Abstract
Background
A periacetabular osteotomy,indicated for adults or adolescents requiring correction of congruency and containment of the femoral head, is a common surgical procedure to address developmental dysplasia of the hip.
Objectives
To describe developmental hip dysplasia, a surgical procedure performed to address the condition, as well as therapeutic exercise and functional progression principles utilized to return a patient to tennis following periacetabular osteotomy.
Case Description
The patient was a 14 year-old female who underwent a Ganz periacetabular osteotomy of the right pelvis due to developmental dysplasia of the hip. Post-operative outpatient physical therapy consisted of strengthening of the hip, thigh, and core musculature, as well as activities to increase muscular and cardiovascular endurance, anaerobic conditioning, lower extremity proprioception, and soft tissue length. A functional progression program to return to tennis was also provided.
Outcomes
The patient was seen in outpatient physical therapy for a total of 34 visits over the course of 42 weeks. Results of a Lower Extremity Functional Scale (LEFS) indicated that heavy activities of daily living, as well as recreational and sporting activities, were improved following the post-operative rehabilitation program.
Discussion
The role of the physical therapist is vital in prescribing and progressing activity levels to facilitate return of function following this periacetabular osteotomy. Surgery that is technically well performed followed by a comprehensive rehabilitation program can allow for resumption of pre-morbid activities, enhancement of the quality of life, and return to sports activities.
Keywords: functional progression, tennis, congenital hip dysplasia
INTRODUCTION
Hip problems in the developing youngster can be congenital or acquired and are frequently encountered by the physical therapist. Sports physical therapists may be comfortable in dealing with acquired hip conditions in active youth, but not as familiar with treating congenital hip dysfunction. On the other hand, pediatric physical therapists may be at ease addressing congenital hip issues but not as well versed in caring for acquired macro or microtrauma of the hip in active, normally developing youngsters. The generalist physical therapist may be somewhere in between these two extremes. The purpose of this case report is to describe developmental hip dysplasia, a surgical procedure performed to address this condition, as well as therapeutic exercise and functional progression principles utilized to return a patient to tennis following periacetabular osteotomy.
Developmental Dysplasia of the Hip
Conditions involving the hip joint in the skeletally immature youngster range from joint dysplasia to joint subluxation and dislocation. Traditionally, all of these conditions have been collectively referred to as congenital dysplasia of the hip; however, the term developmental dysplasia of the hip (DDH) has become more acceptable.1 Developmental dysplasia of the hip more accurately describes situations when hip problems that may not be noticed at birth, become apparent as a child matures and begins to bear weight in a standing position.
The epidemiology, etiology, examination and treatment of DDH are well documented.1–4 In addition to the clinical physical examination, standard anterior-posterior plain film radiographs of the pelvis are helpful in the diagnosis of DDH. Abnormal findings on plain film radiographs suggestive of DDH include the delayed appearance of ossification centers of the hip and pelvis beyond six months, as well as an abnormal relationship between the developing femoral neck and pelvis. As the youngster matures, in addition to the traditional anterior-posterior view of the pelvis, a weight bearing view with the pelvis rotated 25° toward the x-ray beam (faux profile view) may also be helpful in quantifying the relationship between the developing femoral head and the acetabulum.3,5–9
Surgical Intervention for DDH
Many individuals with DDH develop through childhood and adolescence without symptoms. Hip pain when present is typically due to high stresses on the acetabular rim resulting in articular cartilage damage with subsequent increased stresses on underlying subchondral bone. When infants with DDH are not diagnosed until late, or when previous treatment attempts in diagnosed infants are not successful, surgical intervention is indicated. Untreated acetabular dysplasia is the second most common cause of secondary osteoarthrosis with degenerative joint disease from pathological joint-loading forces becoming symptomatic before the age of 50 in 25% to 50% of patients with DDH.10 Surgical options entail capsulorrhaphy, femoral derotation and varisation osteotomy, periacetabular osteotomy, or shelf arthroplasty, of the pelvis. The primary goal of the various procedures is to provide coverage of the developing femoral head.11–18
The Ganz triple osteotomy, also known as the Bernese osteotomy, is a common surgical procedure to address DDH. The Ganz procedure provides for the large bony corrections required to cover the femoral head in all needed directions including lateral rotation, anterior rotation, and medialization of the hip center.13 Ganz first performed his periacetabular osteotomy in 1983.16 The Ganz osteotomy is indicated in adults or adolescents with closed physes who have dysplastic hips requiring correction of congruency and containment of the femoral head. In most cases, the opening of the acetabulum lies in excessive anteversion from the sagittal plane.
