Abstract
Rolling is a movement pattern seldom used by physical therapists for assessment and intervention with adult clientele with normal neurologic function. Rolling, as an adult motor skill, combines the use of the upper extremities, core, and lower extremities in a coordinated manner to move from one posture to another. Rolling is accomplished from prone to supine and supine to prone, although the method by which it is performed varies among adults. Assessment of rolling for both the ability to complete the task and bilateral symmetry may be beneficial for use with athletes who perform rotationally-biased sports such as golf, throwing, tennis, and twisting sports such as dance, gymnastics, and figure skating. Additionally, when used as intervention techniques, the rolling patterns have the ability to affect dysfunction of the upper quarter, core, and lower quarter. By applying proprioceptive neuromuscular facilitation (PNF) principles, the therapist may assist patients and clients who are unable to complete a rolling pattern. Examples given in the article include distraction/elongation, compression, and manual contacts to facilitate proper rolling. The combined experience of the four authors is used to describe techniques for testing, assessment, and treatment of dysfunction, using case examples that incorporate rolling. The authors assert that therapeutic use of the developmental pattern of rolling with techniques derived from PNF is a hallmark in rehabilitation of patients with neurologic dysfunction, but can be creatively and effectively utilized in musculoskeletal rehabilitation.
INTRODUCTION
As humans develop from small, relatively immobile infants at birth into fully developed, amazingly mobile adults, they pass through many predictable patterns of body control and movement. In motor development, these patterns can be described as both reflexive and intentional movements, both of which serve as developmental milestones.1 These concepts are familiar to the therapists who treat pediatric clientele with neurodevelopmental diagnoses. Many therapists who treat adult patients and clients may fail to remember the principles of developmental postures and their sequence. In settings where patients with orthopedic and sports injuries predominate, the therapist can easily become focused on discrete local problems (or impairments) and miss the global effects (functional limitations) these problems create. In mature movement strategies/motor programs, the presence of developmental skills are not readily identifiable, but may in fact be a part of movement. An example of this principle is the movement of rolling. Although most adults do not consider the act of rolling to be an important part of complex movement skills, rolling may be a novel method to assess for, and intervene with, inefficient movements that involve rotation of the trunk and body, weight shifting in the lower body, and coordinated movements of the head, neck, and upper body.
The developmental milestones through which humans progress are related to developmental postures.2 Human infants are initially able to exist in sidelying, prone, or supine and are unable to move between these positions without assistance. These postures offer the infant the greatest amount of support/contact from the surface, and are the beginning of the developmental sequence and the development of motor control. As the infant matures, head control is achieved by four months of age leading to the ability to transition from one posture to the other, also known as rolling.2 Rolling is defined as “moving from supine to prone or from prone to supine position” 1 and involves some aspect of axial rotation. Rotational movements are described as a form of a righting reaction because, as the head rotates, the remainder of the body twists or rotates to become realigned with the head.1,2 Rolling can be initiated either by the upper extremity or the lower extremity, each pattern producing the same functional outcome: movement from prone to supine or supine to prone.
The authors propose four variations of rolling which can be used to accomplish movement from prone to supine and supine to prone. Movement from the start position (either supine or prone) can be accomplished by using one upper extremity or one lower extremity to initiate movement. These four variations will be described in detail in the assessment section of this article. Each of the four variations is performed first with one upper extremity or lower extremity and then with the contralateral upper extremity or lower extremity in order to assess for symmetry, control, quality, and the ability to complete the roll.
When using rolling as an intervention, the upper extremity patterns make use of the fact that movements of the neck facilitate trunk motions3–5 or stated more simply, “where the eyes, head, and neck go, the trunk will follow.” By applying the proprioceptive neuromuscular facilitation (PNF) principle of irradiation (defined later in this article), the following can be utilized therapeutically: neck flexion facilitates trunk flexion, neck extension facilitates trunk extension, and full neck rotation facilitates lateral flexion of the trunk.3,4 Neck patterns can even be used to achieve irradiation into distal parts of the body, for example, neck extension can facilitate extension and abduction of the hip.3,4
Typically an infant can perform basic log rolling, with the body moving as a unit at four to five months of age, typically moving from prone to supine at four months of age, followed by moving from supine to prone (although the order varies in infants). Finally, segmental or “automatic” rolling occurs at six to eight months of age, which involves deliberate, organized progressive rotation of segments of the body.1 Some children actually combine multiple rolls, performed consecutively, as a method of locomotion across a floor. Adults use a form of rolling that is segmental, but has also been described as “deliberate.” Adult rolling described by Richter and colleagues6 found that normal adults use a variety of movement patterns to roll, most likely related to the flexibility and strength (or lack thereof) in the individual performing the movement. Several of the movement patterns described by Richter et al,6 were similar to the original patterns of rolling movement described by Voss et al4 in their original text on PNF. The variability of movement patterns used by adults to roll gives therapists multiple options to use when training or retraining adults in the task of rolling.6
Although the skill of rolling is an early developmental task that continues to be used throughout a lifetime, rolling may become altered or uncoordinated due to muscular weakness, stiffness or tightness of structures, or lack of stability in the core muscles. Several potential dysfunctions and assessments for these problems that affect rolling in adults will be addressed in detail in a subsequent section. Adults often use inefficient strategies to complete the task of rolling, some of which are compensatory and disorganized, serving to perpetuate the dysfunction(s) associated with the movement. The authors assert that when rolling is asymmetrical, the client demonstrates a break in normal patterning (symmetry), which can help the clinician visualize the interplay between the local (impairment level) problem and the global effect (functional limitation).
