Abstract
Background
As physical therapy gradually evolves into a more autonomous profession, physicians continue to play a major role in the clinical practice of physical therapists, particularly as a source of patient referral. The analysis of physicians' referrals to physical therapy may be a practical and effective way to study the relationship between physicians and physical therapists.
Objectives
The objective of this study was to identify the primary reasons for physicians' referrals to an outpatient physical therapy clinic and to determine whether further diagnosis by the physical therapist is necessitated prior to treatment.
Methods
Between January 1, 2001 and March 31, 2003, 544 consecutive physicians' referrals were received in a rural physical therapy outpatient clinic. Physicians' specialties, diagnosis on referral (or reason for referral, if diagnosis not provided), and prescribed orders on referral were all reviewed by the authors.
Results
One-third (33%) of the referrals were sent to physical therapy with no medical diagnosis (non-specified referrals - NSRs), and the most common reason for the referral in this NSR category was “pain” (88%). Commonly recommended treatments accompanying the NSRs included: evaluation & treatment (60%) and routine rehabilitation protocol (24%) for the relevant joints.
Conclusion
One-third (33%) of the referrals sent to physical therapy included no medical diagnosis, with the most common reason for the referral listed as “pain.” Evaluation and treatment was the most recommended treatment accompanying these non-specific referrals (almost 2/3). Physical therapists cannot properly manage patients based on a physician referred diagnosis of “pain,” therefore, it is necessary for physical therapists to make further diagnoses.
Keywords: physical therapy, decision-making, autonomy
INTRODUCTION
Over 20 years ago, physicians played a dominant role in interaction between the physician and the physical therapist (PT). The PT functioned as a technician in a prescriptive role by following the order from the referring physician.1 The referring physician assumed the responsibilities and duties of evaluation, diagnosis, and determination of specific therapeutic interventions and modalities.1 Most physicians perceived the PT as a technician rather than a professional colleague.2–4 Physicians believed that the PT lacked the most complex criteria of medical professionalism: examination and evaluation skills and autonomy of judgment.3
However, the role of physical therapy has been changing rapidly in the past 5 to 10 years. In 2000, the American Physical Therapy Association (APTA) adopted Vision 2020, in which five key areas became the focus of the APTA to make physical therapy a more autonomous profession by the year 2020.5 These key areas include professionalism, direct access, the doctor of physical therapy degree, evidence-based practice, and the PT as the practitioner of choice.5 Achieving significant progress in these key areas will prepare and enable PTs to interact with physicians on a more collegial level and less as “subservient followers of orders”.6 Currently, the PT is assuming greater responsibility for initial assessment and management of musculoskeletal conditions.7–10 Actually, the PT has been functioning as the primary evaluator of neuromusculoskeletal conditions with success in the United States Army since the early 1970s.1 In reaction to this decades-long history of the PT being the autonomous practitioner of choice in the Army, some researchers have suggested that the PT must demonstrate that they have the expertise in examination and treatment of musculoskeletal conditions to assume new roles in healthcare, to increase visibility within healthcare organizations, and to gain more autonomy as professionals.1,9
Ritchey et al11 reported that the role expansion of physical therapy is not likely to occur easily because of the “turf battle” with physicians. The PT is seldom placed in a position to dispute or challenge a physician's decision, or make a physician feel his/her competency is being questioned by subordinates.11 While physical therapy has a long history of clinical practice with some level of autonomy regarding patient intervention, an equally long tradition of consulting with physicians also exists. Additionally, the cognitive and evaluative tasks the PT performs have tended to be secondary or supportive, if not supplementary, to a physician's examination, evaluation, and diagnosis.
The American Medical Association and the American Academy of Orthopedic Surgeons oppose independent practitioner status for the PT because of concerns about improper diagnosis, inappropriate care, and the potential for increased costs.12 Ironically, several physician survey studies indicated that the majority of responding physicians did not know enough about physical therapy services.2,3,13,14 One study identified two areas that physicians lacked familiarity with physical therapy; the first being knowledge of how the PT evaluates their patients and the second being knowledge of modalities used by the PT and how such treatments are performed.13 Recently, physicians' knowledge of physical therapy was surveyed again revealing similar findings.14 These studies advocate for continuing education courses for physicians to increase their knowledge about physical therapy; suggestions that have been supported by the physician participants in the survey studies.2,13,14
Recently, a trend has developed for states to pass laws allowing patients to have direct access to physical therapy. Also, an increasing number of physical therapy education programs in the United States are progressing to the doctor of physical therapy degree program. Physical therapy autonomy is becoming one of the most discussed issues related to daily physical therapy practice. According to the APTA Board of Directors, physical therapy autonomy is characterized by independent and self- determined professional judgment and action during practice.15 In other words, under direct access, the PT needs to be able to independently examine, evaluate, diagnose, and treat patients within their scope of practice.
