Abstract
Objectives
The purpose of this study is to clarify causal relations between coping strategies and burnout in family caregivers of frail elders in Japan.
Methods
Baseline and 1-year follow-up interviews were conducted with 546 caregivers living in suburban Tokyo. Using newly refined measures, five coping strategies of caregivers (Keeping Their Own Pace, Positive Acceptance of Caregiving Role, Diversion, Informal Support Seeking, and Formal Support Seeking), and caregiver burnout were measured, as well as several confounding factors.
Results
After controlling for these confounding factors, results of cross-lagged effects modelling showed that adoption of a Diversion coping strategy decreased caregiver burnout, while increases in burnout decreased caregiver Positive Acceptance of Caregiving Role.
Conclusions
The beneficial effect of an Adaptive Avoidance Coping strategy, Diversion, on caregiver mental health was confirmed in this two-wave longitudinal study. The mechanism by which Diversion appears to work is by containing caregiving stressors from completely spilling over into caregivers’ personal lives. In addition, we also show that preventing a decline in caregiver mental health (i.e. an increase in burnout) allowed caregivers to more easily embrace the caregiving role and, as a result, elder care-recipients were better positioned to receive high quality care.
Keywords: caregiver mental health, caregiving stressors, adaptive avoidance coping
Introduction
While the aged population has been growing among most developed countries in recent years, the number of frail older adults and their family caregivers has also been on the rise. Caregiving for elder relatives is becoming increasingly common, although most international studies show that the risk of mental disorder among family members who routinely provide such care is higher than among those who do not (Dura, Stukenburg, & Kiecolt-Glaser, 1990; Hoyert & Seltzer, 1992; Morimoto, Schreiner, & Asano, 2001; Schreiner & Morimoto, 2003). In addition, at least one longitudinal study showed that increases in behavioural problems of frail elders were likely to predict increases in caregiver role overload (Gaugler, Davy, Pearlin, & Zarit, 2000). Yet, we do not yet completely understand how the adoption of different coping strategies can help ameliorate some of the burdens of caregiving.
It is important to understand how caregivers maintain their own mental health during the caregiving tenure in order to help tailor ameliorative social welfare policies or education programs. In this article, we move towards a greater understanding of some of the causal pathways between coping strategies and burnout in family caregivers of frail elders in Japan, and suggest how the findings might be applicable elsewhere.
Types of coping strategies
Pearlin, Mullan, Semple, and Skaff (1990) considered informal family caregiving to involve chronic role strain for caregivers. However, adopting coping strategies may be protective of at least some of its detrimental effects. Coping strategies have classically been divided into two large categories (Lazarus & Folkman, 1984): problem-focused coping – efforts aimed at managing or altering the source of distress; and emotion-focused coping – efforts directed towards regulating the individual’s emotional response to the problem. Billings and Moos (1984) introduced a third coping strategy: appraisal-focused coping – efforts to define and redefine the personal meaning of the situation. In caregiving situations, three categories of coping strategies which were developed by Pearlin and his colleagues (management of situation, management of distress and management of meaning) roughly correspond to the three categories of coping strategies described above, respectively (Pearlin & Schooler, 1978; Pearlin et al., 1990).
However, two problems with existing measures of different coping strategies have been identified. First, although the measures developed by Lazarus and Billings are presumed to be applicable to general types of stressors, they may not be applicable to particular types of stressors (Stone, Greenberg, Kennedy-Moore, & Newman, 1991). This means that measurement scales developed and used for general situations (e.g. Way of Coping; Lazarus & Folkman, 1984) may not be applicable or sensitive to particular stress-inducing situations such as informal family caregiving. In the caregiving situation, the persistent nature of stressors arising from physical disability and cognitive impairment of elders is very different from stressors arising from transient life events. Second, existing measures of emotion-focused coping strategies were often criticized for being contaminated with emotional stress responses such as unrealistic wishfulness or self-blame (Stanton, Danoff-Burg, Cameronk, & Ellis, 1994). That is, although the primary coping strategy should be active management of the stress situation, these measures included items indicating passive response from the stressful situation. Although there is a well-known coping scale developed for caregiving situations (Pearlin & Schooler, 1978; Pearlin et al., 1990), it does not appear to be free from the confounding content of emotional stress responses. To advance our study of the caregiving stress process, a new coping scale relatively free of contamination from emotional stress responses is needed.
Effects of coping strategies in cross-sectional studies
To summarize the effects of coping strategies on the mental health of family caregivers of frail elders, strategies described in previous studies may be grouped into these three categories described above (problem-focused coping, emotion-focused coping and appraisal-focused coping). Although many studies have examined the relationships between coping strategies and caregiver mental health, most are based on cross-sectional rather than longitudinal designs. In most cross-sectional studies, caregiver mental health is negatively associated with the adoption of emotion-focused coping strategies (Haley, Levine, Brown, & Bartolucci, 1987; Hinrichsen & Niedrehe, 1994; Kramer, 1993; Pratt, Schmall, Wright, & Cleland, 1985; Pruchno & Resch, 1989; M.P. Quayhagen & M. Quayhagen, 1988; Wake, Yatomi, Nakatani, & Shimizu, 1994; Wake, 1996; Wright, Lund, Caserta, & Pratt, 1991; Wallhagen, 1993; Williamson & Schulz, 1993; Knight, Silverstain, McCallum, & Fox, 2000), and positively associated with the adoption of appraisal-focused coping strategies (Borden, 1991; Haley et al., 1987; Hinrichsen & Niedrehe, 1994; Pratt et al., 1985; Pruchno & Resch, 1989; M.P. Quayhagen & M. Quayhagen, 1988; Wake et al., 1994; Wright et al., 1991). The relationships between caregiver mental health and the adoption of problem-focused coping strategies are surprisingly inconsistent. Some find a positive relationship (Haley et al., 1987; Kramer, 1993; Knight et al., 2000; Pratt et al., 1985; Pruchno & Resch, 1989; M.P. Quayhagen &M. Quayhagen, 1988; Wright et al., 1991), while others find a negative (Hinrichsen & Niedrehe, 1994; Wake, 1996) or no relationship at all (Borden, 1991; Vitaliano, Russo, Young, Teri, & Maiuro, 1991; Wake et al., 1994).