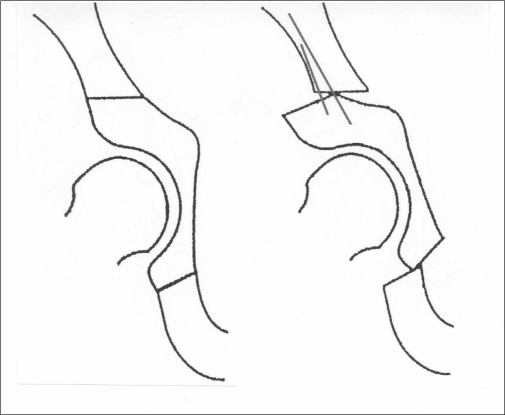
The purpose of the Ganz procedure is to reorient the position of the acetabulum anteriorly and laterally to gain greater coverage of the femoral head and bring the roof of the acetabulum from an oblique position to a more horizontal position through a series of cuts in the innominate bones (Figure 1). Advantages of this periacetabaular osteotomy include using only one approach, the potential for significant correction in all directions (including medial and lateral planes), the posterior column of the hemipelvis remains mechanically intact which allows immediate crutch walking with minimal internal fixation, the shape of the true pelvis is unaltered permitting a normal child delivery later in life, and retaining the hip's center of rotation. Complications of the Ganz procedure include interarticular extension of the osteotomy, temporary femoral nerve palsy, insufficient or excessive overcorrection, secondary subluxation of the femoral head, osteonecrosis, nonunion, heterotopic ossification, vascular compromise or loss of fixation. 6,15,18
Figure 1.
Two-dimensional view of acetabular re-positioning before (A) and after (B) Ganz osteotomy. Note: the roof of the acetabulum has moved more horizontally to cover the femoral head.
CASE DESCRIPTION
History
At the time of the initial physical therapy visit the patient was 15 years old, 68 inches tall, and weighed 129 pounds. The patient was an incoming freshman at a local high school and had previously been involved in recreational and competitive tennis, participating in both singles and doubles.
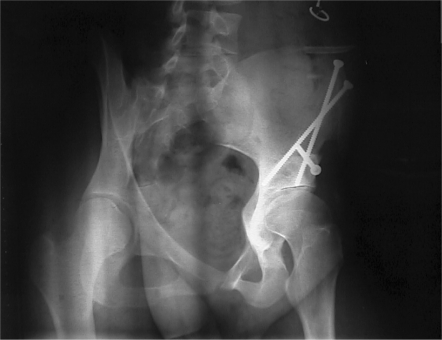
At the age of five months, the patient was diagnosed with bilateral DDH with no occurrence of hip dislocation. Initial treatment for the DDH was via a hip spica cast which was removed at one year of age. Due to complaints of persistently painful clicking in the right hip during childhood the patient underwent a surgical release of the psoas at age ten. The patient was followed by her family physician and local orthopedists but her condition worsened. She was subsequently referred to a regional orthopaedic specialist due to complaints of constant lateral hip pain. Upon reviewing her condition and past history, the surgeon recommended and performed a Ganz periacetabular osteotomy for the right hip. Figures 2 and 3 demonstrate pre- and post-operative radiographs.
Figure 2.
Pre-operative anterior-posterior view (Faux profile) of pelvis and hips demonstrating an increased acetabular index (angle formed by a horizontal line drawn through the inferior part of the ilia and a line drawn across the acetabular roof).
Figure 3.
Post-operative oblique x-ray (Faux profile) of the pelvis and hip demonstrating adequate coverage of the femoral head.
Post-Operative Intervention
The patient had an uneventful hospital stay and after five days was discharged partial weight bearing (PWB) with axillary crutches and a home exercise program of active hip range of motion and gentle isometric hamstring and quadriceps muscle sets. Serial radiographs taken between surgery and the initial physical therapy visit demonstrated normal post-operative findings.
