Abstract
Swimmer's shoulder is a musculoskeletal condition that results in symptoms in the area of the anterior lateral aspect of the shoulder, sometimes confined to the subacromial region. The onset of symptoms may be associated with impaired posture, glenohumeral joint mobility, neuromuscular control, or muscle performance. Additionally, training errors such as overuse, misuse, or abuse may also contribute to this condition. In extreme cases, patients with swimmer's shoulder may have soft tissue pathology of the rotator cuff, long head of the biceps, or glenoid labrum. Physical therapists involved in the treatment of competitive swimmers should focus on prevention and early treatment, addressing the impairments associated with this condition, and analyzing training methods and stroke mechanics. The purpose of this clinical commentary is to provide an overview of the biomechanics of swimming, the etiology of the clinical entity referred to as swimmer's shoulder, and strategies for injury prevention and treatment.
Keywords: Swimmer's shoulder, injury prevention, rotator cuff
INTRODUCTION
The shoulder complex is designed to achieve the greatest range of motion (ROM) with the most degrees of freedom of any joint system in the body.1 The excessive mobility of the shoulder at the glenohumeral and scapulothoracic joints is balanced by the stability of the acromioclavicular (AC) and sternoclavicular joints. At the glenohumeral joint, a complex ligamentous system contributes to primary stability and an elaborate musculotendinous system serves as secondary stabilizers. This support mechanism allows the shoulder to withstand large external forces, while providing enough mobility for the upper extremity to accomplish complex movement patterns.
Perhaps the greatest illustration of the balance between shoulder mobility and stability occurs during sports that require overhead motions. Many overhead sports such as throwing, racket sports, and volleyball require two or three overhead movement patterns. Conversely, swimming requires several overhead movement patterns, involving continuous humeral circumduction in clockwise and counterclockwise directions.2,3 A competitive swimmer usually exceeds 4000 strokes for one shoulder in a single workout, making this sport a common source of shoulder pathology. Shoulder pain is the most common musculoskeletal complaint in swimming4-6 with reports of incidence of disabling shoulder pain in competitive swimmers ranging from 27% to 87%.4-12 The purpose of this clinical commentary is to provide an overview of the biomechanics of swimming, the etiology of the clinical entity referred to as swimmer's shoulder, and strategies for injury prevention and treatment.
SWIMMING BIOMECHANICS
Swimming requires several different shoulder motions, most being performed during circumduction in clockwise and counter-clockwise directions with varying degrees of internal and external rotation and scapular protraction and retraction.2 Swimming is comprised of four different strokes of varying distances, including freestyle (sometimes referred to as the crawl), butterfly, backstroke, and breastroke. Most strokes are divided into two primary phases referred to as the pull-through and recovery. The pull-through is where propulsion is achieved and is further divided into different phases consisting of the hand entry, the catch, mid-pull, and finish or end pull-through. This section will provide an overview of swimming mechanics for each stroke related to the shoulder. For more detailed analysis of swimming biomechanics, the reader is referred to other sources.13
Freestyle requires a combined motion of scapular retraction and elevation, with humeral abduction and external rotation during the recovery.2 During the pull-through phase, the scapula is protracted while the humerus is adducted, extended, and internally rotated. Stroke power is achieved through the shoulder adductors, extenders, and internal rotators with the serratus anterior and latissumus dorsi being the key propulsion muscles for swimmers.2 Because the trunk is rotated away from the side that is beginning to pull, the shoulder avoids a true impingement position of forward flexion with internal rotation and horizontal adduction.
The butterfly has a similar motion at the shoulder as freestyle, but the stresses are different because both arms are moved through the same motion simultaneously rather than alternating. For this reason, no trunk rotation occurs so the demand of the medial scapular stabilizers and retractors during recovery is greater with butterfly than freestyle.2 In addition, the humeral head moves into an impingement position of elevation, horizontal adduction, and internal rotation at hand entry. Much of the propulsion during the butterfly comes from the hips and trunk so inefficiency of these muscle groups can lead to increased stress on the shoulders.
The motion at the shoulder during the backstroke is opposite to the freestyle stroke with the shoulder in retraction, horizontal abduction, and external rotation at hand entry and the beginning of pull-through. This position places increased stress on the anterior capsule. The arm position during the recovery is different than freestyle because the elbow is extended (rather than flexed). Due to trunk rotation, the swimmer is rarely flat on the back during the movement, spending more time on the side.
