Abstract
Athletes with persistent anterolateral ankle discomfort may have developed sinus tarsi syndrome (STS). Sinus tarsi syndrome develops from excessive motions of the subtalar joint that results in subtalar joint synovitis and infiltration of fibrotic tissue into the sinus tarsi space. Physical therapists treating athletes with ankle conditions should examine the talocrural and subtalar joints for signs of hypermobility as injuries can affect both of these important articulations of the lower extremity. Localized ankle discomfort to the sinus tarsi space and feelings of instability with pronation and supination movements of the subtalar joint will help identify STS. Intervention for this condition will focus on enhancing subtalar joint stability and function of the lower extremities. The purpose of this clinical commentary is to discuss the etiologies and signs of STS and describe the components of an intervention plan appropriate for athletes with STS.
Keywords: ankle injuries, subtalar joint, joint instability
INTRODUCTION
Sinus tarsi syndrome (STS) is a clinical entity characterized by persistent anterolateral ankle pain secondary to traumatic injuries to the ankle. Historically, the etiology of this condition has not been well understood. Recent discussions of STS now describe this entity as primarily an instability of the subtalar joint due to ligamentous injuries that results in a synovitis and infiltration of fibrotic tissue into the sinus tarsi space.2,3 This clinical commentary will describe the possible etiologies and examination findings of athletes with STS and treatment options for this condition for the sports physical therapist.
ANATOMICAL AND KINESIOLOGICAL CONSIDERATIONS
The subtalar joint is comprised of the articulation of the talus and calcaneus across an anterior, middle, and posterior facet. These facets may have variations in their structure and alignments that will affect the movement and stability of the subtalar joint.4 Extrinsic and intrinsic ligaments provide static stability for the subtalar joint. Extrinsic ligaments include the calcaneofibular ligament and the deltoid ligament, which also provide stability for the talocrural joint. The talocalcaneal, interosseuous, and cervical ligaments are the intrinsic ligaments that provide a strong connection for the calcaneal and talar joint surfaces.5 Ruptures of the intrinsic ligaments allow increased movement of the subtalar joint that may result in instability.6–8
The motions of the subtalar joint and the entire rearfoot are complex and have been the subject of extensive study and controversy.4,9,10 The osteokinematics of the subtalar joint occur about a triplanar axis to create pronation and supination movements.5 Supination motions of the subtalar joint create a bony stability through the rearfoot and midfoot that is important for propulsive movements through the foot. Pronation motions create increased mobility of the rearfoot and midfoot joints allowing the foot to accommodate to uneven surfaces.5,11 During running activities, athletes may weight bear entirely onto the forefoot, with ground reaction forces creating supination and pronation motions that occur from the midfoot into the rearfoot. Ground reaction forces during running create movements through the subtalar joint at a higher rate of acceleration and forces than during walking activities.12
The sinus tarsi space is filled with many connective tissues that contribute to the stability and the overall proprioception of the ankle. The space is filled with adipose tissue that serves as a bedding for numerous mechanoreceptors and free nerve endings, which along with the ligaments and muscles provide proprioceptive information on the movement of the foot and ankle.2,13 The vascular supply of the sinus tarsi is provided by an anastomosis of the sinus tarsi and tarsal canal arteries.14 The extensor digitorum brevis muscle attaches to the medial and distal aspect of the sinus tarsi, running over the calcaneocuboid joint towards the toes. The inferior extensor retinaculum lies over the lateral aspect of this space and serves as a covering over the sinus tarsi.2
ETIOLOGY
Sinus tarsi syndrome is believed to occur following a single traumatic event or a series of ankle sprains that result in significant injuries to the talocrural interosseous and cervical ligaments.2,5 These injuries cause instability of the subtalar joint resulting in excessive supination and pronation movements. The excessive movement of the subtalar joint imparts increased forces onto the synovium of the subtalar joint and across the sinus tarsi tissues. The excessive forces result in subtalar joint synovitis with chronic inflammation and infiltration of fibrotic tissues in the sinus tarsi that are responsible for the characteristic anterolateral ankle pain of STS.2 These traumatic injuries may also injure ligaments of the tibiotalar and talocalcaneal joints resulting in increased mobility and instability of the rearfoot and midfoot. Athletes with increased mobility of the talocrural and subtalar joints may be at a greater risk for developing instability after an ankle injury.4
The incidence of STS is unknown, but has been associated with ankle sprains that may also result in talocrural joint instability. Keefe and Haddad15 estimated that 10-25% of patients with chronic talocrural joint instability will also have subtalar joint instability. Hertel et al16 found that 9 out of 12 patients with recurrent ankle sprains had signs of increased talocrural and subtalar joint motions upon a radiographic examination. Hubbard and Hertel17 have advocated that a large percentage of injuries classified as an ankle sprain will include an injury to the subtalar joint ligaments.
