Abstract
To prepare an athlete for the wide variety of activities needed to participate in their sport, the analysis of fundamental movements should be incorporated into pre-participation screening in order to determine who possesses, or lacks, the ability to perform certain essential movements. In a series of two articles, the background and rationale for the analysis of fundamental movement will be provided. In addition, one such evaluation tool that attempts to assess the fundamental movement patterns performed by an individual, the Functional Movement Screen (FMS™), will be described. Three of the seven fundamental movement patterns that comprise the FMS™ are described in detail in Part I: deep squat, hurdle step, and in-line lunge. Part II of this series, which will be published in the August issue of NAJSPT, will provide a brief review of the analysis of fundamental movements, as well a detailed description of the four additional patterns that complement those presented in Part I (to complete the total of seven fundamental movement patterns which comprise the FMS™): shoulder mobility, active straight leg raise, trunk stability push-up, and rotary stability.
The intent of this two part series is to introduce the concept of the evaluation of fundamental movements, whether it is the FMS™ system or a different system devised by another clinician. Such a functional assessment should be incorporated into pre-participation screening in order to determine whether the athlete has the essential movements needed to participate in sports activities with a decreased risk of injury.
Keywords: pre-participation screening, performance tests, function
INTRODUCTION
Over the last 20 years, the profession of sports rehabilitation has undergone a trend away from traditional, isolated assessment and strengthening toward an integrated, functional approach, incorporating the principles of proprioceptive neuromuscular fascilitation (PNF), muscle synergy, and motor learning.1 However, it is difficult to develop and refer to protocols as “functional” when a functional evaluation standard does not exist. In many situations, rehabilitation professionals in sports settings are far too anxious to perform specific isolated, objective testing for joints and muscles. Likewise, these clinicians often perform sports performance and specific skill assessments without first examining functional movement. It is important to inspect and understand common fundamental aspects of human movement realizing that similar movements occur throughout many athletic activities and applications. The rehabilitation professional must realize that in order to prepare individuals for a wide variety of activities, fundamental movements should be assessed.
In the traditional sports medicine model, pre-participation physicals are followed by performance assessments. This systematic process doesn't seem to provide enough baseline information when assessing an individual's preparedness for activity. Commonly, the medical pre-participation or rehabilitation examination includes only information that will exclude an individual from participating in certain activities. The perception of many past researchers is that no set standards exist for determining who is physically prepared to participate in activities.2–5 Recently, numerous medical societies have collaborated and attempted to establish more uniformity in this area, however, only suggestions for baseline medical parameters required for participation were provided.6 Ideally, collaboration should also occur among professionals to determine what the baseline for fundamental movement should be and if individuals should be allowed to participate if they are unable to perform movements at a basic level.
In the typical pre-participation screening exam, once the pre-participation medical examination is performed the active individual is then asked to complete performance tests. Commonly recommended performance tests include sit-ups, push-ups, endurance runs, sprints, and agility activities.7 In many athletic and occupational settings these performance activities become more specific to the tasks needed for defined areas of performance.
Performance tests function to gather baseline quantitative information and then attempt to make recommendations and establish goals. The recommendations are based on standardized normative information, which may not be relative to the individual's specific needs. Likewise, in many cases, performance tests provide objective information that fails to evaluate the efficiency by which individuals perform certain movements. Little consideration is given to functional movement deficits, which may limit performance and predispose the individual to micro-traumatic injury.
Prescribed strength and conditioning programs often work to improve agility, speed, and strength without consideration for perfection or efficiency of underlying functional movement. An example would be a person who has an above average score on the number of sit-ups performed during a test but is performing very inefficiently by compensating and initiating the movement with the upper body and cervical spine as compared to the trunk. Compare this person to an individual who scores above average on the number of sit-ups, but is performing very efficiently and doesn't utilize compensatory movements to achieve the sit-up. These two individuals would each be deemed “above average” without noting their individual movement inefficiencies. The question arises: If major deficiencies are noted in their functional movement patterns, then should their performance be judged as equal? These two individuals would likely have significant differences in functional mobility and stability; however, without assessing their functional mobility and stability it is inappropriate to assume differences.
The main goal in performing pre-participation or performance screenings is to decrease injuries, enhance performance, and ultimately improve quality of life.4,6,8 Currently, the research is inconsistent on whether the pre-participation or performance screenings and standardized fitness measures have the ability to achieve this main goal.4,5 A reason for the lack of predictive value of screenings is that the standardized screenings do not provide individualized, fundamental analysis of an individual's movements. The authors of this clinical commentary suggest that analysis of fundamental movements should be incorporated into pre-season screening in order to determine who possesses, or lacks, the ability to perform certain essential movements.