Effects of coping strategies in longitudinal studies
Although many otherwise excellent cross-sectional studies have been conducted in this area, they are usually not able to adequately explain causality between caregiver coping strategies and caregiver mental health. To determine causality, longitudinal designs are needed. For example, Winslow (1997) found no significant causal relationships between appraisal-focused coping and anxiety among family caregivers of persons with dementia over 1-year period. Among daughters providing care for their elderly parents over an 18-month period, Li, Selzer and Greenberg (1999) found that problem-focused coping decreased depression symptoms, and emotion-focused coping increased depression symptoms. Kinny, Ishler, Pargament and Cavanaugh (2003) did not find any effective coping strategies among caregivers for spouses with dementia over a two-month period, though they found emotion-focused coping and a religion-based coping strategy called ‘collaborative coping’ increased depression significantly. Because there are still relatively few studies of the causal relationships between caregiver coping strategies and caregiver mental health – especially in the context of frail elders – more research using longitudinal designs is needed in order to more fully understand the nature of these relationships.
Purpose of this study
Okabayashi, Sugisawa, Takanashi, Nakatani and Shibata (1999) developed an original coping scale consisting of actual behavioural content in caregiving situations and that eliminated emotional stress response items. This coping scale has five first-order factors which were consolidated into three second-order factors (Adaptive Avoidance, Approach, and Support Seeking). While Approach Coping (Positive Acceptance of Caregiving Role) corresponded to appraisal-focused coping, and Support Seeking Coping (Informal Support Seeking and Formal Support Seeking) corresponded to a part of problem-focused coping, Adaptive Avoidance Coping (Diversion and Keeping Their Own Pace) did not seem to correspond to any coping strategies in the existing literature. Adaptive Avoidance Coping means the behavioural (not emotional) effort to avoid becoming too involved with the caregiving role in order to secure their own life and health. Adaptive Avoidance Coping should be differentiated from emotion-focused coping, which is sometimes called ‘avoidant coping’. As mentioned earlier, emotion-focused coping does not mean the effort to avoid being involved in caregiving, rather, it is a part of the emotional stress response of being reluctantly involved in the caregiving role. We tried to re-conceptualize this approach-avoidance dimension in the proper sense of the word, that is, whether caregivers try to approach or avoid a chronic role obligation such as caregiving.
In this study, using longitudinal data over a 1-year period, we examine reciprocal causal relationships between coping strategies and one dimension of mental health, burnout, among family caregivers of frail elders in Japan. The main purpose of this study is to specifically clarify which coping strategy has a beneficial effect on caregiver mental health. This information could be of practical value for family caregivers to ensure optimal mental health during their caregiving tenure, in addition to helping shape public policy and debate in this area.
Though we examine all 1-year cross-lagged effects between coping strategies and caregiver burnout, we can construct the following three main hypotheses based on our previous cross-sectional findings (Okabayashi et al., 1999; Okabayashi et al., 2003), and other findings reviewed above.
(1) Adaptive Avoidance Coping has a beneficial effect on caregiver mental health
Using our original coping scale, we found that a strategy of ‘Keeping Their Own Pace’ decreased caregivers’ burnout directly, while a strategy of ‘Diversion’ decreased it indirectly through caregiving captivity, which was a measure of the degree and intensity of the caregiver’s involvement in the caregiving role (Okabayashi et al., 1999). We also found stress-buffering effects of Keeping Their Own Pace, which buffered the detrimental effects of caregiving captivity on burnout (Okabayashi et al., 2003). These studies showed that the two coping strategies of Adaptive Avoidance Coping – Keeping Their Own Pace and Diversion – had beneficial effects on caregiver mental health. Thus, it is hypothesized that adopting these coping strategies has a positive effect on caregiver mental health.
(2) Deteriorating caregiver mental health increases Support Seeking Coping
Although findings from other literature we have reviewed so far showed an inconsistent relationship between problem-focused coping – a part of which corresponded to our Support Seeking Coping – and caregiver mental health, our previous work (Okabayashi et al., 1999) showed that contrary to intuition, Support Seeking Coping (especially Informal Support Seeking) had a negative relationship with caregiver mental health. It should not be interpreted to mean that seeking more support worsens caregiver mental health, but that exhausted caregivers desire more informal support. Thus, in terms of Support Seeking Coping (especially Informal Support Seeking) it is hypothesized that more exhausted caregivers seek more social support.
(3) Approach Coping has a negative effect on caregiver mental health
Most literature we have reviewed showed appraisal-focused coping, which corresponded to our Approach Coping, had a beneficial effect on caregiver mental health. However, most findings of beneficial effects of appraisal-focused coping on caregiver mental health might be artifactual. There are two reasons to assume so. First, possible confounding factors might not be controlled for when examining these relationships. In our previous cross-sectional study (Okabayashi et al., 1999), we found an indirect detrimental effect of Approach Coping on caregiver mental health through caregiving captivity. However, because there was a negative correlation between Approach Coping and caregiver burnout, we might have misinterpreted it as direct beneficial effect unless we estimated its indirect detrimental effect through caregiving captivity simultaneously. Second, the direction of causation might be misinterpreted. That is, it should not be interpreted to mean that this coping strategy has a beneficial effect on caregiver mental health, rather that caregiver mental health may have some effect on this coping strategy. Although we cannot conclude which alternative is the most likely, according to our previous work we tentatively hypothesize that adopting this coping strategy causes caregivers to be too involved in caregiving and thus to become exhausted over the caregiving period.