Movement at the shoulder during breaststroke can vary, with more motion occurring below the surface of the water than any other stroke. Like the butterfly, the arms are moved simultaneously through a motion that starts in full flexion with internal rotation. However, the elbows remain flexed during the pull-through until the humerus is fully adducted and brought into horizontal adduction with forearms touching each other. Unlike the other strokes, the hands never move below the hips so the tensile forces on the rotator cuff that occurs during the other strokes at the end of pull-thorough does not occur during breaststroke.2
ETIOLOGY OF SWIMMER'S SHOULDER
Most musculoskeletal conditions can be divided into macrotrauma and microtrauma based on the onset.14 A condition with sudden onset that occurs due to one specific incident usually is referred to as macrotrauma.14 Macrotrauma results from external forces and patients usually present with tissue pathology that causes associated impairments such as loss of motion, strength, and proprioception. Swimmer's shoulder is a condition with a gradual onset due to repetitive activity and can be classified as microtrauma. Unlike macrotrauma, the etiology of microtrauma is multifactorial and may be due to intrinsic factors or extrinsic factors.
Intrinsic Factors
Swimmer's shoulder usually presents as subacromial impingement involving the rotator cuff tendon, bicipital tendon, or subacromial bursa.15 Primary subacromial impingement involves compression of these structures between the acromion and greater tuberosity.16 The cause of primary impingement is usually a tight posterior capsule (causing the humeral head to migrate anteriorly) or abnormal acromial morphology. However, primary impingement syndrome is less common in competitive swimmers than secondary impingement.
The mechanism of secondary impingement occurs through a series of impairments, usually initiating in a swimmer with increased anterior glenohumeral laxity.10,15 Shoulder ROM in swimmers is similar to that of overhead athletes, with excessive external rotation and limited internal rotation. This shift in ROM towards increased external rotation is an adjustment to the demands on the glenohumeral joint which goes through approximately 4,000 strokes daily.15 The acquired anterior laxity permits excessive external rotation, but places greater demand on the rotator cuff and the long head of the biceps to reduce humeral head elevation and anterior translation.
Failure of the rotator cuff and the scapular stabilizers to maintain the humeral head in the glenoid fossa can lead to excessive humeral head migration and either increased tensile stress on the tendons 10, 15 or compression of the tendons from abutment of the humeral head on the undersurface of the acromian.15 The proposed mechanism of failure initiates with muscle fatigue. For example, the serratus anterior in the healthy shoulder stabilizes the scapula in upward rotation and protraction, creating adequate subacromial space for the biceps tendon and rotator cuff and maintaining good approximation between the humeral head and the glenoid fossa. During the pulling motion of swimming, the serratus anterior effectively reverses origin and insertion to propel the body over the arm, while maintaining the subacromial space and glenohumeral joint congruency. When the serratus anterior becomes fatigued, the scapula fails to protract and upwardly rotate and the subacromial space may be compromised. Additionally, the space between the humeral head and glenoid increases, contributing to more laxity.
Symptoms that develop as a result of fatigue can also affect stroke mechanics. Research has documented changes in muscle activity that occurs in swimmers with painful shoulders compared to swimmers with healthy shoulders.6 Many swimmers will inherently adjust their stroke to avoid painful movement patterns.17 For example, during early pull-through, the hand usually enters the water close to the midline with the elbow above the surface of the water. The upper extremity then continues to “reach” forward below the surface of the water towards the midline of the body. In swimmers with painful shoulders, the hand enters further away from the midline with the elbow dropped closer to the surface of the water. This change is usually made to avoid an impingement position of full elevation with internal rotation and horizontal adduction. Another adjustment occurs at the end of the pull-through phase, when the hand should be close to the thigh with internal rotation of the shoulder. In swimmers with painful shoulders, the shoulder was externally rotated and the pull-through phase was shortened to avoid impingement.
Another proposed impingement mechanism involves the microvasculature of the rotator cuff. Studies indicate that when the shoulder is abducted, the vessels of the supraspinatus and long head of the biceps are filled.18 Conversely, when the arm is adducted and at the side, the vascular system to these tendons is compromised. This phenomenon is referred to as a “wringing out” of the tendon, causing a temporary avascular zone 1 cm proximal to the insertion on the humeral head. This response also occurs when the humerus is adducted and flexed, a position that occurs with faulty mechanics or muscle fatigue.
Extrinsic Factors
In addition to identifying the impairments that may have contributed to swimmer's shoulder, the clinician must determine if the microtrauma is due to overuse, misuse, abuse, or disuse. Overuse in sports is performing a task with a frequency that does not allow the tissues to recover and symptoms may be due to lack of muscle strength or endurance. An example of overuse would be a swimmer increasing her yardage in a swim workout from 5000 yards to 10,000 yards per day. Misuse is using improper form or equipment, which may put abnormal stress on the tissue structures. An example of misuse is a swimmer using faulty stroke mechanics. One common error is inadequate or excessive body roll during freestyle. A swimmer with excessive body roll may cross the midline of the body during the pull through phase and this increased horizontal adduction can lead to impingement.2 Lack of body roll will also cause the humerus to compensate by moving into further horizontal adduction for adequate propulsion. Abuse is having excessive force going though normal tissues. An example of abuse is a swimmer who trains excessively with hand paddles, increasing strain on the shoulder. Disuse occurs when a swimmer has taken a period of time off without training resulting in atrophy or altered neuromuscular control of the stabilizing shoulder girdle musculature. In all of these cases, the tissues cannot accommodate the repetitiveness, force, or stress that is encountered with a specific activity.
