Abstract
Background and Objectives
Primary prevention of coronary artery disease (CAD) has become a public health issue, according to increasing awareness of the substantial risks posed by asymptomatic atherosclerosis. The aims of this study were to determine the prevalence and characteristics of subclinical CAD using coronary computed tomography angiography (CCTA), and to evaluate the role of this advanced technology in identifying subclinical CAD in asymptomatic Korean individuals, compared with conventional risk stratification.
Subjects and Methods
We enrolled 4,320 consecutive asymptomatic individuals (61% males, aged 50±9 years), who underwent 64-slice CCTA during a routine health check.
Results
Coronary artery plaques were present in 1,053 (24%) individuals. Significant stenosis (diameter stenosis ≥50%) was identified in 139 (3%) subjects, and most of the significant lesions (87%) were located in the left anterior descending artery. CCTA revealed noncalcified plaques in 5% of subjects with a coronary calcium score of zero (n=801). Although 25% (n=10) of those with noncalcified plaque had significant stenosis, most of them (90%) were classified into low- or moderate-risk groups according to National Cholesterol Education Program risk stratification guidelines. In a young population (age ≤55 years for males, ≤65 years for females), 30% of subjects with significant stenosis were classified into a low-risk group and 60% had low (0 to 100) calcium scores.
Conclusion
Subclinical CAD in asymptomatic individuals cannot be ignored for its considerable prevalence, CCTA may be helpful in identifying at-risk subclinical CAD in a noninvasive manner, especially in the young and traditionally low-risk population.
Keywords: Coronary artery disease; Primary prevention; Tomography scanners, X-ray computed
Introduction
Coronary artery disease (CAD) is the single most common cause of death in American men and women.1) After decades of declining CAD death rates, the incidence of acute coronary syndromes has continued to rise in the United States.2) Moreover, approximately 21% of first and recurrent annual myocardial infarctions are silent.3) This has led to increased emphasis on primary prevention of atherosclerotic cardiovascular disease.
Identifying individuals at risk based on classical cardiovascular risk factors is difficult, since 25 to 50% of patients experiencing myocardial infarctions do not have any conventional Framingham risk factors.4) Specific algorithms such as those in the National Cholesterol Education Panel (NCEP) III guidelines have shown limited predictive power, especially in low-risk populations.5) Furthermore, these algorithms underestimate the risk of cardiovascular events, especially in young adults.6) For these reasons, a new screening modality for assessing risk of cardiovascular events in an asymptomatic population is necessary.
Stress testing, including treadmill exercise stress tests or single-photon emission computed tomography (SPECT) imaging, has been known to be inadequate for screening for subclinical CAD.7),8) Although coronary angiography (CAG) is generally used for diagnosing the presence of CAD9), it is undesirable for use as a screening tool in asymptomatic subjects because of its highly invasive nature. With the advent of electron-beam computed tomography (EBCT) in the 1990s, however, there have been attempts to develop coronary artery calcium score (CACS) guidelines for screening for subclinical CAD.10-15) Furthermore, coronary CT angiography (CCTA) can not only determine coronary artery calcium scores (CACSs), but also evaluate stenosis with the same resolution as conventional CAG.16) Therefore, CCTA can determine the characteristics and locations of plaques with reasonable accuracy, and its development as a modality which can replace previous diagnostic methods has been anticipated.17),18)
The purpose of this study was to determine the prevalence of CAD in an asymptomatic population using CCTA, and to discover how the conventional office-based risk stratification methods such as the National Cholesterol Education Program (NCEP) guidelines, and CACSs affect this population.
Subjects and Methods
Study population
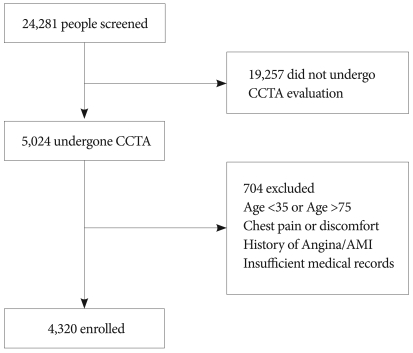
From December 2005 until February 2008, we consecutively enrolled 5,024 self-referred individuals who had undergone CCTA evaluations using 64-slice cardiac multidetector computed tomography (MDCT) during routine general health checks at Seoul National University Bundang Hospital (SNUBH). Excluded from the study analysis were 704 individuals who had chest pain or discomfort prior to enrollment, a history of myocardial infarction or angina, incomplete medical records, or were aged under 35 or over 75 years (Fig. 1). Final enrollment consisted of, 4,320 asymptomatic middle-aged individuals (2,615 men and 1,705 women; aged 50±9 years) free of known cardiovascular diseases. All subjects provided written, informed consent, and the institutional review board approved the study protocol.
