lateral femoral epicondyle to the lateral malleolus). In the first 100 subjects, genu recurvatum was measured while the investigator passively extended the knee until resistance was felt.42 In the later 119 subjects, genu recurvatum was measured while the subjects actively and maximally extended their knees.41 The reason for this change is that over time we have found this later technique to be more comfortable for the participant and easier for the tester. In 15 subjects we verified that this change in procedure resulted in no systematic differences in the measure (4.6° ± 5.6° vs 4.5° ± 5.7°; ICC(2,3) = 0.97; standard error of the mean [SEM] = 1.0°).
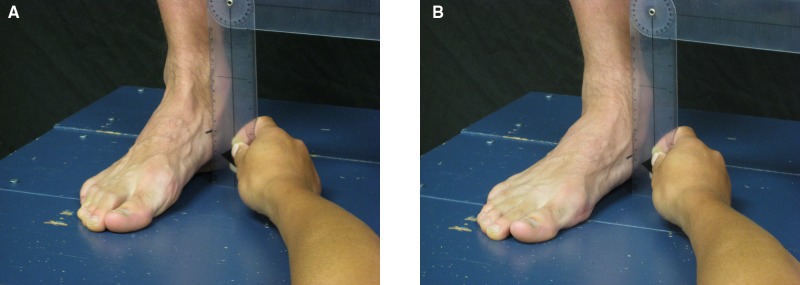
Tibial torsion was measured supine with the femur positioned so that a line between the epicondyles was parallel to the horizontal plane. Then the angle formed between the true vertical (verified with a bubble level) and a line bisecting the bimalleolar axis was measured to the nearest degree.42,46 Navicular drop was measured while the subject stood, as the change in navicular height (mm) between standing subtalar joint neutral and standing relaxed (Figure 1). Subtalar joint neutral was defined as the position where the medial and lateral aspects of the talar head were equally palpable.6 Lastly, femoral and tibial length were measured in centimeters (cm) with a sliding anthropometric caliper as the distance from the superior aspect of the greater trochanter to the lateral joint line of the knee, and the distance from the medial joint line to the most distal aspect of the medial malleolus, respectively.42 From these values the femur to tibia length ratio was computed.
Figure 1.
Measurement of navicular drop as the change in navicular height from standing neutral (A) to standing relaxed (B).
Statistical Analyses
All anatomical variables were measured 3 times on the dominant stance limb, and the average of the 3 measures was used for analysis. Multiple linear regression was used to examine the association between lower extremity alignment and AKL for each sex. All alignment variables were first entered simultaneously so that we could examine the independent effects of each of the variables after controlling for the others. We followed this full regression model with a stepwise removal technique (tolerance = .20). The purpose of the stepwise removal was to determine if the prediction model could be simplified to fewer variables without substantially reducing the variance explained.31 We ran separate regression models for men and women because, as previously stated, the distributions of most of the alignment variables differ significantly by sex30 and it would have been inappropriate to simply “control” or “adjust” for sex in models when examining their relationship with AKL.
Results
Means and standard deviations for each variable separated by sex are presented in Table 1. Table 2 presents the complete (all variables entered) multiple linear regression summary results for men and women. Table 3 presents the coefficients for the regression model following stepwise removal.
Table 1.
Means and standard deviations (SD) for each anatomical variable stratified by sex.
| Women (n = 122) | Men (n = 97) | |
|---|---|---|
| Variable | Mean ± SD (Range) | Mean ± SD (Range) |
| Anterior knee laxity, mm | 7.1 ± 2.1 (3.0 to 15.0) | 7.1 ± 2.1 (3.0 to 14.8) |
| Pelvic angle, ° | 11.9 ± 4.4 (–1.67 to 24.0) | 8.9 ± 4.0 (–1.0 to 18.0) |
| Hip anteversion, ° | 14.5 ± 6.4 (–14.3 to 35.0) | 8.4 ± 5.2 (0.3 to 23.3) |
| Tibiofemoral angle, ° | 11.6 ± 2.4 (5.0 to 16.7) | 9.5 ± 2.6 (4.0 to 16.7) |
| Genu recurvatum, ° | 5.7 ± 4.0 (–2.0 to 21.0) | 3.0 ± 3.3 (–8.0 to 13.0) |
| Tibial torsion, ° | 20.7 ± 7.3 (–4.33 to 37.7) | 18.7 ± 6.9 (2.0 to 35.3) |
| Navicular drop, mm | 7.1 ± 4.6 (–2.70 to 24.0) | 6.1 ± 3.3 (–2.0 to 15.3) |
| Femur to tibial length, ratio | 1.19 ± 0.05 (1.03 to 1.37) | 1.17 ± 0.06 (0.88 to 1.31) |
Table 2.