EXAMINATION
Athletes with STS usually describe a history of a traumatic ankle injury, typically with a supination/inversion mechanism of injury. Athletes involved with jumping sports may incur an injury to the subtalar joint after coming to an abrupt stop after a jump or a fall. This mechanism is thought to create a “whiplash injury” to the rearfoot with the talus moving anteriorly over the calcaneus.15 This mechanism may result in a sprain to the ligaments of the talocrural joint as well. Physical therapists should also be cautious with athletes who have an extended history of talocrural joint instability even after undergoing reconstruction of the lateral ankle ligaments, as these procedures are intended to improve stability of the talocrural joint and may not improve stability at the subtalar joint.18
An acute ankle injury will typically present with pain accompanied by swelling, ecchymosis, and tenderness in the anterolateral ankle. Because the synovitis and fibrotic tissues associated with STS will take time to develop, athletes with injuries to the subtalar joint may not initially have symptoms that can be localized to the sinus tarsi (Figure 1). Athletes with STS will typically describe a feeling of instability of the foot and ankle that is provoked upon walking over uneven ground, stepping off a curb, or running or sprinting activities.5,15,19 Athletes involved with cutting and jumping activities on firm surfaces will have the greatest difficulty with subtalar instability as these activities will cause excessive movements of the subtalar joint to the end ranges of pronation and supination.15,20
Figure 1.
Symptoms associated with STS are usually described as deep in the ankle and can be localized by athlete pointing to the sinus tarsi space.
Assessment of standing posture in athletes with STS may demonstrate a pes planus posture or an asymmetry of the rearfoot angle with the leg, but these are not typical findings.19 Passive range of motion of the ankle and subtalar joint may not reveal excessive motion, but pain over the sinus tarsi at the end range of ankle plantarflexion with foot supination is typical of STS. Muscles that cross the ankle joint should be assessed for any loss of strength, especially the plantarflexor muscles.
Before examining the subtalar joint, a careful assessment of the talocrural joint should be performed. Anterior and posterior glides of the talus on the tibia and a talar tilt test that produces movement of the talus in the frontal plane are recommended for assessing talocrural joint stability.21,22 Mobility of the contralateral ankle and foot joints should be assessed to determine if the athlete has increased joint mobility that will make them susceptible to developing an instability.
Stability of the subtalar joint is assessed with medial and lateral subtalar joint glides performed by moving the calcaneus over a stabilized talus in the transverse plane and with subtalar joint distraction.16,17 Therman et al20 described a stability test that is thought to recreate instability of the subtalar joint (Figure 2). The test is performed with the athlete in supine with the ankle in 10 degrees of dorsiflexion to keep the talocrural joint in a stable position. The fore-foot is first stabilized by the examiners hand, while an inversion and internal rotational force is applied to the calcaneus. Then an inversion force is applied to the forefoot. The examiner assesses for an excessive medial shift of the calcaneus and a reproduction of the athlete's complaint of instability and symptoms.
Figure 2.
Clinical test for reproduction of subtalar instability. The forefoot is first stabilized by the examiners hand, while an inversion and internal rotational force is applied to the calcaneus.