PRESEASON AND CLINICAL ASSESSMENT
Overview
This section will discuss key points when assessing a swimmer during a preseason physical or during the season when symptoms are present. Some individuals may be predisposed to swimmer's shoulder if they have musculoskeletal impairments or engage in improper training methods. A preseason evaluation should screen for these impairments in a similar manner as a physical evaluation used for a swimmer with symptoms. In both cases, the goal is to determine if impairments exist that could lead or have led to swimmer's shoulder. The reader is referred to other sources for a comprehensive orthopedic shoulder assessment.19
During a clinical examination, information is collected in the subjective and objective assessment to determine a potential cause and effect relationship between the tissue pathology and presenting impairments. This information may be used to set up a preventative training program or guide treatment. The exact impairments that may predispose a swimmer to symptoms or tissue pathology are not fully understood as no research has studied impairments in asymptomatic swimmers to determine which impairments were most likely to lead to swimmer's shoulder. Most of the preventative programs are based on addressing impairments that occur as a result of developing swimmer's shoulder.
In swimmers who have already developed symptoms, the primary complaint is usually pain in the subacromial region. These symptoms may be associated with an inflammatory condition such as tendonitis, bursitis, capsulitis, or arthritis and may be labeled as impingement syndrome. While diagnosis of these symptoms and tissue pathology may guide medical treatment of either pharmacological intervention with oral medication or injections, this treatment may not address the causative factors. Physical therapists should focus on the impairments that are associated with the onset of symptoms including glenouhumeral hypermobility or instability, impaired posture, impaired rotator cuff strength, altered scapulohumeral rhythm or poor neuromuscular control, or a tight posterior capsule. Like most microtraumatic conditions, swimmers can usually not single out a specific event so the physical therapist has to discern which of these impairments or training errors may have contributed to the condition or injury. The subjective assessment may help identify the contributing impairments while the physical examination can focus on specific tests and measures to confirm this information.
Subjective Assessment
The subjective examination also provides information about the area, symptom description, and behavior of the symptoms in patients with swimmer's shoulder. This information may help the clinician identify potential sources of the symptoms. For example, a patient who points with one finger to the anterior lateral aspect of the shoulder and describes a sharp pain with overhead movements may have involvement of the subacromial region or AC joint. The physical examination would need to focus on these areas. Conversely, a patient who presents with diffuse pain throughout the shoulder and upper extremity and describes burning, shooting pains may need to have a detailed evaluation of the cervical spine to rule out spinal pathology.
Other subjective information may help the physical therapist determine the appropriate amount of testing performed during the physical examination. The clinician should determine the level of irritability of a condition during the subjective examination. Irritability is characterized by three parameters: pain level, what it takes to provoke the symptoms, and the latency or time it takes the symptoms to resolve after provocation. A highly irritable condition is determined by all three factors. For example, a patient who reports symptoms with a 7/10 pain level that are brought on with lifting the arm above 90 degrees without a load and the symptoms last for several hours, has a highly irritable condition. Conversely, a patient who reports symptoms with a 5/10 pain level that comes on with lifting 200 lbs on a bench press, and last only for a few seconds has low irritability.
In swimmers, low-level shoulder pain that only occurs after heavy training and resolves quickly is low irritability. A swimmer who has high-level shoulder pain during swimming and following training for the remainder of the day has high irritability. The rehabilitation specialist must be cautious during the physical examination of a patient with high irritability because once the symptoms are provoked, results from the remaining tests and measures may be unclear.
One key element in the history is assessing the training program and methods of the swimmer. The physical therapist should determine the number of yards or meters performed in each workout, the number of workouts per week, the dry-land program, and any recent changes in training.