All of these issues suggest there might be a “turf battle” between the PT and the physician, with one side trying to gain greater professional autonomy and role expansion and the other side opposing such expansion. Thus, analysis of physicians' referrals to physical therapy may be a practical and effective way to study the relationship between the physician and the PT. The purpose of this study was to identify the primary reasons for physicians' referrals to an outpatient physical therapy clinic and to determine whether further diagnosis by the PT is necessary prior to treatment.
METHODS
Between January 1, 2001 and March 31, 2003, 544 consecutive physicians' referrals were received in a physical therapy outpatient clinic located between two metropolitan settings in the southeastern United States. For each referral, physician's specialty, referral diagnosis (or reason for referral, if diagnosis was not provided), and prescribed orders on the referral were reviewed by the authors. No informed consent or institutional review board approval was required because the data collection did not require an intervention or an interaction with a living person and no identifiable private information was obtained or contained for this study in a form associable with any individual(s).
RESULTS
Specialty of the Physician
Among 544 referrals from 78 physicians (67 medical doctors, 9 doctors of osteopathy, and 2 podiatrists), 59% of the referrals (321 of 544) were from orthopedists, and 32% (176 of 544) were from family or internal medicine practitioners.
Orthopedic surgeons, family physicians, and internal medicine physicians combined accounted for 91% of the total referrals. The remaining 9% of referrals came from physicians who specialized in neurology (2%), rehabilitation medicine (2%), pain management/anesthesiology (2%), podiatry (1%), general surgery (1%), and otolaryngology (1%).
Reason Provided on Referral
Out of the 544 referrals, 67% (367 of 544) included a specific medical diagnosis in the referral and for purposes of this study were categorized as specified referrals (SRs). (Table 1). The other 33% (177 of 544) did not include a specific medical diagnosis and were categorized as non-specified referrals (NSRs). Since theses NSRs included symptoms (pain, dizziness, weakness) rather than a specific medical condition, these referrals are considered “reasons for referral” rather than diagnoses. Of these 177 NSRs, in 88% (156 of 177) the reason for referral was “pain” (knee pain, back pain, etc).
Table.
Reasons for Referral to Physical Therapy
| Reason | Frequency | Percentage (%) of Total Referrals |
|---|---|---|
| Pain only or specified referral | 367 | 67% |
| Non-specified referral | 177 | 33% |
| Total | 544 referrals | 100% |
To further analyze the data, referrals specifically related to surgery were separated from non-surgical referrals. Among all referrals, 22% (118 of 544) specifically were related to post surgery and had a specific diagnosis included in the referral. The most common post-surgical referrals were for knee arthroscopy, total knee replacement, and rotator cuff repair. In contrast, 78% of all referrals (426 of 544) were non-surgical related referrals.
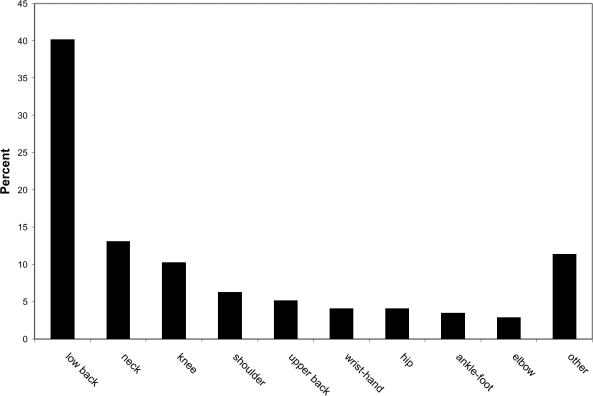
Of the 426 non-surgery related referrals, 249 (58.4%) of them were referred with a specific medical diagnosis (SRs), and 177 (41.6%) were referred without any medical diagnosis (NSRs). Based on the anatomical location of the reason for the referral, the lower back, ankle-foot, shoulder, knee, and neck were the top five locations across all non-surgery related referrals (NSRs and SRs combined; Table 2). Among the 249 SRs, the lower back, ankle-foot, shoulder, knee, and neck were the top five sites of complaints. According to the medical diagnoses on the 249 SRs, lumbar strain, rotator cuff tendonitis/impingement, ankle sprain, cervical strain, and knee osteoarthritis were the top five diagnoses on the specified referrals. (Listed in Table 3 are the three most common physicians' diagnoses for each anatomical location for the SRs.) Further analysis of the 177 NSRs revealed that the low back was the most frequent anatomic location for the reason for the referral. (Figure)
Table 2.
