Abstract
Sports related injuries to the hip have received relatively little attention, in the part because the clinical assessment, imaging studies, and surgical techniques are less sophisticated. The evolution of hip arthroscopy has offered a less invasive technique that allows for recognition and treatment of hip pathologies that previously went unrecognized. The success of hip arthoscopy is dependent on proper patient selection based on the patient's history and diagnosis. The purpose of this clinical commentary is to outline mechanisms of injury and specific lesions that can be addresses using hip arthoscopy.
INTRODUCTION
Sports related injuries to the hip joint have received relatively little attention. This trend is changing but, until recently, few publications exist in peer reviewed journals and the topic has rarely been presented at scientific meetings. This lack of attention is due to three reasons. First, perhaps hip injuries are less common than other joints. Secondly, investigative skills for the hip have been less sophisticated, including clinical assessment and imaging studies. Thirdly, fewer interventional methods are available to treat the hip including both surgical techniques and conservative modalities and, thus, little impetus exists to delve into this unrecognized area.
The evolution of arthroscopy has been intimately tied to sports medicine. The motivating principle has been a less invasive technique that facilitates quicker return to unrestricted athletics. It is now recognized that this basic sports medicine principle applies well to all individuals, whether the goal is to accomplish an earlier return to the work place or simply a return to normal daily activities.
However, hip arthroscopy has followed a distinctly different route. It began as a surgical alternative to only a few recognized forms of hip pathology. These pathologies included removal of loose bodies that could otherwise only be addressed by an extensive arthrotomy and arthroscopic debridement for degenerative arthritis in an effort to postpone the need for hip arthroplasty.1,2
Neither of these early indications found much application in an athletic population. However, as the basic methods of hip arthroscopy were developed, arthroscopy became an option for select cases of unexplained hip pain. Arthroscopy revealed numerous intra-articular sources of disabling hip symptoms that were previously unrecognized but are potentially amenable to arthroscopic intervention.3,4 These pathologies include tearing of the acetabular labrum, traumatic injury to the articular surface, and damage to the ligamentum teres, among others.
The indications for hip arthroscopy fall into two broad categories. In one catagory, arthroscopy offers an alternative to traditional open techniques previously employed for recognized forms of hip pathology such as loose bodies or impinging osteophytes. In the second category, arthroscopy offers a method of treatment for disorders that previously went unrecognized including labral tears, chondral injuries, and disruption of the ligamentum teres. Most athletic injuries fall into this latter category. In the past, athletes were simply resigned to living within the constraints of their symptoms, often ending their competitive careers, diagnosed as a chronic groin injury. Based on the results of arthroscopy among athletes, it is likely that many of these careers could have been resurrected with arthroscopic intervention.5
MECHANISM OF INJURY
The mechanism of injury can be as varied as the sports in which athletes participate. In general, hip disorders attributable to a significant episode of trauma tend to respond better to arthroscopy.6 This positive response is because, other than the damage due to trauma, the athlete usually has an otherwise healthy joint. Insidious onset of symptoms usually suggests either underlying disease or some predisposition to injury that cannot be fully reversed and may leave the joint vulnerable to further deterioration in the future. Therefore, individuals who simply develop progressive onset of symptoms in absence of injury tend to experience a less complete response. Even an acute injury such as a twisting episode, which is known to cause a tear of the acetabular labrum, may be more likely if the labrum is vulnerable to injury and may represent a less certain response to surgery. This vulnerability can be due to abnormal labral morphology or underlying degeneration.
However, these broad generalizations must be tempered in the competitive athlete. Individuals who participate in contact and collision sports simply may not be able to recount which traumatic episode led to the onset of symptoms. Remember that significant intra-articular damage can occur from an episode without the athlete developing incapacitating pain. The athlete may be able to continue to compete and subsequently undergo work-up only when symptoms fail to resolve. Injury can occur from any contact or collision sport or sports involving forceful or repetitive twisting of the hip. The aging joint may also be more vulnerable. These parameters do not exclude many sports.
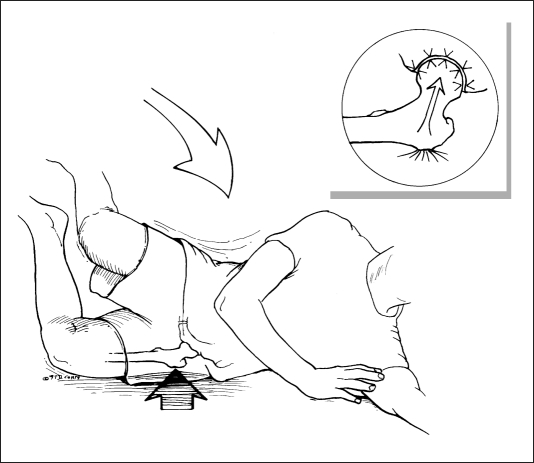
A particular entity that has been identified associated with acute chondral damage7 is a lateral impact injury to the area of the trochanter (Figure 1). Because young adult males are more apt to be participating in contact and collision activities where this mechanism is frequent, this injury is most commonly encountered in this population. With good body conditioning and little adipose tissue overlying the trochanter, much of the force of the blow is delivered directly to the bone. This force is then transferred, unchecked, into the hip joint, resulting in either shearing of the articular surface on the medial aspect of the femoral head at the tide mark, or compression of the articular surface on the superior medial acetabulum, exceeding its structural threshold. The result is a full thickness articular fragment from the femoral head or articular surface breakdown of the acetabulum, possibly with loose bodies, depending on the magnitude of acetabular chondral, or chondro-osseous cell death (Figures 2 and 3). This mechanism is dependent on peak bone density as otherwise the force would result in fracture rather than delivery of the energy to the surface of the joint. The injury usually results in immediate onset of symptoms but may not be disabling. The problem may be assessed as a groin pull, with work-up ensuing only when symptoms persist.
