Abstract
Herein, we report 3 cases of Behçet syndrome that were accompanied by intracardiac thrombus. The 1st patient was a 30-year-old man who presented with dyspnea; a right atrial thrombus was identified upon transthoracic echocardiography. The 2nd patient was a 52-year-old man who was admitted for dyspnea; transthoracic echocardiography revealed an echogenic mass in the right ventricle. The 3rd patient was a 23-year-old man who was hospitalized for hemoptysis; the diagnosis of pulmonary embolism was made, and right ventricular thrombosis was found.
Because these patients had no hemodynamic compromise, medical management consisting of immunosuppressive and anticoagulative therapy was adopted. This treatment resulted in complete dissolution of the thrombi.
Key words: Anti-inflammatory agents; anticoagulants; Behçet syndrome/complications/drug therapy; colchicine/therapeutic use; cyclophosphamide/therapeutic use; embolism, pulmonary; pulmonary artery; thrombosis/drug therapy/epidemiology/etiology
Behçet syndrome is a multisystemic, chronic, inflammatory disorder of unknown cause. It is characterized by recurrent buccal aphthosis, genital ulcers, and uveitis with hypopyon. The mean age at which it occurs is 20 to 30 years; men are 2 to 5 times more often affected than women.1
Additional manifestations in other locations (skin, joints, gastrointestinal tract, genitourinary tract, central nervous system, cardiovascular system, and lungs) can appear and can influence the clinical course and prognosis. Although cardiac involvement during Behçet syndrome is uncommon and intracardiac thrombosis is exceptional, we report here 3 illustrative cases collected at our institution in Rabat, Morocco.
Case Reports
Patient 1
In October 2000, a 30-year-old man with Behçet syndrome was hospitalized for dyspnea that had been evolving for the past 2 months. A diagnosis of Behçet syndrome had been established 3 years earlier, on the basis of mucocutaneous lesions and gastrointestinal disorders, then had been treated with colchicine and corticosteroids.
Physical examination of the patient revealed edema of the face and neck, along with prominent superficial collateral veins over the thorax. The electrocardiogram, chest radiograph, and laboratory test results were normal.
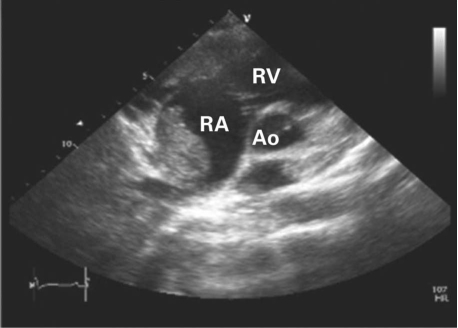
Transthoracic echocardiography showed a homogeneous hyperechoic and sessile mass, 70 × 45 mm in size, attached to the right atrial septum (Fig. 1). These echocardiographic findings were strongly suggestive of a right atrial thrombus. Diagnostic catheterization showed the seat of the thrombosis to be a calcified and thrombosed superior vena cava.
Fig. 1 Patient 1. Transthoracic echocardiography (parasternal short-axis view) shows a cardiac mass in the right atrium (RA). Ao = aorta; RV = right ventricle
We chose a conservative treatment: heparin 500 UI/kg/d for 5 days and an oral anticoagulant (acenocoumarol, a vitamin K antagonist, 3mg/d), methylprednisolone (1 g/day for 3 days) followed by oral prednisone (1 mg/kg/d) and oral cyclophosphamide (1 g/mo) for 6 months, in association with colchicine (1 mg/d). The thrombus in the right atrium decreased substantially in size. At 4 months' follow-up, there was complete resolution of the thrombus in the right atrium and the superior vena cava.
Patient 2
In January 2005, a 52-year-old man with a history of oral ulcers and recurrent phlebitis of the left femoral vein was admitted because of dyspnea (New York Heart Association functional class III).
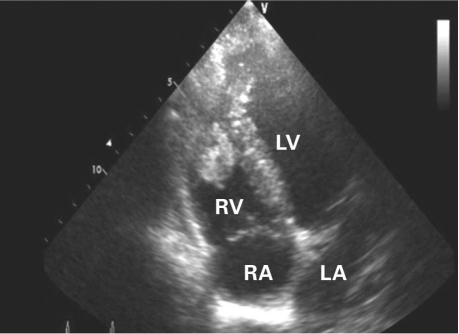
The results of the physical examination were normal. A chest radiograph revealed reticular lung markings and mediastinal lymphadenopathy. Transthoracic echocardiography showed a hyperechoic and homogenous mass, 35 × 30 mm in size and attached at the right ventricular apex (Fig. 2). We diagnosed Behçet syndrome on the basis of the patient's history of recurrent oral ulcers and vascular lesions, a positive pathergy test, and positive human leukocyte antigen (HLA)-B51 serologic typing.