Regression summary results for the complete model when predicting anterior knee laxity based on postural variables, stratified by sex.
| Women (n = 122) | Men (n = 97) | |||||||
|---|---|---|---|---|---|---|---|---|
| Unstandardized Coefficients | Unstandardized Coefficients | |||||||
| Variable | SEa | t Value | P Valueb | SEa | t Value | P Valueb | ||
| Constant (Intercept) | 5.310 | 4.335 | 1.225 | .223 | 6.406 | 4.659 | 1.375 | .173 |
| Pelvic angle, ° | −0.057 | 0.039 | −1.455 | .148 | −0.109 | 0.048 | −2.261 | .026b |
| Hip anteversion, ° | 0.017 | 0.027 | 0.649 | .518 | 0.089 | 0.040 | 2.234 | .028b |
| Tibiofemoral angle, ° | −0.119 | 0.071 | −1.685 | .095 | −0.058 | 0.085 | −0.680 | .498 |
| Genu recurvatum, ° | 0.151 | 0.046 | 3.286 | .001b | 0.177 | 0.061 | 2.898 | .005b |
| Tibial torsion, ° | −0.022 | 0.024 | −0.919 | .360 | 0.020 | 0.028 | 0.706 | .482 |
| Navicular drop, mm | 0.150 | 0.039 | 3.899 | .001b | 0.173 | 0.060 | 2.913 | .005b |
| Femur:tibia length, ratio | 1.778 | 3.438 | 0.517 | .606 | −0.425 | 3.611 | −0.118 | .907 |
SE, standard error.
Significant at P < .05.
Table 3.
Unstandardized regression coefficients remaining in the final regression model (P < .200) following stepwise removal when predicting anterior knee laxity, stratified by sex.
| Women (n = 122) | Men (n = 97) | |||
|---|---|---|---|---|
| Variable (Left Side) | Unstandard Coefficient | P Value | Unstandard Coefficient | P Value |
| Constant (Intercept) | 7.316 | <.001a | 5.682 | <.001a |
| Pelvic angle, ° | −.050 | .197 | −.106 | .029a |
| Hip anteversion, ° | .091 | .016a | ||
| Tibiofemoral angle, ° | −.138 | .045a | ||
| Genu recurvatum, ° | .163 | <.001a | .180 | .003a |
| Tibial torsion, ° | ||||
| Navicular drop, mm | .148 | <.001a | .172 | .004a |
| Femur to tibia length, ratio | ||||
Significant at P < .05.
When examining the complete regression models, the amount of variance explained by the lower extremity alignment variables was similar for men (27.4%; P < .001) and women (29.2%; P < .001) (Table 2). When all variables were accounted for, greater genu recurvatum and navicular drop were significant predictors of AKL in both men and women, and decreased anterior pelvic tilt and greater hip anteversion were predictors of AKL in men. After removing the alignment variables that had little impact on the overall variance explained in AKL (using a P value of > .200 as the criteria for removal), a combination of lower anterior pelvic tilt and tibiofemoral angle and greater genu recurvatum and navicular drop were associated with greater AKL in women, explaining 28.1% of the variance (compared to 29.2% for the full model) in AKL (R2 = 0.281; P < .001) (Table 3). Of these, genu recurvatum and navicular drop were the strongest predictors of AKL, measured both in terms of magnitude of the estimated regression coefficient ( = 0.163 and 0.148, respectively), and in terms of statistical significance (both P < .001). The third most important predictor in the model, again both in terms of magnitude of the coefficient ( = −0.138) and statistical significance (P = .045), was tibiofemoral angle. The P value for the association of pelvic angle with AKL in women did not reach a level of significance in the final stepwise removal model (P = .197) but was negatively associated with AKL ( = −0.050).