Post-Operative - Week Four
Four weeks following the osteotomy the surgeon referred the patient for outpatient physical therapy for three visits per week for six weeks. Physician orders were to advance weight bearing up to 40 pounds on the involved right lower extremity, strengthening, and range of motion work.
At the initial physical therapy visit, the patient had subjective complaints of minimal hip pain at rest and did note numbness in the thigh. The patient was ambulating PWB with an appropriate gait pattern using axillary crutches. In the sitting position she lacked full knee extension by five degrees due to quadriceps weakness. During the exam, the patient could not transfer from sitting to a supine position on the treatment table without manually assisting the involved leg. Observation of the patient in the supine position revealed quadriceps atrophy and an inability to initiate a straight leg raise. The patient was also unable to initiate gravity resisted abduction in the side-lying position. In the standing position hip abduction was with immediate substitution palpated in the quadratus lumborum. Active range of motion of the hips was measured and these values are found in Table 1. In addition, the patient filled out the Lower Extremity Functional Scale. This scale and the results are reported in the Outcomes Section of this case study.
Table 1.
Active range of motion (in degrees) at initial evaluation
| Motion | Uninvolved Left Hip | Involved Right Hip |
|---|---|---|
| Supine abduction | 0–46 | 0–11 |
| Supine adduction | 0–20 | 0 |
| Seated external rotation | 0–26 | 0–4 |
| Seated internal rotation | 0–48 | 0–12 |
| Supine flexion | 0–111 | 0–55 |
| Standing flexion | 0–115 | 0–40 |
| Prone extension | 0–28 | 0–15 |
Treatment in the outpatient clinic included hip flexor strengthening, open kinetic chain and closed kinetic chain quadriceps strengthening, and functional electrical stimulation for the quadriceps. Open kinetic chain quadriceps work was performed at terminal extension to address her extension lag. Closed kinetic chain strengthening was performed on the Shuttle (Contemporary Design Company, Glacier, WA). The Shuttle is a horizontal sliding carriage that allows the patient to perform perform closed chain activities in a gravity eliminated position. Added resistance from 25 to 200 pounds can be applied to the Shuttle by a series of elastic cords. Added resistance to strengthening activities on the Shuttle for the current patient did not exceed 50 pounds. Efforts to strengthen the gluteus medius were increased with manual resistance and resisted isotonic exercise in the supine position.
Post- Operative - Week Eight
After four weeks of rehabilitation (eight weeks after surgery), the patient returned to the physician. At that time the patient's active standing hip flexion had increased to 90°. Hip extensor strength had increased and the patient was able to perform single leg bridging activities. Quadriceps atrophy persisted (one and one-quarter inch difference eight inches proximal to the knee joint line). However, the patient could actively extend the knee completely, and open chain terminal knee extensions were up to seven pounds of resistance. The patient could inconsistently initiate a straight leg raise but did so with a knee extension lag of greater than 30°. Gait was still PWB with axillary crutches.
After the visit to the surgeon, orders were received to continue outpatient treatment twice a week for six weeks with an emphasis on strengthening (especially with hip extension and abduction) and to increase weight bearing to 60 pounds. Crutch use was to be discontinued before the next scheduled visit with the surgeon in approximately twelve weeks.
Rehabilitation now focused on longer lever arm strengthening of the hip musculature with assisted and substitution free straight leg raises (SLR) and gravity resisted gluteus medius strengthening. Hip flexor stretching was initiated. Core strengthening of the abdominals and paravertebral muscles consisting of crunches, assisted leg lowering, diagonal crunches, and prone body weight resisted extension were instituted and progressed. Lower extremity strengthening and gait activities were begun in waist deep water.
The patient was instructed to progress to full weight bearing (FWB) ambulation with crutches at nine weeks following surgery. The patient admitted she was non-compliant with appropriate weight bearing status and had started to ambulate occasionally at home without crutches. During this time, the patient went on a family vacation and did some swimming and more walking than she had done since surgery. At this time the patient noted an inconsistent non-painful popping in the anterior hip, especially after prolonged weight bearing. It was also during this time that the patient noted increased pain at rest and an inability to lie comfortably on the affected side. The patient denied night pain. Decreased weight bearing restrictions were implemented and enforcement of consistent use of crutches. Strengthening efforts in the clinic and at home were de-emphasized. With these restrictions in activity and consistent use of the crutches, the pain at rest was eliminated. No imaging was performed at this time.