Reproduction of the athletes feeling of instability or giving way may be reproduced by having the athlete single leg stand on the affected side and perform rotating motions of the leg and foot that may reproduce their symptoms.5 Therapists may also want to assess the athlete during functional activities of walking, running, stepping down from a step, and hopping on the affected extremity. Activities that produce feelings of instability should be assessed for the relative position of the rearfoot and leg for any compensation through the lower extremity the athletes makes when the instability is produced. The activity levels of athletes with STS can be assessed using the Ankle Disability Index, which includes the athlete's rankings of sports related activities.23
DIFFERENTIAL DIAGNOSIS
Athletes with recurrent ankle sprains or symptoms of ankle instability should be suspected of having instability of the talocrural and subtalar joints. Localization of pain to the sinus tarsi with the presence of ankle instability is a good indication that the athlete has developed STS. Conditions that may also produce lateral ankle discomfort include a cuboid subluxation and peroneal tendon subluxation.24 The diagnosis of STS has typically been confirmed by the cessation of symptoms upon injection of lidocaine into the sinus tarsi.1
IMAGING
Athletes suspected of having subtalar joint instability and STS may be referred for diagnostic imaging. Although imaging studies have been proposed to assess the stability of the subtalar joint, most of these methods have been proven to be inconsistent in their findings with low levels of specificity for subtalar joint instability.15,16 Radiographs of the subtalar joint are usually performed with Broden stress views which are a series of oblique-lateral views performed with the ankle and foot placed in inverted and supinated positions.5 Stress fluoroscopy is a method of visualizing the motions of the subtalar joint in real time using low level radiation. The advantage of fluoroscopy over radiographs is that the examiner can attempt to replicate the movements that are causing the athlete's sensation of instability or discomfort from the sinus tarsi.16
Magnetic resonance imaging (MRI) is the best method to visualize the structure within the sinus tarsi, especially the interosseous and cervical ligaments.2 The most distinct finding for individuals with STS is a bright signal seen on T2 weighted images found in the area for sinus tarsal adipose tissue as this represents an infiltration or replacement of this tissue with inflammatory cells and fibrotic tissue.25,26 The MRI findings may also include alterations in the structure of the interosseous and cervical ligaments and degenerative changes in the subtalar joint.2,25
INTERVENTION
Recommendations for rehabilitation of STS include balance and proprioceptive training, muscle strengthening exercises, bracing, taping, and foot orthosis.2,15,24 No random control trials for the efficacy of a rehabilitation program for STS are available. Instability of the talocrural joint or chronic ankle instability (CAI) is a similar and associated entity to subtalar joint instability and STS. Numerous studies of the effects of balance and proprioceptive training for CAI have been conducted, with improvements found in athletes' balance, joint position sense, and functional abilities.27–29
Athletes with STS have developed a chronic inflammatory process that results in a synovitis and inflammation of connective tissues and may benefit from a trial of nonsteroidal anti-inflammatory medication to help control their symptoms and inflammation.30 Cryotherapies, especially the use of ice massage over the lateral ankle, may also be useful for diminishing local inflammation and pain associated with this condition. Athletes with STS may have limited joint mobility at the talocrural and mid tarsal joints that can be addressed with specific joint mobilization techniques. Precautions should be made not to place excessive stress across the subtalar joint with these techniques. Muscular stiffness of the gastrocnemius, posterior tibialis, or peroneal muscles may also be found in athletes with STS, but stretching activities for these muscles should be carefully provided or avoided as excessive forces across the subtalar joint may be detrimental.31
Orthoses
Stability of the subtalar joint may be initially improved with the use of an orthosis.32 Ankle braces intended for CAI may be useful for some athletes with STS, but the overall design of these braces may not significantly improve the stability of the subtalar joint during athletic activities. Foot orthosis have also been recommended as a method for limiting motion at the subtalar joint and reducing symptoms associated with STS.33 The types of shoes the athlete is using for training, practices, and competition should also be considered, as well constructed shoes can restrict excessive rearfoot movements.34
General recommendations for shoes include those with a straight last, a firm heel counter, and rigid material through the midsole.33 Shoes should also be assessed for wear, as materials within a shoe will be begin to break down before the external material show signs of deterioration. The use of a foot orthosis with an athletic shoe should be considered together, as the effect of an orthosis can be inconsistent.35 An ongoing assessment of shoe and orthosis use is needed to provide adequate support of the foot and ankle throughout an athlete's cycle of training and competition.