Methods
Participants
To screen family caregivers of frail elders, we conducted a mail survey in February-March 1996 of family members of all elders aged 65 or over living in a Tokyo suburb (N = 21,567). If family members reported that elders had at least one physical disability among six items of activities of daily living (Shimizu, 1996), or at least one cognitive impairment among eight items of dementia symptoms (Homma, 1996), they were considered ‘frail’ and their caregivers were potential participants for the baseline survey. From 20,350 responders (response rate 94.4%), we identified 1379 frail elders. According to this definition, the frailty rate of this sample was 6.8%, but no widely available statistic uses the same definition. However, using a slightly different definition, the rate of frail persons eligible for care insurance, the frailty rate of this Japanese city (11.9%) was about the same as the national rate (13.1%) in 2001 (Sugisawa, 2005). Interviewers visited homes and conducted structured baseline interviews in Japanese with family caregivers in 1996. The number of completed responses was 941 (completion rate 68.2%). Of these, 834 responses from primary caregivers engaged in caregiving were used to develop the new coping scale. (For further details see Okabayashi et al., 1999)
A 1-year follow-up survey was conducted in 1997. Because 224 of the original 941 elderly were either hospitalized (60), in a nursing home (43), or deceased (121) at follow-up, these caregivers were not eligible for the follow-up survey. An additional 82 were otherwise lost to follow-up, so the 1-year survey was successfully completed with 635 caregivers (completion rate 88.6%). For this article, we used data from 546 caregivers with no missing responses to the variables under study.
Measurement
Coping strategies
We selected valid items from existing scales, and created additional ones by abstracting free descriptive responses from family caregivers of stroke patients from a previous study (Wake, 1993, 1996; Department of Health Sociology in Tokyo Metropolitan Institute of Gerontology, 1994). Particular attention was paid to those items consisting of actual behavioural content in caregiving situations that were, to the best we could ascertain, free from emotional stress responses. Finally, 20 items were chosen. The leading sentence of the question using these items was: ‘How well have you done each of the following things while caregiving for the elderly?’ Each item was rated from 1 (not at all) to 4 (well done). After preliminary explanatory factor analysis and a first-order factor analysis, a second-order factor model with five first-order factors was examined with 834 responses for 16 items selected from these 20 items of the initial survey. (See Appendix for survey items and factor structure. For further details see Okabayashi et al., 1999).
Five first-order factors of caregiver coping strategies were labelled as follows: (a) the first factor, Keeping Their Own Pace, was a coping strategy of keeping a balance between their own health or life style and their caregiving responsibilities; (b) second, Positive Acceptance of Caregiving Role, was a strategy to give the best care possible to the care-recipient in accord with a positive feeling about doing so; (c) third, Diversion, was a strategy to retain time for themselves in order to meet their friends or do other things they might want to do; (d) fourth, Informal Support Seeking, was a strategy to seek instrumental or emotional support from other family members and friends; and (e) the fifth factor, Formal Support Seeking, was a strategy to seek informational or instrumental support from professionals (e.g. physicians, nurses, or staff in public offices).
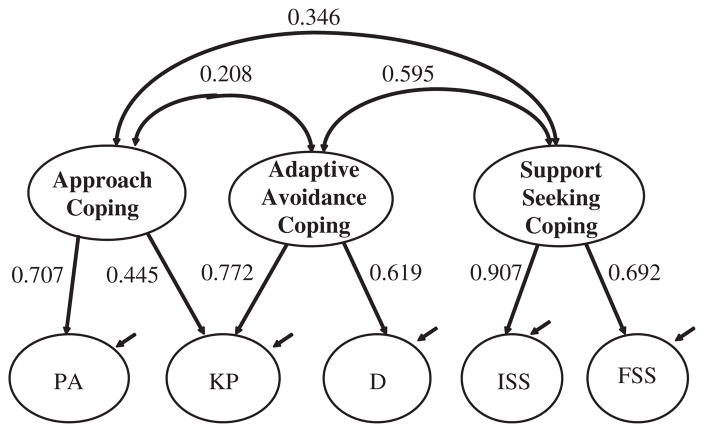
These five first-order factors were organized into three second-order factors: (a) Approach Coping, where caregivers approach and embrace potentially stressful situations and take the caregiving role spontaneously, consists of the Positive Acceptance of the Caregiving Role first-order factor; (b) Support Seeking Coping, where caregivers seek support from others, consists of the Informal Support Seeking and Formal Support Seeking factors; and (c) Adaptive Avoidance Coping, where caregivers avoid being involved with caregiving situations in order to secure their own life and health, consists of the Diversion and Keeping Their Own Pace factors. One path was added from Approach Coping to Keeping Their Own Pace to improve the goodness of fit of model. Also, this adjustment suggests that it is important to keep a balance between approach to and avoidance of the caregiving situation in order to cope with chronic role strain in the caregiving situation. In addition, the variance of Approach Coping was fixed to one (‘1.0’) to identify the model and the error variance of Positive Acceptance of Caregiving Role was constrained to be positive in order to avoid negative error variances. Finally, this model showed satisfactory goodness of fit indices (χ2(96, N = 834) = 417.912, p < 0.001; GFI = 0.925; AGFI = 0.894; RMSEA = 0.0634).
In analyses of cross-lagged effects of this study, observed scores in each item of five first -order factors were used. The α coefficients of these five scales ranged from 0.622 to 0.738 at the initial survey, and from 0.536 to 0.731 at the follow-up survey.
Burnout
We used a Burnout scale for family caregivers adapted by Nakatani (1992, 1996) from the Maslach Burnout Inventory (Maslach & Jackson, 1981). Nakatani revised each of Maslach’s items – originally developed in English for human service professionals – to Japanese items applicable for family caregivers of frail elders. Although the Maslach version was originally considered to contain three subscales, emotional exhaustion; depersonalization and personal accomplishment, there were low correlations between personal accomplishment and the other two subscales in the revised family caregiving version. This suggested that personal accomplishment should not be considered an element of the same construct (Nakatani, 1996). Accordingly, we used only the two emotional exhaustion (eight items) and depersonalization (four items) subscales in this study. The leading sentence of the question using these items was: ‘How much do you agree with the following sentences about your feelings and situation these days?’ Each item was rated from 1 (strongly disagree) to 5 (strongly agree). In analyses of cross-lagged effects, to create a burnout latent variable, two observed variables of emotional exhaustion and depersonalization subscales were used, each of which were calculated by dividing the sum of item scores by the number of items in each scale. The α coefficients of the emotional exhaustion and depersonalization subscales were 0.859 and 0.644 at the initial survey, and 0.876 and 0.655 at follow-up, respectively.
