Abstract
Non-operative and operative complications are common following multiple ligament knee injuries. This article will describe common complications seen by the surgeon and physical therapist following this complex injury. Complications include fractures, infections, vascular and neurologic complications following injury and surgery, compartment syndrome, complex regional pain syndrome, deep venous thrombosis, loss of motion and persistent laxity issues. A brief description of these complications and methods for evaluation and treatment will be described.
Keywords: complications, knee dislocation, vascular, neurologic
INTRODUCTION
Multiple ligament knee injuries (MLKI) are usually the result of knee dislocations following either high energy motor vehicle accidents or low velocity sport injuries.1 Significant morbidity is associated with knee dislocation including multiple ligament disruption and neurovascular damage. The treatment of the MLKI can be very involved. Therefore, the possibility of complications is extremely high. Complication rates are much higher than with standard single-ligament knee injuries. In this article, complications are divided into non-operative and operative and are discussed separately.
NON-OPERATIVE COMPLICATIONS-OPEN DISLOCATIONS
Open dislocations of the knee represent approximately 20–30% of all dislocations. These injuries are serious and are due to high energy trauma, often accompanied by vascular and neurologic injury.2,3 Usually, significant soft tissue injury occurs that must be addressed before any reconstructive procedure is initiated. These other injuries are what ultimately determine the success of any reconstructive effort. Significant risk exists for infection and a higher incidence of above knee amputation in this group.4 Often, the definitive surgical procedure is delayed to allow for eradication of infection and soft tissue healing. Due to the severity of this injury functional expectations following salvage of the limb need to be guarded and realistic goals set.
Associated Fractures
Fracture dislocations are believed to occur in 10–20% of all knee dislocations.5 Most commonly, the fractures include avulsion fractures of the fibular head, tibial spine fractures, and Segund's fractures which is an avulsion fracture of the lateral tibial condyle. Although these are technically fractures, they represent ligament avulsions and are treated by repairing/reconstructing the appropriate ligament. However, tibial plateau fractures are more serious and can compromise the overall success of any surgical procedure. Moore6 classified five types of plateau fractures associated with dislocations. The higher the type, the more serious the fracture. Plateau fractures add an additional dimension to the surgical planning as stable fracture fixation must be achieved along with addressing the ligamentous instability. Due to the fact that plateau fractures involve the articular surface, a greater risk of developing post traumatic osteoarthritis exists and, therefore, the overall functional outcome, because of pain and stiffness, may be compromised.
Vascular Injury
Popliteal vessels have limited mobility and can be injured during knee dislocations. Vascular injury is associated with knee dislocation in 30% to 35% of cases (Figure 1 and 2).7–12 Popliteal vessels can be injured by stretching in anterior dislocations and by direct trauma during posterior dislocations. Injury can be limited to intimal flap (one in which the inner lining, the intima, of the blood vessel is torn while the remaining layers remain intact), or complete vessel rupture (Figure 3 and 4).13–17 The vascular status of a grossly unstable knee should be evaluated immediately by palpation of dorsalis pedis and posterior tibial pulses. Collateral circulation is inadequate to provide distal flow in case of injury to popliteal artery. Absence of pulse mandates an arteriogram to assess vascular integrity.
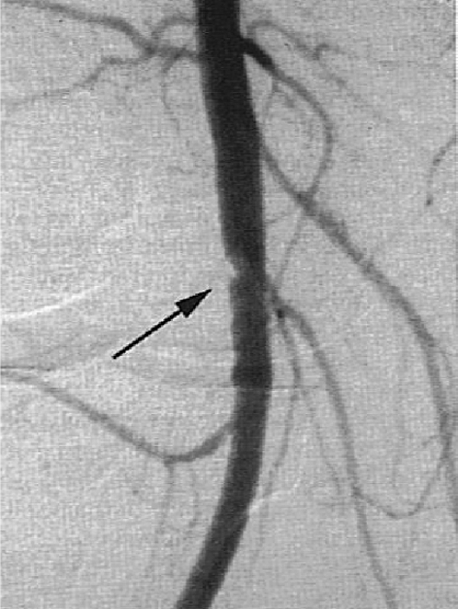
Figure 1.