Figure 1.
Fall results in direct blow to the greater trochanter and, in absence of fracture, the force generated is transferred unchecked to the hip joint. (Reprinted with permission J.W. Thomas Byrd, M.D.)
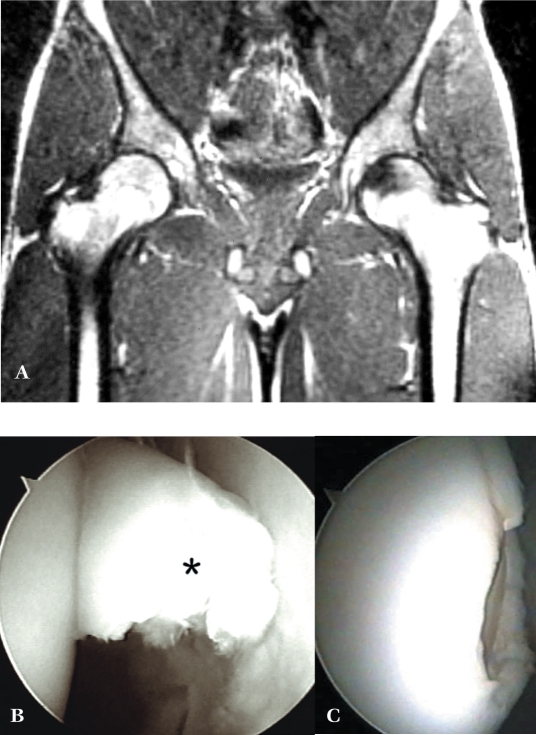
Figure 2.
A 20-year-old male collegiate basketball player with painful catching of the left hip following a fall with lateral impaction of the joint. A. MRI revealed extensive signal changes in the medial aspect of the femoral head characterizing the subchondral injury associated with his fall. B. A full-thickness chondral flap lesion (*) associated with the injury is identified. C. The unstable portion has been excised. (Reprinted with permission.3)
Figure 3.
A. AP radiograph left hip unremarkable. B. Radionuclide scan reveals increased activity, left hip. C. MRI remarkable for pronounced asymmetric effusion, left hip. D. CT coronal reconstruction demonstrates loose bodies. E. Follow-up radiograph 13 months post-injury reveals secondary changes wth superolateral osteophyte formation on the femoral head. F. Loose bodies are evident (*) originating from the acetabulum. Scoring of the femoral head is also evident (arrow) due to third body wear. (Reprinted with permission J.W. Thomas Byrd, M.D.)
Ice hockey is a sport with a particularly high prevalence of hip pathology. Hip flexibility is a premium consideration in this sport. The joint is subjected to violent and repetitive torsional maneuvers and is also subjected to relatively high velocity impact loading. Thus, the labrum is susceptible to tearing from the twisting maneuvers while the articular surface is vulnerable to impact injury. Often, acute episodes are simply superimposed on the cumulative effect of years of exposure (Figure 4).
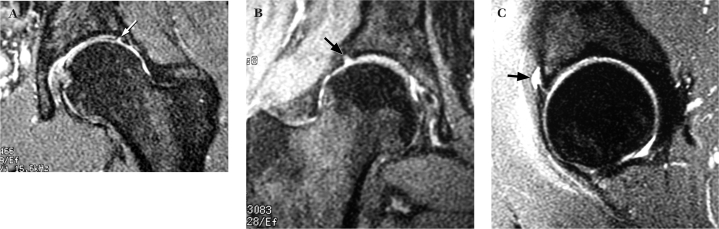
Figure 4.
Three NHL hockey players were referred, each with a two week history of hip pain following an injury on the ice. Each case demonstrated MRI evidence of labral pathology (arrows). These cases were treated with two weeks of rest followed by a two week period of gradually resuming activities. Each of these athletes was able to return to competition and have continued to play for several seasons without needing surgery. A. Coronal image of a left hip demonstrates a lateral labral tear (arrow). B. Coronal image of a right hip demonstrates a lateral labral tear (arrow). C. Sagittal image of a left hip demonstrates an anterior labral tear with associated paralabral cyst (arrow). (Reprinted with permission J.W. Thomas Byrd, M.D.)
Golf is another illustrative sport that seems to have a predilection for precipitating hip symptoms. It is not a contact or collision sport, but the golf swing does incorporate a significant element of twisting of the hip joint. Additionally, golf is a sport where participants can compete with advancing age, even at the professional level. Thus, there is a greater susceptibility to injury of an aging hip as well as the cumulative effect of repetitive trauma over a prolonged career. Tennis shares many of these same attributes.