Control variables
The degrees of cognitive impairment and/or physical disability of care-recipient were considered caregiving stressors. Degree of cognitive impairment was measured by a caregiver checklist of dementia symptoms developed by Homma (1996). It consists of 16 items along the lines of: ‘Does the elder sometimes say that he or she did not have a meal after just having it?’ Caregiver responses were scored 1 (yes) or 0 (no). The range of total scores was from 0 to 16, with higher scores indicating greater cognitive impairment. The α coefficient of this scale at baseline was 0.869. Degree of physical disability of the care-recipient was measured by a caregiver rating scale developed at the Tokyo Metropolitan Institute of Gerontology (Shimizu, 1996). This activity scale consists of six items: walking, eating, dressing, bathing, toileting and a global evaluation of activities of daily living. Items were scored 1 (the elder needs some help to do it) or 0 (the elder can do it him or herself). The range of total scores was from 0 to 6, with higher scores indicating more serious physical disability. The α coefficient of this scale at baseline was 0.759. Demographic factors and socioeconomic status at the initial survey were considered as other control variables. Caregiver age and relationship to the care-recipient were also obtained. The range of caregiver age was 27–92. In terms of their relationships, five dummy variables were created with ‘wives’ as the reference category for ‘husbands’, ‘sons’, ‘daughters’, ‘daughters-in-law’, and ‘others’. Caregiver education was measured ordinally as the highest level of schooling attained, scored 1 (no educational experience), 2 (elementary or junior high school: from 6 to 9 years), 3 (high school: 12 years), 4 (junior college: 14 years), 5 (university or graduate school: 16 years or over). Caregiver satisfaction with their own economic situation was measured ordinally with a global satisfaction item scored 1 (very insufficient), 2 (somewhat insufficient), 3 (moderate), 4 (somewhat sufficient) and 5 (very sufficient).
Models of analysis
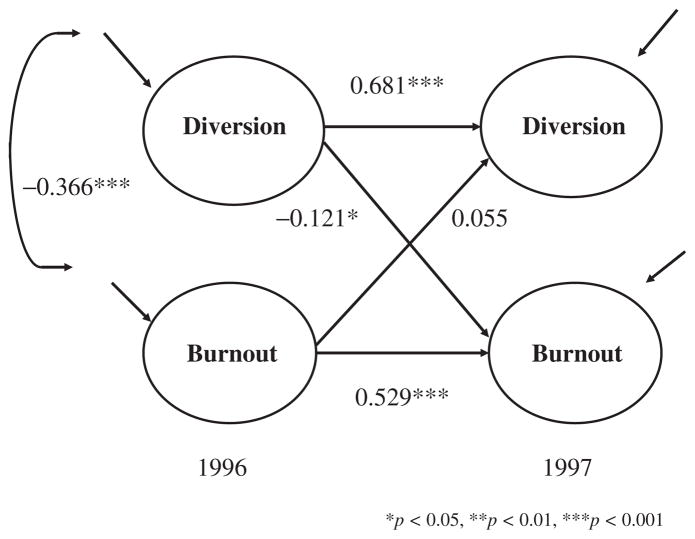
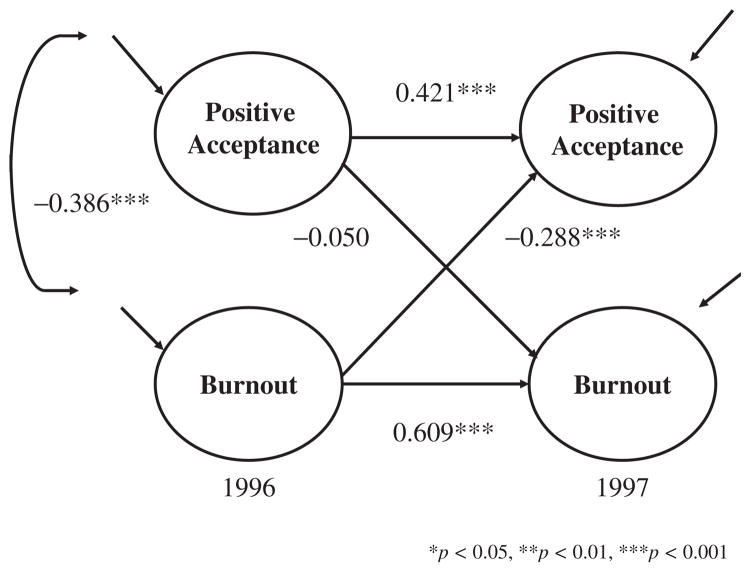
Using longitudinal data, we are able to analyse causal relations between five caregiver coping strategies and burnout. In this longitudinal study, a cross-lagged effects model using structural equation modelling with latent variables (Finkel, 1995) was used to examine reciprocal causal relations between coping strategies and burnout among caregivers (Figures 1 and 2).
Figure 1.
Cross-lagged effects between Diversion and Burnout.
Figure 2.
Cross-lagged effects between Positive Acceptance of Caregiving Role and Burnout.
In this model, the coping strategies latent variables consisted of items that were components of each of the five coping strategies factors described above. The burnout latent score among caregivers consisted of two scores of the two subscales, emotional exhaustion and depersonalization, described above. Because the measurement model at the initial survey and at the follow-up survey was assumed to be stable, factor loadings and error variances of observed variables were constrained to be equal at both time points (Finkel, 1995). We included error covariance parameters between the same observed variables at initial and follow-up surveys. Degree of physical disability and cognitive impairment, caregiver demographic variables and caregiver socioeconomic status variables were treated as control variables. Lisrel 8.30 was used to analyse the model.
Results
Descriptive analysis
The distribution of caregiver relationships to the elders were as follows: husbands 13.9%; wives 28.0%; sons 8.6%; daughters 28.2%; daughters-in-law 20.1%; and others 2.9%. Means and SDs of other control variables were as follows: caregiver age, M = 62.10, SD = 12.31; caregiver educational attainment, M = 3.26, SD = 0.95; and caregiver satisfaction with economic situation, M = 3.05, SD = 0.81. Means and SDs of caregiving stressors were as follows: physical disability, M = 2.99, SD = 1.87; cognitive impairment, M = 2.27, SD = 3.16.