Arteriogram demonstrating complete disruption of the popliteal artery at the knee joint, with minimal distal perfusion. (Reprinted with permission from Wascher DC: High-velocity knee dislocation with vascular injury: Treatment principles. Clin Sports Med. 19:470, 2000)
Figure 2.
Arteriogram demonstrating intimal flap tear of the popliteal artery. (Reprinted with permission from Wascher DC: High-velocity knee dislocation with vascular injury: Treatment principles. Clin Sports Med. 19:472, 2000)
Figure 3.

Posterior-anterior radiograph of a posterior knee dislocation.
Figure 4.

Medial-lateral radiograph of a posterior knee dislocation.
Neurologic Injuries
Tibial and, more commonly, peroneal nerves can be injured during a knee dislocation. Peroneal nerve injury is reported to occur in 14% to 35% of knee dislocations, especially posterolateral dislocations.3 Traction of the peroneal nerve is the most common mechanism of injury.18–20 The severity of the nerve injury can vary from neuroapraxia to complete disruption. Prognosis varies but is generally poor with no recovery in more that 50% of cases.19,20 Peroneal nerve injury clinically manifests as foot drop which may be treated with an ankle-foot orthoses (AFO). Ischemia, induced by vascular injury or compartment syndrome, could also cause neurologic injury.
OPERATIVE COMPLICATIONS
Operative complications of multiple ligamentous reconstruction includes morbidity associated with iatrogenic vascular and nerve injury, anesthesia, compartment syndrome, tourniquet and wound complications, deep venous thrombosis, and failure of the repair.
Iatrogenic Vascular Injury
Previous vascular repair could be compromised or disrupted by direct trauma during surgical reconstruction of the ligaments.21 Intimal flaps undiagnosed by angiography could also occlude during surgery and compromise the extremity circulation (Figure 5). Pre-operative, intra-operative, and post-operative vascular evaluation is important with or without vascular repair. Avoidance of using a tourniquet is recommended after vascular repair. If a tourniquet is used, application should be distant from the vascular repair and the time should be minimumized.21
Figure 5.
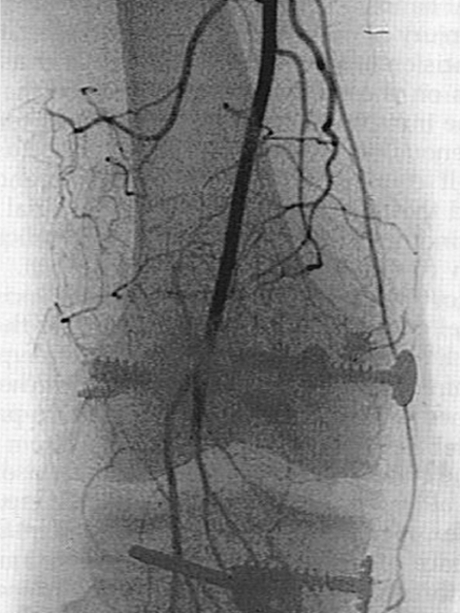
Arteriogram demonstrating vascular occlusion after multiple ligament knee reconstruction. (Reprinted with permission from Hegyes MS, Richardson MW, Miller MD. Knee dislocation: Complications of nonoperative and operative management. Clin Sports Med. 19:529, 2000)
Iatrogenic Nerve Injury
Nerve injury during multiple ligament reconstruction usually is incisional and involves sensory branches. The infrapatellar and sartorial branches of the saphenous nerve on the medial side of the knee are the most affected nerves.21 Hypersensitivity and dysthesias are the most common complaints. Complex regional pain syndrome discussed later in this article could also be caused by cutaneous nerve injury.22 The peroneal nerve, which lies close to the fibular head could be injured during lateral exposures.19
Compartment Syndrome
Compartment syndrome can occur after arthroscopic knee surgery due to extravasation of arthroscopic fluid.21 Patients with MLKI after dislocations have capsular and fascial defects. Extravasation is a leakage of arthroscopic fluid between fascial planes that can be a potential cause of compartment syndrome.20,23,24 Capsular sealing usually occurs in 10–14 days and delaying surgical reconstruction may decrease the risk of this complication.25 Compartment syndrome could also be induced by ischemia due to vascular injury or re-perfusion after vascular repair.
