Abstract
Background
The transversus abdominis (TrA) is a spine stabilizer frequently targeted during rehabilitation exercises for individuals with low back pain (LBP). Performance of exercises on unstable surfaces is thought to increase muscle activation, however no research has investigated differences in TrA activation when stable or unstable surfaces are used.
Objective
The purpose of this study was to investigate whether TrA activation in individuals with LBP is greater when performing bridging exercises on an unstable surface versus a stable surface.
Methods
Fifty one adults (mean ± SD, age 23.1 ± 6.0 years, height 173.60 ± 10.5 cm, mass 74.7 ± 14.5 kg) with stabilization classification of LBP were randomly assigned to either exercise progression utilizing a sling bridge device or a traditional bridging exercise progression, each with 4 levels of increasing difficulty. TrA activation ratio (TrA contracted thickness/TrA resting thickness) was measured during each exercise using ultrasound imaging. The dependent variable was the TrA activation ratio.
Results
The first 3 levels of the sling-based and traditional bridging exercise progression were not significantly different. There was a significant increase in the TrA activation ratio in the sling-based exercise group when bridging was performed with abduction of the hip (1.48 ± .38) compared to the traditional bridge with abduction of the hip (1.22 ± .38; p<.05).
Conclusion
Both types of exercise result in activation of the TrA, however, the sling based exercise when combined with dynamic movement resulted in a significantly higher activation of the local stabilizers of the spine compared to traditional bridging exercise. This may have implications for rehabilitation of individuals with LBP.
Keywords: Core stability, rehabilitation, Rehabilitative Ultrasound Imaging
BACKGROUND
Low back pain (LBP) is a significant problem that affects approximately 50% of the population.1 The majority of individuals with recurrent episodes of LBP do not have an identifiable structural diagnosis.2 A treatment-based classification system has been developed to identify similarities among subsets of individuals with LBP so that clinicians can select appropriate interventions to improve outcomes.3, 4 One subset of the classification system includes individuals who are thought to benefit from spine stabilization exercises.5–7
The stabilization classification is a subgroup of patients who experience LBP as a result of faulty neuromuscular control, rather than from true ligamentous instability.8, 9 Muscular injury, fatigue, or facet or disc degeneration can compromise the stabilizing effects resulting in shearing forces that cause the pain.10 A decrease in muscular control can have damaging effects on postural control and intersegmental stability which may lead to degeneration of spinal structures.10 Therefore, this subgroup of patients would likely respond to a spinal neuromuscular rehabilitation program that targets the spinal stabilizers.
The abdominal drawing-in maneuver (ADIM) has been described as the best way to activate the TrA11–14 and is often a fundamental exercise in a traditional stabilization program for LBP.15, 16 The ADIM is an inward movement of the lower abdominal wall in which the patient is instructed to draw the umbilicus toward the spine.15, 16 A key feature is to teach the patient to preferentially activate the TrA while maintaining relaxation of the more superficial musculature (rectus abdominus, external oblique). The ADIM is often used to facilitate the re-education of neuromuscular control mechanisms provided by the local stabilizing muscles.16 This training of the TrA has been shown to improve pain and function in patients with chronic LBP17–19 because activating these muscles is thought to assist in dynamic spine stabilization during functional tasks.20
Once the motor skill of the ADIM is taught, it is combined with varied postures including supine or prone and advancing from stable to increasingly unstable surfaces.16, 17 The traditional stabilization exercise interventions have been successful at treating LBP,17, 21–24 however there is often recurrence of LBP that has been illustrated in several studies.20,25–30 This recurrence rate may be an indicator that patients may be performing these exercises without properly activating the TrA or that a timing dysfunction exists. Hodges et al.25 proposed that the TrA contracts prior to limb movement in healthy individuals, while the pre-activation is poor in those with LBP. Exercise intervention should focus on the best method to target the stabilizing musculature, and therefore the recruitment of the TrA during specific exercises should be examined.
Sling exercise therapy has been proposed to activate local spine stabilizers during the activity in a pain free manner without substitution of global muscles.26 Sling therapy exercise is performed while the pelvis or lower extremities are supported or suspended in a sling (Figure 1). The exercises can be made easier by providing assistance with a sling and elastic cord to offset body weight, or made more difficult by providing an unstable surface to perform the exercises. The patient must bear weight through the cords and balance him or herself during the exercise. Stuge et al. found that doing specific stabilization exercises using sling exercise therapy in post-partum women with pelvic pain was effective in reducing pain, improving functional status, and improving health-relating quality of life after a 20 week intervention27 and at a 2 year follow up.28 However, the underlying mechanism for improvement in their outcomes was unknown. Stuge proposed that increased activation of local stabilizer muscles with the sling exercise therapy may have contributed to improved outcomes compared to traditional therapy.
Figure 1.

Sling exercise.