Developmentally important positions, such as kneeling and quadruped, are useful to the breakdown of complex motor patterns.7 While these two postures are used commonly by the sports physical therapist in interventions for orthopedic pathology by addressing muscular strength, core control, balance, and coordination, rolling is not. Although this article deals with the movement of rolling, these other postures are still important to the examination and training of athletes whose sports involve the use of rotation (tennis, golf, swimming, baseball).
Once a human is upright for motor tasks, rolling becomes less important for movement or access to the environment and, thus, is used less. Adults generally only use rolling to transition from prone to supine, as if turning over in bed. Most adults do not consciously make use of rolling in everyday mobility tasks, exercise routines, or as a part of more difficult rotational movements/skills. Rolling is a good choice for assessment and training because rolling is not commonly practiced. Therefore, compensation and incorrect performance can be easily observed. Rolling can be used as both a functional activity and an exercise for the entire body.3 It is the assertion of the authors of this article that many sports physical therapists forget or ignore rolling as an assessment and rehabilitative technique.
The Relationship of Rolling to Rotation
Frequently, even highly functional patients demonstrate dysfunctional sequencing or poor coordination during active rotational movements that are part of their functional demands/tasks. Rolling patterns can easily illuminate rotational movement pattern dysfunction, especially when comparing between sides. It should be noted that the movement dysfunction is usually a problem with sequence and stabilization rather than a deficiency in strength of a prime mover. Theoretically, a person should be able to roll (rotate) equally easily to either the right or the left. Frequently athletes have a typical pattern or habitual “good side” for rotational activities. Consider the gymnast, thrower, or golfer; each of whom rotates to the same direction repeatedly, according to the demands of their sport. Examples include the twisting and spinning motions used during tumbling, the unidirectional rotation used during the throwing motion, and the same-side rotational motions that comprise the golf swing. In each of these examples, the athlete has a preferential side, and a pattern of rotation (e.g. always to the left in a right handed thrower or golfer) which is typical for the performance of their sport, and may have asymmetry in rolling to the opposite side.
The Relationship of Rolling to Other Movement Tasks
Although described in relationship to rotational tasks and movements, rolling is not only related to rotational tasks. The rolling patterns can function as a basic assessment of the ability to shift weight, cross midline, and coordinate movements of the extremities and the core. Abnormalities of the rolling patterns frequently expose proximal to distal and distal to proximal sequencing errors or proprioceptive inefficiency that may present during general motor tasks. Finally, many adults have lost the ability to capture the power or utilize the innate relationship of the head, neck, and shoulders to positively affect coordinated movements.
Rolling as Assessment
As indicated previously, many high level tasks performed are often in a prescribed and unilateral motion. Even though a task or sport specific skill may be demonstrated by patients and clients at high levels, the fundamentals of the task of rolling should not be altered when compared bilaterally. Whether rolling is initiated by the upper or lower extremities, the state of optimal muscle recruitment, coordination, and function is reached when symmetry is present. For example, a right handed thrower should be able to complete all four variations of rolling, with equal ease regardless of direction. If during assessment the different rolling tasks are not symmetrical and equal, the clinician should consider that foundational mobility or neuromuscular coordination may be compromised.
Because rolling precedes other locomotion activities in the developmental postures of infants and children, rolling can be used as a discriminatory test that uses regression to a more basic developmental task to locate and identify dysfunction in the form of poor coordination and stability of rotation. Without a doubt, mobility, core stability, controlled mobility, and properly sequenced loading of the segments of the body are required to perform these rolling tests correctly. Assessment of necessary precursor abilities should always precede common measurements of function which include strength, endurance, balance, gait, etc. Simply stated, movement quality appraisal should precede movement quantity appraisal.
Patients or clients who are being asked to perform the rolling tests must have sufficient trunk, upper extremity, and lower extremity mobility. An example of this principle is the use of the seated trunk rotation test that is designed to identify how much rotational mobility is present in the thoracolumbar spine. To pass this screen the patient must demonstrate sufficient mobility to ensure greater than 30 degrees of rotation bilaterally (Figure 1).
Figure 1.

Seated rotation test used to identify thoracolumbar rotational mobility. Begin in a seated position with knees and feet together, body upright and erect, arms crossed across the chest, while maintaining a gaze to the front. Ask patient to rotate the trunk to the right and to the left as far as possible. Examine for asymmetry by measuring with a goniometer. Normal is 30° bilaterally.
If a patient or client cannot roll, it may simply be due to a mobility impairment in the thoracic spine. A mobility problem should not be addressed by a stability exercise. It is imperative that potentially contributory mobility problems are addressed prior to assessing the functional rolling motions. Figures 2a and 2b depict an example intervention for a patient or client who fails the rotation screen secondary to diminished thoracic rotation. Note how the anteriorly tilted position of the pelvis in the quadruped position locks the lumbar spine in extension which allows for a targeted stretch of the thoracic spine. Once the rotation motion is equal bilaterally (patient can pass the rotation screen test) or has significantly progressed toward appropriate mobility, interventions for assisted rolling may begin. In this case, rolling may be viewed as an adjunct exercise to encourage mobility.
Figure 2A.
Example mobility technique for lower thoracic rotation, note pelvic position to ensure locking of lumbar segments. Therapist can use an interlocked arm to assist patient into rotation.
Figure 2B.
Example mobility technique for upper thoracic rotation. Again, note pelvic position to ensure locking of lumbar segments.