Common Findings on Physical Examination
A preseason physical or clinical examination of a swimmer with shoulder symptoms will screen for several impairments. Initial observation may reveal common postural impairments related to the shoulder girdle. A common postural deviation observed with swimmers is a forward head, rounded shoulder posture. This posture is a combination of upper quarter impairments including increased thoracic kyphosis, decreased cervical lordosis, protracted scapulae, and internally rotated/anterior humeral head.20,21 Soft tissue findings associated with this posture include restricted anterior shoulder musculature, lengthened and weak medial scapular stabilizers, tight glenohumeral posterior capsule, and weak anterior cervical flexors.22
Physical examination of swimmer's shoulder will usually reveal alterations in active ROM of the shoulder, particularly at the midrange or end range of elevation. Swimmers with impingement may have a painful arc from 60-120 degrees if the head of the humerus is not maintained in the glenohumeral joint.4,11,15 Altered scapulohumeral rhythm may be observed with excessive elevation or upward rotation of the scapula. Kibler23 has presented an assessment technique to measure lateral scapular slide, by measuring the distance between the medial border of the scapula and the spine during elevation. Assessment of passive ROM will usually show excessive external rotation and horizontal abduction due to hypermobility of the anterior glenohumeral joint capsule. These swimmers will usually have a sulcus sign, a positive load and shift, a positive relocation test, and may have a positive apprehension sign.5,7,10 However, hypermobility determined by these tests may be the result of ligamentous laxity.7,10 Hypermobility is not instability unless the secondary stabilizers do not function adequately and symptoms occur. In swimmers with instability, weakness of the rotator cuff and scapular stabilizers will be noted. If these structures are inflamed, impingement tests will be positive and resisted tests may be painful.
If these provocation tests are positive, the clinician must rule out sources of primary impingement such as abnormal acromial morphology (through x-ray) or a tight posterior capsule. In addition, if tissue pathology is suspected by the physical therapist based on the findings in the physical examination, the swimmer may need to be referred back to the physician for additional tests. Chronic swimmer's shoulder can result in pathology of the rotator cuff, glenoid labrum, and long head of the biceps.
PRINCIPLES OF PREVENTION AND TREATMENT
Introduction
The foundation for establishing a prevention or treatment plan for the swimmer's shoulder is having a clear understanding of the impairments, underlying tissue pathologies, and resultant functional limitations. Treatment and prevention of swimmer's shoulder focuses on addressing impairments and the training errors of overuse, misuse, or abuse as described earlier in this chapter. Achieving functional goals also requires knowledge of swimming mechanics and training techniques, as well as the stress placed on the shoulder during swimming. This knowledge will guide the physical therapist to choose exercises that place demands on the shoulder similar to those encountered with a specific sport or position.
Address Impairments
The first step in treating swimmer's shoulder is to address any related impairments. Because the clinical presentation usually involves pain related to inflammation, initial treatments may use modalities and manual techniques, such as grade I or II mobilizations, to address pain. As pain resolves, the physical therapist should prioritize the problem list related to the symptoms. Potential common impairments that need to be addressed include postural deviations, tight anterior chest musculature, hypomobility of the thoracic spine, loss of joint mobility or excessive joint mobility, tight posterior capsule, and impaired strength and endurance of the rotator cuff and scapular stabilizers.
Posture
Postural impairments are managed through joint /soft tissue mobilization, flexibility, and strengthening/stabilization exercises of the scapular retractors and deep cervical flexors. Tight anterior shoulder musculature including the pectoralis minor can be self stretched or manually stretched. Care must be taken to avoid over-stretching the anterior capsule. One method that allows the anterior chest to be stretched without overstressing the anterior capsule is to apply a low load on the anterior aspects of the shoulder using cuff weights while the patient lies supine over a bolster (Figure 1). This position allows the scapulae to retract over the bolster so the stretch is concentrated on the anterior chest musculature.
Figure 1.
Anterior capsule stretch using cuff weights; supine over bolster.
Joint Mobility
In swimmer's shoulder, posterior capsule tightness may accompany anterior shoulder laxity and should be addressed by the physical therapist. Posterior capsule mobilizations can be performed with the patient in supine and the shoulder blade supported in the scapular plane using a mobilization wedge or folded towel. The clinician holds the arm in mid range abduction, applies a gentle glenohumeral distraction while providing a posterior glide to the proximal humerus (Figure 2). A self stretch to the posterior capsule can also be applied by lying on the involved side with the shoulder flexed to 90 degrees. The patient applies a self stretch by applying a downward force to the distal forearm towards the plinth (Figure 3).
Figure 2.
Posterior guide to humerus (posterior bolster).
Figure 3.
Self stretch of posterior capsule.
Scapular Stabilization
Scapular stability and proper scapulohumoral rhythm is an essential element of shoulder rehabilitation and prevention. Scapular position directly affects humeral head position and determines the length tension relationship for the rotator cuff as these muscles originate on the scapula.23 An unstable scapula or faulty movement patterns can change the demands on the rotator cuff muscles, potentially leading to microtrauma injuries. The physical therapist should assess the muscles essential to scapular stability such as the middle and lower trapezius, serratus anterior, and rhomboids. Scapular position and improper movement patterns are treated with a combination of soft tissue release and neuromuscular re-education to inhibit overactive, dominant muscles and facilitate weak, inhibited muscles.