Location of Non-Surgery Related Referrals
| Low Back | Ankle-Foot | Shoulder | Knee | Neck | Upper Back | Wrist-Hand | Hip | Elbow | Other area(s) | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Specified Referrals | 67 | 53 | 43 | 26 | 17 | 8 | 10 | 8 | 4 | 15 | 249 |
| Non-specified Referrals | 71 | 6 | 11 | 18 | 23 | 9 | 7 | 7 | 5 | 20 | 177 |
| Subtotal | 138 | 59 | 54 | 44 | 40 | 17 | 17 | 13 | 9 | 35 | 426 |
Table 3.
Categorization of Diagnoses on the Specified Referrals
| Pain Area | Most Commonly Referred Diagnoses |
| Neck | cervical strain, cervical degenerative disease, cervical disk herniation |
| Upper Back | trapezius spasm/strain, whiplash, thoracic strain |
| Low Back | lumbar strain, post diskectomy (> 1 year post-surgery), lumbar radiculopathy |
| Shoulder | rotator cuff tendonitis, impingement, humeral fracture, rotator cuff tear |
| Elbow | elbow tendonitis, radial head fracture, minor league syndrome |
| Wrist - Hand | cubital tunnel syndrome, fracture, tendonitis |
| Hip | trochanteric bursitis, ischial tuberosity bursitis, sacroiliac joint dysfunction |
| Knee | osteoarthritis, patellofemoral syndrome, patellar subluxation/dislocation |
| Ankle - Foot | ankle sprain, plantar fasciitis, achilles tendonitis |
| Systemic / Other | fibromyalgia, temporomandibular joint dysfunction, post-polio syndrome, rheumatoid arthritis |
FIGURE.
Location on Non-Specified Referrals
Prescribed Orders on Referrals
As seen in Table 4, the most commonly prescribed orders made by physicians on the 544 referrals were evaluation and treatment (47%), routine rehabilitation protocol (22%) for the relevant joints (i.e. routine knee rehab), strengthening and range of motion (15%), and specified modalities (13%). The most commonly recommended orders on the 177 NSRs included evaluation and treatment (60%), routine rehabilitation protocol (24%), and strengthening and range of motion (9%). Among those 22% (118 of 544) of referrals (including both SRs and NSRs) with routine rehabilitation protocol as the prescribed order, 11 of the 118 (9%) were accompanied with either a copy of the treatment protocol (9 of 11) or a reference to a published book or article (2 of 11). However, 107 of the 118 (91%) referrals presented no details of the treatment protocol. Of these 109 referrals, most came from orthopedists (51%) or family/internal medicine physicians (39%).
Table 4.
Recommended Action / Orders on Referrals
| Orders | All Referrals | Only Non-Specified Referrals | ||
|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | |
| Evaluate & Treat | 254 | 47% | 107 | 60% |
| Routine Rehab Protocol | 118 | 22% | 42 | 24% |
| Strengthening & Range of Motion | 82 | 15% | 16 | 9% |
| Modalities Only | 74 | 13% | 8 | 5% |
| Other | 16 | 3% | 4 | 2% |
| Total | 544 | 100% | 177 | 100% |
DISCUSSION
Physician Specialties
More and more states are passing direct access to physical therapy laws, but the long-standing trend continues to be that third parties such as Medicare, Medicaid, and private insurance companies reimburse physical therapy services only if the physical therapy service is prescribed by a physician.16 Therefore, physicians continue to play a major role in referral of patients to physical therapy and the prescription of physical therapy services seems to be determined, in part, by physician specialties and patients' insurance status. Namely, orthopedic surgeons, followed by general practitioners and internal medicine specialists, are still the main referral sources for physical therapy.11,17,18
Likewise, this study showed similar results with orthopedists (59%) and family and internal medicine practitioners (32%) accounting for 91% of the total referrals.