THE FUNCTIONAL MOVEMENT SCREEN™
The Functional Movement Screen (FMS)™ is one evaluation tool that attempts to assess the fundamental movement patterns of an individual.9–11 This assessment tool fills the void between the pre-participation/ pre-placement screenings and performance tests by evaluating individuals in a dynamic and functional capacity. A screening tool such as this offers a different approach to injury prevention and performance predictability. When used as a part of a comprehensive assessment, the FMS™ will lead to individualized, specific, functional recommendations for physical fitness protocols in athletic and active population groups.
The FMS™ is comprised of seven fundamental movement patterns that require a balance of mobility and stability. These fundamental movement patterns are designed to provide observable performance of basic locomotor, manipulative, and stabilizing movements. The tests place the individual in extreme positions where weaknesses and imbalances become noticeable if appropriate stability and mobility is not utilized. It has been observed that many individuals who perform at very high levels during activities are unable to perform these simple movements.11,12 These individuals should be considered to be utilizing compensatory movement patterns during their activities, sacrificing efficient movements for inefficient ones in order to perform at high levels. If compensations continue, then poor movement patterns are reinforced leading to poor biomechanics and ultimately the potential of micro- or macro-traumatic injury.
The FMS™ tests were created based on fundamental proprioceptive and kinesthetic awareness principles. Each test is a specific movement, which requires appropriate function of the body's kinetic linking system. The kinetic link model, used to analyze movement, depicts the body as a linked system of interdependent segments. These segments often work in a proximal-to-distal sequence, in order to impart a desired action at the distal segment.13 An important aspect of this system is the body's proprioceptive abilities. Proprioception can be defined as a specialized variation of the sensory modality of touch that encompasses the sensation of joint movement and joint position sense.14 Proprioceptors in each segment of the kinetic chain must function properly in order for efficient movement patterns to occur.
During growth and development, an individual's proprioceptors are developed through reflexive movements in order to perform basic motor tasks. This development occurs from proximal to distal, the infant learning to first stabilize the proximal joints in the spine and torso and eventually the distal joints of the extremities. This progression occurs due to maturation and learning. The infant learns fundamental movements by responding to a variety of stimuli, through the process of developmental motor learning. As growth and development progresses, the proximal to distal process becomes operational and has a tendency to reverse itself. The process of movement regression slowly evolves in a distal to proximal direction.15 This regression occurs as individuals gravitate toward specific skills and movements through habit, lifestyles, and training.
Application Examples
Firefighters initially train through controlled, voluntary movements. Then, through repetition, the movement becomes stored centrally as a motor program. The motor program eventually requires fewer cognitive commands leading to improved subconscious performance of the task. This subconscious performance involves the highest levels of central nervous system function, know as cognitive programming.14 In this example, problems would arise when the movements and training being “learned” are performed incorrectly, inefficiently, or asymmetrically.
A sport-specific example is a football lineman entering preseason practice who does not have the requisite balance of mobility or stability to perform a specific skill such as blocking. The athlete may perform the skill utilizing compensatory movement patterns in order to overcome the stability or mobility inefficiencies. The compensatory movement pattern will then be reinforced throughout the training process. In such an example, the individual creates a poor movement pattern that will be subconsciously utilized whenever the task is performed. Programmed altered movement patterns have the potential to lead to further mobility and stability imbalances, which have previously been identified as risk factors for injury.16–18
An alternative explanation for development of poor movement patterns is the presence of previous injuries. Individuals who have suffered an injury may have a decrease in proprioceptive input, if untreated or treated inappropriately.14,19 A disruption in proprioceptive performance will have a negative effect on the kinetic linking system. The result will be altered mobility, stability, and asymmetric influences, eventually leading to compensatory movement patterns. This may be a reason why prior injuries have been determined to be one of the more significant risk factors in predisposing individuals to repeat injuries.19,20
Determining which risk factor has a larger influence on injury, previous injuries or strength/flexibility imbalances, is difficult. In either case, both lead to deficiencies in functional performance. It has been determined that these functional deficits lead to pain, injury, and decreased performance. Cholewicki et al 21 demonstrated that limitations in stability in the spine led to muscular compensations, fatigue, and pain. Gardner-Morse et al 22 determined that spinal instabilities result in degenerative changes due to the muscle activation strategies, which may be disrupted due to previous injury, stiffness, or fatigue. In addition, Battie et al23 demonstrated that individuals with previous low-back pain performed timed shuttle runs at a significantly lower pace than individuals who did not have previous low-back pain.