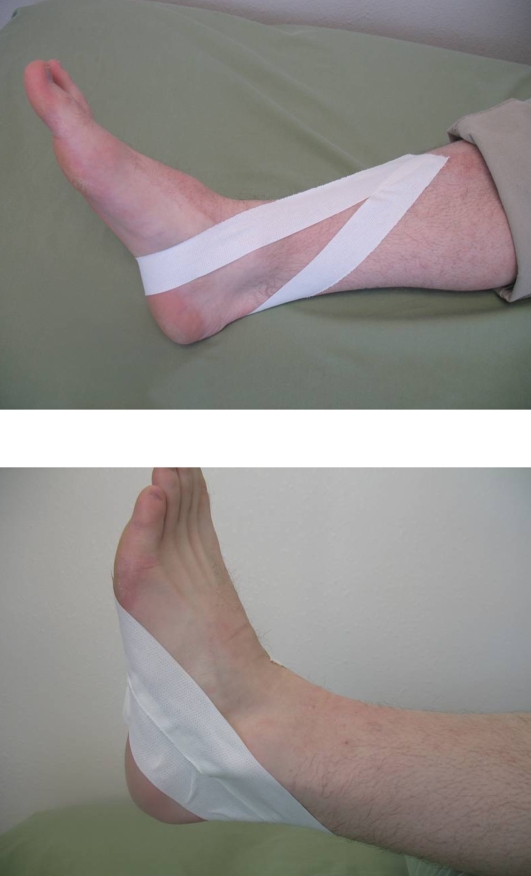
Taping or strapping has also been used to specifically limit movements of the subtalar joint and the midfoot. Wilkerson et al36 have described a taping procedure that combines a closed basket weave with a subtalar sling to control movements at the talocrural and subtalar joints. Viczenzio et al37 have described a modified Low-Dye taping method that uses a calcaneal sling intended to provide support to the medial longitudinal arch of the foot (Figure 3). This method could be used to control or reduce the amount of pronation through the subtalar joint during walking and running activities. Taping techniques have been used as a precursor for the use and selection of specific types of shoes and foot orthotics.37
Figure 3.
Taping for stabilizing the rearfoot. These taping methods can be used in addition to an closed ankle basket weave or a foot Low-Dye method. Figure on the top shows a calcaneal sling with a long strip to control rearfoot pronation, figure on the bottom shows heel lock strips to control rearfoot supination.
Stability Training
Training programs to improve the stability of the subtalar joint and lower extremity function will be the hallmark of treatment plans for STS. Joint stability relies on passive joint structures, dynamic muscular responses, and neurological control. Because tears or ruptures of the interosseous and cervical ligaments of the subtalar joint are believed to be the essential lesions that lead to STS, the dynamic muscular responses and neurological control of the rearfoot will need to be emphasized to compensate for the loss of passive stability.38,39
The muscles that cross the subtalar joint are important for maintaining stability, as they act as force transducers to guide and control the pronation and supination motions of the subtalar joint. The relative strength of these muscles is important, but their reaction time to joint perturbations and the ability to work in a coordinated fashion is even more important for the rehabilitation of STS.40,41 Dynamic stability will also rely on the proprioceptive information from the muscle spindles and Golgi tendon organs of these muscles to compensate for the lack of proprioceptive information from the stabilizing ligaments of the joint.42 The endurance of the muscles will also be important to maintain stability during long bouts of exercise or sports activities.
