Several continuous-flow left ventricular assist devices (LVADs) have been developed over the last decade and are now in various stages of clinical validation. Compared with their pulsatile-output predecessors, continuous-flow LVADs are smaller, quieter, and easier to implant. Perhaps of even greater importance, however, is the fact that—absent flexible membranes, pusher plates, and valves—these newer pumps are significantly less susceptible to mechanical wear. Despite these advances, many patients still suffer significant morbidity or even death in association with the implantation procedure itself. Therefore, the field is still viewed by many as somewhat experimental, and it remains an option of last resort in very-late-stage patients. New implantation techniques that decrease operative morbidity might improve results to the extent that patients are referred earlier in the course of their illness, which in turn would further improve results.
Early work directed at LVAD implantation without cardiopulmonary bypass (CPB) has resulted in reports of small series from several groups.1–4 Although there are no randomized prospective trials as yet, early results suggest that the technique has merit. That notwithstanding, off-pump LVAD implantation is still a technically challenging procedure with potential for misadventure, especially when compared with LVAD implantation with CPB.
LVAD Implantation with CPB. In conventional LVAD implantation with CPB, normothermia is maintained and the heart continues to beat while a cylindrical blade excises a core of myocardium from the apex. This is readily accomplished in the decompressed, bypassed heart. The LVAD sewing ring is then sutured to the margins of the apical hole. During these maneuvers, neither hemostasis nor hemodynamic stability is difficult to maintain, due to maintenance of CPB and to the availability of a cardiotomy sucker. Only when the LVAD is secured in position is the ventricle pressurized and are efforts made to wean the patient from CPB. In this way, LVAD implantation with CPB has become a very simple and safe procedure.
Off-Pump LVAD Implantation: Current Technique. In contrast, the placement of a HeartMate® II LVAD (Thoratec Corporation; Pleasanton, Calif) without CPB—using the current, unmodified technique—presents several challenges. The heart must be reflected to the right to expose the apex, without compromising hemodynamic stability. Typically, deep pericardial sutures or lap pads are used to facilitate this. In some instances, hemodynamic stability cannot be maintained, and CPB must be initiated.
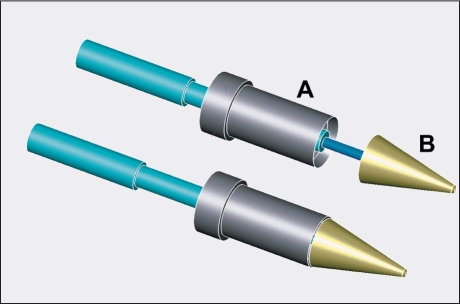
Once the apex is successfully exposed, the LVAD sewing ring is sutured circumferentially to the intact epicardial surface of the heart with multiple discrete pledgeted sutures. At this point, a cruciate transmural incision is made in the center of the apical heart muscle as circumscribed by the sewing ring, in preparation for removing a cylindrical plug of myocardium. The cruciate incision must be adequate to enable the conical anvil of a myocardial punch (Jarvik Heart, Inc.; New York, NY) to be inserted completely into the left ventricular (LV) cavity (Fig. 1). Because the external diameter of the conical anvil is only slightly smaller than the internal diameter of the HeartMate II sewing ring, the cruciate incision must be fairly generous.
Fig. 1 Current technique. Many coring devices used for off-pump LVAD insertion consist of a cylindrical knife (A) that follows the axis of a conical anvil (B). A transmural cruciate incision is generally required to insert the anvil into the left ventricular chamber. Once the anvil has entered the left ventricle, the blade is advanced, excising a cylinder of heart muscle and trapping it between blade and anvil.
LVAD = left ventricular assist device
Once the incision is made, the resulting hole is quickly obturated by the surgeon's finger, which both minimizes blood loss and dilates the hole, facilitating insertion of the conical anvil. The finger is rapidly withdrawn and replaced with the myocardial punch, again to minimize hemorrhage. The anvil is manipulated to ensure that it is completely inside the left ventricle. In this way, all 4 quadrants of the cruciate incision are in position to be excised by the cylindrical coring knife. While holding the anvil in position, the surgeon advances the coring knife through the myocardium with a twisting motion, until the metal blade is felt to strike the back of the plastic anvil. While holding the blade tightly against the anvil to maintain capture of the excised myocardium, the surgeon rapidly removes the myocardial plug and replaces it with a finger, both to minimize hemorrhage and to check for any retained myocardial fragments, which will be present if one of the quadrants was missed by the cylindrical blade. If the hole is adequate, the finger is rapidly withdrawn and replaced with the inflow cannula of the LVAD, which is secured in position with a ligature or band-tie.