Rehabilitative Ultrasound Imaging (RUSI) is a non-invasive method to visualize the lateral abdominal wall and qualitatively and quantitatively assess deep muscular activity with exercise. Muscle thickness change during the ADIM has been validated with EMG studies29,30 and is an indicator of muscle activation.16, 31 The TrA activation ratio has been developed to examine the recruitment of the TrA during an active contraction, thus normalizing the measurement to the resting thickness of the muscle.32 Therefore, comparisons in the TrA activation ratio during specific therapeutic exercise interventions can help identify those exercises that preferentially recruit the local stabilizers.16 The purpose of this study was to compare the TrA activation ratio during a progression of traditional stabilization exercise to a similar progression of sling based exercise.
Methods
Study Design
A randomized trial with one between factor, exercise group (standard bridge, sling bridge) and one within factor, level of exercise (decreasing support) was used to examine the effects of exercise on TrA activation ratio. The main outcome variable was the ratio of TrA thickness during the exercise versus in the relaxed position (TrA activation ratio).
Subject demographics between groups were compared using independent t-tests. A 2×2 mixed model ANOVA was performed to compare TrA thickness ratios during either the traditional bridge or sling bridge exercise. The level of statistical significance was set a priori at P< 0.05. Statistical analyses were performed with SPSS Version 16.0 (SPSS Inc., Chicago, IL).
Sample size calculations indicated the number of participants required was 24 per group in order to detect a 0.3 difference in TrA contraction ratio between groups. This was based on standard deviations (0.36) from a previous study,32 an a priori significance level of P= 0.05 and a power of 0.80.
Subjects
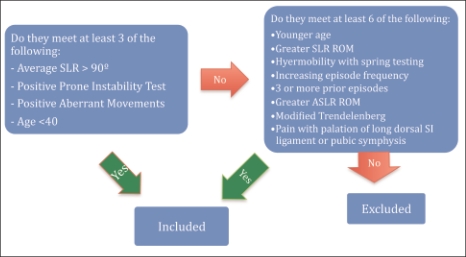
Fifty-one adults aged 18-53 with a current episode of LBP were recruited to participate in this study (males=8; females=33). Demographic information is found in Table 1. Subjects were recruited from the university community and from an athletic therapy clinic. The subjects met either 3 out of 4 criteria that categorized them in the lumbar stabilization classification or 6 criteria for best-fit categorization (Figure 2). The criteria for the lumbar stabilization classification clinical prediction rule were patients that are a younger age (<40), greater flexibility including hamstring range of motion of 91°, positive prone instability test, and an instability catch or aberrant movements in flexion/ extension motions.5 Subjects that did not meet 3 out of these 4 criteria were further evaluated to see if they met at least 6 of the following best fit criteria: spring test hypermobility, increased episode frequency, more than 3 previous episodes, positive posterior pelvic pain provocation test, active straight leg raise range motion of 60-90°, modified Trendelenburg, or pain with palpation of the long dorsal sacroiliac ligament or pubic symphysis. If they met 6 of these criteria, then they were considered a best fit for the stabilization classification (Figure 3). The study was approved by the Institutional Review Board of the University of Virginia, and written informed consent was obtained from all the participants before testing.
Table 1.
Subject demographics.
| Total | Traditional Exercise Croup | Sling Exercise Group | |
|---|---|---|---|
| Age | 23.1 ± 6.0 | 23.8±7.0 | 22.5 ± 5.1 |
| Height (cm) | 173.6 ± 10.5 | 171.5 ± 10.6 | 175.7 ± 10.2 |
| Mass (kg) | 74.7 ± 14.5 | 72.7 ± 12.9 | 76.7 ± 15.8 |
| BMI | 24.6 ± 2.8 | 24.6 ± 2.4 | 24.6 ± 3.2 |
| Oswestry Score | 12.8 ± 5.0 | 13.3 ± 5.4 | 12.4 ± 4.7 |
| FABQ Score (physical activity) | 14.9 ± 5.9 | 15,2 ± 6.4 | 14.7 ± 5.5 |
| FABQ Score (work) | 5.5 ± 7.3 | 7.0 ± 8.3 | 4.0 ± 7.6 |
| Duration of Symptoms (months) | 30.0 ± 41.0 | 44.55.2 | 33.3 ± 9.2 |
| TrA Contraction Ratio | 1.58 ±.27 | 1.55 ±.22 | 1.61 ±.30 |
Figure 2.
Inclusion criteria.