Rehabilitation and prevention of swimmer's shoulder should incorporate neuromuscular reeducation and strengthening of the scapular stabilizers. Research has documented the effectiveness of different prone exercises for recruiting the scapular stabilizers.24 Prone scapular stability exercises are assessed by the ability to recruit targeted muscles is positions that simulate swimming. For prone exercises, the clinician should instruct the patient to maintain the scapula in retraction/depression while palpating the upper trapezius to ensure no compensation is occurring.
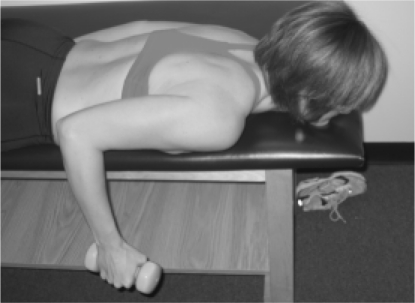
Figures 4–11 illustrate some common prone table exercises used for shoulder strengthening and scapular stabilization. The rowing motion is accomplished with humeral extension with elbow flexion (Figure 4). For prone extension, the patient extends the shoulder with the elbow extended and thumb facing away from the body (Figure 5). For prone horizontal abduction, the patient horizontally abducts the arm with the elbow extended and either neutral rotation or external humeral rotation (Figure 6). During these exercises, the clinician should instruct the patient to retract the scapula prior to and during the humeral motion. The patient should also know not to advance the humerus beyond the plane of the body, particularly if an injury or postoperative condition warrants protection of the anterior capsule. Figure 7 is an example of an exercise used in our clinic to recruit the lower trapezius. The patient lies prone with the humerus abducted to 150 degrees and the elbow is flexed to 90 degrees. The patient is instructed to lift the hand off the table by externally rotating the shoulder.
Figure 4.
Rowing in prone.
Figure 11.
“TYI Exercises.” I: Shoulders in full bilateral elevation with elbow extension.
Figure 5.
Prone extension.
Figure 6.
Prone horizontal abduction
Figure 7.
Recruitment of the lower trapezius. Lift the hand off the table by externally rotating the shoulder.
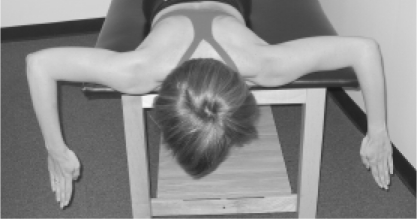
Figures 8 though 11 represent bilateral scapular stabilization exercises. “Supermans” are performed in prone with the elbows in full extension and the shoulders externally rotated at the sides of the body (Figure 8). The patient is instructed to retract the scapulae and lift the hands and arms off the table. Figure 9 is the first in a progressive sequence of three exercises that we refer to as TYI exercises because of the patterns formed. The patient retracts the scapulae with the arms abducted to 90 degrees and moves the humerus into horizontal abduction forming a “T”. As the patient advances, the shoulders are externally rotated with the elbows flexed to 90 degrees, forming a “Y” (Figure 10). The final exercise requires the patient to move into a position of full bilateral elevation with elbow extension, forming an “I” (Figure 11).
Figure 8.
“Superman.”
Figure 9.
“TYI Exercises.” T: Prone on mat. Retract scapulae with arms abducted to 90 degrees and humerus in horizontal abduction.
Figure 10.
“TYI Exercises.” Y: Shoulders externally rotate with elbow flexed to 90 degrees.
Scapular protraction and stabilization in the protracted position are trained through a series of exercises, starting with a supine punch. The patient is positioned supine with the arm held in 90 degrees flexion with full elbow extension and maintained in the scapular plane. During the movement, the patient is told to move the hand towards the ceiling, by protracting the scapula. Manual resistance or weights can be added to this motion as the patient advances (Figure 12). These exercises may also be used in conjunction with weight bearing exercises.
Figure 12.

Protraction of scapula.