Training programs to improve joint stability have been described as multiphase processes that start the athlete at an appropriate level of activity and progresses to higher levels of activities while maintaining joint stability.40,42 To help the athlete understand this process the progression of three phases are called: Attain, Maintain, and Sustain. The Attain phase will determine postures or positions the athlete is able to attain in a stable fashion. The Maintain phase will develop coordinated isometric and eccentric muscle contractions of the muscles crossing the joint. The Sustain phase will involve integrating all of the neuromuscular subsystems needed for stability during sports specific activities (Table 1).
Table 1:
Progression through three stages of stability training.
| Stage | Activities | Criteria for Progression |
|---|---|---|
| Attain | Single leg standing – Eyes open and closed | Athlete demonstrates ability to attain a stable position through the foot and ankle. |
| Maintain | Single leg standing – Hip swings, and Star pattern reaching. Heel raises, oscillation with theraband, and impulse with medicine ball. |
Athlete demonstrates ability to maintain stability and good alignment through the lower extremities. |
| Sustain | Lunges and step down exercises Bilateral and single leg hops Forward and backward acceleration and deceleration Pivoting and cutting maneuvers |
Athlete demonstrates the ability to tolerate loading and pushing-off the involved lower extremity. |
The Attain phase for subtalar joint instability is usually started with the athlete in standing positions. Single leg standing, with the contralateral limb held in approximately 30 degrees of hip flexion and 90 degrees of knee flexion, will emphasize ankle balance strategies.43 The clinician should closely observe the arch of the foot and rear-foot to assess the athlete's ability to attain a stable position for the subtalar joint while avoiding excessive pronation movements (Figure 4). The Attain phase begins with the eyes open and attempting to hold the single leg position for 30 to 60 seconds with minimal alterations in body position. Once the athlete is able to hold a single leg standing position consistently, a progression to eyes closed conditions can be made.
Figure 4.
Foot held in an excessive pronated position.
The second phase, Maintain, is performed with perturbations to the single leg positions. Perturbation forces are imparted near the level of the athlete's center of gravity to replicate the type of forces that produce subtalar joint instability during athletic activities. The perturbating forces are intended to facilitate rapid isometric and eccentric contractions of the stabilizer muscles of the ankle.42 Perturbations to standing balance are begun with movements from the contralateral hip starting in the sagittal and coronal planes of motion, progressing to transverse plane motions. Observations of the athlete's rearfoot and hip stability will indicate his/her ability to maintain this position. The clinician needs to insure that the athlete is not using excessive compensatory motions at the rearfoot or hip to maintain a single leg standing position.
The star excursion balance test activities can also be used in this phase, with the athlete in the single leg standing position and touching different lines drawn on the floor in a star pattern.27 Standing heel raises and lowering exercises can be performed at a slow speed in double leg and single leg standing. Emphasis is placed on promoting controlled concentric and eccentric muscle contraction of the ankle plantarflexors and subtalar joint pronator muscles.24 External perturbations can be imparted with the athlete holding a two-foot length of theraband. With both hands in front of the umbilicus, the therapist can then pull on the theraband with oscillating motions. Catching and throwing a small ball or medicine ball while in single leg standing can also be used for perturbations in multiple directions and different timing.40
The Sustain phase will begin with the athlete learning to “close the chain” meaning moving from an open kinematic chain to a stable closed kinematic chain position. The emphasis is on developing the feedforward motor control of the lower extremities.40 This activity can be started by having the athlete perform lunging steps and then stepping down from a 4 or 8 inch step onto the involved extremity into a single leg standing position. Progression can be to lateral lunge steps and lateral step downs. Observations of the athlete's overall control of motion through the lower extremities with an emphasis on alignment of the knee and foot will insure that excessive subtalar joint motion is not occurring.
Progressions of the Sustain phase can be performed with the athlete jumping or hopping in place and then into hopping in different directions. Running activities can begin by acceleration and deceleration with forward and backward motions. Athletes needing to perform pivoting or cutting maneuvers can begin these activities at a slow speed maintaining good alignment of the foot and leg and avoiding excessive motions through the rearfoot.