Rolling tasks occur about diagonal axes.3 Figures 3a and 3b depict the two diagonals that comprise the axes of movement used by humans during the task of rolling. These graphics also demonstrate the starting positions for supine to prone rolling and prone to supine rolling movements, respectively. Typically, the axis for rolling does not involve the extremity that leads the movement.
Figure 3A.
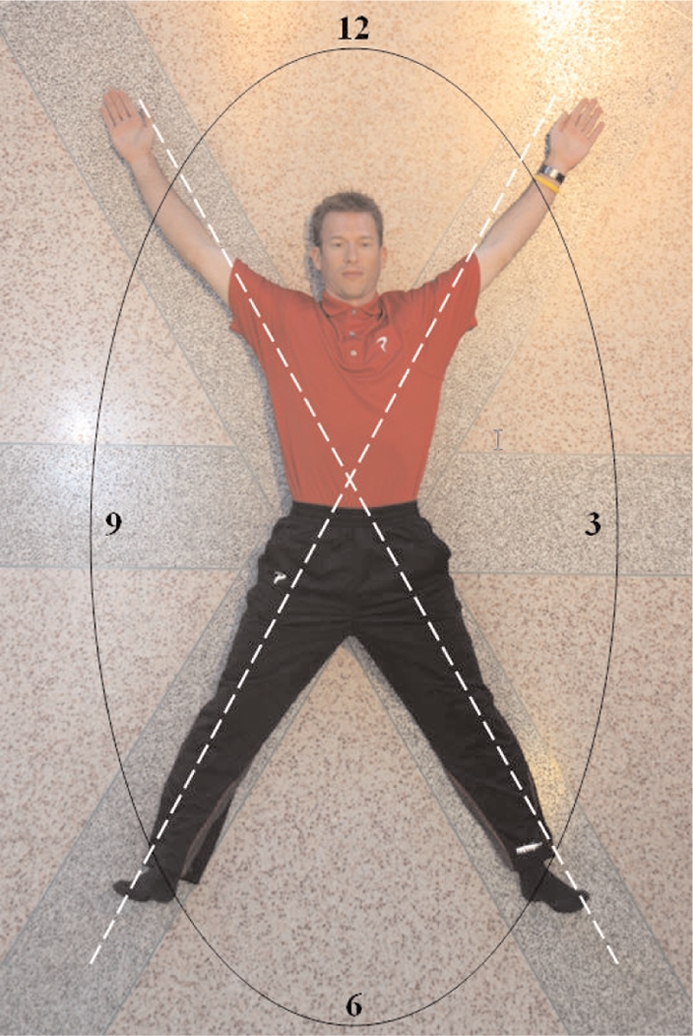
(Left) Diagonal axes of rotation shown in supine, and beginning position for supine to prone rolling.
Figure 3B.
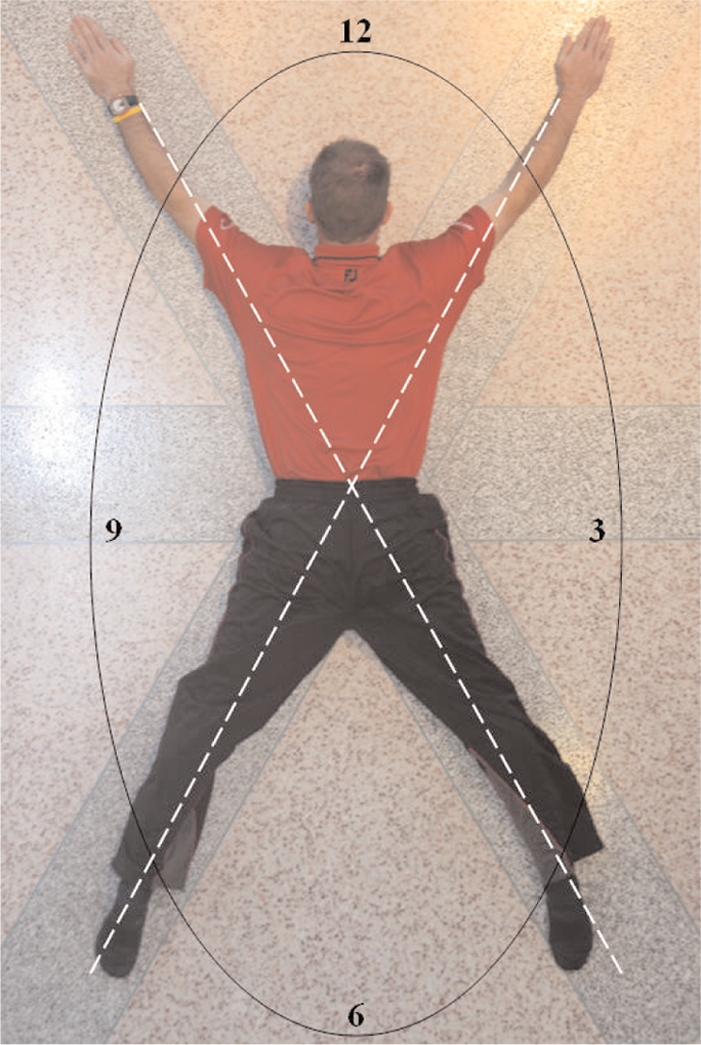
(Right) Diagonal axes of rotation shown in prone, and beginning position for prone to supine rolling.
Several neurophysiologic principles of PNF can be applied to the assessment and enhancement of the task of rolling. During treatment, the therapist may use visual, verbal, and tactile techniques to cue and resist the neck, trunk, or extremities to promote a maximal response from muscle groups used during rolling.3–5 These cues serve to enhance the quality of the skilled motion and to move the patient toward functional gains. Verbal cues will be described with each variant of rolling, as well as suggestions for visual and tactile cues to enhance overflow or irradiation.
