Abstract
Background
Thoracic Outlet Syndrome (TOS) involves compression of the brachial plexus, subclavius artery and vein. Many studies discuss efficacy of surgery and few discuss conservative treatment. It is unknown what specific forms of conservative treatment are best.
Objective
Describe conservative management for TOS using unique exercises.
Case Description
A collegiate football player reported numbness/tingling down his right arm after a right brachial plexus stretch injury. Seven months later, he was diagnosed with recurrent cervical traction neuropraxia. Two months later, he reported bilateral symptoms and was diagnosed with functional TOS. The athlete began shoulder strengthening (deltoid, middle trapezius, rhomboids, pectoralis major, latissimus dorsi, biceps, upper trapezius and rotator cuff) and stretching (pectoralis, scalene and upper trapezius) which failed to resolve his symptoms after four weeks. Surgical resection of bilateral first ribs and quitting football was recommended by four physicians. Unique therapeutic exercises developed by the Postural Restoration Institute™ were used to optimize respiration/posture via muscle activation and inhibition. After six weeks, the athlete was asymptomatic and returned to football but still experienced paresthesia with contact. Additional exercises were prescribed and remaining symptoms were abolished.
Outcomes
The Northwick Park Neck Pain Questionnaire was 55.5% at initial and 0% at four weeks and discharge.
Discussion
Athlete did not demonstrate relief of symptoms from shoulder stretching and strengthening. Intervention designed to optimize respiration/posture by repositioning the pelvis/trunk via specific muscle inhibition and activation resulted in abolishing the athlete's symptoms. Management that aims to optimize respiration via muscle inhibition, activation, and repositioning warrants further research.
Keywords: thoracic outlet syndrome, postural restoration, respiration
INTRODUCTION
Thoracic outlet syndrome (TOS), also known as neurovascular compression syndrome, consists of a group of distinct disorders that affect the nerves or vascular structures between the base of the neck and axilla.1,2 Specifically, these disorders result from positional compression of the subclavian artery or vein, and the brachial plexus nerves in a variety of locations including the cervical spine (from cervical rib), scalene interval, infraclavicular space or under the pectoralis minor tendon.3 The brachial plexus is divided into an upper plexus (median nerve distribution) and a lower plexus (ulnar nerve distribution).4 Upper plexus compression was initially described by Swank and Simeone4 with symptoms secondary to C5, C6, and C7 nerve root compression. Sensory changes will primarily occur in the first three fingers, and associated muscle weakness or pain in the anterior chest, triceps, deltoids, and parascapular muscles, as well as down the outer forearm to the extensor muscles.4 Lower plexus irritation involves C8 and T1 nerve root compression. Sensory changes primarily occur in the fourth and fifth fingers, with muscle weakness or pain from the rhomboid and the scapular muscles to the posterior axilla, down the ulnar distribution of the forearm, involving the elbow, wrist flex-ors, and the intrinsic muscles of the hand.4
Thoracic outlet syndrome disorders are complex, poorly defined, and a diagnosis of exclusion that can cover a wide range of ailments each producing various signs and symptoms arising from the upper extremity and the chest, neck, and head.2,5,6 An accurate diagnosis of TOS requires a thorough history and physical examination. Several tests exist that may be used to assist in diagnosing TOS, including nerve conduction velocity (NCV), electromyography (EMG), radiographs, computed tomography (CT) scan, and magnetic resonance imaging (MRI).4 Authors have attempted to study the thoracic outlet region by CT scan or MRI. One of the limitations is that the compromise of the neurovascular bundle is often positional and intermittent.2 In neurogenic TOS, electrophysiological testing is often entirely normal. EMG can sometimes detect neurogenic C8/T1 signs.2
Thoracic outlet syndrome can be a result of postural alterations, hypertrophic muscles, muscle imbalances, an elevated first rib, presence of a cervical rib, and macrotrauma such as automobile accidents.5 These syndromes have been categorized into anatomical and functional TOS.5 Anatomical TOS includes congenital anomalies or traumatic osseous and soft tissue injury. Functional TOS includes postural adaptations as a result of work or sport participation, respiratory changes, and psychological conditions.