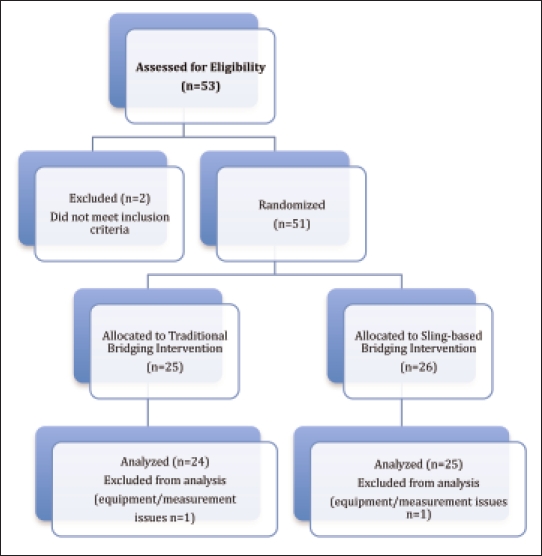
Figure 3.
CONSORT flow chart
Instruments
Ultrasonography
Resting ultrasound images of the TrA were obtained using a LOGIQ Book XP (GE Healthcare Products, Milwaukee, WI) with an 8 MHz linear transducer while the subject was in the supine hook-lying position. Ultrasound imaging is a reliable and valid technique to measure muscle thickness changes. It has been compared to MRI, which is considered the gold standard for the measurement of muscle geometry,33 and it has been compared to EMG as a standard technique for monitoring muscle activation.29, 30
The images were recorded in B mode with the transducer placed just superior to the iliac crest on the right side in the transverse plane along the mid-axillary line.34 To standardize the placement of the transducer among subjects, the hyperechoic interface between the TrA and the thoracolumbar fascia was the right most structure of the ultrasound image. The angle of the transducer was altered to ensure the best image was captured and the fascial layers of the abdominal muscles were parallel on the screen.34 Images were viewed ipsilateral to the side of LBP, or on the right side if the participant had central pain. The transducer was consistently placed transversely over the lateral aspect of the abdomen as previously reported with the medial edge of the transversus abdominis was visualized on the far right side of the screen.34,35 (Figure 4) The thickness of the TrA, Internal Oblique (IO), External Oblique (EO), and total lateral abdominal thickness were measured using Image J software (Version 1.41o, Wayne Rasband National Institutes of Health; USA). On each image, the scale was set for one centimeter using the numeric scale on the right side of the image. The thickness of the TrA, EO, and IO were then measured using the distance between the superior edge of the deep hyperechoic fascial line to the inferior edge of the superior fascial line. Then, the total lateral abdominal thickness was measured by the distance between the superior portion of the deep fascial border of the TrA to the inferior portion of the superior fascial border of the EO.34 The thickness measurements were then saved into Microsoft Excel® where TrA activation ratios were calculated.
Figure 4.
Resting and contracting with ADIM ultrasound image of lateral abdominal wall.
To minimize bias, the series of images were stored with no indication of which group the subject had been randomized. The images were later measured by a blinded examiner with previously established intrarater reliability (ICC3,k) equal or greater than 0.99 for the TrA thickness measurements.
Prior to enrolling subjects, both examiners underwent a supervised training program for the RUSI by an experienced physical therapist. After training, a pilot study that consisted of 10 participants was used to establish intrarater reliability for the RUSI measurement technique. Two images were taken, one during rest and 1 during a single ADIM contraction. This sequence was repeated 3 times for a total of 6 images for each rater. This sequence was then repeated a second time. Measurements were taken of the lateral abdominal wall and the measurement values were then compared and it was found that the intraclass correlation coefficient (ICC) for intrarater, interimage reliability was greater than or equal to 0.99 for the TrA muscle thickness measure (at rest and contracted). Reliability for this rater was determined to be excellent compared to previous reports of this measurement technique.32,34,36
Testing procedures
Pre-Testing Training
The examiner utilized ultrasound imaging during pre-testing training in order to monitor all participant's progress while practicing the ADIM. The technique established by Teyhen et al.34 was used to train the subjects to perform an ADIM. Participants were instructed how to perform this contraction through traditional methods, without using visual feedback from the ultrasound image.16 Participants were given verbal cueing instructions to gently pull their navel to the spine at the end of a normal exhalation and to hold this contraction for 10 seconds while continuing normal respiration. A plateau in ADIM performance was thought to occur when the participant could perform 3 isolated TrA contractions without a specific increase in EO and IO muscle thickness.
Initial Measurements
After ADIM training was complete, three baseline, resting images were recorded at the end of exhalation. These images were stored for later measurement by a blinded investigator.
Intervention Procedures
Following baseline measurement of lateral abdominal muscle thickness, participants were randomly assigned to either a traditional bridging exercise group or the sling exercise bridging group using pre-printed cards enclosed in sealed envelopes.