When examining the final stepwise removal regression model for men, a combination of less anterior pelvic tilt and greater hip anteversion, genu recurvatum, and navicular drop were associated with greater AKL, explaining 26.5% of the variance (R2 = 0.265; P < .001; compared to 27.4% for the full model) (Table 3). As with women, greater genu recurvatum and navicular drop were the strongest predictors of greater AKL in men among the variables examined, both in terms of magnitude of the coefficients ( = 0.180 and 0.172, respectively) and statistical significance (both P < .004), and the strength of these coefficients were somewhat higher than women. Unlike women, greater hip anteversion ( = 0.091; P = .016) and less anterior pelvic tilt ( = −0.106; P = .029) were also significant predictors of greater AKL in men.
Discussion
This is the first study to our knowledge that has examined the collective alignment of the pelvis, hip, knee, and ankle and its relationship to AKL. Our primary findings were that lower extremity alignment variables explained approximately 28% and 27% of the variance in AKL in women and men, respectively. Given that an R2 value of 0.25 or greater is considered a large effect,31 the amount of variance in AKL explained by lower extremity alignment is substantial. However, our hypothesis was only partially supported. While greater genu recurvatum and navicular drop were associated with greater AKL in both men and women as expected, greater hip anteversion and decreased anterior pelvic tilt were only related to greater AKL in men, while lower tibiofemoral angles was only related to AKL in women. Further, the relationships noted between tibiofemoral angle and anterior pelvic tilt with AKL were negative rather than positive.
Consistent with previous literature,7,47 greater foot pronation (as measured by navicular drop) had a strong association with greater AKL in both men and women. As the foot excessively pronates during the stance phase of gait, there is an obligatory internal rotation of the tibia on the foot that is thought to lead to internal rotation of the tibia on the femur,1,3,8,9 with the later increasing ACL loads in the weightbearing knee.11 But while a relationship between foot pronation and ACL injury has been documented in several retrospective studies,3,16,24,50 the biomechanical relationships between foot pronation (as measured by rearfoot eversion) and internal rotation of the tibia on the femur remain unclear.23,28 During walking, no differences in tibial rotation at the knee were observed,23 but during running, approximately 3° greater tibial internal rotation motion was observed in subjects with excessive pronation.28 These studies used relatively small samples and did not account for the alignment of the hip and knee, which could also contribute to the net rotatory motions observed at the knee. Future investigations during more dynamic activity (eg, landing or cutting) while also accounting for alignment of the hip and knee may further clarify these biomechanical relationships.
