Abstract
Glenohumeral joint instability is a common pathology encountered in the orthopaedic and sports medicine setting. A wide range of symptomatic shoulder instabilities exist ranging from subtle subluxations due to contributing congenital factors to dislocations as a result of a traumatic episode. Non-operative rehabilitation is utilized in patients diagnosed with shoulder instability to regain their previous functional activities through specific strengthening exercises, dynamic stabilization drills, neuromuscular training, proprioception drills, scapular muscle strengthening program and a gradual return to their desired activities. The specific rehabilitation program should be varied based on the type and degree of shoulder instability present and desired level of function. The purpose of this paper is to outline the specific principles associated with non-operative rehabilitation for each of the various types of shoulder instability and to discuss the specific rehabilitation program for each pathology type.
Keywords: Dynamic stabilization, neuromuscular control, shoulder joint
INTRODUCTION
Shoulder instability is a common pathology often seen in the orthopaedic and sports medicine setting. The glenohumeral joint allows tremendous amounts of joint mobility to function, thus, making the joint inherently unstable and the most frequently dislocated joint in the body.1 Due to the joint's poor osseous congruency and capsular laxity, it greatly relies on the dynamic stabilizers and neuromuscular system to provide functional stability.2 Therefore, differentiation between normal translation and pathological instability is often difficult to determine. A wide range of shoulder instabilities exist from subtle subluxations to gross instability. Often the success of the rehabilitation program is based on the recognition and treatment program designed to treat the specific type of instability present.
Non-operative rehabilitation is often implemented in patients diagnosed with a variety of shoulder instabilities. These instability patterns can range from congenital multidirectional instabilities to traumatic unidirectional dislocations. We have classified glenohumeral joint instabilities into two broad categories: traumatic and atraumatic. Based on the classification system of glenohumeral instability, as well as several other factors, a non-operative rehabilitation program may be developed. The purpose of this paper is to discuss and overview these factors along with the non-operative rehabilitation programs for the various types of shoulder instability in order to return the patient to their previous level of function.
REHABILITATION FACTORS
Seven key factors should be considered when designing a rehabilitation program for a patient with an unstable shoulder (Table). These factors and their significance to the rehabilitation program will be presented.
Table.
Seven key factors to consider in the rehabilitation of the unstable shoulder
|
Onset of Pathology
The first factor to consider in the rehabilitation of a patient with shoulder instability is the onset of the pathology. Pathological shoulder instability may result from an acute, traumatic event or chronic, recurrent instability. The goal of the rehabilitation program may vary greatly based on the onset and mechanism of injury. Following a traumatic subluxation or dislocation, the patient typically presents with significant tissue trauma, pain, and apprehension. The patient who has sustained a dislocation often exhibits more pain due to muscle spasm than a patient who has only subluxed their shoulder. Furthermore, a first-time episode of dislocation is generally more painful than the repeat event. Rehabilitation for the patient with a first-time traumatic episode will be progressed based on the patient's symptoms with emphasis on early controlled range of motion, reduction of muscle spasms and guarding, and relief of pain.
Conversely, a patient presenting with atraumatic instability often presents with a history of repetitive injuries and symptomatic complaints. Often the patient does not complain of a single instability episode but, rather, a feeling of shoulder laxity or an inability to perform specific tasks. Rehabilitation for this patient should focus on early proprioception training, dynamic stabilization drills, neuromuscular control, scapular muscle exercises, and muscle strengthening exercises to enhance dynamic stability due to the unique characteristic of excessive capsular laxity and capsular redundancy in this type of patient.
Degree of Instability
The second factor is the degree of instability present in the patient and the effect on their function. Varying degrees of shoulder instability exist such as a subtle subluxation or gross instability. The term subluxation refers to the complete separation of the articular surfaces with spontaneous reduction. Conversely, a dislocation is a complete separation of the articular surfaces and requires a specific movement or manual reduction to relocate the joint, resulting in underlying capsular tissue trauma. The degree of trauma to the soft tissue of the glenohumeral joint with a shoulder subluxation is can be quite extensive. Speer et al3 has reported that in order for a shoulder dislocation to occur, a Bankart lesion and soft tissue trauma must be present on both sides of the glenohumeral joint capsule. Thus, in the situation of an acute traumatic dislocation, the anterior capsule may be avulsed off the glenoid (Bankart lesion) and the posterior capsule may be stretched, allowing the humeral head to dislocate. Warren et al4 refer to this damage to both the anterior and posterior capsule as the “circle stability concept.”
The rate of progression of the rehabilitation program will vary based upon the degree of instability and persistence of symptoms. For example, a patient with mild subluxations and muscle guarding may initially tolerate strengthening exercises and neuromuscular control drills more than a patient with a significant amount of muscular guarding.
Frequency of Dislocation
The next factor to influence the rehabilitation program is the frequency of dislocation or subluxation. The primary traumatic dislocation is most often treated conservatively with immobilization in a sling and early controlled passive range of motion (ROM) exercises, especially with first time dislocations. The incidence of recurrent dislocation ranges from 17-96% with a mean of 67% in patient populations between the ages of 21-30 years old.1,5–15 Therefore, the rehabilitation program should progress cautiously in young athletic individuals. It should be noted that Hovelius et al8,16,17 has demonstrated that the rate of recurrent dislocations is based on the patient's age and not affected by the length of post-injury immobilization. Individuals between the ages of 19 and 29 years are the most likely to experience multiple episodes of instability. Hovelius et al8,16,17 noted patients in their 20's exhibited a recurrence rate of 60%, whereas, patients in their 30′s to 40′s had less than a 20% recurrence rate. In adolescents, the recurrence rate is as high as 92%18 and 100% with an open physes.19
Chronic subluxations, as seen in the atraumatic, unstable shoulder may be treated more aggressively due to the lack of acute tissue damage and less muscular guarding and inflammation. Rotator cuff and periscapular strengthening activities should be initiated while ROM exercises are progressed. Caution is placed on avoiding excessive stretching of the joint capsule through aggressive ROM activities. The goal is to enhance strength, proprioception, dynamic stability and neuromuscular control, especially in the specific points of motion or direction which results in instability complaints.
Direction of Instability
The fourth factor is the direction of instability present. The three most common forms include anterior, posterior, and multidirectional. Anterior instability is the most common traumatic type of instability seen in the general orthopaedic population, representing approximately 95% of all traumatic shoulder instabilities12. Following a traumatic event in which the humeral head is forced into extremes of abduction and external rotation, or horizontal abduction, the glenolabral complex and capsule may become detached from the glenoid rim resulting in anterior instability. This type of detachment is referred to a Bankart lesion.(Figure 1) Baker et al20 have identified four types of Bankart lesions based on the size and the degree of tissue involvement. Conversely, rarely will a patient with atraumatic instability due to capsular redundancy dislocate their shoulder. It is the author's opinion that these patients are more likely to repeatedly sublux the joint without complete separation of the humerus from the glenoid rim. Capsular avulsions can occur on the glenoid side (Bankart lesion) or on the humeral head side referred to as a HAGL lesion (humeral avulsion of the inferior glenohumeral ligament).21–23
Figure 1.