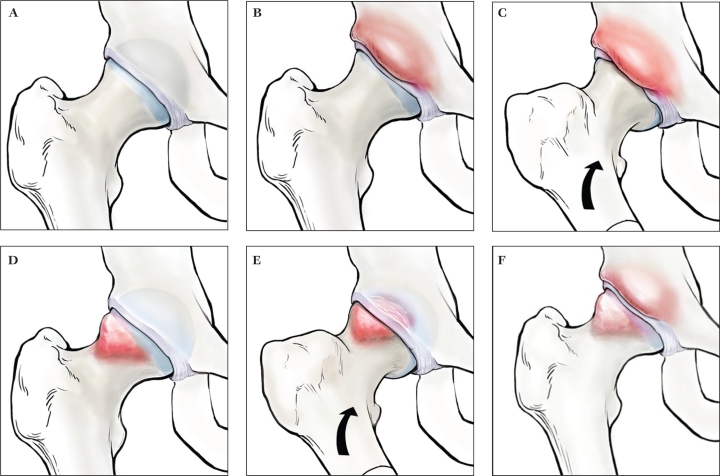
Femoro-acetabular impingement (FAI) is a condition that warrants particular attention.8 Abnormal morphology of the joint can lead to labral and articular breakdown commonly encountered in active individuals (Figure 5). Two types of impingement exist. Pincer impingement occurs from a bony prominence of the anterior acetabulum that crushes the labrum when it is compressed against the proximal femur during hip flexion. Cam impingement is created by a non-spherical femoral head that engages against the articular cartilage of the acetabulum during flexion and results in shear failure of the surface.
Figure 5.
A. Normal joint morphology. B. Pincer lesion created by prominence of anterior acetabulum. C. Joint damage and pain is created by crushing of the labrum underneath the pincer lesion with hip flexion. D. Cam lesion is characterized by bony prominence of anterolateral femoral head/neck junction. E. Pathology and pain develops due to shearing of the acetabular articular surface by a bump during hip flexion. F. Combined pincer and cam impingement can occur. (Reprinted with permission J.W. Thomas Byrd, M.D.)
Pincer impingement is most common in females, especially as they approach middle age. Cam impingement is seen more frequently in young adult males. Cam impingement is also a cause of early onset osteoarthritis of men in their fifth and sixth decades. However, joint destruction is being observed among males in their second and third decades, accelerated by the intensity of competitive sports and activities.
Athletic pubalgia is characterized by a constellation of tendonopathy surrounding the insertion of the lower abdominal muscles, the origin of the hip adductors, and the pelvic floor.9 A significant correlation of FAI and athletic pubalgia in high demand athletes, predominantly male. Diminished hip range of motion is compensated by increasing pelvic motion, which overworks the pelvic stabilizers and results in tissue breakdown of the pelvic structures, culminating in athletic pubalgia. Clinically, difficulty exists in distinguishing the two conditions. The two conditions commonly co-exist, but can also occur separately.
Historically, rupture of the ligamentum teres is associated with hip dislocation. Although this injury can occur without dislocation, occurrence has been described only as case reports.10–13 Disruption appears to be attributable to a twisting injury and is increasingly recognized as a source of intractable hip pain. In a review of 23 cases of traumatic injury to the ligamentum teres, 17 (74%) occurred without accompanying dislocation of the hip.14
PATIENT SELECTION
Successful hip arthroscopy is most clearly dependent on proper patient selection. A well- executed procedure will fail when performed for the wrong reasons. Patient expectation is paramount. The athlete should have reasonable goals and knows what can be accomplished with arthroscopy, which is only partially dictated by the nature of the pathology. Remember that much is not fully understood regarding the pathomechanics, pathoanatomy, and natural history of many of these lesions that are now being surgically addressed. However, an increasing amount of clinical experience exists upon which patients can be offered reasonable statistical data on likely outcomes.
Athletes are often set apart by their drive, discipline, and motivation as they push their bodies to their physiologic limits. However, the most uniquely challenging aspect of deciding on surgical intervention in this population is time constraints: How quickly does the surgeon decide to operate and how quickly will the patient recover? This decision is a year round issue, whether it is attempting to return for the current season, preparing for the upcoming season, or simply resuming the necessary off-season conditioning regimen. With the exception of loose bodies, no literature exists to suggest that harm is caused by not recommending early surgical intervention for most of the problems that are now being recognized.15 Most disorders will declare themselves over time through failure of response to conservative measures but unfortunately, for athletes, time is often not an ally.
Extra-articular injuries far outnumber intra-articular problems in the hip region. Thus, it is best to temper the interest to perform an extensive intra-articular work-up for every athlete with pain around the hip. However, in our study of athletes who underwent arthroscopy with documented pathology, the hip was not initially recognized as the source of symptoms in 60% of the cases. These athletes were managed for an average of seven months before the hip was considered as a potential contributing source.5 The most common preliminary diagnoses were various types of musculotendinous strains. Thus, it is prudent to at least consider possible intra-articular pathology in the differential diagnosis when managing a strain around the hip joint. Thoughtful follow-up and re-assessment is critical when these injuries do not respond as expected.
A careful history and examination will usually indicate whether the hip is the source of symptoms. Single plane activities such as straight ahead running are often well-tolerated while torsional and twisting maneuvers are more problematic in precipitating painful symptoms. Stairs and inclines may be more troublesome, and the same athlete who can run pain-free on level surfaces may have more difficulty running hills. Prolonged hip flexion such as sitting can be uncomfortable and catching symptoms are often experienced when rising from a seated or squatted position.
Hip symptoms are most commonly referred to the anterior groin and may radiate to the medial thigh. However, a very characteristic clinical feature which has been described is the “C-sign”.16 A patient describing deep interior hip pain will grip their hand above the greater trochanter with their thumb lying posteriorly and the fingers cupped within the anterior groin. It may appear that they are describing lateral pain such as from the iliotibial band or trochanteric bursa, but characteristically, they are reflecting pain within the joint.