Greater genu recurvatum was also a strong predictor of AKL in both men and women once all postural variables were accounted for. Loudon et al24 also observed greater genu recurvatum (with pronation) in ACL-injured women, but Trimble et al47 reported no relationships between genu recurvatum and AKL. The lack of relationship noted by Trimble et al47 may be due in part to the different approaches in data analyses. While Loudon et al24 studied only women and we examined men and women separately, Trimble et al analyzed men and women together. Because they found that genu recurvatum was significantly greater in women (5.8° ± 4.2°) compared to men (3.2° ± 1.5°), genu recurvatum was likely highly correlated with sex, which would have prevented genu recurvatum from entering the model once sex was accounted for. Further, the bivariate correlations they observed between genu recurvatum and AKL for their combined sample (r = 0.184) was lower than what we found within women (r = 0.404) and men (r = 0.338) in the current study. Hence, it is possible that the independent relationship between genu recurvatum and AKL is stronger within a particular sex given that there are substantial differences between men and women in their overall lower extremity posture.30
Research has shown that hyperextension with and without internal tibial torques can dramatically increase ACL tensile forces,26,27 and retrospective studies have identified an association between greater genu recurvatum and ACL injury.22,24,32,35 Considering these findings in light of our results, individuals with greater genu recurvatum may experience chronic tensioning on the ACL over time, leading to greater AKL. This is supported by Jagondzinski et al,18 who examined 15 healthy knees and found that the amount of knee hyperextension range of motion (9.0° ± 4.8°) past the point of impingement of the ACL against the intercondylar notch roof (6.3° ± 3.8°) was positively correlated with AKL (r = 0.77) as measured by maximum manual displacement of the tibia on the femur. Higher ACL loads have been reported when internal rotation torques were applied along with the knee hyperextended.26,27 This is consistent with our findings that the combination of greater navicular drop (resulting in tibial internal rotation) and genu recurvatum (resulting in knee hyperextension) were related to greater AKL. However, it is important to note that these mechanical connections remain theoretical, as our regression analyses do not establish cause and effect. Another plausible explanation for these relationships is that genu recurvatum is related to AKL simply because they both represent measures of joint laxity. To confirm that this was not simply a hyperlaxity situation, we ran an exploratory analysis on a subset of these data where we had also obtained general joint laxity measures using the Beighton and Horan Joint Mobility Index4 (n = 95). When examining the relationships between individual joint scores (ie, presence or absence of hyperlaxity) for the elbow, thumb, fifth finger, knee, and forward flexion with anterior knee laxity, the correlations were very low for thumb, fifth finger, elbow, and trunk (Pearson r range, .022-.144; P > .05), yet the correlations between the knee scores were higher and reached a level of significance (.207-.283; P < .05). Therefore, the relationship between genu recurvatum and AKL does not appear to be based on a situation of hyperlaxity alone.
Although it is not clear why greater hip anteversion was only found to be a strong predictor of AKL in men, it is logical that this may also promote greater rotary stress on the knee when combined with navicular drop and genu recurvatum. Greater hip anteversion is commonly associated with an intoeing gait,14,45 which can lead to compensations in other parts of the lower extremity, including excessive internal rotation of the tibia and overpronation of the subtalar joint during walking.45
Based on clinical observations17,20 and previous research,21 our expectation was that greater anterior pelvic tilt would be related to greater AKL concomitant to its proposed effect on alignment of the hip (femoral internal rotation), knee (valgus and genu recurvatum), and ankle (pronation). However, if an increase in anterior pelvic tilt allows for more internal femoral rotation, this would allow the femur to follow the tibia into internal rotation, effectively reducing rather than increasing rotatory stress at the knee in those with excessive pronation. Hence, less anterior pelvic tilt (maintaining the femur in more external rotation) and greater pronation (promoting greater tibial internal rotation), may potentially combine to increase rotatory stress at the knee. While more work is needed in this area, these findings emphasize the importance of accounting for alignment of the entire lower extremity when screening individuals for anatomical factors that may influence knee loads, joint laxity, and injury risk.
Contrary to our hypothesis, tibiofemoral angle was a negative predictor of AKL in women and had little to no relationship with AKL in men. Frontal plane knee alignment has been shown to influence the load distribution in the frontal plane,36 and excessive varus and valgus alignment has been associated with greater varus-valgus knee laxity.49 Given previous work that identified strong associations between AKL and varus-valgus knee laxity,44 we expected greater tibiofemoral angles to be related to greater AKL. However, in women, a more varus knee was associated with greater AKL once other postural variables were accounted for. Based on our collective findings, it appears that alignment factors that have the potential to combine to produce excessive rotary stress at the knee (ie, pelvic angle, hip anteversion, genu recurvatum, and navicular drop) may represent the more important predictors of greater AKL.