Simple 1-year changes in coping strategies and burnout were tested using paired t-tests. Among the five coping strategies on the 1–4 scale, only the mean value of Formal Support Seeking at follow-up (M = 2.54, SD = 0.72) was significantly higher than at baseline (M = 2.48, SD = 0.72), t(545) = 2.43, p < 0.05. In terms of burnout on the 1–5 scale, the mean value of emotional exhaustion at follow-up (M = 2.33, SD = 0.82) was significantly higher than at baseline (M = 2.25, SD = 0.78), t(545) = 2.61, p < 0.01.
Cross-lagged effects
Cross-lagged effects were analysed in five models corresponding to each of the five coping strategies. In these models, all factor loadings (i.e. standardized regression coefficients from latent variables to the corresponding observed variables) of the coping strategies and burnout were over 0.40 (p < 0.001). Because there were negative variances in the emotional exhaustion subscale in three models (in the analyses of Diversion, Informal Support Seeking and Formal Support Seeking), and a negative error covariance between the observed depersonalization subscale at baseline and follow-up in one model (in the analysis of Positive Acceptance of Caregiving Role), the following adjustments were made: Negative error variances of the emotional exhaustion subscale in the analyses of these three coping strategies were fixed to the value (0.1519) that was found in the analysis of Keeping Their Own Pace; and the negative error covariance of the observed depersonalization subscale scores between the two survey administrations was constrained to be positive. As a result of these adjustments, only one unexpected result among these five models remained: a non-significant covariance of the Diversion items between the two surveys. In addition, all GFI and AGFI values of these models were above.90 and all RMSEA values were below 0.06 (Table 1). As a whole, the measurement characteristics suggest that these models are satisfactory for further analysis.
Table 1.
Causal relations between coping strategies and burnout in cross-lagged effects models (N = 546).
| Goodness of fit |
Coping T1→Coping T2 | Burnout T1→Burnout T2 | Coping T1→Burnout T2 | Burnout T1→Coping T2 | |||||
|---|---|---|---|---|---|---|---|---|---|
| df | χ2 | GFI | AGFI | RMSEA | |||||
| Keeping Their Own Pace | 93 | 245.485 | 0.957 | 0.904 | 0.054 | 0.364**a (0.339)b | 0.543*** (0.578) | −0.106 (−0.156) | −0.203 (−0.137) |
| Diversion | 58 | 181.241 | 0.967 | 0.903 | 0.058 | 0.681*** (0.677) | 0.529*** (0.559) | −0.121* (−0.112) | 0.055 (0.063) |
| Positive Acceptance of Caregiving Role | 133 | 337.157 | 0.948 | 0.901 | 0.052 | 0.421*** (0.392) | 0.609*** (0.635) | −0.050 (−0.059) | −0.288*** (−0.239) |
| Informal Support Seeking | 94 | 183.106 | 0.968 | 0.929 | 0.040 | 0.589*** (0.555) | 0.590*** (0.625) | 0.049 (0.061) | 0.020 (0.016) |
| Formal Support Seeking | 134 | 249.683 | 0.962 | 0.927 | 0.038 | 0.816*** (0.809) | 0.593*** (0.629) | 0.033 (0.040) | 0.081 (0.070) |
Notes: T1 = Initial survey. T2 = Follow-up survey.
Standardized regression coefficient.
Metric (unstandardized) coefficient.
p < 0.05,
p < 0.01,
p < 0.001.
Regression coefficients in these five cross-lagged effects model are shown in Table 1. All standardized regression coefficients of the same coping strategies latent variables and burnout from the baseline to the follow-up survey were over 0.36 (p < 0.001). This suggests that these psychological attitudes within individuals have been relatively stable over the 1-year assessment duration. Two significant cross-lagged effects were found: first, Diversion at the initial survey decreased burnout at the follow-up survey (b = −0.112, β = −0.121, p < 0.05) (Figure 1). Second, burnout at the initial survey decreased Positive Acceptance of Caregiving Role at the follow-up survey (b = −0.239, β = −0.288, p = < 0.001) (Figure 2).
Discussion
Descriptive analysis
Although about 23.8% of participants from the initial survey did not complete the follow-up because of hospitalization, institutionalization, or death of the care-recipient, the completion rates among eligible caregivers were very high at both the initial and follow-up surveys (68.2%; 88.6%). Thus, the large number of participants and relatively high completion rates in this study suggest a high degree of generalizability of the findings.
In terms of change over 1 year, the overall level of Formal Support Seeking slightly increased. The overall level of the emotional exhaustion component of burnout also slightly increased. This indicates that though these changes were relatively modest, caregivers came into greater contact with specialists such as doctors or other professional care personnel, utilized more in-home caregiving services, and they became more emotionally exhausted over time.
Cross-lagged effects
Most measurement characteristics and all goodness of fit indices showed that the five cross-lagged effects models in this study were appropriate and met satisfactory statistical assumptions. All significant positive regression coefficients between the same latent constructs of coping strategies and burnout from baseline to follow-up indicate that there is high stability of these psychological attitudes within individuals, as well as high reliability of these scales.
In terms of our three hypotheses, the first hypothesis was partly supported. That is, one of the Adaptive Avoidance Coping strategies, Diversion, decreased caregiver burnout significantly at a modest level, though another Adaptive Avoidance Coping strategy, Keeping Their Own Pace, did not show significant effects. This suggests that caregivers should take time for themselves in order to avoid becoming overwhelmed. ‘Diversion’ (See items in Table A1) means caregivers take time away from their caregiving role obligations for themselves. Caregivers employing this coping strategy attempt to keep away from the often uncontrollable nature of caregiving stressors and make personal time for themselves. As a result, it can help prevent caregivers from being overwhelmed by caregiving stressors. The effectiveness of Diversion suggested by our previous cross-sectional studies using the same baseline sample data as this study (Okabayashi et al., 1999) was confirmed in this longitudinal study.