Overflow or irradiation can be defined as the increase in facilitation that alters the excitatory threshold level at the anterior horn cell.8 By facilitating the stronger portions of a pattern, the motor unit activation of the involved or weaker portions is enhanced, thereby strengthening the response of the involved segments.9 Normally, overflow occurs into those muscles that offer synergistic support for the prime movers used during a motor task. Overflow can occur from proximal to distal or vice versa. The increased peripheral feedback that occurs when more than the involved segment participates in the activity may enhance the ability to respond and to learn the motor task.9
For example, when using tubing for axis elongation facilitation, the patient's upper extremity or lower extremity is placed and held in a traction or elongated position, thereby pre-activating the phasic Type II receptors and promoting stretching of the synergistic trunk musculature. These elongated muscles provide a stable base upon which rolling occurs and utilize multiple segments to enhance motor learning. Conversely, joint approximation by compression of joint surfaces stimulates the static Type I receptors that facilitate the postural extensors and stabilizers.9 This technique, applied to the upper extremity or lower extremity which are a part of the rolling axis, can be used to improve the performance of a person having difficulty with the rolling task.
Four different rolling tasks are described. Each description will include the axis of rotation, specific instructions for performance of the test, verbal cues, and potential tactile or resistance cues.
Supine to Prone Leading with the Upper Body
This pattern isolates shoulder flexion/horizontal adduction, which leads to trunk flexion/rotation, culminating in pelvic rotation/hip flexion that allows for completion of the roll. The patient lies supine with legs extended and slightly abducted; arms flexed overhead, also slightly abducted. Head is in neutral rotation (Refer to Figure 3a for the start position). When rolling to the left, the axis of rotation is formed by the upper extremity of the side that the individual is rolling towards and the lower extremity of the side the individual is rolling from.
Ask patient to actively roll his or her body to the prone position starting with his or her left arm by reaching obliquely across body.
The patient's head and neck should flex and turn toward the right axilla. Remember, the head and neck are connected to the core, therefore where the head and neck lead the body will follow. (Figure 4) Facilitation of rolling from supine to prone from the cranial end of the body involves activation of the flexor chain: the neck, trunk, and hip flexors sequentially.
The lower body should not contribute to the roll. Cue the patient to resist the temptation to push with the left lower extremity.
The therapist can also give visual reference by placing his or her body on the side toward which the rotation is occurring, in this case, on the right side.
Evaluate for quality, ease of movement, synergy, and ability to complete the roll.
Repeat to the opposite side, leading with the right arm. Evaluate carefully for symmetry between the rolling to the right and rolling to the left.
Figure 4.

Intermediate position for rolling supine to prone, leading with left upper extremity.
Verbal cueing:
Look with the eyes and head
Reach arm across body and turn head into shoulder
-
Elongate the axis:
- Make the axis (left) leg long – “reach”
- Make the axis (right) arm long – “reach”
- Stay long through the axis
- Verbal sequence: “Reach-lift arm-look into shoulder-roll”
NOTE:
The following techniques are not used during the initial assessment, rather, may be used when dysfunctional patterns of movement are identified. These facilitory techniques are intended to be used for short term assistance and then eliminated as soon as technique is improved and perfected.
Tactile/resistance cueing to assist rolling:
Use proximal manual contacts to facilitate protraction of the scapula by the therapist positioning him or herself on the side toward which the patient is rolling, while cueing the patient to “pull your shoulder down toward your opposite hip.”
Use distal manual contacts to approximate the upper extremity of the axis arm to facilitate elongation of the axis. For example, in an upper body driven roll led with the left upper extremity, offer manual approximation through the right upper extremity at the wrist/hand to encourage the response of elongation.
Use tubing to cue the patient/client to elongate the axis either through the lower or upper body. For example, in an upper body driven roll led with the left upper extremity, place tubing on either the right distal upper extremity anchored lower on the body or on the left distal lower extremity to encourage the response of elongation.
Prone to Supine Leading with Upper Body
This pattern begins with isolated shoulder flexion, leading to trunk extension/rotation, culminating in pelvic rotation that allows for the completion of the roll. Patient lies prone with legs extended and slightly abducted; arms flexed overhead, also slightly abducted as depicted in Figure 3b. When rolling toward the left side of the body, the axis of rotation is formed by the upper extremity of the side that the individual is rolling towards and the lower extremity of the side the individual is rolling from, or in this case the left upper extremity and right lower extremity, respectively.
Ask patient to actively roll his or her body to the supine position starting with his or her left arm only. The head should extend and rotate toward the opposite side. Remember, the head and neck are connected to the core, therefore where the head and neck lead the body will follow.
During this form of the test, the lower body should not contribute to the roll.
The body will always follow the head. Facilitation of rolling from prone to supine from the cranial end of the body, involves activation of the extensor chain: the neck, trunk, and hip extensors, sequentially.
The therapist can also give visual/auditory reference by placing his or her body on the side toward which the rotation is occurring, in this case the left side. (Figure 5 demonstrates the therapist giving a cue while placed on the right side.)
Evaluate for quality, ease of movement, synergy, and ability to complete the roll.
Repeat to the opposite side leading with the right arm. Evaluate carefully for symmetry between rolling to the right and rolling to the left.
Figure 5.
Intermediate position for rolling prone to supine, leading with left upper extremity, with therapist placed in visual field for cueing, also using auditory cueing by snapping fingers.