Fig. 1.
Study protocol. CCTA: coronary CT angiography, AMI: acute myocardial infarction.
Risk stratification
Basic demographic and clinical data were acquired from a database maintained by the SNUBH Health Promotion Center. Framingham risk scores were calculated base on the NCEP guidelines.19) According to the revised NCEP guidelines, all subjects were assigned to three different risk groups: high-risk {coronary heart disease (CHD), CHD risk equivalents, or 10-year risk >20%}, moderate-risk (more than 2 risk factors and 10-year risk ≤20%) and low-risk group (0 to 1 risk factor).
Data acquisition
Patients with a heart rate >70 beats per minute received intravenous esmolol, 10-30 mg (Jeil Pharm. Co., Ltd., Korea) before MDCT imaging. CCTA was performed using a 64-slice MDCT scanner (Brilliance 64; Philips Medical Systems, Best, The Netherlands). A standard scanning protocol was applied, with 64×0.625 mm section collimation, 420 msec/rotation gantry speed, 120 kV tube voltage, 800 mA tube current. A bolus of 80 mL iomeprol (Iomeron 400; Bracco, Milan, Italy) was intravenously injected (4 mL/sec) followed by a 50 mL saline chaser.
A region of interest was placed within the lumen of the descending thoracic aorta, and image acquisition was automatically initiated once a selected threshold {150 Hounsfield units (HU)} had been reached using bolus tracking. The patient's electrocardiogram was simultaneously recorded to allow for retrospective segmental data reconstruction. Images were initially reconstructed at the mid-diastolic phase (80% of R-R interval) of the cardiac cycle. Additional reconstructions were performed if motion artifacts were present. The mean radiation exposure of CTA was 13.2±0.8 mSv (13.2±0.8 for males and 13.3±0.8 for females).
Image analysis
All scans were independently analyzed using 3-dimensional workstation (Brilliance; Philips Medical Systems, Best, The Netherlands), by each of two experienced investigators, who were blinded to the clinical information. After the independent evaluations, a consensus interpretation was made to obtain the final MDCT diagnosis. Each lesion was identified using a multiplanar reconstruction (MPR) technique and maximum intensity projection (MIP) of the short-axis, 2-chamber, and 4-chamber views.
The contrast-enhanced portion of the coronary lumen was semiautomatically traced at the site of maximum stenosis. The luminal diameters of the maximal stenotic site were compared with the mean value of proximal and distal reference sites. If the image was inadequate or of poor quality, coronary segments were visually scored to grade coronary artery stenosis. The severity of diameter stenosis was graded as normal (0 to 24%), mild (25 to 49%), moderate (50 to 74%), and severe (≥75%) narrowing. A diameter stenosis more than 50% was defined as significant.
Coronary artery calcium score category definition
We divided the coronary artery into 15 segments and analyzed plaque characteristics, degree of coronary stenosis, and CACS from each segment. On the basis of the CACS, all plaques were categorized as follows: no, 0; mild, 0.1 to 100; moderate, 100.1 to 400; and severe calcification, >400.
Statistical analysis
Continuous variables are expressed as means±standard deviation (SD), whereas categorical variables are presented as absolute values and percentages. Differences between continuous variables were analyzed by the unpaired Student t-test, and those between categorical variables by the chi-square test or the Fisher exact test, as appropriate. A p of <0.05 was considered statistically significant. All statistical analyses were performed using Statistical Package for the Social Sciences, version 16.0.