On examination, log rolling the leg back and forth is the most specific maneuver for hip pathology since this rotates only the femoral head in relation to the acetabulum and capsule and does not stress any of the surrounding neurovascular or musculotendinous structures. More sensitive examination maneuvers include forced flexion combined with internal rotation or abduction combined with external rotation. Sometimes these movements will produce an accompanying click, but it is more important to determine if these maneuvers reproduce the athlete's pain.
For long-standing conditions, athletes may secondarily develop extra-articular symptoms of tendinitis or bursitis or may have a co-existent extra-articular pathology. A useful test for distinguishing the intra-articular origin of symptoms is a fluoroscopically guided intra-articular injection of anesthetic. The hallmark is temporary alleviation of symptoms during the anesthetic effect. With the more recent technology of gadolinium arthrography (MRA) combined with magnetic resonance imaging (MRI), it is important that anesthetic be included with the injection to elicit this useful diagnostic response.17
SPECIFIC LESIONS
Loose bodies represent the clearest indication for hip arthroscopy but are not a common problem among athletes (Figure 6).1 The work of Epstein et al15 has demonstrated the importance of removing loose bodies to prevent the secondary damage they can cause. Loose bodies can occur from trauma, disease such as synovial chondromatosis, or other disorder such as osteochondritis dissecans.1, 18–19 Recovery can be complete within weeks but depends on the amount of associated damage. Loose bodies can secondarily develop as a consequence of degenerative arthritis. In this setting, the results of loose body removal are not favorable because the degenerative disease cannot be corrected.
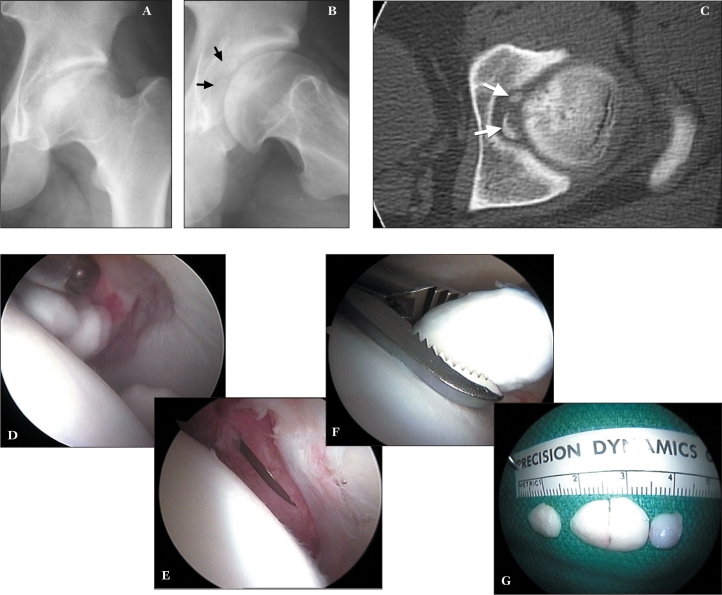
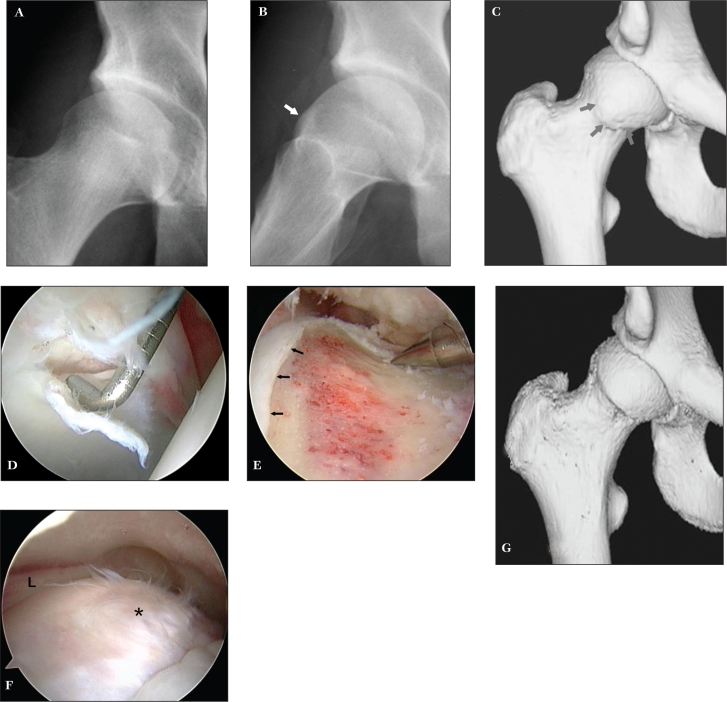
Figure 6.
A 20 year old male with a three month history of acute left hip pain. A. AP radiograph demonstrates findings consistent with old Legg-Calvé Perthes disease. B. Lateral view defines the presence of intraarticular loose bodies (arrows). C. CT scan substantiates the intraarticular location of the fragments (arrows). D. Arthroscopic view medially demonstrates the loose bodies. E. Viewing anteriorly, the anterior capsular incision is enlarged with an arthroscopic knife to facilitate removal of the fragments. F. One of the fragments is being retrieved. G. Loose bodies are able to be removed whole. (Reprinted with permission.3)
Labral lesions are the most common hip pathology, present in 61% of athletes undergoing arthroscopy.5 Labral debridement has resulted in 82% successful outcomes at 10 year follow-up when arthritis is not present (Figure 7).20
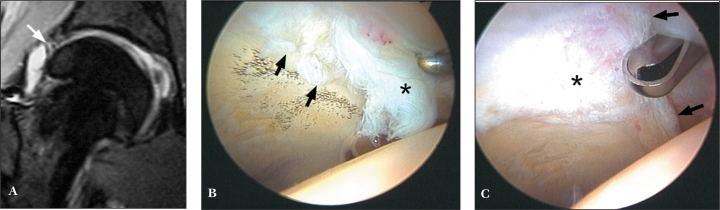
Figure 7.