Therefore, an important factor in preventing injuries and improving performance is to quickly identify deficits in mobility and stability because of their influences on creating altered motor programs throughout the kinetic chain. The complexity of the kinetic linking system makes the evaluation of weaknesses using conventional, static methods difficult. For that reason, utilizing functional tests that incorporate the entire kinetic chain need to be utilized to isolate deficiencies in the system.8,19,23 The FMS™ is designed to identify individuals who have developed compensatory movement patterns in the kinetic chain. This identification is accomplished by observing right and left side imbalances and mobility and stability weaknesses. The seven movements in the FMS™ attempt to challenge the body's ability to facilitate movement through the proximal-to-distal sequence. This course of movement in the kinetic chain allows the body to produce movement patterns more efficiently. The correct movement patterns were initially formed during growth and development. However, due to a weakness or dysfunction in the kinetic linking system, a poor movement pattern may have resulted. Once an inefficient movement pattern has been isolated by the FMS™, functional prevention strategies can be instituted to avoid problems such as imbalance, micro-traumatic breakdown, and injury.
Scoring the Functional Movement Screen™
The scoring for the FMS™ consists of four possibilities. The scores range from zero to three, three being the best possible score. The four basic scores are quite simple in philosophy. An individual is given a score of zero if at any time during the testing he/she has pain anywhere in the body. If pain occurs, a score of zero is given and the painful area is noted. A score of one is given if the person is unable to complete the movement pattern or is unable to assume the position to perform the movement. A score of two is given if the person is able to complete the movement but must compensate in some way to perform the fundamental movement. A score of three is given if the person performs the movement correctly without any compensation. Specific comments should be noted defining why a score of three was not obtained
The majority of the tests in the FMS™ test right and left sides respectively, and it is important that both sides are scored. The lower score of the two sides is recorded and is counted toward the total; however it is important to note imbalances that are present between right and left sides.
Three tests have additional clearing screens which are graded as positive or negative. These clearing movements only consider pain, if a person has pain then that portion of the test is scored positive and if there is no pain then it is scored negative. The clearing tests affect the total score for the particular tests in which they are used. If a person has a positive clearing screen test then the score will be zero.
All scores for the right and left sides, and those for the tests which are associated with the clearing screens, should be recorded. By documenting all the scores, even if they are zeros, the sports rehabilitation professional will have a better understanding of the impairments identified when performing an evaluation. It is important to note that only the lowest score is recorded and considered when tallying the total score. The best total score that can be attained on the FMS™ is twenty-one.
DESCRIPTION OF THE FMS™ TESTS
The following are descriptions of three of the seven specific tests used in the FMS™ and their scoring system. Each test is followed by tips for testing developed by the authors as well as clinical implications related to the findings of the test.
Deep Squat
Purpose.
The squat is a movement needed in most athletic events. It is the ready position and is required for most power movements involving the lower extremities. The deep squat is a test that challenges total body mechanics when performed properly. The deep squat is used to assess bilateral, symmetrical, functional mobility of the hips, knees, and ankles. The dowel held overhead assesses bilateral, symmetrical mobility of the shoulders as well as the thoracic spine.
Description.
The individual assumes the starting position by placing his/her feet approximately shoulder width apart and the feet aligned in the sagittal plane. The individual then adjusts their hands on the dowel to assume a 90-degree angle of the elbows with the dowel overhead. Next, the dowel is pressed overhead with the shoulders flexed and abducted, and the elbows extended. The individual is then instructed to descend slowly into a squat position. The squat position should be assumed with the heels on the floor, head and chest facing forward, and the dowel maximally pressed overhead. As many as three repetitions may be performed. If the criteria for a score of III is not achieved, the athlete is then asked to perform the test with a 2x6 block under their heels. (Figures 1–4)
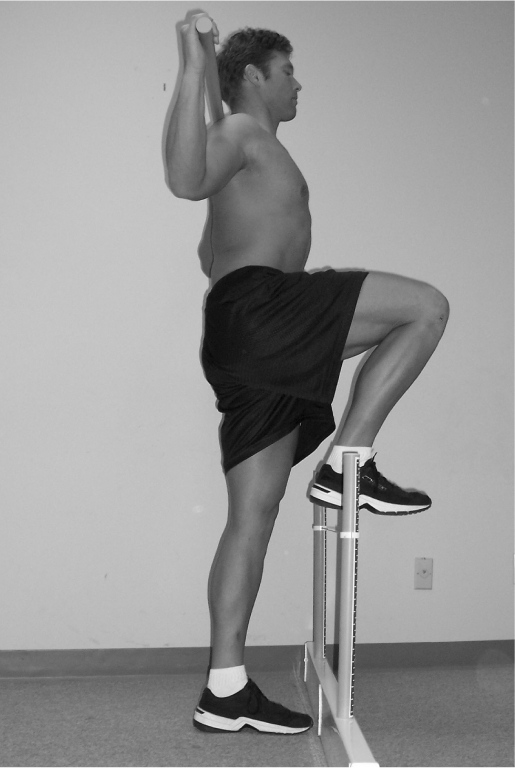
Figure 1.