Although this procedure is technically feasible, it generally requires 2 cardiac surgeons and some daring maneuvers. One must be ready to institute CPB if blood pressure cannot be maintained while the heart is elevated, if uncontrollable hemorrhage occurs, or if myocardial fragments are retained after coring. Moreover, to prevent fatal hemorrhage, several steps involve rapid exchanges: between the knife and the surgeon's finger, the finger and the coring knife, the coring knife and the finger once again, and the finger and the LVAD. Tools and techniques that eliminate some of these steps and facilitate the creation of a clean circular hole without retained myocardial fragments may be of value.
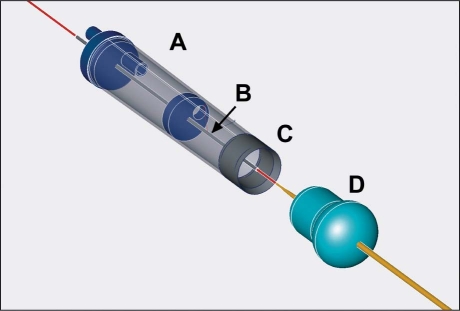
Off-Pump LVAD Implantation: New Technique. We have designed a hybrid system that comprises multiple components and a new, modified off-pump LVAD implantation technique that may accomplish many of these objectives. The system consists of a vacuum stabilizer that holds the sewing ring in position while exposing the LV apex, an over-the-wire vacuum-assisted myocardial coring tool, and an endoventricular occlusion balloon, placed under fluoroscopic guidance, that prevents hemorrhage while obviating the need for rapid exchanges (Fig. 2).
Fig. 2 Investigative technique. The vacuum-assisted coring tool is advanced through the heart wall over a guidewire. The transparent chamber (A) enables visualization of the excised myocardial tissue, which is pulled into the chamber by suction. The small metal tube (B) that is coaxial with respect to the coring tool prevents the cylindrical blade (C) from coming into contact with the endoventricular occlusion balloon (D), which is placed retrograde via femoral arterial access. After complete excision of the myocardial plug has been confirmed, the coring tool is withdrawn, which pulls the occlusion balloon into position, minimizing hemorrhage. When the LVAD is inserted, the balloon is displaced into the left ventricle, then deflated and removed through the femoral arterial sheath.
LVAD = left ventricular assist device
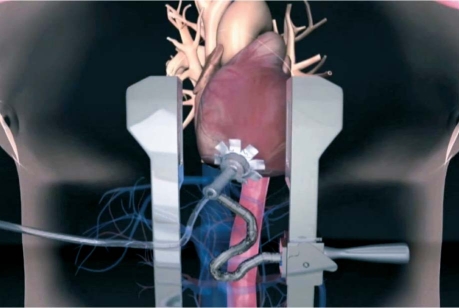
The vacuum stabilizer is similar to the commercially available devices developed to position the heart during off-pump coronary artery bypass surgery. It is well known that the heart tolerates repositioning better if LV and right ventricular end-diastolic volumes are not affected. When laparotomy pads are placed behind the heart to elevate the apex, pressure on the lateral wall of the LV can decrease LV filling. If, instead, the apex is elevated with a suction device, filling is not compromised and hemodynamics can more readily be maintained. The suction device we have developed is unique in that it is designed to fit coaxially down the center of the LVAD sewing ring. In this way, it does not interfere with suturing the sewing ring to the surface of the heart, and it holds the sewing ring in position during the suturing process (Fig. 3).
Fig. 3 Investigative technique. The LVAD sewing ring is held in position on the cardiac apex by a coaxial suction device that stabilizes the sewing ring, exposes the cardiac apex, and minimizes hemodynamic impact.