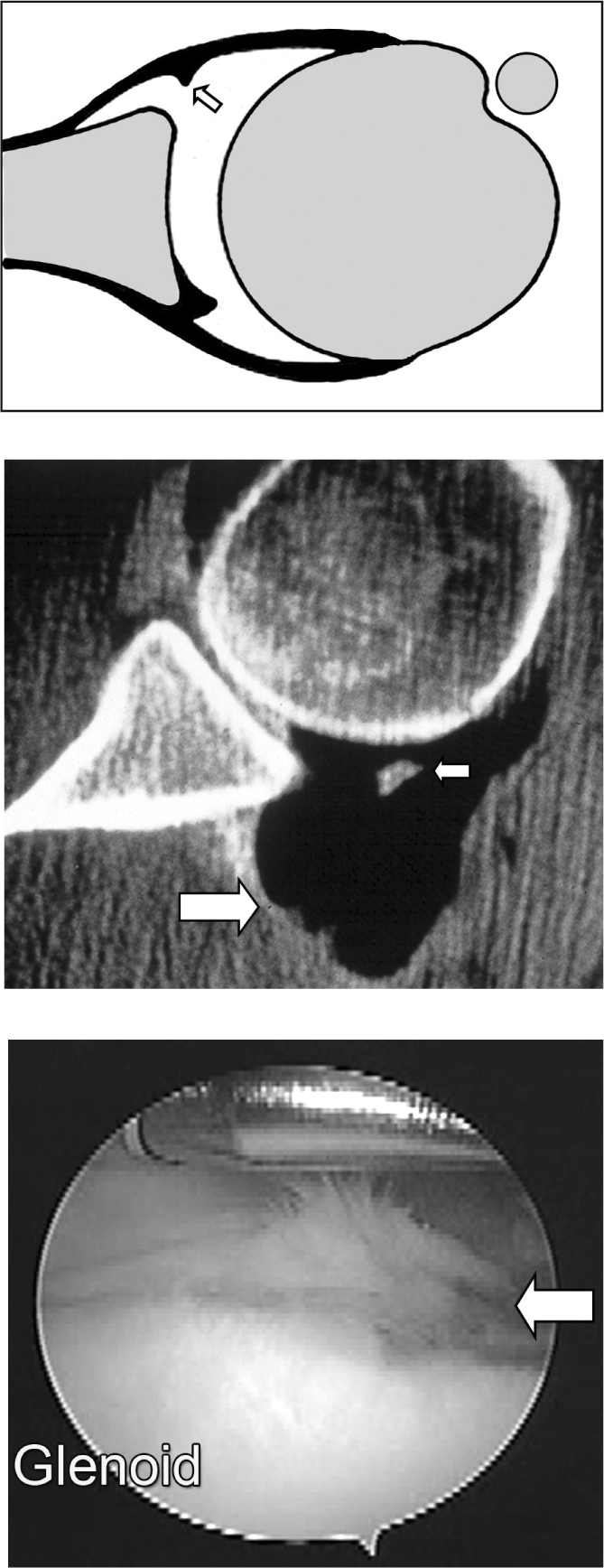
Bankart lesion commonly observed with a traumatic dislocation.
1a. Drawing illustrating a Bankart lesion. The arrow denotes the avulsed capsule from the glenoid.
1b. CT arthrogram of a bony Bankart lesion. The large arrow shows the dye that has leaked out of the capsule. The small arrow shows the bony lesion which has pulled away from the glenoid rim.
1c. An arthroscopic view of a Bankart lesion.
Posterior instability occurs less frequently, only accounting for less than 5% of traumatic shoulder dislocations.24,25 This type of instability is often seen following a traumatic event such as falling onto an outstretched hand or from a pushing mechanism. However, patients with significant atraumatic laxity may complain of posterior instability especially with shoulder elevation, horizontal adduction and excessive internal rotation due to the strain placed on the posterior capsule in these positions. In professional or collegiate football, the incidence of posterior shoulder instability appears higher than the general population. This is especially true in linemen. Mair et al26 reported on nine athletes with posterior instability in which eight of nine were linemen and seven were offensive linemen. Often, these patients require surgery as Mair et al26 also reported 75% required surgical stabilization. Kaplan et al27 reported in a study of collegiate football players that 78% required surgical stabilization.
Multidirectional instability (MDI) can be identified as shoulder instability in more than one plane of motion. Patients with MDI have a congenital predisposition and exhibit ligamentous laxity due to excessive collagen elasticity of the capsule. Furthermore, Rodeo et al28 reported that this type of patient turns over collagen at a faster rate. The authors consider an inferior displacement of greater than 8-10mm during the sulcus maneuver (Figure 2) with the arm adducted to the side as significant hypermobility, thus suggesting significant congenital laxity.2
Figure 2.
Sulcus maneuver to assess inferior capsular laxity
Due to the atraumatic mechanism and lack of acute tissue damage, ROM is often normal to excessive. Patients with recurrent shoulder instability due to MDI generally have weakness in the rotator cuff, deltoid muscle, and scapular stabilizers with poor dynamic stabilization and inadequate static stabilizers. Initially, the focus of the rehabilitation program is on maximizing dynamic stability, scapula positioning, proprioception, and improving neuromuscular control in mid ROM. Also, rehabilitation should focus on improving the efficiency and effectiveness of glenohumeral joint force couples through co-contraction exercises, rhythmic stabilization, and neuromuscular control drills. Isotonic strengthening exercises for the rotator cuff, deltoid muscle, and scapular muscles are also emphasized to enhance dynamic stability. Morris et al29 reported the EMG activity of the rotator cuff and deltoid muscle in MDI and asymptomatic subjects. The authors noted the most significant difference was in the deltoid muscles compared to the rotator cuff muscles in their groups.
Concomitant Pathologies
The fifth factor involves considering other tissues that may have been affected and the premorbid status of the tissue. Disruption of the anterior capsulolabral complex from the glenoid commonly occurs during a traumatic injury resulting in an anterior Bankart lesion. Often osseous lesions may be present such as a concomitant Hill Sach's lesion caused by an impaction of the postero-lateral aspect of the humeral head as it compresses against the anterior glenoid rim during relocation. This Hill Sach's lesion has been reported in up to 80% of dislocations.30–32 Conversely, a reverse Hill Sach's lesion may be present on the anterior aspect of the humeral head due to a posterior dislocation.33 Occasionally, a bone bruise may be present in individuals who have sustained a shoulder dislocation as well as pathology to the rotator cuff. In rare cases of extreme trauma, the brachial plexus may become involved as well.34 Other common injuries in the unstable shoulder may involve the superior labrum (SLAP lesion) such as a type V SLAP lesion characterized by a Bankart lesion of the anterior capsule extending into the anterior superior labrum.35 These concomitant lesions may significantly slow down the rehabilitation program in order to protect the healing tissue.
Neuromuscular Control
The sixth factor to consider is the patient's level of neuromuscular control, particularly at end range. Neuromuscular control may be defined as the efferent, or motor, output in reaction to an afferent, or sensory input.2,10 The afferent input is the ability to detect the glenohumeral joint position and motion in space with resultant efferent response by the dynamic stabilizers as they blend with the joint capsule to assist in stabilization of the humeral head. Injury with resultant insufficient neuromuscular control could result in deleterious effects to the patient. As a result, the humeral head may not center itself within the glenoid, thereby, compromising the surrounding static stabilizers. The patient with poor neuromuscular control may exhibit excessive humeral head migration with the potential for injury, an inflammatory response, and reflexive inhibition of the dynamic stabilizers.
Several authors have reported that neuromuscular control of the glenohumeral joint may be negatively affected by joint instability. Lephart et al10 compared the ability to detect passive motion and the ability to reproduce joint positions in patients with normal, unstable, and surgically repaired shoulders. The authors reported a significant decrease in proprioception and kinesthesia in the shoulders with instability when compared to both normal shoulders and shoulders undergoing surgical stabilization procedures. Smith and Brunoli36 reported a significant decrease in proprioception following a shoulder dislocation. Blasier et al37 reported that individuals with significant capsular laxity exhibited a decrease in proprioception compared to patients with normal laxity. Zuckerman et al38 noted that proprioception is affected by the patient's age with older subjects exhibiting diminished proprioception than a comparably younger population. Thus, the patient presenting with traumatic or acquired instability may present with poor neuromuscular control.
Activity Level
The final factor to consider in the non-operative rehabilitation of the unstable shoulder is the arm dominance and the desired activity level of the patient. If the patient frequently performs an overhead motion or sporting activities such as a tennis, volleyball, or a throwing sport, then the rehabilitation program should include sport specific dynamic stabilization exercises, neuromuscular control drills, and plyometric exercises in the overhead position once full, pain free ROM and adequate strength has been achieved. Patients whose functional demands involve below shoulder level activities will follow a progressive exercise program to return full ROM and strength. The success rates of patients returning to overhead sports after a traumatic dislocation of their dominant arm are extremely low.39 Arm dominance can also significantly influence the successful outcome. The recurrence rates of instabilities vary based on age, activity level, and arm dominance. In athletes involved in collision sports, the recurrence rates have been reported collision sports, the recurrence rates have been reported between 86-94%.6,40–42
REHABILITATION GUIDELINES
Patients may be classified into two common forms of shoulder instability - traumatic and atraumatic. Specific guidelines to consider in the rehabilitation of each patient population will be outlined. A four-phase rehabilitation program will be discussed for traumatic shoulder instability, followed by an overview of variations and key rehabilitation principles for atraumatic shoulder instability (congenital and acquired laxity).