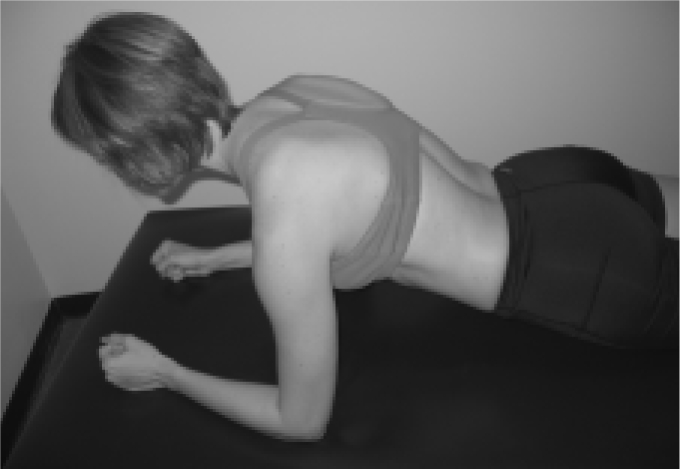
Weight bearing exercises for scapular stabilization are illustrated in figures 13-19. Exercises are advanced from prone on elbows (Figure 13) to quadruped (Figure 14) to a push up position (Figure 15). As the patient improves, the lower extremities can be elevated to increase resistance (Figure 16). A dynamic component can be added to higher level athletes who demonstrate good control with the preceding exercises. These patients can perform these exercises with the upper extremities on a wobble board (Figure 17),“walk-outs” with their upper extremities with the lower quarter on a gym ball (Figure 18), or “step-overs” using the upper extremities to “walk” up and down over a foot stool (Figure 19). A slide board is also an excellent device to use for dynamic upper extremity stabilization. Patients can be progressed from performing horizontal abduction and adduction on their knees and eventually on their toes. For these exercises, patients are instructed to maintain scapular protraction during the activity to strengthen the serratus anterior.
Figure 13.
Prone, supported on elbows.
Figure 19.
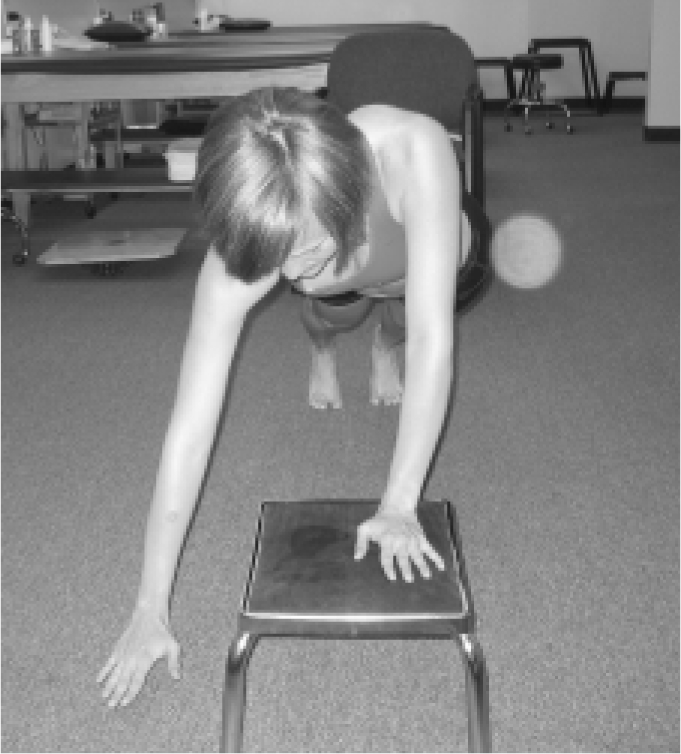
“Step-overs.”
Figure 14.

Quadruped position.
Figure 15.

Push up position.
Figure 16.

Push up position; legs elevated in chair.
Figure 17.

Push up position; hands placed on wobble board.
Figure 18.
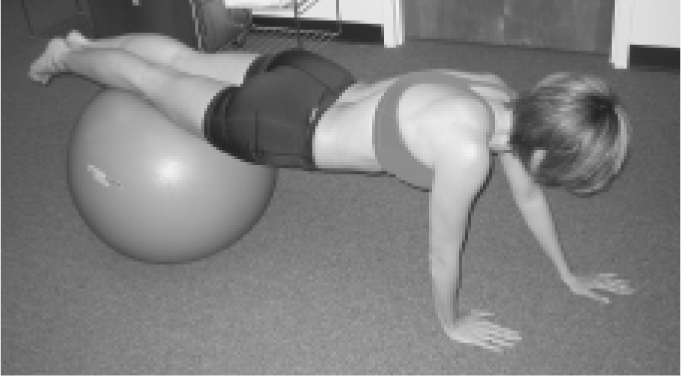
“Walk-outs.”
Rotator Cuff Strength
Strengthening exercises for the rotator cuff are progressed based on the presenting condition and the ability of the patient. The range of rotator cuff strengthening exercises may include isometric, concentric, eccentric, and plyometric activities. As healing allows, shoulder strengthening is initiated with isometric exercises including rhythmic stabilization drills, which are exercises to challenge a patient to maintain the upper extremity in a variety of positions while the rehabilitation specialist challenges the position with manual resistance. The exercise selection should be based on positions that do not overstress the healing tissues. This activity helps restore proprioceptive feedback to the central nervous system through mechanoreceptors of the shoulder girdle and prepares the shoulder for isotonic strengthening.