The literature suggests that a variety of methods have been traditionally used to manage TOS.2,5,7 Conservative interventions focus on pain control,7,8 edema control, verbal posture education and ergonomics,7,9–14 relaxation,15 stretching, strengthening, and nerve gliding exercises.7,16,17 Additional interventions include moist heat,7,18,19 massage,20 acupuncture,20 cervical traction, manual joint mobilization,21 first rib mobilization,15,19 braces,22 and aerobic exercises.9 Exercises to manage TOS may focus on stretching the levator scapulae, lower trapezius, scalenes, and pectoralis muscles,2,7,19,21 and strengthening the cervical extensors, scapular adductors, and shoulder retractor muscles.2,7,19,21 Additionally, cervical traction, isometric exercises (cervical spine and shoulder girdle), and manual joint mobilization (cervical-thoracic spine, sternoclavicular joint, acromioclavicular joint and costothoracic joint) has been described in the literature.21
Any of the described methods have been advocated to alter posture in some way.2,5,7 Authors of a recent literature review for TOS conclude that although conservative treatment may reduce symptoms and improve function, it is not known if this approach is significantly better than no treatment or placebo.5 The most commonly recommended interventions are strengthening and stretching of the shoulder girdle musculature.2,7,19,21 However, little agreement exists on which muscles need strengthening and which ones need lengthening.5 These types of exercises do not detail how they address functional TOS as a result of respiratory alterations and they do not aim to inhibit muscle.1,5,19
Postural Restoration is a holistic posture based approach to patient management that considers the influence of dys-functional respiration on posture and utilizes therapeutic exercises that activate or inhibit specific muscles and manual trunk techniques as needed in order to achieve optimal respiration and posture.23 Postural Restoration also recognizes patterns of postural asymmetries (similar to Kendall's24 right handed pattern) that are believed to be present in most people to varying degrees. Clinicians who use Postural Restoration, therefore, often target intervention to correct the asymmetrical pattern.23,25 This pattern is consistent with the pre-existent vertebral rotation in “normal” individuals.26 The postural restoration methodology has been used to manage patients with sciatica and low back pain,27 asthma,28 anterior knee pain,29,30 and trochanteric bursitis.31 This approach has appeared to be successful in managing athletes with iliotibial band syndrome,32 and patients with chronic pain33 and knee pain,34 however, the evidence for these three conditions remains anecdotal. To date, no case studies describing the use of Postural Restoration for a patient with TOS have been published. The purpose of this case is to describe management of a collegiate football player with bilateral functional TOS who was first managed with traditional therapeutic exercises and then with unique Postural Restoration therapeutic exercises to address his faulty posture and suboptimal respiration.
CASE DESCRIPTION
The athlete was a 22-year-old male collegiate football player (tight end). Social history included living with three other football players in an apartment with parents living an hour away. Other than his current condition, his general health including physical, psychological, and social function was excellent. Athlete denied use of alcohol, tobacco, or any drugs. He had an unremarkable medical and family history. The chief complaint for this football player included sustaining a right brachial plexus injury during the fall football season. Approximately seven months later, the athlete suffered multiple brachial plexus injuries to his right neck during spring football practice. Cervical spine radiographs were taken and he was seen by the team orthopedic surgeon. Radiographs revealed mild-moderate posterior osteophyte formation at C6- C7 greater than C5- C6 with elevation of the ribs. The physician diagnosed the athlete with cervical traction neurapraxia and prescribed Ibuprofen and Vicodin.
Due to the athlete's signs and symptoms progressively becoming worsened, he altered his posture to favor the involved side. This compensation in his posture potentially led to the left side becoming involved. He then began developing radicular pain down his left arm and into his hand. Now his signs and symptoms consisted of bilateral numbness, tingling, and weakness into his hands (median nerve distribution), achy pain in shoulders, and a shooting sensation down both arms, pain at Erb's point,7 tenderness to palpation over anterior chest and neck muscles, and tenderness and pain between his right scapula and vertebral column at the level of T4. These findings were consistent with someone who has sustained an upper plexus compression injury.35
Postural observation revealed bilateral: hypertrophic/over-developed latissimus dorsi, pectoralis, upper trapezius and bicep muscles, anterior rib flares (ribs are in a position of external rotation/elevation which is a combined position of chest expansion with pump handle and bucket handle motions),36 increased lumbar lordosis (over-active paraspinal muscles), left pelvic forward rotation, forward head posture, and over-active neck musculature. He reported that he was unable to sleep on either side and had to sleep prone with his face buried in his hands. The athlete had several positive tests including Adson's,37 Allen's, Military Brace and Roos.3,37–39
Two months later he was sent for a cervical spine MRI, a bilateral brachial plexus MRI, a nerve conduction velocity test, and an EMG. The cervical spine MRI was normal. The bilateral brachial plexus MRI revealed muscular hypertrophy in the neck and shoulders. All other structures appeared normal. The nerve conduction velocity test and EMG studies revealed ulnar nerve compression at the elbow on the right. The test results were negative on the left. It was interesting to note that the athlete did not have any neurological symptoms in the ulnar distribution of his hand. An orthopaedic surgeon diagnosed him with bilateral functional TOS. The physician recommended that he should discontinue playing football. Multiple physicians advised him to consider having surgery for resection of both first ribs as a last resort. The athlete decided to take a conservative approach to see if he could benefit from non-surgical management. He was managed by three different clinicians over the course of care and seen daily in the athletic training room. See Table 1 for dosage of interventions.
Table 1.
Interventions Prescribed for Football Player with Bilateral Thoracic Outlet Syndrome.