Traumatic Shoulder Instability
Phase I-Acute Phase
Following a first time traumatic shoulder dislocation or subluxation, the patient often presents in considerable pain, muscle spasm, and an acute inflammatory response. The patient usually self-limits their motion by guarding the injured extremity in an internally rotated and adducted position against the side of their body to protect the injured shoulder. The goals of the acute phase are to 1) diminish pain, inflammation, and muscle guarding 2) promote and protect healing soft tissues, 3) prevent the negative effects of immobilization, 4) re-establish baseline dynamic joint stability, and 5) prevent further damage to glenohumeral joint capsule. (Appendix 1)
Immediate limited and controlled motion is allowed following a traumatic dislocation in patients between the ages of 18-28 years but immobilize patients between the ages of 29-54 years old. However, motion is restricted so as to not to cause further tissue attenuation. A short period of immobilization in a sling to control pain and to allow scar tissue to form for enhanced stability may be necessary for 7-14 days although no long-term benefits regarding recurrence rates and immobilization have been made in younger patients between the ages of 18-28 years old.8,43 Individuals above the age of 28 are usually immobilized for 2-4 weeks to allow scarring of the injured capsule. Potential complications with immobilization may include a decrease in joint proprioception, muscle disuse and atrophy, and a loss of ROM in specific age groups. Therefore, prolonged use of immobilization following a traumatic dislocation may not be recommended in all patients.
The ideal position to immobilize the glenohumeral has traditionally been in internal rotation with the arm close to the body. Recent studies by Itoi et al44,45 examined positional differences of immobilization and compared the rates of recurrent dislocations. The authors concluded that immobilization in external rotation significantly reduced the recurrence rate of instability in chronic and first-time dislocators. Itoi et al45 has recommended immobilization with the arm in 30 degrees of abduction and external rotation, compared to a group of patients immobilized in internal rotation. The results indicated a 0% recurrence rate in external rotation and 30% incidence of instability in the group immobilized in internal rotation. The authors stated that the resultant Bankart lesion had improved coaptation to the glenoid rim with immobilization in external rotation versus conventional immobilization in a sling.
Passive ROM is initiated in a restricted and protected range based on the patient's symptoms. The early motion is intended to promote healing, enhance collagen organization, stimulate joint mechanoreceptors, and aid in decreasing the patient's pain through neuromuscular modulation.14,46–48 Painfree active-assisted ROM exercises such as pendulums and external/internal rotation at 45 degrees of abduction using an L-bar (Breg Corp. Vista, CA) may also be initiated. Passive ROM exercises are also performed in a painfree arc of motion. Modalities such as ice, transcutaneous electrical nerve stimulation (TENS), and high voltage stimulation may also be beneficial to decrease pain, inflammation, and muscle guarding.
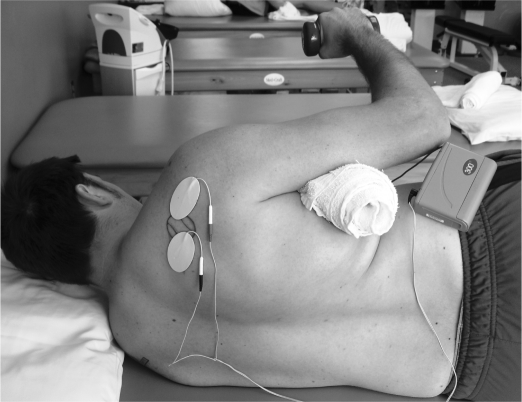
Strengthening exercises are initially performed through submaximal, painfree isometric contractions to initiate muscle recruitment and retard muscle atrophy. Electrical stimulation of the posterior cuff musculature may also be incorporated to enhance the muscle fiber recruitment process early on in the rehabilitation process and also in the next phase when the patient initiates iso-tonic strengthening activities.(Figure 3) Reinold et al49 believe that the use of electrical stimulation may improve force production of the rotator cuff particularly the external rotators immediately after an acute injury.
Figure 3.
Electrical stimulation to the posterior rotator cuff during exercise activity to improve muscle fiber recruitment and contraction
Dynamic stabilization exercises are also performed to re-establish dynamic joint stability. The patient maintains a static position as the rehabilitation specialist performs manual rhythmic stabilization drills to facilitate muscular co-contractions. These manual rhythmic stabilization drills are performed for the shoulder internal and external rotators in the scapular plane at 30 degrees of abduction and are performed at painfree angles which do not compromise the healing capsule. Rhythmic stabilization for flexion and extension may also be performed with the shoulder at 100 degrees of flexion and 10 degrees of horizontal abduction. Strengthening exercises are also performed for the scapular retractors and depressors to reposition the scapula in its proper position. Scapula strengthening is critical for successful rehabilitation. Closed kinetic chain exercises such as weight shifting on a ball are performed to produce a co-contraction of the surrounding glenohumeral musculature and to facilitate joint mechanoreceptors to enhance proprioception. Weight shifts are usually able to be performed immediately following the injury unless posterior instability is present.
Phase II-Intermediate phase
During the intermediate phase, the program emphasizes regaining full ROM along with progressing strengthening exercises of the rotator cuff, and re-establishing muscular balance of the glenohumeral joint, scapular stabilizers, and surrounding shoulder muscles. Before the patient enters Phase II, certain criteria must be met which include diminished pain and inflammation, satisfactory static stability, and adequate neuromuscular control.
To achieve the desired goals of this phase, passive ROM is performed to the patient's tolerance with the goal of attaining nearly full ROM. Active-assisted ROM exercises using a rope and pulley along with flexion and external/internal rotation exercises at 90 degrees of abduction using an L-bar may be progressed to tolerance without stressing the involved tissues. External rotation at 90 degrees of abduction is generally limited to 65-70 degrees to avoid overstressing the healing anterior capsuloligamentous structures for approximately 4-8 weeks but eventually increasing ROM to full motion as the patient tolerates.
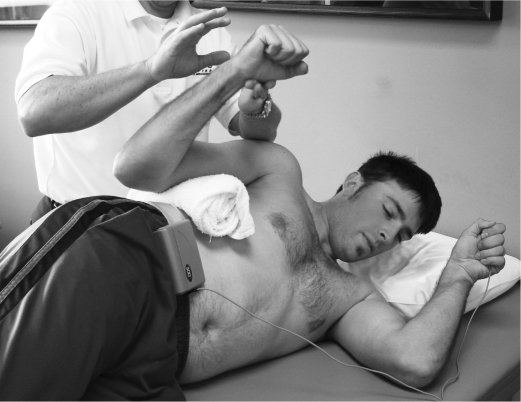
Isotonic strengthening exercises are also initiated during this phase. Emphasis is placed on increasing the strength of the internal and external rotators and scapular muscles to maximize dynamic stability. The ultimate goal of the strengthening phase is to re-establish muscular balance following the injury. Kibler1 noted that scapular position and strength deficits have been shown to contribute to glenohumeral joint instability. Exercises initially include external and internal rotation with exercise tubing at 0 degrees of abduction along with sidelying external rotation and prone rowing. During the latter part of this phase, isotonic exercises are progressed to emphasize rotator cuff and scapulothoracic muscle strength. Manual resistive exercises such as sidelying external rotation and prone rowing may also prove beneficial by having the clinician vary the resistance throughout the ROM. Incorporating manual concentric and eccentric manual exercises and rhythmic stabilization drills at end range to enhance neuromuscular control and dynamic stability is also recommended.(Figure 4)
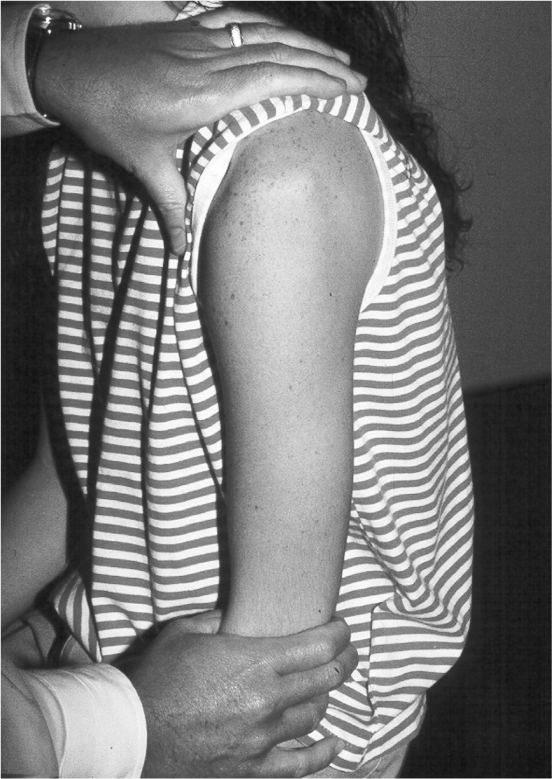
Figure 4.