Results
Clinical characteristics of study population
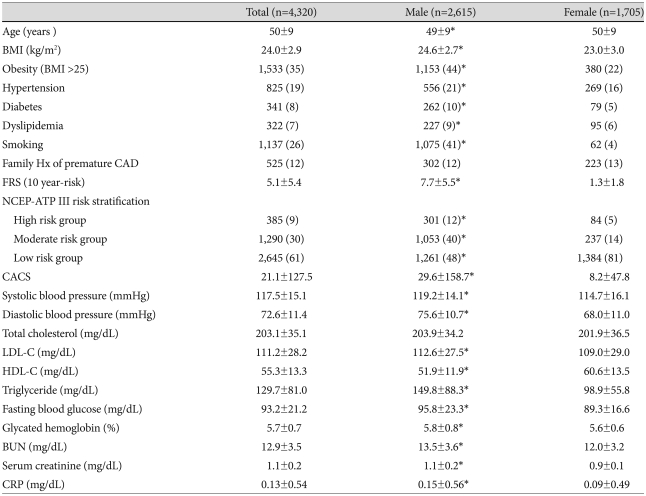
Clinical characteristics of the study population are described in Table 1.
Table 1.
Clinical characteristics of an asymptomatic study population
Data are expressed as number (%) or means±standard deviation. *p<0.05 compared with female group. BMI: body mass index, CAD: coronary artery disease, FRS: framingham risk score, NCEP-ATP: National Cholesterol Education Program-Adult Treatment Program, CACS: coronary artery calcium score, LDL-C: low density lipoprotein-cholesterol, HDL-C: high density lipoprotein-cholesterol, BUN: blood urea nitrogen, CRP: C-reactive protein
Most of the study population (n=3,935, 91%) were classified into the low- (n=2,645, 61%) or moderate- (n= 1,290, 30%) risk groups according to NCEP guidelines; whereas the high-risk group comprised 9% of the study population (n=385). Most female subjects (n=1,384, 81%) were in the low-risk group, whereas half (n=1,261, 48%) the male subjects were classified into that group.
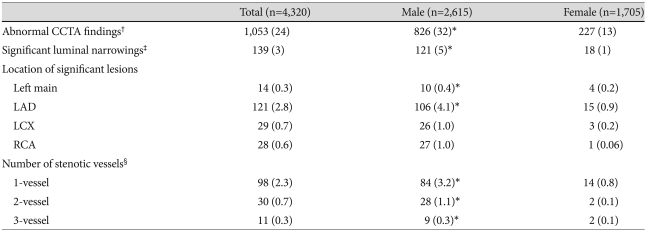
Prevalence of subclinical coronary artery disease
An abnormal finding on CCTA, defined as the presence of any plaque or a CACS greater than 0, was seen in 24% (n=1,053) of the total population. Subjects with significant stenosis (n=139) made up 3% of the total study population and 13% of the group with abnormal findings. Most of those with significant stenosis (n=121) had lesions which were located in the left anterior descending coronary artery (LAD), and 10% (n=14) had significant stenotic lesions in the left main coronary artery. While 98 subjects with significant stenosis (71%) had single-vessel disease, multi-vessel disease was found in 29% (n=41) of those with significant stenosis, or about 1% of the total population (Table 2).
Table 2.
Subclinical coronary artery disease on CCTA
Data are expressed as number (%). *p<0.05 compared with female group, †Any plaque or any abnormal coronary calcium score, ‡Luminal diameter stenosis greater than 50%, §Diseased vessel having significant luminal diameter stenosis. CCTA: coronary computed tomography angiography, LAD: left anterior descending artery, LCX: left circumflex artery, RCA: right coronary artery
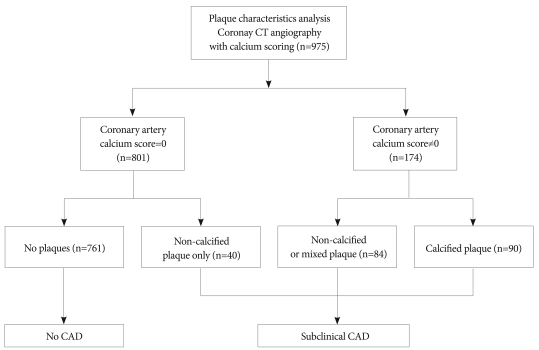
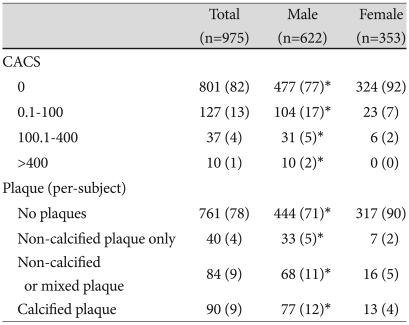
Plaque characteristics
There were 975 subjects randomly selected for plaque analysis (Fig. 2). Clinical characteristics of the selected population are described in supplemental Table 1. They were similar to the characteristics of the total study population; the population generally was at low or intermediate risk and men were more predisposed to CHD risk than women. Most subjects (n=801, 82%) had coronary calcium scores of 0, whereas 1% (n=10) of the total selected population had severe calcification (CACS >400). Similarly, there were no plaques seen in most subjects (n=761, 78%), whereas 40 individuals (4%) had noncalcified plaques only (Table 3). Although 25% (n=10) of those with noncalcified plaques had significant stenosis, 40% (n=4) of them were classified into the low-risk group according to conventional risk stratification methods (the revised NCEP guidelines).