A 25 year old top ranked professional tennis player sustained a twisting injury to his right hip. A. Coronal MRI demonstrates evidence of labral pathology (arrow). B. Arthroscopy reveals extensive tearing of the anterior labrum (asterisk) as well as an adjoining area of Grade III articular fragmentation (arrows). C. The labral tear has been resected to a stable rim (arrows) and chondroplasty of the Grade III articular damage (*) is being performed. (Reprinted with permission J.W. Thomas Byrd, M.D.)
However, not all labral tears are the same with regards to etiology, associated pathology, treatment, and outcomes. Arthritis is a poor prognostic indicator, and various studies have demonstrated that articular damage is present in association with more than half of all labral tears.21–24 Often it is the extent of articular pathology that is the limiting factor as far as the success of arthroscopic intervention (Figure 8). Use of MRIs and MRAs are best at identifying labral lesions, but poor at demonstrating accompanying articular pathology.17 Thus, the uncertain presence of articular damage is often the “wild card” in predicting the outcome of arthroscopy and should temper the surgeon's enthusiasm for predicting uniform success in the presence of imaging evidence of labral damage.
Figure 8.
A 23 year old elite professional tennis player sustained an injury to his right hip. A. Coronal MRI demonstrates evidence of labral pathology (arrow). B. Arthroscopy reveals the labral tear (arrows), but also an area of adjoining Grade IV articular loss (*). C. Microfracture of the exposed subchondral bone is performed. D. Occluding the inflow of fluid confirms vascular access through the areas of perforation. The athlete was maintained on a protected weight-bearing status emphasizing range of motion for 10 weeks with return to competition at three and a half months. (Reprinted with permission J.W. Thomas Byrd, M.D.)
Imaging (MRI and MRA) evidence of labral pathology must be carefully interpreted. Studies have shown evidence of labral abnormality even among asymptomatic volunteers and labral degeneration occurs naturally as part of the aging process.22, 25–27 It is uncertain whether labral tears will spontaneously heal, but observations have been made among athletes of tears that became clinically asymptomatic without surgery.28
A common etiologic factor in the association of co-existent labral and articular pathology, may be FAI.8 Pincer impingement caused by an overhanging lip of bone from the acetabulum can be corrected by reshaping the acetabular rim (Figure 9). Cam impingement, the most common type among athletes, is corrected by contouring the bony prominence at the junction of the femoral head and neck to recreate the spherical shape of the femoral head (Figure 10).
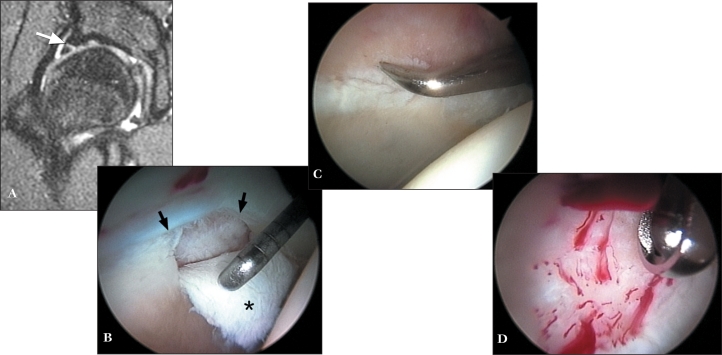
Figure 9.
A 16 year old high school football player develops acute onset of right hip pain doing squats. A. Sagittal image MR arthrogram demonstrates a macerated anterior labrum (arrows). B. Viewing from the anterolateral portal, a macerated tear of the anterior labrum is probed along with articular delamination at its junction with the labrum C. The damaged anterior labrum has been excised, revealing an overhanging lip of impinging bone from the anterior acetabulum. D. Excision of the impinging portion of the acetabulum (acetabuloplasty) is performed with a burr. (Reprinted with permission J.W. Thomas Byrd, M.D.)
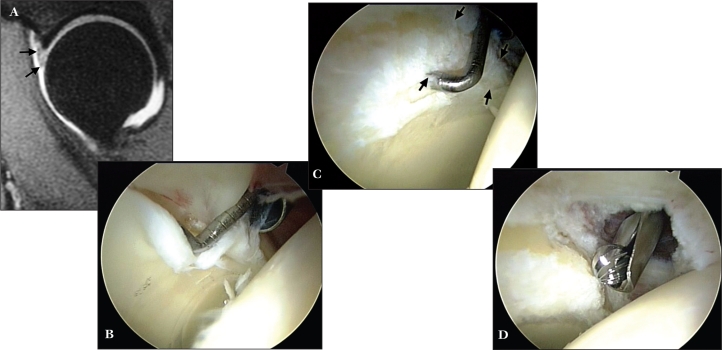
Figure 10.