In summary, less anterior pelvic tilt, and less tibiofemoral angle (women only), and greater amounts of hip anteversion (men only), genu recurvatum, and navicular drop had the strongest association with greater AKL. These results, along with findings of pelvic angle, genu recurvatum, and navicular drop being more prevalent in ACL-injured populations,16,24,32,35,50 suggest that variations in these alignment factors may be associated with or create abnormal loading patterns at the knee that ultimately stress the capsuloligamentous structures and promote greater AKL. However, these findings are limited to the assessment of AKL in vivo, and biomechanical studies are needed to further clarify how variations in these alignment factors impact actual knee joint–loading patterns. As many of these lower extremity alignment characteristics develop during pubertal growth,41 examining these relationships in a maturing youth population would also be beneficial. These findings also reinforce the need for clinicians to consider the alignment of the entire lower extremity when screening for injury risk, as relationships between alignment variables, knee joint loading, and AKL may be quite different depending on what other alignment variables are accounted for.37 An improved understanding of these relationships may allow clinicians to better screen for and identify athletes who are prone to excessive joint laxity and who may experience greater challenges in dynamically stabilizing the knee during sport activity.
Acknowledgments
This project was supported by Grant Number R01- AR53172 NIH-NIAMS.
Footnotes
NATA Members: Receive 3 free CEUs each year when you subscribe to Sports Health, take, and pass the related online quizzes! Not a subscriber? Not a member? The Sports Health–related CEU quizzes are also available for purchase. For more information and to take the quiz for this article, visit www.nata.org/sportshealthquizzes.
No potential conflict of interest declared.
References
- 1. Bates BT, Osternig LR, Mason B, et al. Foot orthotic devices to modify selected aspects of lower extremity mechanics. Am J Sports Med. 1979;7(6):338-342 [DOI] [PubMed] [Google Scholar]
- 2. Baxter MP. Assessment of normal pediatric knee ligament laxity using the genucom. J Ped Orthop. 1988;8:543-545 [DOI] [PubMed] [Google Scholar]
- 3. Beckett ME, Massie DL, Bowers KD, et al. Incidence of hyperpronation in the ACL-injured knee: a clinical perspective. J Athl Train. 1992;27(1):58-60 [PMC free article] [PubMed] [Google Scholar]
- 4. Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Annals Rheum Dis. 1973;32:413-418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Beynnon BD, Bernstein I, Belisle A, et al. The effect of estradiol and progesterone on knee and ankle joint laxity. Am J Sports Med. 2005;33(9):1298-1304 [DOI] [PubMed] [Google Scholar]
- 6. Brody DM. Techniques in the evaluation and treatment of the injured runner. Orthop Clin North Am. 1982;13(3):541-558 [PubMed] [Google Scholar]
- 7. Coplan JA. Rotational motion of the knee: a comparison of normal and pronating subjects. J Orthop Sports Phys Ther. 1989;10:366-369 [DOI] [PubMed] [Google Scholar]
- 8. Cornwall MW, McPoil TG. Footwear and foot orthotic effectiveness research: a new approach. J Orthop Sports Phys Ther. 1995;21(6):337-344 [DOI] [PubMed] [Google Scholar]
- 9. Cowan DN, Jones BH, Frykman PN, et al. Lower limb morphology and risk of overuse injury among male infantry trainees. Med Sci Sports Exerc. 1996;28(8):945-952 [DOI] [PubMed] [Google Scholar]
- 10. Deie M, Sakamaki Y, Sumen Y, et al. Anterior knee laxity in young women varies with their menstrual cycle. International Orthop. 2002;26:154-156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fleming BC, Renstrom PA, Beynnon BD, et al. The effect of weightbearing and external loading on anterior cruciate ligament strain. J Biomech. 2001;34(3):163-170 [DOI] [PubMed] [Google Scholar]