Sidelying manual external rotation while the clinician imparts rhythmic stabilization drills at end range
Closed kinetic chain exercises are progressed to include a hand on the wall stabilization drills in the plane of the scapular at shoulder height as the patient tolerates. (Figure 5) Push-ups are performed first with hands on a table then progressed to a push-up on a ball or unstable surface while the rehabilitation specialist performs rhythmic stabilization to the involved and uninvolved upper extremity along with the trunk to integrate dynamic stability and core strengthening (tilt board, ball, etc.).(Figure 6) Caution should be placed while performing closed kinetic chain exercises in patients with posterior instability for 6-8 weeks at allow for adequate healing and strength gains. Furthermore, patients with significant scapular winging should perform push-ups until adequate scapular strength is accomplished. Core stabilization drills should also be performed to enhance scapular control. Additionally, strengthening exercises may be advanced in regards to resistance, repetitions, and sets as the patient improves. End range rhythmic stabilization drills with the arm at 0 degrees of adduction or at 45 degrees of abduction are also performed. Exercises such as tubing with manual resistance and end range rhythmic stabilization drills are also performed.(Figure 7) The goal of these exercise drills is to improve proprioception and neuromuscular control at end range.
Figure 5.
Wall stabilization drills in the plane of the scapula
Figure 6.
Rhythmic stabilization drills on an unstable surface to further challenge the patient's neuromuscular control.
Figure 7.
External rotation with tubing while the therapist applies an external force throughout the ROM
Phase III- Advanced Strengthening
In the advanced strengthening phase, the focus is on improving strength, dynamic stability, and neuromuscular control near end range through a series of progressive strengthening exercises for a gradual return to the patient's activity. Criteria to enter this phase include: 1) minimal pain and tenderness, 2) full range of motion, 3) symmetrical capsular mobility, 4) good (at least ⅘ manual muscle test) strength, endurance and dynamic stability of the scapulothoracic and upper extremity musculature.
Muscle fatigue has also been associated with a decrease in neuromuscular control. Carpenter et al50 observed the ability to detect passive motion of shoulders positioned at 90 degrees of abduction and 90 degrees of external rotation. The investigators reported a decrease in both the detection of external and internal rotation movement following an isokinetic fatigue protocol. Therefore, exercises designed to enhance endurance in the upper extremity such as using low resistance and high repetitions (20-30 repetitions per set) are incorporated during this phase. Also, exercise sets utilizing time may be incorporated, such as 30 second or 60 second exercise bouts. These exercises may include tubing external and internal rotation, plyoball wall dribbling, and submaximal manual resistance drills.
Aggressive upper body strengthening through the continuation of a progressive isotonic resistance program is recommended. A gradual increase in resistance as well as a progression to a more functional position by performing tubing exercises at 90 degrees of abduction to strengthen the external and internal rotators is also recommended. Additionally, more aggressive isotonic strengthening exercises such as bench press, seated row, and latissimus pull-downs may be incorporated in a protected range of motion during this phase. During bench press and seated rows, the patient is instructed to not extend the upper extremities beyond the plane of the body to minimize stress on the shoulder capsule. Latissimus pulldowns are performed in front of the head and the patient is instructed to avoid full extension of the arms to minimize the amount of traction force applied to the shoulder joint. Also during this phase, the patient continues to perform rhythmic stabilization drills with the rehabilitation specialist and gradually progresses to a position of apprehension utilizing tubing at 90 degrees of abduction with end range rhythmic stabilization drills to enhance dynamic stability.
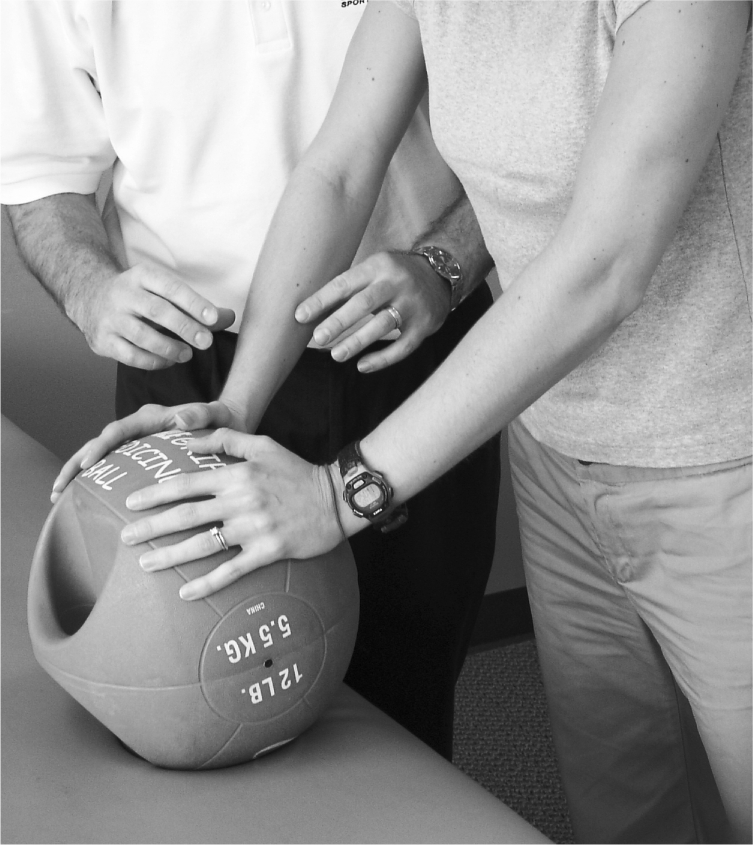
A patient wishing to return to athletic participation may be instructed to perform plyometric exercises for the upper extremity. These activities are incorporated to regain any remaining functional ROM as well as improving neuromuscular control and to train the extremity to produce and dissipate forces. Initially, 2-handed drills close to the body such as chest pass, side-to-side and overhead soccer throws (Figure 8) using a 3-5 pound medicine ball may be performed to enhance dynamic stabilization of the glenohumeral joint. Exercises are initiated with 2-hand drills close to the center of gravity and gradually progressed to longer lever arms away from the patient's body. Drills are progressed to challenge the dynamic stabilizers of the shoulder.
Figure 8.

2- handed plyometric throw into a trampoline
After approximately two weeks of pain free 2-handed drills, the athlete progresses to 1-handed plyometric drills using a small medicine ball (1-2 lbs) and throwing into a plyoback. Plyoball wall dribbles in the 90/90 position (Figure 9) to improve overhead muscle endurance may also be incorporated.
Figure 9.
Wall dribbles in the 90/90 position
Phase IV- Return to Activity Phase
In the return to activity phase, the goal is to increase, gradually and progressively, the functional demands on the shoulder in order for the patient to return to unrestricted, sport or daily activities. Other goals of this phase are to maintain the patient's muscular strength and endurance, dynamic stability and functional range of motion. The criteria to progress into this phase include: 1) full functional ROM, 2) adequate static stability, 3) satisfactory muscular strength and endurance, 4) adequate dynamic stability, and 5) a satisfactory clinical exam.
The general orthopaedic patient continues to perform a maintenance program to improve strength, dynamic stability, and neuromuscular control as well as maintaining full, functional and painfree ROM. The athlete continues to perform aggressive strengthening exercises such as plyometrics, proprioceptive neuromuscular facilitation drills, and isotonic strengthening. In addition, the athlete may begin functional sport activities through an interval return to sport program. These activities are designed to gradually return motion, function, and confidence in the upper extremity by progressing through graduated sport-specific activities.51–53 These interval sport programs are set up to minimize the chance of re-injury while training the patient for the demands of each individual sport. Each program should be individualized based on the patient's injury, skill level, and goals. The duration of each program is based on several factors including the extent of the injury, the sport and level of play, along with the time of season. The athlete is allowed to return to unrestricted sports activities after completion of an appropriately designed rehabilitation program and a successful clinical exam including full ROM, strength along with adequate dynamic stability and neuro-muscular control.