A 20 year old hockey player with a four year history of right hip pain. A. AP radiograph is unremarkable. B. Frog lateral radiograph demonstrates a morphological variant with bony build up at the anterior femoral head/neck junction (arrow) characteristic of cam impingement. C. A 3D CT scan further defines the extent of the bony lesion (arrows). D. Viewing from the anterolateral portal, the probe introduced anteriorly displaces an area of articular delamination from the anterolateral acetabulum characteristic of the peel back phenomenon created by the bony lesion shearing the articular surface during hip flexion. E. Viewing from the peripheral compartment the bony lesion is identified (*) immediately below the free edge of the acetabular labrum (L). F. The lesion has been excised, recreating the normal concave relationship of the femoral head/neck junction immediately adjacent to the articular surface (arrows). Posteriorly, resection is limited to the mid portion of the lateral neck to avoid compromising blood supply to the femoral head from the lateral retinacular vessels. G. Post operative 3D CT scan illustrates the extent of bony resection. (Reprinted with permission J.W. Thomas Byrd, M.D.)
Recovery from simple labral debridement can be as little as one to two months. Correcting impingement results in a more protracted recovery, partly because of the more extensive nature of the procedure, but also the severity of the joint damage is usually more extensive. The bone must be allowed to remodel for three months and return to competitive activities is anticipated at four to six months.
The severity of associated articular damage also influences the recovery. Full thickness Grade IV articular loss with exposed subchondral bone is best treated with microfracture (Figure 8).29 This surgery is used to stimulate a fibrocartilaginous healing response and requires protected weightbearing for the first two months post-op while the defect matures. This surgery is an imperfect solution, but offers 86% positive results and is presently the standard of the industry.30 Microfracture is a harbinger of a more prolonged recovery, not because of the procedure but because of the severity of the problem for which it is implemented.
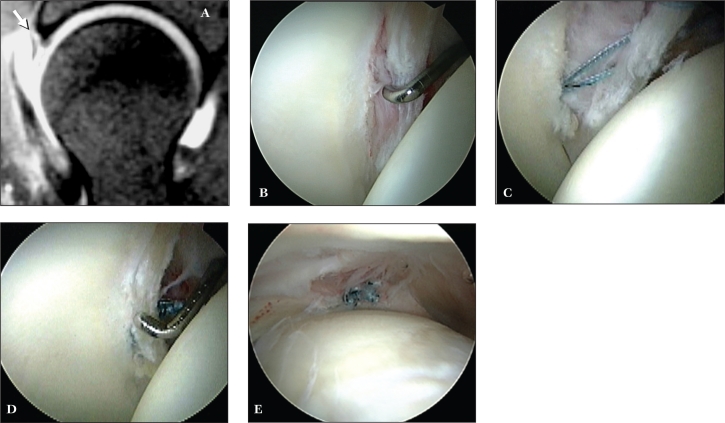
Related to labral repair (Figure 11), the technology developed in the shoulder has been readily applied to the hip.31,32 However, labral function and pathogenesis of labral lesions in the hip is different and the understanding of which are amenable to repair is less clear. As the selection process improves, the results of labral repair will become more favorable. Recovery requires more time to protect the repair site.
Figure 11.
A 37-year-old female with recalcitrant mechanical right hip pain. A. Sagittal MRA image demonstrates an anterior labral tear (arrow). B. Arthroscopy reveals a traumatic detachment of the anterior labrum (probe). C. An anchor has been placed with suture limbs passed in a mattress fashion through the detached labrum. D. The labrum has been re-approximated to the articular edge. E. Viewing the peripheral aspect of the labrum, demonstrates the suture on its capsular surface, avoiding contact with the articular surface of the femoral head. (Reprinted with permission J.W. Thomas Byrd, M.D.)
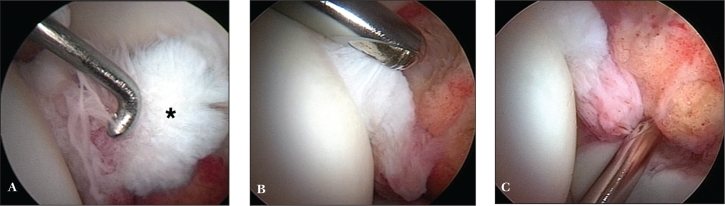
Injury to the ligamentum teres is the third most common problem encountered among athletes undergoing hip arthroscopy. The disrupted fibers catch within the joint and can be quite painful. Resection of these disrupted fibers has found remarkable success based on the magnitude of improvement with a 93% successful outcome (Figure 12).14
Figure 12.
A 16 year old cheerleader has a two year history of catching and locking of the left hip following a twisting injury. A. Arthroscopic view from the anterolateral portal reveals disruption of the ligamentum teres (*). B. Debridement is begun with a synovial resector introduced from the anterior portal. The acetabular attachment of the ligamentum teres in the posterior aspect of the fossa is addressed from the posterolateral portal. (A,B reprinted with permission J. W. Thomas Byrd, M.D. C reprinted with permission Byrd JWT, Jones KS14)
Clinical and radiographic evidence of arthritis is a poor prognostic indicator of the results of arthroscopy.2,21,33,34 Advanced disease with complete joint space loss is a contraindication because of uniformly unsuccessful results. Lesser disease may serve only as a relative contraindication depending on the goals of the procedure and the expectations of the athlete. For example, labral debridement or loose body removal in the presence of arthritis will not result in the same successful outcomes that have been reported for athletes in absence of arthritic changes. The expectations of the athlete must be more modest and practical. Otherwise, the procedure will be a failure by not accomplishing the desired outcome.