- 12. Flynn JM, Mackenzie W, Kolstad K, et al. Objective evaluation of knee laxity in children. J Ped Orthop. 2000;20:259-263 [PubMed] [Google Scholar]
- 13. Gilliam J, Brunt D, MacMillan M, et al. Relationship of the pelvic angle to the sacral angle: measurement of clinical reliability and validity. J Orthop Sports Phys Ther. 1994;20(4):193-199 [DOI] [PubMed] [Google Scholar]
- 14. Gulan G, Matovinovic D, Nemec B, et al. Femoral neck anteversion: values, development, measurement, common problems. Colleg Antropol. 2000;24(2):521-527 [PubMed] [Google Scholar]
- 15. Heitz NA. Hormonal changes throughout the menstrual cycle and increased anterior cruciate ligament laxity in females. J Athl Train. 1999;343(2):144-149 [PMC free article] [PubMed] [Google Scholar]
- 16. Hertel JN, Dorfman JH, Braham RA. Lower extremity malalignments and anterior cruciate ligament injury history. J Sports Sci Med. 2004;3:220-225 [PMC free article] [PubMed] [Google Scholar]
- 17. Hruska R. Pelvic stability influences lower extremity kinematics. Biomechanics. 1998;6:23-29 [Google Scholar]
- 18. Jagodzinski M, Richter GM, Pässler HH. Biomechanical analysis of knee hyperextension and of the impingement of the anterior cruciate ligament: a cinematographic MRI study with impact on tibial tunnel positioning in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2000;8(1):11-19 [DOI] [PubMed] [Google Scholar]
- 19. Kanamori A, Woo SLY, Ma B, et al. The forces in the anterior cruciate ligament and knee kinematics during a simulated pivot-shift test: a human cadaveric study using robotic technology. Arthroscopy. 2000;16(6):633-639 [DOI] [PubMed] [Google Scholar]
- 20. Kendall FP, McCreary EK, Provance PG. Muscles Testing and Function. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1993:72-98 [Google Scholar]
- 21. Khamis S, Yishar Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait & Posture. 2007;25(1):127-134 [DOI] [PubMed] [Google Scholar]
- 22. Kramer LC, Denegar CR, Buckley WE, et al. Factors associated with anterior cruciate ligament injury: history in female athletes. J Sports Med Phys Fit. 2007;47:446-454 [PubMed] [Google Scholar]
- 23. LaFortune MA, Cavanagh PR, Sommer HJ, et al. Foot inversion-eversion and knee kinematics during walking. J Orthop Res. 1994;12(3):412-420 [DOI] [PubMed] [Google Scholar]
- 24. Loudon JK, Jenkins W, Loudon KL. The relationship between static posture and ACL injury in female athletes. J Orthop Sports Phys Ther. 1996;24(2):91-97 [DOI] [PubMed] [Google Scholar]
- 25. Magee DJ. Othopedic Physical Assessment. 2nd ed. Philadelphia, PA: WB Saunders; 1992 [Google Scholar]
- 26. Markolf KL. Direct measurement of resultant forces in the anterior cruciate ligament. J Bone Joint Surg Am. 1990;72-A:557-567 [PubMed] [Google Scholar]
- 27. Markolf KL, O’Neil G, Jackson SR, et al. Effects of applied quadriceps and hamstrings muscle loads on forces in the anterior and posterior cruciate ligaments. Am J Sports Med. 2004;32(5):1144-1149 [DOI] [PubMed] [Google Scholar]
- 28. McClay I, Manal K. Coupling parameters in runners with normal and excessive pronation. J Appl Biomech. 1997;13:109-125 [Google Scholar]
- 29. Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Jt Surg. 1987;69(5):745-749 [PubMed] [Google Scholar]
- 30. Nguyen AD, Shultz SJ. Sex differences in lower extremity posture. J Orthop Sports Phys Ther. 2007;37(7):389-398 [DOI] [PubMed] [Google Scholar]
- 31. Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 2nd ed. Upper Saddle River, NJ: Prentice Hall; 2000 [Google Scholar]
- 32. Ramesh R, VonArx O, Azzopardi T, et al. The risk of anterior cruciate ligament rupture with generalised joint laxity. J Bone Jt Surg. 2005;87-B:800-803 [DOI] [PubMed] [Google Scholar]