Tourniquet Complications
Tourniquet complications are believed to be time-dependent and related to duration of compression.21 Age of the patient, excessive pressure, local anatomy, and insufficient pressure are also other contributing factors.26 Patients with MLKI after knee dislocation may have non-occlusive vascular injury. Tourniquet induced stasis might lead to formation of an arterial thrombus in these patients which may cause to limb ischemia and subsequent amputation.21 Use of a properly functioning tourniquet, accurate application, limb exsanguination (the process by which blood is removed from the leg by elevation or use of a compressive device or elastic wrap before tourniquet application), checking the pressure level during surgery, and reducing tourniquet time are believed to decrease complications associated with tourniquet application.21
Wound Problems
Superficial or deep wound infections may happen after ligamentous knee surgery with an incidence of 0.30 to 12.5% in open reconstructions.23,27,28 Patient's age, general health, skin condition, steroid use, prolonged tourniquet time, and prior knee operation are all contributing factors.29,30 Prophylactic antibiotic therapy before and after knee reconstruction for 24 hours (or until drain removal) is recommended and is shown to decrease the risk of wound infections.21 Additionally, excessive traction can cause blistering during wound closure (Figure 6).
Figure 6.

Skin blisters from excessive traction during wound closure. (Reprinted with permission from Hegyes MK, Richardson MW, Miller MD. Knee dislocation: Complications of nonoperative and operative management. Clin Sports Med. 19:533, 2000)
Complex Regional Pain Syndrome
Complex regional pain syndrome, also known as reflex sympathetic dystrophy, can occur after knee surgery and is characterized by pain with the intensity out of proportion to the severity of injury, prolonged functional recovery, vasomotor imbalances, edema, and atrophy. Hypersensitivity to painful stimuli, atrophy, stiffness, hypervascularity, and osteopenia are the common clinical findings in the affected patients.21 The severe pain can lead to muscle inhibition and soft tissue contractures of the knee and cause slow progression and painful physical therapy. Early recognition is important to prevent frustrating complications. Steroids and nonsteroidal anti-inflammatory drugs, as well as sympathetic blocks, have been shown to have some benefit.21,31,32
Deep Vein Thrombosis
An unusual complication following any knee surgery or period of prolonged immobilization is a deep venous thrombosis (DVT).33 Conditions such as trauma, surgery, or prolonged immobilization may impair venous return, leading to endothelial injury and excessive clotting of blood in the lower extremity. Deep venous thrombosis can be classified as either proximal or distal depending on the site of formation either proximal or distal to the trifurcation of the popliteal vein. Because the proximal versions are larger than the distal, the proximal DVT are thought to be more likely to end up as a pulmonary embolism.34,35 A pulmonary embolism occurs when a dislodged fragment of the blood clot travels to the lungs where it can block one of the pulmonary arteries or one of its branches. This blockage in the lung is an obvious medical emergency as it can be life threatening.
Due to decreased hospital stays, undiagnosed or silent DVT and pulmonary embolisms may be seen by physical therapists. Physical therapists routinely see patients following outpatient surgical procedures such as reconstruction for MLKI's. Common signs and symptoms of a DVT include calf pain, swelling, discoloration of the affected area, and warmth to palpation of the surrounding skin. The major problem with diagnosing this potentially life threatening condition is that the same identical symptoms occur after most lower extremity surgical procedures. Additionally, it must be understood that some DVT produce minimal symptoms and can present completely “silent.”
One of the more common physical examination tests used by physical therapists to diagnosis a DVT is the Homans' sign. Homans' sign is tested by passively dorsiflexing the patient's foot with the knee fully extended. Pain in the calf indicates a positive sign for DVT.36 Tenderness can also be found with palpation of the posterior calf. Unfortunately, previous reports suggest that the Homans' sign has essentially no diagnostic value.37,38
Fortunately, clinical decision rules have been developed to assist in the diagnosis of DVT. A clinical decision rule is described as a way to quantify individual contributions of components of the medical history and physical examination to make a correct diagnosis.39 Wells and colleagues40–42 have used a series of studies to determine that patients can be placed in categories dependent on their clinical decision rule scores. Their clinical decision rule is based on nine medical history items and physical findings (Table 1). Patient's scores and their proposed probability of DVT are listed in Table 2.