Hip instability can occur, but is much less common than instability in the shoulder. The primary reason is due to the inherent stability provided by the constrained ball and socket bony architecture of the hip joint. Also, the labrum is not as critical to stability of the hip as it is in the shoulder as no true capsulolabral complex exists. On the acetabular side, the capsule attaches directly to the bone, separate from the acetabular labrum.27 An entrapped labrum has been reported as a cause of an irreducible posterior dislocation and a Bankart type detachment of the posterior labrum has been identified as a cause of recurrent posterior instability.35,36 These circumstances have only rarely been reported, but may be recognized with increasing frequency as the understanding and intervention of hip injuries evolves.
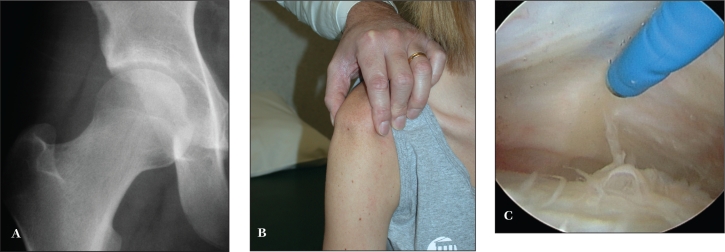
Instability may occur simply due to an incompetent capsule. This instability is seen in hyperlaxity states and less often encountered in athletics. The most common cause is a collagen vascular disorder such as Ehlers-Danlos syndrome. With normal joint geometry, thermal capsular shrinkage has been met with successful results (Figure 13). If subluxation or symptomatic instability is due to a dysplastic joint, it is likely that bony correction for containment is necessary to achieve stability.
Figure 13.
A 19 year old female had undergone two previous arthroscopic procedures on her right hip for reported lesions of the ligamentum teres. Following each procedure, she developed recurrent symptoms of “giving way.” A. Radiographs revealed normal joint geometry. B. She was noted to have severe diffuse physiologic laxity best characterized by a markedly positive sulcus sign. C. With objective evidence of laxity and subjective symptoms of instability, an arthroscopic thermal capsulorrhaphy was performed, accessing the redundant anterior capsule from the peripheral compartment. Modulation of the capsular response was controlled by a hip spica brace for eight weeks postoperatively with a successful outcome. (Reprinted with permission J.W. Thomas Byrd, M.D.)
Based on this author's observations, posterior instability is associated with macrotrauma. Mechanisms of injury include dashboard injuries and axial loading of the flexed hip encountered in collision sports. Atraumatic instability, or instability due to repetitive microtrauma, is anterior and develops when the normally occurring anterior translation of the femoral head exceeds the physiologic threshold and becomes pathological. Symptoms may be due to primary instability, secondary intra-articular damage, or a combination of both.
In general, for properly selected cases, hip arthroscopy has a high rate of improvement, but does not always assure returning to the rigors of athletic activities. Among a heterogenous group of athletes, 93% were improved, but only 76% returned to their sport symptom-free and unrestricted or at an increased level of performance. Eighteen percent either chose to not return or were unable to return to their primary sport. Among a group of elite athletes, 96% were improved, but only 85% were able to successfully return to their sport.
CONCLUSIONS
Hip joint problems in athletes may go unrecognized for a protracted period of time. With an increased awareness of intra-articular disorders, these problems are now being diagnosed earlier. However, understanding of the pathogenesis and natural history of many of these lesions is incomplete, and may influence the strategies of both surgical and conservative treatment. Nonetheless, arthroscopy has defined numerous sources of intra-articular hip pathology. In many cases, operative arthroscopy has been met with significant success. For some athletes, arthroscopy offers a distinct advantage over traditional open techniques, but for many, arthroscopy offers a method of treatment where none existed before.
REFERENCES
- 1.Byrd JWT. Hip arthroscopy for post-traumatic loose fragments in the young active adult: Three case reports. Clin Sports Med. 1996:6;129–134 [DOI] [PubMed] [Google Scholar]
- 2.Villar RN. Arthroscopic debridement of the hip: A minimally invasive approach to osteoarthritis. J Bone Joint Surg. 1991:73B;170–171 [Google Scholar]
- 3.Byrd JWT. Indications and Contraindications. In Byrd JWT. (ed): Operative Hip Arthroscopy, Second Edition New York, Springer,2005,6–35 [Google Scholar]
- 4.Byrd JWT. Hip Arthroscopy: Patient Assessment and Indications. Instr Course Lect. Sports Medicine. 2003;711–719 [PubMed] [Google Scholar]
- 5.Byrd JWT, Jones KS. Hip arthroscopy in athletes. Clin Sports Med. 2001;20:749–762 [PubMed] [Google Scholar]
- 6.Byrd JWT, Jones KS. Prospective analysis of hip arthroscopy: Two year follow-up. Arthroscopy. 2000;16:578–587 [DOI] [PubMed] [Google Scholar]
- 7.Byrd JWT. Lateral impact injury: A source of occult hip pathology. Clin Sports Med. 2001;20:801–816 [PubMed] [Google Scholar]