There are many aspects of caregivers’ lives besides caregiving: parenting, working, being married, and other personal activities and responsibilities. It could be overwhelming if caregiving stressors spilled over to other aspects of their lives and interfered with other roles. A recent study of adult daughter caregivers of parents (Stephans, Townsend, Martire, & Druley, 2001) showed that one way parental care stress exerted its deleterious effects on the well-being of adult daughters was through the incompatible pressures of parent care and other roles. Farkas and Himes (1997) also suggested that family caregivers may be using outside activities such as voluntary activities as a way to relieve the stress of the caregiving tasks. ‘Diversion’ aims to carve out personal time away from the caregiving situation, thus preventing caregiving stressors from spilling over into personal time. In other words, this coping strategy is a means of compartmentalizing caregiving stressors away from other aspects of their lives. A lifestyle that regularly carves out personal time for oneself may be highly adaptive when enduring chronic stress situations such as family caregiving. This finding may be useful for designing practical interventions such as providing some kinds of supports for family caregivers.
The second hypothesis was rejected. That is, caregiver burnout did not only increase use of two strategies of Support Seeking Coping, but there were also not any reciprocal relations between these two coping strategies and caregiver burnout. Although formal and informal supports in this study did not show any beneficial effects on caregiver mental health, we have to think carefully about the situations under which social support would improve caregiver mental health. Support Seeking Coping was considered a part of problem-focused coping, which did not necessarily show beneficial effects in previous studies we have reviewed. The reason why informal and formal supports in this study were not particularly effective may be that the provision of these supports were not seen as dependable or efficacious enough for caregivers to feel comfortable taking their own time away from their frail older care-recipients. To make these supports effective, some additional conditions may be needed. One type of formal support that may be efficacious is the provision of high quality respite services to caregivers, who would otherwise have few opportunities to leave the care-recipient alone. Additional research on the conditions under which different types of social support become effective is also needed.
Finally, the third hypothesis was rejected. That is, Approach Coping (Positive Acceptance of Caregiving Role) did not have any effect on caregiver burnout. However, in the opposite causal direction, caregiver burnout suppressed adoption of an Approach Coping strategy. Caregiver burnout appears to prevent caregivers from giving care in a positive manner. That is, unless caregivers maintain their own mental health, they are less able to assume the caregiving role positively. Though most cross-sectional studies we reviewed found positive relations between appraisal-focused coping (which corresponded to Approach Coping) and mental health, the findings from the analysis of cross-lagged effects in this study show that caregiver mental health may have an effect on appraisal-focused coping, rather than appraisal-focused coping having an effect on mental health. Also, in Figure 2, we found a significant negative correlation (−0.386, p < 0.001) between Approach Coping and caregiver burnout at baseline. Without using a cross-lagged effects model for longitudinal data, we might misinterpret this correlation as a beneficial effect of Approach Coping on caregiver mental health.
In this study, one of the Adaptive Avoidance Coping strategies, Diversion, has a beneficial effect on caregiver mental health, while improving caregiver mental health urges caregivers to adopt Approach Coping. These findings suggest that there were reciprocal effects between coping strategies and burnout. Thus, to provide good care to frail elders, caregivers should maintain their own health. To do so, they may have to protect some time for themselves.
Conclusion
The purpose of this study was to clarify reciprocal relationships between coping strategies and caregiver burnout. Though it seems to be paradoxical, it is important for family caregivers to spend some portion of their own time away from caregiving obligations in order to maintain not only their own mental health but also their ability to provide high quality care for the frail elders during chronic stress periods. In other words, even if caregivers want to provide care with all due good intentions, they will not be able to do so over an enduring caregiving period without also taking care of themselves. Only if caregivers can get away from the caregiving obligation regularly and use some time for their own needs, will they be able to provide high quality care. Thus, the paradox of providing good care is confounded by the need to sometimes provide less care.
The effectiveness of one of the Adaptive Avoidance Coping strategies, Diversion, in caregiving situations may be generalized to other situations during which other chronic role strains arise. Developing a more comprehensive theory of stress and coping in these contexts (e.g. examining the effectiveness of Adaptive Avoidance Coping on continuing relationships with others in the family or on the job) may be an additional fruitful line of research.
Though our new coping scale used in this study was helpful to find a new effective coping strategy (Diversion), the effect of Diversion on burnout was relatively small, and the absolute value of the coefficient is relatively low. We have to consider that this finding is tentative. One of the reasons why the effect of Diversion on burnout was relatively small (but statistically significant) may be that the sensitivity of this scale was not sufficient for small numbers of items. Further development of this coping measure with larger numbers of items may be needed. We need further replications with similar findings to confirm the effectiveness of Adaptive Avoidance Coping.
Cultural differences in family structure and role responsibilities (e.g. the daughter-in-law role) need to be kept in mind. For example, Sugihara, Sugisawa, Nakatani, and Hougham (2004) recently found that wives and daughters-in-law among Japanese caregivers are more likely to be emotionally exhausted over a 30-month caregiving duration than their US counterparts. However, findings from international studies suggest that family caregivers, whatever their culture, may share more similarities than differences. Though there may be cultural variations in caregiving situations between different countries, and these variations may moderate the stress-coping mechanisms we discuss here, we believe that stress-coping mechanisms in chronic role strain are essentially universal. But, only by accumulating empirical findings using adequate methodologies in a variety of cultural settings we will be able to reach theoretical convergence about stress-coping mechanisms in chronic role strain situations. We hope that these findings will contribute to such an enduring effort.
Acknowledgments
This research was supported by Grant-in-Aid for Scientific Research B10410061 (Hidehiro Sugisawa, PI) and Grant-in-Aid for Encouragement of Young Scientists 09710162 (Hideki Okabayashi, PI) from the Ministry of Education, Culture, Sports, Science and Technology in Japan.
The authors would like to thank Taro Fukaya, MA; Hiroshi Shibata, MD, PhD; Harumi Sato, MA; Katsuhide Kawamoto, PhD; and Chieko Tanaka, MA for assistance with data collection and management, the research participants, and staff members of related organizations for their contributions. The first author would also like to thank the following individuals at Pennsylvania State University for commenting on earlier versions of the manuscript: Andrea S. Schreiner, PhD, MHA, BSN; Steven H. Zarit, PhD; and Michel Rovine, PhD.
Appendix
Table A1.