We routinely perform a combination of isokinetic testing for our overhead athletes, which we refer to as the “Thrower's Series.”54,55 Criteria to begin an interval sport program includes an external rotation/internal rotation strength ratio of 66-76% or higher at 180°/second, an external rotation to abduction ratio of 67-75% or higher at 180°/second.54,55 Patients returning to contact sports such as hockey, football, rugby, etc may be required to wear a shoulder stability brace (Don-Joy) for the initiation of the sport return.(Figure 10)
Figure 10.

Don Joy brace used during sports activities to prevent excessive shoulder ROM
Rehabilitation for Atraumatic Shoulder Instability
Rehabilitation of the patient with congenital shoulder instability poses a significant challenge for the rehabilitation specialist. The patient typically presents with several episodes of instability which limits them from performing certain tasks which may include daily work tasks as well as recreational or sports activities. This type of instability may arise from several factors including excessive redundancy and capsular laxity, poor osseous configuration such as a flattened glenoid fossa, or weakness in the glenohumeral and scapular musculature resulting in poor neuromuscular control. Any of these factors, individually or in combination, may contribute to pathological glenohumeral instability.
The focus of the rehabilitation program for the patient with atraumatic instability is similar to the traumatically unstable shoulder, however, this program involves a slower progression with careful consideration to avoid excessive stretching to the capsular tissue. Furthermore, early goals include improving proprioception, dynamic stability, neuromuscular control, and scapular muscle strengthening to gradually return the patient to functional activities without limitations. As previously mentioned, the early phase of rehabilitation involves reducing shoulder pain and muscular inhibition while abstaining from activities that cause apprehension.
Shoulder muscle activation has been shown to differ in patients with congenital laxity versus in a normal, stable shoulder.29,56–59 Normal force coupling that exists to dynamically stabilize the glenohumeral joint is altered resulting in excessive humeral head migration and a feeling of subluxation by the patient. Rockwood and Burkhead39 found that an exercise program was effective in the management of 80% of atraumatic instability. A recent study by Misamore et al60 found improved results in 49% (28 of 59) of patients in a long term follow up study of atraumatic, athletic patients.
The rehabilitation program (Appendix 2) for the patient with atraumatic instability involves regaining full ROM without excessive stress to the involved tissues. The patient often presents with excessive ROM, therefore, passive ROM activities are not the focus of the rehabilitation program. Special attention is placed to avoid excessive stretches to the involved tissues. Modalities such as cryotherapy, phonophoresis, high voltage stimulation, and TENS may be used to minimize pain and inflammation. The reduction of shoulder pain may also be accomplished through gentle motion activities to neuromodulate pain, NSAIDs prescribed by the physician and abstaining from painful arcs of active and passive ROM.
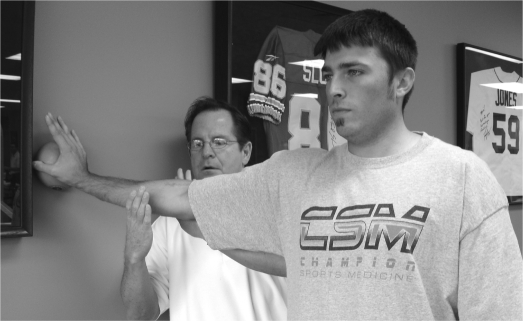
The focus of the early phase of the rehabilitation program is to minimize any further muscle atrophy and reflexive inhibition resulting from disuse, repeated subluxation episodes, and pain. Isometric contraction exercises may be performed for the glenohumeral muscles particularly the rotator cuff. Rhythmic stabilization drills may also be performed to facilitate a muscular co-contraction/co-activation to improve neuromuscular control and enhance the sensitivity of the afferent mechanoreceptors.10(Figure 11) The goal is to create a more efficient agonist/antagonist co-contraction to improve force coupling and joint stability during active movements.
Figure 11.

Manual rhythmic stabilization drills to promote a co-contraction and improve dynamic stability
The authors of this paper believe that exercises such as rhythmic stabilization drills and closed kinetic chain exercises to promote a co-contraction and an improvement in proprioception are beneficial for this patient population. Axial compression exercises are progressed from standing weight shifts on a table top to then include the quadruped and tripod positions (Note - this position should be avoided if posterior instability is present). Rhythmic stabilization of the involved extremity as well as at the core and trunk may be applied during these closed kinetic chain drills to further challenge the patient's dynamic stability and neuromuscular control. Unstable surfaces such as tilt boards, foam, large exercise balls, and the Biodex stability system (Biodex Corp., Shirley, NY) may be incorporated to further challenge the patient's dynamic stability while in the closed chain position to further promote a co-activation or cocontraction of the surrounding musculature.(Figure 12)
Figure 12.
Axial compression drill on an unstable surface while the rehabilitation performs rhythmic stabilizations to the patient's involved shoulder and trunk.
Patients with congenital laxity often present with significant rotator cuff and scapular strength deficits, particularly the external rotators, scapular retractors, and scapular depressors. A progressive isotonic strengthening program may be initiated to improve rotator cuff and scapular musculature strength, endurance, and dynamic stability. Proper scapula stability and movement is vital for asymptomatic function. Scapula strengthening will improve proximal stability and therefore enable distal segment mobility for during the patient's functional tasks. These exercises may include external rotation at 0 degrees of abduction, sidelying external rotation, standing external rotation at 90 degrees of abduction, prone external rotation, prone rowing, prone extension and prone horizontal abduction at 100 degrees with external rotation. Other scapular training exercises commonly incorporated include supine serratus punches and a dynamic hug for serratus anterior strengthening. Bilateral external rotation with scapular retraction and table lifts may also be performed to strengthen the lower trapezius. Neuromuscular control drills are performed for the scapular musculature by having the rehabilitation specialist manually resist scapula movements. The goal of these drills is to enhance strength, endurance, and scapula proprioception.
The function of neuromuscular control system must not be overlooked in this patient population. Functional exercise drills that include positions of instability to induce a reflexive muscular response may protect against future injury or recurring episodes of instability. 2,61,62 Active joint repositioning tasks, proprioceptive neuromuscular facilitation (PNF) and plyometric exercises may be beneficial as well to evoke a neuromuscular response.
Once sufficient strength of the scapular stabilizers and posterior cuff has been achieved, the patient is encouraged to use the shoulder only in the most stable positions; those in the plane of the scapular during humeral elevation. Activities that promote a feeling of joint instability with or without subluxation or dislocation should be avoided. Only when coordination and confidence are achieved through progressive strengthening should the patient attempt activities in an intrinsically unstable position. Bracing of the glenohumeral joint for return to sporting activities may also be necessary to provide immobilization or controlled ROM to protect against further injury.
The primary focus of the rehabilitation program for the congenitally unstable shoulder patient is to enhance strength and balance in the rotator cuff, improve scapular position and core stability, along with improved proprioception and neuromuscular control. Once symptoms have subsided and sufficient strength has been achieved, the patient may resume normal shoulder function, which may include sport activities.
CONCLUSION
The glenohumeral joint is an inherently unstable joint that relies on the interaction of the dynamic and static stabilizers to maintain stability. Disruption of this interplay or poor development of any of these factors may result in instability, pain, and a loss of function. Rehabilitation will vary based on the type of instability present and the key principles described. A comprehensive program designed to establish full range of motion, balance capsular mobility, along with maximizing muscular strength, endurance, proprioception, dynamic stability and neuromuscular control is essential. A functional approach to rehabilitation using movement patterns and sport specific positions along with an interval sport program will allow a gradual return to athletics. The focus of the program should minimize the risk of re-injury and ensure that the patient can safely produce and dissipate forces at the glenohumeral joint.