Return to play criteria is based on the athlete's ability to move in all directions and at appropriate speeds. Athletes performing cutting and jumping maneuvers on firm surfaces, such as basketball and volleyball players, should be returned to full activities over a period of days to insure their tolerance to these stressful maneuvers.15,20 A progression of the athletic activities should be assessed with the athlete in his or her normal practice or competitive environment. The athlete's anterolateral ankle symptoms will need to be well controlled to insure that the return to competition will not create chronic inflammation of the sinus tarsi tissues.
Surgery
Athletes who fail a course of rehabilitation may need an arthroscopic exploration and reconstruction of the subtalar joint in order to return to their athletic pursuits. Arthroscopy of the subtalar joint has allowed for a more precise examination of the subtalar joint and the sinus tarsi. A synovectomy of the subtalar joint along with an arthrotomy of the subtalar joint can be used to remove chronic synovitis and arthrofibrosis that is commonly found in STS.44 Surgical reconstructions of the cervical and interosseous ligaments are made by splitting the tendon of the peroneus brevis and routing the graft through bone tunnels made through the calcaneus and the talus.2,18 Patients with instability of the talocrural and subtalar joints may require a tri-ligamentous reconstruction of the anterior talofibular, calcaneofibular, and cervical ligaments.18 Patients who present with significant joint degeneration or continue to have persistent symptoms even after ligamentous reconstruction may require an arthodesis resulting in an isolated fusion of the subtalar joint.45
Athletes who have undergone ligamentous reconstructions will commonly be immobilized for a 6-week period, followed by a rehabilitation program to regain normal ankle mobility, strength, and balance. Return to athletic activities usually begins at 4 to 6 months post-operatively.18 Common post-operative problems are transient loss of sensation of the lateral ankle and foot and persistent peroneal weakness.3
SUMMARY
Sinus tarsi syndrome is a condition of the ankle and foot that results from instability of the subtalar joint. Athletes with this condition typically have complaints of instability with functional activities and persistent anterolateral ankle discomfort. The joints of the ankle should be assessed for mobility and reproduction of feelings of instability and discomfort. Treatments for this condition will need to control the athlete's ankle discomfort and improve the overall stability of the foot and ankle. Therapists should design intervention plans based on the athlete's need for training and competition.
REFERENCES
- 1.O'Connor D. Sinus tarsi syndrome: A clinical entity. J Bone Joint Surg. 1958;40:720–726 [Google Scholar]
- 2.Pisani G, Pisani PC, Parino E. Sinus tarsi syndrome and subtalar joint instability. Clin Pod Med Surg. 2005;22:63–77 [DOI] [PubMed] [Google Scholar]
- 3.Frey C, Feder KS, DiGiovanni C. Arthroscopic evaluation of the subtalar joint: Does sinus tarsi syndrome exist? Foot Ankle Int. 1999;20:185–191 [DOI] [PubMed] [Google Scholar]
- 4.Barbaix E, VanRoy P, Clarys JP. Variations of anatomical elements contributing to subtalar joint stability. Ergonomics. 2000;43:1718–1725 [DOI] [PubMed] [Google Scholar]
- 5.Budny A. Subtalor joint instability: Current clinical concepts. Clin Pod Med Surg. 2004;21:449–460 [DOI] [PubMed] [Google Scholar]