There were four levels of bridging exercises in each group, each progressively more difficult. The investigator monitored success at each level prior to advancing to the next stage of the exercise. The investigator observed the pelvic alignment in the horizontal plane and or any compensatory movements and asked participants about whether the activity increased their pain. Once the exercise was performed properly, images during the exercises were recorded during a 5 second hold. The examiner positioned the ultrasound transducer on the lateral abdomen to appropriately view the TrA and at the completed position of each exercise, recorded the image for the contracted position. Five repetitions were performed at each level of the exercise and the investigators recorded the RUSI during repetitions 2-4. At least one contracted image was obtained during each of the four levels of exercise progression. The images were stored and saved according to the participant number and the level of exercise. The images were measured after data collection by an examiner who was blinded to the exercise condition.
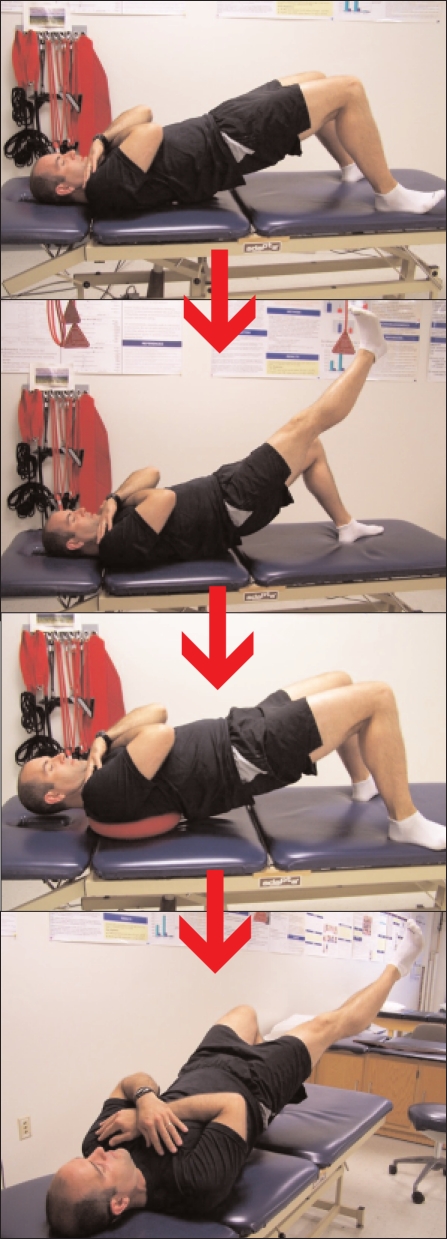
Traditional Bridge Exercise Progression
Each exercise began with the participants in the supine hook-lying position on the treatment table with their knees bent to 90°, feet flat on the table, and arms crossed over the chest. The participants were then instructed to perform an ADIM and then push through the heels to lift their hips into the air while maintaining straight alignment of the knees, hips, and shoulders. In the first level, the participants held this position for 5 seconds and then were instructed to lower their back and hips back to the starting position. The second level consisted of the participants extending their right knee for 3 seconds, returning their foot to the ground, followed by left knee extension for 3 seconds and then lowering back to the starting position. In the third level, the participant had a DynaDisc™ placed between their scapulae to perform the exercise on an unstable proximal surface and in the fourth level they were instructed to alternately extend their knees (as in condition two) as well as abduct the hip 45°. Participants performed 5 repetitions on each level of the exercise (Figure 5).
Figure 5.
Traditional bridge exercise progression.
Sling Bridge Exercise
The Redcord™ sling exercise therapy device (Redcord AS; Staubo, Norway) was used for the sling bridge exercise. There were four possible levels of the sling-bridging exercise (Figure 6). The participants in the sling exercise group began by laying supine on the treatment table with their hips and knees bent to 90°. The participant's knees were placed in a sling that was suspended from the ceiling. The first level consisted of the participants lifting their hips into the air while maintaining straight alignment of the knees, hips, and shoulders. Participants were not instructed to perform an ADIM prior to sling exercise, as suggested in product literature (RedCord™). The participants held this position for 5 seconds while an image was recorded then lowered themselves back to the starting position. In the second level, the participants left knee remained in the sling and the right knee was not in the sling. The participant was instructed to hold their right leg at the same level as the left and to lift their hips into the air while maintaining straight alignment of the knees, hips, and shoulders. They held this position for 5 seconds and then lowered back to the starting position. In the third level, the participant had both knees placed in the sling and a DynaDisc™ was placed in between their scapulae to provide an unstable proximal surface upon which to perform the bridge. In the fourth level, the participants' ankles were placed in two separate slings and they were instructed to perform the bridge and then abduct their legs one at a time before lowering back to the starting position. Participants performed 5 repetitions on each level of the exercise and US images were recorded on repetitions 2-4.
Figure 6.
Sling-Bridge exercise progression.