Deep squat anterior view.
- Upper torso is parallel with tibia or toward vertical
- Femur below horizontal
- Knees are aligned over feet
- Dowel aligned over feet
Figure 4.

Deep squat anterior view.
- Tibia and upper torso are not parallel
- Femur is not below horizontal
- Knees are not aligned over feet
- Lumbar flexion is noted
- 2×6 board required under feet
Figure 2.
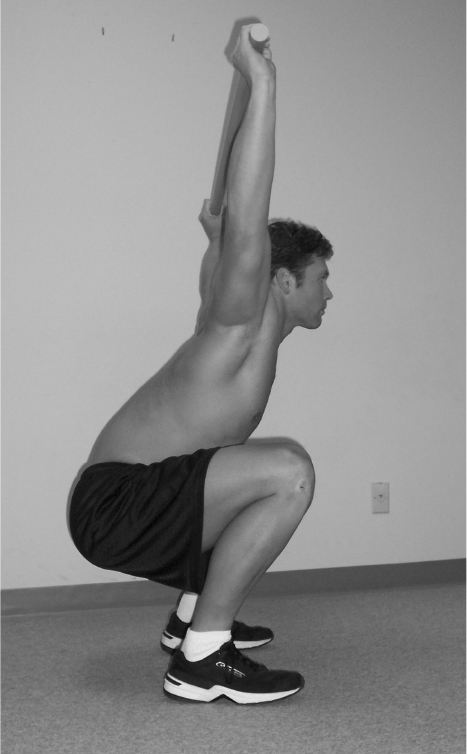
Deep squat lateral view.
Figure 3.
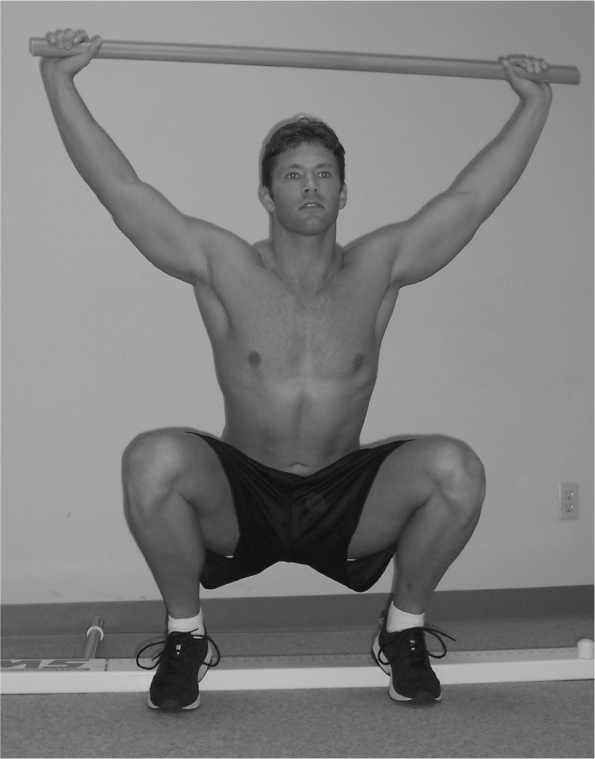
Deep squat anterior view.
- Upper torso is parallel with tibia or toward vertical
- Femur is below horizontal
- Knees are aligned over feet
- Dowel is aligned over feet
- 2×6 board required under feet
Tips for Testing:
When in doubt, score the subject low.
Try not to interpret the score while testing.
Make sure if you have a question to view individual from the side.
Clinical Implications for Deep Squat
The ability to perform the deep squat requires closed-kinetic chain dorsiflexion of the ankles, flexion of the knees and hips, extension of the thoracic spine, and flexion and abduction of the shoulders.
Poor performance of this test can be the result of several factors. Limited mobility in the upper torso can be attributed to poor glenohumeral and thoracic spine mobility. Limited mobility in the lower extremity including poor closed-kinetic chain dorsiflexion of the ankles or poor flexion of the hips may also cause poor test performance.
When an athlete achieves a score less than III, the limiting factor must be identified. Clinical documentation of these limitations can be obtained by using standard goniometric measurements. Previous testing has identified that when an athlete achieves a score of II, minor limitations most often exist either with closed-kinetic chain dorsiflexion of the ankle or extension of the thoracic spine. When an athlete achieves a score of I or less, gross limitations may exist with the motions just mentioned, as well as flexion of the hip.
Hurdle Step
Purpose.
The hurdle step is designed to challenge the body's proper stride mechanics during a stepping motion. The movement requires proper coordination and stability between the hips and torso during the stepping motion as well as single leg stance stability. The hurdle step assesses bilateral functional mobility and stability of the hips, knees, and ankles.
Description.