Fig. 2.
Study population according to analysis of plaque characteristics. CAD: coronary artery disease.
Table 3.
Plaque characteristics on CCTA
Data are expressed as number (%). *p<0.05 compared with female group. CACS: coronary artery calcium score
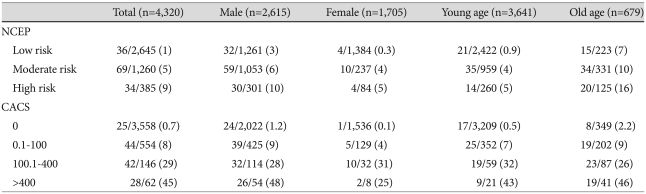
Significant subclinical coronary artery disease-prevalence and the relationship to National Cholesterol Education Program risk stratification and coronary artery calcium score according to age
As described above, the prevalence of significant subclinical CAD in this asymptomatic study population was 3% (n=139). When the total study population was divided according to age, the prevalence of significant subclinical CAD in the older age group (age >55 years for male, age >65 years for female) was higher than that in the younger age group (10% vs. 2%, respectively; p<0.001).
When subjects were divided according to NCEP risk stratification, the prevalences of significant subclinical CAD in each risk group were as follows: 1%, 5%, and 9% in low-, moderate-, and high-risk groups respectively. Especially in the low-risk population, the higher prevalences of significant subclinical CAD were seen in male subjects or subjects in the older age group {1% in total low-risk population, 3% in male, 7% in older age group (Table 4)}.
Table 4.
Prevalence of significant subclinical atherosclerosis according to NCEP-ATP III risk stratification or coronary artery calcium score
Data are expressed as number of subjects with significant subclinical atherosclerosis/number of total subjects in each subgroup (%). NCEP-ATP: National Cholesterol Education Program-Adult Treatment Panel, CACS: coronary artery calcium score
Similarly, when subjects were divided according to CACS, the prevalence of significant subclinical CAD in each categorized group (no, 0; mild, 0.1 to 100; moderate, 100.1 to 400; and severe calcification, >400) were as follows: 0.7%, 8%, 29%, and 45% in no, mild, moderate and severe calcification groups, respectively. Also, among those with a calcium score of 0, which means no calcification, the prevalence of significant subclinical CAD was about 2-fold (1.2%) greater in males and about 3-fold (2.2%) higher in the older age group than the prevalence among all subjects with coronary calcium scores of 0 (Table 4).
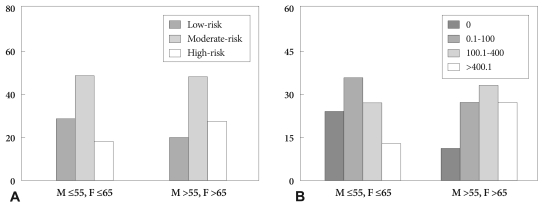
Moreover, when the group with significant stenosis (n=139) was divided according to NCEP risk stratifications, 26% (n=36) of those with significant stenosis were classified into the low-risk group, which was more pronounced in the younger age group than in older group (30% vs. 22%, respectively; p=0.356) (Fig. 3A). Also, when subjects with significant stenosis were categorized according to CACS, almost half (50%) (n=69) of them had mild calcification (CACS 0.1 to 100) or no calcification (CACS 0). In those with significant stenosis, the younger age group was shown to have less calcification (≤100 CACS) than the older age group (60% vs. 39%, respectively; p=0.046). Otherwise, 28 (20%) subjects with significant stenosis had severe calcification (CACS >400), with higher prevalence in the older age group than in the younger group (28% vs. 13%, respectively; p=0.046) (Fig. 3B).