Results
The traditional exercise and sling exercise groups did not differ (P > .05) in terms of demographic stabilization classification criteria, or pre-intervention TrA activation ratio. It was not possible to obtain clear images for 2 participants; therefore the data for these participants was not included in the analysis. All participants were able to progress through the first two levels of their respective exercise progression in a pain free manner with correct technique. One individual was not able to progress to Level 3 of the traditional bridging exercise, while all individuals in the sling bridge progression were able to complete Level 3. Level 4 presented the greatest technical challenge with 18 (75%) individuals able to complete the traditional bridging exercise and 22 (88%) individuals completing the sling bridge progression. No individual in either group reported pain during the exercise intervention at any level.
Although consistently higher in the sling exercise group, there were no significant differences (P>.05) in TrA activation ratios between traditional bridging and sling bridging when comparing the first 3 levels of the exercise progression (Table 2). TrA activation ratio was significantly greater (P=.04) when performing sling bridging with hip abduction (Level 4) compared to traditional bridge with hip abduction (Table 2).
Table 2.
Transverse abdominis activation during bridging exercise.
| Traditional | Sling | P value | |
|---|---|---|---|
| Normal | 1.20 ± .37 | 1.33 ± .5 | .29 |
| Single Leg | 1.22 ± .39 | 1.25 ± .46 | .79 |
| Unstable Surface | 1.23 ± .4 | 1.33 ± .47 | .41 |
| Hip Abduction | 1.22 ± .38 | 1.48 ± .38 | .04* |
Significant P<-05
Discussion
The goal of a rehabilitation program for patients with LBP is often based on an ability to regain neuromuscular control of the TrA, in conjunction with other segmental stabilizers such as the multifidus. This treatment is the recommended plan for “stabilization” classification of LBP patients who may have poor motor control especially during dynamic tasks. These patients are typically young, have increased flexibility and experience recurrent episodes of LBP. On examination, there is typically a positive prone instability test37 or other provocative maneuvers that amplify abnormal motion in the spine. These individuals often present with subacute symptoms and may function at a relatively high level despite ongoing or recurrent LBP.
The TrA activation ratio has been proposed as an index to determine the ability of the local musculature to stabilize the spine.29,32,38 There is a preponderance of literature that has utilized ultrasound imaging to examine the function of the TrA reporting either muscle thickness during contraction39,40 or the difference in thickness during contraction compared to a resting state.41 The TrA activation ratio compares the muscle thickness during contraction to the thickness during a resting state in a similar manner to the method that reports strength measures as normalized to body weight. Although the terminology of “activation” ratio implies a neuromuscular influence, ultrasound imagining is only able to measure cross sectional thickness of the muscle rather than a true measure of the reactivity or excitability of the specific muscle being examined. Changes in thickness are thought to be representative of increased muscle activation.29,42 Although the TrA activation ratio seems to be the most consistent and representative measure, normative data for the TrA activation ratio in both normals and individuals with LBP is lacking.43
Average TrA activation ratio during the ADIM for both groups prior to the intervention was 1.58. This ratio seems low compared to a previous study by Teyhen et al34 who observed TrA activation ratios of approximately 2.0 during the ADIM. However that study used active duty soldiers with non-specific LBP and utilized ultrasound imaging for biofeedback during the testing.34 The TrA activation ratio observed in the present study was consistent with the values reported by Kiesel et al.44 for those with stabilization classification LBP where there was a 50% increase in thickness during contraction.
The authors of the current study examined a series of exercises performed in two different modes in order to determine which exercises had the greatest effect on changes in thickness of the deep spinal stabilizers. The rehabilitative exercises using the sling based therapy resulted in the highest value in TrA activation ratio of the dynamic exercises that were examined, but only in the most challenging exercise condition. As documented by other investigators,34,42 the authors also found that the ADIM in the hook lying position was an effective method to activate the TrA. This static task may contribute to the initial retraining of the neuromuscular control, however, the most complex task, bridge with hip abduction with sling support comparatively resulted in a thickness change in the TrA, without volitional contraction of the abdominal musculature. Since the role of local stabilizers is reflexive in nature, the use of exercises, which activate these muscles, without conscious contraction, may translate to other functional activities.
The use of unstable surfaces for exercise training and rehabilitation has been hypothesized to challenge the motor control system more than a stable surface and therefore increase the contraction speed, intensity and muscle activity levels of the stabilizers of the spine.45–47 Using unstable surfaces also improves the coordination of neuro-muscular reflexes reaction responses in movement.48 Vera-Garcia et al.45 found that doing curl-ups on a labile surface challenged the motor control system which increased abdominal muscle activity and co-activation because of the increased demand on the stabilizing muscles. They found that this increase in activation of these muscles would challenge the endurance capacities which would lead to a better training approach although the exercise also recruited the global muscles rather than just the spinal stabilizers.45 Although their study showed evidence that the use of labile surfaces is beneficial, the research still has mixed results on whether those exercises better results than traditional exercise.49,50
A large percentage of the participants were able to perform all levels of the traditional (75%) and sling (88%) bridging progression. Completion of an exercise, however does not necessarily translate into an ability to concurrently stabilize the spine during the task. The exercise progressions that were chosen for this study were thought to be equal tasks that could be comparable in terms of difficulty and muscular demand. The clinician's goal with exercise intervention is to find the most challenging exercise level that patients perform correctly, without causing pain. Both progressions were nearly identical in terms of limb positions and movements. However, the sling exercise group had an unstable surface in every level. The authors believe that this factor contributed to the increased muscular demands in this group compared to the traditional group, particularly to maintain balance and alignment during the exercise. Furthermore, a higher percentage of subjects in the sling exercise group were able to complete all levels of progression suggesting that sling exercise programs provide an alternative exercise modality in patients with LBP.