Isotonic strengthening of the rotator cuff can be accomplished with different types of resistance in different positions. Resistance can be applied manually, with resistive bands, or with weights. The advantage of using manual resistance is that the therapist can vary the resistance to accommodate the output from the patient. The advantage of using resistive bands is that the patient can perform functional movement patterns against resistance. However, these forms of resistance do not allow a clinician to quantify the amount of resistance, which is the advantage of using weights. When choosing a position for rotator cuff strengthening, the rehabilitation specialist should have a goal for the exercise. If the goal is to stabilize the scapula, exercising in supine may be the best position because the scapula is fixed against the table. Patients can be progressed to a sidelying position to work against gravity or in standing position to simulate functional movement patterns. Patients should be encouraged to exercise in the scapular plane and the position of humeral abduction can advance to reproduce the position the arm is in during a specific sport.
Rotator cuff exercises are performed and advanced based on the available ROM. Due to the importance of the eccentric component of the rotator cuff in overhead sports, this mode of exercise should be integrated into the rehabilitation program, particularly for external rotation. The infraspinatus and teres minor contract to stabilize the humeral head by maintaining a posterior pull to counter any anterior translatory forces.
Address Training Errors
Overuse is a classic training error that occurs in swimming as athletes typically train 10-12 hours per week in the water in addition to dry-land training. Swimmers can average 10,000 yards per day of training. The high level of repetitions, estimated at 4,000 strokes per side, that occur during training sessions can cause fatigue, leading to the conditions discussed earlier. Modification of swim yardage may need to be emphasized if the swimmer wants to prevent progression of an injury.
Abuse is another training error that can occur in swimming, causing increased external stress on the shoulder. The use of hand paddles increases stress on the upper extremity by increasing surface area and resistance to movement. Kickboards put the arm in position of full elevation and internal rotation, leading to subacromial joint compression. Use of these devices should be omitted or limited for a swimmer returning from a shoulder injury.
Misuse in swimming occurs if an individual has faulty stroke mechanics. An example of improper technique is when the hand crosses the mid-line during the pull-through phases of the freestyle stroke. This motion is common in swimmers who have excessive body roll and can predispose them to impingement. Optimal body roll allows the arm to stay close to the plane of the scapula, thus reducing the stress of soft tissue structures in the anterior shoulder region.25 Optimal body roll also allows greater lengthening of the abdominal oblique muscles, shoulder adductors/medial rotators, and scapular retractors so that at the beginning of the pull-through these muscles have a mechanical advantage.2 Conversely, a lack of adequate body roll forces the recovering arm into a greater range of shoulder extension, horizontal abduction, and medial rotation in order to clear the hand from the water, causing encroachment of the subacromial space.
An important issue to consider when working with swimmers is their reluctance to stay out of the water.25 Although swimmers are involved in dry-land training, no suitable substitute exists for swimming. Modification of training schedules and techniques allow the patient to continue swimming, enabling the physical therapist to establish or maintain credibility with the swimmer.15, 25 In extreme cases, the swimmer may need a short dry-land period to allow for adequate soft tissue healing. In these cases, the rehabilitation specialist should educate the swimmer so that the reason for the lay-off is understood. Time spent out of the water should be kept as short as possible, even if the swimmer is doing primarily kicking activities. Although returning to the water may not be ideal for rehabilitation, keeping a swimmer out of the water for a lengthy period may result in a rehabilitation program that is ignored. Activity modification in swimming may consist of the following tasks:
Temporarily reduce training distance and frequency.
Alter training patterns so that different strokes are used more frequently throughout the practice. This alteration will reduce the repetitive pattern at the glenohumeral and allow the muscles to function differently.
Avoid the use of hand paddles, kickboards, and surgical tubing.
Use swim fins to enhance the propulsion from the legs and reduce the stress on the shoulder
SUMMARY
Swimmers shoulder is a condition that may be prevented with adequate preseason screening that can identify impairments and training errors that may lead to symptoms. If a swimmer does become symptomatic during the season, the physical therapist should identify the most likely impairments or training errors and rule out any significant tissue pathology that would warrant a referral to an orthopedic surgeon. A comprehensive rehabilitation program usually includes strengthening of the rotator cuff and scapular stabilizers, stretching anterior chest musculature that may be shortened, and implementing activity modification so the athlete can still participate in the sport. Future research should focus on determining if addressing specific impairments prior to the season can reduce the incidence of swimmer's shoulder and assessing which impairments are the greatest risk factors.