Fig. 3.
Conventional risk stratification according to (A) NCEP risk stratification and (B) coronary artery calcium scores (CACSs), in an asymptomatic, significantly atheroscleroticsis population identified by using CCTA. NCEP: National Cholesterol Education Program, CCTA: coronary computed tomography angiography.
Discussion
The clinical characteristics of the asymptomatic study population according to gender are listed in Table 1. This table shows that men are more likely to have CHD risk factors, which makes them particularly susceptible to acute coronary syndromes. The study population generally was at low or intermediate risk, and low and intermediate risk was more frequent in females. Findings from this study should be cautiously applied, because all subjects in the study were self-referred and were drawn from the same ethnic background and geographical region. Additionally, in such a low-risk population, the prognostic accuracy of CAD screening is far from perfect, as previously reported.5),6) Hence, the incorporation of CCTA imaging data into a conventional CAD risk scoring system may improve the existing algorithms for risk stratification.
The present study revealed that the prevalence of subclinical CAD in asymptomatic individuals was not negligible. A significant percentage of the population (24%) had evidence of subclinical CAD despite the absence of symptoms, and of those, 3% (n=139) had at least one significant stenotic coronary artery. Moreover, most significant subclinical stenosis was found in the left main or proximal LAD. The presence of left main or proximal LAD atherosclerotic disease as documented by multi-slice CCTA, has been known to be associated with a worse prognosis.20)
A number of individuals with subclinical CAD or even with significant stenosis were frequently misclassified into the low-risk group by conventional risk stratification algorithms. The CACS, however, provides prognostic information over traditional risk factors, and recently was proposed as an index parameter of routine screening, especially among those with low or intermediate risk.11),12) Patients with high coronary calcium were at higher risk for obstructive and nonobstructive CAD than patients with low or zero coronary calcium, and probably for coronary events as well. Asymptomatic individuals with low calcium scores were less likely to have obstructive atherosclerosis, and the negative predictive value for predicting near-future coronary events was high (92-98%).21),22)
Then what is the additional diagnostic value of CCTA im aging compared with EBCT coronary calcium scanning? Although CACS does reflect plaque burden and consequently remains an unequivocal biomarker for the presence and extent of atherosclerotic disease,10),11) EBCT alone cannot detect noncalcified or mixed plaques. However, CCTA can not only document the presence of coronary atherosclerosis, but also can provide comprehensive information on CAD, including location, severity, and plaque characteristics, as demonstrated in a previous study.18) In the of those present study, asymptomatic subjects usually had negative findings by coronary calcium scanning, but 5% found by CCTA were seen to have noncalcified plaques, and the presence of noncalcified plaques was the only manifestation of subclinical CAD. Our result is consistent with other previous studies showing a considerable prevalence of noncalcified plaques.23),24) Despite the high known negative predictive value of CACS for coronary events, a low or even zero calcium score does not rule out significant subclinical atherosclerosis. Particularly in young adults, significant atherosclerosis can be present without any detectable calcium, which implies that there is a possibility that conventional CACS used as a screening tool could underestimate subclinical CAD, especially in the young age group. Therefore, comprehensive coronary imaging using CCTA to assess total coronary plaque burden and characteristics may be superior to simple calcium scoring.
Multidetector CCTA has been reported to have sufficient diagnostic accuracy for significant coronary artery stenosis, with 90% sensitivity, 94% specificity, and 95% negative predictive value.25) However, the positive and negative predictive values of CCTA are dependent on the pretest probability of disease, so that the diagnostic accuracy of CCTA substantially declines in the asymptomatic low risk population. Apart from diagnostic utility, CCTA still has some important limitations as a screening tool. First, CCTA cannot provide functional information, and there have been few studies to demonstrate that CCTA-guided early treatment improves outcomes. Also, cost-effectiveness and radiation hazards should be taken into consideration when performing CT screening.
In conclusion, noninvasive CCTA imaging detected considerable subclinical CAD, even in the young or traditionally low-risk population. Although there have been few studies showing that CCTA imaging in asymptomatic subjects will result in better risk stratification and improvement of outcomes compared with calcium scoring alone CCTA imaging of coronary plaques may provide better insight into subclinical CAD. However, additional studies should be carried out before integrating CCTA into the overall assessment of cardiac risk and employing it as a cost-effective method for guiding the provision of expensive and prolonged preventive therapy.