Five factors of coping strategies and those Itemsa.
| Coping strategies | Factor loadingsc |
|---|---|
| Keeping Their Own Pace (three items) | |
| You take care of an elderly person within your own ability avoiding being overloaded.b | 0.662 |
| You take care of your own health because it would be more trouble if you get sick. | 0.582 |
| You spend cheerfully every day without giving up your hope. | 0.638 |
| Diversion (two items) | |
| You refresh yourself by doing things you like or seeing your friends.b | 0.644 |
| You take time for yourself intentionally to avoid being tied up by caregiving. | 0.828 |
| Positive Acceptance of Caregiving Role (four items) | |
| You communicate well with an elderly person and respect his/her own feelings and intentions.b | 0.958 |
| You treat an elderly person with your whole heart. | 0.856 |
| You try to meet a request from an elderly person as soon as possible. | 0.794 |
| You take care of an elderly person as hard as possible. | 0.669 |
| Informal Support Seeking (three items) | |
| You encourage each other among caregivers.b | 0.698 |
| You ask your family, relatives and friends to listen to your worries. | 0.567 |
| You ask your family, relatives and friends to help with care for avoiding doing everything yourself. | 0.632 |
| Formal Support Seeking (four items) | |
| You seek advice from specialists: medical doctor, nurse, and social worker etc. about caregiving.b | 0.596 |
| You collect the helpful information for caregiving. | 0.634 |
| You use in-home care services actively. | 0.500 |
| You make preparation for the sudden changes in the condition of elderly person. | 0.481 |
Notes: In this table, contents of Japanese literature (Okabayashi et al., 1999) were translated into English.
χ2 (96, N = 834) = 417.912, p < 0.001; GFI = 0.925; AGFI = 0.894; RMSEA = 0.0634.
reference indicators.
standardized coefficients.
Figure A1.
The second-order factors of coping strategies.
Notes: In this figure, contents of Japanese literature (Okabayashi et al., 1999) were translated into English. PA = Positive Acceptance of Caregiving Role; KP = Keeping Their Own Pace; D = Diversion; ISS = Informal Support Seeking; FSS = Formal Support Seeking.
References
- Billings AG, Moos RH. Coping, stress, and social resources among adults with unipolar depression. Journal of Personality and Social Psychology. 1984;46:877–891. doi: 10.1037//0022-3514.46.4.877. [DOI] [PubMed] [Google Scholar]
- Borden W. Stress, coping, and adaptation in spouses of older adults with chronic dementia. Social Work Research & Abstract. 1991;27:14–21. [Google Scholar]
- Department of Health Sociology at the Tokyo Metropolitan Institute of Gerontology. A longitudinal survey on life style and health among stroke patients and their caregivers. Tokyo, Japan: Tokyo Metropolitan Institute of Gerontology; 1994. [Google Scholar]
- Dura JR, Stukenberg KW, Kiecolt-Glaser JK. Chronic stress and depressive disorders in older adults. Journal of Abnormal Psychology. 1990;99:284–290. doi: 10.1037//0021-843x.99.3.284. [DOI] [PubMed] [Google Scholar]
- Farkas JI, Himes CL. The influence of caregiving and employment on the voluntary activities of midlife and older women. Journal of Gerontology: Social Sciences. 1997;52B:S180–S189. doi: 10.1093/geronb/52b.4.s180. [DOI] [PubMed] [Google Scholar]
- Finkel SE. Causal analysis with panel data. CA, USA: Sage publications; 1995. [Google Scholar]
- Gaugler JE, Davey A, Pearlin LI, Zarit SH. Modeling caregiver adaptation over time: The longitudinal impact of behavior problems. Psychology and Aging. 2000;15:437–450. doi: 10.1037//0882-7974.15.3.437. [DOI] [PubMed] [Google Scholar]
- Haley WE, Levine EG, Brown SL, Bartolucci AA. Stress, appraisal, coping, and social support as predictors of adaptational outcome among dementia caregivers. Psychology and Aging. 1987;2:323–330. doi: 10.1037//0882-7974.2.4.323. [DOI] [PubMed] [Google Scholar]
- Hinrichsen GA, Niederehe G. Dementia management strategies and adjustment of family members of older patients. Gerontologist. 1994;34:95–102. doi: 10.1093/geront/34.1.95. [DOI] [PubMed] [Google Scholar]
- Homma A. Department of Social Welfare at the Tokyo Metropolitan Institute of Gerontology. Family caregiving for the elderly and their needs for caregiving services. Tokyo, Japan: Kouseikan; 1996. Assessment method of cognitive impairment; pp. 123–129. [Google Scholar]
- Hoyert DL, Seltzer MM. Factors related to the well-being and life activities of family caregivers. Family Relations. 1992;41:74–81. [Google Scholar]
- Kinney JM, Ishler KJ, Pargament KI, Cavanaugh JC. Coping with the uncontrollable: The use of general and religious coping by caregivers to spouses with dementia. Journal of Religious Gerontology. 2003;14:171–188. [Google Scholar]
- Knight BG, Silverstein M, McCallum TJ, Fox LS. A sociocultural stress and coping model for mental health outcomes among African American caregivers in Southern California. Journal of Gerontology. 2000;53B:142–150. doi: 10.1093/geronb/55.3.p142. [DOI] [PubMed] [Google Scholar]
- Kramer BJ. Expanding the conceptualization of caregiver coping: The importance of relationship-focused coping strategies. Family Relations. 1993;42:383–391. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Springer; 1984. [Google Scholar]
- Li WL, Seltzer MM, Greenberg JS. Change in depressive symptoms among daughter caregivers: An 18-month longitudinal study. Psychology andAging. 1999;14:206–219. doi: 10.1037//0882-7974.14.2.206. [DOI] [PubMed] [Google Scholar]
- Maslach C, Jackson SE. The measurement of experienced burnout. Journal of Occupational Behavior. 1981;2:99–113. [Google Scholar]