| Clinician | Intervention | Dosage |
|---|---|---|
| One | Moist heat to cervical spine and tops of shoulders (sitting) | 15 minutes Twice daily |
| Stretching bilateral scalenes, upper trapezius, and pectoralis major muscles | 3 repetitions 30 second hold time Twice daily |
|
| Verbal posture education | Once at initial session | |
| Exercises to strengthen bilateral rotator cuff, deltoids, pectoralis major, latissimus dorsi, biceps, and upper trapezius muscles | 15 repetitions 3 sets Twice daily |
|
| Two | Exercises to activate lower trapezius, serratus anterior, triceps, hamstrings, and abdominal muscles | 15 repetitions 2 sets Twice daily |
| Exercises to inhibit bilateral upper trapezius, pectoralis major, biceps, and paraspinal muscles | 15 repetitions 2 sets Twice daily |
|
| Exercises to reposition head and inhibit anterior neck | 5 repetitions 5 breaths (hold time ∼ 45 secs) Twice daily |
|
| Manual therapy of the trunk (ribs, sternum, clavicle) | 5 breaths for each technique Twice daily |
|
| Three | Exercises to activate lower trapezius, middle trapezius, rhomboids, serratus anterior, triceps, hamstrings, abdominals, and quadriceps muscles | 5 repetitions 4-5 breaths - hold time Twice daily |
| Exercises to inhibit paraspinal, upper trapezius, biceps, and pectoralis major muscles | 5 repetitions 4-5 breaths - hold time Twice daily |
|
| Exercise to stretch pectoralis major and latissimus dorsi muscles | 5 repetitions 20-30 seconds - hold time Twice daily |
Intervention – Clinician 1
The first clinician focused on traditional recommended interventions, primarily guided by information on a web-site for TOS including stretching and strengthening exercises.19 Specific interventions (done twice a day, seven days a week) consisted of: moist heat for fifteen minutes (over the neck and both shoulders in sitting to prepare for stretching), self stretching exercises (three repetitions x 30 seconds) for bilateral neck, shoulder, and chest muscles (scalenes, upper trapezius, pectoralis major muscles), verbal postural education (to keep head and shoulders back, and chin and chest up) and shoulder strengthening using tubing for the rotator cuff (internal and external rotation muscles), deltoid, pectoralis major, latissimus dorsi, supraspinatus, biceps, and upper trapezius muscles. All stretches were performed three times for 30 seconds each, the exercises were done in three sets of fifteen each, and all treatment was done twice a day everyday for four weeks. With this type of conservative treatment the athlete did not see much improvement and continued to progressively get worse after each lifting and conditioning session. After a month of conservative treatment, the athlete began to contemplate having surgery and ending his football career. Because the athlete was not making progress, clinician one asked another clinician to take over his case.
Intervention – Clinician 2
During weeks 5–11, this new clinician changed the focus of treatment by addressing the athlete's specific impairments of faulty posture via activation and inhibition of specific muscles to change position of bones and soft tissue rather than through verbal education alone. Faulty posture noted via visual observation included: over-developed latissimus dorsi, pectoralis, biceps, and upper trapezius muscles, over-active anterior neck muscles, increased lumbar lordosis (anterior pelvic tilt with left forward rotation), elevated ribs, downwardly rotated scapula, and forward head posture. Exercises and manual therapy techniques developed by the Postural Restoration Institute™40 were utilized to optimize posture of the trunk/scapula and pelvis via activation, inhibition, and lengthening of specific muscles.
The initial exercises were prescribed in order to restore a normal pelvic and rib cage position (from left pelvic anterior tilt/forward rotation and elevated, externally rotated ribs toward neutral) by doing a 90/90 hip shift with hemibridge and balloon (Figure 1). The exercise activated left hamstring muscles which facilitate left hip extension (posterior pelvic tilt). Forced exhalation into the balloon should activate transversus thoracis (triangularis sterni), internal and external inter-costals, and abdominal oblique muscles which facilitate depression/internal rotation of the ribs and inhibition of paraspinal muscles (lumbar flexion). Additionally, via the back pressure of the balloon, opening of the right apical chest wall is facilitated upon inhalation without using neck or paraspinal muscles. Depression of the ribs was thought to allow for a more optimal rest position of the scapula and, thereby, an optimal infraclavicular space to minimize the opportunity for compromise of the subclavius artery, vein, and brachial plexus nerves. This exercise was done twice daily with two sets of 15 repetitions.
Figure 1.
90/90 hip shift exercise
The second exercise was also designed to address the athlete's faulty postural position. A sternal positional Swiss ball release was prescribed to reposition the head over the shoulder girdles and inhibit the anterior neck muscles, to decrease forward head posture and lengthen the bilateral pectoralis major muscles. This was done twice daily for five repetitions and held for five breaths (Figure 2). Manual techniques consisted of four techniques: left anterior interior chain (L AIC), superior T4, subclavius stretch (right and left), and infraclavicular pump with opposition.23,28,41 These techniques were done to assist with the postural correction goals for repositioning of the pelvis and trunk including soft tissue and bones. These were done for five breaths, each twice daily.
Figure 2.
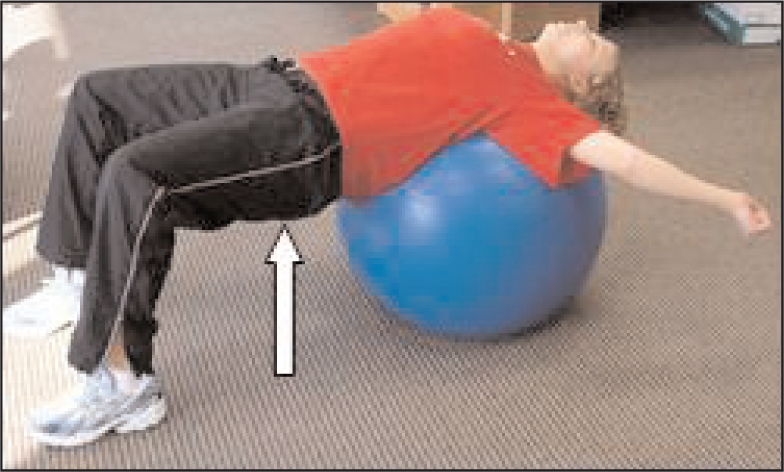
Sternal postitional swiss ball stretch
After six weeks of Postural Restoration techniques, the athlete was completely asymptomatic, and he was cleared to return to football. Upon returning to football, the athlete realized that all of his symptoms would come back once he made contact. During the entire football season, the athlete continued doing his Postural Restoration exercises. He did not practice during the week and played on Saturdays. Although he was much improved, his body did not remain symptom-free in a contact situation when he played football, so additional intervention seemed warranted.