- 33. Rosene JM, Fogarty TD. Anterior tibial translation in collegiate athletes with normal anterior cruciate ligament integrity. J Athl Train. 1999;34(2):93-98 [PMC free article] [PubMed] [Google Scholar]
- 34. Rozzi SL, Lephart SM, Gear WS, et al. Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am J Sports Med. 1999;27(3):312-319 [DOI] [PubMed] [Google Scholar]
- 35. Scerpella TA, Stayer TJ, Makhuli BZ. Ligamentous laxity and noncontact anterior cruciate ligament tears: a gender-based comparison. Orthopaedics. 2005;28(7):656-660 [DOI] [PubMed] [Google Scholar]
- 36. Sharma L, Song JS, Felson DT, et al. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286(2):188-195 [DOI] [PubMed] [Google Scholar]
- 37. Shultz SJ, Carcia CR, Gansneder BG, et al. The independent and interactive effects of navicular drop and quadriceps angle on neuromuscular responses to a weightbearing perturbation. J Ath Train. 2006;41(3):251-259 [PMC free article] [PubMed] [Google Scholar]
- 38. Shultz SJ, Carcia CR, Perrin DH. Knee joint laxity affects muscle activation patterns in the healthy knee. J Electromyogr Kinesiol. 2004;14:475-483 [DOI] [PubMed] [Google Scholar]
- 39. Shultz SJ, Kirk SE, Sander TC, et al. Sex differences in knee laxity change across the female menstrual cycle. J Sports Med Phys Fit. 2005;45(4):594-603 [PMC free article] [PubMed] [Google Scholar]
- 40. Shultz SJ, Nguyen A. Bilateral asymmetries in clinical measures of lower-extremity anatomic characteristics. Clin J Sport Med. 2007;17(5):357-361 [DOI] [PubMed] [Google Scholar]
- 41. Shultz SJ, Nguyen A, Schmitz RJ. Differences in lower extremity anatomical and postural characteristics in males and females between maturation groups. J Orthop Sports Phys Ther. 2008;38(3):137-149 [DOI] [PubMed] [Google Scholar]
- 42. Shultz SJ, Nguyen A, Windley TC, et al. Intratester and intertester reliability of clinical measures of lower extremity anatomical alignment. Implications for multicenter studies. Clin J Sports Med. 2006;16:155-161 [DOI] [PubMed] [Google Scholar]
- 43. Shultz SJ, Shimokochi Y, Nguyen A, et al. Nonweightbearing anterior knee laxity is related to anterior tibial translation during transition from nonweightbearing to weightbearing. J Orthop Res. 2006;24(3):516-523 [DOI] [PubMed] [Google Scholar]
- 44. Shultz SJ, Shimokochi Y, Nguyen A, et al. Measurement of varus-valgus and internal-external rotational knee laxities in vivo. Part II: relationship with anterior-posterior and general joint laxity in males and females. J Orthop Res. 2007;25(8):989-996 [DOI] [PubMed] [Google Scholar]
- 45. Staheli LT. Torsional deformity. Ped Clinics North Am. 1977;24(4):799-811 [DOI] [PubMed] [Google Scholar]
- 46. Stuberg W, Temme J, Kaplan P, et al. Measurement of tibial torsion and thigh-foot angle using goniometry and computed tomography. Clin Ortho Rel Res. 1991;272:208-212 [PubMed] [Google Scholar]
- 47. Trimble MH, Bishop MD, Buckley BD, et al. The relationship between clinical measurements of lower extremity posture and tibial translation. Clin Biomech. 2002;17:286-290 [DOI] [PubMed] [Google Scholar]
- 48. Uhorchak JM, Scoville CR, Williams GN, et al. Risk factors associated with noncontact injury of the anterior cruciate ligament. Am J Sports Med. 2003;31(6):831-842 [DOI] [PubMed] [Google Scholar]
- 49. VanderEsch M, Steultjens M, Wieringa H, et al. Structural joint changes, malalignment, and laxity in osteoarthritis of the knee. Scand J Rheumatol. 2005;34:298-301 [DOI] [PubMed] [Google Scholar]
- 50. Woodford-Rogers B, Cyphert L, Denegar CR. Risk factors for anterior cruciate ligament injury in high school and college athletes. J Athl Train. 1994;29(4):343-346 [PMC free article] [PubMed] [Google Scholar]