Table 1.
Clinical Decision Rule Developed by Wells and Colleagues.41
| Clinical Finding | Score |
|---|---|
| Advanced cancer (within 6 months of diagnosis or palliative care). | 1 |
| Paralysis, paresis, or recent plaster immobilization of lower extremity. | 1 |
| Recently bedridden more than 3 days or major surgery with 4 weeks of application of clinical decision rule. | 1 |
| Localized tenderness along distribution of the deep venous system. | 1 |
| Entire lower-extremity swelling | 1 |
| Calf swelling by more than 3 cm compared with asymptomatic lower extremity. | 1 |
| Pitting edema (greater in the symptomatic lower extremity). | 1 |
| Collateral superficial veins (nonvaricose). | 1 |
| Alternative diagnosis as likely, or greater than that, of deep vein thrombosis. | −2 |
Table 2.
Probability of having DVT using Wells et al41 Clinical Prediction Rule.
| Score | Probability | Confidence Interval |
|---|---|---|
| 0 or < | 3% | 1.7–5.9% |
| 1–2 | 17% | 12–23% |
| 3 or > | 75% | 63–84% |
Loss of Motion
Loss of knee motion may occur after any injury to the knee and is the most common long-term complication following MLKI.18,43–47 Multiple reasons exist for knee stiffness following this injury. Soft tissues injury, hemarthrosis with secondary adhesions, excessive scarring due to immobilization, joint or muscle contractures, complex regional pain syndrome, quadriceps scarring, notch scarring, infection, delayed or rushed surgical procedures,21,48 excessive graft tension, mal-positioned graft,49–51 and graft choice all can cause limitations of motion.43,44,52–54 To combat motion loss several applications are typically applied to the patient post-surgery as described by Irrgang and Fitzgerald.55
Reconstruction of anterior cruciate ligament is more associated with loss of extension versus posterior cruciate ligament reconstruction which is associated more with lack of flexion. Medial collateral ligament reconstruction involves flexion and extension equally and has the highest rate of motion loss after surgery. Lateral collateral ligament repair is not believed to have a significant impact on postoperative range of motion.47 Intercondylar notch scarring and capsulitis are the most common causes of knee stiffness after ligament reconstruction. Intercondylar notch scarring is caused by scar formation in the notch which can block extension.47
To protect the healing of replaced ligaments, the patient is placed in a postoperative brace locked in full extension for the first 4–6 weeks.25 Emphasis is placed on gaining equal full terminal extension, except in cases of those with posterolateral corner reconstruction. With a posterolateral reconstruction emphasis of passive knee extension is to 0 degrees and not equal terminal extension bilaterally. Passive knee flexion is limited to less than 90 degrees during the first 6 weeks. Passive flexion is performed cautiously with a hand placement that will decrease the amount of posterior translation of the tibia (“drop-back”) during knee flexion range of motion (Figure 7). Active knee flexion via hamstring muscle contraction is avoided for 6 weeks to prevent posterior tibial translation which could be detrimental to the posterior cruciate reconstruction. Depending on ligament damage, a slight varus or valgus force may be applied during knee flexion and extension exercises to take additional stress off of the healing medial collateral or lateral collateral ligaments, respectively (Figures 8 and 9). If extension motion is lost, treatment is physical therapy and possible use of extension dropout cast to maintain extension.56
Figure 7.

Passive flexion done with hand placement to prevent posterior tibial drop-back.
Figure 8.

Passive knee flexion done with slight varus force to protect healing medial collateral ligament.
Figure 9.

Passive knee flexion done with slight valgus force to protect healing lateral collateral ligament.