Intervention – Clinician 3
After the season, the athlete made an out-of-state trip to see the physical therapist who developed the Postural Restoration techniques to discuss further recommendations. Postural observation revealed bilateral over-developed upper trapezius, pectoralis, biceps, and latissimus muscles, and under-developed right lower trapezius and bilateral triceps muscles (right>left), with anterior rib flares (left > right), bilateral abnormal scapular resting position (abduction, retraction, elevation and downward rotation) (Figure 3), and increased lumbar lordosis. Horizontal shoulder abduction was measured in supine at 15 degrees bilaterally. Hand held spirometry revealed an average of 5300cc upon forced exhalation. The therapist noted that this value was 1000cc over the reported norm for his age and sex and, therefore, interpreted the results to indicate hyperinflation.42,43 When the therapist applied manual pressure over the athlete's left ribs for depression and had him exhale again in to the spirometer, his numbers decreased.
Figure 3.

The therapist prescribed additional exercises to further progress the athlete's existing program in order to achieve optimal respiration and postural position of his pelvis/trunk and scapula that would carryover during football. These exercises allowed him to practice and play everyday. Key goals for the exercises were to train the athlete to be able to keep his ribs down during breathing and, at the same time, open his apical chest wall without using his neck or paraspinal muscles to inhale, and get bilateral scapulae to depress/upwardly rotate and protract. In order to achieve scapular protraction, the exercises targeted bringing his ribs back on the scapula (rather than the scapula forward on the ribs) and knees forward (to help keep ribs down and spine flexed). Eight exercises were prescribed by the physical therapist including 1. seated resisted serratus punch with left hamstring muscles, 2. standing resisted bilateral serratus press through, 3. standing serratus squat, 4. paraspinals release with left hamstrings, 5. two point stance on the left and right sides, 6. all four belly lift reach, 7. long sitting press downs and 8. lattisumus dorsi hang with low trap activation (Figures 4–11). This high number of exercises was prescribed in a single visit because the patient traveled by airplane to the out-of-state appointment.
Figure 4.

Seated resisted serratus punch with left hamstrings
Figure 11.

Lat hang with low trap
These exercises focused on neuromuscular re-education to alter or reposition the pelvis, ribs, and scapula to prevent compression of the brachial plexus nerves. After the athlete performed several repetitions of exercise one, the therapist rechecked his breathing (by visual observation of the athlete in supine), and noted that his upper trapezius muscle tone had noticeably decreased and he seemed to be breathing only with his diaphragm. The athlete was aware of his altered breathing and he noted that he was almost short of breath when not compensating with accessory respiratory muscles. The therapist then rechecked his horizontal shoulder abduction and it was 45 degrees, bilaterally. The therapist interpreted this increase in passive range of motion to be reflective of a decrease in tone/activity of the pectoralis and biceps musculature. A squat position was added to the second exercise to help train the quadriceps muscles since the therapist perceived the athlete using his paraspinal muscles more than his quadriceps muscles to run and push forward. After exercise number three, postural observation of the shoulder girdles revealed normal bilateral scapular rest position. This resting scapular portion was interpreted as the athlete having his ribs down (relatively depressed/internally rotated position) compared to his initial position of rib flares (anterior rib elevation/external rotation). This positioning allowed the athlete's scapula to rest on the ribs and no longer required the scapula to be held up by upper trapezius muscles.
The athlete was instructed to work on the first three exercises until five repetitions of each could be performed easily before progressing to the exercises in Figures 7–11. With the exercise in Figure 7, it was noted that the athlete's right upper extremity was weaker than the left. The exercise required lifting his right leg up to force his right upper extremity to work harder. The athlete was encouraged to achieve balance and work on the exercise until it was as easy to do lifting his right leg as it was lifting his left leg. The exercise in Figure 8 was designed to teach the athlete to learn how to move his thorax on his scapulas. The exercises were instructed to be done on both the right and left sides but with different breathing instructions during certain phases of movement for each side to facilitate more air flow into the right chest wall rather than the left.
Figure 7.
Paraspinals release with left hamstrings
Figure 8.

Two-point stance exercise
After several repetitions of each exercise were performed, the hand-held spirometer was used again and his values dropped to 4300cc. This was the reported norm for a 22-year-old male.43 The therapist attributed the drop in air exhaled into the spirometer as a result of taking away his compensatory strategies of using upper trapezius and paraspinal muscles and putting his ribs and diaphragm in a better position so the diaphragm could be better used as the primary muscle of respiration. When the ribs are elevated and externally rotated, the diaphragm was more linear/flat and less surface area of the diaphragm was available for a dome or zone of apposition (ZOA).44 The ZOA (area of the diaphragm from the most cephalad portion of the dome to the inferior attachments on the sternum and ribs) is important for optimal respiration and when it is decreased, the diaphragm functions more as a postural stabilizing muscle rather than as a primary muscle of respiration.45,46 The diaphragm is also important for exercise tolerance and decreasing shortness of breath.47 At the end of the session, the therapist perceived that the athlete had a good prognosis and would be able to play football without eliciting his symptoms when he made contact. He was additionally instructed to do his exercises before going to sleep (to avoid a dry mouth, tense neck, and upper extremity numbness) and to do them immediately before any weight lifting and to avoid any upper trapezius or latissimus muscle strengthening. A comparison of the muscles targeted for activation, lengthening, and inhibition for the traditional versus the Postural Restoration phases of rehabilitation for this athlete are presented in Tables 2–4. These charts highlight what the clinician's intended goals were as it related to activating, lengthening, and inhibiting specific muscles during the rehabilitation of the athlete.