LVAD = left ventricular assist device
Once the sewing ring has been sutured securely in place, an 18G angiocatheter is used to introduce a 260-cm, .035-in J-tipped guidewire into the LV. Under fluoroscopic guidance, the wire is advanced across the aortic valve, around the aortic arch, and down the descending and abdominal aorta to the iliac bifurcation. A wire snare is then inserted through a 9F sheath in the left femoral artery and is used to capture the J-tipped end of the guidewire and deliver it through the femoral arterial sheath. At this point, 100 cm of the J-tipped wire protrudes from the femoral sheath; the other end of the wire protrudes from the LV apex, axisymmetric to the sewing ring.
The endoventricular occlusion balloon is then threaded over the wire, up the femoral sheath, across the aortic valve, and into the LV. The balloon is aggressively de-aired and filled with 30 cc of dilute contrast. The geometry of the balloon integrates an oblate sphere with an elongate cylinder. The cylindrical portion is intended to obturate the hole created in the ventricular wall by the coring device; the spherical portion is intended to keep the balloon from being ejected through the hole during cardiac systole.
The vacuum-assisted coring device is then threaded over the wire protruding from the ventricular apex. Unlike the currently available off-pump myocardial punch, there is no conical anvil to insert into the LV, so no cruciate incision is necessary. Instead, suction is used to capture the excised core of myocardium and pull it into a clear cylindrical housing, where complete excision can be confirmed visually. Thus, a perfect cylinder of myocardium is always excised, with decreased likelihood of retained fragments. In addition, the vacuum-assisted coring device has an integrated hypotube that runs coaxially down the center and accommodates the guidewire. In this manner, a standoff is maintained between the cylindrical blade and the thin-walled balloon: both are threaded over the same wire (albeit from opposite ends), which makes it impossible for the blade to rupture the balloon. Once the myocardial core has been drawn into the coring device, the coring device is removed, which pulls the endoventricular occlusion balloon into the sewing ring. In this way, hemostasis is maintained throughout the process without need for rapid exchanges. Because the vacuum-assisted coring device is applied to the intact heart without need for a cruciate incision, the core is excised as a single cylindrical piece, ensuring a clean cylindrical hole without retained fragments. Moreover, while the endoventricular occlusion balloon is in place, the LV cavity can be transilluminated through the balloon, and the hole can be examined. It then becomes a simple task to insert the LVAD inflow cannula and displace the balloon into the LV, after which it is deflated and removed through the femoral arterial sheath.
We have performed a number of animal studies with the system, and it seems to be of merit. Although one might question why we think that avoiding CPB will be of significant value in LVAD implantation, we are hopeful that this procedure will enable safe, rapid, and reproducible implantation of LVADs without CPB.
Footnotes
Address for reprints: William E. Cohn, MD, Director, Minimally Invasive Surgical Technology, Texas Heart Institute at St. Luke's Episcopal Hospital, MC 2–114A, P.O. Box 20345, Houston, TX 77225–0345
E-mail: wcohn@heart.thi.tmc.edu
Presented at the 18th Annual Texas Heart Institute Summit, “Heart Failure in the Next Decade: The Impact of Novel Therapies on Current Treatment Strategies,” 5–6 March 2010, Houston.
Program Director: Roberta C. Bogaev, MD, FACC
References
- 1.Frazier OH, Gregoric ID, Cohn WE. Initial experience with non-thoracic, extraperitoneal, off-pump insertion of the Jarvik 2000 Heart in patients with previous median sternotomy. J Heart Lung Transplant 2006;25(5):499–503. [DOI] [PubMed]
- 2.Cohn WE, Frazier OH. Off-pump insertion of an extracorporeal LVAD through a left upper-quadrant incision. Tex Heart Inst J 2006;33(1):48–50. [PMC free article] [PubMed]
- 3.Selzman CH, Sheridan BC. Off-pump insertion of continuous flow left ventricular assist devices. J Card Surg 2007;22 (4):320–2. [DOI] [PubMed]
- 4.Sun BC, Firstenberg MS, Louis LB, Panza A, Crestanello JA, Sirak J, Sai-Sudhakar CB. Placement of long-term implantable ventricular assist devices without the use of cardiopulmonary bypass. J Heart Lung Transplant 2008;27(7):718–21. [DOI] [PubMed]