Capsulitis results from inflammation in the periarticular tissue. Diffuse pain, tenderness, effusion, weakness of extensor mechanism, and flexion contracture are common problems which can result in a flexed knee during gait.21 Early recognition can prevent further loss of motion. Early treatment includes the use of nonsteroidal anti-inflammatory drugs with non aggressive physical therapy. Additionally, patellofemoral mobilization is performed for medial/lateral and superior/inferior glides to ensure adequate mobility for full functional return of the quadriceps mechanism (Figures 10 and 11). In most cases, the decision can be made by three months that surgical intervention is indicated.57–59 Surgical intervention usually includes lysis of adhesions and a lateral release to restore patellar motion.60 Physical therapy emphasizing improvement of extension is started after surgery.21 Severe cases might require arthrotomy, quadricepsplasty, and salvage procedures such as patellectomy and total knee replacement.58
Figure 10.
Passive patellar superior glide to ensure terminal knee extension motion.
Figure 11.
Passive patellar inferior glide to ensure full knee flexion motion.
Persistent Laxity
Knee instability is not as common as stiffness after multiple ligamentous reconstruction and can be caused by failure to recognize associated injuries, non-isometric ligament reconstruction, and graft failures.21,25 Posterior sag is the most common form of persistent laxity which can happen after posterior cruciate ligament reconstruction due to failure to address posteromedial or posterolateral injuries, improper graft tensioning or placement, graft weakness, and early open chained hamstring muscles exercise.25,61–66 Failure to recognize associated ligament injuries is believed to be the most common cause of suboptimal outcomes after combined anterior and posterior cruciate ligament surgery. Complete history and physical exam including magnetic resonance imaging (MRI), examination under anesthesia, and arthroscopy for diagnostic purpose in selected cases can help identify the correct pathology.25 Post-operative physical therapy can affect the outcome of posterior cruciate ligament reconstruction leading to posterior sag and persistent laxity.62–65 Open chain hamstring muscles exercise and weight bearing in flexion in the early post-operative period can increase forces in the posterior cruciate ligament and cause laxity with posterior sag.
Miscellaneous Complications
Medial femoral condyle osteonecrosis has been reported as one of the complications of the posterior cruciate ligament repair. The cause is believed to be increased pressure causing vascular insufficiency in the bone. Medial knee pain with tenderness on the medial femoral condyle are the most common signs and symptoms.25,67 Anterior knee pain can be seen after posterior cruciate ligament reconstructions with posterior sag due to increase patellofemoral forces that lead to early patellofemoral osteoarthritis.44,48 Pain in the graft harvest site, synovitis, and prominent hardware are other causes of anterior knee pain after ligament reconstruction.25
Summary
Significant morbidity is frequently associated with MLKI before and after operative intervention. Early diagnosis of these complications can play a significant role in improving outcome.
REFERENCES
- 1.Kennedy JC. Complete dislocation of the knee joint. J Bone Joint Surg. 1963;45A:889–904 [PubMed] [Google Scholar]
- 2.Meyers M, Harvey JP. Traumatic dislocation of the knee joint. J Bone Joint Surg. 1971;53A:16–29 [PubMed] [Google Scholar]