Verbal cueing:
Lift arm and look up and over the opposite shoulder.
-
Elongate the axis (see tactile cues below):
- Make the axis (right) leg long – “reach”
- Make the axis (left) arm long – “reach”
- Stay long through the axis
- Verbal sequence: “Reach-lift arm-look over shoulder-roll”
NOTE:
The following techniques are not used during the initial assessment, rather, these may be used when dysfunctional patterns of movement are identified. These facilitory techniques are intended to be used for short term assistance and then eliminated as soon as the technique is improved and perfected.
Tactile/resistance cueing to assist rolling:
Use proximal manual contacts to facilitate retraction of the scapula by the therapist positioning him or herself on the side toward which the patient is rolling, using the verbal cue “lift and pull your shoulder blade down and in.” (Figure 6)
Use manual contacts to approximate the upper extremity of the axis arm to facilitate elongation of the axis. For example, in an upper body driven roll led with the right upper extremity, offer manual approximation through the left upper extremity to encourage the response of elongation.
Use tubing to cue the patient/client to elongate the axis either through the lower or upper body. For example, in an upper body driven roll led with the right upper extremity, place tubing on either the left distal upper extremity anchored lower on the body or on the right distal lower extremity to encourage the response of elongation.
Figure 6.

Intermediate position for rolling prone to supine, leading with right upper extremity, using manual contact on scapula for facilitation.
Supine to Prone Leading with the Lower Body
This pattern isolates hip flexion, which leads to pelvic rotation/lumbar flexion, and culminates in trunk flexion/rotation to allow for completion of the roll. The patient lies supine on the ground with his or her legs extended and his or her arms flexed over his or her head on the ground. The head is in neutral rotation. (Refer to Figure 3a for start position.) Like the upper extremity initiated supine to prone roll, this task utilizes a flexed posture and is often easier than the prone to supine task. When rolling to the left, the axis of rotation is formed by the lower extremity of the side that the individual is rolling towards and the upper extremity of the side the individual is rolling from, or in this case the left lower extremity and right upper extremity, respectively.
Ask patient to actively roll his or her body to the prone position starting with the right leg only.
Lead with right hip flexion followed by the adduction of the extended leg.
The upper body should and not contribute to the roll. During lower body initiated rolls, the head and neck play less of a role, and are therefore not cued.
Evaluate for quality, ease of movement, synergy, and ability to complete the roll.
Repeat to the opposite side, leading with the left lower extremity. Evaluate carefully for symmetry between rolling to the right and rolling to the left.
Verbal cueing:
-
Elongate the axis:
- Make the axis (right) leg long – “reach”
- Make the axis (left) arm long – “reach”
- Stay long through the axis
- Verbal sequence: “Reach – lift leg across body – roll”
NOTE:
The following techniques are not used during the initial assessment, rather, may be used when dysfunctional patterns of movement are identified. These facilitory techniques are intended to be used for short term assistance and then eliminated as soon as technique is improved and perfected.
Tactile/resistance cueing to assist rolling:
Use proximal manual contacts to facilitate protraction of the pelvis by the therapist positioning him or herself on the side toward which the patient is rolling, using the verbal cue “pull your pelvis up and forward.”
Use distal manual contacts to approximate the lower extremity of the axis leg to facilitate elongation of the axis. For example, in a lower body driven roll led with the right lower extremity, offer manual approximation through the sole of the foot to encourage the response of elongation.
Use tubing to cue the patient to elongate the axis either through the lower body or through the upper body. For example, in a lower body driven roll led with the right lower extremity, place tubing on either the left distal lower extremity anchored higher on the body or on the right distal upper extremity to encourage the response of elongation.
Prone to Supine Leading with the Lower Body
This pattern begins with hip extension which initiates the roll and leads to pelvic rotation/lumbar extension and culminates in trunk extension/rotation, completing the roll. This pattern helps to identify weak gluteal muscles by isolating hip extension/lateral rotation. Patient lies prone with legs extended and slightly abducted; arms flexed overhead, also slightly abducted. Head is in neutral rotation. (Refer again to Figure 3b.) When rolling toward the left side of the body the axis of rotation is formed by the lower extremity of the side that the individual is rolling toward and the upper extremity of the side the individual is rolling from, or in this case the left lower extremity and right upper extremity, respectively.
Ask patient to actively roll his or her body to the supine position starting with the right leg only.
Attempt to perform with a fully extended lower extremity, but if unable to complete the roll, the patient may flex the knee if needed in order to initiate the roll. Cue to extend at the hip and then at the knee.
During this form of the test, the upper body should not contribute to the roll. During lower body initiated rolls the head and neck play less of a role, and are therefore not cued.
Evaluate for quality, ease of movement, synergy, and ability to complete the roll.
Repeat to the opposite side, leading with the left lower extremity. Evaluate carefully for symmetry between rolling to the right and rolling to the left.
Verbal cueing:
-
Elongate the axis:
- Make the axis (right) leg long – “reach”
- Make the axis (left) arm long – “reach”
- Stay long through the axis
- Verbal sequence: “Reach – lift leg across body – roll”
NOTE:
The following techniques are not used during the initial assessment; rather, these may be used when dysfunctional patterns of movement are identified. These facilitory techniques are intended to be used for short term assistance and then eliminated as soon as the technique is improved and perfected.
Tactile/resistance cueing to assist rolling:
Use proximal manual contacts to facilitate retraction of the pelvis by the therapist positioning him or herself on the side toward which the patient is rolling using the verbal cue “lift and pull your pelvis back” (Figure 7)
Use distal manual contacts to approximate the lower extremity of the axis leg to facilitate elongation of the axis. For example, in a lower body driven roll led with the right lower extremity, offer manual approximation through the sole of the foot to encourage the response of elongation.