The individual assumes the starting position by first placing the feet together and aligning the toes touching the base of the hurdle. The hurdle is then adjusted to the height of the athlete's tibial tuberosity. The dowel is positioned across the shoulders below the neck. The individual is then asked to step over the hurdle and touch their heel to the floor while maintaining the stance leg in an extended position. The moving leg is then returned to the starting position. The hurdle step should be performed slowly and as many as three times bilaterally. If one repetition is completed bilaterally meeting the criteria provided, a III is given. (Figures 5–8)
Figure 5.
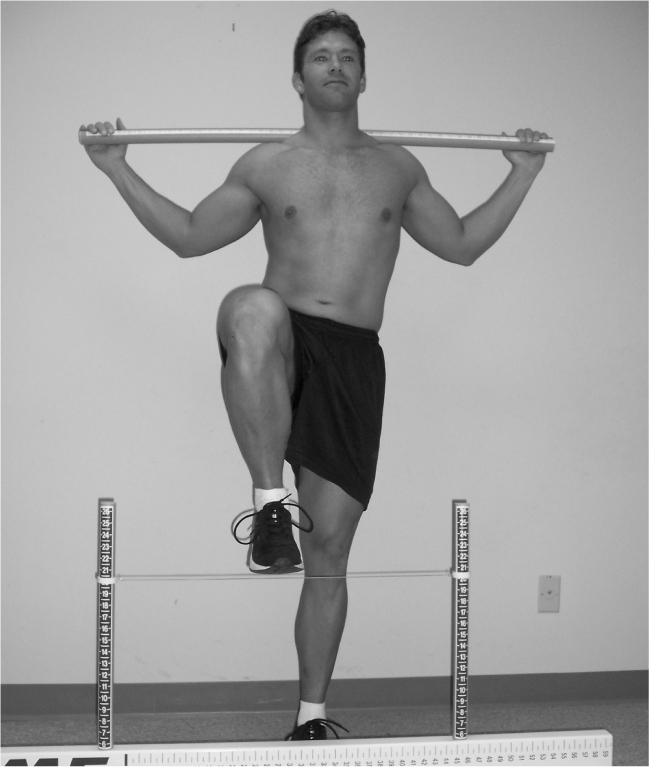
Hurdle step anterior view.
- Hips, knees and ankles remain aligned in the sagittal plane
- Minimal to no movement is noted in lumbar spine
- Dowel and string remain parallel
Figure 8.
Hurdle step anterior view.
- Contact between foot and string occurs
- Loss of balance is noted
Figure 6.
Hurdle step anterior view.
Figure 7.
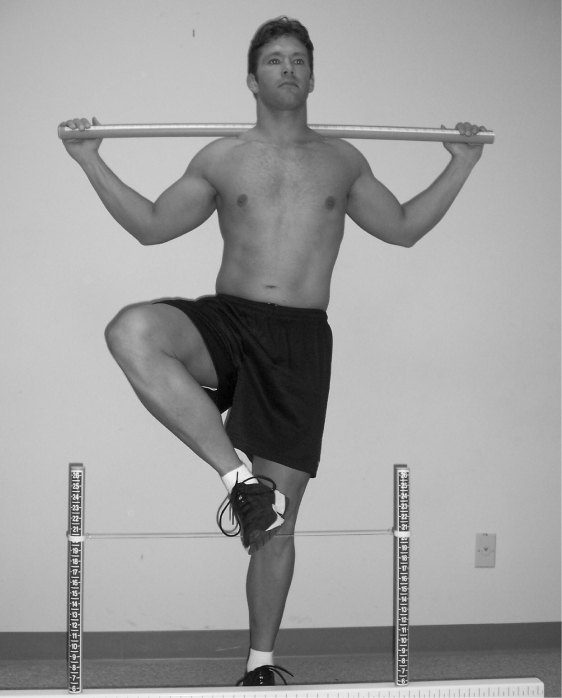
Hurdle step anterior view.
- Alignment is lost between hips, knees, and ankles
- Movement is noted in lumbar spine
- Dowel and string do not remain parallel
Tips for Testing:
Score the leg that is stepping over the hurdle
Make sure the individual maintains a stable torso
Tell individual not to lock knees of the stance limb during test
Maintain proper alignment with the string and the tibial tuberosity
When in doubt score subject low
Do not try to interpret the score when testing
Clinical Implications for Hurdle Step
Performing the hurdle step test requires stance-leg stability of the ankle, knee, and hip as well as maximal closed-kinetic chain extension of the hip. The hurdle step also requires step-leg open-kinetic chain dorsiflexion of the ankle and flexion of the knee and hip. In addition, the athlete must also display adequate balance because the test imposes a need for dynamic stability.