- 3.Shields I, Mital M, Cave EF. Complete dislocation of the knee. Experience at the Massachusetts General Hospital. J Trauma. 1969;9:192–215 [PubMed] [Google Scholar]
- 4.Wright DG, Covey DC, Born CT, Sadasivan KK. Open dislocation of the knee. J Orthop Trauma. 1995;9:135–140 [DOI] [PubMed] [Google Scholar]
- 5.Cole BJ, Harner CD. The multiple ligament injured knee. Clin Sports Med. 1999;8: 241–262 [DOI] [PubMed] [Google Scholar]
- 6.Moore TM. Fracture-dislocation of the knee. Clin Orthop. 1981;56:128–140 [PubMed] [Google Scholar]
- 7.Fabian TC, Tukelson ML, Connelly TL, et al. Injury to the popliteal artery. Am J Surg. 1982;143:225–228 [DOI] [PubMed] [Google Scholar]
- 8.Frassica FJ, Sim FH, Shaeheli JW, et al. Dislocation of the knee. Orthop Clin North Am. 1991;263:200–205 [PubMed] [Google Scholar]
- 9.Harrell DJ, Spain DA, Bergamini TM, et al. Blunt popliteal trauma: A challenging injury. Am Surg. 1997;63:228–231 [PubMed] [Google Scholar]
- 10.Jones RE, Smith EC, Bone GE. Vascular and orthopedic complication of knee dislocation. Surg Gynecol Obst. 1979;149:554–558 [PubMed] [Google Scholar]
- 11.O'Donnell TF, Brewster DC, Darling RC, et al. Arterial injuries associated with fractures and/or dislocations of the knee. J Trauma. 1977;17:775–783 [DOI] [PubMed] [Google Scholar]
- 12.Ottolenghi CE. Vascular and nerve complications in injuries of the knee joint. Joint Recon Surg Trauma. 1974;14:114. [PubMed] [Google Scholar]
- 13.Eger M, Huler T, Hirsh M. Popliteal artery occlusion associated with dislocation of the knee joint. Br J Surg. 1970; 57: 315– 325 [DOI] [PubMed] [Google Scholar]
- 14.Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg. 1977;59A:236–239 [PubMed] [Google Scholar]
- 15.Merrill KD. Knee dislocation with vascular injuries. Orthop Clin North Am. 1994;25:707–713 [PubMed] [Google Scholar]
- 16.Roth JH, Bray RC. Popliteal artery injury during anterior cruciate ligament reconstruction: Brief report. J Bone Joint Surg. 1988;70B:840. [DOI] [PubMed] [Google Scholar]
- 17.Varnell RM, Coldwell DM, Sangeorzan BJ, et al. Arterial injury complicating knee disruption. Am Surg. 1989; 55: 669– 704 [PubMed] [Google Scholar]
- 18.Sisto DJ, Warren RF. Complete knee dislocation: A follow up study of operative treatment. Orthop Clin North Am. 1985;198:94–101 [PubMed] [Google Scholar]
- 19.White J. The results of traction injuries to the common peroneal nerve. J Bone Joint Surg. 1968;50B:346. [PubMed] [Google Scholar]
- 20.Wood MB. Peroneal nerve repair: Surgical results. Clin Orthop. 1991; 267: 206– 210 [PubMed] [Google Scholar]
- 21.Hegyes MS, Richardson MW, Miller MD. Knee dislocation: Complications of operative and non operative management. Clin Sports Med. 2000;19:519–543 [DOI] [PubMed] [Google Scholar]
- 22.Poehling GG, Pollock FE, Jr, Korman LA. Reflex sympathetic dystrophy of the knee after sensory nerve injury. Arthroscopy. 1988;4:31–35 [DOI] [PubMed] [Google Scholar]
- 23.Graf B, Uhr F. Complications of intra-articular anterior cruciate ligament reconstruction. Clin Sports Med. 1988;7:835–842 [PubMed] [Google Scholar]
- 24.Noyes FR, Spievack ES. Extraarticular fluid dissection in tissues during arthroscopy: A report of clinical cases and a study of intraarticular thigh pressure in cadavers. Am J Sports Med. 1982;12:1006–1011 [DOI] [PubMed] [Google Scholar]
- 25.Fanelli GC. Complications of multiple ligametous knee injuries. In: Scheneck RC: Multiple Ligamentous Knee Injury in the Athlete. Rosemont, IL: American Academy of Orthopedic Surgeons, 2002 [Google Scholar]
- 26.Bruner JM. Safety factors in the use of pneumatic tourniquets for hemostasis in surgery of the hand. J Bone Joint Surg. 1951;33A:221–229 [PubMed] [Google Scholar]