A limitation of this study was the individuals with LBP who met stabilization classification criteria were not actively seeking medical care for their pain. Although, subjects in the present study did demonstrate a level of dysfunction as measured by the Oswestry and Fear Avoidance Beliefs Questionnaire (FABQ) self report measures, it is possible that individuals with greater dysfunction may have TrA activation ratios that are different with this exercise progression. Additionally results for other exercise progressions on stable or unstable surfaces (i.e. side-bridge or front plank) are unknown. Additional research is necessary to determine the contribution of sling exercise therapy in acute muscle activation as well its effect on long term patient oriented outcomes.
Conclusions
Activation of the TrA is a commonly used in rehabilitation exercise because of its ability to actively stiffen the spine,16,51–53 maintain safe spinal orientation prior to movement,25, 54,55 and control shearing forces on the spine.52 Both types of exercise that were studied in this investigation were capable of recruiting the TrA. However, the results of this investigation indicate that sling based exercise is equivalent to traditional mat based exercise in increasing the TrA activation ratio. Our findings further suggest that individuals with LBP may be better able to recruit the TrA during the more complex sling based task. Clinically, sling-based therapy can be used to train the neuromuscular system of the deep spinal stabilizers in subjects with low back pain.
ACKNOWLEDGEMENTS
Redcord, AS provided the exercise equipment necessary for this study.
Footnotes
Trial Registration: NCT01015846
REFERENCES
- 1. Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from US national surveys, 2002. Spine. 2006;31(23):2724. [DOI] [PubMed] [Google Scholar]
- 2. Abenhaim L, Rossignol M, Gobeille D, Bonvalot Y, Fines P, Scott S. The prognostic consequences in the making of the initial medical diagnosis of work-related back injuries. Spine. 1995;20(7):791–795 [DOI] [PubMed] [Google Scholar]
- 3. Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther. 1995;75(6):470–485; discussion 485-479 [DOI] [PubMed] [Google Scholar]
- 4. Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007;37(6):290–302 [DOI] [PubMed] [Google Scholar]
- 5. Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005;86(9):1753–1762 [DOI] [PubMed] [Google Scholar]
- 6. Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: a randomized clinical trial. Spine. 2003;28(13):1363–1371 [DOI] [PubMed] [Google Scholar]
- 7. O'Sullivan P. Classification of lumbopelvic pain disorders–why is it essential for management? Man Ther. 2006;11(3):169–170 [DOI] [PubMed] [Google Scholar]
- 8. Nachemson ALF. Lumbar spine instability: a critical update and symposium summary. Spine. 1985;10(3):290. [PubMed] [Google Scholar]
- 9. Dupuis P, Yong-Hing K, Cassidy D, Kirkaldy-Willis W. Radiological diagnosis of degenerative spinal instability. Spine. 1985;10(3):262–276 [DOI] [PubMed] [Google Scholar]
- 10. Gardner-Morse M, Stokes IAF, Laible JP. Role of muscles in lumbar spine stability in maximum extension efforts. Jour Ortho Res. 1995;13(5):802–808 [DOI] [PubMed] [Google Scholar]
- 11. Strohl KP, Mead J, Banzett RB, Loring SH, Kosch PC. Regional differences in abdominal muscle activity during various maneuvers in humans. Journal of Applied Physiology. 1981;51(6):1471–1476 [DOI] [PubMed] [Google Scholar]
- 12. Goldman JM, Lehr RP, Millar AB, Silver JR. An electromyographic study of the abdominal muscles during postural and respiratory manoeuvres. Journal of Neurology, Neurosurgery & Psychiatry. 1987;50(7):866–869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. De Troyer A, Estenne M, Ninane V, Van Gansbeke D, Gorini M. Transversus abdominis muscle function in humans. J Appl Physio. 1990;68(3):1010–1016 [DOI] [PubMed] [Google Scholar]
- 14. Urquhart DM, Hodges PW, Allen TJ, Story IH. Abdominal muscle recruitment during a range of voluntary exercises. Man Ther. 2005;10(2):144–153 [DOI] [PubMed] [Google Scholar]
- 15. Lacôte M, Thomas D, Thomas J. Clinical evaluation of muscle function. Churchill Livingstone; 1987 [Google Scholar]