REFERENCES
- 1.Abelew T. Kinesiology of the shoulder. In: Tovin BJ. Evaluation and treatment of the shoulder: an integration of the guide to physical therapist practice. Philadelphia: FA Davis Co; 2001:25 [Google Scholar]
- 2.Shapiro C. Swimming. In Shamus E, Shamus J. (eds)Sports injury prevention and rehabilitation. New York: McGraw-Hill;2001:103–154 [Google Scholar]
- 3.Ciullo JV, Stevens GG. The prevention and treatment of injuries to the shoulder in swimming. Sports Med. 1989;7:182–204 [DOI] [PubMed] [Google Scholar]
- 4.Bak K. Nontraumatic glenohumeral instability and coracoacromial impingement in swimmers. Scand J Med Sci Sports. 1996;6:132–144 [DOI] [PubMed] [Google Scholar]
- 5.Bak K, Faunø P. Clinical findings in competitive swimmers with shoulder pain. Am J Sports Med. 1997;25:254–260 [DOI] [PubMed] [Google Scholar]
- 6.Bak K, Magnusson SP. Shoulder strength and range of motion in symptomatic and pain-free elite swimmers. Am J Sports Med. 1997;25:454–460 [DOI] [PubMed] [Google Scholar]
- 7.Beach ML, Whitney SL, Dickoff-Hoffman SA. Relationship of shoulder flexibility, strength and endurance to shoulder pain in competitive swimmers. J Orthop Sports Phys Ther. 1992;16:262–268 [DOI] [PubMed] [Google Scholar]
- 8.McMaster WC. Anterior glenoid labrum damage: a painful lesion in swimmers. Am J Sports Med. 1986;14:383–387 [DOI] [PubMed] [Google Scholar]
- 9.McMaster WC, Troup J. A survey of interfering shoulder pain in United States competitive swimmers. Am J Sports Med. 1993;21:67–70 [DOI] [PubMed] [Google Scholar]
- 10.McMaster WC, Roberts A, Stoddard T. A correlation between shoulder laxity and interfering pain in competitive swimmers. Am J Sports Med. 1998;26:83–87 [DOI] [PubMed] [Google Scholar]
- 11.Richardson AB, Jobe FW, Collins HR. The shoulder in competitive swimming. Am J Sports Med. 1980;8:159–163 [DOI] [PubMed] [Google Scholar]
- 12.Stocker D, Pink M, Jobe FW. Comparison of shoulder injury in collegiate-and master's-level swimmers. Clin J Sport Med. 1995;5:4–8 [DOI] [PubMed] [Google Scholar]
- 13.Counsilman JE. The complete book of swimming, New York: Atheneum, 1977 [Google Scholar]
- 14.Johanson MA, Donatelli R, Greenfield BH. Rehabilitation of microtrauma injuries. In Greenfield BH. (ed) Rehabilitation of the Knee: A Problem-Solving Approach. Philadelphia: FA. Davis Co; 1993: 139– 173 [Google Scholar]
- 15.Allegrucci M, Whitney SL, Irrgang JJ. Clinical implications of secondary impingement of the shoulder in freestyle swimmers. J Orthop Sports Phys Ther. 1994;20:307–318 [DOI] [PubMed] [Google Scholar]
- 16.Neer CS. Impingement lesions. Clin Orthop. 1983;173:70–77 [PubMed] [Google Scholar]
- 17.Scovazzo ML, Browne A, Pink M, et al. The painful shoulder during freestyle swimming. Am J Sports Med. 1991;19:577–582 [DOI] [PubMed] [Google Scholar]
- 18.Rathbun JB, McNab I. The microvascular pattern of the rotator cuff. J Bone Joint Surg. 1970;52B:540–553 [PubMed] [Google Scholar]
- 19.Magee DJ. Orthopedic Physical Assessment. 4th Ed.Philadelphia: Saunders, 2002 [Google Scholar]
- 20.Rocabado M. Biomechanical relationship of the cranial, cervical, and hyoid regions. J Craniomandiular Pract. 1983;11:3. [DOI] [PubMed] [Google Scholar]
- 21.Ayub E, Glasheen-Wray M, Kraus S. Head posture: a study of the effects on the rest postion of the mandible. J Orthop Sports Phys Ther. 1984;5:179. [DOI] [PubMed] [Google Scholar]
- 22.Janda V. Muscles, central nervous motor regulation and back problems. In Korr IM. (ed). Neurobiologic Mechanisms in Manipulative Therapy. New York: Plenum; 1979 [Google Scholar]
- 23.Kibler B. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325–339 [DOI] [PubMed] [Google Scholar]
- 24.Mosely JB, Jobe FW, Pink M, Perry J, Tibone J. EMG analysis of the scapular muscles during a shoulder rehabilitation program. Am J Sports Med. 1992;20:128–134 [DOI] [PubMed] [Google Scholar]
- 25.Murphy TC. Shoulder injuries in swimming. In: Andrews JR, Wilk KE. (eds). The Athlete's Shoulder.,New York: Churchill Livingstone;1994:411–424 [Google Scholar]