Table 2.
Comparison of muscles that were targeted with exercise prescription in the two phases of rehabilitation for the athlete with thoracic outlet syndrome.
| Muscles Activated | Traditional Exercises | Postural Restoration Exercises |
|---|---|---|
| Serratus Anterior | No | Yes |
| Lower Trapezius | No | Yes |
| Triceps | No | Yes |
| Middle Trapezius | Yes | Yes |
| Rhomboids | Yes | Yes |
| Hamstrings | No | Yes |
| Abdominals | No | Yes |
| Triangularis Sterni | No | Yes |
| Intercostals | No | Yes |
| Pectorals | Yes | No |
| Deltoids | Yes | No |
| Latissimus Dorsi | Yes | No |
| Rotator Cuff | Yes | No |
| Biceps | Yes | No |
Table 4.
Comparison of muscle stretching in the two phases of rehabilitation for the football player with bilateral thoracic outlet syndrome.
| Muscles Lengthened | Traditional Exercises | Postural Restoration Exercises |
|---|---|---|
| Upper Trapezius/Levator Scapulae | Yes | No |
| Pectoralis | Yes | Yes |
| Neck Extensors | Yes | No |
| Neck Rotators | Yes | No |
| Latissimus Dorsi | No | Yes |
| Scalenes | Yes | No |
| Subclavius | No | Yes |
Table 3.
Comparison of muscle inhibition that were targeted with exercise prescription in the two phases of rehabilitation for the athlete with thoracic outlet syndrome.
| Muscle Inhibition | Traditional Exercises | Postural Restoration Exercises |
|---|---|---|
| Upper Trapezius | No | Yes |
| Pectoralis | No | Yes |
| Biceps Brachii | No | Yes |
| Paraspinals | No | Yes |
| Anterior Neck | No | Yes |
OUTCOME
The Northwick Park Neck Pain Questionnaire (NPNPQ)48 was used for the initial examination, after his initial course of traditional conservative intervention (four weeks), and after his second course of conservative intervention (10 weeks). This questionnaire was developed at Northwick Park Hospital in Middlesex England in order to measure neck pain and the consequent patient disability. The parameters consist of nine areas: 1. neck pain intensity, 2. neck pain and sleeping, 3. pins and needles or numbness in the arms at night, 4. duration of symptoms, 5. carrying, 6. reading and watching television, 7. working and housework, 8. social activities, and 9. driving. Each category has a scoring of 0-4 with (0) being no pain and (4) being the worst pain. The minimum score is 0 and a maximum score is 36. The NPNPQ percentage = (neck pain score) / 36 × 100%. The percentage range is from 0 to 100%, where the higher the percentage the greater the disability. The results of the initial NPNPQ were 55.5%. His NPNPQ was redone at four weeks and did not change, remaining at 55.5%. At 10 weeks, his NPNPQ dropped to 0% representing a 100% improvement in function. The minimal clinically meaningful difference is 5% on the NPNPQ.49
DISCUSSION
Thoracic outlet syndrome is often difficult to diagnose and manage.1 Traditional management has focused on upper body musculature to improve posture via stretching and strengthening of shoulder girdle muscles even though different perspectives exist on which muscles need to be stretched versus which muscles need to be strengthened. Several conservative management strategies have been studied and seem to be effective at reducing symptoms and facilitating return to work in the majority of subjects; however it is not known what type of conservative treatment is best. Types of treatment which have been described in the literature include upper trapezius muscle activation (shoulder elevation) followed by relaxation;50 a strapping device for shoulder elevation and shoulder girdle exercises;22 stretching for upper trapezius and levator scapulae muscles; chin retraction and strengthening of lower scapular stabilizers; aerobic conditioning;9 active mobilization of the cervical spine; stretching of the upper trapezius, pectoralis minor, and scalenes muscles; strengthening of the scapular stabilizers;15 shoulder girdle massage; strengthening of shoulder adduction (pectoralis major and latisimus muscles); shoulder extension (posterior deltoid and triceps muscles); cervical spine isometrics; and manual traction.5 None of these types of interventions focus on muscle inhibition or specifically correcting respiratory alterations, as was used with this patient.
In this case, two different conservative approaches were used by the treating clinicians to manage the athlete. During the first approach, the clinician prescribed traditional shoulder girdle stretching and strengthening exercises, however the athlete did not show improvement after this course of treatment. For the second approach, the clinicians included non-manual exercises and manual techniques developed by the Postural Restoration Institute™40 to optimize breathing and posture of the pelvis, ribs, and scapula via activation and inhibition of specific muscles.