Poor performance during this test can be the result of several factors. It may simply be due to poor stability of the stance leg or poor mobility of the step leg. Imposing maximal hip flexion of one leg while maintaining hip extension of the opposite leg requires the athlete to demonstrate relative bilateral, asymmetric hip mobility.
When an athlete achieves a score less than III, the limiting factor must be identified. Clinical documentation of these limitations can be obtained by using standard goniometric measurements of the joints as well as muscular flexibility tests such as Thomas test or Kendall's test for hip flexor tightness.24 Previous testing has identified that when an athlete achieves a score of II, minor limitations most often exist with ankle dorsiflexion and hip flexion with the step leg. When an athlete scores a I or less, relative asymmetric hip immobility may exist, secondary to an anterior tilted pelvis and poor trunk stability.
In-Line Lunge
Purpose.
The in-line lunge attempts to place the body in a position that will focus on the stresses as simulated during rotational, decelerating, and lateral type movements. The in-line lunge is a test that places the lower extremities in a scissor style position challenging the body's trunk and extremities to resist rotation and maintain proper alignment. This test assesses hip and ankle mobility and stability, quadriceps flexibility, and knee stability.
Description.
The tester attains the individual's tibia length, by either measuring it from the floor to the tibial tuberosity or acquiring it from the height of the string during the hurdle step test. The individual is then asked to place the end of their heel on the end of the board or a tape measure taped to the floor. The previous tibia measurement is then applied from the end of the toes of the foot on the board and a mark is made. The dowel is placed behind the back touching the head, thoracic spine, and sacrum. The hand opposite to the front foot should be the hand grasping the dowel at the cervical spine. The other hand grasps the dowel at the lumbar spine. The individual then steps out on the board or tape measure on the floor placing the heel of the opposite foot at the indicated mark. The individual then lowers the back knee enough to touch the surface behind the heel of the front foot and then returns to starting position. The lunge is performed up to three times bilaterally in a slow controlled fashion. If one repetition is completed successfully then a three is given for that extremity (right or left). (Figures 9–12)
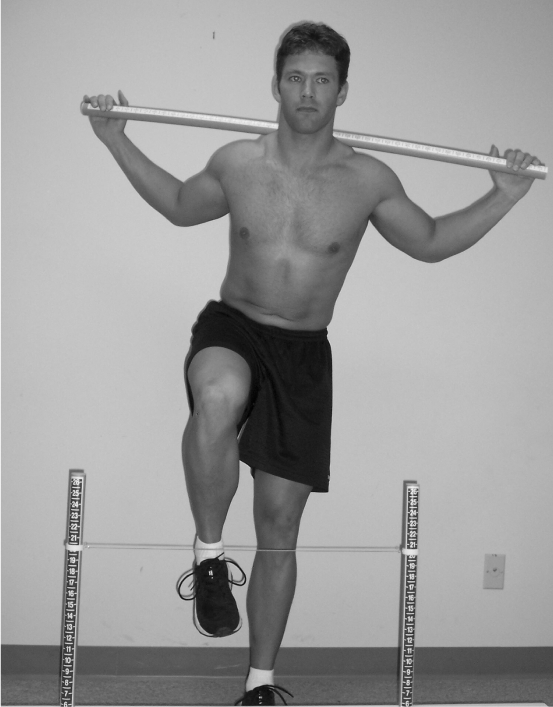
Figure 9.
In Line Lunge anterior view.
- Dowel contacts remain with lumbar spine extension
- No torso movement is noted
- Dowel and feet remain in sagittal plane
- Knee touches board behind heel of front foot
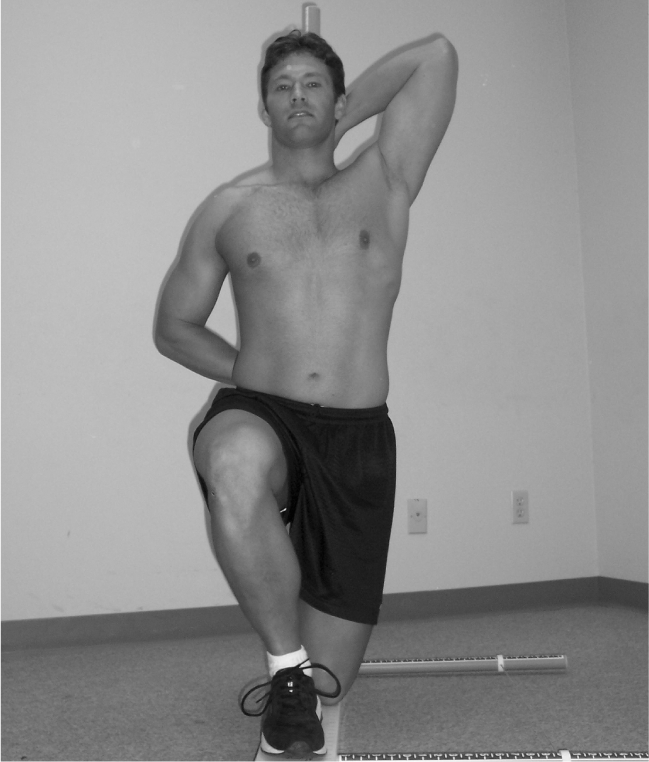
Figure 12.