- Morimoto T, Schreiner AS, Asano H. Perceptions of burden among family caregivers of post-stroke elderly in Japan. International Journal of Rehabilitation Research. 2001;24:1–6. doi: 10.1097/00004356-200109000-00007. [DOI] [PubMed] [Google Scholar]
- Nakatani Y. Social Gerontology. Vol. 36. Tokyo, Japan: Tokyo Metropolitan Institute of Gerontology; 1992. Burnout among family caregiver of the frail elderly: Application of the Maslach burnout inventory; pp. 15–26. [Google Scholar]
- Nakatani Y. Department of Social Welfare at the Tokyo Metropolitan Institute of Gerontology. Family caregiving for the elderly and their needs for caregiving services. Tokyo, Japan: Kouseikan; 1996. Burden among family caregivers; pp. 266–306. [Google Scholar]
- Okabayashi H, Sugisawa H, Takanashi K, Nakatani Y, Shibata H. The factor structure of coping strategies and their effects on burnout among primary caregivers of impaired elderly person. Japanese Journal of Psychology. 1999;69:486–493. doi: 10.4992/jjpsy.69.486. [DOI] [PubMed] [Google Scholar]
- Okabayashi H, Sugisawa H, Takanashi K, Nakatani Y, Sugihara Y, Fukaya T, et al. Stress-buffering effects of coping strategies among caregivers for impaired Japanese elderly. Japanese Journal of Psychology. 2003;74:57–63. doi: 10.4992/jjpsy.74.57. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social Behavior. 1978;19:2–21. [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pratt CC, Schmall VL, Wright S, Cleland M. Burden and coping strategies of caregivers to Alzheimer’s patients. Family Relations. 1985;34:27–33. [Google Scholar]
- Pruchno RA, Resch NL. Mental health of caregiving spouses: Coping as mediator, moderator, or main effect. Psychology and Aging. 1989;4:454–463. doi: 10.1037//0882-7974.4.4.454. [DOI] [PubMed] [Google Scholar]
- Quayhagen MP, Quayhagen M. Alzheimer’s stress: Coping with the caregiving role. Gerontologist. 1988;28:391–396. doi: 10.1093/geront/28.3.391. [DOI] [PubMed] [Google Scholar]
- Schreiner AS, Morimoto T. The relationship between mastery and depression among Japanese family caregivers. International Journal of Aging and Human Development. 2003;56:301–321. doi: 10.2190/7ERL-TF1D-KW2X-3C7Y. [DOI] [PubMed] [Google Scholar]
- Shimizu Y. Department of Social Welfare at the Tokyo Metropolitan Institute of Gerontology. Family caregiving for the elderly and their needs for caregiving services. Japan: Kouseikan; 1996. Assessment method of physical disability; pp. 123–129. [Google Scholar]
- Stanton AL, Danoff-Burg S, Cameronk CL, Ellis AP. Coping through emotional approach: Problems of conceptualization and confounding. Journal of Personality and Social Psychology. 1994;66:350–362. doi: 10.1037//0022-3514.66.2.350. [DOI] [PubMed] [Google Scholar]
- Stephans MAP, Townsend AL, Martire LM, Druley JA. Balancing parent care with other roles: Interrole conflict of adult daughter caregivers. Journal of Gerontology Series B: Psychological Sciences. 2001;56:24–34. doi: 10.1093/geronb/56.1.p24. [DOI] [PubMed] [Google Scholar]
- Stone AA, Greenberg MA, Kennedy-Moore E, Newman MG. Self-report, situation-specific coping questionnaires: What are they measuring? Journal of Personality and Social Psychology. 1991;61:648–658. doi: 10.1037//0022-3514.61.4.648. [DOI] [PubMed] [Google Scholar]
- Sugihara Y, Sugisawa H, Nakatani Y, Hougham GW. Longitudinal change in the well-being of Japanese caregivers: Variations across kin relationships. Journal of Gerontology: Psychological Sciences. 2004;59B:177–184. doi: 10.1093/geronb/59.4.p177. [DOI] [PubMed] [Google Scholar]
- Sugisawa H. Introduction. In: Sugisawa H, Nakatani Y, Sugihara Y, editors. Evaluation on elderly care insurance system: From the view point of the elderly and their families. Tokyo, Japan: Sanwashobo; 2005. pp. 7–34. [Google Scholar]
- Vitaliano PP, Russo J, Young HM, Teri L, Maiuro RD. Predictors of burden in spouse caregivers of individuals with Alzheimer’s Disease. Psychology and Aging. 1991;6:392–402. doi: 10.1037//0882-7974.6.3.392. [DOI] [PubMed] [Google Scholar]
- Wake (Midorikawa) J. Social Gerontology. Vol. 37. Tokyo, Japan: Tokyo Metropolitan Institute of Gerontology; 1993. Coping styles of family caregivers for impaired elderly; pp. 16–26. [Google Scholar]
- Wake J, Yatomi N, Nakatani Y, Shimizu Y. Social Gerontology. Vol. 39. Tokyo, Japan: Tokyo Metropolitan Institute of Gerontology; 1994. Coping styles of family caregiver for the impaired elderly: The impact of coping styles on caregiver burnout and implications for social work intervention; pp. 23–34. [Google Scholar]
- Wake J. Department of Social Welfare in Tokyo Metropolitan Institute of Gerontology. Family caregiving for the elderly and their needs for caregiving services. Tokyo, Japan: Kouseikan; 1996. Coping styles and these characteristics among family caregivers; pp. 307–309. [Google Scholar]
- Wallhagen MI. Perceived control and adaptation in elder caregivers: Development of an explanatory model. International Journal of Aging and Human Development. 1993;36:219–237. doi: 10.2190/ba90-aqx3-t6ce-abek. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Schulz R. Coping with specific stressors in Alzheimer’s disease caregiving. Gerontologist. 1993;33:747–755. doi: 10.1093/geront/33.6.747. [DOI] [PubMed] [Google Scholar]
- Winslow BW. Effects of formal supports on stress outcomes in family caregivers of Alzheimer’s patients. Research in Nursing & Health. 1997;20:27–27. doi: 10.1002/(sici)1098-240x(199702)20:1<27::aid-nur4>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Wright SD, Lund DA, Caserta MS, Pratt C. Coping and caregiver well-being: The impact of maladaptive strategies. Journal of Gerontological Social Work. 1991;17:75–91. [Google Scholar]