- 6.Kjaerrsgarrd-Anderson P, Wethelung JO, Helmig P, et al. The stabilizing effect of the ligamentous structures in the sinus and canalis tarsi on movments in the hindfoot: An experimental study. Am J Sports Med. 1988;16:512–516 [DOI] [PubMed] [Google Scholar]
- 7.Mullen JE, O'Malley MJ. Sprains--residual instability of subtalar, Lisfranc joints, and turf toe. Clin Sports Med. 2001;23:97–121 [DOI] [PubMed] [Google Scholar]
- 8.Tochigi Y, Amendola A, Rudert MJ, et al. The role of the interosseous talocalcaneal ligament in subtalar joint stability. Foot Ankle Int. 2004;25:588–596 [DOI] [PubMed] [Google Scholar]
- 9.Sarrafin S. Biomechanics of the subtalor joint complex. Clin Orthop. 1993;290:17–26 [PubMed] [Google Scholar]
- 10.McPoil TC, Hunt GC. Evaluation and management of foot and ankle disorders: Present problems and future directions. J Orthop Sports Phys Ther. 1995;21:381–388 [DOI] [PubMed] [Google Scholar]
- 11.Neumann DA. Kinesiology of the Musculoskeletal System. St. Louis: Mosby; 2002 [Google Scholar]
- 12.Areblad M, Nigg BM, Ekstrand JM, et al. Three-dimensional measurement of rearfoot motion during running. J Biomech. 1990;23:933–940 [DOI] [PubMed] [Google Scholar]
- 13.Akiyami K, Takakura Y, Tomita Y, et al. Neurohistology of the sinus tarsi and sinus tarsi syndrome. J Orthop Sci. 1999;4:299–303 [DOI] [PubMed] [Google Scholar]
- 14.Andermahr J, Helling HJ, Rehm KE, et al. The vascularization of the os calcaneum and the clinical consequences. Clin Orthop Relat Res. 1999;363:212–218 [PubMed] [Google Scholar]
- 15.Keefe DT, Haddad SL. Subtalar instability – Etiology, diagnosis, and management. Foot Ankle Clinics. 2002;7:577–609 [DOI] [PubMed] [Google Scholar]
- 16.Hertel J, Denegar CR, Monroe MM, Stokes WL. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sports Exerc. 1999;31:1501–1508 [DOI] [PubMed] [Google Scholar]
- 17.Hubbard TJ, Hertel J. Mechanical contribution to chronic lateral ankle instability. Sports Med. 2006;36:263–277 [DOI] [PubMed] [Google Scholar]
- 18.Schon LC, Clanton TO, Baxter DE. Reconstruction for the subtalar instability: A review. Foot Ankle. 1991;11:319–325 [DOI] [PubMed] [Google Scholar]
- 19.Shear MS, Baitch SP, Shear DB. Sinus Tarsi Syndrome: The importance of biomechanically-based evaluation and treatment. Arch Phys Med Rehabil. 1993;74:777–781 [DOI] [PubMed] [Google Scholar]
- 20.Thermann H, Zwipp H, Tshcernes H. Treatment algorithm of chronic ankle and subtalar instability. Foot Ankle. 1997;18:163–169 [DOI] [PubMed] [Google Scholar]
- 21.Meyer JM, Garcia J, Hoffmeyer P, et al. The subtalar sprain. A roentgenographic study. Clin Orthop Relat Res. 1988;226:169–173 [PubMed] [Google Scholar]
- 22.Renstrom PA. Persistently painful sprained ankle. J Am Acad Orthop Surg. 1994;2:270–280 [PubMed] [Google Scholar]
- 23.Hale SA, Hertel J. Reliability and sensitivity of the Foot and Ankle Disability Index in subjects with chronic ankle instability. J Athl Train. 2005;40:35–40 [PMC free article] [PubMed] [Google Scholar]
- 24.Hunter S, Prentice WE. Rehabilitation of the ankle and foot. In: Prentice WE, Voight ML. Techniques in Musculoskeletal Rehabilitation. New York: McGraw Hill; 2001:603–641 [Google Scholar]
- 25.Lektrakul N, Chung CB, Yeong-man L, et al. Tarsal sinus: Arthographic, MR imaging, MR arthrographic, and pathological findings in cadavers and retrospective study data in patients with sinus tarsi syndrome. Radiology. 2001;219:802–810 [DOI] [PubMed] [Google Scholar]
- 26.Klein MA, Spreitzer AM. MR imaging of the tarsal sinus and canal: Normal anatomy, pathological findings, and features of the sinus tarsi syndrome. Radiology. 1993;186:233–240 [DOI] [PubMed] [Google Scholar]