In Line Lunge anterior view.
- Loss of balance is noted
Figure 10.
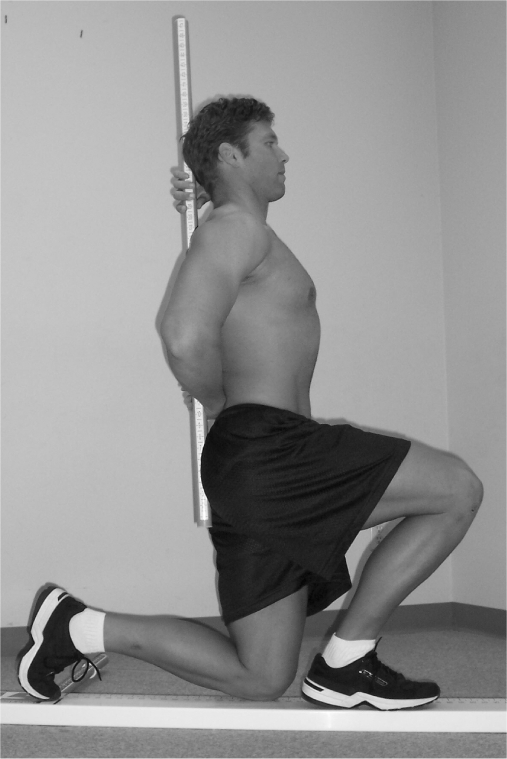
In Line Lunge lateral view.
Figure 11.

In Line Lunge lateral view.
- Dowel contacts do not remain with lumbar spine extension
- Movement is noted in torso
- Dowel and feet do not remain in sagittal plane
- Knee does not touch behind heel of front foot
Tips for Testing:
The front leg identifies the side being scored
Dowel remains in contact with the head, thoracic spine, and sacrum during the lunge
The front heel remains in contact with the surface and back heel touches surface when returning to starting position
When in doubt score the subject low
Watch for loss of balance
Remain close to individual in case he/she has a loss of balance.
Clinical Implications for In-Line Lunge
The ability to perform the in-line lunge test requires stance leg stability of the ankle, knee, and hip as well as apparent closed kinetic-chain hip abduction. The in-line lunge also requires step-leg mobility of hip abduction, ankle dorsiflexion, and rectus femoris flexibility. The athlete must also display adequate balance due to the lateral stress imposed.
Poor performance during this test can be the result of several factors. First hip mobility may be inadequate in either the stance leg or the step leg. Second, the stanceleg knee or ankle may not have the required stability as the athlete performs the lunge. Finally, an imbalance between relative adductor weakness and abductor tightness in one or both hips may cause poor test performance. Limitations may also exist in the thoracic spine region which may inhibit the athlete from performing the test properly.
When an athlete achieves a score less than III, the limiting factor must be identified. Clinical documentation of these limitations can be obtained by using standard goniometric measurements of the joints as well as muscular flexibility tests such as Thomas test or Kendall's test for hip flexor tightness.24
Previous testing has identified that when an athlete achieves a score of II, minor limitations often exist with mobility of one or both hips. When an athlete scores a I or less, a relative asymmetry between stability and mobility may occur around one or both hips.
SUMMARY
The research related to movement-based assessments is extremely limited, mainly because only a few movement-based quantitative assessment tests are being utilized. According to Battie et al,23 the ultimate test of any pre-employment or pre-placement screening technique is its effectiveness in identifying individuals at the highest risk of injury. If the FMS™, or any similarly developed test, can identify at risk individuals, then prevention strategies can be instituted based on their scores. A proactive, functional training approach that decreases injury through improved performance efficiency will enhance overall wellness and productivity in many active populations. {The next issue -Volume 1; Number 3, August, 2006 of NAJSPT will provide the final four fundamental tests incorporated into the Functional Movement Screen (FMS)™.}
Footnotes
The Functional Movement Screen™ is the registered trademark of FunctionalMovement.com with profits from the sale of these products going to Gray Cook and Lee Burton. The Editors of NAJSPT emphasize (and the authors concur) that the use of fundamental movements as an assessment of function is the important concept to be taken from Part I and Part II of this series and can be performed without the use of the trademarked equipment.