Fig. 2 Patient 2. Transthoracic echocardiography (apical 4-chamber view) shows a cardiac mass in the right ventricle (RV). LA = left atrium; LV = left ventricle; RA = right atrium
The patient was given a bolus of intravenous methylprednisolone (1 g/d for 3 days) followed by oral prednisone (1 mg/kg/d) and oral cyclophosphamide (1 g/mo for 6 mos); simultaneously, we administered oral acenocoumarol (2 mg/d) to maintain an international normalized ratio (INR) between 2 and 3. Resolution of the thrombus was achieved by the time of the 6-month follow-up visit.
Patient 3
In April 2006, a 23-year-old man, with a history of recurrent oral and genital ulcers, was admitted for investigation of iterative abundant hemoptysis. Clinical examination found penile and scrotal scarring and minor aphthae on the oral mucosa. Chest radiography showed hilar enlargement and ill-defined pulmonary nodular opacities.
Computed tomography of the thorax revealed vascular-like nodular formations. Angiography showed an aneurysm in the pulmonary bifurcation and a very peripheral, thrombosed 2nd aneurysm.
Transthoracic echocardiography revealed an echogenic mass in the right ventricle, 20 × 21 mm in size. The right cavities of the heart were dilated, due to moderate pulmonary artery hypertension. Laboratory tests revealed an inflammatory syndrome (C-reactive protein, 68 mg/L; erythrocyte sedimentation rate, 110 min) and positive HLA-B51 serologic typing.
Treatment progressed favorably under a regimen of oral colchicine (1 mg/d); a bolus of intravenous methylprednisolone (1 g/d for 3 days) followed by an oral maintenance dose of methylprednisolone (1 mg/kg/d), in addition to oral cyclophosphamide (1 g/mo) and anticoagulation with acenocoumarol (2 mg/d). At the 3-month follow-up visit, both the pulmonary artery aneurysm and the intracardiac thrombus had disappeared.
Discussion
The prevalence of vascular involvement in Behçet syndrome varies from 7.7% to 43%, in accordance with the ethnicity of the population under study.2
Pathogenesis. The pathogenic mechanism underlying the thrombotic tendency among patients with Behçet syndrome is not well known. Several causal factors have been suggested:
Endothelial cell ischemia or disruption, which leads to enhancement of platelet aggregation.3–5
The presence of antiphospholipid antibodies, which is reported to occur in 18% of cases.3–5
The presence of prothrombotic factors, such as deficiencies of protein S, protein C, and antithrombin.6
Elevated von Willebrand factor antigen levels, which have recently been observed in association with Behçet syndrome.7
Fibrinolysis anomaly due to endothelial cell damage after the deposition of antigen-antibody (immune complex disease).8
Homozygosis for the factor V Leiden mutation or the prothrombin gene, which increases the risk of thrombosis by a factor of 6 or 3, respectively.5,6,9
Epidemiology. Thrombosis is the most frequent lesion.10 Usually, arterial thrombosis occurs later than does venous thrombosis.11 Thrombosis is very often associated with (and predictive of) ocular involvement in Behçet syndrome.2
Despite the high incidence of vascular damage in this disease (more than one third of patients experience it), cardiac involvement is uncommon.12 It varies from 1% to 5% in clinical series and was 16.5% in a register of Behçet autopsy cases in Japan.3
Intracardiac thrombi are exceptional. From the 1st description by Buge in 197713 through Hammami's brief review of the literature in 2005,9 only about 50 cases had been reported—some associated with endomyocardial fibrosis and some not. The appearance of such thrombi often precedes other manifestations of Behçet syndrome, and it is rarely inaugural.14 Intracardiac thrombus is associated with deep vein thrombosis and with thrombosis of the vena cava, respectively, in 50% and 22% of cases.3,14,15 Thrombus can also be associated with an aneurysm of the pulmonary artery, as it was in our patient 3, or with endomyocardial fibrosis.16
Diagnosis. Transesophageal and transthoracic echocardiography are generally sufficient to enable a diagnosis of cardiac thrombosis. The mass is usually heterogeneous and echogenic, involving the ventricles rather than the atria15 and the right heart more often than the left.3 In our patient 1, the thrombus was found in the right atrium, whereas it was found in the right ventricle in our other 2 patients. Ultrasonic imaging might suggest a differential diagnosis—a large vegetation, for example, or an intracardiac tumor such as a myxoma, or endomyocardial fibrosis—but the clinical context helps to clarify the diagnosis.17 In any event, the resolution of the mass under anticoagulant or antiplatelet therapy establishes a retrospective diagnosis, because it distinguishes thrombus from tumor.3
Therapy. There is no consensus regarding the treatment of cardiac thrombosis in association with Behçet syndrome. The aim of treatment is to control the underlying disease and to resolve the cardiac thrombus. Anticoagulant and antithrombotic agents are the 1st line of therapy.5 However, an associated aneurysm of the pulmonary artery—especially the presence of large or bilateral aneurysms—makes the use of these therapies difficult because of the risk of a devastating hemoptysis.
Surgery might become necessary in cases of cardiac thrombosis that is massive, is recurrent after medical treatment, or is associated with cardiac congestion.18
In the cases presented here, we find that Behçet syndrome was controlled by immunosuppressive drugs and corticosteroids in our patients 2 and 3. In all of our patients, we were able to obtain complete resolution of cardiac thrombosis by means of 3 to 6 months of anticoagulant treatment with vitamin K antagonists (target INR range, 2–3).