During the course of the next two weeks the patient was able to ambulate FWB with two crutches and was gradually weaned from the crutches to begin full weight bearing gait without an assistive device. The patient demonstrated a slight gluteus maximus lurch with slight trunk extension at heel strike. Gait training along with weight bearing strengthening and balance were instituted. Aerobic and anaerobic conditioning efforts were instituted on the recumbent bike.
Post-Operative - Week Eighteen
At the time of the surgeon's follow-up visit three and a half months post-operatively, despite the increased quadriceps strength, the patient still could not consistently initiate a SLR. No extension lag was present with the eccentric SLR from 90° to 60°, but a lag of five degrees was present from 60° to 0°. The surgeon suggested another month of strengthening prior to allowing a return to tennis and scheduled the patient for a return visit in three months. Clinic visits focused on core and lower extremity strengthening, early functional progression activities, and progressing the functional progression program. Table 2 summarizes the rehabilitation program.
Table 2:
Rehabilitation Summary
| Immediate Post-Op | Pre-Full Weight Bearing | Post-Full Weight Bearing |
|---|---|---|
| Post-Op: Week 4-8 | Post-Op: Week 8-12 | Post-Op: Week 12 |
|
|
|
Functional Progression
Functional progression is a series of sport-specific, basic movement patterns graduated according to difficulty of the skill and the athlete's tolerance.19 The end goal of functional progression is an athlete's timely and safe return to competition. From post-operative week 24 to week 42, the patient was progressed along a continuum of increasingly more difficult activities culminating in her playing tennis.
At week 24, lower extremity efforts began with bilateral non-support activities, jumping side-to-side and front-to-back. Transition to unilateral non-support activities (hopping) was initially performed at a single point until the contralateral hip did not drop indicating adequate dynamic gluteus medius muscle strength. Jumping was followed by alternating single leg hopping on the involved extremity and uninvolved extremity upon command and in place. Again, once this activity was performed without substitution, progression was allowed to hopping side-to-side and front-to-back
Since no healing time concerns existed for the patient's upper extremities, upper extremity tennis drills (forehand and backhand ground, over head returns, serves) could be progressed quickly. Effective power generation for all of these upper extremity movements, however, require force generation and force coupling from the lower extremities and the trunk. The patient was right hand dominant, so forehand ground strokes involving a neutral pelvis transitioning to hip extension and internal rotation were instituted. Backhand ground strokes involving more hip internal rotation followed by right trunk rotation over the fixed pelvis followed. Both of these strokes began with gentle volleys from mid court and were progressed to the baseline. Overhand returns and serves to incorporate more hip extension were also stressed. Emphasis was placed on a neutral spine while minimizing excessive trunk flexion due to concerns of gluteus maximus weakness and fatigue.
From post-operative weeks 26 to 32, figure-of-eights were progressed from full court to half court beginning with a jog and progressing to full speed. Acceleration and deceleration activities in the half court forwards, backwards, and side shuffling were then stressed from weeks 32 to 40 (Figure 4). Once the patient progressed through the acceleration and deceleration drills, she was then instructed to incorporate either a forehand or backhand stroke into the dynamic drills. After the patient was fluid in the acceleration/deceleration activities with twisting strokes, she began to play teammates, first doubles and then singles. When the coach and athlete were comfortable with her level of performance, the patient was allowed to compete. The functional progression program is summarized in Table 3.
Figure 4.