Use tubing to cue the patient to elongate the axis either through the lower body or through the upper body. For example, in a lower body driven roll led with the right lower extremity, place tubing on either the left distal lower extremity anchored higher on the body or on the right distal upper extremity to encourage the response of elongation.
Figure 7.

Intermediate position for rolling prone to supine, leading with right lower extremity, using manual contact to the pelvis for facilitation.
Dysfunctional Patterns of Rolling and Contributory Factors
Knowledge of typical functional movement patterns of the body enables the therapist to identify dysfunctional patterns of motion. As each of the four described rolling tasks are performed, the therapist should carefully observe and document the qualitative differences between upper and lower body initiated rolls and side to side differences. Outcomes that display less than optimal performance include: inability to complete the roll, use of inertia or swinging of the extremities to complete the roll, use of extremities not being tested during the roll, and pushing or bracing with the opposite lower or upper extremity in order to artificially supply stability during the attempt. Many contributory factors may play a role in a patient's ability or inability to roll in a smooth, coordinated, and controlled manner. These factors include: strength of the pelvis and scapula (proximal links) and the extremities, length/stiffness of important muscle groups, and insufficient coordination of all the moving parts of the system.4,9 The ideal is for the individual to be able to roll easily and symmetrically while adjusting to various demands.
Patients with many diagnoses may demonstrate difficulty with attempts to roll. Some examples of these diagnoses include: poor neuromuscular control and stability of the core muscles, low back pain of multiple origins, sacroiliac pain/dysfunction, and various upper and lower extremity mobility or stability problems. The following examples illustrate the power of rolling as an assessment strategy.
Case Example-Upper Extremity
Consider the pitcher has undergone a right rotator cuff repair and has progressed through the rehabilitation process, as prescribed by the therapist, regaining full active range of motion in all planes, manual muscle test scores for the muscles of the shoulder complex of 4+/5 or better, and functional abilities to perform all activities of daily living with 10 pounds at shoulder height without dysfunctional movement. He still complains of “fatigue and lack of endurance” with the initiation of a return to throwing program. When assessed using the rolling tasks, the patient was able to roll from supine to prone leading with each of the extremities, but was unable to roll from prone to supine when leading with the right upper extremity.
Case Example-Lower Extremity
Consider the recreational soccer player who has undergone a partial medial menisectomy on the left knee. The patient has progressed well throughout the rehabilitation process and has full active and passive range of motion, normal manual muscle test scores of the lower quarter, and knee flexion/extension isokinetic scores that demonstrate less than 10% difference in peak torque when compared bilaterally to the uninjured lower extremity.
The patient can perform a full, painfree functional squat and can jump and land without difficulty (single limb hop for a given distance is within 90% of uninvolved lower extremity). Functionally, this soccer player still has difficulty with performance of cutting and lateral movements. When assessed using the rolling tasks, the patient was able to perform all upper extremity initiated rolls without difficulty. Lower extremity initiated rolls by the right lower extremity were also achieved without difficulty. He was unable to roll from supine to prone to the right (initiating movement with the left lower extremity) and also was unable to roll prone to supine to the right (also initiating with the left lower extremity). The patient had difficulty crossing the midline of the body with the left lower extremity initiated rolling task.
Although impairments had been addressed and quantitative performance tests were essentially symmetrical to the uninvolved extremity, qualitative performance assessment of rolling revealed a deficiency in each of the two case examples. This assessment indicated the inability to effectively coordinate, time, and sequence the movements of the extremities and the trunk during a lower level developmental task. Normal impairment measures and quantitative functional measures do not necessarily imply normal function.
ROLLING AS INTERVENTION
Rolling has thus far been described as an assessment. After the assessment is complete, the therapist must draw conclusions about bilateral symmetry and rolling ability, as well as possible causes for less-than-optimal rolling. Multiple interventions exist that can assist the patient or client to enhance the ability to roll, and thereby enhance core stability, rotational function, and overall function of the upper and lower extremities. Many alternate exercise postures and modifications to the task of rolling exist, each attempting to begin to elicit core control of the scapula and pelvis or diminish the demands of the task.
The quadruped posture can be used to recruit and facilitate underutilized proximal musculature such as the scapular stabilizers and gluteal muscles (Figures 8 and 9). Another example that could be used for a patient who is unable to complete the roll is the use of assistance in the form of a rolled airex mat or foam roller behind the trunk or pelvis to place him or her in an easier starting position when rolling from supine to prone (Figure 10), referred to as assisted or facilitated rolling.
Figure 8.
Quadruped with tubing to facilitate scapular control/stability.
Figure 9.
Quadruped with tubing to facilitate core/scapular/pelvic stability.
Figure 10.
Assisted rolling supine to prone, left upper extremity led. Note the use of a half foam roll behind the trunk for assistance.
Recall the patient that underwent a rotator cuff repair who demonstrated the inability to roll from prone to supine leading with the involved upper extremity. For this patient, an exercise progression might include the following:
Quadruped position stabilization for the scapula (Figure 8)
Resisted rolling with manual contact on the scapula (Figure 6)
Axis elongation using manual contact or tubing applied to the uninvolved upper extremity
Early exercises encourage the use of the scapula in a facilitated, stabilized position, and then subsequent exercises progress to the recruitment of the scapular prime movers, which serve to facilitate coordinated upper extremity and trunk movement as well as to provide opportunities to cross the midline. Although the patient in this case had all of their impairments addressed (range of motion, manual muscle test, etc.), the qualitative assessment of the task of rolling revealed an alteration of timing and coordination between the involved upper extremity and the trunk. This examination of a lower level developmental task revealed another area for potential intervention. Rolling was an effective low-level functional intervention because of its requisite demands of timing and reflex stabilization between the extremities and trunk which serve to “reset” the timing and coordination necessary for higher level function, such as throwing.