The nine Postural Restoration Institute (PRI) exercises prescribed for this athlete with bilateral TOS, would potentially be beneficial to other patients/athletes with faulty posture, faulty respiration, and over-developed musculature. The 90/90 hip shift exercise (Figure 1) could be used for any patient with an anterior pelvic tilt, elevated ribs, over-active paraspinal muscles, weak abdominal muscles, over-active neck muscles, or long hamstring muscles. Because the exercise puts the pelvis into a posterior pelvic tilt and the ribs into depression, the technique discourages the paraspinal and neck muscles from firing (inhibits) and assists with shortening hamstrings via hamstring muscle contraction. In a published case study, this exercise was used to manage a female with sciatica and low back pain.51
The sternal postitional swiss ball stretch (Figure 2) could be used for any patient with weak gluteus maximus muscles, over-active or short pectoralis musculature, or acquired forward head posture. This exercise is designed to activate the gluteal muscles in a sagittal plane against gravity, to lengthen the pectoral muscles, and to some extent the latisimus muscles, and bring the head out of a forward head position. The seated resisted serratus punch with left hamstrings (Figure 4) could be used to manage any patient/athlete with elevated ribs, over-developed paraspinal muscles, excessive lumbar lordosis, and weak serratus anterior muscles. The exercise is designed to help depress the ribs, discourage activation of the paraspinal muscles via lumbar flexion, and may be especially helpful to individuals who run since the exercise mimics a closed kinetic chain position in one lower extremity while the contralateral upper extremity is in a forward swing position.
The standing resisted bilateral serratus press through (Figure 5) may be beneficial for patients/athletes who need lumbar flexion training (to inhibit over-active paraspinal muscles), scapular depression (to oppose over-active upper trapezius muscles and accessory respiratory breathing), and inhibition of over-active/developed pectoral muscles. With the exercise done in the squat position it would also be beneficial for strengthening quadriceps muscles. The standing serratus squat (Figure 6) could be used for any patient needing activation of serratus anterior and low trapezius muscles for proper scapular position and dynamics without allowing excessive lumbar lordosis and over-activation of latissimus muscles to occur. This exercise is designed to train an individual to breathe with the ribs down, pelvis back, spine flexed, latisimus muscles elongated, and quadriceps muscles firing. The paraspinals release with left hamstrings (Figure 7) may be beneficial for any patient/athlete who needs to strengthen one or both upper extremities (lower trapezius, rhomboids, and triceps muscles) in a closed kinetic chain position with the lumbar spine in a flexed position (rather than an anteriorly tilted position). This particular position would discourage over-activation of the patient/athlete's paraspinal muscles and encourage ribs to depress and abdominal muscles to work in a shortened (rather than lengthened) position.
Figure 5.

Standing resisted bilateral serratus press through
Figure 6.

Standing serratus squat
The two-point stance exercise (Figure 8) could be prescribed for any higher level patient/client needing to activate/strengthen core musculature, lower trapezius, rhomboids and serratus anterior muscles and needing to lengthen pectoral muscles and expand their apical chest wall. The all four belly lift reach (Figure 9) may be beneficial for a higher level patient/athlete to progress from the seated resisted serratus punch (Figure 4) because the exercise is similar (when they reach toward the floor) but in a four point/quadruped position. The exercise likely requires more abdominal muscle activation, because the position requires the abdominal muscles to work/activate against gravity. Lastly, the lat hang with low trap (Figure 11) could be prescribed for any patient/client who has the strength and shoulder range of motion to do the exercise with proper form that may benefit from latissimus lengthening and lower trapezius muscle activation. The exercise is thought to be beneficial for patients who need to lengthen their latissimus muscles while maintaining a posterior tilted pelvic position (rather than a pelvic anteriorly tilted and excessively lumbar lordotic position). The exercise is designed to activate/strengthen the lower trapezius muscles too, which would oppose over-active/developed upper trapezius muscles.
Figure 9.

All four belly lift reach
Figure 10.

For the football player in this case study, rather than clinicians two and three focusing on stretching the upper trapezius, levator scapulae, scalene, and pectoralis muscles, the focus was on inhibiting these muscles. Rather than focusing on strengthening (rotator cuff, biceps, deltoids, pectoralis, latissimus, and upper trapezius muscles) the focus was on identifying the muscles the patient was using to breathe with (upper trapezius, paraspinal, and anterior neck muscles), and the concomitant position the body was in (rib elevation/external rotation, lumbar lordosis, scapular elevation, retraction, and downward rotation) and what muscles were over-developed (upper trapezius, pectoral, and latissimus muscles). Specific exercise prescription was then recommended by the therapist to alter the athlete's postural position and muscle activation patterns to optimize respiration.
Although mobilization of the first rib has been discussed in the literature, altering the position of multiple ribs via activation of hamstring muscles has not been presented in the literature. Activation of the hamstring muscles puts the pelvis in a posterior pelvic tilt helping the abdominal muscles obtain an optimal position/length to facilitate spinal flexion and to inhibit the paraspinal muscles to prevent lumbar extension (lordosis). Serratus anterior muscle activation to reposition the ribs posteriorly rather than to move the scapula forward (protraction) has also not been discussed in the literature. Triceps muscle activation to inhibit biceps muscle and reposition the scapula in a relatively abducted position is another novel concept. The Postural Restoration techniques resulted in remarkable outcomes: the athlete was able to avoid surgery, return to full symptom-free football even during contact, and improved his function by 100% based on the NPNPQ.
Further research is needed to help guide clinicians toward effective interventions for patients with TOS. Case studies may be a good choice to establish efficacy of conservative management for TOS because of the variation in impairments that patients have that may contribute to TOS. A case study may be written in the near future by the author after having success treating three other patients who also have had TOS but other impairments as well. Further research is also warranted to explore the benefits of therapeutic exercises to inhibit muscles rather than to stretch them and to optimize respiration via specific muscle repositioning techniques.