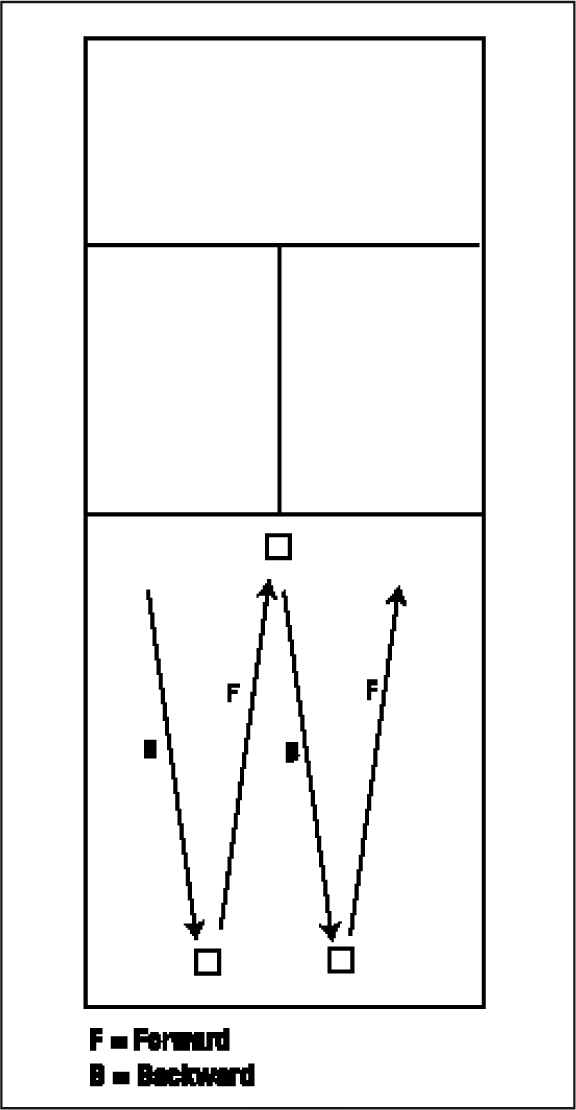
Forward and backward acceleration/deceleration drills on the tennis court. Diagonal sprinting to the net and backpedaling to the backcourt.
Table 3:
Function Progression Summary
| Activity | Dosage | Onset |
|---|---|---|
| Bilateral non-support | ||
| Single plane front-to-back | 3 sets – 2 minutes | Week 24 |
| Single plane side-to-side | 3 sets – 2 minutes | |
| Serving | ||
| Baseline ground strokes | ||
| Unilateral non-support | ||
| Stationary | 3 sets – 1 minute | Week 25 |
| Stationary alternating legs | 3 sets – 1 minute | |
| Single plane front-to-back | 3 sets – 1 minute | |
| Single plane side-to-side | 3 sets – 1 minute | |
| Serving | ||
| Baseline ground strokes | ||
| Figure-eights | ||
| Full court jog | 10 repetitions | Week 26 |
| Full court half-sprint | 10 repetitions | Week 27 |
| Full court sprint | 10 repetitions | Week 28 |
| Half court jog | 10 repetitions | Week 29 |
| Half court half-sprint | 10 repetitions | Week 30 |
| Half court sprint | 10 repetitions | Week 31 |
| Light volleys | ||
| Acceleration/deceleration (sagittal) | ||
| Jog, no racquet | 10 repetitions | Week 32 |
| Half-sprint, no racquet | 10 repetitions | Week 34 |
| Full sprint, no racquet | 10 repetitions | Week 36 |
| Jog, racquet, swing | 10 repetitions | Week 38 |
| Half-sprint, racquet, swing | 10 repetitions | Week 39 |
| Full sprint, racquet, swing | 10 repetitions | Week 40 |
| Volleys | ||
| Acceleration/deceleration (lateral) | ||
| As above | 10 repetitions | Week 40 |
| Doubles tennis | Week 40 | |
| Singles tennis | Week 42 |
OUTCOME
Forty-two weeks transpired from the time of surgery to completion of the functional progression and a return to tennis competition. During this time the patient was seen a total of 34 physical therapy visits. At the time of discharge the patient was performing at a level that allowed her to play number two doubles on her high school tennis team. The patient was also participating in singles tennis at a level the coach rated subjectively superior to before the surgery.
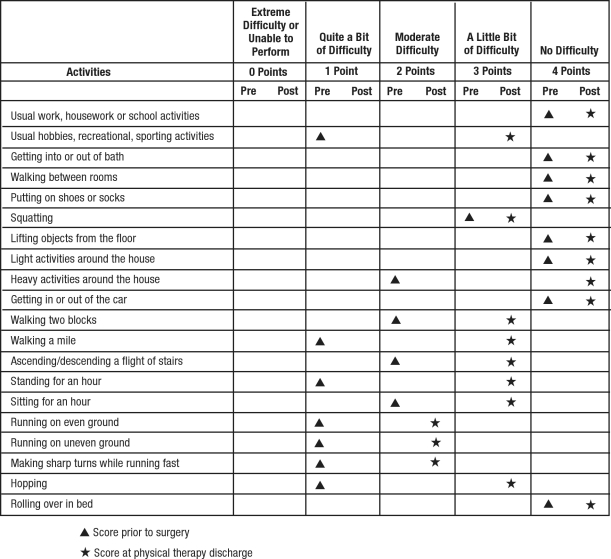
Prior to surgery and at the end of the physical therapy intervention, the patient completed the Lower Extremity Functional Scale (LEFS).20 The LEFS is used to qualitatively assess individual's functional status during 20 specific functional tasks on a scale from 0 (unable to perform actively) to 4 (no difficulty). The maximum score of the assessment test is 80. Binkley et al20 have reported the LEFS to be reliable, valid, and sensitive to change.