Now return to the patient who underwent the partial medial menisectomy of the left knee and was unable to roll from supine to prone or prone to supine when leading with the involved lower extremity. This patient might use a similar exercise progression, including the following:
Bridging exercises for stabilization of the pelvis/gluteals, using a tubing loop for abduction resisitance
Quadruped stabilization of pelvis/gluteals, core, and scapula, using tubing (Figure 9)
Hip abduction with core stabilization might follow to address both proximal lower extremity strength and stability (through gluteus medius and minimus muscles) and core stability (Figure 11) or the side plank with abduction for same (Figure 12)
Proximal stabilization/manual contacts during rolling via pelvic resistance (Figure 7), (Note that this principle could also be applied to the supine to prone task by utilizing anterior pelvic contact.)
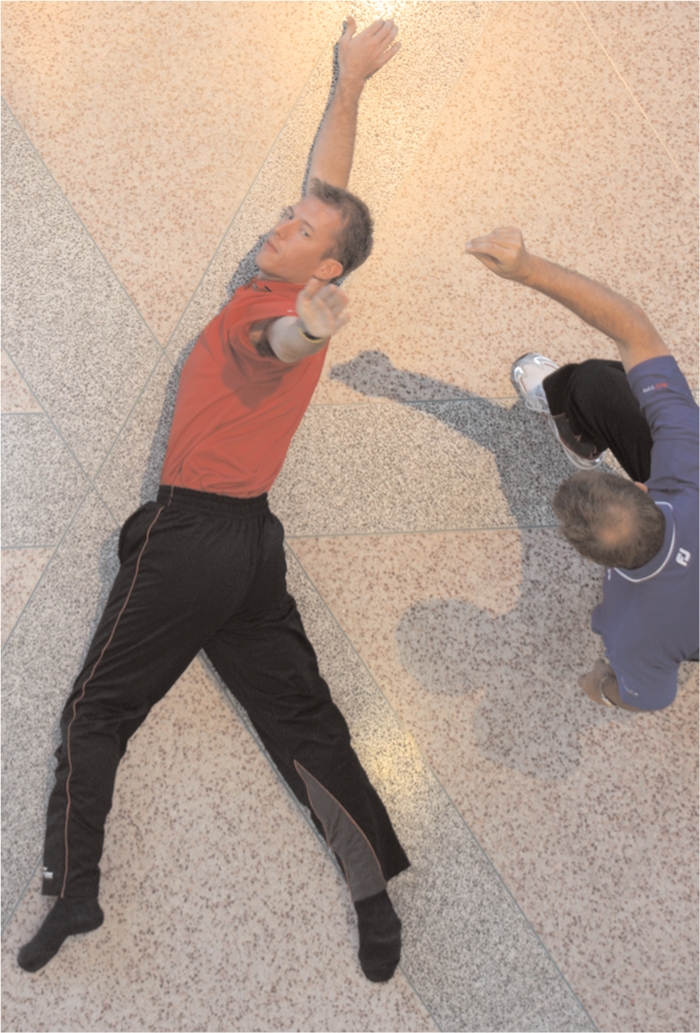
The rolling task itself, facilitated with tubing in the form of the Starfish 1 drill for supine to prone (Figures 13A & B) and the Starfish 2 drill (Figures 14A & B)
Figure 11.
Sidelying hip abduction with core resistance. Note that tube is anchored to bottom lower extremity and also anchored at top of door height. During the exercise the trunk is held stabilized in sidelying while upper extremities perform the lift pattern.
Figure 12.
Side plank with lower extremity abduction.
Figure 13A.

Start position for “Starfish 1” pattern, used for training of supine to prone rolling, leading with the lower extremity. Note tubing loops have been placed around both feet; with the length of the band around both upper extremities. To start, the lead hip is flexed, abducted, and slightly internally rotated while the knee is flexed. The rolling movement is initiated by extending, adducting, and externally rotating the hip while extending the knee. Note that the patient is concurrently elongating the opposite lower extremity (axis lower extremity) against the tubing.
Figure 13B.

Intermediate position “Starfish 1.” Patient will finish in the prone position with all four extremities extended and slightly abducted.
Figure 14A.
Start position for “Starfish 2” pattern, used for training of prone to supine rolling, leading with the lower extremity. Tubing placed as described previously, the lead leg then is flexed, abducted, and externally rotated. The rolling movement is initiated by extending, adducting, and internally rotating the hip, while extending the knee. Note that the patient is concurrently elongating the opposite lower extremity (axis lower extremity) against the tubing.
Figure 14B.

Intermediate position “Starfish 2” pattern. Patient will finish in the supine position with all four extremities slightly abducted.
Early exercises encourage the use of the pelvic and core muscles in a facilitated, stabilized position, and then progress to the recruitment of the movements of the hip/pelvis to facilitate coordinated lower extremity and trunk movement, as well as to provide opportunities to cross the midline. Again, although the patient in this case had all of their impairments addressed (range of motion, manual muscle test, isokinetic scores, etc.), the qualitative assessment of the task of rolling revealed an alteration of timing and coordination between the involved lower extremity and the trunk. This examination of a lower level developmental task revealed another area for potential intervention. Rolling was an effective low-level functional intervention because of its requisite demands of timing and reflex stabilization between the extremities and trunk. The task of rolling serves to “reset” the timing and coordination necessary for higher level function, such as lower extremity movements that cross the midline and require high proprioceptive acuity.