CONCLUSION
Postural Restoration management of a collegiate football player with bilateral TOS using exercises (developed by the PRI) designed to optimize respiration/posture by repositioning the pelvis/trunk via specific muscle inhibition and activation resulted in abolishing the athlete's symptoms and allowed him to participate in football without further complications. Management that aims to optimize respiration via muscle inhibition, activation, and repositioning warrants further research.
ACKNOWLEDGEMENTS
We would like to thank the Postural Restoration Institute™ for their creative development of the specific therapeutic exercises that were prescribed for the patient in this case report.
REFERENCES
- 1.National Institute of Neurological Disorders and Stroke (NINDS) Thoracic Outlet Syndrome Information Page, Available at: http://www.ninds.nih.gov/disorders/thoracic/thoaracic.htm Accessed March 16, 2007
- 2.Dubuisson A. The Thoracic Outlet Syndrome, Available at: http://www.medschool.lsuhsc.edu/neurosurgery/nervecenter/tos.html Accessed December 5, 2008
- 3.Dutton M. Orthopaedic Examination, Evaluation, and Intervention. York, PA: The McGraw-Hill Companies; 2004:1083 [Google Scholar]
- 4.Urschel HC, Kourlis H. Thoracic outlet syndrome: A 50-year experience at Baylor University Medical Center. Proc (Bayl Univ Med Cent) 2007;20:125–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vanti C, Natalini L, Romeo A, et al. Conservative treatment of thoracic outlet syndrome. Eura Medicophys. 2007;43:55–70 [PubMed] [Google Scholar]
- 6.Toso C, Robert J, Berney T, et al. Thoracic outlet syndrome: Influence of personal history and surgical technique on long-term results. Eur J Cardiothorac Surg. 1999;16:44–47 [DOI] [PubMed] [Google Scholar]
- 7.Crosby CA, Wehbe MA. Conservative treatment for thoracic outlet syndrome. Hand Clin. 2004;20:43–49 [DOI] [PubMed] [Google Scholar]
- 8.Walsh M. Therapist management of thoracic outlet syndrome. J Hand Ther. 1994;7:131–43 [DOI] [PubMed] [Google Scholar]
- 9.Novak CB, Collins ED, Mackinnon SE. Outcome following conservative management of thoracic outlet syndrome. J Hand Surg. 1995;20:542–548 [DOI] [PubMed] [Google Scholar]
- 10.Leffert R. Thoracic outlet syndrome. In: Tubiana R, ed. The Hand. Philadelphia: W.B. Saunders Co.; 1991 [Google Scholar]
- 11.Leffert R. Thoracic outlet syndrome. J Am Acad Orthop Surg. 1994;2:3173–3225 [DOI] [PubMed] [Google Scholar]
- 12.Novak C. Conservative management of thoracic outlet syndrome. Semin Thorac Cardiovasc Surg. 1996;8:201–207 [PubMed] [Google Scholar]
- 13.Walsh M. Therapist's management of brachial plexopathies. In: Hunter JM, M E, Callahan AD, ed. Rehabilitation of the Hand and Upper Extremity. Philadelphia: Mosby, Inc.; 2002 [Google Scholar]
- 14.Tyson RR, Kaplan GF. Modern concepts of diagnosis and treatment of the thoracic outlet syndrome. Orthop Clin N Am. 1975;6:507–518 [PubMed] [Google Scholar]
- 15.Lindgren K. Conservative treatment of thoracic outlet syndrome: A 2-year follow-up. Arch Phys Med Rehabil. 1997;78:373–378 [DOI] [PubMed] [Google Scholar]
- 16.Walsh M. Rational and indications for the use of nerve mobilization and nerve gliding as a treatment approach. In: Hunter JM, M E, Callahan AD. ed. Rehabilitation of the Hand and Upper Extremity. Philadelphia: Mosby, Inc.; 2002 [Google Scholar]
- 17.Butler D. Adverse mechanical tension in the nervous system: A model for assessment and treatment. Aust J Physiotherapy. 1989;35:227–238 [DOI] [PubMed] [Google Scholar]
- 18.Peet RM, Henriksen JD, Anderson TD, et al. Thoracic outlet syndrome: Evaluation of a therapeutic exercie program. Proc Mayo Clin. 1956;131:281–287 [PubMed] [Google Scholar]
- 19.Plone Foundation Physical Therapy Corner: Thoracic Outlet Syndrome. Available at: http://www.nismat.org/ptcor/thoracicoutlet Accessed March 16, 2007
- 20.Peng J. 16 cases of scalenus syndrome treated by massage and acupoint-injection. J Tradit Chin Med. 1999;19A:218–220 [PubMed] [Google Scholar]
- 21.Boissonot P, Roubieu A. Criticisms of the Peet gymnastics. Proposal of a new exercise program for the patient. Rev Med Interne. 1999;20:500–5005 [DOI] [PubMed] [Google Scholar]
- 22.Natatsuchi Y, Saitoh S, Hosaka M. Conservative treatment of thoracic outlet syndrome using an orthosis. J Hand Surg (Br). 1995;20:34–39 [DOI] [PubMed] [Google Scholar]
- 23.Boyle K. Ethnography of the Postural Restoration Subculture: A Posture Based Approach to Patient/Client Management. Fort Lauderdale, FL: Nova Southeastern University; 2006 [Google Scholar]