The LEFS was administered to the patient to document perceived function prior to surgery with a resultant score of 63% (50 out of 80 points). The LEFS was also administered to the patient to document perceived function at the termination of postoperative rehabilitation with a resultant score of 83% (66 out of 80 points) (See Table 4).
Table 4.
Lower Extremity Function Scale (LEFS) before surgery and at the completion of physical therapy
All parameters of the LEFS to assess simple activities of daily living did not present problems for the patient prior to surgery or following rehabilitation after surgery. Heavy activities around the house presented moderate difficulty prior to surgery and following the post-operative course these activities no longer presented any difficulty. Prolonged activities such as walking two blocks and standing for an hour, negotiating stairs, and sitting for an hour presented only a little bit of difficulty after post-operative rehabilitation. At a more strenuous level, walking a mile, recreational activities, sporting events, and squatting also caused the patient a little bit of difficulty following post-operative rehabilitation. Running on even and uneven ground, along with making sharp turns while running still presented moderate difficulty after post-operative rehabilitation.
DISCUSSION
The rehabilitation of the patient after periacetabular osteotomy for DDH is much like that of a stable fracture following open reduction and internal fixation with similar healing time constraints and weight bearing restrictions. Range of motion in this case returned quickly as there were no significant intra-articular concerns of the hip joint. Specific strengthening of the affected hip musculature along with strengthening of the core for proximal stability was paramount. Restricted weight bearing until bony healing had occurred can limit closed kinetic chain strengthening. However, weight bearing strengthening activities on a device like the Shuttle provides safe and functional loading. Since core strength is vital in the translation of lower extremity power to the upper body and shoulder, core strengthening can and should commence early. Cardiovascular endurance activities also must progress according to weight bearing restrictions.
Long lever arm function of the hip is limited in activities of daily living and in many sports including tennis. It is vital, however, to assure that function of the rectus femoris, a primary muscle responsible for long lever arm function is recovered. Isolated function and control of the rectus femoris was delayed after the periacetabular oteotomy. In this patient, potential contributing factors to the temporary rectus femoris weakness may be due to involvement of the femoral nerve and a change of the length tension relationship from detachment and re-attachment of the muscle during surgery. Although the patient did demonstrate transient sensory changes following surgery, transient motor involvement cannot be ruled out.
Transient gait deviations, specifically a slight gluteus maximus lurch at heel strike, was also a concern. It is difficult to ascertain how much of this problem with gait was due to the patient's gait prior to surgery. Even though gluteal strength gains occurred quickly and gains were subsequently sufficient enough to approximate the contralateral side, slight deviations occurred and were more pronounced at faster gait speeds. Walking backwards (retro-walking) in the clinic with and without external resistance from rubber cords and retro-walking in the pool were helpful in correcting gait deviations.
Exercise dosage and activity modification can be difficult to prescribe. In a young and otherwise healthy individual, the tendency is for the patient to be overzealous. As the patient began to move about better, she did not feel the need to utilize crutches as instructed. This increased weight bearing with concomitant advancement of a therapeutic exercise regime may result in excessive stress on the healing tissue. This was the case in managing this patient. Muscle discomfort immediately following work-outs were common and to be expected. As the patient was allowed to do more in one area (weight bearing, exercise) another area was de-emphasized. When the patient became more aggressive in performing the prescribed exercises, when she increased her overall level of activity and disregarded the consistent use of crutches, she became symptomatic at rest. Symptoms at rest are when activities needed to be significantly restricted to allow the healing areas to accommodate to the added stress.