Conclusion
We conclude that thrombi, especially in the right-heart cavities, are possible complications of Behçet syndrome that can lead to pulmonary embolism. Early echocardiography is advisable for the detection of cardiac involvement, and medical treatment should be the 1st choice of therapy.
Footnotes
Address for reprints: Fedoua El louali, MD, 16 I 8 Rue Narjiss, Hay Riad, Rabat, Morocco
E-mail: f.ellouali@hotmail.com
References
- 1.Behcet H. Uber rezidivierende, aphthose, durch ein virus verursachte geschwure im mund, am auge und an den genitalien [in German]. Dermatol Wochenschr 1937;105:1152–7.
- 2.Ames PR, Steuer A, Pap A, Denman AM. Thrombosis in Behcet's disease: a retrospective survey from a single UK centre. Rheumatology (Oxford) 2001;40(6):652–5. [DOI] [PubMed]
- 3.Wechsler B, Du LT, Kieffer E. Cardiovascular manifestations of Behcet's disease [in French]. Ann Med Interne (Paris) 1999;150(7):542–54. [PubMed]
- 4.Baykan M, Celik S, Erdol C, Baykan EC, Durmus I, Bahadir S, et al. Behcet's disease with a large intracardiac thrombus: a case report. Heart 2001;85(4):E7. [DOI] [PMC free article] [PubMed]
- 5.Mogulkoc N, Burgess MI, Bishop PW. Intracardiac thrombus in Behcet's disease: a systematic review. Chest 2000;118 (2):479–87. [DOI] [PubMed]
- 6.Akar N. Site specific mutagenesis: usage for the mutation detection in thrombosis. Turk J Haematol 1998;15:123–4.
- 7.Kiraz S, Ertenli I, Ozturk MA, Haznedaroglu IC, Celik I, Calguneri M. Pathological haemostasis and “prothrombotic state” in Behcet's disease. Thromb Res 2002;105(2):125–33. [DOI] [PubMed]
- 8.Gul A, Ozbek U, Ozturk C, Inanc M, Konice M, Ozcelik T. Coagulation factor V gene mutation increases the risk of venous thrombosis in Behcet's disease. Br J Rheumatol 1996;35 (11):1178–80. [DOI] [PubMed]
- 9.Hammami S, Mahjoub S, Ben-Hamda K, Brahem R, Gamra H, Ben Farhat M. Intracardiac thrombus in Behcet's disease: two case reports. Thromb J 2005;3:9. [DOI] [PMC free article] [PubMed]
- 10.Houman MH, Ben Ghorbel I, Khiari Ben Salah I, Lamloum M, Ben Ahmed M, Miled M. Deep vein thrombosis in Behcet's disease. Clin Exp Rheumatol 2001;19(5 Suppl 24):S48–50. [PubMed]
- 11.Harmouche H, Tazi Mezalek Z, Adnaoui M, Aouni M, Mohattane A, Maaouni A, Berbich A. Association of pulmonary artery aneurysm, right heart thromboses and antiphospholipid antibodies in Behcet's disease [in French]. Rev Med Interne 1998;19(7):512–5. [DOI] [PubMed]
- 12.Koc Y, Gullu I, Akpek G, Akpolat T, Kansu E, Kiraz S, et al. Vascular involvement in Behcet's disease. J Rheumatol 1992; 19(3):402–10. [PubMed]
- 13.Buge A, Escourolle R, Chomette G, Rancurel G, Dechy H, Hauw JJ, et al. Behcet's disease with neurologic manifestations and endocardial fibrosis of the right heart. Anatomoclinical study of a case [in French]. Ann Med Interne (Paris) 1977;128(5):411–9. [PubMed]
- 14.el-Ramahi KM, Fawzy ME, Sieck JO, Vanhaleweyk G. Cardiac and pulmonary involvement in Behcet's disease. Scand J Rheumatol 1991;20(5):373–6. [DOI] [PubMed]
- 15.Islim IF, Gill MD, Situnayake D, Watson RD. Successful treatment of right atrial thrombus in a patient with Behcet's disease. Ann Rheum Dis 1994;53(8):550–1. [DOI] [PMC free article] [PubMed]
- 16.Houman M, Ksontini I, Ben Ghorbel I, Lamloum M, Braham A, Mnif E, Miled M. Association of right heart thrombosis, endomyocardial fibrosis, and pulmonary artery aneurysm in Behcet's disease. Eur J Intern Med 2002;13(7):455. [DOI] [PubMed]
- 17.Marc K, Iraqui G, Jniene A, Benamor J, Bourkadi JE. Intracardiac thrombus and pulmonary artery aneurysm in Behcet's disease [in French]. Rev Mal Respir 2008;25(1):69–72. [DOI] [PubMed]
- 18.Darie C, Knezinsky M, Demolombe-Rague S, Pinede L, Perinetti M, Ninet JF, Ninet J. Cardiac pseudotumor revealing Behcet's disease [in French]. Rev Med Interne 2005;26(5): 420–4. [DOI] [PubMed]