REFERENCES
- 1.Gray G. Lower Extremity Functional Profile. Winn Marketing; 1995 [Google Scholar]
- 2.Fields KB, Delaney M. Focusing on the pre-participation sports examination. J Fam Pract. 1989;30:304–312 [PubMed] [Google Scholar]
- 3.Kibler WB, Chandler TJ, Uhl T, Maddux RE. A musculoskeletal approach to the preparticipation physical examination: preventing injury and improving performance. Am J Sports Med. 1989;17:525–527 [DOI] [PubMed] [Google Scholar]
- 4.Meeuwisse WH, Fowler PJ. Frequency and predictability of sports injuries in intercollegiate athletes. Can J Sport Sci. 1988;13:35–42 [PubMed] [Google Scholar]
- 5.Metzl JD. The adolescent pre-participation physical examination: Is it helpful? Clin Sports Med. 2000;19:577–592 [DOI] [PubMed] [Google Scholar]
- 6.Physician and Sportsmedicine The Preparticipation Physical Evaluation. 3rd ed.New York: McGraw-Hill; 2005 [Google Scholar]
- 7.American College of Sports Medicine ACSM's Guidelines for Exercise Testing and Prescription. 6th ed.Philadelphia: Lippincott Williams and Wilkins; 2000 [Google Scholar]
- 8.Meeuwisse WH. Predictability of sports injuries: What is the epidemiological evidence? Sports Med. 1991;12:8–15 [DOI] [PubMed] [Google Scholar]
- 9.Cook G. Baseline sports-fitness testing. In Foran B, ed. High Performance Sports Conditioning. Champaign: Human Kinetics; 2001 [Google Scholar]
- 10.Cook G, Burton L, Fields K, Kiesel K. The Functional Movement Screen. Danville, VA: Athletic Testing Services, Inc; 1998 [Google Scholar]
- 11.Cook G, Burton L, Fields K, et al. Functional movement screening: Upper and lower quarter applications. Presented at the Mid-America Athletic Trainer's Annual Symposium Sioux Falls, South Dakota; 1999 [Google Scholar]
- 12.Cook G. Advance concepts in core training. Presented at the Functional Training Summit Providence, RI; 2004 [Google Scholar]
- 13.McMullen J, Uhl T. A kinetic chain approach for shoulder rehabilitation. Athletic Training. 2000;35:329–337 [PMC free article] [PubMed] [Google Scholar]
- 14.Lephart SM, Pincivero DM, Giraldo JL, Fu FH. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25:130–138 [DOI] [PubMed] [Google Scholar]
- 15.Gallahue DL, Ozmun JC. Understanding Motor Development. 3rd ed.Madison, WI: Brown and Benchmark; 1995 [Google Scholar]
- 16.Baumhauer JF, Alosa DM, Renstrom PA, et al. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23:564–570 [DOI] [PubMed] [Google Scholar]
- 17.Knapik JJ, Bauman CL, Jones BH, et al. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991;19:76–81 [DOI] [PubMed] [Google Scholar]
- 18.Nadler SF, Malanga GA, Feinberg JH, et al. Relationship between hip muscle imbalance and occurrence of low back pain in collegiate athletes: a prospective study. Am J Phys Med Rehabil. 2001;80:572–577 [DOI] [PubMed] [Google Scholar]
- 19.Nadler SF, Moley P, Malanga GA, et al. Functional deficits in athletes with a history of low back pain: A pilot study. Arch Phys Med Rehabil. 2002;88:1753–1758 [DOI] [PubMed] [Google Scholar]
- 20.Neely FG. Intrinsic risk factors for exercise-related lower limb injuries. Sports Med. 1998;26:253–263 [DOI] [PubMed] [Google Scholar]
- 21.Cholewicki J, Panjabi MM, Khachatryn A. Stabilizing function of trunk flexor-extensor muscles around a neutral spine posture. Spine. 1997;22:2207–2212 [DOI] [PubMed] [Google Scholar]
- 22.Gardner-Morse M, Stokes I, Laible JP. Role of muscles in lumbar spine stability in maximum extension efforts. J Orthop Res. 1995;13:802–808 [DOI] [PubMed] [Google Scholar]
- 23.Battie MC, Bigos SJ, Fisher LD, et al. Isometric lifting strength as a predictor of industrial back pain reports. Spine. 1989;14:851–856 [DOI] [PubMed] [Google Scholar]
- 24.Kendall FP, McCreary EK. Muscles Testing and Function. 3rd ed.Baltimore: Williams and Wilkins; 1983 [Google Scholar]
- 25.Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis: Mosby; 2002 [Google Scholar]
- 26.Richardson C, Hodges P, Hides J. Therapeutic Exercise for Lumbopelvic Stabilization: A Motor Control Approach for the Treatment and Prevention of Low Back Pain. Edinburgh: Churchill Livingstone; 2004 [Google Scholar]