CONCLUSION
This case study describes the rehabilitation program employed following periacetabular osteotomy in a 14 year-old female tennis player. The role of the physical therapist is vital in prescribing and progressing activity levels to facilitate return of function following this surgical procedure. Goals of the periacetabular osteotomy were to allow resumption of pre-morbid activities and enhance the patient's quality of life and prevent early osteoarthtic changes in the hip. Surgery that is technically well performed followed by a comprehensive rehabilitation program allowed for a return to sports activities following periacetabular osteotomy.
REFERENCES
- 1.Salter RB. Textbook of Disorders and Injuries of the Musculoskeletal System. 3rd Edition Philadelphia: Lippincott, Williams & Wilkins; 1999 [Google Scholar]
- 2.Leach J. Orthopedic Conditions. In: Campbell SK, ed. Physical Therapy for Children. Philadelphia: W.B. Saunders Company; 2000:398–428 [Google Scholar]
- 3.Greenspan A. Orthopedic Radiology: A Practical Approach 3rd Edition Philadelphia: Lippincott, Williams & Wilkins; 2000 [Google Scholar]
- 4.Weinstein SL, Mubarak SJ, Wenger DR. Developmental hip dysplasia and dislocation: Part One. J Bone Joint Surg. 2003;85A:1824–1832 [Google Scholar]
- 5.Garbuz DS, Masri BA, Haddad F, Duncan CP. Clinical and radiographic assessment of the young adult with symptomatic hip dysplasia. Clin Orthop. 2004;418:18–22 [DOI] [PubMed] [Google Scholar]
- 6.Gillingham BL, Sanchez AA, Wenger DR. Pelvic osteotomies for the treatment of hip dysplasia in children and young adults. J Am Acad Orthop Surg. 1999;7:325–337 [DOI] [PubMed] [Google Scholar]
- 7.McKinnis LN. Fundamentals of Orthopedic Radiology. Philadelphia: FA Davis Company; 1997:240 [Google Scholar]
- 8.Troum OM, Crues JV. The young adult with hip pain: Diagnosis and medical treatment circa 2004. Clin Orthop. 2004;418:9–17 [DOI] [PubMed] [Google Scholar]
- 9.Magee DJ. Orthopedic Physical Assessment. 4th Ed.Philadelphia: Saunders; 2002:626 [Google Scholar]
- 10.Leunig M, Podeszwa D, Beck M, Werlan S, Ganz R. Magnetic resonance arthrograpy of labral dysplasia and impingement. Clin Orthop. 2004;418:74–80 [DOI] [PubMed] [Google Scholar]
- 11.Leunig M, Siebenrock KA, Ganz R. Rationale of periacetabular osteotomy and background work. Instructional Course Lectures, American Academy of Orthopaedic Surgeons; 2001:229–238 [PubMed] [Google Scholar]
- 12.Salter RB. Innominate osteotomy in the treatment of congenital dislocation of the hip. J Bone Joint Surg. 1961;43-B:518–539 [PubMed] [Google Scholar]
- 13.Sutherland HD, Greenfield R. Double innominate osteotomy. J Bone Joint Surg. 1977;59-A:1082–1091 [PubMed] [Google Scholar]
- 14.Trousdale RT. Acetabular osteotomy: Indications and results. Clin Orthop. 2004;429:182–187 [PubMed] [Google Scholar]
- 15.Canale ST, ed. Campbell's Operative Orthopaedics. Tenth Edition Philadelphia: Mosby; 2003:939–942 [Google Scholar]
- 16.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: Technique and preliminary results. Clin Orthop. 1988; 232:357–369 [PubMed] [Google Scholar]
- 17.Lazennec JY, Valladares NM, Laudet CG, et al. Anatomical bases of a new technique of juxta-acetabluar osteotomy: technical principles and performance. Surg Radiol Anat. 1998;20:153–159 [PubMed] [Google Scholar]
- 18.Hussell JG, Mast JW, Mayo KA, et al. A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop. 1999;363:64–72 [PubMed] [Google Scholar]
- 19.Tippett SR, Voight ML. Functional Progressions for Sport Rehabilitation. Champaign, IL: Human Kinetics: 1995 [Google Scholar]
- 20.Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (LEFS): Scale development, measurement, properties, and clinical application. Phys Ther. 1999;79:371–383 [PubMed] [Google Scholar]