Reason for Referral and Physical Therapy Autonomy
The physician members of the American Medical Association and the American Academy of Orthopedic Surgeons have traditionally opposed increased autonomy by physical therapists in the practice of physical therapy.12 Yet, as the primary source of referrals to physical therapy, their non-specified referrals from physicians are somewhat inconsistent with this viewpoint. This study identified pain, muscle weakness, and decreased range of motion (all of which are impairments/symptoms) as the three most common reasons physicians referred their patients to out-patient physical therapy. Interestingly, one-third (33%) of the referrals did not have a medical diagnosis with the most frequent location of the complaint being the lower back and the most frequent reason for the referral being “pain.” Clearly, additional skillful, independent examination and assessment of the patient by the PT is warranted in such instances. Two things may potentially be inferred from this finding. First, referring physicians may view the PT as a consultant/ expert rather than as a subordinate with regard to management of some patients with musculoskeletal conditions. Secondly, a PT may be empowered to view him/herself more as a physician's colleague rather than a technician or subordinate. Such ideals are also facilitated by the progression of physical therapy education to the doctor of physical therapy degree level, characterized by greater breadth and depth of content and instruction in skilled, proactive, and independent clinical decision making. Physical therapists do not identify disease in the sense of pathology, but they do identify clusters of signs, symptoms, and other relevant information from subjective and objective examination of the patient. These clusters can be labeled as classifications or diagnoses by the PT.19 Based on the present study, pain is the most common impairment that the PT encounters in an outpatient setting. Thus, the ability to understand and differentiate the multitude of signs and symptoms relevant to pain and then to be able to synthesize this information with data from patient history, and radiology and lab test results will greatly assist the PT in the management of their patients, especially in instances where medical diagnosis information from the referring physician is lacking.
Brogan17 reported that physicians probably do not recognize the extent to which their patients need physical therapy services and, in addition, may not adequately refer their patients for such physical therapy services. This might be due to the lack of physicians' knowledge of physical therapy, which was indicated by a study performed 20 years ago by Stanton et al,14 and also by another similar but more recent study by English et al.13 These studies recommended increased and enhanced communication between the physician and the PT and that the physician should learn more about physical therapy. Olsen20 encouraged increased communication between the PT and their referral sources not only for marketing purposes, but also for improved patient management. A study by Hendriks et al21 suggested that primary care physicians seek a one-time physical therapy consultation as an appropriate and beneficial component of the primary care patient management process.
Physician referrals to physical therapy have been studied by others.4,11,22 Twenty years ago, physicians often did a physical therapy referral for patients with the assumption that the patient was not in need of any further assessment, evaluation, or decision-making by the PT.22 Several years later, Ritchey et al11 found that 30% of physicians gave no diagnosis on the physical therapy referral, which is similar to results of this study (29%). Hulme et al22 reported that although both physicians and physical therapists agreed that inclusion of the medical diagnosis on physical therapy referrals was a priority, many physical therapists reported the diagnosis was often omitted from referrals, was incomplete, or was a list of impairments/symptoms rather than a medical diagnosis. In the view of the PT, even a preliminary diagnosis was important for the purposes of serving as a starting place for the examination and evaluation and for assistance in excluding many pathological conditions that may cause the symptoms.22
Further discussion regarding physician support of greater autonomy in physical therapy practice relates to decision-making regarding plan of care and interventions. According to this study, a substantial number of referrals state “evaluate and treat” (47% of all referrals). Among the NSRs, the percentage is 60% of NSR referrals. These observations seem to add additional support to the notion that greater autonomy of the PT, regarding all aspects of patient management, is being encouraged by physicians by the nature of their physical therapy referrals.
Future Study
In future research, data should be collected on a larger number of referrals from both rural and urban outpatient physical therapy clinical settings in different geographic areas of North America. Any association between physicians' years of working experience and the frequency of specified and non-specified referrals should be investigated. Also, future research should focus on the relationship between physician specialty and any prescribed orders, recommended treatment duration, radiological or laboratory documentation, and treatment precautions stated on referrals. Such investigations, in combination with the results of the present study, will further assist both physicians and physical therapists in understanding their roles in the contemporary healthcare environment and may also serve to identify some continuing education needs of both professions.
CONCLUSION
Review of 544 physician referrals to a physical therapy outpatient clinic indicated that 1/3 (33%) of the referrals included no medical diagnosis. Within these non-specified referrals, “pain” was the reason listed most frequently (88%) and the low back was the most frequent location (40%). However, pain is a symptom/impairment rather than a medical diagnosis. Physical therapists cannot properly manage patients based on a referred diagnosis of “pain,” making it necessary for the PT to make further diagnoses. Greater independence and involvement in the diagnostic process, as well as patient management in general, is indirectly encouraged through non-specific physician referrals.