Appendix 1. Traumatic dislocation protocol
NON-OPERATIVE REHABILITATION TRAUMATIC DISLOCATION OF THE SHOULDER
The program will vary in length for each individual depending on several factors:
Severity and onset of symptoms
Degree of instability symptoms
Direction of instability
Concomitant pathologies
Age and Activity Level of Patient
Arm dominance
Desired Goals and activities
I. PHASE I - ACUTE MOTION PHASE
Goals:
Protect healing capsular structures
Re-establish non-painful range of motion
Decrease pain, inflammation, and muscular spasms
Retard muscular atrophy / Establish voluntary muscle activity
Reestablish dynamic stability
Improve proprioception
Note: During the early rehabilitation program, caution must be applied in placing the capsule under stress until dynamic joint stability is restored. It is important to refrain from activities in extreme ranges of motion early in the rehabilitation process.
Decrease Pain/Inflammation:
Sling or ER brace for comfort and depending on age of patient (MD preference)
Therapeutic modalities (ice, TENS, etc.)
NSAIDs
Gentle joint mobilizations (grade I-II) for pain neuromodulation
* Do not stretch injured capsule
Range of Motion Exercises:
Gentle ROM only, no stretching
Pendulums
-
Rope & Pulley
-Elevation in scapular plane to tolerance
-
Active-assisted ROM L Bar to tolerance
-Flexion
-Internal Rotation with arm in scapular plane at 30° abduction
-External Rotation with arm in scapular plane at 30° abduction
- Motion is performed in Non-Painful arc of motion only *
⋆ DO NOT PUSH INTO ER OR HORIZONTAL ABDUCTION with anterior instability
⋆ Avoid excessive IR or horizontal adduction with posterior instability
Strengthening/Proprioception Exercises:
Isometrics (performed with arm at side)
- Flexion
- Abduction
- Extension
- Biceps
- Internal Rotation (multi-angles)
- External Rotation (multi-angles)
- Electrical muscle stimulation may be used to ER during isometrics
- Scapular retract/protract elevate/depress (seated manual resist.)
Rhythmic Stabilization
ER/IR in scapular plane (pain-free multi-angles)
Flex/Ext in scapular plane(pain-free angles, multi-angles)
Weight Shifts - standing hands on table (CKC Exercises) – (ant. instability only)
Proprioception training drills - Active joint reproduction proprioceptive drills(ER,IR,Flex)
II. Phase II - Intermediate Phase
Goals:
Regain and improve muscular strength
Normalize arthrokinematics
Enhance proprioception and kinesthesia
Enhance dynamic stabilization
Improve neuromuscular control of shoulder complex
Criteria to Progress to Phase II:
Nearly Full to Full Passive ROM (ER may be still limited)
Minimal Pain or Tenderness
“Good” MMT of IR, ER, Flexion, and Abduction
Baseline proprioception and dynamic stability
Progress range of motion activities at 90 degrees abduction to tolerance (painfree)
Initiate isotonic strengthening
Emphasis on external rotation and scapular strengthening
- ER/IR Tubing
- Scaption raises (full can)
- Abduction to 90 degrees
- Sidelying external rotation to 45 degrees
- Standing ER with tubing with manual resistance
- Hand on ball against wall resistance stabilization
- Prone extension to neutral
- Prone horizontal adduction
- Prone rowing
- Lower and middle trapezius
- Sidelying neuromuscular exercise drills
- Push-ups onto table
- Seated manual scapular resistance
- Biceps curls
- Triceps pushdowns
- Electrical muscle stimulation may be used to ER during exercises
Improve Neuromuscular control of Shoulder Complex
- Initiation of proprioceptive neuromuscular facilitation
- Rhythmic stabilization drills
- ER/IR at 90 degrees abduction (limit degree of ER)
- Flexion/Extension/Horizontal at 100 degrees flexion, 10 degrees horizontal abduction
- Progress to mid and end range of motion
- Progress OKC program
- PNF
- Manual resistance ER (supine ‡ sidelying Æ eccentrics), prone row
- ER/IR tubing with stabilization
- Progress CKC exercises with rhythmic stabilizations
- Wall stabilization on ball
- Hand on wall – wall circles for rotator cuff endurance
- Hand on wall – side to side motion for scapular muscles and deltoid
- Static holds in push-up position on ball
- Push-ups on tilt board
- Core
- Abdominal strengthening
- Trunk strengthening / Low back
- Gluteal strengthening
Continue Use of Modalities (as needed)
- Ice, electrotherapy modalities
III. Phase III - ADVANCED Strengthening Phase
Goals:
Improve strength/power/endurance
Improve neuromuscular control
Enhance dynamic stabilizations
Prepare patient/athlete for activity
Criteria to Progress to Phase III:
Full non-painful range of motion
No palpable tenderness
Continued progression of resistive exercises
Good - normal muscle strength, dynamic stability, neuromuscular control
Continue use of modalities (as needed)
Continue isotonic strengthening (progress resistance)
- Continue Thrower's Ten
- Progress to end range stabilization drills
- Progress to full ROM strengthening
- Progress to bench press in restricted ROM (restrict horizontal abduction ROM)
- Progress to flat & incline chest press (weighted) restrict motion
- Program to seated rowing and lat pull down (in front) in restricted ROM
Emphasize PNF
Manual D2 with RS at 45, 90, & 145 degrees
Advanced neuromuscular control drills (for athletes)
- Ball flips on table
- ER tubing at 90 deg abduction with manual resistance & RS at end range
- Push-ups on ball/rocker board with rhythmic stabilizations
- Manual scapular neuromuscular control drills
- Initiate perturbation activities (ER with exercise tubing with end range rhythmic stab)
Endurance training
- Timed bouts of exercises – 30-60 seconds
- Increase number of repetitions (sets of 15/20 reps)
- Multiple bouts throughout day (3x)
Initiate plyometric training
-
- 2-hand drills:
- Chest pass throw
- Side to side throw
- Overhead soccer throw
-
- Progress to 1-hand drills:
- 90/90 baseball throws
- Wall dribbles
- 90/90 baseball throws against wall
⋆ Continue to avoid excessive stress on joint capsule
IV. Phase IV - RETURN TO ACTIVITY PHASE
Goals:
Maintain optimal level of strength/power/endurance
Progressively increase activity level to prepare patient/athlete for full functional return to activity/sport
Criteria to Progress to Phase IV:
Full ROM
No pain or palpable tenderness
Satisfactory isokinetic test
Satisfactory clinical exam
Continue all exercises as in Phase III
Progress isotonic strengthening exercises
Resume normal lifting program (Physician will determine)
Initiate interval sport program (as appropriate)
Continue modalities- ice, e-stim, etc. (as needed)
Consider GH joint stabilizing brace for contact sports
FOLLOW-UP
Isokinetic Test (ER/IR & Abd/Add)
Progress Interval Program
Maintenance of Exercise Program
Appendix 2. Atraumatic Instability protocol
Non-operative Rehabilitation for Atraumatic Instability
This multi-phased program is designed to allow the patient/athlete to return to their previous functional level as quickly and safely as possible. Each phase will vary in length for each individual depending upon the severity of injury, ROM/strength deficits, and the required activity demands of the patient.
PHASE I - ACUTE PHASE
Goals:
Decrease pain/inflammation
Re-establish functional range of motion
Establish voluntary muscular activation
Re-establish muscular balance
Improve proprioception
-
Decrease Pain/Inflammation
-Therapeutic modalities (ice, electrotherapy, etc.)
-NSAIDS
-Gentle joint mobilizations (Grade 1 and II) for neuromodulation of pain
Range of Motion Exercises
Gentle ROM exercises – no stretching
Pendulum exercises
Rope and pulley
Elevation to 90 degrees, progressing to 145/150 degrees flexion
L-Bar
Flexion to 90 degrees, progressing to full ROM
Internal rotation with arm in scapular plane at 45 degrees abduction
External rotation with arm in scapular plane at 45 degrees abduction
Progressing arm to 90 degrees abduction
Strengthening Exercises
Isometrics (performed with arm at side)
Flexion
Abduction
Extension
External rotation at 0 degrees abduction
Internal rotation at 0 degrees abduction
Scapular isometrics
Biceps
Retraction/protraction
Elevation/depression
Weight shifts with arm in scapular plane (closed chain exercises)
Rhythmic stabilizations (supine position)
External/internal rotation at 30 degrees abduction
Flexion/extension at 45 and 90 degrees flexion
⋆Note: It is important to refrain from activities and motion in extreme ranges of motion early in the rehabilitation process in order to minimize stress on joint capsule.