In the two case examples, rolling was being used for its impact on neuromuscular time and coordination of movement, as well as recruitment of important muscles of the proximal extremities and core. It is important that the patient be instructed to perform the tasks associated with rolling with precision and perfection. When attempting to determine dosage for the previously described exercises, it is important to dose below the threshold of the inappropriate motor pattern domination. If the patient has difficulty with more than one rolling pattern, begin with the component parts of the roll that are most dysfunctional. Select an exercise that is achievable for the patient (may be a lower developmental posture or assisted rolling exercise) and select the number of repetitions based upon the ability to perform the repititions with precision and accuracy. A simple pneumonic for this is “PMRS”, Position, Movement, Resistance, Speed. Begin the intervention by choosing the position in which the patient can successfully challenge muscles that are weak/dysfunctional in movements that address the dysfunction. This movement may be isolated (scapula, pelvis, or limb) or a functional movement such as rolling. It is entirely possible that resistance, the next element, could be minimal to none, but subsequent sessions may build upon it. Finally, the addition of speed to a carefully selected posture, movement, and resistance exercise can make the activity more difficult, noting that speed masks substitution and requires a base of strength to be effective as a training parameter.
For example, the patient with rotator cuff dysfunction described previously might be able to perform quadruped stabilization with scapular movement without any resistance 18 times before a form break. Start with that number of repetitions, and have the patient attempt to perform two or more sets. Progress the quadruped exercise by adding the resistance of tubing, again determining the number of repetitions that can be performed with precision. Next, progress to the roll itself, using an assisted or facilitated technique, yet again determining the number of repetitions that can be performed properly, without substitution or compensation, and dose accordingly. Eventually the assistance will not be needed and resistance (manual contacts or tubing) can be added to the roll. Finally, the speed at which the exercise is being performed can be altered to mimic more functional motion demands.
Learning the building blocks of a motor sequence and the control of the rolling movement is paramount to perfecting the task. The rolling task maximally challenges the core muscle stabilizers and extremities during a developmental, atypical movement. As motor learning occurs, the patient or client accomplishes the control and skilled use of mobility to accomplish the task of rolling. The authors of this article believe that rolling can facilitate enhanced use of the trunk, core musculature, and the extremities during a wide variety of functional tasks.
CONCLUSION
The human body is built on and relies upon symmetry. During static postures and dynamic functional tasks, length, strength, and stability/mobility must exhibit delicate integration or balance.8 Side-to-side and anterior-posterior balance are both important to healthy, normal function. Without symmetry, a state of asymmetry occurs which may eventually lead to injury, imbalance, and dysfunction. Normal functional activities are rhythmic and reversing, which both establishes and depends upon balance and interaction between stabilizers, agonists, and antagonists.5 Often, athletes become “stuck” in patterns of movement that do not promote symmetry and reversal, such as tasks that require rotation in one direction, including pitching, tennis, and golf. Determining alterations in symmetry or the inability to reverse a movement is the first step to successfully addressing dysfunction. Treatment must facilitate movement in both directions in order to enhance normal functional movement and provide adequate postural responses to motion.5 Improvement of motor ability depends on motor learning which can be enhanced by auditory, tactile, and visual stimuli.3–5 During intervention, specific developmental postures may be used to enhance the use of the head, neck, and trunk as important parts of the movement. The use of the skill of rolling as an assessment and intervention technique can serve as a possible method by which symmetry, reversal, and motor learning can be achieved.
REFERENCES
- 1.Cech DJ, Martin S. Functional Movement Development Across the Lifespan, 2nd Edition Philadelphia, PA: WB Saunders; 2002 [Google Scholar]
- 2.Piper MC, Darrah J. Motor Assessment of the Developing Infant. Philadelphia, PA: WB Saunders; 1994 [Google Scholar]
- 3.Adler SS, Beckers D, Buck M. PNF in Practice: An Illustrated Guide. New York, NY: Springer; 2007 [Google Scholar]
- 4.Voss DE, Ionta MK, Myers BJ. Proprioceptive Neuromuscular Facilitation. Patterns and Techniques. Philadelphia, PA: Harper & Row Publishers; 1985 [Google Scholar]
- 5.Hall CM, Thein-Brody LM. Proprioceptive neuromuscular facilitation, in: Therapeutic Exercise: Moving Toward Function, 2nd edition.Philadelphia, PA: Lippincott Williams & Wilkins; 2004 [Google Scholar]
- 6.Richter R, VanSant AF, Newton RA. Description of adult rolling movements and hypothesis of developmental sequences. Phys Ther. 1989;69:63–71 [DOI] [PubMed] [Google Scholar]
- 7.Voight ML, Hoogenboom BJ, Cook G. The chop and lift reconsidered: Integrating neuromuscular principles into orthopedic and sports rehabilitation. N Am J Sports Phys Ther. 2008;3:151–159 [PMC free article] [PubMed] [Google Scholar]
- 8.Sherrington, C. The Integrative Action of the Nervous System. New Haven, CT: Yale University Press; 1961 [Google Scholar]
- 9.Sullivan PE, Markos PD. Clinical Decision Making in Therapeutic Exercise. Norwalk, CT: Appleton & Lange; 1995 [Google Scholar]