- 8.Byrd JWT. Hip morphology and related pathology. In Johnson DH, Pedowitz RA: Practical Orthopaedic Sports Medicine & Arthroscopy. Lippincott Williams & Wilkins, Pennsylvania, 2007, 491–503 [Google Scholar]
- 9.Meyers WC, Foley DP, Garrett WE, et al. Management of severe lower abdominal or inguinal pain in high-performance athletes. Am J Sports Med. 18:2–8,2000 [DOI] [PubMed] [Google Scholar]
- 10.Delcamp DD, Klarren HE, Van Meerdervoort HFP. Traumatic avulsion of the ligamentum teres without dislocation of the hip. J Bone Joint Surg. 1988;70A:933–935 [PubMed] [Google Scholar]
- 11.Barrett IR, Goldberg JA. Avulsion fracture of the ligamentum teres in a child. A case report. J Bone Joint Surg. 1989;71A:438–439 [PubMed] [Google Scholar]
- 12.Ebrahim NA, Salvolaine ER, Fenton PJ, Jackson WT. Calcified ligamentum teres mimicking entrapped intraarticular bony fragments in a patient with acetabular fracture. J Orthop Trauma. 1991;5:376–378 [DOI] [PubMed] [Google Scholar]
- 13.Kashiwagi N, Suzuki S, Seto Y. Arthroscopic treatment for traumatic hip dislocation with avulsion fracture of the ligamentum teres. Arthroscopy. 2001;17:67–69 [DOI] [PubMed] [Google Scholar]
- 14.Byrd JWT, Jones KS. Traumatic rupture of the ligamentum teres as a source of hip pain. Arthroscopy. 2004;20:385–391 [DOI] [PubMed] [Google Scholar]
- 15.Epstein H. Posterior fracture-dislocations of the hip: Comparison of open and closed methods of treatment in certain types. J Bone Joint Surg. 1961;43A:1079–1098 [Google Scholar]
- 16.Byrd JWT. Physical Examination, In Byrd JWT. (ed) Operative Hip Arthroscopy, Second Edition New York, Springer, 2005,36–50 [Google Scholar]
- 17.Byrd, JWT, Jones KS. Diagnostic accuracy of clinical assessment, MRI, gadolinium MRI, and intraarticular injection in hip arthroscopy patients. Am J Sports Med. 32:1668–1674;2004 [DOI] [PubMed] [Google Scholar]
- 18.McCarthy JC, Bono JVV, Wardell S. Is there a treatment for synovial chondromatosis of the hip joint? Arthroscopy. 1997;13:409–410 [Google Scholar]
- 19.Medlock V, Rathjen KE, Montgomery JB. Hip arthroscopy for late sequelae of Perthes disease. Arthroscopy. 1999;15:552–553 [Google Scholar]
- 20.Byrd JWT, Jones KS. Prospective analysis of hip arthroscopy with ten year follow up. Presented at AAOS 74th Annual Meeting San Diego, CAFebruary 16, 2007 [Google Scholar]
- 21.Byrd JWT, Jones KS. Prospective analysis of hip arthroscopy with five year follow up. Presented at AAOS 69th Annual Meeting Dallas, TX, February 14, 2002 [Google Scholar]
- 22.McCarthy JC, Noble PC, Schuck MR, et al. The watershed labral lesion: Its relationship to early arthritis of the hip. J Arthroplasty. 2001:16(8 Supp 1);81–87 [DOI] [PubMed] [Google Scholar]
- 23.Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labrum tears. Arthroscopy. 1999:15;132–137 [DOI] [PubMed] [Google Scholar]
- 24.Santori N, Villar RN. Acetabular labral tears: Result of arthroscopic partial limbectomy. Arthroscopy. 2000:16;11–15 [DOI] [PubMed] [Google Scholar]
- 25.Cotton A, Boutry N, Demondio X, et al. Acetabular labrum: MRI in asymptomatic volunteers. J Comput Assist Tomogr. 1998:22;1–7 [DOI] [PubMed] [Google Scholar]
- 26.Lecouvet FE, VandeBerg BC, Malghen J, et al. MR imaging of the acetabular labrum: Variations in 200 asymptomatic hips. Am J Roentgenol. 1996:167;1025–1028 [DOI] [PubMed] [Google Scholar]
- 27.Seldes RM, Tan V, Hunt J, et al. Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop. 2001:382;232–240 [DOI] [PubMed] [Google Scholar]
- 28.Byrd JWT. Hip arthroscopy in athletes. Instr Course Lect. 52:701–709;2003 [PubMed] [Google Scholar]
- 29.Byrd JWT, Jones KS. Inverted acetabular labrum and secondary osteoarthritis: Radiographic diagnosis and arthroscopic treatment. Arthroscopy. 2000;16:417. [DOI] [PubMed] [Google Scholar]
- 30.Byrd JWT, Jones KS. Microfracture for grade IV chondral lesions of the hip. Arthroscopy. 20:SS–89,41;2004 [Google Scholar]
- 31.Kelly BT, Weiland DE, Schenker ML, et al. Arthroscopic labral repair in the hip: Surgical technique and review of the literature. Arthroscopy. 2005:1496–504 [DOI] [PubMed] [Google Scholar]
- 32.Murphy KP, Ross AE, Javernick MA, et al. Repair of the adult acetabular labrum. Arthroscopy. 2006:22:1–3 [DOI] [PubMed] [Google Scholar]
- 33.Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for degenerative joint disease. Arthroscopy. 1998;14:435 [Google Scholar]
- 34.Santori N, Villar RN. Arthroscopic findings in the initial stages of hip osteoarthritis. Orthopedics. 1999;22:405–409 [DOI] [PubMed] [Google Scholar]
- 35.Paterson I. The torn acetabular labrum: A block to reduction of dislocated hip. J Bone Joint Surg. 1957; 39B:306–309 [DOI] [PubMed] [Google Scholar]
- 36.Dameron TB. Bucket-handle tear of acetabular labrum accompanying posterior dislocation of the hip. J Bone Joint Surg. 1959;41A:131–134 [PubMed] [Google Scholar]