Proprioception/Kinesthesia
Active joint reposition drills for ER/IR
PHASE II - INTERMEDIATE PHASE
Goals:
Normalize arthrokinematics of shoulder complex
Regain and improve muscular strength of glenohumeral and scapular muscle
Improve neuromuscular control of shoulder complex
Enhance proprioception and kinesthesia
Criteria to Progress to Phase II:
Full functional ROM
Minimal pain or tenderness
“Good” MMT
Initiate Isotonic Strengthening
Internal rotation (sidelying dumbbell)
External rotation (sidelying dumbbell)
Scaption to 90 degrees
Abduction to 90 degrees
Prone horizontal abduction
Prone rows
Prone extensions
Biceps
Lower trapezius strengthening
Initiate Eccentric (surgical tubing) Exercises at Zero Degrees Abduction
Internal rotation
External rotation
Improve Neuromuscular Control of Shoulder Complex
Rhythmic stabilization drills at inner, mid, and outer ranges of motion (ER/IR, and Flex/Ext)
Initiate proprioceptive neuromuscular facilitation
Scapulothoracic musculature
Glenohumeral musculature
Open kinetic chain at beginning and mid ranges of motion
PNF
Manual resistance
External rotation
Begin in supine position progress to sidelying
Prone rows
ER/IR tubing with rhythmic stabilization
Closed kinetic chain
-
Wall stabilization drills
- Initiated in scapular plane
- Progress to stabilization onto ball
Weight shifts had on ball
-
Initiate core stabilization drills
- Abdominal
- Erect spine
Gluteal strengthening
Continue Use of Modalities (as needed)
Ice, electrotherapy
PHASE III - ADVANCED STRENGTHENING PHASE
Goals:
Enhance dynamic stabilization
Improve strength/endurance
Improve neuromuscular control
Prepare patient for activity
Criteria to Progress to Phase III:
Full non-painful ROM
No pain or tenderness
Continued progression of resistive exercises
Good to normal muscle strength
Continue Use of Modalities (as needed)
Continue Isotonic Strengthening (PRE's)
Fundamental shoulder exercises II
Continue Eccentric Strengthening
Emphasize PNF Exercises (D2 pattern) With Rhythmic Stabilization Hold
Continue to Progress Neuromuscular Control Drills
Open kinetic chain
PNF and manual resistance exercises at outer ranges of motion
Closed kinetic chain
Push-ups with rhythmic stabilization
Progress to unsteady surface
Medicine ball
Rocker board
Push-ups with stabilization onto ball
Wall stabilization drills onto ball
Program Scapular Neuromuscular Control Training
Sidelying manual drills
Progress to RS and movements (quadrant)
Emphasize Endurance Training
Time bouts of exercise 30-60 sec
Increase number of reps
Multiple boots bouts during day
PHASE IV - RETURN TO ACTIVITY PHASE
Goals:
Maintain level of strength/power/endurance
Progress activity level to prepare patient/athlete for full functional return to activity/sport
Criteria to Progress to Phase IV:
Full non-painful ROM
No pain or tenderness
Satisfactory isokinetic test
Satisfactory clinical exam
Continue all exercises as in Phase III
Initiate Interval Sport Program (if appropriate)
Patient Education
REFERENCES
- 1.Kibler WB. The role of the scapular in athletic shoulder function. Am J Sports Med. 1998;26:325–337 [DOI] [PubMed] [Google Scholar]
- 2.Wilk KE, Arrigo CA, Andrews JR. Current concepts: The stabilizing structures of the glenohumeral joint. J Orthop Sports Phys Ther. 1997;25:364–379 [DOI] [PubMed] [Google Scholar]
- 3.Speer KP, Deng X, Borrero S, et al. Biomechanical evaluation of a simulated Bankart lesion. J Bone Joint Surg. 1994;76A:1819–1826 [DOI] [PubMed] [Google Scholar]
- 4.Warren RF, Kornblatt IB, Marchand R. Static factors affecting posterior shoulder instability. Orthop Trans. 1984;89 [Google Scholar]
- 5.Aronen JG, Regan K. Decreasing the incidence of recurrence of first time anterior dislocations with rehabilitation. Am J Sports Med. 1984;12:283–291 [DOI] [PubMed] [Google Scholar]
- 6.Henry JH, Genung JA. Natural history of glenohumeral dislocation revisited. Am J Sports Med. 1982;10:135–137 [DOI] [PubMed] [Google Scholar]
- 7.Hoelen MA, Burgers AMJ, Rozing PM. Prognosis of primary anterior dislocations in young adults. Arch Orthop Trauma Surg. 1990;110:51–54 [DOI] [PubMed] [Google Scholar]
- 8.Hovelius L, et al. Primary Anterior dislocation of the shoulder in young patients: A ten-year prospective study. J Bone Joint Surg. 1996;78A:1677–1684 [DOI] [PubMed] [Google Scholar]
- 9.Kazar B, Relouszky E. Prognosis of primary dislocation of the shoulder. Acta Orthop Scand. 1969;40:216–219 [DOI] [PubMed] [Google Scholar]
- 10.Lephart SM, Warner JJP, Borsa, PA, Fu FH. Proprioception of the shoulder joint in healthy, unstable, and surgically repaired shoulders. J Shoulder Elbow Surg. 1994;3:371–380 [DOI] [PubMed] [Google Scholar]
- 11.McLaughlin HL, MacLellan DI. Recurrent anterior dislocation of the shoulder: A comparative study. J Trauma. 1967;7:191–201 [DOI] [PubMed] [Google Scholar]
- 12.Rowe CR. Prognosis in dislocations of the shoulder. J Bone Joint Surg. 1956;38A:957–977 [PubMed] [Google Scholar]
- 13.Simonet WT, Colfield RH. Prognosis in anterior dislocation. Am J Sports Med. 11084:12:19–23 [DOI] [PubMed] [Google Scholar]
- 14.Tipton CM, Mattes RD, Maynard JA. The influence of physical activity on ligaments and tendons. Med Sci Sports Exerc. 1975;7:165–175 [PubMed] [Google Scholar]
- 15.Yoneda B, Welsh RP, MacIntosh DL. Conservative treatment of shoulder dislocations in young males. J Bone Joint Surg. 1982;64B:254–255 [Google Scholar]
- 16.Hovelius L. Anterior dislocation of the shoulder in teenagers and young adults. Five year prognosis. J Bone Joint Surg. 1987;69A:393–399 [PubMed] [Google Scholar]
- 17.Hovelius L, Eriksson K, Fredin H, et al. Recurrences after initial dislocation of the shoulder. Results of a prospective study of treatment. J Bone Joint Surg. 1983;65:343–349 [PubMed] [Google Scholar]
- 18.Postacchini F, Gumini S, Cinotti G. Anterior shoulder dislocation in adolescents. J Shoulder Elbow Surg. 2000;9:470–474 [DOI] [PubMed] [Google Scholar]
- 19.Marans HJ, Angel KR, Schmeitsch EH, et al. The fate of traumatic anterior dislocation of the shoulder in children. J Bone Joint Surg. 1992;74A:1242–4 [PubMed] [Google Scholar]
- 20.Baker CL, Uribe JW, Whitman C. Arthroscopic evaluation of acute initial anterior shoulder dislocations. Am J Sports Med. 1990;18:25–28 [DOI] [PubMed] [Google Scholar]
- 21.Richards DP, Burkhart SS. Arthroscopic humeral avulsion of the glenohumeral ligament (HAGL) repair. Arthroscopy. 2004;20-Suppl 2:134–141 [DOI] [PubMed] [Google Scholar]
- 22.Spang JT, Karas SG. The HAGL lesion: An arthroscopic technique for repair of humeral avulsion of the glenohumeral ligaments. Arthroscopy. 2005;21:498–502 [DOI] [PubMed] [Google Scholar]
- 23.Wolf EM, Cheng JC, Dickson K. Humeral avulsion of glenohumeral ligaments as a cause of anterior shoulder instability. Arthroscopy. 1995;11:600–607 [DOI] [PubMed] [Google Scholar]
- 24.Blaiser RB, Burkus K. Management of posterior fracture-dislocations of the shoulder. Clin Orthop. 1998;232:197–204 [PubMed] [Google Scholar]