To identify asymptomatic patients at risk for acute ischemic events more accurately, we should reinforce the existing guidelines for screening, especially in the young and traditionally low-risk population, and also avoid recommending unproven therapies or expensive tests based on CT technology that is still evolving.
Acknowledgments
This work was financially supported by grants from The Korean Society of Cardiology in 2006.
Supplement
Supplemental Table 1. Clinical characteristics of population randomly selected for plaque analysis
Data are expressed as number (%) or means ± standard deviation. *p<0.05 compared with female group. BMI: body mass index, CAD: coronary artery disease, FRS: Framingham risk score, NCEP-ATP: National Cholesterol Education Program-Adult Treatment Panel, CACS: coronary artery calcium score, LDL: low density lipoprotein, HDL: high density lipoprotein, BUN: blood urea nitrogen, CRP: C-reactive protein
References
- 1.National Center for Health Statistics, Centers for Disease Control and Prevention. Atlanta, Ga: centers for disease control and prevention; [Accessed May 29, 2008]. Compressed mortality file: underlying cause of death, 1979 to 2005. Available at: http://wonder.cdc.gov/mortSQL.html. [Google Scholar]
- 2.Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics-2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21–e181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 3.Boland LL, Folsom AR, Sorlie PD, et al. Occurrence of unrecognized myocardial infarction in subjects aged 45 to 65 years (the ARIC Study) Am J Cardiol. 2002;90:927–931. doi: 10.1016/s0002-9149(02)02655-3. [DOI] [PubMed] [Google Scholar]
- 4.Zelinger A, Wayhs R, Graboys TB, Tavel ME. Asymptomatic coronary artery disease: choices in evaluation. Chest. 2002;121:1684–1687. doi: 10.1378/chest.121.5.1684. [DOI] [PubMed] [Google Scholar]
- 5.Cho Y, Yoon Y, Kim J, et al. Comparison of primary prevention strategies for coronary heart disease in asymptomatic individuals: the National Cholesterol Education Program-Adult Treatment Panel III guideline versus the screening for heart attack prevention and education guideline. Korean Circ J. 2008;38:483–490. [Google Scholar]
- 6.Akosah KO, Schaper A, Cogbill C, Schoenfeld P. Preventing myocardial infarction in the young adult in the first place: how do the National Cholesterol Education Panel III guidelines perform? J Am Coll Cardiol. 2003;41:1475–1479. doi: 10.1016/s0735-1097(03)00187-6. [DOI] [PubMed] [Google Scholar]
- 7.Froelicher VF, Thompson AJ, Longo MR, Jr, Triebwasser JH, Lancaster MC. Value of exercise testing for screening asymptomatic men for latent coronary artery disease. Prog Cardiovasc Dis. 1976;18:265–276. doi: 10.1016/0033-0620(76)90022-0. [DOI] [PubMed] [Google Scholar]
- 8.Pilote L, Pashkow F, Thomas JD, et al. Clinical yield and cost of exercise treadmill testing to screen for coronary artery disease in asymptomatic adults. Am J Cardiol. 1998;81:219–224. doi: 10.1016/s0002-9149(97)00871-0. [DOI] [PubMed] [Google Scholar]
- 9.Thaulow E, Erikssen J, Sandvik L, Erikssen G, Jorgensen L, Cohn PF. Initial clinical presentation of cardiac disease in asymptomatic men with silent myocardial ischemia and angiographically documented coronary artery disease. Am J Cardiol. 1993;72:629–633. doi: 10.1016/0002-9149(93)90875-d. [DOI] [PubMed] [Google Scholar]
- 10.Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area: a histopathologic correlative study. Circulation. 1995;92:2157–2162. doi: 10.1161/01.cir.92.8.2157. [DOI] [PubMed] [Google Scholar]
- 11.Arad Y, Spadaro LA, Goodman K, Newstein D, Guerci AD. Prediction of coronary events with electron beam computed tomography. J Am Coll Cardiol. 2000;36:1253–1260. doi: 10.1016/s0735-1097(00)00872-x. [DOI] [PubMed] [Google Scholar]