- 16. Richardson C. Therapeutic exercise for spinal segmental stabilization in low back pain. Churchill Livingstone; Edinburgh; 1999 [Google Scholar]
- 17. O'Sullivan PB, Phyty DM, Twomey LT, Allison GT. Evaluation of Specific Stabilizing Exercise in the Treatment of Chronic Low Back Pain With Radiologic Diagnosis of Spondylolysis or Spondylolisthesis. Spine. 1997;22(24):2959. [DOI] [PubMed] [Google Scholar]
- 18. Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine. 1996;21(23):2763. [DOI] [PubMed] [Google Scholar]
- 19. O'Sullivan P, Twomey L, Allison G, Sinclair J, Miller K. Altered patterns of abdominal muscle activation in patients with chronic low back pain. Aust J Physiother. 1997;43(2):91–98 [DOI] [PubMed] [Google Scholar]
- 20. Richardson CA, Jull GA. Muscle control-pain control. What exercises would you prescribe? Man Ther. 1995;1(1):2–10 [DOI] [PubMed] [Google Scholar]
- 21. Danneels LA, Vanderstraeten GG, Cambier DC, et al. Effects of three different training modalities on the cross sectional area of the lumbar multifidus muscle in patients with chronic low back pain. BASM. 2001:186–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Richardson CA, Snijders CJ, Hides JA, Damen L, Pas MS, Storm J. The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine. 2002;27(4):399. [DOI] [PubMed] [Google Scholar]
- 23. Saal JA. Dynamic muscular stabilization in the nonoperative treatment of lumbar pain syndromes. Orthop Rev. 1990;19(8):691–700 [PubMed] [Google Scholar]
- 24. Hides JA, MphtySt BP, Jull GA, Mphty F, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine. 2001;26(11):e243. [DOI] [PubMed] [Google Scholar]
- 25. Hodges P, Cresswell A, Thorstensson A. Preparatory trunk motion accompanies rapid upper limb movement. Experimental Brain Research. 1999;124(1):69–79 [DOI] [PubMed] [Google Scholar]
- 26. Ljunggren AE, Weber H, Kogstad O, Thom E, Kirkesola G. Effect of exercise on sick leave due to low back pain: a randomized, comparative, long-term study. Spine. 1997;22(14):1610. [DOI] [PubMed] [Google Scholar]
- 27. Stuge B, Laerum E, Kirkesola G, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a randomized controlled trial. Spine. February 15 2004;29(4):351–359 [DOI] [PubMed] [Google Scholar]
- 28. Stuge B, Veierod MB, Laerum E, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a two-year follow-up of a randomized clinical trial. Spine. May 15 2004;29(10):E197–203 [DOI] [PubMed] [Google Scholar]
- 29. Hodges PW, Pengel LH, Herbert RD, Gandevia SC. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve. 2003;27(6):682–692 [DOI] [PubMed] [Google Scholar]
- 30. McMeeken JM, Beith ID, Newham DJ, Milligan P, Critchley DJ. The relationship between EMG and change in thickness of transversus abdominis. Clinical Biomechanics. 2004;19(4):337–342 [DOI] [PubMed] [Google Scholar]
- 31. Kermode F. Benefits of utilising real-time ultrasound imaging in the rehabilitation of the lumbar spine stabilising muscles following low back injury in the elite athlete -a single case study. Physical Therapy in Sport. 2004;5(1):13–16 [Google Scholar]
- 32. Teyhen DS, Rieger JL, Westrick RB, Miller AC, Molloy JM, Childs JD. Changes in deep abdominal muscle thickness during common trunk-strengthening exercises using ultrasound imaging. J Orthop Sports Phys Ther. 2008;38(10):596. [DOI] [PubMed] [Google Scholar]
- 33. Hides JA, Richardson CA, Jull GA. Magnetic resonance imaging and ultrasonography of the lumbar multifidus muscle: comparison of two different modalities. Spine. 1995;20(1):54. [DOI] [PubMed] [Google Scholar]
- 34. Teyhen DS, Miltenberger CE, Deiters HM, et al. The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J Orthop Sports Phys Ther. 2005;35(6):346–355 [DOI] [PubMed] [Google Scholar]
- 35. Teyhen DS, Gill NW, Whittaker JL, Henry SM, Hides JA, Hodges P. Rehabilitative ultrasound imaging of the abdominal muscles. J Orthop Sports Phys Ther. 2007;37(8):450–466 [DOI] [PubMed] [Google Scholar]
- 36. Hides JA, Miokovic T, Belavý DL, Stanton WR, Richardson CA. Ultrasound imaging assessment of abdominal muscle function during drawing-in of the abdominal wall: an intrarater reliability study. J Orthop Sports Phys Ther. 2007;37(8):480. [DOI] [PubMed] [Google Scholar]