- 27.Hale S, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2007;37:303–311 [DOI] [PubMed] [Google Scholar]
- 28.Rozzi SL, Lephart SM, Sterner R, et al. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29:478–486 [DOI] [PubMed] [Google Scholar]
- 29.Eils E, Rosenbaum D. A multi-station proprioceptive exercise program in athletes with ankle instability. Med Sci Sports Exerc. 2001;33:1991–1998 [DOI] [PubMed] [Google Scholar]
- 30.Schelhase EM, Chen JT, Jordan J, et al. Pharmacology and its impact on the rehabiliation process. In: Magee DJ, Zachajewski JE, Quillen WS. Scientific Foundations and Principles of Practice in Musculoskeletal Rehabilitation. St. Louis: Elsevier; 2007:255–281 [Google Scholar]
- 31.Maffrey LL. Arthrokinematics and mobilization of musculoskeletal tissue: The principles. In: Magee DJ, Zachajewski JE, Quillen WS. Scientific Foundations and Principles of Practice in Musculoskeletal Rehabilitation. St. Louis: Elsevier; 2007:487–526 [Google Scholar]
- 32.Kato T. The diagnosis and treatment of instability of the subtalar joint. J Bone Joint Surg Br. 1990;77:400–406 [PubMed] [Google Scholar]
- 33.Yamashita MH. Evaluation and selection of shoe wear and orthoses for the runner. Phys Med Rehabil Clin N Am. 2005;16:801–829 [DOI] [PubMed] [Google Scholar]
- 34.Nawoczenski DA, Janisse DJ. Foot orthoses in rehabilitation–what's new. Clin Sports Med. 2004;23:157–167 [DOI] [PubMed] [Google Scholar]
- 35.Nigg B, Stergiou P, Cole G, et al. Effect of shoe inserts on kinematics, center of pressure, and leg joint moments during running. Med Sci Sports Exerc. 2003;35:314–319 [DOI] [PubMed] [Google Scholar]
- 36.Wilkerson DB, Kovaleski JE, Meyer M, Stawiz C. Effects of the subtalar sling ankle taping technique on combined talocrural-subtalar joint motions. Foot Ankle Intl. 2005;26:239–246 [DOI] [PubMed] [Google Scholar]
- 37.Vicenzino B, Franettovich M, McPoil T, et al. Initial effects of anti-pronation tape on the medial longitudinal arch during walking and running. Br J Sports Med. 2005;39:939–943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Delahunt E, Monaghan K, Caulfield B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. Am J Sports Med. 2006;34:1970–1976 [DOI] [PubMed] [Google Scholar]
- 39.Delahunt E, Monaghan K, Caulfield B. Ankle function during hopping in subjects with functional instability of the ankle joint. Scand J Med Sci Sports. 2007;17:641–648 [DOI] [PubMed] [Google Scholar]
- 40.Voight ML, Cook G. Impaired neuromuscular control: Reactive neuromuscular training. In: Prentice WE, Voight ML. Techniques in Musculoskeletal Rehabilitation. New York: McGraw Hill; 2001:93–124 [Google Scholar]
- 41.Karlsson J, Andreasson GO. The effect of external ankle support in chronic lateral ankle instability. An electromyographic study. Am J Sports Med. 1992;20:257–261 [DOI] [PubMed] [Google Scholar]
- 42.Magee DJ, Zachazewski JE. Principles of stabilization training. In: Magee DJ, Zachajewski JE, Quillen WS. Scientific Foundations and Principles of Practice in Musculoskeletal Rehabilitation. St. Louis: Elsevier; 2007: 388–413 [Google Scholar]
- 43.Maki BE, McIlroy WE. The role of limb movements in maintaining upright stance: The “change-insupport” strategy. Phys Ther. 1997;77:488–507 [DOI] [PubMed] [Google Scholar]
- 44.Ollof LM, Schulhofer SD, Bocko AP. Subtalor joint arthroscopy for sinus tarsi syndrome: A review of 29 cases. J Foot Ankle Surg. 2001;40:152–157 [DOI] [PubMed] [Google Scholar]
- 45.Mann RA, Beaman DN, Horton GA. Isolated subtalar arthrodesis. Foot Ankle Int. 1998;19:511–519 [DOI] [PubMed] [Google Scholar]