Footnotes
Material in this manuscript was presented at the 2004 Combined Section Meeting of American Physical Therapy Association in Nashville, TN in Feburary 2004
REFERENCES
- 1.James JJ, Stuart RB. Expanded role for the physical therapist. Phys Ther. 1975;55:121–131 [DOI] [PubMed] [Google Scholar]
- 2.Dunkel RH. Survey of attitudes of Arkansas physicians and physical therapists toward the professional capacity of the physical therapist. Phys Ther. 1974;54:584–587 [DOI] [PubMed] [Google Scholar]
- 3.Silva DM, Clark SD, Raymond G. California physicians' professional image of physical therapists. Phys Ther. 1981;61:1152–1157 [DOI] [PubMed] [Google Scholar]
- 4.Uili RM, Shepard KF, Savinar E. Physician knowledge and utilization of physical therapy procedures. Phys Ther. 1984;64:1523–1530 [DOI] [PubMed] [Google Scholar]
- 5.Massey BF. Making vision 2020 a reality. Phys Ther. 2003;83:1023–1026 [PubMed] [Google Scholar]
- 6.Rothstein JM. Autonomy or professionalism? Phys Ther. 2003;83:206–207 [PubMed] [Google Scholar]
- 7.Monahan B. Autonomy, access and choice: New models of primary care. PT Magazine. 1996;4:54–58 [Google Scholar]
- 8.Monahan B. Physical therapists as primary care providers. PT Magazine. 1994;2:46–49 [Google Scholar]
- 9.Smith KL, Tichenor CJ, Schrodeer M. Orthopaedic residency training: A survey of the graduates' perspective. J Orthop Sports Phys Ther. 1999; 29:635–655 [DOI] [PubMed] [Google Scholar]
- 10.Tichenor CJ. Kaiser Permanente moves forward with physical therapists in primary care. Orthop Phys Ther Pract. 1998;10:19 [Google Scholar]
- 11.Ritchey FJ, Pinkston D, Goldbaum JE, et al. Perceptual correlations of physician referral to physical therapists: Implications for role expansion. Soc Sci Med. 1989;28:69–80 [DOI] [PubMed] [Google Scholar]
- 12.Barr J. It's time to be direct about direct access. Physical Therapy Today. Spring, 1991 [Google Scholar]
- 13.Stanton PE, Fox FK, Franfos KM, et al. Assessment of resident physicians' knowledge of physical therapy. Phys Ther. 1985;65:27–30 [DOI] [PubMed] [Google Scholar]
- 14.English ML, Rudy DL, Castle JM, Mesnard C. Collaborative education in an internal medicine residents' clinic. Proceedings of the American Physical Therapy Association, Combined Sections Meeting, Nashville, TN, February 2004 [Google Scholar]
- 15.American Physical Therapy Association Board of Directors Autonomous physical therapist practice: Definition and privileges. In: Professional and Societal Policies, Positions, and Guidelines. Alexandria, VA: American Physical Therapy Association; July, 2004 [Google Scholar]
- 16.Jette AM, Davis KD. A comparison of hospital-based and private outpatient physical therapy practices. Phys Ther. 1991;71:366–75; discussion 376-81 [DOI] [PubMed] [Google Scholar]
- 17.Brogan DR. Rehabilitation service needs: Physicians' perceptions and referral. Arch Phys Med Rehab. 1981;62:215–219 [PubMed] [Google Scholar]
- 18.Freburger JK, Holmes GM, Carey TS. Physician referrals to physical therapy for the treatment of musculoskeletal conditions. Arch Phys Med Rehab. 2003;84:1839–1849 [DOI] [PubMed] [Google Scholar]
- 19.Delitto A, Snyder-Mackler L. The diagnostic process: Examples in orthopedic physical therapy. Phys Ther. 1995;75:203–211 [DOI] [PubMed] [Google Scholar]
- 20.Olsen D. A descriptive survey of management and operations at selected sports medicine centers in the United States. J Orthop Sports Phys Ther. 1996;24:315–322 [DOI] [PubMed] [Google Scholar]
- 21.Hendriks EJ, Kerssens JJ, Nelson RM, et al. One-time physical therapist consultation in primary health care. Phys Ther. 2003;83:918–931 [PubMed] [Google Scholar]
- 22.Hulme JB, Bach BW, Lewis JW. Communication between physicians and physical therapists. Phys Ther. 1988;68:26–31 [DOI] [PubMed] [Google Scholar]