- 37. Fritz JM, Childs JD, Flynn TW. Pragmatic application of a clinical prediction rule in primary care to identify patients with low back pain with a good prognosis following a brief spinal manipulation intervention. BMC Fam Pract. 2005;6(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kiesel KB, Uhl T, Underwood FB, Nitz AJ. Rehabilitative ultrasound measurement of select trunk muscle activation during induced pain. Man Ther. 2008;13(2):132–138 [DOI] [PubMed] [Google Scholar]
- 39. Koppenhaver SL, Hebert JJ, Fritz JM, Parent EC, Teyhen DS, Magel JS. Reliability of rehabilitative ultrasound imaging of the transversus abdominis and lumbar multifidus muscles. Arch Phys Med Rehabil. 2009;90(1):87–94 [DOI] [PubMed] [Google Scholar]
- 40. Mannion AF, Pulkovski N, Gubler D, et al. Muscle thickness changes during abdominal hollowing: an assessment of between-day measurement error in controls and patients with chronic low back pain. European Spine Journal: Official Publication Of The European Spine Society, The European Spinal Deformity Society, And The European Section Of The Cervical Spine Research Society. 2008;17(4):494–501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hides JA, Wong I, Wilson SJ, Belavy DL, Richardson CA. Assessment of abdominal muscle function during a simulated unilateral weight-bearing task using ultrasound imaging. J Orthop Sports Phys Ther. 2007;37(8):467–471 [DOI] [PubMed] [Google Scholar]
- 42. Hides J, Wilson S, Stanton W, et al. An MRI investigation into the function of the transversus abdominis muscle during “drawing-in” of the abdominal wall. Spine. 2006;31(6):E175. [DOI] [PubMed] [Google Scholar]
- 43. Beazell JR, Grindstaff TL, Magrum EM, Cullay M, Shen FH, Hart JM. Abdominal muscle recruitment patterns during an abdominal drawing-in maneuver in individuals with and without low back pain using ultrasound imaging. Research in Sports Medicine. In Press [DOI] [PubMed] [Google Scholar]
- 44. Kiesel KB, Underwood FB, Mattacola CG, Nitz AJ, Malone TR. A comparison of select trunk muscle thickness change between subjects with low back pain classified in the treatment-based classification system and asymptomatic controls. J Orthop Sports Phys Ther. 2007;37(10):596–607 [DOI] [PubMed] [Google Scholar]
- 45. Vera-Garcia FJ, Grenier SG, McGill SM. Abdominal muscle response during curl-ups on both stable and labile surfaces. Physical Therapy. 2000;80(6):564. [PubMed] [Google Scholar]
- 46. McGill SM. Low back exercises: evidence for improving exercise regimens. Physical Therapy. 1998;78(7):754. [DOI] [PubMed] [Google Scholar]
- 47. Riemann BL, Myers JB, Lephart SM. Comparison of the ankle, knee, hip, and trunk corrective action shown during single-leg stance on firm, foam, and multiaxial surfaces. Arch Phys Med and Rehabil. 2003;84(1):90–95 [DOI] [PubMed] [Google Scholar]
- 48. Liebenson C. Spinal stabilization training: the therapeutic alternative to weight training. Journal of Bodywork & Movement Therapies. 1997;1(2):87–90 [Google Scholar]
- 49. Lehman GJ, Gordon T, Langley J, Pemrose P, Tregaskis S. Replacing a Swiss ball for an exercise bench causes variable changes in trunk muscle activity during upper limb strength exercises. Dynamic Medicine. 2005;4(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lehman GJ, Hoda W, Oliver S. Trunk muscle activity during bridging exercises on and off a Swissball. Chiropractic & Osteopathy. 2005;13(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. McGill SM, Norman RW. Reassessment of the role of intra-abdominal pressure in spinal compression. Ergonomics. 1987;30(11):1565–1588 [DOI] [PubMed] [Google Scholar]
- 52. Gracovetsky S, Farfan H, Helleur C. The abdominal mechanism. Spine. 1985;10(4):317–324 [DOI] [PubMed] [Google Scholar]
- 53. Bergmark A. Stability of the lumbar spine. A study in mechanical engineering. Acta Orthop Scand Suppl. 1989;230:1–54 [DOI] [PubMed] [Google Scholar]
- 54. Cresswell AG, Oddsson L, Thorstensson A. The influence of sudden perturbations on trunk muscle activity and intra-abdominal pressure while standing. Experimental Brain Research. 1994;98(2):336–341 [DOI] [PubMed] [Google Scholar]
- 55. Hodges PW, Cresswell AG, Daggfeldt K, Thorstensson A. Three dimensional preparatory trunk motion precedes asymmetrical upper limb movement. Gait & Posture. 2000;11(2):92–101 [DOI] [PubMed] [Google Scholar]