- 27.Almekinders LC, Logan TC. Results following treatment of traumatic dislocations of the knee joint. Orthop Clin North Am. 1992;284:203–207 [PubMed] [Google Scholar]
- 28.Hughston J. Complications of anterior cruciate ligament surgery. Orthop Clin North Am. 1985;16:237–245 [PubMed] [Google Scholar]
- 29.Silski JM. Evaluation and treatment of dislocation of the knee. Orthopedics. 1992;10:1–7 [Google Scholar]
- 30.Wascher DC, Becker JR, Dexter JG, et al. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Am J Sports Med. 1999;27:186–189 [DOI] [PubMed] [Google Scholar]
- 31.Graur JD, Kabo JM, Dorey FJ, et al. The effects of dexamethasone on periarticular swelling and joint stiffness following fracture in a rabbit hind limb model. Clin Orthop. 1989;242:277–284 [PubMed] [Google Scholar]
- 32.Lindenfield TN, Bach JR, Wojtys EM. Reflex sympathetic dystrophy and pain dysfunction syndrome in lower extremity. J Bone J Surg. 1996;78A:1936–1944 [Google Scholar]
- 33.Geerts WH, Heit JA, Claget GP, et al. Sixth ACCP concensus conference on antithroboitic therapy: Prevention of venous throboembolism. Chest. 2001;119Suppl 1:132s– 175s [DOI] [PubMed] [Google Scholar]
- 34.Prandoni P, Mannucci PM. Deep vein thrombosis of the lower limbs: Diagnosis and management. Baillieres Best Pract Clin Haematol. 1999;12:533–554 [DOI] [PubMed] [Google Scholar]
- 35.Kearon C. Natural history of venous thromboembolism. Circulation. 2003;107Suppl 1:I22– I30 [DOI] [PubMed] [Google Scholar]
- 36.Magee D. Orthopedic Physical Assessment, 5th edition Saunders: St. Louis, 2008 [Google Scholar]
- 37.O'Donnell TF, Abbott WM, Athanasoulis CA, et al. Diagnosis of deep venous thrombosis in the outpatient by venography. Surg Gynecol Obst. 1980;150:69–74 [PubMed] [Google Scholar]
- 38.Haeger K. Problems of acute deep venous thrombosis, I: The interpretation of signs and symptoms. Angiology. 1969;20:219–223 [DOI] [PubMed] [Google Scholar]
- 39.McGinn TG, Guyatt GH, Wyer PC, et al. User's guides to the medical literature XXII: How to use articles about clinical decision rules. JAMA. 2000;384:79–84 [DOI] [PubMed] [Google Scholar]
- 40.Wells PS, Hirsh J, Andersen DR, et al. Accuracy of clinical assessment of deep-vein thrombosis. Lancet. 1995;345:1326–1330 [DOI] [PubMed] [Google Scholar]
- 41.Wells PS, Andersen DR, Bormanis J, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997;350:1795–1798 [DOI] [PubMed] [Google Scholar]
- 42.Wells PS, Hirsh J, Andersen DR, et al. A simple clinical model for the diagnosis of deep vein thrombosis combined with impedance plethsmography: Potential for an improvement in the diagnostic process. J Intern Med. 1998;243:15–23 [DOI] [PubMed] [Google Scholar]
- 43.Noyes FR, Barber-Westin SD. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Use of early protected postoperative motion to decrease arthrofibrosis. Am J Sports Med. 1997;25:769–768 [DOI] [PubMed] [Google Scholar]
- 44.Shapiro MS, Freedman EL. Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation. Am J Sports Med. 1995;23:580–587 [DOI] [PubMed] [Google Scholar]
- 45.DeLee JC. Complications of arthroscopy and arthroscopic surgery. Results of a national survey. Arthroscopy. 1985;1:214–220 [PubMed] [Google Scholar]
- 46.Fu FH, Irrgang JJ, Sawhney R, et al. Loss of knee motion following anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:557–562 [Google Scholar]
- 47.Harner CD, Irrgang JJ, Dearwater PJ, et al. Loss of motion after anterior cruciate ligament reconstruction. Am J Sports Med. 1992;20:499–506 [DOI] [PubMed] [Google Scholar]