- 25.Schwartz E, Warren RF, O'Brien SJ, et al. Posterior shoulder instability. Orthop Clin North Am. 1987;18:409–19 [PubMed] [Google Scholar]
- 26.Mair SD, Zarzour R, Speer KP. Posterior labral injury in contact athletes. Am J Sports Med. 1998;26:753–758 [DOI] [PubMed] [Google Scholar]
- 27.Kaplan LD, Flanigan DC, Norwig J, et al. Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med. 2005;33:1142–1146 [DOI] [PubMed] [Google Scholar]
- 28.Rodeo SA, Suzuki K, Yamauchi M, et al. Analysis of collagen fibers in shoulder capsule in patients with shoulder instability. Am J Sports Med. 1998;26:634–643 [DOI] [PubMed] [Google Scholar]
- 29.Morris AD, Kemp GJ, Frostick SP. Shoulder electromyography in multidirectional instability. J Shoulder Elbow Surg. 2004;13:24–29 [DOI] [PubMed] [Google Scholar]
- 30.Caspari RB, Geissler WB. Arthroscopic manifestations of shoulder subluxation and dislocation. Clin Orthop 1993;291:54–66 [PubMed] [Google Scholar]
- 31.O'Brien SJ, Warren RF, Schwartz E. Anterior shoulder instability. Orthop Clin North Am. 1987;18:395–408 [PubMed] [Google Scholar]
- 32.Warner JJ, Flatbow EL. Anatomy and biomechanics. In: Bigliani LU, ed. The Unstable Shoulder. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1996 [Google Scholar]
- 33.Beltran J, Rosenberg ZS, Chandnani VP, et al. Glenohumeral instability: Evaluation with MR arthrography. Radiographics 1997;17:657–673 [DOI] [PubMed] [Google Scholar]
- 34.Goubier JN, Duranthon LD, Vandenbussche E, et al. Anterior dislocation of the shoulder with rotator cuff injury and brachial plexus palsy: a case report. J Shoulder Elbow Surg. 2004;13:362–363 [DOI] [PubMed] [Google Scholar]
- 35.Maffet MW, Gartsman GM, Moseley B. Superior labrum-biceps tendon complex lesions of the shoulder. Am J Sports Med. 1995;23:93–98 [DOI] [PubMed] [Google Scholar]
- 36.Smith RL, Brunoli J. Shoulder kinesthesia after anterior glenohumeral joint dislocation. Phys Ther. 1989;69:106–112 [DOI] [PubMed] [Google Scholar]
- 37.Blasier RB, Carpenter JE, Huston LJ. Shoulder proprioception. Effect of joint laxity, joint position, and direction of motion. Orthop Rev. 1994;23:45–50 [PubMed] [Google Scholar]
- 38.Zuckerman JD, Gallagher MA, Lehman C, et al. Normal shoulder proprioception and the effect of lidocaine injection. J Shoulder Elbow Surg. 1999;8:11–6 [DOI] [PubMed] [Google Scholar]
- 39.Rockwood CA, Burkhead WZ: Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg. 1992;74A:890–896 [PubMed] [Google Scholar]
- 40.Arciero RA, Wheeler JH, Ryan JB, et al. Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med. 1994;22:589–594 [DOI] [PubMed] [Google Scholar]
- 41.Larrain MV, Botto GJ, Montenegro HJ, et al. Arthroscopic repair of acute traumatic anterior shoulder dislocation in young athletes. Arthroscopy. 2001;17:373–377 [DOI] [PubMed] [Google Scholar]
- 42.Wheeler JH, Ryan JB, Arciero RA, et al. Arthroscopic versus nonoperative treatment of acute shoulder dislocations in young athletes. Arthroscopy. 1989;5:213–217 [DOI] [PubMed] [Google Scholar]
- 43.Kiviluoto O, Pasila M, Jaromea H, Sundholm A. Immobilization after primary dislocation of the shoulder. Acta Orthop Scand. 1980;51:915–919 [DOI] [PubMed] [Google Scholar]
- 44.Itoi E, Sashi R, Minigawa H, et al. Position of immobilization after dislocation of the glenohumeral joint. A study with use of magnetic resonance imaging. J Bone Joint Surg. 2002;84A:873–8744 [DOI] [PubMed] [Google Scholar]
- 45.Itoi E, Hatakeyama Y, Kido T. A new method of immobilization after traumatic anterior dislocation of the shoulder: a preliminary study. J Shoulder Elbow Surg. 2003;12:413–415 [DOI] [PubMed] [Google Scholar]
- 46.Dehre E, Tory R. Treatment of joint injuries by immediate mobilization based upon the spinal adaption concept. Clin Orthop. 1971;77:218–232 [PubMed] [Google Scholar]
- 47.Haggmark T, Eriksson E, Jansson E. Muscle fiber type changes in human muscles after injuries and immobilization. Orthopaedics. 1986;9:181–189 [DOI] [PubMed] [Google Scholar]
- 48.Salter RB, Hamilton HW, Wedge JH. Clinical application of basic science research on continuous passive motion for disorders of injuries and synovial joints. J Orthop Res. 1984:1:325–333 [DOI] [PubMed] [Google Scholar]
- 49.Reinold MM, Wilk KE, Macrina LC, et al. The effect of electrical stimulation of the infraspinatus on shoulder external rotation force production following rotator cuff repair surgery. Presented at American Physical Therapy Association Combined Sections Meeting, February, 2005 [Google Scholar]
- 50.Carpenter JE, Blaiser RB, Pellizon GG. The effects of muscle fatigue on shoulder joint position sense. Am J Sports Med 1998:26:262–265 [DOI] [PubMed] [Google Scholar]
- 51.Ellenbecker TS, Mattalino AJ. The elbow in sport. Champaign, IL: Human Kinetics; 1997;171–177 [Google Scholar]
- 52.Reinold MM, Wilk KE, Reed J, et al. Interval sport programs: Guidelines for baseball, tennis and golf. J Orthop Sports Phys Ther. 2002;32:293–298 [DOI] [PubMed] [Google Scholar]
- 53.Wilk KE, Reinold MM, Andrews JR. Postoperative treatment principles in the throwing athlete. Sports Med Arthrosc Rev. 2001;9:69–95 [Google Scholar]
- 54.Wilk KE, Andrews JR, Arrigo CA, et al. The strength characteristics of internal and external rotator muscles in professional baseball pitchers. Am J Sports Med. 1993;21:61–66 [DOI] [PubMed] [Google Scholar]
- 55.Wilk KE, Andrews JR, Arrigo CA: The abductor and adductor strength characteristics of professional baseball pitchers. Am J Sports Med. 1995;23:307–311 [DOI] [PubMed] [Google Scholar]
- 56.Barden JM, Balyk R, Raso VJ, et al. Atypical shoulder muscle activation in multidirectional instability. Clin Neurophysiol. 2005;116:1846–1857 [DOI] [PubMed] [Google Scholar]
- 57.Kronberg M, Brostrom LA, Nemeth G. Differences in shoulder muscle activity between patients with generalized joint laxity and normal controls. Clin Orthop Relat Res. 1991;269:181–192 [PubMed] [Google Scholar]
- 58.Myers JB, Ju YY, Hwang JH, et al. Reflexive muscle activation alterations in shoulders with anterior glenohumeral instability. Am J Sports Med. 2004;32:1013–1021 [DOI] [PubMed] [Google Scholar]
- 59.von Eisenhart-rothe R, Jager A, Enlmeier KH, et al. Relevance of arm position and muscle activity on three-dimensional glenohumeral translation in patients with traumatic and atraumatic shoulder instability. Am J Sports Med. 2002;30:514–522 [DOI] [PubMed] [Google Scholar]
- 60.Misamore GW, Sallay PI, Didelot W. A longitudinal study of patients with multidirectional instability of the shoulder with seven- to ten-year follow-up. J Shoulder Elbow Surg. 2005;14:466–470 [DOI] [PubMed] [Google Scholar]
- 61.Wilk KE, Arrigo CA. Current concepts in the rehabilitation of the athletic shoulder. J Orthop Sports Phys Ther. 1993;18:365–378 [DOI] [PubMed] [Google Scholar]
- 62.Wilk KE, Voight ML, Keirns MA, et al. Stretch-shortening drills for the upper extremities: Theory and clinical application. J Orthop Sports Phys Ther. 1993;17:225–239 [DOI] [PubMed] [Google Scholar]