- 24.Kendall FP, McCreary EK, Provance PG, et al. Muscles Testing and Function with Posture and Pain. Philadelphia: Lippincott Williams and Wilkins; 2005 [Google Scholar]
- 25.Boyle K. Postural Restoration. Musculoskeletal Physiotherapy Australia InTouch Magazine, 2007;13–15 [Google Scholar]
- 26.Kouwenhoven JM, Vinchen KL, Bartels LW, et al. Analysis of preexistent vertebral rotation in the normal spine. Spine. 2006;31:1467–1472 [DOI] [PubMed] [Google Scholar]
- 27.Boyle K. Conservative Management for patients with low back pain: A case series. J Ortho Sports Phys Ther. 2008;38:A67 [Google Scholar]
- 28.Coughlin KJ, Hruska R, Masek J. Cough-variant asthma: Responsive to integrative management and Postural Restoration. Explore (NY). 2005;1:377–379 [DOI] [PubMed] [Google Scholar]
- 29.Timm K. Randomized controlled trial of Protonics on patellar pain, position, and function. Med Sci Sports Exerc. 1998;30:665–670 [DOI] [PubMed] [Google Scholar]
- 30.Schneider F, Labs K, Wagoner S. Chronic patellofemoral pain syndrome: Alternatives for cases of therapy resistance. Knee Surg, Sports Traumatol, Arthrocs. 2001;9:290–295 [DOI] [PubMed] [Google Scholar]
- 31.Boyle K, Jansa S, Lauseng C, et al. Management of a woman diagnosed with trochanteric bursitis with the use of a Protonics® neuromuscular system. Journal on the Section of Women's Health. 2003;27:12–17 [Google Scholar]
- 32.Roers M. Hometown HeroesMeritCare Today Spotlight. Bemidji. 2006 [Google Scholar]
- 33.Helseth C. Therapeutic Technology Rids Patients of Chronic Pain. RiverView Health. Crookston, 2005 [Google Scholar]
- 34.Cleary J. Thanks to therapist, fencer wins silver. Str-Gazette. Elmira, 2005 [Google Scholar]
- 35.Swank RI, Simeone FA. The scalenus anticus syndrome. Arch Neurol Psychiatry. 1944;51:432–450 [Google Scholar]
- 36.Oatis C. Structure and Function of the Bones and Joints of the Thoracic Spine. In: Oatis C, ed. Kinesiology The Mechanics and Pathomechanics of Human Movement. Philadelphia: Lippincott Williams and Wilkins; 2004 [Google Scholar]
- 37.Magee D. Shoulder. Orthopedic Physical Assessment. St Louis, MO: Saunders Elsevier; 2008 [Google Scholar]
- 38.Konin JG, Wiksten DL, Isear JA, et al. Special Tests for Orthopedic Examination. Thorofare, NJ: SLACK Incorporated; 2006 [Google Scholar]
- 39.Starkey C, Ryan J. Evaluation of Orthopedic and Athletic Injuries. Philadelphia, PA: FA Davis Company; 2002 [Google Scholar]
- 40.Ebmeier J, Hruska R. Postural Restoration Institute Web site, Available at: http://www.posturalrestoration.com Accessed March 17, 2008
- 41.Hruska R. Postural Respiration: An Integrated Approach to Treatment of Patterned Thoraco-Abdominal Pathomechanics. Chandler, AZ: Postural Restoration Institute; 2007 [Google Scholar]
- 42.Sadowsky H. Pulmonary Diagnostic Tests and Procedures. Essentials of Cardiopulmonary Physical Therapy. Philadelphia, PA: Saunders Elsevier; 2001 [Google Scholar]
- 43.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–187 [DOI] [PubMed] [Google Scholar]
- 44.DeTroyer A, Estenne M. Respiratory Anatomy of the Respiratory Muscles. Clin Chest Med. 1988;9:175–193 [PubMed] [Google Scholar]
- 45.Hodges PW, Butler JE, McKenzie DK, et al. Contraction of the human diaphragm during rapid postural adjustments. J Physiol. 1997;505:539–548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hodges PW, Heijnen I, Gandevia SC. Postural activity of the diaphragm is reduced in humans when respiratory demand increases. J Physiol. 2001;537:999–1008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lando Y, Boiselle PM, Shade D, et al. Effect of lung volume reduction surgery of diaphragm length in severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;159:796–805 [DOI] [PubMed] [Google Scholar]
- 48.Leak AM, Cooper J, Dyer S, et al. The Northwick Park Neck Pain Questionnaire, devised to measure neck pain and disability. British J Rheumatol. 1994;33:469–474 [DOI] [PubMed] [Google Scholar]
- 49.Moffett JK, Jackson DA, Richmond S, et al. Randomised trial of a brief physiotherapy intervention compared with usual physiotherapy for neck pain patients: Outcomes and patients' preference. BMJ. 2004;330:7482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kenny RA, Traynor GM, Withington D, et al. Thoracic outlet syndrome: A useful exercise treatment option. Am J Surg. 1993;165:282–283 [DOI] [PubMed] [Google Scholar]
- 51.Boyle K, Demske J. Management of a female with chronic sciatica and low back pain: A case report. Physiother Theory Pract. 2009;25:44. [DOI] [PubMed] [Google Scholar]