- 48.Tzurbakis M, Diamantopoulos A, Zenakis T, Georgoulis A. Surgical treatment of multiple knee ligament injuries in 44 patients: 2-8 years follow-up results. Knee Surg Sports Traumatol Arthrosc. 2006;14:739–749 [DOI] [PubMed] [Google Scholar]
- 49.Fu FH, Harner CD, Johnson DL, et al. Biomechanics of knee ligaments: Basic concepts and clinical application. Inst Course Lect. 1994;43:137–148 [PubMed] [Google Scholar]
- 50.Millet PJ, Williams RJ, III, Wickiewicz TL. Open debridement and soft tissue release as a salvage procedure for the severely arthrofibrotic knee. Am J Sports Med. 1999;27:552–561 [DOI] [PubMed] [Google Scholar]
- 51.Millet PJ, Wickiewicz TL, Warren RF. Motion loss after ligament injuries to the knee. Part I: Causes. Am J Sports Med. 2001;29:664–675 [DOI] [PubMed] [Google Scholar]
- 52.Fanelli GC, Edson CJ. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthroscopy. 2002;18:703–714 [DOI] [PubMed] [Google Scholar]
- 53.Harner CD, Waltrip RL, Bennett CH, et al. Surgical management of knee dislocations. J Bone Joint Surg. 2004;86A:262–273 [DOI] [PubMed] [Google Scholar]
- 54.Mariani PP, Margheritini F, Camillieri G. One-stage arthroscopically assisted anterior and posterior cruciate ligament reconstruction. Arthroscopy. 2001;17:700–707 [DOI] [PubMed] [Google Scholar]
- 55.Irrgang JJ, Fitzgerald GK. Rehabilitation of the multipleligament-injured knee. Clin Sports Med. 2000;19:545–571 [DOI] [PubMed] [Google Scholar]
- 56.Sprague NF, O'Conner RL, Fox JM. Arthroscopic treatment of postoperative knee arthrofibrosis. Clin Orthop. 1982;166:165–172 [PubMed] [Google Scholar]
- 57.Thomas P, Rud B, Jensen U. Stability and motion after traumatic dislocation of the knee. Acta Orthop Scand. 1984;55:278–283 [DOI] [PubMed] [Google Scholar]
- 58.Thompson T. Quadricepsplasty to improve knee faction. J Bone Joint Surg. Am 1944;26A:359–365 [Google Scholar]
- 59.Shelbourne KD, Wilckens JH, Mollabashy A, et al. Arthrofibrosis in the acute anterior cruciate reconstruction: The effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19:332–336 [DOI] [PubMed] [Google Scholar]
- 60.Kolowich PA, Paulos LE, Rosenberg TD, et al. Lateral release of the patella: Indications and contraindications. Am J Sports Med. 1990;18:359–365 [DOI] [PubMed] [Google Scholar]
- 61.Noyes FR, Barber-Westin SD. Posterior cruciate ligament allograft reconstruction with and without a ligament augmentation device. Arthroscopy. 1994;10:371–382 [DOI] [PubMed] [Google Scholar]
- 62.Ogata, McCarthy JA. Measurements of length and tension patterns during reconstruction of the posterior cruciate ligament. Am J Sports Med. 1992;20:351–355 [DOI] [PubMed] [Google Scholar]
- 63.Thomann YR, Gaechter A. Dorsal approach for reconstruction of the posterior cruciate ligament. Arch Orthop Trauma Surg. 1994;113:142–148 [DOI] [PubMed] [Google Scholar]
- 64.Ogata K. Posterior cruciate ligament reconstruction: A comparative study of two different methods. Bull Hosp Jt Dis Orthop Inst. 1991;51:186–198 [PubMed] [Google Scholar]
- 65.Paulos LE, Wnorowski DC, Beck CL. Rehabilitation following knee surgery: Recommendations. Sports Med. 1991;11:257–275 [DOI] [PubMed] [Google Scholar]
- 66.Burns WC, II, Dranganich LF, Pyevich M, Reider B. The effect of femoral tunnel position and graft tensioning technique on posterior laxity of the posterior cruciate ligament-reconstructed knee. Am J Sports Med. 1995;23:424–430 [DOI] [PubMed] [Google Scholar]
- 67.Athanasian EA, Wickiewicz TL, Warren RF. Osteonecrosis of the femoral medial condyle after arthroscopic reconstruction of a cruciate ligament: Report of two cases. J Bone Joint Surg. 1995;77A:1418–1422 [DOI] [PubMed] [Google Scholar]