- 12.Rumberger JA, Brundage BH, Rader DJ, Kondos G. Electron beam computed tomographic coronary calcium scanning: a review and guidelines for use in asymptomatic persons. Mayo Clin Proc. 1999;74:243–252. doi: 10.4065/74.3.243. [DOI] [PubMed] [Google Scholar]
- 13.Budoff MJ, Shaw LJ, Liu ST, et al. Long-term prognosis associated with coronary calcification: observations from a register of 25,253 patients. J Am Coll Cardiol. 2007;49:1860–1870. doi: 10.1016/j.jacc.2006.10.079. [DOI] [PubMed] [Google Scholar]
- 14.Naghavi M, Falk E, Hecht HS, et al. From vulnerable plaque to vulnerable patient: part III. executive summary of the screening for Heart Attack Prevention and Education (SHAPE) Task Force report. Am J Cardiol. 2006;98:2H–15H. doi: 10.1016/j.amjcard.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 15.Kim KS. Imaging markers of subclinical atherosclerosis. Korean Circ J. 2007;37:1–8. [Google Scholar]
- 16.Achenbach S. Computed tomography coronary angiography. J Am Coll Cardiol. 2006;48:1919–1928. doi: 10.1016/j.jacc.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 17.Choi YS, Youn HJ, Jung SE, et al. The association between coronary artery calcification on MDCT and angiographic coronary artery stenosis. Korean Circ J. 2007;37:167–172. [Google Scholar]
- 18.Choi EK, Choi SI, Rivera JJ, et al. Coronary computed tomography angiography as a screening tool for the detection of occult coronary artery disease in asymptomatic individuals. J Am Coll Cardiol. 2008;52:357–365. doi: 10.1016/j.jacc.2008.02.086. [DOI] [PubMed] [Google Scholar]
- 19.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 20.Min JK, Shaw LJ, Devereux RB, et al. Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol. 2007;50:1161–1170. doi: 10.1016/j.jacc.2007.03.067. [DOI] [PubMed] [Google Scholar]
- 21.Watkins SP, Andrews TC. Guidelines for interpretation of electron beam computed tomography calcium scores from the Dallas Heart Disease Prevention Project. Am J Cardiol. 2001;87:1387–1388. doi: 10.1016/s0002-9149(01)01558-2. [DOI] [PubMed] [Google Scholar]
- 22.O'Rourke RA, Brundage BH, Froelicher VF, et al. American College of Cardiology/American Heart Association Expert Consensus document on electron-beam computed tomography for the diagnosis and prognosis of coronary artery disease. Circulation. 2000;102:126–140. doi: 10.1161/01.cir.102.1.126. [DOI] [PubMed] [Google Scholar]
- 23.Rubinshtein R, Gaspar T, Halon DA, Goldstein J, Peled N, Lewis BS. Prevalence and extent of obstructive coronary artery disease in patients with zero or low calcium score undergoing 64-slice cardiac multi-detector computed tomography for evaluation of a chest pain syndrome. Am J Cardiol. 2007;99:472–475. doi: 10.1016/j.amjcard.2006.08.060. [DOI] [PubMed] [Google Scholar]
- 24.Cheng VY, Lepor NE, Madyoon H, Eshaghian S, Naraghi AL, Shah PK. Presence and severity of non-calcified coronary plaque on 64-slice computed tomography coronary angiography in patients with zero and low coronary artery calcium. Am J Cardiol. 2007;99:1183–1186. doi: 10.1016/j.amjcard.2006.12.026. [DOI] [PubMed] [Google Scholar]
- 25.Ehara M, Surmely JF, Kawai M, et al. Diagnostic accuracy of 64-slice computed tomography for detecting angiographically significant coronary artery stenosis in an unselected consecutive patient population: comparison with conventional invasive angiography. Circ J. 2006;70:564–571. doi: 10.1253/circj.70.564. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. Clinical characteristics of population randomly selected for plaque analysis
Data are expressed as number (%) or means ± standard deviation. *p<0.05 compared with female group. BMI: body mass index, CAD: coronary artery disease, FRS: Framingham risk score, NCEP-ATP: National Cholesterol Education Program-Adult Treatment Panel, CACS: coronary artery calcium score, LDL: low density lipoprotein, HDL: high density lipoprotein, BUN: blood urea nitrogen, CRP: C-reactive protein